Abstract
To explore the effect of exercise intervention on fundamental movement skills (FMS) of children with attention deficit hyperactivity disorder (ADHD) and/or autism spectrum disorder (ASD). Following the principle of PICOS, randomized controlled trials of the effect of exercise intervention on the FMS of ADHD/ASD children were searched. A total of 12 articles and 396 participants were included. Review Manager5.4 and Stata16.0 software were used to process and analyze the data. The results revealed that (1) exercise intervention can improve the gross motor skills of children with ADHD/ASD (p < 0.00001). Aquatic therapy (SMD = 56.54, 95% CI = 38.83–74.25) has a better effect on stability skills, and FMS intervention (SMD = 17.58, 95% CI = 1.78–33.38) has a better effect on locomotor skills and object control skills. (2) Exercise intervention can improve the fine motor skills of children with ADHD/ASD (p = 0.001). Table tennis exercise (SMD = 9.91, 95% CI = 0.23–19.59) and horse-riding program (SMD = 9.50, 95% CI = 5.20–13.80) have better effects on fine manual control and hand–eye coordination. (3) The closed-skill intervention for 60 min each time, twice a week, for at least 12 weeks had the best effect on the improvement in the FMS in children with ADHD/ASD (p < 0.00001). Exercise intervention may effectively improve FMS in children with ADHD/ASD. Intervention form, time, frequency, and duration are important moderator variables that positively impact the FMS of children with ADHD/ASD.
1. Introduction
Attention deficit hyperactivity disorder (ADHD) and autism spectrum disorder (ASD) are the most common neurodevelopmental disorders in children, which have a significant impact on children’s physical and mental health [1]. Children with ADHD are characterized by inattention, hyperactivity, impulsivity, difficulty in controlling behavior, or such comprehensive symptoms, while children with ASD have apparent deficits in social communication skills and repetitive stereotyped behavior patterns [2,3]. Despite significant differences in the core symptoms between children with ADHD and ASD, clinical studies have supported the similarity of the behavioral disorders, and the findings suggest that the two types of children not only have highly shared heritability, but also represent the performance of the same endophenotype and can be classified into the same diagnostic entity [4,5]. While evidence of atypical brain development suggests that children with both ADHD and ASD may be affected by cerebral laterality and develop severe motor coordination deficits, it is worth noting that children with developmental coordination disorder (DCD) are the most common co-occurring disorder in the above two types of children, but the underlying mechanism evidence is insufficient, so only ADHD and ASD children are discussed and studied [6].
Movement disorders are common behavioral disorders in children with ADHD and ASD, especially fundamental movement skills (FMS) disorders such as low levels of gross and fine motor skills, difficulty in motor coordination, and poor posture, which may be related to delayed maturation of the prefrontal cortex [7,8,9]. FMS is the basis for children’s movement, play, and lifelong physical activity and can be divided into gross motor skills and fine motor skills. The development of gross motor skills involves control of the trunk or legs including locomotor, object control, and stability skills, and the development of fine motor skills involves control of the hands and eyes including fine manual control, hand–eye coordination, etc. [10]. In addition, some studies have found that children with ADHD and ASD have difficulty with age-appropriate FMS, and more attention should be given to the teaching, practice, and feedback of skills in specific domains to promote FMS acquisition and proficiency [11,12].
Exercise interventions and pharmacological interventions are promising interventions for children with ADHD/ASD. Exercise interventions are considered to be physical activity interventions that maintain or enhance an individual’s movement capacity through planned, structured, and repetitive physical activity [13]. Adequate exercise intervention can induce neuroplasticity in brain structure and function as well as effectively enhance FMS, executive function, learning performance, and emotion regulation in children with ADHD and ASD [14,15]. However, some pharmacological interventions are ineffective for children with ADHD and ASD and are associated with certain side effects including insomnia, loss of appetite, growth retardation, and headache [16,17]. In comparison, exercise interventions are more beneficial for the treatment of ADHD/ASD children’s movement disorders and improves the FMS in both types of children.
Currently, a series of studies such as motor skill intervention [18], aerobic exercise training [19], aquatic program [20], and mini-basketball training program [21] have confirmed the positive effects of different exercise interventions on FMS in children with ADHD and ASD, but so far, no studies have been conducted to date for meta-analysis, and there are large differences in the form, time, frequency, and duration of exercise interventions among studies, and the results of individual studies are still inconclusive. Therefore, based on the PICOS principle, a meta-analysis of the effects of exercise intervention on the FMS of children with ADHD and/or ASD was conducted to further explore the moderating effects of exercise intervention form, time, frequency, and duration on the FMS of both types of children.
2. Method
2.1. Search Strategy
Articles were searched in the PubMed, Web of Science, Cochrane Library, and CNKI databases. The search strategy was based on the following syntax: (#1) (“children” OR “preschooler*” OR “student*”) AND (#2) (“attention deficit hyperactivity disorder*” OR “attention deficit disorders with hyperactivity” OR “attention deficit disorder*” OR “hyperkinetic syndrome” OR “ADHD” OR “autism spectrum disorder*” OR “ASD”) AND (#3) (“movement skill*” OR “motor skill*” OR “motor abilit*”) AND (#4) (“exercise” OR “physical activit*” OR “sport*” OR “training”). The literature search period was from 1 January 2010 to 31 October 2022.
2.2. Inclusion and Exclusion Criteria
The PICOS principle is a structured method for searching the literature and is the basis for formulating the eligibility criteria for a meta-analysis. The PRISMA statement divides the PICOS principle into five main components: participants, interventions, comparisons, outcomes, and study design [22]. Following the PICOS principle, the inclusion criteria were: (1) the participants were children with ADHD and/or ASD; (2) the experimental group received structured exercise intervention, while the control group did not receive structured exercise intervention; (3) the outcome indicators were rating scales related to FMS of ADHD/ASD children; (4) the study design was a randomized controlled trial (RCT); and (5) no medication or other exercise interventions were used in the experimental group and the control group. The exclusion criteria were: (1) neither children with ADHD nor children with ASD; (2) the experimental group was an unstructured exercise intervention or a mixed intervention; (3) no outcome data was shown; (4) non-RCTs; and (5) conference papers, reviews, or duplicate published studies.
2.3. Data Extraction
To improve the quality of literature information extraction, two researchers independently performed information extraction. The following information was included in the design of the data extraction form: the first author, year of publication, diagnostic standard, subject type, data from the experimental and control groups (sample size and age), exercise intervention (form, time, frequency, and duration), assessment scales, and outcome indicators.
2.4. Risk of Bias Assessment
Risk of bias assessment for included studies is an important part of the literature quality assessment. The Cochrane risk of bias assessment tool [23] is the most widely used in randomized controlled trials, mainly including seven items: random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcomes assessment, incomplete outcome data, selective reporting, and other biases. Each item was judged to be low risk of bias, unclear risk of bias, and high risk of bias. The risk of bias was assessed by two researchers independently, and if there was any disagreement, this was resolved by mutual agreement or determined by a third reviewer.
2.5. Data Analysis and Synthesis
Review Manager 5.4 software was used for the heterogeneity test and subgroup analysis, and Stata 16.0 software was used for the sensitivity analysis and publication bias test. Continuous outcomes were expressed as the standardized mean differences (SMDs) with 95% confidence intervals (CIs).
Heterogeneity was tested by p value and I2. When p > 0.10 and I2 < 50%, it will be considered that there was no heterogeneity and a fixed-effects model was used for meta-analysis. When p < 0.10 and I2 > 50%, it was considered that there was heterogeneity and a random-effects model was used for meta-analysis. Subgroup analysis was conducted for categorical variables such as the type, time, frequency, and duration. Sensitivity analysis was used to test the stability of the meta-analysis results by excluding individual studies one by one. Publication bias was identified by plotting funnel plots and Egger linear regression.
3. Results
3.1. Study Characteristics
The flowchart of the literature selection process is shown in Figure 1. A total of 1056 articles were initially searched through the database and other channels (Google Scholar). Endnote software was used to remove 228 duplicate articles, and 781 articles were excluded after reading the title and abstract. In addition, 35 articles were excluded for the following reasons: (1) non-RCTs; (2) mixed intervention; (3) no outcome data was shown, and 12 articles (six ADHD, six ASD) were finally included in the meta-analysis.
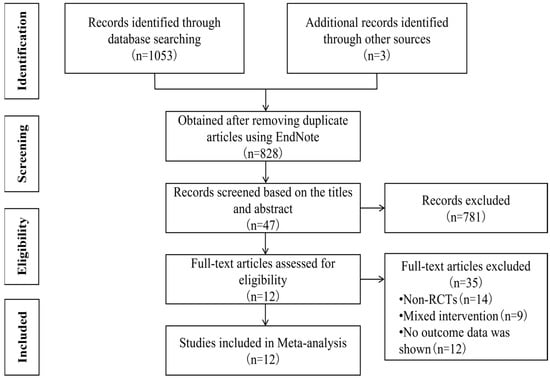
Figure 1.
Flowchart of the literature selection process.
Table 1 shows the basic information of the 12 included articles including the references, diagnostic standard, characteristics of the children, exercise interventions (form, time, frequency, and duration), assessment scales, and outcome indicators (gross and fine motor skills). A total of 379 children with ADHD and ASD were included, 190 in the experimental group and 189 in the control group. The sample sizes for both the experimental and control groups were 5–42 individuals, aged 3–16 years. The exercise intervention time was 35–90 min, the frequency was 1–5 times/week, and the duration was 4–20 weeks.

Table 1.
Basic information of the included studies.
3.2. Risk of Bias
The results of the bias risk assessment are shown in Figure 2. The risk of selective reporting and other biases in 12 articles was low risk of bias, the risk of blinding bias for allocation concealment and outcome assessment was unclear, and the blinding of the participants and personnel was high risk of bias. In addition, the risk of bias in random sequence generation was unclear in three articles [24,32,34], and only four articles [25,30,32,35] mentioned complete outcome indicators. In summary, the 12 articles included may have the risk of bias.
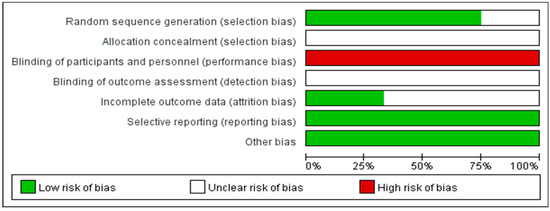
Figure 2.
Risk of bias assessment for the included studies.
3.3. Summary of the Meta-Analysis Results
3.3.1. The Effect of Exercise Intervention on Gross Motor Skills of ADHD/ASD Children
There were 12 studies on the effect of exercise intervention on the gross motor skills of ADHD/ASD children. The total sample size of the experimental group was 190, and the total sample size of the control group was 189. As shown in Figure 3, due to the heterogeneity among the study results (p < 0.00001, I2 = 79%), a random effect model was used for the meta-analysis. The results showed that there was a significant difference between the experimental group and the control group (p < 0.00001), indicating that exercise intervention may improve the gross motor skills in ADHD/ASD children (SMD = 5.93, 95% CI = 4.05–7.82). Among them, Feng’s aquatic therapy (SMD = 56.54, 95% CI = 38.83–74.25) was more effective in improving the stability skills of the ADHD/ASD children, and Dong’s FMS intervention (SMD = 17.58, 95% CI = 1.78–33.38) was more effective in improving the locomotor skills and object control skills of both types of children.
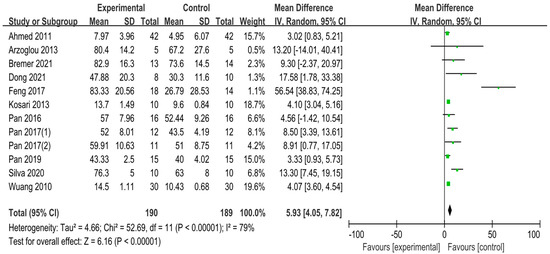
Figure 3.
Forest plot of the gross motor skills of ADHD/ASD children [24,25,26,27,28,29,30,31,32,33,34,35].
3.3.2. The Effect of Exercise Intervention on Fine Motor Skills of ADHD/ASD Children
There were four studies on the effect of exercise intervention on the fine motor skills of ADHD/ASD children. The total sample size of the experimental group was 69, and the total sample size of the control group was 69. As shown in Figure 4, due to the heterogeneity among the study results (p = 0.05, I2 = 62%), a random effect model was used for the meta-analysis. The results showed that there was a significant difference between the experimental group and the control group (p = 0.001), indicating that exercise intervention might improve the fine skills of ADHD/ASD children (SMD = 6.32, 95% CI = 2.42–10.21). Among them, Pan’s table tennis exercise (SMD = 9.91, 95% CI = 0.23–19.59) and horse-riding program (SMD = 9.50, 95% CI = 5.20–13.80) had better effects on the fine manual control and hand–eye coordination in both types of children.
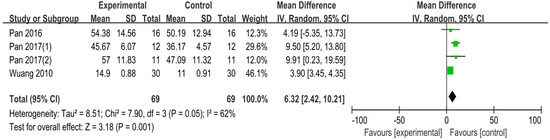
Figure 4.
Forest plot of the fine motor skills of ADHD/ASD children [26,27,33,35].
3.4. Subgroup Analysis
To further explore potential sources of heterogeneity, we analyzed the FMS of the subgroups according to the moderator variables (see Table 2), suggesting that the source of heterogeneity may be related to the intervention form, time, frequency, and duration. Among them, the closed-skill intervention for 60 min each time, twice a week, for at least 12 weeks, had the best effect on the improvement in the FMS in children with ADHD/ASD (p < 0.00001).

Table 2.
Subgroup analysis of FMS.
3.5. Sensitivity Analysis
In the included studies, samples of gross motor skills were mainly distributed on the left side, and samples of fine motor skills were distributed on the right side. By excluding individual studies one by one, a sensitivity analysis was performed to test the stability of the overall experimental results. As shown in Figure 5, the effect sizes of both sides of the sample after excluding each study were within the upper and lower limits of the 95% confidence interval. Wuang’s study had a high degree of scatter, but it had little effect on the overall experimental results, which indicates that the population effect size of this study was not affected by one-tailed bias. The results showed that in the study on the FMS of children with ADHD and ASD affected by exercise intervention, there was no significant change in the experimental results, suggesting that the results were relatively stable and reliable.
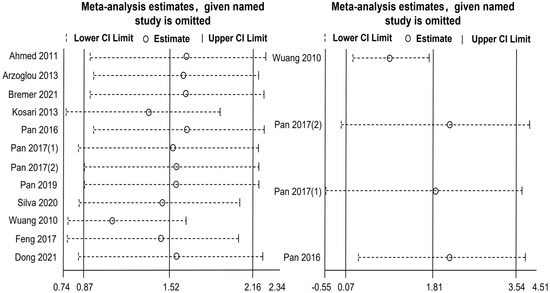
Figure 5.
Sensitivity analysis of the FMS [24,25,26,27,28,29,30,31,32,33,34,35].
3.6. Publication Bias
Publication bias was first tested by plotting a funnel plot. The scatter points in Figure 6 represent the studies included in the meta-analysis. Most of the scatter points were located in the middle of the funnel and were asymmetrical on the left and right sides of the vertical line. There may be publication bias in the preliminary analysis. Next, Egger linear regression was used to further test for publication bias. As shown in Figure 7, the left vertical line is the confidence interval corresponding to the intercept α, which had a 95% CI (−0.29, 9.12), p = 0.063 > 0.05, indicating that there was no publication bias in the included studies. In summary, the findings indicated that this study was less affected by publication bias and that the findings were reliable.
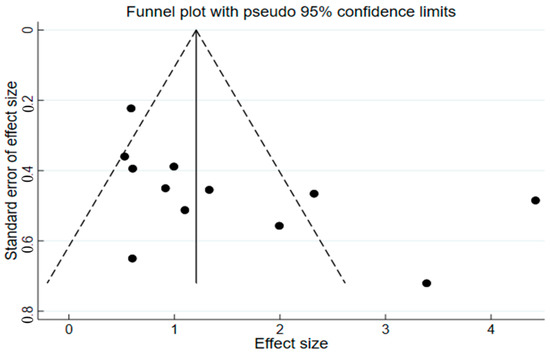
Figure 6.
Publication bias funnel plot.
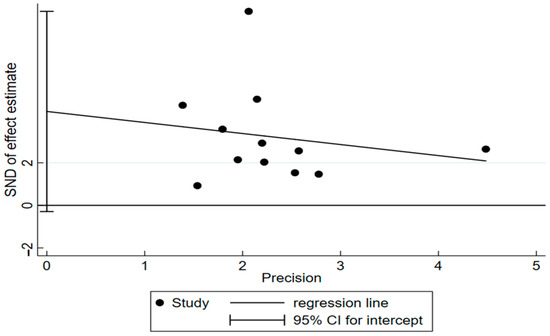
Figure 7.
Egger linear regression plot.
4. Discussion
4.1. Exercise Intervention Has a Significant Effect on Gross Motor Skills of ADHD/ASD Children
Meta-analysis studies have shown that exercise intervention can improve the gross motor skills in children with ADHD/ASD, which is consistent with the findings of Ruggeri et al. [12,36]. The underlying mechanism by which exercise intervention induces improvements in gross motor skills may be related to neuroanatomy [9,37]. On one hand, exercise intervention can cause a series of biological reactions in the muscles and organs, promoting neurogenerative, neuroadaptive, and neuroprotective processes to favorably affect the structural development and functional neurocognitive development of the brain primarily through the regulation of the brain’s neural circuitry, mediation of executive function, and lasting impact on the developmental trajectory of gross motor skills in children with ADHD/ASD [38,39]. On the other hand, exercise intervention may help the prefrontal cortex of the brain to formulate and improve perception–motor related skill tasks, while the prefrontal cortex of the brain can get away to focus on cognitive and adaptive functions, allowing for the gradual automation of gross motor skills [40].
Among the gross motor skill interventions, six types [24,26,27,28,29,30,31,33,34,35] of exercise interventions could improve the locomotor skills of ADHD/ASD children, and only two types [24,30,31] could improve the object control skills for both types of children. Of these, the FMS intervention [30,31] and the table tennis exercise [24] had the potential to improve both the locomotor skills and object control skills in both types of children, but the enhancing effect of the FMS intervention was better. Further analysis found that the FMS intervention could not only provide a goal-oriented, structured, and progressive guidance strategy, positively change the functional connection of the brain’s neural network and have an impact on the brain’s neurogenesis, adaptation, and protection [38,41], but in particular, it created the best stimulating environment in the learning situation and helped children with ADHD/ASD to create a positive self-perception and experience [30]. In addition, six types [25,26,27,28,32,33,34,35] of exercise interventions could improve the stability skills in children with ADHD/ASD, but aquatic therapy had the best improvement effect. Aquatic therapy mainly applies the principles of hydrodynamics to provide multiple sensory stimulations through water temperature, weight reduction, and vestibular input to promote gross motor skill execution [42].
4.2. Exercise Intervention Has a Significant Effect on Fine Motor Skills of ADHD/ASD Children
The findings that exercise intervention improves the fine motor skills in children with ADHD/ASD are not consistent with the results of Zhang et al. [1]. These differences may be due to the sample size, the form and intensity of the intervention, the tactile sensitivity, and the overall lack of social imitation being different [43]. It has been shown that exercise intervention may not only promote the brain to make connections in visual feedback and motor commands, but also form connectivity with both the visual network and the dorsomedial motor region, and most likely through visual imitation to improve the hand–eye coordination ability and upper limb motor skills in children with ADHD/ASD. It may also promote central nervous system plasticity and increase neurotransmitter secretion, increasing the level of brain arousal, and thereby improving executive function and enhancing the fine manual control of both types of children [44,45].
Among the studies included in the meta-analysis, only four studies [26,27,33,35] focused on the effect of exercise intervention on the fine motor skills of children with ADHD/ASD. The table tennis exercise and horse-riding program were important interventions to improve their fine motor skills, but the specific exercise patterns differed. The successful performance of table tennis exercises mainly depends on visual perception and executive function, that is, accurately predicting the spatial trajectory and arrival time of the table tennis ball, and immediately making the selection and execution of the ball response. Table tennis exercise is based on the principle of constraint-induced exercise therapy, which guides children with ADHD/ASD to perform repetitive exercises, conceal motor potential through different strategies and tasks, and promote hand–eye coordination, fine manual control, and executive function of both types of children [27,33]. Through active vision and somatosensory control, the horse-riding program coordinated the connection between vision and the limbs and performed the movements of the limbs correctly. ADHD/ASD children are required to grasp the handle of the horse-riding machine during the horse-riding program, and alter the posture and speed of their upper limbs from time to time according to the visual information and trunk movement, improving hand–eye coordination and fine manual control [26,35]. Currently, the fine motor skills of most children with ADHD/ASD show structural defects and are lower than the level of children of the same age [5,46]. Therefore, it is hoped that more appropriate exercise interventions can be used to improve the fine motor skills of both types of children.
4.3. Effects of Moderator Variables in Exercise Intervention on FMS in ADHD/ASD Children
The results of this study show that although both open-skill and closed-skill can improve FMS in children with ADHD/ASD, the improvement effect of closed-skill was better. The motor environment is considered to be the main sign that distinguishes open-skill from closed-skill. Closed-skill (running, cycling, swimming, etc.) are performed in a relatively consistent, controllable, and self-regulating environment; open-skill (table tennis, football, basketball, etc.) refer to responding in an environment that is dynamic, unpredictable, and influenced by external factors. In general, open-skill interventions tend to be more complex [47,48]. The analysis of this study demonstrates that children with ADHD/ASD have defects in complex tasks, adaptive behavior, and motor development, and that performance on the FMS is significantly poorer than that of children of the same age. Therefore, simple, regular, and predictable closed-skill are more suitable for the development of FMS of both types of children [49,50].
In addition to the form of intervention, the FMS of ADHD/ASD children was also affected by the time, frequency, and duration of the intervention, which is consistent with previous meta-analysis studies [16]. This study found that an exercise intervention of 60 min each time, twice a week, for at least 12 weeks was the most beneficial for improving the FMS in children with ADHD/ASD. In terms of intervention time, each 60-min improvement effect was the best. For example, tai chi training [51] and the FMS intervention [9] implemented a 60-min structured intervention program to effectively improve the children’s movements and skills. With regard to the frequency of intervention, exercise intervention once or twice a week may improve FMS in children with ADHD/ASD, and the improvement effect was better twice a week, which is consistent with the aquatic therapy of Pan [52]. Exercise intervention three times or more per week had no significant effect on improving the FMS of the two types of children, indicating that intensive exercise intervention may not be suitable for the development of both types of children, probably because the development of FMS of both types of children lags behind that of normal children, and the frequency of intervention should be consistent with their actual developmental abilities [29,34]. In terms of intervention duration, the improvement effect is better for 12 weeks or more. Long-term exercise intervention may increase the brain growth factors in children with ADHD/ASD, promote brain activity, improve cognitive ability, and enhance the practice effect of the FMS [38]. Lourenço et al. pointed out that exercise intervention lasting at least 12 weeks may stimulate the long-term attention and FMS proficiency of the two types of children to a greater extent [53,54]. In conclusion, to maximize the benefits of exercise interventions, the potential effect of moderator variables should be considered.
5. Conclusions and Implications
5.1. Conclusions
The results of the meta-analysis showed that exercise intervention could improve the gross and fine motor skills in children with ADHD/ASD; the closed-skill intervention for 60 min each time, twice a week, for at least 12 weeks had the best effect on the improvement in the FMS in both types of children. This study provides exercise intervention ideas for medical institutions, occupational therapists, special education teachers, physical education teachers, and parents of children with ADHD/ASD, and provides a basis for future research into the improvement of the FMS of both types of children.
5.2. Limitations and Future Research
One important limitation of this study was the small sample size of children with ADHD/ASD included in the study, which may have impacted the statistical analysis and limited the generalizability of the results. Another limitation of this study is the lack of follow-up studies analyzed from a longitudinal perspective, which makes it difficult to scientifically reflect the long-term timeliness of exercise intervention on the FMS of both types of children. Moreover, this study mainly focused on school-based interventions, lacked an exploration of family and community-based interventions, and ignored the effect of integration across different modes of intervention. However, there were still some shortcomings in this study. In terms of the neural mechanism, although children with ADHD/ASD have abnormalities in brain structure and function, there is still a lack of neuroanatomical evidence for the intrinsic connection between exercise intervention and the brain. In terms of the subgroup analysis, the discussion of moderator variables was not sufficiently comprehensive. Currently, only the intervention form, time, frequency, and duration have been studied.
Based on the above discussion, several suggestions are offered for exercise intervention to improve the FMS of children with ADHD/ASD. First, to further expand the sample size of randomized controlled trials on the effect of exercise intervention on the FMS of children with ADHD/ASD to ensure the applicability of the research results. Second, pay attention to whether the long-term longitudinal follow-up study has a positive effect on the FMS for both types of children, and provide ideas and directions for the experimental design of later exercise interventions. Third, to build a cooperative exercise intervention model for families, schools, and communities, and to explore the effect of the comprehensive intervention model on the FMS of both types of children. Fourth, to continue to explore the brain structure and functional mechanisms in both types of children. As above-mentioned, children with ADHD/ASD have abnormal cerebral lateralization, but how to integrate the functions of the two sides of the brain through exercise intervention to improve the FMS of both types of children has yet to be explored. Finally, by considering the adjusting variable of increasing exercise intensity, the effects of different intensities of exercise on the FMS of both types of children were compared.
Author Contributions
Conceptualization, K.N., B.W. and Y.Y.; Methodology, Y.Y. and K.N.; Software, Y.Y. and K.N.; Validation, C.S.; Formal analysis, Y.Y.; Investigation, Y.Y.; Resources, Y.Y.; Data curation, Y.Y.; Writing—original-draft preparation, Y.Y. and C.S.; Writing—review and editing, K.N. and B.W.; Visualization, Y.Y.; Supervision, K.N.; Project administration, K.N.; Funding acquisition, K.N. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by the Major Program of the National Fund of Philosophy and Social Science of China, grant number 22BTY051.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
No new data were created or analyzed in this study. Data sharing is not applicable to this article.
Acknowledgments
The authors would like to thank the National Fund of Philosophy and Social Science of China for its support.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Zhang, M.; Liu, Z.; Ma, H.; Smith, D.M. Chronic Physical Activity for Attention Deficit Hyperactivity Disorder and/or Autism Spectrum Disorder in Children: A Meta-Analysis of Randomized Controlled Trials. Front. Behav. Neurosci. 2020, 14, 564886. [Google Scholar] [CrossRef] [PubMed]
- Gapin, J.; Etnier, J.L. The relationship between physical activity and executive function performance in children with attention-deficit hyperactivity disorder. J. Sport Exerc. Psychol. 2010, 32, 753–763. [Google Scholar] [CrossRef] [PubMed]
- Lord, C.; Elsabbagh, M.; Baird, G.; Veenstra-Vanderweele, J. Seminar Autism spectrum disorder. Lancet 2018, 392, 508–520. [Google Scholar] [CrossRef]
- Hanson, E.; Cerban, B.M.; Slater, C.M.; Caccamo, L.M.; Bacic, J.; Chan, E. Brief report: Prevalence of attention deficit/hyperactivity disorder among individuals with an autism spectrum disorder. J. Autism Dev. Disord. 2013, 43, 1459–1464. [Google Scholar] [CrossRef]
- Kaiser, M.-L.; Schoemaker, M.; Albaret, J.-M.; Geuze, R. What is the evidence of impaired motor skills and motor control among children with attention deficit hyperactivity disorder (ADHD)? Systematic review of the literature. Res. Dev. Disabil. 2015, 36, 338–357. [Google Scholar] [CrossRef]
- Murray, M.J. Attention-deficit/hyperactivity disorder in the context of autism spectrum disorders. Curr. Psychiatry Rep. 2010, 12, 382–388. [Google Scholar] [CrossRef] [PubMed]
- Scharoun, S.; Bryden, P.; Otipkova, Z.; Musalek, M.; Lejcarova, A. Motor skills in Czech children with attention-deficit/hyperactivity disorder and their neurotypical counterparts. Res. Dev. Disabil. 2013, 34, 4142–4153. [Google Scholar] [CrossRef] [PubMed]
- Xing, Y. Effects of Gross Motor Skill Learning on Fundamental Motor Skill Level of Children with Autism Spectrum Disorder. J. Cap. Univ. Phys. Educ Sport 2020, 32, 13–17. [Google Scholar] [CrossRef]
- Wang, Y.; Zuo, C.; Xu, Q.; Hao, L.; Zhang, Y. Attention-deficit/hyperactivity disorder is characterized by a delay in subcortical maturation. Prog. Neuropsychopharmacol. Biol. Psychiatry 2021, 104, 110044. [Google Scholar] [CrossRef]
- Payne, G.; Geng, P.X.; Liang, G.L. Introduction to Human Motor Development; People’s Education Press: Beijing, China, 2008. [Google Scholar]
- Cho, H.; Ji, S.; Chung, S.; Kim, M.; Joung, Y.-S. Motor function in school-aged children with attention-deficit/hyperactivity disorder in Korea. Psychiatry Investig. 2014, 11, 223–227. [Google Scholar] [CrossRef]
- Ruggeri, A.; Dancel, A.; Johnson, R.; Sargent, B. The effect of motor and physical activity intervention on motor outcomes of children with autism spectrum disorder: A systematic review. Autism Int. J. Res. Pract. 2020, 24, 544–568. [Google Scholar] [CrossRef]
- American College of Sports Medicine. ACSM’s Guidelines for Exercise Testing and Prescription; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2013. [Google Scholar]
- Huang, J.; Yeh, C.; Chan, Y. Effect of Physical Activity on Behavior and Cognition in Children with Attention Deficit/Hyperactivity Disorder. Sport Res. Rev. 2017, 141, 43–51. [Google Scholar]
- Müller, P.; Duderstadt, Y.; Lessmann, V.; Müller, N.G. Lactate and BDNF: Key mediators of exercise induced neuroplasticity? J. Clin. Med. 2020, 9, 1136. [Google Scholar] [CrossRef]
- Sun, W.; Yu, M.; Zhou, X. Effects of physical exercise on attention deficit and other major symptoms in children with ADHD: A meta-analysis. Psychiatry Res. 2022, 311, 114509. [Google Scholar] [CrossRef]
- Wigal, S.B.; Emmerson, N.; Gehricke, J.-G.; Galassetti, P. Exercise: Applications to childhood ADHD. J. Atten. Disord. 2013, 17, 279–290. [Google Scholar] [CrossRef]
- Ketcheson, L.; Hauck, J.; Ulrich, D. The effects of an early motor skill intervention on motor skills, levels of physical activity, and socialization in young children with autism spectrum disorder: A pilot study. Autism Int. J. Res. Pract. 2017, 21, 481–492. [Google Scholar] [CrossRef] [PubMed]
- Brand, S.; Jossen, S.; Holsboer-Trachsler, E.; Pühse, U.; Gerber, M. Impact of aerobic exercise on sleep and motor skills in children with autism spectrum disorders—A pilot study. Neuropsychiatr. Dis. Treat. 2015, 11, 1911–1920. [Google Scholar] [CrossRef] [PubMed]
- Ennis, E. The effects of a physical therapy-directed aquatic program on children with autism spectrum disorders. J. Aquat. Phys. Ther. 2011, 19, 4–10. [Google Scholar]
- Cai, K.-L.; Wang, J.-G.; Liu, Z.-M.; Zhu, L.-N.; Xiong, X.; Klich, S.; Maszczyk, A.; Chen, A.-G. Mini-basketball training program improves physical fitness and social communication in preschool children with autism spectrum disorders. J. Hum. Kinet. 2020, 73, 267–278. [Google Scholar] [CrossRef] [PubMed]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. Ann. Intern. Med. 2009, 151, 264–269. [Google Scholar] [CrossRef]
- Zhan, S.Y. Systematic Review and Meta-Analysis; People’s Health Publishing House: Beijing, China, 2019. [Google Scholar]
- Pan, C.-Y.; Tsai, C.-L.; Chu, C.-H.; Sung, M.-C.; Huang, C.-Y.; Ma, W.-Y. Effects of physical exercise intervention on motor skills and executive functions in children with ADHD: A pilot study. J. Atten. Disord. 2019, 23, 384–397. [Google Scholar] [CrossRef] [PubMed]
- Silva, L.A.D.; Doyenart, R.; Henrique Salvan, P.; Rodrigues, W.; Felipe Lopes, J.; Gomes, K.; Thirupathi, A.; Pinho, R.A.D.; Silveira, P.C. Swimming training improves mental health parameters, cognition and motor coordination in children with Attention Deficit Hyperactivity Disorder. Int. J. Environ. Health Res. 2020, 30, 584–592. [Google Scholar] [CrossRef] [PubMed]
- Pan, C.-Y.; Chang, Y.-K.; Tsai, C.-L.; Chu, C.-H.; Cheng, Y.-W.; Sung, M.-C. Effects of physical activity intervention on motor proficiency and physical fitness in children with ADHD: An exploratory study. J. Atten. Disord. 2017, 21, 783–795. [Google Scholar] [CrossRef] [PubMed]
- Pan, C.-Y.; Chu, C.-H.; Tsai, C.-L.; Lo, S.-Y.; Cheng, Y.-W.; Liu, Y.-J. A racket-sport intervention improves behavioral and cognitive performance in children with attention-deficit/hyperactivity disorder. Res. Dev. Disabil. 2016, 57, 1–10. [Google Scholar] [CrossRef] [PubMed]
- Kosari, S.; Hemayat-Talab, R.; Arab-Ameri, E.; Keyhani, F. The effect of physical exercise on the development of gross motor skills in children with attention deficit/hyperactivity disorder. Zahedan J. Res. Med. Sci. 2013, 15, e93113. [Google Scholar]
- Ahmed, G.M.; Mohamed, S. Effect of regular aerobic exercises on behavioral, cognitive and psychological response in patients with attention deficit-hyperactivity disorder. Life Sci. J. 2011, 8, 366–371. [Google Scholar]
- Dong, L.S.; Bo, J.; Shen, B.; Pang, Y.L.; Song, Y.; Xing, Y. The Effect of Ten-week Exercise Intervention on Fundamental Motor Skills and Social Ability of Children with Autism Spectrum Disorders. Chin. J. Sport Med. 2021, 40, 171–180. [Google Scholar] [CrossRef]
- Bremer, E.; Lloyd, M. Baseline behaviour moderates movement skill intervention outcomes among young children with autism spectrum disorder. Autism Int. J. Res. Pract. 2021, 25, 2025–2033. [Google Scholar] [CrossRef] [PubMed]
- Feng, Y.Q.; Hou, X.H.; Pan, H.L.; Wu, Y.D.; Ma, Z.M.; Zhu, Z.P. Effects of Aquatic Therapy on Behaviors of Children with Autism: Based on Halliwick Technology. J. Tianjin Univ. Sport 2017, 32, 429–433. [Google Scholar] [CrossRef]
- Pan, C.-Y.; Chu, C.-H.; Tsai, C.-L.; Sung, M.-C.; Huang, C.-Y.; Ma, W.-Y. The impacts of physical activity intervention on physical and cognitive outcomes in children with autism spectrum disorder. Autism Int. J. Res. Pract. 2017, 21, 190–202. [Google Scholar] [CrossRef]
- Arzoglou, D.; Tsimaras, V.; Kotsikas, G.; Fotiadou, E.; Sidiropoulou, M.; Proios, M.; Bassa, E. The effect of [alpha] tradinional dance training program on neuromuscular coordination of individuals with autism. J. Phys. Educ. Sport 2013, 13, 563–569. [Google Scholar]
- Wuang, Y.-P.; Wang, C.-C.; Huang, M.-H.; Su, C.-Y. The effectiveness of simulated developmental horse-riding program in children with autism. Adapt. Phys. Act. Q. 2010, 27, 113–126. [Google Scholar] [CrossRef]
- Den Heijer, A.E.; Groen, Y.; Tucha, L.; Fuermaier, A.B.; Koerts, J.; Lange, K.W.; Thome, J.; Tucha, O. Sweat it out? The effects of physical exercise on cognition and behavior in children and adults with ADHD: A systematic literature review. J. Neural Transm. 2017, 124, 3–26. [Google Scholar] [CrossRef]
- Pontifex, M.B.; Saliba, B.J.; Raine, L.B.; Picchietti, D.L.; Hillman, C.H. Exercise improves behavioral, neurocognitive, and scholastic performance in children with attention-deficit/hyperactivity disorder. J. Pediatr. 2013, 162, 543–551. [Google Scholar] [CrossRef] [PubMed]
- Dishman, R.K.; Berthoud, H.R.; Booth, F.W.; Cotman, C.W.; Edgerton, V.R.; Fleshner, M.R.; Gandevia, S.C.; Gomez-Pinilla, F.; Greenwood, B.N.; Hillman, C.H. Neurobiology of exercise. Obesity 2006, 14, 345–356. [Google Scholar] [CrossRef] [PubMed]
- Berwid, O.G.; Halperin, J.M. Emerging support for a role of exercise in attention-deficit/hyperactivity disorder intervention planning. Curr. Psychiatry Rep. 2012, 14, 543–551. [Google Scholar] [CrossRef]
- Blyth, S.G. The Well Balanced Child Movement and Early Learning; Nanjing Normal University Press: Nanjing, China, 2021. [Google Scholar]
- Verret, C.; Guay, M.-C.; Berthiaume, C.; Gardiner, P.; Béliveau, L. A physical activity program improves behavior and cognitive functions in children with ADHD: An exploratory study. J. Atten. Disord. 2012, 16, 71–80. [Google Scholar] [CrossRef] [PubMed]
- Mortimer, R.; Privopoulos, M.; Kumar, S. The effectiveness of hydrotherapy in the treatment of social and behavioral aspects of children with autism spectrum disorders: A systematic review. J. Multidiscip. Healthc. 2014, 7, 93–104. [Google Scholar]
- Lloyd, M.; MacDonald, M.; Lord, C. Motor skills of toddlers with autism spectrum disorders. Autism Int. J. Res. Pract. 2013, 17, 133–146. [Google Scholar] [CrossRef]
- Nebel, M.B.; Eloyan, A.; Nettles, C.A.; Sweeney, K.L.; Ament, K.; Ward, R.E.; Choe, A.S.; Barber, A.D.; Pekar, J.J.; Mostofsky, S.H. Intrinsic visual-motor synchrony correlates with social deficits in autism. Biol. Psychiatry 2016, 79, 633–641. [Google Scholar] [CrossRef]
- Lin, T.-W.; Kuo, Y.-M. Exercise benefits brain function: The monoamine connection. Brain Sci. 2013, 3, 39–53. [Google Scholar] [CrossRef]
- Caputo, G.; Ippolito, G.; Mazzotta, M.; Sentenza, L.; Muzio, M.R.; Salzano, S.; Conson, M. Effectiveness of a multisystem aquatic therapy for children with autism spectrum disorders. J. Autism Dev. Disord. 2018, 48, 1945–1956. [Google Scholar] [CrossRef]
- Voss, M.W.; Kramer, A.F.; Basak, C.; Prakash, R.S.; Roberts, B. Are expert athletes ‘expert’ in the cognitive laboratory? A meta-analytic review of cognition and sport expertise. Appl. Cogn. Psychol. 2010, 24, 812–826. [Google Scholar] [CrossRef]
- Wang, C.-H.; Chang, C.-C.; Liang, Y.-M.; Shih, C.-M.; Chiu, W.-S.; Tseng, P.; Hung, D.L.; Tzeng, O.J.; Muggleton, N.G.; Juan, C.-H. Open vs. closed skill sports and the modulation of inhibitory control. PLoS ONE 2013, 8, e55773. [Google Scholar] [CrossRef] [PubMed]
- Jeyanthi, S.; Arumugam, N.; Parasher, R.K. Effectiveness of structured exercises on motor skills, physical fitness and attention in children with ADHD compared to typically developing children-A pilot study. eNeurologicalSci 2021, 24, 100357. [Google Scholar] [CrossRef]
- Najafabadi, M.G.; Sheikh, M.; Hemayattalab, R.; Memari, A.-H.; Aderyani, M.R.; Hafizi, S. The effect of SPARK on social and motor skills of children with autism. Pediatr. Neonatol. 2018, 59, 481–487. [Google Scholar] [CrossRef] [PubMed]
- Sarabzadeh, M.; Azari, B.B.; Helalizadeh, M. The effect of six weeks of Tai Chi Chuan training on the motor skills of children with Autism Spectrum Disorder. J. Bodyw. Mov. Ther. 2019, 23, 284–290. [Google Scholar] [CrossRef] [PubMed]
- Pan, C.-Y. The efficacy of an aquatic program on physical fitness and aquatic skills in children with and without autism spectrum disorders. Res. Autism. Spectr. Disord. 2011, 5, 657–665. [Google Scholar] [CrossRef]
- Lourenço, C.; Esteves, D.; Corredeira, R.; Seabra, A. The effect of a trampoline-based training program on the muscle strength of the inferior limbs and motor proficiency in children with autism spectrum disorders. J. Phys. Educ. Sport 2015, 15, 592–597. [Google Scholar]
- Huang, J.; Du, C.; Liu, J.; Tan, G. Meta-analysis on intervention effects of physical activities on children and adolescents with autism. Int. J. Environ. Res. Public Health 2020, 17, 1950. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).