A Six-Week Follow-Up Study on the Sustained Effects of Prolonged Water-Only Fasting and Refeeding on Markers of Cardiometabolic Risk
Highlights
- Significant improvements in markers of cardiometabolic health, including total body weight, blood pressure, cholesterol, hsCRP, fatty liver index, and abdominal circumference, were observed immediately following intervention and persisted for at least six weeks.
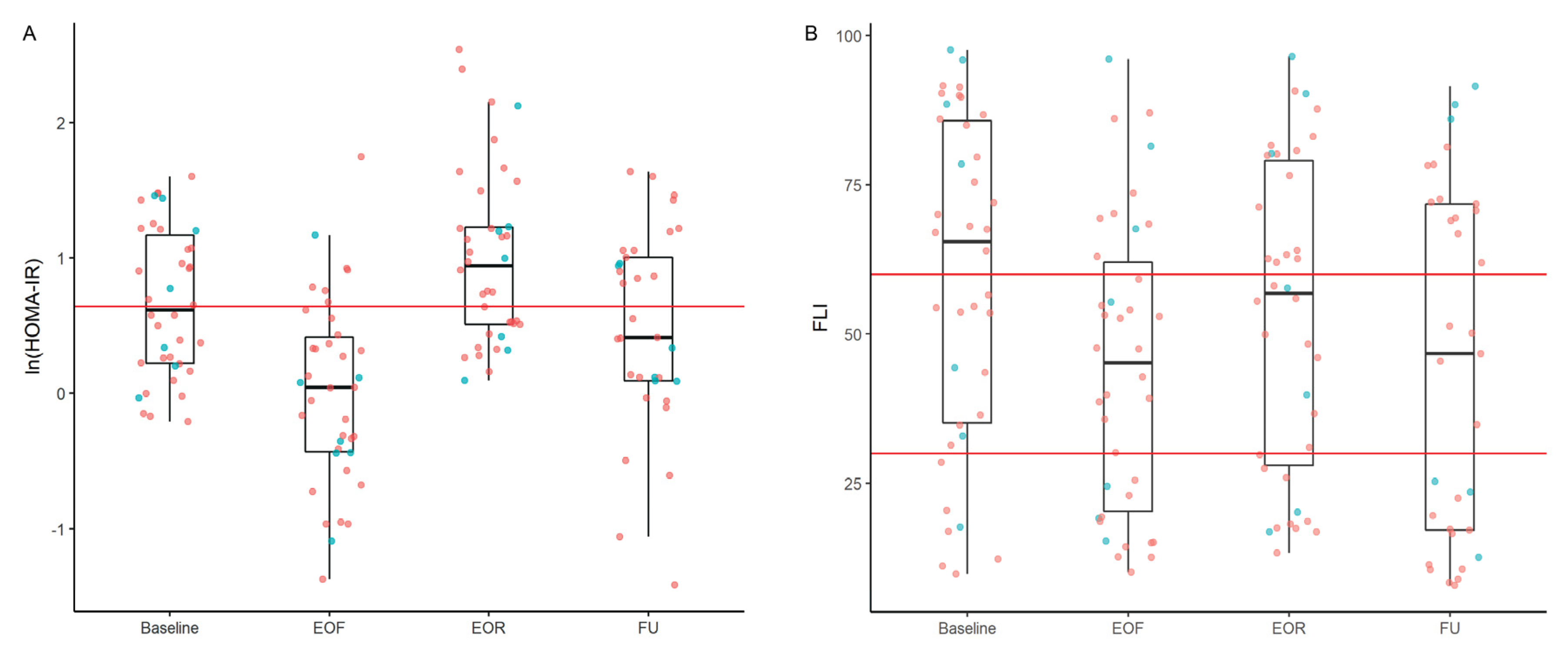
- Triglycerides and HOMA-IR temporarily increased during the refeeding phase but returned to the baseline levels within six weeks, suggesting that these changes reflect transient metabolic adaptations.
- Prolonged water-only fasting followed by a diet made of whole plant foods holds potential as a long-term strategy for managing cardiometabolic health, particularly in individuals with overweight or obesity.
Abstract
1. Introduction
2. Materials and Methods
2.1. Ethical Statement
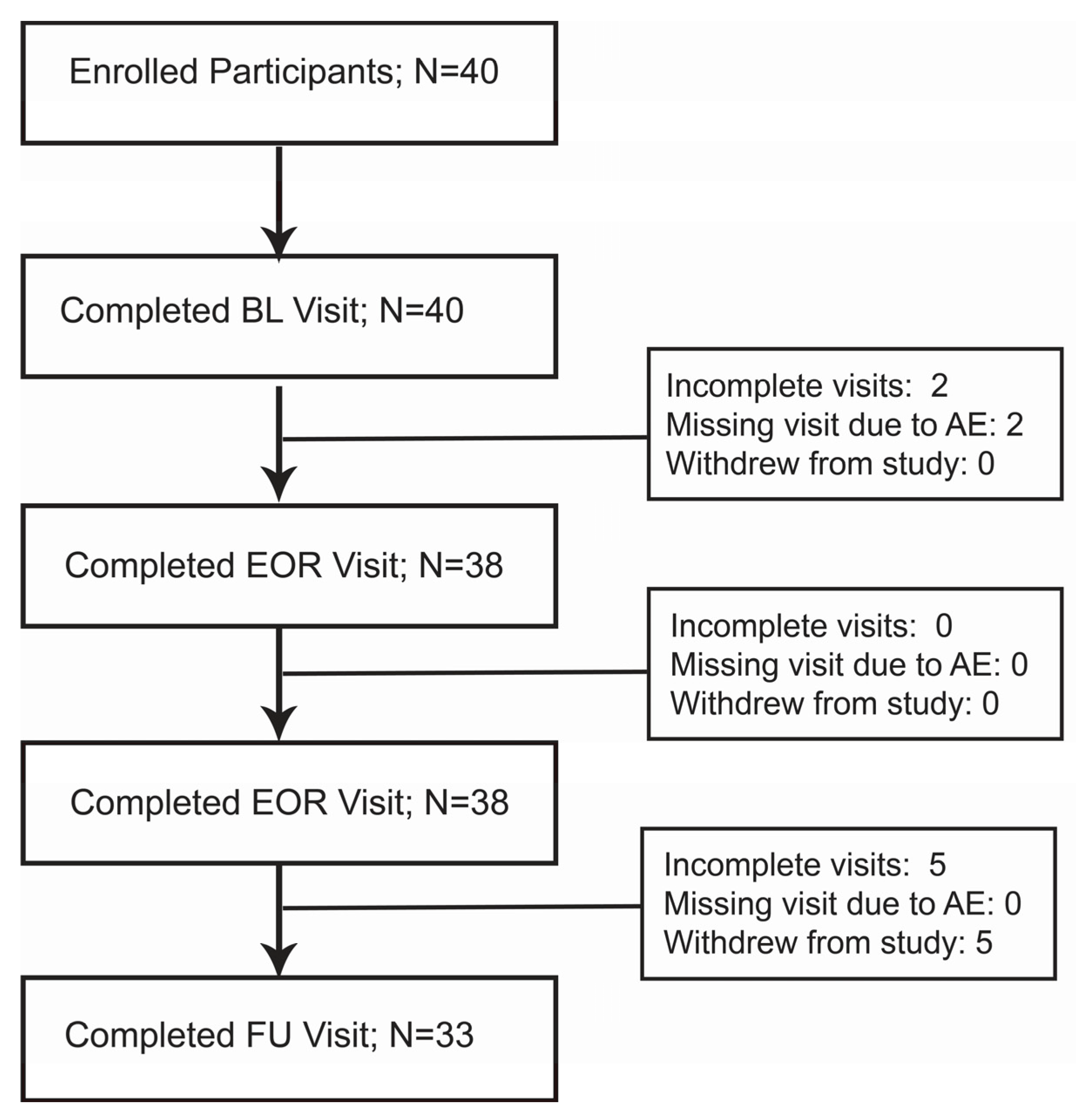
2.2. Participation and Visit Characteristics
2.3. Medically Supervised, Water-Only Fasting and Refeeding Protocol
2.4. Study Design
2.5. Clinical Measurements
2.6. Laboratory Measurements
2.7. SOS-Free Diet Screener
2.8. Statistical Analysis
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Raghupathi, W.; Raghupathi, V. An Empirical Study of Chronic Diseases in the United States: A Visual Analytics Approach. Int. J. Environ. Res. Public Health 2018, 15, 431. [Google Scholar] [CrossRef] [PubMed]
- Silveira Rossi, J.L.; Barbalho, S.M.; Reverete de Araujo, R.; Bechara, M.D.; Sloan, K.P.; Sloan, L.A. Metabolic syndrome and cardiovascular diseases: Going beyond traditional risk factors. Diabetes Metab. Res. Rev. 2022, 38, e3502. [Google Scholar] [CrossRef]
- Garcia-Garcia, F.J.; Monistrol-Mula, A.; Cardellach, F.; Garrabou, G. Nutrition, Bioenergetics, and Metabolic Syndrome. Nutrients 2020, 12, 2785. [Google Scholar] [CrossRef] [PubMed]
- Crupi, A.N.; Haase, J.; Brandhorst, S.; Longo, V.D. Periodic and Intermittent Fasting in Diabetes and Cardiovascular Disease. Curr. Diabetes Rep. 2020, 20, 83. [Google Scholar] [CrossRef] [PubMed]
- Drinda, S.; Grundler, F.; Neumann, T.; Lehmann, T.; Steckhan, N.; Michalsen, A.; de Toledo, F.W. Effects of Periodic Fasting on Fatty Liver Index-A Prospective Observational Study. Nutrients 2019, 11, 2601. [Google Scholar] [CrossRef]
- Scharf, E.; Zeiler, E.; Ncube, M.; Kolbe, P.; Hwang, S.Y.; Goldhamer, A.; Myers, T.R. The Effects of Prolonged Water-Only Fasting and Refeeding on Markers of Cardiometabolic Risk. Nutrients 2022, 14, 1183. [Google Scholar] [CrossRef] [PubMed]
- Stange, R.; Pflugbeil, C.; Michalsen, A.; Uehleke, B. Therapeutic fasting in patients with metabolic syndrome and impaired insulin resistance. Complement. Med. Res. 2013, 20, 421–426. [Google Scholar] [CrossRef]
- Finnell, J.S.; Saul, B.C.; Goldhamer, A.C.; Myers, T.R. Is fasting safe? A chart review of adverse events during medically supervised, water-only fasting. BMC Complement. Alt. Med. 2018, 18, 67. [Google Scholar] [CrossRef]
- Fang, Y.; Gu, Y.; Zhao, C.; Lv, Y.; Qian, J.; Zhu, L.; Yuan, N.; Zhang, S.; Wang, L.; Li, M.; et al. Impact of supervised beego, a traditional Chinese water-only fasting, on thrombosis and haemostasis. BMJ Nutr. Prev. Health 2021, 4, 4–17. [Google Scholar] [CrossRef]
- Jiang, Y.; Yang, X.; Dong, C.; Lu, Y.; Yin, H.; Xiao, B.; Yang, X.; Chen, W.; Cheng, W.; Tian, H.; et al. Five-day water-only fasting decreased metabolic-syndrome risk factors and increased anti-aging biomarkers without toxicity in a clinical trial of normal-weight individuals. Clin. Transl. Med. 2021, 11, e502. [Google Scholar] [CrossRef]
- Anton, S.D.; Moehl, K.; Donahoo, W.T.; Marosi, K.; Lee, S.A.; Mainous, A.G., 3rd; Leeuwenburgh, C.; Mattson, M.P. Flipping the Metabolic Switch: Understanding and Applying the Health Benefits of Fasting. Obesity 2018, 26, 254–268. [Google Scholar] [CrossRef] [PubMed]
- Hedblad, B.; Nilsson, P.; Janzon, L.; Berglund, G. Relation between insulin resistance and carotid intima-media thickness and stenosis in non-diabetic subjects. Results from a cross-sectional study in Malmo, Sweden. Diabet. Med. 2000, 17, 299–307. [Google Scholar] [CrossRef] [PubMed]
- Cuthbertson, D.J.; Koskinen, J.; Brown, E.; Magnussen, C.G.; Hutri-Kahonen, N.; Sabin, M.; Tossavainen, P.; Jokinen, E.; Laitinen, T.; Viikari, J.; et al. Fatty liver index predicts incident risk of prediabetes, type 2 diabetes and non-alcoholic fatty liver disease (NAFLD). Ann. Med. 2021, 53, 1256–1264. [Google Scholar] [CrossRef] [PubMed]
- Sampson, M.; Ling, C.; Sun, Q.; Harb, R.; Ashmaig, M.; Warnick, R.; Sethi, A.; Fleming, J.K.; Otvos, J.D.; Meeusen, J.W.; et al. A New Equation for Calculation of Low-Density Lipoprotein Cholesterol in Patients With Normolipidemia and/or Hypertriglyceridemia. JAMA Cardiol. 2020, 5, 540–548. [Google Scholar] [CrossRef]
- Sotos-Prieto, M.; Bhupathiraju, S.N.; Mattei, J.; Fung, T.T.; Li, Y.; Pan, A.; Willett, W.C.; Rimm, E.B.; Hu, F.B. Association of Changes in Diet Quality with Total and Cause-Specific Mortality. N. Engl. J. Med. 2017, 377, 143–153. [Google Scholar] [CrossRef]
- Peters, N.C.; Contento, I.R.; Kronenberg, F.; Coleton, M. Adherence in a 1-year whole foods eating pattern intervention with healthy postmenopausal women. Public Health Nutr. 2014, 17, 2806–2815. [Google Scholar] [CrossRef]
- McElreath, R. Statistical Rethinking: A Bayesian Course With Examples in R and Stan; Chapman & Hall/CRC: London, UK, 2015. [Google Scholar]
- Hox, J.; McNeish, D. Small Samples in Multilevel Modeling. In Small Sample Size Solutions, 1st ed.; Routledge: London, UK, 2020; pp. 215–225. [Google Scholar] [CrossRef]
- Vehtari, A.; Gelman, A.; Simpson, D.; Carpenter, B.; Bürkner, P.-C. Rank-Normalization, Folding, and Localization: An Improved Rˆ for Assessing Convergence of MCMC (with Discussion). Bayesian Anal. 2021, 16, 667–718. [Google Scholar] [CrossRef]
- Roy, V. Convergence Diagnostics for Markov Chain Monte Carlo. Annu. Rev. Stat. Its Appl. 2020, 7, 387–412. [Google Scholar] [CrossRef]
- Gelman, A.; Hill, J. Data Analysis Using Regression and Multilevel/Hierarchical Models; Cambridge University Press: Cambridge, UK, 2007. [Google Scholar] [CrossRef]
- NHLBI. Classification of Overweight and Obesity by BMI, Waist Circumference, and Associated Disease Risks. Available online: https://www.nhlbi.nih.gov/health/educational/lose_wt/BMI/bmi_dis.htm (accessed on 31 August 2022).
- Genuth, S.M. Effects of prolonged fasting on insulin secretion. Diabetes 1966, 15, 798–806. [Google Scholar] [CrossRef]
- Rynders, C.A.; Thomas, E.A.; Zaman, A.; Pan, Z.; Catenacci, V.A.; Melanson, E.L. Effectiveness of Intermittent Fasting and Time-Restricted Feeding Compared to Continuous Energy Restriction for Weight Loss. Nutrients 2019, 11, 2442. [Google Scholar] [CrossRef]
- Patikorn, C.; Roubal, K.; Veettil, S.K.; Chandran, V.; Pham, T.; Lee, Y.Y.; Giovannucci, E.L.; Varady, K.A.; Chaiyakunapruk, N. Intermittent Fasting and Obesity-Related Health Outcomes: An Umbrella Review of Meta-analyses of Randomized Clinical Trials. JAMA Netw. Open 2021, 4, e2139558. [Google Scholar] [CrossRef]
- Fazeli, P.K.; Zhang, Y.; O’Keefe, J.; Pesaresi, T.; Lun, M.; Lawney, B.; Steinhauser, M.L. Prolonged fasting drives a program of metabolic inflammation in human adipose tissue. Mol. Metab. 2020, 42, 101082. [Google Scholar] [CrossRef] [PubMed]
- Li, C.; Ostermann, T.; Hardt, M.; Ludtke, R.; Broecker-Preuss, M.; Dobos, G.; Michalsen, A. Metabolic and psychological response to 7-day fasting in obese patients with and without metabolic syndrome. Complement. Med. Res. 2013, 20, 413–420. [Google Scholar] [CrossRef] [PubMed]
- Jackson, I.M.; McKiddie, M.T.; Buchanan, K.D. The effect of prolonged fasting on carbohydrate metabolism: Evidence for heterogeneity in obesity. J. Endocrinol. 1968, 40, 259–260. [Google Scholar] [CrossRef] [PubMed]
- Stannard, S.R.; Thompson, M.W.; Fairbairn, K.; Huard, B.; Sachinwalla, T.; Thompson, C.H. Fasting for 72 h increases intramyocellular lipid content in nondiabetic, physically fit men. Am. J. Physiol. Endocrinol. Metab. 2002, 283, E1185–E1191. [Google Scholar] [CrossRef] [PubMed]
- Rhee, E.P.; Cheng, S.; Larson, M.G.; Walford, G.A.; Lewis, G.D.; McCabe, E.; Yang, E.; Farrell, L.; Fox, C.S.; O’Donnell, C.J.; et al. Lipid profiling identifies a triacylglycerol signature of insulin resistance and improves diabetes prediction in humans. J. Clin. Investig. 2011, 121, 1402–1411. [Google Scholar] [CrossRef]
- Cahill, G.F., Jr. Starvation in man. N. Engl. J. Med. 1970, 282, 668–675. [Google Scholar] [CrossRef]
- Hatting, M.; Tavares, C.D.J.; Sharabi, K.; Rines, A.K.; Puigserver, P. Insulin regulation of gluconeogenesis. Ann. N. Y. Acad. Sci. 2018, 1411, 21–35. [Google Scholar] [CrossRef]
- Fazeli, P.K.; Lun, M.; Kim, S.M.; Bredella, M.A.; Wright, S.; Zhang, Y.; Lee, H.; Catana, C.; Klibanski, A.; Patwari, P.; et al. FGF21 and the late adaptive response to starvation in humans. J. Clin. Investig. 2015, 125, 4601–4611. [Google Scholar] [CrossRef] [PubMed]
- Eichelmann, F.; Schwingshackl, L.; Fedirko, V.; Aleksandrova, K. Effect of plant-based diets on obesity-related inflammatory profiles: A systematic review and meta-analysis of intervention trials. Obes. Rev. 2016, 17, 1067–1079. [Google Scholar] [CrossRef]
- Medawar, E.; Huhn, S.; Villringer, A.; Veronica Witte, A. The effects of plant-based diets on the body and the brain: A systematic review. Transl. Psychiatry 2019, 9, 226. [Google Scholar] [CrossRef] [PubMed]
- Myers, T.R.; Saul, B.; Karlsen, M.; Beauchesne, A.; Glavas, Z.; Ncube, M.; Bradley, R.; Goldhamer, A.C. Potential Effects of Prolonged Water-Only Fasting Followed by a Whole-Plant-Food Diet on Salty and Sweet Taste Sensitivity and Perceived Intensity, Food Liking, and Dietary Intake. Cureus 2022, 14, e24689. [Google Scholar] [CrossRef]
| Characteristic | Overall (N = 38) | Female (n = 31) | Male (n = 7) |
|---|---|---|---|
| Age, y | 60 (52, 65) | 61 (53, 66) | 59 (51, 62) |
| Fast Length, d | 14 (13, 19) | 14 (13, 19) | 14 (12, 15) |
| Refeed Length, d | 6 (4, 8) | 6 (5, 8) | 5 (4, 6) |
| Follow-up Lengthλ, d | 45 (43, 50) | 46 (44, 50) | 43 (41, 47) |
| BL | FU | |
|---|---|---|
| Total Non-Adherence Score | 10 (7, 16) | 6 (3, 8) |
| Median (IQR) | ||||
|---|---|---|---|---|
| BL | EOF | EOR | FU | |
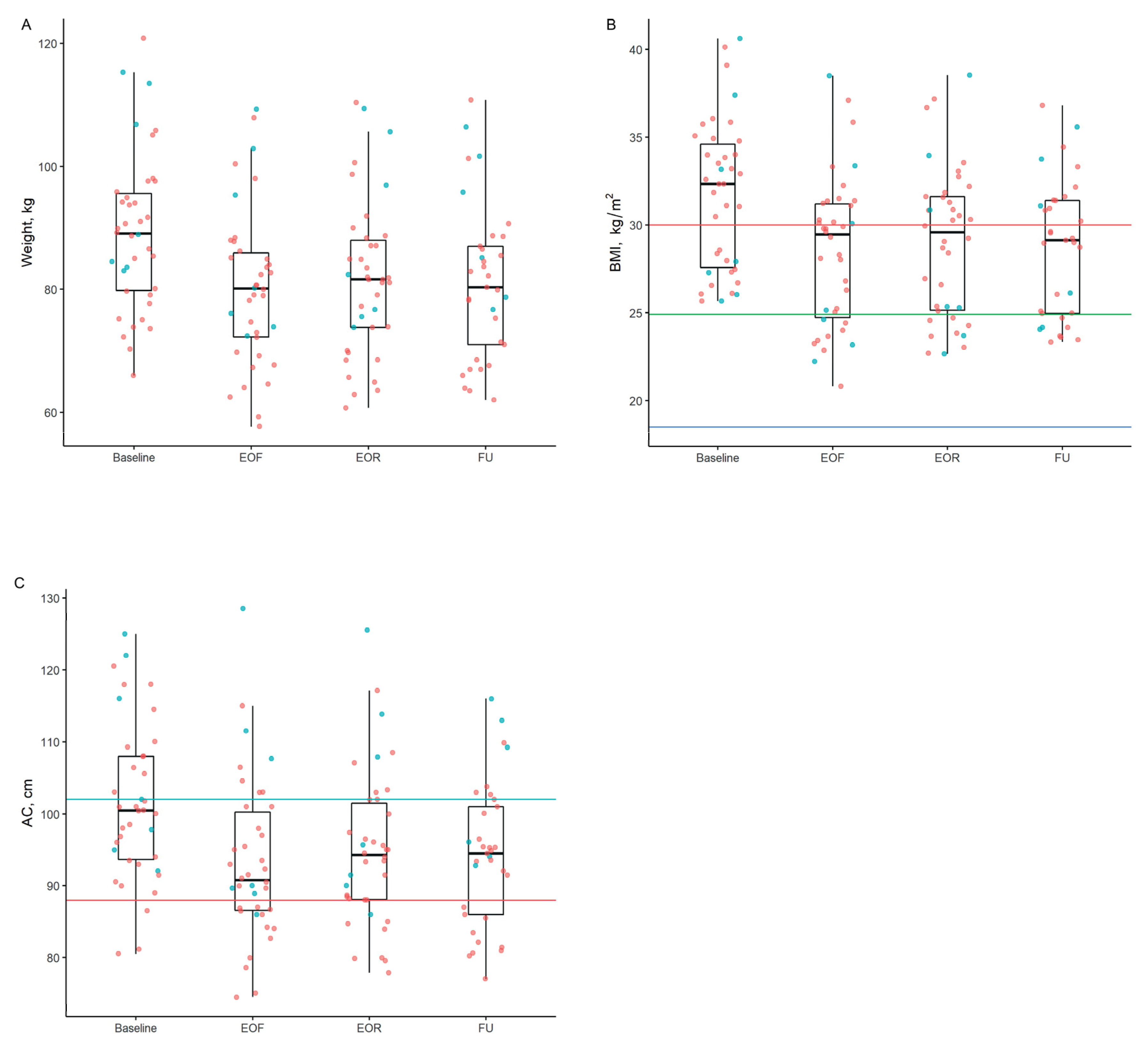
| BW, kg | 89.1 (79.8, 95.6) | 80.1 (72.2, 85.9) | 81.6 (73.8, 88.0) | 80.3 (71.0, 87.0) |
| BMI, kg/m2 (18.5–24.9 kg/m2) | 32.3 (27.6, 34.6) | 29.5 (24.7, 31.2) | 29.6 (25.1, 31.6) | 29.1 (25.0, 31.4) |
| AC, cm (<88 cm for women) | 100.4 (93.2, 107.2) | 91.0 (86.2, 97.5) | 94.0 (88.0, 98.7) | 93.6 (84.5, 98.3) |
| AC, cm (<102 cm for men) | 102.0 (96.4, 119.0) | 90.0 (89.3, 109.6) | 95.7 (90.8, 110.8) | 102.7 (94.5, 112.0) |
| SBP, mmHg (<120 mmHg) | 123 (111, 131) | 113 (105, 125) | 110 (103, 115) | 114 (110, 122) |
| DBP, mmHg (<80 mmHg) | 78 (73, 85) | 80 (73, 85) | 76 (70, 79) | 78 (71, 80) |
| TC, mmol/L (2.59–5.15 mmol/L) | 5.10 (4.38, 5.56) | 5.06 (4.36, 5.55) | 4.65 (4.01, 5.30) | 4.61 (4.27, 5.36) |
| LDL, mmol/L (<2.56 mmol/L) | 3.17 (2.51, 3.76) | 3.28 (2.65, 3.89) | 2.72 (2.02, 3.21) | 2.72 (2.43, 3.37) |
| HDL, mmol/L (>1.01 mmol/L) | 1.29 (1.04, 1.62) | 1.15 (0.96, 1.30) | 1.14 (0.96, 1.33) | 1.19 (0.96, 1.48) |
| VLDL, mmol/L (0.13–1.04 mmol/L) | 0.49 (0.44, 0.64) | 0.60 (0.54, 0.69) | 0.69 (0.58, 0.92) | 0.57 (0.41, 0.78) |
| TG, mmol/L (< 3.86 mmol/L) | 1.16 (1.05, 1.56) | 1.48 (1.29, 1.65) | 1.68 (1.40, 2.32) | 1.45 (1.01, 1.88) |
| Glucose, mmol/L (3.61–5.49 mmol/L) | 5.19 (4.79, 5.59) | 4.38 (3.89, 4.61) | 5.47 (5.12, 5.83) | 5.00 (4.72, 5.38) |
| Insulin, pmol/L (15.6–149.4 pmol/L) | 50 (33, 76) | 31 (24, 43) | 62 (41, 90) | 41 (31, 72) |
| Insulin ‡, pmol/L (2.75–5.01 pmol/L) | 3.92 (3.51, 4.34) | 3.43 (3.16, 3.76) | 4.12 (3.72, 4.50) | 3.72 (3.42, 4.28) |
| HOMA-IR (<1.9 insulin sensitive) | 1.85 (1.25, 3.22) | 1.04 (0.65, 1.51) | 2.56 (1.66, 3.41) | 1.51 (1.10, 2.73) |
| HOMA-IR ‡ (<0.64 insulin sensitive) | 0.61 (0.22, 1.17) | 0.04 (−0.43, 0.41) | 0.94 (0.51, 1.23) | 0.41 (0.09, 1.00) |
| GGT ζ, nmol/(s*L) (<1000 nmol/(s*L)) | 250 (200, 333) | 250 (200, 283) | 250 (200, 367) | 233 (167, 317) |
| GGT ‡ζ, nmol/(s*L) (<6.91 nmol/(s*L) | 5.52 (5.30, 5.81) | 5.52 (5.30, 5.65) | 5.52 (5.30, 5.90) | 5.45 (5.12, 5.76) |
| FLI ζ (<30 is optimal) | 65 (35, 86) | 45 (20, 62) | 57 (28, 79) | 47 (17, 72) |
| hsCRP, mg/L (<3 mg/L) | 1.83 (0.98, 3.81) | 2.63 (1.46, 5.10) | 1.06 (0.54, 2.00) | 0.90 (0.45, 2.14) |
| hsCRP‡, mg/L (<1.10 mg/L) | 0.61 (−0.03, 1.34) | 0.97 (0.38, 1.63) | 0.05 (−0.62, 0.69) | −0.11 (−0.80, 0.76) |
| EOF − BL | EOR − BL | FU − BL | EOR − EOF | FU − EOF | FU − EOR | |
|---|---|---|---|---|---|---|
| Estimate (95% CI) | ||||||
| BW, kg | −8.98 * (−9.69, −8.25) | −7.48 * (−8.19, −6.78) | −7.52 * (−8.43, −6.61) | 1.50 * (0.79 2.22) | 1.46 * (0.55, 2.37) | −0.04 (−0.93, 0.87) |
| BMI, kg/m2 | −3.20 * (−3.45, −2.96) | −2.68 * (−2.92, −2.43) | −2.70 * (−3.01, −2.39) | 0.53 * (0.27, 0.78) | 0.50 * (0.19, 0.82) | −0.02 (−0.34, 0.30) |
| AC, cm | −8.13 * (−9.00, −7.26) | −6.51 * (−7.36, −5.67) | −6.58 * (−7.68, −5.48) | 1.62 * (0.78, 2.48) | 1.55 * (0.44, 2.66) | −0.07 (−1.16, 1.03) |
| SBP, mmHg | −11.49 * (−15.17, −7.84) | −14.58 * (−18.28, −10.91) | −7.68 * (−12.31, −3.04) | −3.09 (−6.70, 0.55) | 3.81 (−0.82, 8.40) | 6.90 * (2.19, 11.54) |
| DBP, mmHg | −0.54 (−2.40, 1.32) | −3.33 * (−5.18, −1.48) | −2.44 * (−4.92, −0.01) | −2.79 * (−4.67, −0.89) | −1.90 (−4.38, 0.60) | 0.88 (−1.56, 3.31) |
| TC, mmol/L | −0.04 (−0.26, 0.18) | −0.51 * (−0.72, −0.29) | −0.35 * (−0.63, −0.07) | −0.47 * (−0.68, −0.25) | −0.31 * (−0.59, −0.03) | 0.16 (−0.12, 0.44) |
| HDL, mmol/L | −0.16 * (−0.22, −0.10) | −0.15 * (−0.21, −0.09) | −0.05 (−0.12, 0.03) | 0.01 (−0.05, 0.07) | 0.11 * (0.03, 0.19) | 0.10 * (0.02, 0.18) |
| LDL, mmol/L | 0.09 (−0.11, 0.29) | −0.59 * (−0.79, −0.39) | −0.34 * (−0.59, −0.09) | −0.68 * (−0.88, −0.48) | −0.42 * (−0.67, −0.18) | 0.26 * (0.00, 0.51) |
| VLDL, mmol/L | 0.03 (−0.03, 0.09) | 0.23 * (0.17, 0.29) | 0.04 (−0.04, 0.11) | 0.20 * (0.14, 0.26) | 0.01 (−0.07, 0.08) | −0.20 * (−0.27, −0.12) |
| TG, mmol/L | 0.08 (−0.07, 0.22) | 0.58 * (0.43 0.73) | 0.08 (−0.11, 0.27) | 0.50 * (0.36, 0.65) | −0.00 (−0.18, 0.19) | −0.50 * (−0.69, −0.31) |
| Glucose, mmol/L | −0.79 * (−0.97, −0.61) | 0.53 * (0.35, 0.71) | −0.13 (−0.36, 0.10) | 1.32 * (1.13, 1.50) | 0.66 * (0.43, 0.89) | −0.66 * (−0.89, −0.43) |
| Insulin ‡, pmol/L | −0.42 * (−0.58, −0.26) | 0.44 * (0.29, 0.60) | −0.06 (−0.27, 0.14) | 0.86 * (0.70, 1.02) | 0.35 * (0.15, 0.55) | −0.51 * (−0.71, −0.31) |
| HOMA-IR ‡ | −0.58 * (−0.76, −0.41) | 0.54 * (0.36, 0.71) | −0.09 (−0.32, 0.14) | 1.12 * (0.94, 1.30) | 0.50 * (0.27, 0.72) | −0.63 * (−0.85, −0.40) |
| GGT ‡ζ, nmol/(s*L) | −0.06 (−0.16, 0.05) | 0.02 (−0.08, 0.12) | −0.09 (−0.19, 0.02) | 0.07 (−0.03, 0.18) | −0.03 (−0.14, 0.08) | −0.10 (−0.21, 0.00) |
| FLI ζ | −14.62 * (−18.09, −11.07) | −6.12 * (−9.67, −2.59) | −11.80 * (−15.49, −8.11) | 8.49 * (4.96, 12.01) | 2.82 (−0.81, 6.52) | −5.67 * (−9.38, −1.93) |
| hsCRP ‡, mg/L | 0.29 * (0.10, 0.49) | −0.48 * (−0.68, −0.29) | −0.42 * (−0.67, −0.17) | −0.77 * (−0.97, −0.57) | −0.71 * (−0.97, −0.45) | 0.06 (−0.19, 0.31) |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Gabriel, S.; Ncube, M.; Zeiler, E.; Thompson, N.; Karlsen, M.C.; Goldman, D.M.; Glavas, Z.; Beauchesne, A.; Scharf, E.; Goldhamer, A.C.; et al. A Six-Week Follow-Up Study on the Sustained Effects of Prolonged Water-Only Fasting and Refeeding on Markers of Cardiometabolic Risk. Nutrients 2022, 14, 4313. https://doi.org/10.3390/nu14204313
Gabriel S, Ncube M, Zeiler E, Thompson N, Karlsen MC, Goldman DM, Glavas Z, Beauchesne A, Scharf E, Goldhamer AC, et al. A Six-Week Follow-Up Study on the Sustained Effects of Prolonged Water-Only Fasting and Refeeding on Markers of Cardiometabolic Risk. Nutrients. 2022; 14(20):4313. https://doi.org/10.3390/nu14204313
Chicago/Turabian StyleGabriel, Sahmla, Mackson Ncube, Evelyn Zeiler, Natasha Thompson, Micaela C. Karlsen, David M. Goldman, Zrinka Glavas, Andrew Beauchesne, Eugene Scharf, Alan C. Goldhamer, and et al. 2022. "A Six-Week Follow-Up Study on the Sustained Effects of Prolonged Water-Only Fasting and Refeeding on Markers of Cardiometabolic Risk" Nutrients 14, no. 20: 4313. https://doi.org/10.3390/nu14204313
APA StyleGabriel, S., Ncube, M., Zeiler, E., Thompson, N., Karlsen, M. C., Goldman, D. M., Glavas, Z., Beauchesne, A., Scharf, E., Goldhamer, A. C., & Myers, T. R. (2022). A Six-Week Follow-Up Study on the Sustained Effects of Prolonged Water-Only Fasting and Refeeding on Markers of Cardiometabolic Risk. Nutrients, 14(20), 4313. https://doi.org/10.3390/nu14204313






