Abstract
A clean environment is essential for human health and well-being. A significant share of total waste is represented by hospital waste that is produced in increasing quantities by sanitary units, with the appearance of the disposable tools. Taking into account the unfavourable environmental impact, the biological danger that this waste represents, and the restrictive legislation imposed by the European Union, urgent measures are needed to reduce their quantities. In this regard, the paper refers to the design of a completely reusable thoracic drainage system and to the positive implications that this system has on the amount of hospital waste. The research starts with the presentation of the medical system from Romania, continues with the classification of the hospital waste, then highlights the dangers and the risks caused by this and analyzes the impact on the sensitive groups. Furthermore, the paper presents the disposable bicameral and tricameral thoracic drainage device systems used in hospitals and then the advantages of using a completely reusable thoracic drainage system. The paper introduces also a research method based on the “opinion questioning”. The method uses a questionnaire with 23 items, addressed to physicians, because, despite restrictive legislation related to hospital waste management, this is not always respected. Each participant of the study works in a different hospital so that the questioned sample is representative.
1. Introduction
1.1. Medical Ambulatory Care in Romania
The medical specialty ambulatory care is provided by specialized units as specialized ambulatories, medical and dental centers, polyclinics, and diagnostic and treatment centres, most of them being located in the urban environment. The network of independent specialty medical practices is also located mostly in the urban environment.
While 10.7 thousand independent specialty medical practices have operated in the urban environment, in the rural environment operated only 403 medical practices. Consequently, in 2016, the number of inhabitants who were allocated to an independent specialty medical practice was about 23 times bigger in the rural environment compared to the urban environment. In 2017, for 10,000 inhabitants in the rural environment were allocated like in 2016, an average number of only 0.4 independent specialty medical practices compared to 10.1 medical practices in the urban environment in 2017 and 9.8 medical practices in 2016 [1,2,3,4].
1.2. Primary Care in Romania
The primary care, provided through the family medical practices, represents the first contact of the population with the medical care system, both for diagnosis and treatment of some diseases and for being subject to preventive health exams. Most of the family medical practices operated in the urban environment, representing 6.6 thousand medical practices, compared to 4.5 thousand medical practices in the rural environment, like in 2016. In the rural environment were allotted to a family medical practice (belonging to the resident population) with 1.3 times more inhabitants compared to a medical practice in the urban environment [3].
1.3. Classification of Hospital Waste
The waste resulted from the medical activity is classified, depending on practical criteria, as non-hazardous waste and hazardous waste. Waste resulted from medical activity represents all the hazardous and non-hazardous waste being produced in the medical unit. Hazardous waste results during the medical activities of diagnostic, treatment, surveillance, preventions of diseases and medical recovery, medical research and production, testing, storage and distribution of medicines and biological products. Non-hazardous waste represents waste assimilated to household waste resulting from the activity of medical, technical and medical, administrative, accommodation, feeding blocks, and food distribution office services. This waste is collected and disposed just like household waste. Household assimilated waste stops to be non-hazardous when it is mixed with any amount of hazardous waste. The following materials are included in the category of non-hazardous waste: packages of sterile materials, infusion vials that did not come in contact with blood or with other biological fluids, gypsum that is not contaminated with biological fluids, paper, food remains (except for those coming from sections of contagious diseases), sacks and other plastic material packaging, glass recipients that did not get into contact with blood or with other biological fluids, etc. [5,6].
Hazardous wastes resulting from healthcare activities are classified in:
- anatomic-pathological wastes and anatomical parts including, biopsy material resulting from surgical and obstetric surgery theatres (fetuses, placentas), anatomical parts from autopsy laboratories, animal corpses resulting from research and experimentation activities;
- infectious wastes representing liquid or solid waste containing or having come in contact with blood or other biological fluids, as well as with viruses, bacteria, parasites and/or toxins of microorganisms (syringes, needles, threaded needles, catheters, tube infusion pumps, containers that contained blood or other biological fluids, surgical drapes, gloves, tubes and other disposable materials, pads, dressings and other contaminated materials, dialysis bags, plastic bags for collecting urine, used laboratory materials [7]);
- sharps and cutting wastes that can cause mechanical lesions by pricking or cutting (needles, threaded needles, catheters, syringes with needle, tube infusion pumps, disposable scalpel blades, pipettes, laboratory glassware that have come in contact with infected materials);
- chemical and pharmaceutical wastes, representing solid, liquid or gaseous chemicals that may be toxic, corrosive or flammable [8];
- radioactive wastes, representing solid, liquid and gaseous wastes from nuclear-medical, diagnostic and treatment activities, containing radioactive materials;
- special wastes which are represented by genotoxic and cytotoxic wastes, pressure vessels, broken thermometers, used batteries, waste generated by the activity of nuclear medicine laboratories, etc [9].
The quantities of waste generated by medical units are increasing, mainly due to the increasing use of disposable materials. In addition, the sterilization of the instrumentation in packaged kits using special porous materials leads to a significant increase in the quantity of wastes. All this packaging is not hazardous if it is not contaminated with blood. The separation of non-hazardous from hazardous waste from the place of generation would also lead to a decrease in the quantity of hazardous wastes [10]. The quantities, as well as the types of waste, resulting from the medical activity vary according to several factors such as the size of the medical health care unit, the characteristics of the activity and services provided, the number of patients assisted or hospitalized, and the time of year. Each producer is responsible for knowing the types and quantities of waste generated and the method for handling, transporting and eliminating the waste. Data recording represents the producer’s method for keeping under control the cycle of generation–transport– and final disposal. The types and quantities of the waste generated by the medical healthcare unit are determined by monthly and quarterly monitoring based on a well-established methodology.
A number of hazards and risks generated by medical wastes are shown below. Contact with hazardous medical wastes may cause illness or injury [11,12]. The risks represented by the medical wastes are caused by the following characteristics: contain infectious agents, are genotoxic, contain toxic or hazardous chemical or pharmaceutical products and can be radioactive. All the individuals coming in contact with hazardous medical wastes are exposed to a potential risk of becoming ill. The individuals working in medical healthcare units generating medical wastes, as well as those working outside these medical units, handling such wastes or coming in contact with them as a result of incorrect handling, are also exposed. The main risk groups are doctors, nurses, healthcare facility support and maintenance staff, patients, visitors, workers providing related services such as laundry, and workers responsible for waste collection, transport, and disposal of the waste within the medical healthcare unit.
1.4. Risks Generated by Infectious and Sharp and Cutting Wastes
The potentially infectious waste may contain a wide variety of pathogenic micro-organisms. Infectious agents can survive in sufficient quantities to cause an infection after coming in contact with these wastes [13]. The basic ways through a person can get ill by contact with potentially infectious waste are: pricking, scratching or cutting through the mucous membranes from the eye, mouth and nose level, and inhaling or ingesting of the infectious agents.
The risks generated by medical wastes creating the greatest concern include the possibility of contracting hepatitis B or C, or AIDS, following pricking by contaminated needles or the contact with blood or other contaminated fluids, or with open wounds or mucous membranes [14].
The presence in the medical healthcare units of the antibiotics resistant bacteria and the chemical disinfectants can contribute to the danger represented by the incorrect waste management. For example, it has been demonstrated that the plasmids from the laboratory samples present in medical wastes, have been transferred to the indigenous bacteria [15].
1.5. Risks Generated by Chemical and Pharmaceutical Wastes
Many chemicals and pharmaceuticals used in medical healthcare units are dangerous due to the fact that they have the following characteristics: they may be toxic, genotoxic, corrosive, flammable or explosive. Larger quantities of such waste are generated when unwanted or expired chemical and pharmaceutical chemicals are eliminated. These can cause poisoning by absorption through the skin or mucous membranes, by inhalation or ingestion. Chemical and pharmaceutical products may also cause lesions on the skin, eyes, mucous membrane of the airways. The most common injuries are the burns. The chemical waste eliminated through the drains may have toxic effects on the water ecosystems in which they were discharged. Pharmaceutical wastes may also have similar effects, as they may contain antibiotics and other drugs, heavy metals, such as mercury, phenol and derivatives, disinfectants and antiseptics [16,17].
1.6. Risks Generated by Chemical Genotoxic Wastes
Great attention must be paid when handling genotoxic wastes, as any release of this type of waste in the environment may have disastrous ecological consequences. Many cytotoxic drugs are very irritating and have local harmful effects on direct contact with the skin or the eyes.
1.7. Risks Generated by the Final Waste Elimination Methods
The incineration of medical wastes containing plastic that includes chlorine, determines the production of dioxin. Dioxin is a known carcinogen. Once formed, dioxin binds to organic particles that are carried by wind, and then it settles on soil and water. The half-life of dioxin is estimated at 25 to 100 years. Dioxin binds to nuclear DNA and it behaves as a potential tumour promoter, weakens the immune response and is associated with many negative effects on development and reproduction (endometriosis, genetic defects, low level of testosterone). All these effects are due to the exposure to low levels of dioxin. Mercury, from the heavy metal group, can be found in thermometers, batteries, fluorescent lamps, etc. The incineration of medical wastes containing heavy metals is forbidden [18,19].
1.8. Thoracic Drainage Systems Used in Hospitals
The pleural drainage is one of the most simple but most useful surgical procedures in the thoracic surgery specialty, most of the time being the only surgical procedure required to save the patient’s life in emergency medical cases, such as pneumothorax, hemothorax, pleural effusion, thoracic wounds, etc. [20].
In a section of thoracic surgery, most patients will have one or more pleural drains during their hospitalization, varying from one day to a few weeks, a situation that is requiring a connection to a pleural drainage system, ensuring the collection of fluids drained from the pleural cavity such as blood, pleural fluid, pus, lymph. Several types of pleural drainage systems are currently known, from a simple collection container called the unicameral system, shown in Figure 1, to bicameral or even tricameral systems.

Figure 1.
The disposable unicameral pleural drainage system.
The disposable bicameral pleural drainage system is shown in Figure 2. As it was mentioned above, a disposable tricameral drainage system as shown in Figure 3 is also currently used. Almost all of these disposable systems are made of plastic being thrown away after a single use, along with the entire quantity of collected liquid. The collected liquids represent biologically contaminated products that persist in the environment for tens or even hundreds of years if they are not neutralized by incineration in special incineration plants, which does not actually happen in 100% of the cases, thus representing a true biological ticking bomb.
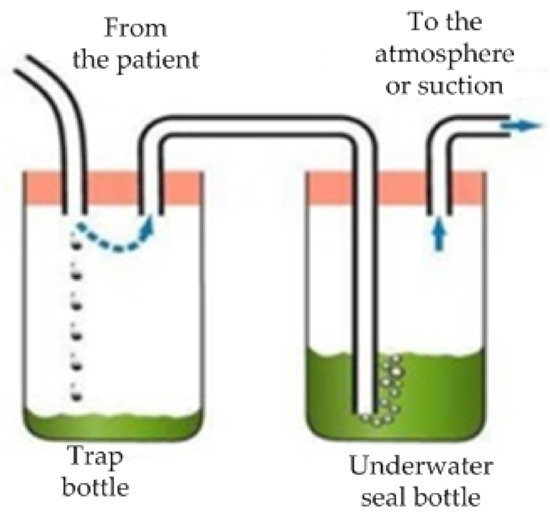
Figure 2.
The disposable bicameral pleural drainage system.

Figure 3.
The disposable tricameral thoracic drainage system.
In the medical literature is known and used in practice a pleural effusion drainage device consisting of a double lumen central venous catheter connected with a transfusion joint and a conical joint through a pipe connecting device. In this model, at the one bottom, the pipe connections are mounted between the transfusion joint, cone joint, and the pipe connecting device. The bottom of the cone is connected to the pipe and in the middle of the pipeline, there is an hourglass passage with a filter mesh and a flow regulating device which is externally disposed on the lower part of the hourglass. The second bottom of the pipe is connected to a disposable drainage bag, the device being safe, airtight, sterile and portable.
The disadvantages of the current solutions mentioned above, mainly refers to the fact that all of these devices allow only a single use, being subsequently destroyed by incineration together with the collected biological content, or eliminated in the environment, where they will persist for tens or hundreds of years during the entire lifetime of the plastic material they are made of, representing a real biological hazard. In addition, the use of these devices is very expensive, particularly due to the fact that they are disposable.
Taking into consideration the aforementioned aspects, it would be very beneficial to design a completely reusable thoracic drainage system, ensuring on one hand, the patient’s protection against infection with various viruses or other pathogens and on the other hand solving those two weak issues of the traditional drainage systems regarding the biological danger generated by their elimination in the environment and the high costs due to their disposable character.
2. Materials and Methods
2.1. The Completely Reusable Thoracic Drainage System Design
This paper presents an invention of a completely reusable thoracic drainage system which solves the problems related to the traditional drainage systems. This complete and reusable thoracic drainage system is used in the chest cavity surgical procedures where the patient’s pleural drainage is necessary. The constructive scheme of the completely reusable thoracic drainage system is presented in Figure 4.
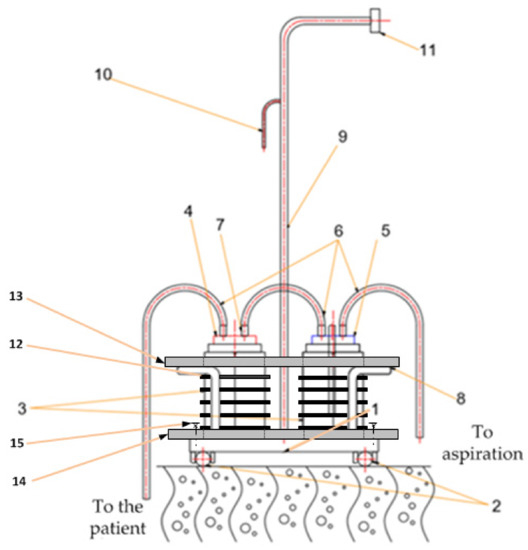
Figure 4.
The constructive scheme of the complete and reusable pleural drainage system: 1—supporting plate; 2—legs; 3—graduated glass containers; 4—silicone covers; 5—centering prism; 6—tube connections; 7—communication channels; 8—supporting wires; 9—rod; 10—hook; 11—handle; 12—rubber protection ring; 13—upper protection plate; 14—lower protection plate; 15—fixing screw.
As it can be noted from Figure 4, the complete reusable thoracic drainage system, according to the invention, consists of a metal supporting device with a supporting plate with legs, two supporting wires for securing two graduated glass containers with silicone covers, with two, respectively three communication channels made of stainless steel that can be connected by silicone tube connections (the only disposable elements!) interconnecting and connecting to the patient’s pleural cavity and to an air suction device, a rod with a handle being also clamped on the supporting plate, due to which the system can also be used for support, as well as a hook for securing the entire device on stretchers or wheelchairs for transporting the patients. The only disposable elements are the silicone tube connections. The protection against the breakage of the graduated glass containers is ensured by five rubber rings attached to each container and by using two lower and upper protection plates made of duroflex. Keeping in mind that duroflex is a reinforced rubber with a higher rigidity than regular rubber, the two protection plates, protect against the breakage of graduated containers in the event of overturning the entire device. The lower protection plate is secured to the base plate by four screws placed in the corners. In this way, the whole system is rigid, providing, for each container, the blocking of all six freedom degrees in space, providing in this way the protection against breakage.
The technical problem solved by the thoracic drainage system invented is obtaining a completely reusable and ergonomic chest drainage system, easy to handle by the medical staff, as well as by the patient, its main advantage being the special environmentally friendly character due to the fact that it minimizes the required disposable material for each patient and completely safe re-use, in optimal conditions, of a large part of the system after decontamination and re-sterilization. Also, we consider that the complete reusable thoracic drainage system can be used for support, by the patient, but in this regard, we have not yet tested on patients. To prevent the cracking of the graduated glass containers, five removable rings made of rubber with thickness and width of 5 mm can be mounted on their circumference. These rings are discharged prior to sterilization and have only a protective role against the breakage of containers as a result of accidental overturns. The jars and caps of the thoracic drainage system presented in the paper are sterilized by autoclaving. The silicone from which the caps are made is resistant to 134 degrees Celsius for autoclaving. The glass is much more resistant at the temperature than the silicone. The complete thoracic drainage system invented is very easy to assemble and in this regarding Figure 5a can be observed the system assembled according to the invention and in Figure 5b the semi-assembled system.
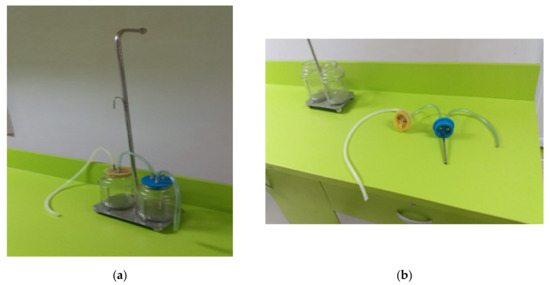
Figure 5.
The construction of the complete reusable thoracic drainage system: (a) completely assembled system; (b) semi-assembled system.
During the treatment of the patients in the thoracic surgery section, it was necessary to use certain devices. These devices were created in the past according to a certain vision and using technologies and materials outdated today. More concretely, it was necessary to make a “customized plug/stopper” with the following functionalities and restrictions: to serve as human medical devices and to be capable of multiple and repeated use, with the possibility of sterilization under required conditions. Constructively, the plug/stopper has many execution constraints. Some of these elements are further exemplified:
- its shape and size must be unique, relative to the container in which it is mounted, totally dimensionless for the vessel of the products used at present
- its shape should be slightly troconic for easy mounting/dismounting by the specialized medical staff and for achieving its functional purpose for which it was designed
- the materials used in the manufacture of the plug/stopper are two-silicone component approved and recommended for human medical devices, stainless steel pipe, guide, fastening and centering elements, these elements being adjusted only for this product.
For the stopper fabrication, a mold was designed in a CAD/CAM program. Then the mold was built using a 3D printer. The details of silicone fabrication, molding and blending until the homogeneity was achieved, have been respected. The silicone was molded in the vacuum controlled environment in order to achieve the performance required by the final product. To avoid the premature destruction, have been used centering prisms fabricated from inert material to the casting process and subsequent sterilization, as can be seen in Figure 6.
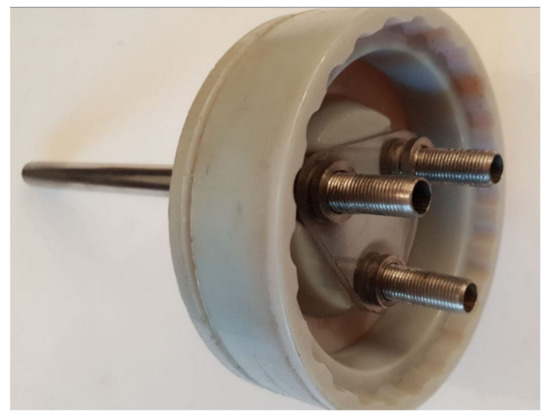
Figure 6.
The construction of the centering prism.
These prisms were 3D modelled and then cut with laser technology for the accuracy of the pipes centering holes and the tightness needed in the vacuum of the device. The nuts were dimensionally in order to reduce the weight of the product and the pipes were turned on the heads of an automatic lathe, as can be seen in Figure 7.

Figure 7.
The connection elements.
The complete reusable thoracic drainage system presents some advantages compared to the classic systems, some of them being presented below. Therefore the innovative system minimizes the amount of medical waste collected by the reusable feature of the device and the collected biological liquids can be removed by simply decanting from the collector container in the bio-waste containers existing in each surgical section. The only consumables requiring neutralization by incineration is a silicone tube with approximately 120 cm length and 10 mm diameter, all the other components being reused and decontaminated. Through the robustness of the system components (metallic support), the device can be used for support by the patient, allowing rapid postoperative mobilization and shortening the duration of hospitalization. Cost reductions should also be mentioned because the only consumable is the silicon tube. We must mention that the innovative system has not been tested on an industrial scale on humans, but in this regard, we will address to the National Agency for Medicines and Medical Devices from Romania.
The major disadvantage of the classical thoracic drainage solution compared to the innovative system presented in the paper, refers to the fact that all classical devices allow one single use, being subsequently destroyed by incineration together with the biologically collected content or removed to the environment where tens or hundreds of years will remain, representing a real biological danger.
2.2. Samples
422 doctors were chosen from the hospitals in all of Romania who filled in the questionnaire related to their opinion/attitude regarding the collection and destruction of hospital wastes and the utilisation of some modern completely reusable devices used for thoracic drainage. The questionnaire was applied by phone or on-line (through e-mail or social networking means). The discussed subjects were of great interest to the doctors and the rate of responsiveness was of 93.77% (from the total of 450 interviewed doctors, 15 refused to answer and 13 answered incompletely, so their questionnaires were eliminated).
2.3. Developed Questionnaire
The chosen research method was based on the “questioning of opinion” starting from a questionnaire with 23 items presented in Table 1, addressed to the doctors because, in spite of the restrictive legislation related to the storing and destroying of hospital wastes, it is not always observed. Each participant in the study works in a different hospital, therefore the questioned sample group is illustrative.

Table 1.
Items related to the collection and recycling of wastes and the utilization of fully reusable devices.
The set of questions and the variants for answers were developed by consulting the representatives of the Craiova College of Physicians. They analysed carefully the legislation and the provisions in force, the medical practice in the field, and they had preliminary discussions even with Romanian doctors in the European Union. The items were conceived so as to identify, on the one hand, the factors which determine the inadequate recycling of hospital wastes and on the other hand, to test the availability of implementing new medical devices, like the thoracic drainage one, that is fully reusable. The questions were of an open type. The interviewed doctors were informed about the subject of the questionnaire and its purpose, and they were asked if they agreed to participate in the study. If the doctors did not have enough time to answer the questionnaire by phone, it was sent to them to be filled in via e-mail. All the data was centralized and processed in Excel.
The questionnaire has four sections. The first section refers to the collection of hospital wastes and the implementation of the fully reusable devices for thoracic drainage, the second section asks questions about the attitude regarding the procedure of collecting and incinerating hospital wastes, the third section refers to the knowledge related to the pollution of the environment with hospital wastes and the final section asks questions about certain social and demographic characteristics.
3. Results
3.1. Social and Demographic Characteristics
As one may notice in Table 2, with regard to the social and demographic characteristics of the sample group of 422 questioned medical practitioners, 70.61% come from the urban area, 82.9% from independent hospitals, 71.09% are doctors and 59.24% are younger than 35 years old.

Table 2.
Social and demographic characteristics of the sample group.
3.2. Collection of Hospital Wastes and Implementation of Fully Reusable Devices for Thoracic Drainage
The habits of the hospitals related to collecting/recycling of wastes are illustrated in Table 3, where it can be noticed that out of the sample group of 422 medical practitioners who were questioned with regard to the hospital wastes and the implementation of fully reusable devices for thoracic drainage, 83.4% have responsibilities concerning decision making, 92.18% answered that the hospitals collected the wastes in order to incinerate them, 49.6% showed that the annual costs for collecting and recycling was up to EUR 100 and 46.20% showed that the hospital collected annually less than 50 kg of wastes. Furthermore, it turns out that 65.16% of the respondents stated that they utilized fully reusable devices for thoracic drainage and 34.84% of them did not know what amount of wastes resulted from the thoracic drainage. 50.94% of the respondents stated that the amount of hospital wastes decreased through the utilizing of fully reusable devices for thoracic drainage and 93.60% of them stated that it was not normal for the hospital to bear the expenses for the collecting and recycling of hospital wastes.

Table 3.
Habits of the hospitals related to collecting/recycling of hospital wastes.
3.3. Attitude Regarding the Procedure (Legislation)
Regarding the assessment of the waste collecting procedure, as it can be seen in Table 4, 24.22% from the questioned group consider that the procedure is not satisfactory at all. It is noticeable that in a percentage of 31.99% the hospital procedure was not observed in what concerns collection and recycling of the wastes. With regard to the information concerning the legislation for collection and recycling, 43.86% consider that they are little informed and 42.41% consider that the legislation is incomplete.

Table 4.
Opinion of the medical practitioners about the collecting procedure.
As it can be seen in Table 5, out of a number of 102 medical practitioners who think that the hospital waste collection and recycling procedure is not satisfactory at all, 41.19% consider that, as an alternative to the procedure in force, the creation of regional hospital waste collecting centres would be advisable, and 15% take into account as an alternative the hiring of a specialized company that would handle, at the level of the sanitary unit, the collection and destruction of hospital wastes.

Table 5.
Alternative procedures suggested by the medical practitioners.
According to the data in Table 6, out of the total number of 135 respondents who stated that there were cases when the hospital procedure related to hospital waste collection and recycling was not fully complied with, 38.53% explained that this happened because the procedure was too difficult and time-consuming. Only 11.1% of the respondents think that the reason for the non-compliance with the procedure of hospital waste collecting was the policy of the hospital.

Table 6.
The main reasons for non-compliance with the hospital waste collecting procedure.
3.4. Attitude Related to the Hospital Waste Pollution
In the opinion of practitioners in relation to hospital waste pollution (Table 7), out of the total of 422 doctors interviewed, 41.48% believe they are poorly informed about the dangers of this type of waste, and 3.55% are very little informed; it can also be seen that 60.32% believe it is extremely important to achieve a higher level of information for the population regarding hospital waste pollution, while 2.6% believe that this would have very little importance.

Table 7.
Attitude of the medical practitioners in relation to the pollution with hospital wastes.
4. Conclusions
The complete and reusable thoracic drainage system presented in this paper has the main advantage the environmentally friendly feature, due to minimization of the quantity of disposable components required for each patient, as a large part of the system elements can be safely re-used after decontamination.
The research also found that there are some deficiencies in the hospitals of Romania regarding the collection and recycling of the hospital waste that need to be corrected. Hospitals should have a greater involvement in the collection and recycling of the medical waste by a better empowering of the staff, better information on legislation regarding the collection and recycling of medical waste, use safety conditions, and use as many reusable medical devices as possible.
By the results of the research done in the Romanian hospitals, the complete reusable devices for thoracic drainage are used in a satisfactory proportion, which determines the significant decrease of the amount of hospital waste. Also, the reusable systems eliminate a number of disadvantages related to waste management, existing in the case of the classic disposable drainage systems.
Author Contributions
A.D.D., M.C.C., A.S., O.R.C. and G.P. have patented the device. C.B., G.M., O.N. and I.M. have contributed to the experimental research, the writing of the paper and its translation.
Funding
This research received no external funding.
Conflicts of Interest
The authors declare no conflict of interests.
References
- NafizKorkut, E. Estimations and analysis of medical waste amounts in the city of Istanbul and proposing a new approach for the estimation of futuremedical waste amounts. Waste Manag. 2018, 81, 168–176. [Google Scholar]
- Kalogiannidou, K.; Nikolakopoulou, E.; Komilis, D. Generation and composition of waste from medical histopathology laboratories. Waste Manag. 2018, 79, 435–442. [Google Scholar] [CrossRef] [PubMed]
- Qin, L.; Xing, F.; Zhao, B.; Chen, W.; Han, J. Reducing polycyclic aromatic hydrocarbon and its mechanism by porous alumina bed material during medical waste incineration. Chemosphere 2018, 212, 200–208. [Google Scholar] [CrossRef] [PubMed]
- Su, E.C.Y.; Chen, Y.T. Policy or income to affect the generation of medical wastes: An application of environmental Kuznets curve by using Taiwan as an example. J. Clean. Prod. 2018, 188, 489–496. [Google Scholar] [CrossRef]
- Komilis, D.; Makroleivaditis, N.; Nikolakopoulou, E. Generation and composition of medical wastes from private medical microbiology laboratories. Waste Manag. 2017, 61, 539–546. [Google Scholar] [CrossRef] [PubMed]
- Windfeld, E.S.; Brooks, M.S.L. Medical waste management—A review. J. Environ. Manag. 2015, 163, 98–108. [Google Scholar] [CrossRef] [PubMed]
- Papamarkou, S.; Sifaki, C.; Tsakiridis, P.E.; Bartzas, G.; Tsakalakis, K. Synthetic wollastonitic glass ceramics derived from recycled glass and medical waste incinerator fly ash. J. Environ. Chem. Eng. 2018, 6, 5812–5819. [Google Scholar] [CrossRef]
- Klein, A. Medical waste chemicals found in beetles. New Sci. 2018, 240, 7. [Google Scholar] [CrossRef]
- Mastorakis, N.E.; Bulucea, C.A.; Oprea, T.A.; Bulucea, C.A.; Dondon, P. Environmental and health risks associated with biomedical waste management. Dev. Energy Environ. Econ. 2010, 287–294. Available online: https://www.researchgate.net/profile/Nikos_Mastorakis2/publication/278805529_Environmental_and_health_risks_associated_with_biomedical_waste_management/links/57f2406508ae280dd0b355e0.pdf (accessed on 17 May 2019).
- Mastorakis, N.E.; Bulucea, C.A.; Oprea, T.A.; Bulucea, C.A.; Dondon, P. Holistic approach of biomedical waste management system with regard to health and environmental risks. Int. J. Energy Environ. 2011, 5, 309–318. [Google Scholar]
- Bataduwaarachchi, V.R.; Weeraratne, C.L. Global medication waste management practices: Challenges and opportunities in developing countries. Int. J. Basic Clin. Pharmacol. 2016, 5, 2290–2294. [Google Scholar] [CrossRef]
- Blenkharn, J.I. Healthcare Wastes. In Reference Module in Earth Systems and Environmental Sciences; Elsevier: Amsterdam, The Netherlands, 2015. [Google Scholar] [CrossRef]
- Bungau, S.; Tit, D.M.; Fodor, K.; Cioca, G.; Agop, M.; Iovan, C.; Nistor Cseppento, D.C.; Bumbu, A.; Bustea, C. Aspects regarding the pharmaceutical waste management in Romania. Sustainability 2018, 10, 2788. [Google Scholar] [CrossRef]
- Bungau, S.; Suciu, R.; Bumbu, A.; Cioca, G.; Tit, D.M. Study on hospital waste management in medical rehabilitation clinical hospital, Baile Felix. J. Environ. Prot. Ecol. 2016, 16, 980–987. [Google Scholar]
- Komilis, D.P. Issues on medical waste management research. Waste Manag. 2016, 48, 1–2. [Google Scholar] [CrossRef] [PubMed]
- Ruhoy, I.S.; Daughton, C.G. Types and quantities of leftover drugs entering the environment via disposal to sewage—Revealed by coroner records. Sci. Total Environ. 2007, 388, 137–148. [Google Scholar] [CrossRef] [PubMed]
- Seehusen, D.A.; Edwards, J. Patient practices and beliefs concerning disposal of medicines. J. Am. Board Fam. Med. 2006, 19, 542–547. [Google Scholar] [CrossRef] [PubMed]
- Oli, A.N.; Ekejindu, C.C.; Adje, D.U.; Ezeobi, I.; Ejiofor, O.S.; Ibeh, C.C.; Ubajaka, C.F. Healthcare waste management in selected government and private hospitals in Southeast Nigeria. Asian Pac. J. Trop. Biomed. 2016, 6, 84–89. [Google Scholar] [CrossRef]
- Abah, S.O.; Ohimain, E.I. Healthcare waste management in Nigeria: A case study. J. Public Health Epidemiol. 2011, 3, 99–110. [Google Scholar]
- Longe, E.O.; Williams, A. A preliminary study on medical waste management in Lagos Metropolis, Nigeria. J. Environ. Health Sci. Eng. 2006, 3, 133–139. [Google Scholar]
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).