Abstract
Breast milk iodine concentration (BMIC) can be different when median urinary iodine concentration (UIC) is similar. The BMIC, UIC/creatinine (Cr), estimated 24-h urinary iodine excretion (24-h UIE) of lactating women in Taiwan is unknown. This study enrolled lactating women from Taipei Veterans General Hospital (August 2021–February 2023). Each participant provided a random spot urine sample, two breast milk samples, a blood sample, and completed a food frequency questionnaire on the same day. Iodine measurement was performed by inductively coupled plasma mass spectrometry. The median UIC of the enrolled 71 women was 91.1 μg/L, indicating insufficient iodine status; however, the median BMIC was 166.6 μg/L and this suggested that the amount of iodine delivered through breast milk was adequate for the breastfed infants. BMIC was correlated with UIC/Cr and 24-h UIE (both rs = 0.49) but not with UIC (rs = 0.18) or thyroid stimulating hormone (rs = 0.07). Women who did not consume dairy products (adjusted odds ratio: 24.41, 95% confidence interval: 1.26–471.2) and multivitamins (adjusted odds ratio: 8.26, 95% confidence interval: 1.76–38.79) were at increased odds for having lower BMIC. The results suggest that measuring maternal UIC alone may not be sufficient, as BMIC, UIC/Cr, and 24-h UIE are all important biomarkers. Ingestion of dairy products and multivitamins were independently associated with BMIC.
1. Introduction
Iodine is especially vital in pregnancy and early life to ensure the fetus’s and infant’s growth and neurodevelopment [1,2]. The World Health Organization recommended a daily intake of 250 μg iodine for pregnant and lactating women, which is higher than that for general adults who need 150 μg per day [3]. The current standard to assess iodine nutritional status in both lactating mothers and breastfed infants is to use the median urinary iodine concentration (UIC), where values ≥100 μg/L indicate iodine sufficiency [3,4]. This value is much lower than the recommended dietary allowances because iodine is secreted into breast milk, unlike the usual condition when 90% of dietary iodine is excreted into the urine [4,5,6,7].
In order to determine infants’ iodine status, assessing their median UIC is important but this may be compromised by difficulties in sample collection [3,4]. According to a recent meta-analysis, the iodine nutritional status of breastfed infants can be reflected by the median breast median iodine concentration (BMIC) [8]. Assessing maternal UIC alone can be misleading because studies have shown that BMIC can be completely different in exclusively breastfeeding women with similar maternal UIC and that populations with maternal median UIC ≥100 μg/L may still have inadequate BMIC values [9,10]. The correlation between BMIC and UIC has not always been consistent in the literature [11,12,13]. While UIC may be affected by maternal fluid intake, maternal UIC adjusted by creatinine (UIC/Cr) or estimated 24-h urine iodine excretion (24-h UIE) has been proposed to be better predictors of BMIC, but relevant literature is limited [12,14,15].
In our previous study evaluating iodine status of lactating women in Taiwan, the maternal median UIC of those who fed their babies with more breast milk (>50%) was lower than the other two groups who fed their babies with 50% or less than 50% of breast milk (UIC: 86.1, 118.2, and 154.1 μg/L for breast milk >50%, 50%, and <50%, p = 0.004) [16]. Infant diet composition (breastfed percentage) was significantly associated with maternal UIC < 100 μg/L in multivariable analysis. The possible loss of iodine from breastfeeding may contribute to the result, but unfortunately, BMIC was not measured in that study [16]. The correlation between maternal UIC, UIC/Cr, 24-h UIE, and BMIC is uncertain in Taiwan, an area with borderline iodine adequacy. The study aims to determine the BMIC in lactating women in Taiwan and to explore the association between maternal UIC, UIC/Cr, 24-h UIE, dietary habits and thyroid function with BMIC.
2. Materials and Methods
2.1. Study Design and Sample Collection
This cross-sectional, hospital-based study enrolled lactating women aged 20 years or above who visited Taipei Veterans General Hospital for routine checkups during the postpartum 15- to 90-day period, from August 2021 to February 2023. Women who were diagnosed with hypothyroidism, hyperthyroidism, and those who were taking anti-thyroid drugs or levothyroxine were excluded. All samples were collected on the same day, including a random spot urine sample for measurement of UIC and Cr, two random breast milk samples (one from each breast) for determination of BMIC, and a blood sample for measurement of thyroid stimulating hormone (TSH), free T4, anti-thyroglobulin antibodies (aTG), and anti-thyroid peroxidase antibodies (aTPO). A simple food frequency questionnaire (FFQ) was completed on the day of sample collection. This study was approved by the local Institutional Review Board (IRB No: 2021-06-006B). Written informed consent was obtained from all participants prior to enrollment.
2.2. Iodine and Thyroid Function Measurements
All samples were kept frozen at −20 °C after being collected. Urine samples were thawed at room temperature and breast milk samples were heated in the oven at 40 °C for 20 min before analysis. Urinary and breast milk iodine measurements were performed using an Agilent 7700 Series inductively coupled plasma mass spectrometry system as previously described [17,18]. Whole milk powder reference material (National Institute of Standards and Technology, NIST, 1549 non-fat milk powder purchased from NIST, Washington, DC., USA), urine reference material (REF 8847, REF 8849 purchased from RECIPE Co. Munich, Germany), and human urine samples from the Ensuring the Quality of Urinary Iodine Procedures program (Centers for Disease Control and Prevention, Washington DC, USA) were measured in each run for quality control. The limit of detection for urinary iodine measurement was 1.0 μg/L and for breast milk analysis was 0.78 μg/L [17,18].
Serum TSH, free T4, aTG, and aTPO were measured by an electrochemiluminescence immunoassay (cobas e 801; Roche Diagnostics GmbH., Mannheim, Germany). The reference value of aTG and aTPO is <115 IU/mL and <60 U/mL, respectively. The reference value of TSH is 0.27–4.20 uIU/mL and free T4 is 0.93–1.7 ng/dL. The department of pathology and laboratory medicine of the hospital was commissioned to test for urine Cr (Roche Cobas c 701, Roche Diagnostics GmbH., Mannheim, Germany). The estimated 24-h UIE was calculated as: UIC/Cr (μg/g) × predicted 24-h Cr (g/day) [19,20,21]. The predicted 24-h Cr (g/day) = 0.00163 × [140 − age (years)] × [weight (kg)1.5 × height (cm)0.5] × [1.429 − 0.0198 × body mass index (kg/m2)]/1000 [20,21].
2.3. Food Frequency Questionnaire
The FFQ was similar to that which had been previously described [16]. It contained questions surveying the frequency of consumption of iodine-containing food types, whether it was 1, 3, 5, 7 days per week, or never. The food types included (1) seaweeds, (2) fish, (3) seafood (except fish), (4) dairy foods, (5) multivitamins, and (6) iodized salt. Participants viewed an illustrated chart of multivitamins and postpartum nourishment diets to identify the brands. Information on breastfeeding conditions was also collected.
2.4. Statistical Analysis
UIC, UIC/Cr, 24-h UIE and BMIC were not normally distributed and were presented as median with inter-quartile range, while the other continuous variables were expressed as mean ± standard deviation. The Mann-Whitney U test was performed for comparison of continuous variables. The categorical variables were presented as numbers with percentages and analyzed by the Spearman’s Chi-square test. Variables with a p-value < 0.2 in univariable analysis were further analyzed in multivariable logistic regression models to determine the risk factors for lower median BMIC. In multivariable analysis, the Akaike information criterion was used to compare the goodness-of-fit of different models. The relationship between UIC, UIC/Cr, 24-h UIE, BMIC, and TSH was assessed by the Spearman’s rank correlation test. All data analyses were performed using the SAS software, version 4.9. A two-tailed p-value of <0.05 was considered statistically significant.
3. Results
3.1. Baseline Characteristics
The characteristics of the study population are shown in Table 1. A total of 71 women, with a mean age of 34.0 ± 4.1 years old (range: 25–44 years), were enrolled at a mean of 44.8 ± 9.4 days postpartum. Among them, 23.9% (n = 17) of the women were exclusively breastfeeding and most of them (n = 58, 81.7%) were not under a postpartum nourishment diet.

Table 1.
Characteristics of the study population.
The consumption frequency of various iodine-containing food types is presented in Table 2. Dairy products were the most frequently consumed food type whereas seafood, fish, and seaweeds were less frequently eaten. The consumption frequency of multivitamins varied, with 28.2% (n = 20) of the women taking a multivitamin every day, some ingesting it occasionally (19.7%, n = 14), while the remaining 52.1% (n = 37) never took multivitamins.

Table 2.
The result of FFQ: number of days per week in consuming various foods.
3.2. Iodine Concentration Analysis
The median UIC, UIC/Cr and 24-h UIE of the study population were 91.1 μg/L (IQR: 42.6–145.0 μg/L), 132.8 μg/g (IQR: 86.7–214.1 μg/g) and 138.0 μg/day (IQR: 88.2–234.2 μg/day), respectively (Table 1). The overall median BMIC was 166.6 μg/L (IQR: 116.9–256.9 μg/L) and the results were similar between the right and left breast (right: 165.8 μg/L, IQR: 112.3–266.7 μg/L; left: 177.9 μg/L, IQR: 112.8–278.3 μg/L). No variables were significantly associated with lower UIC (Supplementary Table S1). Variables associated with lower median BMIC <166.6 μg/L were analyzed, and the results showed that lower UIC/Cr (p < 0.001), lower 24-h UIE (p < 0.001), intake of seafood (p = 0.004) and no ingestion of multivitamins (p = 0.008) were significantly associated with lower median BMIC (Table 3).

Table 3.
The proportion of women with BMIC ≥ or < 166.6 μg/L.
In multivariable logistic regression models, intake of seafood [adjusted odds ratio (OR): 16.0, 13.3, 12.2, 12.1; 95% confidence interval (CI): 2.3–111.4, 2.9–60.7, 2.3–66.2, 2.1–70.9], no ingestion of dairy products (adjusted OR: 24.41, 11.38, 17.07, 20.07; 95% CI: 1.26–471.2, 1.09–119.19, 1.21–240.44, 1.23–328.54) and no intake of multivitamins (adjusted OR: 8.26, 5.22, 5.62, 7.28; 95% CI: 1.76–38.79, 1.47–18.58, 1.44–21.96, 1.74–30.37) were independently associated with BMIC <166.6 μg/L in all models; whereas UIC (adjusted OR: 0.99; 95% CI: 0.98–1.0) in model two, UIC/Cr (adjusted OR: 0.98; 95% CI: 0.97–0.99) in model three and 24-h UIE (adjusted OR: 0.98; 95% CI: 0.97–0.99) in model four were also independent risk factors (Table 4).

Table 4.
Multivariable analysis of factors associated with lower median BMIC.
Characteristics of lactating women who exclusively breastfed were presented in Table 5. Compared to the women who fed their babies with both breast milk and infant formula, the UIC/Cr values of the exclusively breastfeeding women (103.0 μg/g vs. 145.9 μg/g, p = 0.04) were significantly lower, but the other variables, including UIC, 24-h UIE, and BMIC were not significantly different.

Table 5.
Characteristics of lactating women who exclusively breastfed.
3.3. Correlation between UIC, BMIC and Thyroid Function
The result of the correlation analysis is presented in Figure 1. BMIC was correlated with UIC/Cr (rs = 0.49, p < 0.001), Figure 1b, and 24-h UIE (rs = 0.49, p < 0.001), Figure 1c, but not correlated with UIC (rs = 0.18, p = 0.14), Figure 1a and TSH (rs = 0.07, p = 0.55), Figure 1d.
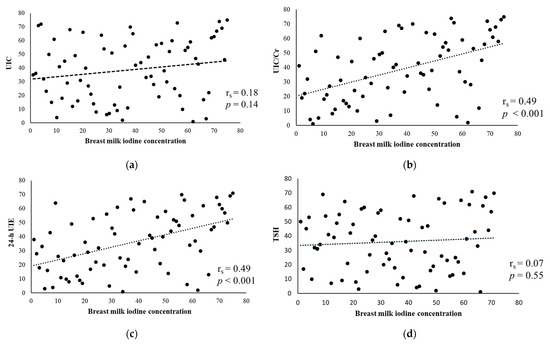
Figure 1.
Scatter plots of the correlation between BMIC and (a) UIC, urinary iodine concentration; (b) UIC/Cr, urinary iodine concentration/creatinine; (c) 24-h UIE, 24-h urinary iodine excretion; (d) TSH, thyroid stimulating hormone.
4. Discussion
This is the first time data on maternal UIC, UIC/Cr, 24-h UIC and BMIC were reported in an area with borderline iodine adequacy. The median UIC, UIC/Cr, 24-h UIE, and BMIC were 91.1 μg/L, 132.8 μg/g, 138.0 μg/day and 166.6 μg/L, respectively. The median UIC value was <100 μg/L in the study population, and this indicates insufficient maternal iodine status [3,4]. However, the median BMIC was ≥100 µg/L and this suggests that the iodine supply in the breast milk is sufficient for the breastfed infants [10,22,23,24,25,26]. The values of UIC/Cr and 24-h UIE were higher than the UIC value and better correlated with BMIC. There was no correlation between TSH and BMIC, and the maternal UIC value in the study population was considered sufficient to maintain euthyroidism [27,28]. Risk factors related to lower median BMIC included intake of seafood, no ingestion of dairy products and multivitamins.
Measuring infant UIC is the gold standard for assessing infant iodine status, but this measurement can be biased by difficulties in sample collection [3,4]. For exclusively breastfed infants, the supply of iodine relies solely on the iodine in breast milk. A significant correlation between BMIC and infant UIC has been demonstrated and this makes BMIC a promising biomarker [22,29,30]. Based on the average lactation volume of 670 mL in the Asian population, the estimated average iodine amount in breast milk of the study population is 111.6 μg/day (IQR: 78.3–172.1), which is sufficient for infants aged 0–6 months in general (adequate intake: 110 μg/day) [3,31]. In this study, the median BMIC of the exclusively breastfed infant group was 138.3 µg/L and the calculated infant’s iodine intake from breast milk was 121.7 μg per day, based on the average breast milk intake of exclusively breastfed infants of 880 mL/day [3,31]. Assuming that 90% of the ingested iodine is secreted into breast milk or urine, the estimated maternal iodine intake is 277 μg/day [(24-h UIE 138.0 μg/day + iodine amount in breast milk 111.6 μg/day) ÷ 90%], which is higher than the recommended intake of 250 μg/day for lactating women [3]. Although the median UIC value suggests insufficient maternal iodine status, the estimated maternal iodine intake meets the current recommendation after considering the amount of iodine secreted into breast milk.
Studies have shown that the UIC in spot urine samples can be largely influenced by the amount of fluid intake, and the values present high day-to-day variability [14,15,32]. The 24-h UIE has been regarded as the gold standard, but the time required and inconvenience in sample collection limit its widespread use in population studies [32,33,34]. The UIC adjusted by Cr in spot urine samples, or the estimated 24-h UIE, emerged as alternatives to overcome these limitations [14,15]. It has been shown that UIC/Cr can more precisely reflect iodine intake in non-lactating subjects [33,35]. In breastfeeding women, BMIC can be better predicted by maternal UIC/Cr and 24-h UIE, while UIC generally has no correlation with BMIC [11,12,13]. The result of the current study implies that the iodine supply to the breastfed infants is more reliably evaluated by BMIC, maternal UIC/Cr, and estimated 24-h UIE, but not by maternal UIC value.
In areas with sufficient iodine intake, the median BMIC and UIC can both be ≥100 μg/L; in places with low iodine intake, the BMIC and UIC can both be <100 μg/L rendering the breastfed infants at risk for iodine deficiency. In an area with borderline iodine adequacy such as Taiwan, the median BMIC and UIC values can be discrepant [9,11,12,13,15,23,24,30,36,37,38]. Maternal fluid intake is one of the reasons; another possible explanation is the preferential secretion of iodine into breast milk when iodine intake is at the border for adequacy [9,15]. According to the Nutrition and Health Survey in Taiwan, the median UIC was 100 μg/L for adults over 19 years old in 2005–2008, 96 μg/L for people aged over 6 years in 2013, and 104 μg/L for adults over 19 years old in 2017–2020 [39,40,41]. The change of salt iodization policy from mandatory to voluntary after Taiwan joined the World Trade Organization in 2002 contributed to the mildly deficient or borderline adequate iodine status in the past 20 years [39,40,41]. To ensure adequate iodine nutrition to the breastfed infants, absorbed dietary iodine can be partitioned more into breast milk under the regulation of prolactin and other hormones through the sodium-iodide symporter [42,43]. At the expense of maternal iodine reserve and lower UIC value, this compensates for the slightly inadequate maternal iodine status and provides sufficient iodine supply to the breastfed infants [42].
Universal salt iodization has been recommended since 1993 [44]; nevertheless, most of the available salts in the market in Taiwan are non-iodized [45]. In the current study, only half of the women used iodized salt, and the common phenomenon of eating non- self-prepared foods made salt an unstable source of iodine nutrition. Iodine-containing foods and supplements were therefore very important. In this study, women who did not ingest dairy products had an increased chance of having a lower BMIC, and this finding was compatible with other studies that demonstrated lower BMIC in women with less intake of dairy products [38,46]. In a survey measuring iodine content in 76 samples of milk types in Taiwan, the iodine concentrations of whole milk, low-fat milk, flavored milk drinks, and milk alternative drinks were determined to be 210.4 μg/L, 263.2 μg/L, 100.0 μg/L, and 65.6 μg/L on average [47]. Drinking a carton of whole milk or low-fat milk (400 c.c.) would provide one-third of the daily iodine requirement for lactating women, and this should be regarded as an important dietary source of iodine nutrition.
Interestingly, women who ingested seafood were also at increased odds for lower BMIC, which is in contrast to the common understanding that seafood is a type of iodine-rich food. It is possible that women did not ingest seafood in amounts sufficient to supply much iodine and it is also reasonable to think that when women ingest seafood in larger amounts, the intake frequency of other iodine-containing food types became less. Unfortunately, the amount of iodine ingested from seafood could not be determined in the current study because there was no information about the portion size in the FFQ, and the iodine content in seafood is still unknown in Taiwan.
In order to provide sufficient iodine nutrition to breastfed infants, the American Thyroid Association has recommended that lactating women, similar to pregnant women, should ingest iodine supplements containing 150 μg iodine per day [48]. Studies have demonstrated that BMIC tends to be higher in women with habitual intake of iodine supplement [15,36]. Among the women who took multivitamins in this study, 70.4% of them took the brands that contained iodine, which should result in higher iodine levels in breast milk. Non-consumption of multivitamins was an independent predictor of lower median BMIC in the study population, and based on this result, iodine supplementation during lactation could be recommended.
It is part of the traditional Chinese culture that women receive specialized postpartum care and ingest a postpartum nourishment diet for 15–45 days after delivery [49,50]. In our previous study evaluating the iodine status of lactating women, the time of enrollment was 13.6 days after delivery, and 74% of the women were ingesting a postpartum nourishment diet, which was significantly higher than 18.3% in this study when women were enrolled at 44.8 days after delivery [16]. Fish and seafood are not common food types in daily life in Taiwan but appear very often in the postpartum nourishment diet. All these factors taken into account together contributed to the differences in iodine intake in women in these two studies, and thus the difference in median UIC (120.4 μg/L vs. 91.1 μg/L) [16].
There are several limitations. First, the infant’s UIC and thyroid function were not measured due to difficulties in sample collection. Second, although the present FFQ could not be used to calculate the actual amount of iodine ingested, it did, to some extent, reflect the iodine intake of the studied women. Third, this study was conducted in a tertiary referral center in the capital city and could not be generalized to other areas in Taiwan. We also did not record the time of the collection of the random urine and breast milk samples and their proximity to the last meal and breastfeeding. We acknowledge that circadian rhythm, post-meal peaks and downward trend post-breastfeeding may be potential sources for unknown bias to influence the iodine concentration in urine and breast milk [51,52].
5. Conclusions
The results of the current study suggest that BMIC, UIC/Cr, and 24-h UIE are all important biomarkers to assess iodine nutritional status in lactating women. The iodine supply to the breastfed infants could not be accurately evaluated by measuring maternal UIC alone. Ingestion of dairy products and multivitamins was independently associated with BMIC in lactating women in Taiwan.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/nu15194125/s1, Table S1: The proportion of women with UIC ≥ or <100 μg/L.
Author Contributions
Conceptualization, C.-J.H., F.-F.W., C.-C.Y. (Chang-Ching Yeh) and C.-C.Y. (Chen-Chang Yang); methodology, C.-J.H., J.-Z.L., C.-M.H., H.-S.C., F.-F.W., C.-C.Y. (Chang-Ching Yeh) and C.-C.Y. (Chen-Chang Yang); data collection, C.-J.H., J.-Z.L., C.-C.Y. (Chang-Ching Yeh) and C.-C.Y. (Chen-Chang Yang); data analysis, C.-J.H., J.-Z.L., C.-M.H., H.-S.C., F.-F.W., C.-C.Y. (Chang-Ching Yeh) and C.-C.Y. (Chen-Chang Yang); writing—original draft preparation, C.-J.H. and J.-Z.L.; funding acquisition, C.-J.H. All authors have read and agreed to the published version of the manuscript.
Funding
This research was partially supported by funding from the National Science and Technology Council, Taiwan (NSTC 111-2314-B-075-071, NSTC 112-2314-B-075-025); Taipei Veterans General Hospital (V111B-001, V112B-003); Taipei Veterans General Hospital-National Taiwan University Hospital Joint Research Program (VN112-09), and Szu-Yuan Research Foundation of Internal Medicine to C.-J.H.
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the institutional review board of Taipei Veterans General Hospital on 18 June 2021 (IRB No: 2021-06-006B).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Data are available on request from the corresponding author.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Korevaar, T.I.M.; Medici, M.; Visser, T.J.; Peeters, R.P. Thyroid disease in pregnancy: New insights in diagnosis and clinical management. Nat. Rev. Endocrinol. 2017, 13, 610–622. [Google Scholar] [CrossRef]
- Zimmermann, M.B.; Boelaert, K. Iodine deficiency and thyroid disorders. Lancet Diabetes Endocrinol. 2015, 3, 286–295. [Google Scholar] [CrossRef]
- World Health Organization; UNICEF; ICCIDD. Assessment of Iodine Deficiency Disorders and Monitoring Their Elimination. A Guide for Programme Managers, 3rd ed.; World Health Organization: Geneva, Switzerland, 2007. [Google Scholar]
- United Nations International Children’s Emergency Fund (UNICEF). Guidance on the Monitoring of Salt Iodization Programmes and Determination of Population Iodine Status. 2018. Available online: https://reurl.cc/LAO9py (accessed on 7 August 2023).
- Nath, S.K.; Moinier, B.; Thuillier, F.; Rongier, M.; Desjeux, J.F. Urinary excretion of iodide and fluoride from supplemented food grade salt. Int. J. Vitam. Nutr. Res. 1992, 62, 66–72. [Google Scholar] [PubMed]
- Jahreis, G.; Hausmann, W.; Kiessling, G.; Franke, K.; Leiterer, M. Bioavailability of iodine from normal diets rich in dairy products—Results of balance studies in women. Exp. Clin. Endocrinol. Diabetes 2001, 109, 163–167. [Google Scholar] [CrossRef] [PubMed]
- Mizokami, T.; Fukata, S.; Hishinuma, A.; Kogai, T.; Hamada, K.; Maruta, T.; Higashi, K.; Tajiri, J. Iodide Transport Defect and Breast Milk Iodine. Eur. Thyroid J. 2016, 5, 145–148. [Google Scholar] [CrossRef]
- Nazeri, P.; Kabir, A.; Dalili, H.; Mirmiran, P.; Azizi, F. Breast-Milk Iodine Concentrations and Iodine Levels of Infants According to the Iodine Status of the Country of Residence: A Systematic Review and Meta-Analysis. Thyroid 2018, 28, 124–138. [Google Scholar] [CrossRef]
- Dold, S.; Zimmermann, M.B.; Aboussad, A.; Cherkaoui, M.; Jia, Q.; Jukic, T.; Kusic, Z.; Quirino, A.; Sang, Z.; San, L.T.O.; et al. Breast Milk Iodine Concentration Is a More Accurate Biomarker of Iodine Status than Urinary Iodine Concentration in Exclusively Breastfeeding Women. J. Nutr. 2017, 147, 528–537. [Google Scholar] [CrossRef] [PubMed]
- Nazeri, P.; Dalili, H.; Mehrabi, Y.; Hedayati, M.; Mirmiran, P.; Azizi, F. Breast Milk Iodine Concentration Rather than Maternal Urinary Iodine Is a Reliable Indicator for Monitoring Iodine Status of Breastfed Neonates. Biol. Trace Elem. Res. 2018, 185, 71–77. [Google Scholar] [CrossRef]
- Pal, N.; Samanta, S.K.; Chakraborty, A.; Chandra, N.K.; Chandra, A.K. Interrelationship between iodine nutritional status of lactating mothers and their absolutely breast-fed infants in coastal districts of Gangetic West Bengal in India. Eur. J. Pediatr. 2018, 177, 39–45. [Google Scholar] [CrossRef] [PubMed]
- Pearce, E.N.; Leung, A.M.; Blount, B.C.; Bazrafshan, H.R.; He, X.; Pino, S.; Valentin-Blasini, L.; Braverman, L.E. Breast milk iodine and perchlorate concentrations in lactating Boston-area women. J. Clin. Endocrinol. Metab. 2007, 92, 1673–1677. [Google Scholar] [CrossRef]
- Ordookhani, A.; Pearce, E.N.; Hedayati, M.; Mirmiran, P.; Salimi, S.; Azizi, F.; Braverman, L.E. Assessment of thyroid function and urinary and breast milk iodine concentrations in healthy newborns and their mothers in Tehran. Clin. Endocrinol. 2007, 67, 175–179. [Google Scholar] [CrossRef] [PubMed]
- Chan, S.S.; Hams, G.; Wiley, V.; Wilcken, B.; McElduff, A. Postpartum maternal iodine status and the relationship to neonatal thyroid function. Thyroid 2003, 13, 873–876. [Google Scholar] [CrossRef]
- Andersen, S.L.; Møller, M.; Laurberg, P. Iodine concentrations in milk and in urine during breastfeeding are differently affected by maternal fluid intake. Thyroid 2014, 24, 764–772. [Google Scholar] [CrossRef] [PubMed]
- Huang, C.J.; Cheng, C.P.; Lee, L.H.; Chen, H.S.; Hwu, C.M.; Tang, K.T.; Shih, C.W.; Yeh, C.C.; Yang, C.C.; Wang, F.F. Iodine nutritional status of lactating women in northern Taiwan in 2019. J. Chin. Med. Assoc. 2021, 84, 400–404. [Google Scholar] [CrossRef]
- Huang, C.J.; Lee, L.H.; Cheng, C.P.; Chen, H.S.; Hwu, C.M.; Tang, K.T.; Shih, C.W.; Yeh, C.C.; Wang, F.F.; Yang, C.C. Analytical validation of an inductively coupled plasma mass spectrometry method for urinary iodine concentration measurements in Taiwan. J. Formos. Med. Assoc. 2023, 122, 757–765. [Google Scholar] [CrossRef] [PubMed]
- Huang, C.J.; Li, J.Z.; Hwu, C.M.; Chen, H.S.; Yeh, C.C.; Wang, F.F.; Yang, C.C. Determination of the Elemental Iodine in Human Breast Milk by Inductively Coupled Plasma Mass Spectrometry. Biol. Trace Elem. Res. 2023. [Google Scholar] [CrossRef] [PubMed]
- Kesteloot, H.; Joossens, J.V. On the determinants of the creatinine clearance: A population study. J. Hum. Hypertens. 1996, 10, 245–249. [Google Scholar]
- Perrine, C.G.; Cogswell, M.E.; Swanson, C.A.; Sullivan, K.M.; Chen, T.C.; Carriquiry, A.L.; Dodd, K.W.; Caldwell, K.L.; Wang, C.Y. Comparison of population iodine estimates from 24-hour urine and timed-spot urine samples. Thyroid 2014, 24, 748–757. [Google Scholar] [CrossRef]
- Mage, D.T.; Allen, R.H.; Kodali, A. Creatinine corrections for estimating children’s and adult’s pesticide intake doses in equilibrium with urinary pesticide and creatinine concentrations. J. Expo. Sci. Environ. Epidemiol. 2008, 18, 360–368. [Google Scholar] [CrossRef] [PubMed]
- Nazeri, P.; Dalili, H.; Mehrabi, Y.; Hedayati, M.; Mirmiran, P.; Azizi, F. Is there any difference between the iodine statuses of breast-fed and formula-fed infants and their mothers in an area with iodine sufficiency? Br. J. Nutr. 2018, 119, 1012–1018. [Google Scholar] [CrossRef] [PubMed]
- Groufh-Jacobsen, S.; Mosand, L.M.; Bakken, K.S.; Solvik, B.S.; Oma, I.; Gjengedal, E.L.F.; Brantsæter, A.L.; Strand, T.A.; Henjum, S. Mild to Moderate Iodine Deficiency and Inadequate Iodine Intake in Lactating Women in the Inland Area of Norway. Nutrients 2020, 12, 630. [Google Scholar] [CrossRef]
- Kart, P.Ö.; Türkmen, M.K.; Anık, A.; Ünüvar, T. The association of lactating mothers’ urinary and breast milk iodine levels with iodine nutrition status and thyroid hormone levels of newborns. Turk. Arch. Pediatr. 2021, 56, 207–212. [Google Scholar] [CrossRef]
- Semba, R.D.; Delange, F. Iodine in human milk: Perspectives for infant health. Nutr. Rev. 2001, 59, 269–278. [Google Scholar] [CrossRef] [PubMed]
- Nazeri, P.; Mirmiran, P.; Shiva, N.; Mehrabi, Y.; Mojarrad, M.; Azizi, F. Iodine nutrition status in lactating mothers residing in countries with mandatory and voluntary iodine fortification programs: An updated systematic review. Thyroid 2015, 25, 611–620. [Google Scholar] [CrossRef] [PubMed]
- Zimmermann, M.B.; Andersson, M. Assessment of iodine nutrition in populations: Past, present, and future. Nutr. Rev. 2012, 70, 553–570. [Google Scholar] [CrossRef]
- Charlton, K.E.; Ware, L.J.; Baumgartner, J.; Cockeran, M.; Schutte, A.E.; Naidoo, N.; Kowal, P. Iodine Status Assessment in South African Adults According to Spot Urinary Iodine Concentrations, Prediction Equations, and Measured 24-h Iodine Excretion. Nutrients 2018, 10, 736. [Google Scholar] [CrossRef] [PubMed]
- Andersson, M.; Aeberli, I.; Wüst, N.; Piacenza, A.M.; Bucher, T.; Henschen, I.; Haldimann, M.; Zimmermann, M.B. The Swiss iodized salt program provides adequate iodine for school children and pregnant women, but weaning infants not receiving iodine-containing complementary foods as well as their mothers are iodine deficient. J. Clin. Endocrinol. Metab. 2010, 95, 5217–5224. [Google Scholar] [CrossRef] [PubMed]
- Chen, Y.; Gao, M.; Bai, Y.; Hao, Y.; Chen, W.; Cui, T.; Guo, W.; Pan, Z.; Lin, L.; Wang, C.; et al. Variation of iodine concentration in breast milk and urine in exclusively breastfeeding women and their infants during the first 24 wk after childbirth. Nutrition 2020, 71, 110599. [Google Scholar] [CrossRef]
- Rios-Leyvraz, M.; Yao, Q. The Volume of Breast Milk Intake in Infants and Young Children: A Systematic Review and Meta-Analysis. Breastfeed. Med. 2023, 18, 188–197. [Google Scholar] [CrossRef] [PubMed]
- König, F.; Andersson, M.; Hotz, K.; Aeberli, I.; Zimmermann, M.B. Ten repeat collections for urinary iodine from spot samples or 24-hour samples are needed to reliably estimate individual iodine status in women. J. Nutr. 2011, 141, 2049–2054. [Google Scholar] [CrossRef]
- Vejbjerg, P.; Knudsen, N.; Perrild, H.; Laurberg, P.; Andersen, S.; Rasmussen, L.B.; Ovesen, L.; Jørgensen, T. Estimation of iodine intake from various urinary iodine measurements in population studies. Thyroid 2009, 19, 1281–1286. [Google Scholar] [CrossRef]
- Chen, W.; Wu, Y.; Lin, L.; Tan, L.; Shen, J.; Pearce, E.N.; Guo, X.; Wang, W.; Bian, J.; Jiang, W.; et al. 24-Hour Urine Samples Are More Reproducible than Spot Urine Samples for Evaluation of Iodine Status in School-Age Children. J. Nutr. 2016, 146, 142–146. [Google Scholar] [CrossRef] [PubMed]
- Kim, H.K.; Lee, S.Y.; Lee, J.I.; Jang, H.W.; Kim, S.K.; Chung, H.S.; Tan, A.H.; Hur, K.Y.; Kim, J.H.; Chung, J.H.; et al. Usefulness of iodine/creatinine ratio from spot-urine samples to evaluate the effectiveness of low-iodine diet preparation for radioiodine therapy. Clin. Endocrinol. 2010, 73, 114–118. [Google Scholar] [CrossRef] [PubMed]
- Jin, Y.; Coad, J.; Zhou, S.J.; Skeaff, S.; Benn, C.; Brough, L. Use of Iodine Supplements by Breastfeeding Mothers Is Associated with Better Maternal and Infant Iodine Status. Biol. Trace Elem. Res. 2021, 199, 2893–2903. [Google Scholar] [CrossRef] [PubMed]
- Osei, J.; Andersson, M.; Reijden, O.V.; Dold, S.; Smuts, C.M.; Baumgartner, J. Breast-Milk Iodine Concentrations, Iodine Status, and Thyroid Function of Breastfed Infants Aged 2-4 Months and Their Mothers Residing in a South African Township. J. Clin. Res. Pediatr. Endocrinol. 2016, 8, 381–391. [Google Scholar] [CrossRef]
- Petersen, E.; Thorisdottir, B.; Thorsdottir, I.; Gunnlaugsson, G.; Arohonka, P.; Erlund, I.; Gunnarsdottir, I. Iodine status of breastfed infants and their mothers’ breast milk iodine concentration. Matern. Child Nutr. 2020, 16, e12993. [Google Scholar] [CrossRef]
- Pan, W.H. Health Promotion Administration Ministry of Health and Welfare. Nutrition and Health Survey in Taiwan (NAHSIT) 2017–202. 2022. Available online: https://www.hpa.gov.tw/Pages/List.aspx?nodeid=3998 (accessed on 7 August 2023).
- Tang, K.T.; Wang, F.F.; Pan, W.H.; Lin, J.D.; Won, G.S.; Chau, W.K.; Lin, H.D.; Hsieh, Y.T. Iodine status of adults in Taiwan 2005-2008, 5 years after the cessation of mandatory salt iodization. J. Formos. Med. Assoc. 2016, 115, 645–651. [Google Scholar] [CrossRef] [PubMed]
- Wang, F.F.; Tang, K.T.; Pan, W.H.; Won, J.G.; Hsieh, Y.T.; Huang, C.J. Iodine Status of Taiwanese Population in 2013: 10 Years after Changing from Mandatory to Voluntary Salt Iodization. Food Nutr. Bull. 2018, 39, 75–85. [Google Scholar] [CrossRef] [PubMed]
- Dror, D.K.; Allen, L.H. Iodine in Human Milk: A Systematic Review. Adv. Nutr. 2018, 9, 347S–357S. [Google Scholar] [CrossRef] [PubMed]
- Azizi, F.; Smyth, P. Breastfeeding and maternal and infant iodine nutrition. Clin. Endocrinol. 2009, 70, 803–809. [Google Scholar] [CrossRef]
- Pearce, E.N. The American Thyroid Association: Statement on Universal Salt Iodization. Thyroid 2017, 27, 137. [Google Scholar] [CrossRef] [PubMed]
- Shaw, N. Monitoring iodine contents of salt products and related health risk. In Project of Food and Drug Administration Publishing Ministry of Health and Welfare in Taiwan (DOH101-FDA-31410); Food and Drug Administration: Taipei, Taiwan, 2012. [Google Scholar]
- Jorgensen, A.; O’Leary, P.; James, I.; Skeaff, S.; Sherriff, J. Assessment of Breast Milk Iodine Concentrations in Lactating Women in Western Australia. Nutrients 2016, 8, 699. [Google Scholar] [CrossRef] [PubMed]
- Chang, T.Y.; Wang, F.F.; Yang, C.C.; Liu, Y.L.; Huang, C.J. Iodine Concentration Determination in Commercial Dairy Milk and Plant-based Substitutes in Northern Taiwan. In Proceedings of the 43th Annual Meeting of the Endocrine Society and the Diabetes Association of the R.O.C., Taipei, Taiwan, 19–20 March 2022. [Google Scholar]
- Stagnaro-Green, A.; Abalovich, M.; Alexander, E.; Azizi, F.; Mestman, J.; Negro, R.; Nixon, A.; Pearce, E.N.; Soldin, O.P.; Sullivan, S.; et al. Guidelines of the American Thyroid Association for the diagnosis and management of thyroid disease during pregnancy and postpartum. Thyroid 2011, 21, 1081–1125. [Google Scholar] [CrossRef] [PubMed]
- Li, N.; Su, X.; Liu, T.; Sun, J.; Zhu, Y.; Dai, Z.; Zhang, Y.; Pan, L.; Jiang, W.; Zhu, W. Dietary patterns of Chinese puerperal women and their association with postpartum weight retention: Results from the mother-infant cohort study. Matern. Child Nutr. 2021, 17, e13061. [Google Scholar] [CrossRef] [PubMed]
- Zhao, A.; Lan, H.; Szeto, I.M.Y.; Huo, S.; Yang, Y.; Yang, J.; Zhang, Y. Traditional postpartum customs in modern urban Chinese women and its association with dietary quality. Glob. Transit. 2022, 4, 82–89. [Google Scholar] [CrossRef]
- Zhang, Y.; Zhao, X.; Shan, L.; Jia, X.; Liu, J.; Gu, W.; Zhang, Z.; Zhang, X.; Sang, Z. Variations in Breast Milk Iodine Concentration over 24 h among Lactating Women in Northern China. J. Nutr. 2023, 153, 208–214. [Google Scholar] [CrossRef] [PubMed]
- Guo, W.; Wu, W.; Gao, M.; Yang, Y.; Pearce, E.N.; Li, S.; Ren, Z.; Zhang, N.; Zhang, K.; Pan, Z.; et al. Characteristics and predictors of breast milk iodine in exclusively breastfed infants: Results from a repeated-measures study of iodine metabolism. Front. Nutr. 2022, 9, e1017744. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).