1. Introduction
The duration of orthodontic treatment presents a significant challenge for both orthodontists and patients, and even deters some patients from undergoing treatment [
1]. Shortening the duration of orthodontic treatment is a primary goal for both orthodontists and patients, especially adult patients [
2], as prolonged treatment can lead to adverse effects such as root resorption, periodontal disease, and dental caries [
3,
4]. Furthermore, patients often experience discomfort and pain associated with various stages of therapy, with pain being the most disliked aspect of orthodontic treatment [
5].
Several methods have emerged to improve orthodontic tooth movement and shorten the duration of orthodontic treatment, with surgical methods being the most popular, including traditional corticotomy [
6,
7], and interseptal alveolar surgery. However, these techniques have shown low acceptance among patients due to their invasive nature and postoperative complications.
Minimally invasive techniques, such as piezocision [
8,
9], micro-osteoperforations (MOPs) [
10], corticision [
11], and laser-assisted flapless corticotomy [
12], have gained popularity due to their ability to minimize postoperative discomfort and reduce recovery time. On the other hand, non-surgical interventions like low-level laser therapy (LLLT) [
13,
14], light vibrational forces [
15], light-emitting diodes [
16], and pulsed electromagnetic waves [
17] are currently widely used.
LLLT has been shown to be effective in accelerating tooth movement and reducing pain, as supported by recent studies [
14,
18]. Consequently, there is a growing interest in using LLLT as an adjunct to traditional orthodontic treatment to take advantage of the acceleration properties of minimally invasive methods and the analgesic and acceleration properties of LLLT [
19,
20].
Reviewing the literature reveals some recent research work combining two or more acceleration methods to accelerate the orthodontic movement, such as combining self-ligating brackets with one or more acceleration methods [
21], or the use of LLLT with minimally invasive methods like corticotomy [
22], MOPs [
23], and piezocision for canine retraction [
24]. A recent systematic review showed that there were several published studies about the levels of pain and discomfort when using surgically assisted acceleration methods [
25]. However, no studies have examined patient-reported outcome measures associated with the combination of piezocision with LLLT in the context of the en masse retraction of upper anterior teeth. Therefore, the aim of the current RCT was to assess the patient-reported outcome measures when accelerating the en masse retraction of upper anterior teeth in adult patients using piezocision combined with the subsequent application of LLLT compared to piezocision alone, or with no acceleration method.
The null hypothesis (H0) stated that there were no significant differences between the piezocision plus subsequent LLLT application, piezocision alone, and traditional en masse retraction groups in terms of the levels of pain, discomfort, swelling sensation, chewing difficulties, satisfaction, and acceptance at all assessment times.
The research hypothesis (H1) stated that there were significant differences between piezocision with subsequent LLLT application, piezocision alone, and traditional en masse retraction groups in the levels of pain, discomfort, swelling sensation, chewing difficulties, satisfaction, and acceptance at all assessment times
3. Statistical Analysis
SPSS® Version 20 (SPSS for Windows, version 20, IBM Corporation, New York, NY, USA) was the chosen software for statistical analysis. The Shapiro–Wilk test was used to distinguish the normal distribution of data. One-way ANOVA test or its alternative nonparametric test (i.e., Kruskal–Wallis test) was utilized to make a comparison between the three groups. For pairwise comparisons, the post hoc Bonferroni, LSD, or Games–Howell tests, or the latter’s alternative nonparametric test (i.e., Mann–Whitney test) was applied. Bonferroni’s correction of the significance level was applied due to the multiplicity of pairwise comparisons, and the results of all tests were considered significant at p ≤ 0.017.
5. Discussion
The current study appears to be the first randomized clinical trial that evaluates the patient-reported outcome measures when using the combined piezocision-LLLT-assisted en masse retraction of upper anterior teeth in comparison with the precision-only-assisted retraction and the traditional method. Various surgical techniques have been developed to expedite dental movement, primarily relying on cortical cutting. These include traditional corticotomy [
28], vestibular incision subperiosteal tunnel access [
29], and flapless corticotomy using piezosurgery [
30]. Among these, piezocision was selected for our study because it is considered the least aggressive among the methods mentioned. Surgical procedures for accelerating orthodontic tooth movement can be adopted in daily orthodontic treatment, provided they do not put an additional burden on patients, such as pain, discomfort, or functional impairments [
25].
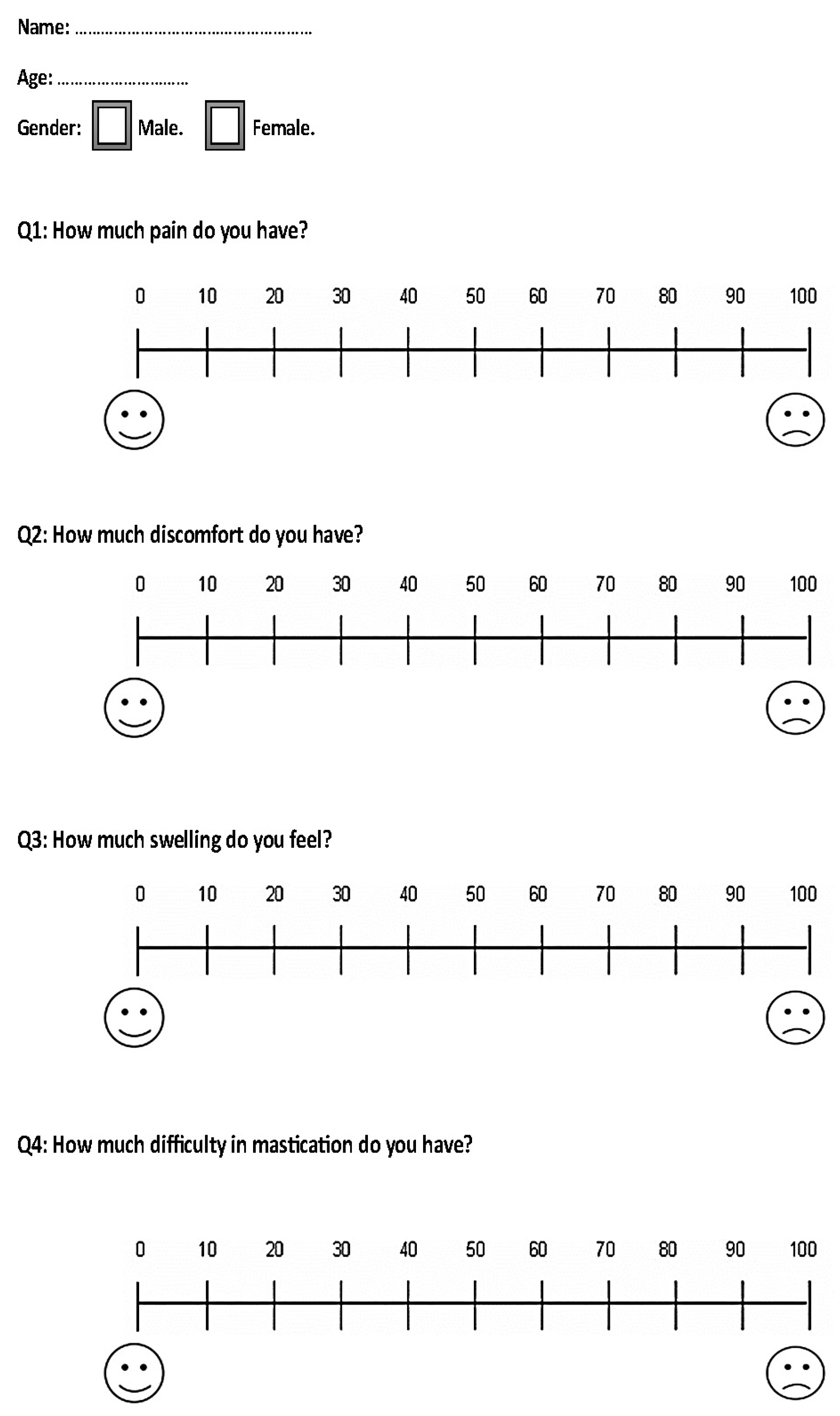
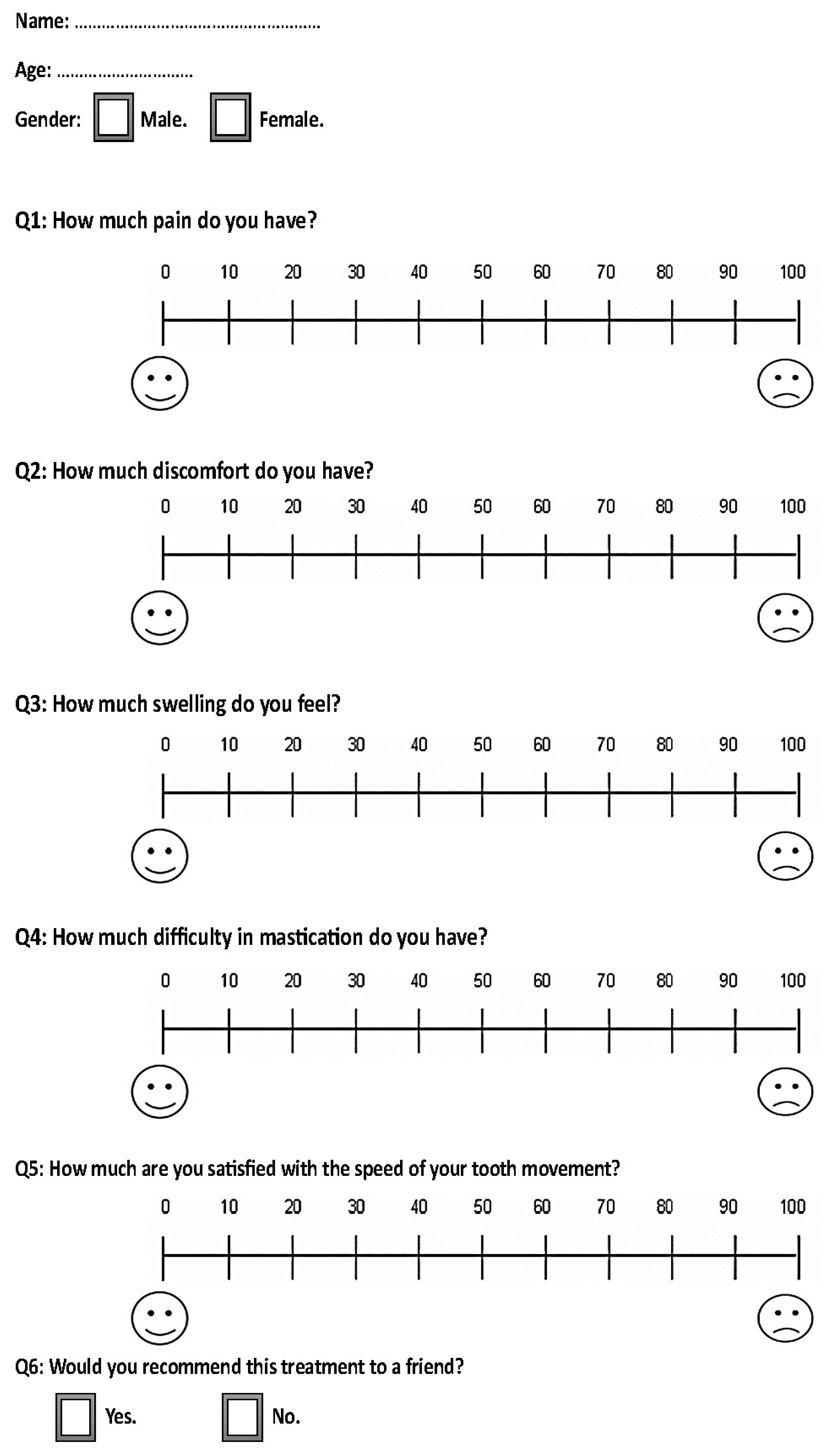
The VAS was used in this study for pain assessment. Despite its widespread acceptance in clinical research, it is crucial to note that the VAS is inherently subjective. This subjectivity is rooted in the fact that pain is a deeply personal experience. As such, the VAS scores reported in this study reflect the participants’ individual perception of their pain. This could potentially introduce a degree of variability into our results. However, despite this potential limitation, the VAS continues to be a valuable tool in research due to its simplicity and adaptability.
The patient-reported outcome measures were evaluated in the first and third months of retraction. The piezocision was only applied in the first month for both experimental groups, whereas the LLLT was only applied in the FC+LLLT experimental group in the third month.
5.1. The First Month of Assessment
Given that piezocision was applied in both experimental groups before retraction, the comparisons made are confined to the first month only regarding studies that employed piezocision-assisted orthodontic tooth movement. The pain and discomfort levels were in the ‘mild to moderate’ category after 24 h of retraction in the three groups. However, after 72 h of retraction, they were classified as ‘mild to moderate’ in the experimental groups, and ‘mild’ in the control group. Additionally, the levels of pain and discomfort were significantly greater in FC+LLLT and FC groups compared to the control group after 12, 24, and 72 h (p < 0.001). The greater pain levels in both FC+LLLT and FC groups may be attributed to the surgical procedure applied to the patients of these groups compared to the control group.
The current results were inconsistent with those of the study of Hatrom et al. [
31], in which the pain levels were mild in the piezocision and control groups during the first 24 h after the initiation of retraction. This discrepancy may be attributed to the fact that in the current trial, incisions were made on both the buccal and palatal sides of the alveolar bone, whereas in Hatrom’s study, the incisions were only placed buccally.
The results of this study disagreed with those reported by Alfawal et al., who evaluated the patient-reported outcome measures associated with canine retraction accelerated by piezosurgery or laser-assisted flapless corticotomy in a compound design RCT. Alfawal et al. found that the levels of pain were moderate and the levels of discomfort were severe in the piezocision group after 24 h of canine retraction in the Alfawal et al. study [
32]. This inconsistency may be due to the difference in the onset of retraction force, which was on the same day of the surgical intervention in the study of Alfawal et al. [
32], whereas it was four days postoperatively in the current work. The study of Alfawal et al. had a compound design, i.e., two parallel groups with a split-mouth design in each group. This kind of study design may distort patient perception of pain that may originate only from one side of the mouth. Additionally, the assessment of pain on one side of the mouth does not provide a whole picture of the pain that would be encountered when the procedure is performed bilaterally [
25].
Patient perception of swelling was ‘mild to moderate’ in the experimental groups and ‘mild’ in the control group after 12, 24, and 72 h of retraction. This can be attributed to edema caused by the surgical procedure in both the FC+LLLT and FC groups. This is consistent with a study by Gibreal et al., which also found increased perception of swelling following piezocision-assisted leveling and alignment [
27].
After 24 h of retraction commencement, patients in the experimental groups reported ‘moderate’ levels of chewing difficulty, while those in the control group reported ‘mild to moderate’ levels. Then, after 72 h, the levels of chewing difficulties decreased to the ‘mild to moderate’ category in the experimental groups and were classified as mild in the control group. This can be attributed to the pain and swelling caused by the surgical procedure in the FC+LLLT and FC groups. These findings are consistent with those reported by Alfawal et al. and Gibreal et al. [
27,
33].
5.2. The Third Month of Assessment
In the third month of retraction, frequent LLLT application was continued in the FC+LLLT group, while the FC and CONT groups did not undergo any further intervention. The primary aim of the laser application was to accelerate orthodontic tooth movement, as previous reports have demonstrated that laser irradiation can accelerate the en masse retraction of upper anterior teeth by 26–54% [
34,
35,
36]. However, in this study, the focus was on patient-centered outcomes during the acceleration of orthodontic tooth movement, with the application of laser from the sixth week following retraction initiation. Therefore, comparisons in the third month were made with other studies that have utilized LLLT-assisted acceleration.
After 12, 24, and 72 h of re-activating the coil springs for the en masse retraction, patients in the FC+LLLT group experienced lower levels of pain and discomfort compared to the FC and CONT groups. After 24 h, the levels were classified as ‘mild to moderate’ in the FC and CONT groups, while they were classified as ‘mild’ in the FC+LLLT group. These lower levels in the FC+LLLT group can be attributed to the dual mechanism of low-level laser therapy, which targets both local and systemic aspects of pain [
37], in addition to its role in accelerating orthodontic tooth movement.
The results of this study agreed with those reported by Bhat et al., who found that the LLLT was effective in relieving pain when retracting upper anterior teeth [
20]. However, the pain level was assessed only at one time point, which was 7 days after laser application, when most of the pain resulting from orthodontic treatment had already subsided spontaneously [
38].
On the other hand, the results of this study disagreed with those of the study of Dalaie et al., who studied the effects of LLLT on canine retraction in a split-mouth-designed RCT. They found that the pain levels were classified as ‘mild to moderate’ after 24 h of retraction in both the experimental and control groups, with no differences between them [
39]. This discrepancy can be explained by the differences in laser irradiation parameters. In their study, the retracted canines in the LLLT group were irradiated with an 880 nm Ga-Al-As laser at a dosage of 5 j/cm2 for 10 s at 8 spots, while in the current study, a similar device was used but with a dosage of 4 joules/point for 15 s per point at 32 spots.
The levels of chewing difficulty were classified as ‘mild’ in the FC+LLLT group, whereas they were ‘mild to moderate’ in the FC and CONT groups at 24 h following force application in the third month. This can be explained by the effect of LLLT in the FC+LLLT group, which resulted in reduced levels of pain, and, therefore, reduced chewing difficulties.
The assessment of patient satisfaction in OTM speed with the applied acceleratory procedures revealed a high level of satisfaction in both experimental groups, but the mean scores were greater in the FC+LLLT group than the FC group, and this could be explained by the additional effect of LLLT during the third month of treatment. The finding of high satisfaction was similar to what was observed by Alfawal et al., who reported a mean VAS satisfaction score of 82.94 mm. Additionally, there was an agreement with the study of Khlef et al., which evaluated the patient-reported outcome measures associated with piezocision-assisted en masse retraction of upper anterior teeth, and found that most patients in the piezocision group would recommend the accelerated treatment modality to their friends [
40].