Abstract
Since their discovery, cancer stem cells have become a hot topic in cancer therapy research. These cells possess stem cell-like self-renewal and differentiation capacities and are important factors that dominate cancer metastasis, therapy-resistance and recurrence. Worse, their inherent characteristics make them difficult to eliminate. Colorectal cancer is the third-most common cancer and the second leading cause of cancer death worldwide. Targeting colorectal cancer stem cells (CR-CSCs) can inhibit colorectal cancer metastasis, enhance therapeutic efficacy and reduce recurrence. Here, we introduced the origin, biomarker proteins, identification, cultivation and research techniques of CR-CSCs, and we summarized the signaling pathways that regulate the stemness of CR-CSCs, such as Wnt, JAK/STAT3, Notch and Hh signaling pathway. In addition to these, we also reviewed recent anti-CR-CSC drugs targeting signaling pathways, biomarkers and other regulators. These will help researchers gain insight into the current agents targeting to CR-CSCs, explore new cancer drugs and propose potential therapies.
1. Introduction
In 1994, John and Bonnet isolated and identified cancer cells with stemness from leukemia cells and proposed the concept of “leukemia stem cells (LSCs)” [1]. This was the first confirmation of the existence of stem cells in cancer, a major breakthrough in the field of cancer stem cell (CSC) research. In 2003, Dontu and colleagues isolated CSCs from breast cancer cells [2], providing the first proof of the existence of CSCs in solid tumors. In the following years, CSCs were found in brain tumors, prostate cancer, lung cancer, colorectal cancer and other tumors [3,4,5,6]. Nowadays, the theory of CSCs has gained consensus and has attracted much attention in cancer treatment research. CSCs are a small population of cancer cells with stemness like stem cells. They can achieve self-renewal through symmetrical division and asymmetric division to produce daughter cells with stemness or normal cancer cells [7]. Moreover, CSCs are capable of forming cancer cells with different degrees of differentiation and reassembling the complete cancer cell repertoire of the original cancer. In addition, normal cancer cells without CSC properties can dedifferentiate back into CSCs through a bidirectional interconversion process [8,9]. Normal cancer cells without CSC properties can dedifferentiate back into CSCs through a bidirectional interconversion process [10]. This is a major reason for cancer cell heterogeneity [11]. Cancer cells with or without CSC characteristics must be eradicated to achieve good therapeutic effects. During cancer development, CSCs are important factors that lead to metastasis, therapy-resistance and recurrence [12,13,14]. CSCs are often accompanied by an epithelial to mesenchymal transition phenotype, and they interact with stromal cells, endothelial cells and others to promote angiogenesis, promote stem-like cancer cell differentiation and accelerate metastasis [15]. The cell cycle of CSCs arrests in the G0 phase, so they are resistant to cycle specific chemotherapy drugs [16]. Due to their DNA synthesis asynchrony and enhanced DNA repair, CSCs are resistant to DNA damaging drugs [16]. Moreover, CSCs highly express drug transporters and anti-apoptotic proteins such as Bcl-2, which endows them with the ability to pump chemotherapy drugs out of the cell and resist programmed cell death [16]. Recent research has suggested that resting cancer stem cells can evade immune surveillance and lay the seeds for cancer recurrence [17,18]. This makes CSCs more difficult to eliminate than other cancer cells.
Colorectal cancer (CRC) is the third most common malignant tumor type. In recent years, with the popularization of early screening for colorectal cancer and the advancement of treatment methods, the mortality rate associated with colorectal cancer has decreased [19]. However, metastasis and recurrence are still the leading causes of death in most end-stage CRC patients. Reducing metastasis and recurrence remains an urgent problem in CRC therapy. Colorectal cancer stem cells (CR-CSCs) may be the initial cells of colon cancer [20], promoting colon cancer metastasis [21,22] and also one of the main culprits of therapy-resistance and recurrence [23] (Figure 1). Eliminating CR-CSCs can promote therapeutic effects against colon cancer [24,25,26]. Here, we reviewed the origin and identification of colorectal stem cells, and we summarized the potential therapeutic targets of CR-CSCs and the current research status of agents targeting CR-CSCs. This will help researchers to gain insight into the current agents targeting CR-CSCs, explore new drugs and propose potential therapies.
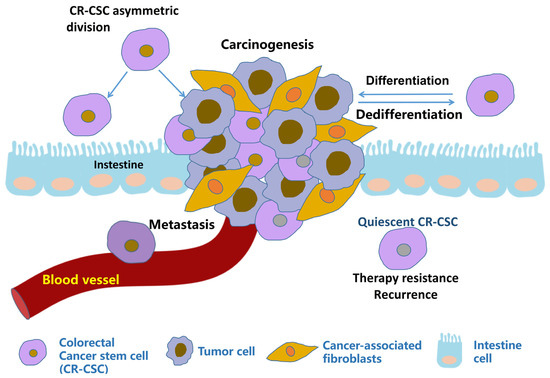
Figure 1.
Illustration of metastasis, therapy resistance and recurrence promoted by CR-CSCs.
CR-CSCs not only divide into CR-CSCs, but can also produce ordinary cancer cells through proliferation or differentiation. Due to their quiescent state, high differentiation activity, secreting cytokines to make normal cells malignant and other properties, CR-CSCs can promote metastasis, therapeutic resistance and recurrence.
2. Colorectal Cancer Stem Cells
2.1. Origin of CR-CSCs
Researchers generally consider CSCs to have two main origins, derivation from normal cells that acquire mesenchymal properties [27] or transformation from normal adult stem cells [28]. The same holds true for the origin of CR-CSCs. In intestine, leucine-rich repeat-containing G-protein coupled receptor 5 (Lgr5) is expressed selectively in the crypt-base columnar cells [29] and was the first proven biomarker of CR-CSCs. In mouse models, genetic inactivation of the key colorectal cancer (CRC) driver gene Adenomatous Polyposis Coli (Apc) in Lgr5+ cells precipitated rapid tumor induction [30]. By downregulating β-Catenin and YAP signaling pathways, Protein kinase C ζ (PKC ζ) can inhibit intestinal stem cell function. PKC ζ deficiency can lead to an increase in stem cell activity in organoid cultures. Furthermore, tumorigenic activity increased in Lgr5+PKC ζ deficient mice [31]. This evidence suggests that CR-CSCs seem to originate from intestinal stem cells. However, selective and effective killing of Lgr5+ cells had no impact on primary tumor growth [24], and cells that disseminate and colonize distant organs were frequently Lgr5− [32]. Recent research using single cell sequencing technology has shown that the rDNA transcription and protein synthesis of Lgr5+ and Lgr5− cancer cell subsets were increased, which showed the characteristics of functional stem cells [33] and that lineage conversion between cell types can be driven by a combination of key CRC driver genes and microenvironmental extracellular signaling [34].Vazquez and colleagues also confirmed that the intestine contains two types of stem cells, Lgr5+ crypt-base columnar stem cells (CBCs) and Lgr5 regenerative stem cells (RSCs) using single cell sequencing technology. The two stem cell populations can coexist during tumorigenesis, exhibit dynamic plasticity, and complement each other to achieve homeostasis. The relative abundance of CBC-RSC is related to epithelial mutation and microenvironment signal destruction [35]. With the advancement of research technology, it is certain to uncover the origin of CR-CSCs.
2.2. Identification of CR-CSCs
The sorting of cancer stem cells mainly relies on flow cytometry and magnetic activation sorting. The most commonly used basis is for sorting cancer stem cell biomarker proteins. Previous studies have found that CSCs have specific biomarkers, including CD133, ALDH1, CD44 and EpCAM [36]. CSC biomarkers vary with the tumor type. There are also some biomarkers for CR-CSCs. The marker proteins located on the cell membrane include Lgr5 [37], CD133 [38,39], CD44 [40], CD26 [41], CD24 [42], CD29 [43], CD166 [44] and EpCAM [45]. Aldehyde dehydrogenase1 (ALDH1) is an intracellular enzyme that oxidizes aldehydes and mediates the control of differentiation pathways. It is currently widely used as a marker for identifying and isolating various types of normal stem cells and CSCs [44,46]. Oct4 [47], Sox2 [48] and Nanog [49] are transcription factors used as biomarker located in the nucleus (Figure 2). The biological functions of most biomarkers are related to cell stemness.
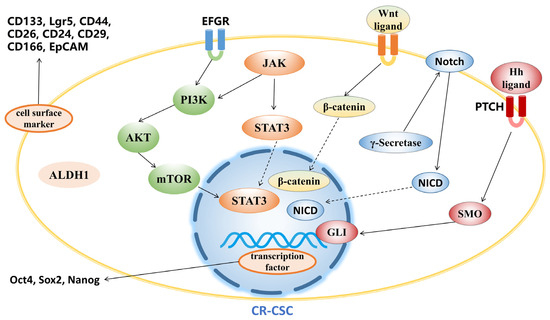
Figure 2.
Biomarker proteins and regulators in pathways in CR-CSCs.
Biomarker proteins and regulators in the pathway are the most prominent targets in CR-CSC therapy.
By combining fluorescent labeled antibodies with cancer stem cell biomarkers, flow cytometry can be used to select CSCs expressing the related biomarkers from cancer cells. The side population (SP) cells with strong drug resistance are also considered to have the stemness of tumor stem cells. The characteristic of these cells is that they can expel the fluorescent dye hoechst33342 out of the cell, and it is shown as a non-fluorescent cell when detected via flow cytometry. CSCs with strong drug resistance in SP cells can be obtained by flow sorting [50]. Magnetic activated cell sorting utilizes antibodies attached to magnetic beads to bind to CSC biomarkers, adsorbing the corresponding cancer stem cells onto a separation column, while unbound cells pass through the separation column. Cancer stem cells with positive surface labeling can be obtained by mean of elution from the separation column [51,52] Single-cell omics technology is a powerful tool for exploring CSCs [53,54]. Single-cell omics technology can characterize and type CSCs in tumors, and establishing a stemness model has prospective clinical implications for prognostic evaluation [35,55].
2.3. Cultivation of CR-CSCs
It is worth emphasizing that although the research results on cancer stem cells have broad prospects for practical clinical applications, they are still in the initial stage. In order to successfully unleash the enormous potential of cancer stem cell research achievements, there are still many urgent issues to address. To understand the physiological activity of CSCs, the first step is to obtain them. For solid tumors, the most commonly used method to enrich cancer stem cells is non-adhesive culture with serum-free culture [56,57]. CSCs with self-renewal capacity are able to survive under non-adherent conditions and maintain clonogenic activity, whereas non-CSCs undergo anoikis by loss of anchorage.
Three-dimensional (3D) culture has emerged as a cell culture method in vitro in recent years. By using hydrogel to mimic the extracellular matrix and applying different culture conditions, 3D culture can mimic in vivo microenvironment [58]. Different gel materials have different porosity, permeability, surface chemical and mechanical properties, which will have different effects on cell growth and differentiation [59]. Three-dimensional culture can be used to enrich stem cells or study cell differentiation [60]. Organoid is an advanced version of 3D culture, which is a 3D micro cell cluster formed by directional differentiation of stem cells [61]. Organoids have the abilities to self-renew and self-organize, and can highly mimic the structure and function of organs in vivo. They have been widely used in the study of organ diseases, drug toxicity and cancer therapy [62,63].
3. Agents Targeting CR-CSCs
3.1. Targeting CR-CSC Biomarkers
Biomarker proteins are targets for the rapid screening of CRCs. In order to enhance the specificity of therapeutic strategies, researchers often choose ligands or antibodies against CSC surface makers (Table 1). MCLA-158 is an EGFR and Lgr5 targeting bispecific antibody with strong growth inhibitory effects on CRC organoids. Simultaneously, it exhibits strong anti-tumor activity in xenograft models derived from patients with high expression of Lgr5 and EGFR [64]. In mouse orthotopic xenograft models derived from CRC patients, MCLA-158 treatment not only reduced the size of the primary tumor but also effectively suppressed metastasis, including that of KRAS mutant tumors resistant to Cetuximab. Currently, researchers are conducting clinical trials of MCLA-158 in various solid tumors (NCT03526835) [64]. Catumaxomab was the first T cell binding bispecific antibody approved by the European Medicines Agency (EMA) in 2009 for the treatment of malignant ascites [65]. Catumaxomab is a trifunctional bispecific antibody that binds to EpCAM on cancer cells and CD3 on T cells. It also binds to FcγR to recruit immune helper cells [65]. Catumaxomab can effectively eliminate CD133+/EpCAM+CSCs in malignant ascites in patients with advanced ovarian cancer, gastric cancer and pancreatic cancer, which indicates that it has potential therapeutic applications in eradicating CSCs of epithelial cancers [66,67]. Similar to catumaxomab, solidomab is also a bispecific antibody targeting EpCAM and CD3. Solidomab treatment was found to effectively eradicated EpCAM+CSCs, originating from colon or pancreatic cancer patients that were inoculated into NOD/SCID mice [68,69].

Table 1.
Agents targeting to CR-CSC biomarkers and Wnt pathway.
In addition to antibodies, there are oncolytic virotherapies and CSC vaccines for targeted biomarker therapies. Oncolytic viruses are a class of viruses with tumor-killing functions. Oncolytic virotherapy is an emerging new tumor treatment that utilizes oncolytic viruses to selectively destroy tumor cells while leaving normal cells intact. Using the properties of oncolytic viruses combined with receptors on tumor cells, researchers have screened or engineered oncolytic viruses that target cancer stem cells [96]. Due to the characteristics of virus vectors, oncolytic virotherapy can trigger immunogenic cell death, release tumor-related antigens and elicit anti-tumor immune response, which can exert stronger anti-cancer effect [96]. Oncolytic viruses with a CD133-targeting motif effectively infected and killed CD133+CR-CSCs, and inhibited the growth of CRC xenotransplantation models [74]. Oncolytic virotherapy is one potential therapy strategy, but it still needs further research. CSCs vaccines are also a type of immunotherapy under research. For example, B16F10 CD133+/CD44+CSCs vaccine can effectively inhibit melanoma growth in mice and reduce the CSC population within tumors [97]. Although no cancer stem cell vaccine has entered clinical trials at this time, the demonstrated efficacy of a vaccine targeting metastatic CRC is reassuring and raises hope [98].
3.2. Targeting Signaling Pathway
Multiple signaling pathways are involved in the self-renewal, proliferation, apoptosis and angiogenesis processes of CR-CSCs. Currently, it is believed that specifically targeting cell signaling pathways to inhibit the effects of CR-CSCs is a major development direction for CRC therapy.
3.2.1. Wnt Signaling Pathway
The Wnt pathway plays a critical role in controlling epithelial stem cell self-renewal, and its dysregulation causes colorectal carcinogenesis [99,100]. The canonical Wnt pathway downstream signaling is regulated by the level of β-catenin (Figure 2). TRAF2- and NCK-interacting kinase (TNIK) is an essential activator of Wnt target genes [99]. The inhibitory activity of TNIK inhibitors such as NCB0846 on CR-CSCs has been confirmed [75]. Epigallocatechin gallate (EGCG) is a kind of the catechins found in green tea. It has been proven to effectively inhibit stem cells from various cancers [101,102]. EGCG can inhibit the stemness of CRC cells by downregulating the expression of biomarkers such as CD133, CD44, NANOG, OCT4, ALDH1 and Wnt/β-catenin signaling pathway [76,77]. The small molecule inhibitor XAV939 was shown to significantly downregulate CSC biomarkers in colon cancer cells and increased apoptosis induced by chemotherapy drugs [78]. Phenethyl isothiocyanate (PEITC) and sulforaphane are natural products extracted from cruciferae plants with anti-cancer activities [79,103]. PEITC suppressed the characteristics of CR-CSCs by reducing the activity of the Wnt/β-catenin pathway, leading to a decline in the proportion of CD133+ cells [79,80]. Salinomycin, an anti-bacterial polyether isolated from Streptomyces albus, was found to selectively eliminate CD133+ cells in CRC [104]. Salinomycin induced apoptosis of human CR-CSCs by activating caspase, increasing DNA damage and disrupting of the Wnt/β-catenin/TCF complex. Tumor growth and expression of CSC-related Wnt genes, including Lgr5 were decreased [82,105]. In addition to these, there are many drugs that reduce CSC stemness by targeting the Wnt signaling pathway, such as pan-inhibitor of histone demethylases JIB04 [83] and lysine-specific demethylase 1 inhibitor CBB1003 [84] (Table 1).
3.2.2. Hedgehog Signaling Pathway
The Hedgehog (Hh) signaling pathway plays an essential role in the growth and differentiation of gastrointestinal tissue [106]. The canonical Hh signal involves Hh ligands (sonic Hh, Indian Hh or desert Hh) binding to the patched (PTCH) receptor, releasing smoothened (SMO) and causing the receptor to activate. In this process, GLI protein will be activated and become transcriptional activators of the downstream targets of the Hh signaling pathway. The Hh-GLI pathway is involved in maintaining the self-renewal ability of CR-CSCs [107,108] (Figure 2).
Vismodegib (also named Ericdge, GDC-0449) is a Hedgehog signaling pathway inhibitor used in clinical practice and approved by the US Food and Drug Administration for the treatment of basal cell carcinoma. Vismodegib targets a subpopulation of CSCs in basal cell carcinoma [109]. Studies have shown that vismodegib can inhibit the stemness of CR-CSC and the expression of biomarkers CD44 and ALDH1 [110]. Cyclopamine is a natural alkaloid that can inhibit the Hh-GLI signaling pathway by inhibiting SMO. After cyclopamine treatment, the mRNA levels of CSC biomarkers and genes related to Hh signaling, including PTCH1, SMO and GLI1 were found to decreased in stem cells derived from HCT116 [111]. Given the regulation of CR-CSCs by Hh signaling pathway, more new inhibitors are being developed (Table 2).

Table 2.
Agents targeting to signaling pathway.
3.2.3. Notch Signaling Pathway
Notch signaling is involved in the regulation of cell differentiation, proliferation and tumorigenesis [134]. The pathway consists of four receptors (Notch1-4) and five ligands (Jagged-1, Jagged-2, Delta-1, Delta-3, Delta-4) and DNA-binding proteins. The interaction between receptors and ligands initiates protein cleavage cascade reactions, leading to the activation of Notch target genes [135]. Gamma secretase inhibitors (GSIs) can inhibit Notch signaling by preventing the proteolytic cleavage of Notch receptors [136] (Figure 2). However, RO4929097, one of the GSIs, failed to achieve excellent results in clinical trials [113]. More GSIs are under investigation. DLL4 is an activator protein of the non-canonical Notch signaling pathway.DLL4 antibody was confirmed to be effective against both KRAS wild-type and mutant CRC cells, effectively eradicating CR-CSCs and enhancing the antitumor effect of irinotecan [114,137]. In addition, Honokiol, Quercetin and others have also been shown to have the ability to inhibit CR-CSC stemness [115,116] (Table 2).
3.2.4. PI3K/Akt/mTOR Signaling Pathway
The PI3K/Akt/mTOR signaling pathway plays a crucial role in cell metabolism and proliferation, and it is closely related to the CR-CSC phenotype [138]. Studies have demonstrated that components of the PI3K/Akt signaling pathway are overexpressed in CRC in vitro and in vivo [130,139]. PI3K and MEK inhibitors used in combination can induce CR-CSC death and the regression of tumor xenografts [140]. BEZ235, a dual pathway inhibitor of mTOR and PI3K, could inhibit the proliferation of CR-CSCs and the expression of its biomarkers CD133 and Lgr5, thus suppressing the stemness of CR-CSCs [118]. LY294002 is a PI3K inhibitor based on the flavonoid quercetin. LY294002 blocked Akt phosphorylation through the PI3K/Akt signaling pathway and inhibited liver CSC proliferation and tumorigenicity in vitro and in vivo [120]. LY294002 treatment led to a decrease in proliferation, spheroid formation and self-renewal properties, as well as a decrease in Akt phosphorylation and cyclin D1 expression in CR-CSCs in vitro [120]. Piplartine is an alkaloid amide isolated from peppers. It was reported to inhibit stemness properties in leukemia and oral cancer [121,140]. In combination with auranofin, piplartine reduced the expression levels of surface biomarker CD44v9, eliminated CR-CSCs and inhibited CRC growth [121]. Rapamycin is an mTOR inhibitor and is used clinically as an immunosuppressive drug. In CRC cell lines, it has the potential to decrease the spheroid-forming ability and ALDH1 activity [123]. In cotreatment with 5-FU and oxaliplatin, rapamycin reduced the CR-CSCs subpopulation. Metformin is also reported to reduce the CSC population in different types of cancers [141]. Metformin not only reduced the proliferation of CSC population in mouse xenografts [125], but also effectively reduced CSC population in colorectal and other gastrointestinal cancers in a pilot clinical trial [142]. There are also many drugs that target the PI3K/Akt/mTOR signaling pathway to inhibit CR-CSCs, such as Atractylenolide I and Torin-1 [126,127].
3.2.5. JAK/STAT3 Signaling Pathway
JAK/STAT signaling is closely related to cancer growth and metastasis. In cancer cells, JAK/STAT signaling can be activated by multiple mechanisms, most notably by STAT3 activation [143]. High STAT3 activity was found in CRC-SCs, but not in normal colon epithelial cells [144]. Another study revealed that the JAK2/STAT3 signaling pathway promoted the persistence and radio-resistance of CR-CSCs [145]. Curcumin is a polyphenol from Curcuma longa, and GO-Y030 is a novel curcumin analog. Curcumin and its analog GO-Y030 were proposed drug candidates to eliminate CR-CSCs by suppressing STAT3 activity [132]. Napabucasin, also named BBI608, is an orally administered STAT3 inhibitor with anti-CSC activity against various types of cancer [146,147]. However, unfortunately, napabucasin failed to achieve satisfactory results in phase 3 clinical trials for the treatment of colorectal cancer [133]. ls. Napabucasin may be the first anti-CRC drug approved for clinical use targeting CSCs
There are other signaling pathways such as TGF-β and Hippo, regulating CSCs stemness. These various signaling pathways do not operate independently and often act via crosstalk to influence cancer progression [22,106,148,149,150] (Table 2).
3.3. Other Agents Targeting CR-CSCs
FBXL5 E3 ligase plays an important role in maintaining the stemness of CR-CSCs. The anandamide uptake inhibitor AM404 can suppress FBXL5 expression and inhibit CR-CSC dedifferentiation, migration and drug resistance [151]. Prexasertib, also named LY2606368, is an investigational checkpoint kinase inhibitor. By inhibiting checkpoint kinase (CHK) 1, LY2606368 affected DNA replication in most CR-CSCs [152]. ASR352 and NSC30049 are both CHK1 inhibitor [153,154]. RAB5/7, which is associated with the endo lysosomal pathway, plays an important role in the survival and maintenance of CSCs through the mitophagic pathway. Mefloquine, an anti-malaria drug, has been identified as a new inhibitor of RAB. In the PDX model of colorectal cancer, mefloquine can target RAB5/7 to inhibit the mitophagic pathway and induce mitochondrial-induced apoptosis, thereby exerting anti-tumor effects without significant side effects [155]. At present, there are many other types of CR-CSC antagonists, such as pitavastatin [156], histone deacetylase inhibitor trichostatin A [157] and inhibitors of the post-translational sumoylation modification pathway [158]. They may play an important role in targeting CR-CSCs in future (Table 3).

Table 3.
Agents targeting CR-CSCs.
4. Future Prospects
Despite significant progress in research on therapeutic drugs for CR-CSCs, cancer treatment still faces many challenges. Tumor microenvironment (TME) plays a major role in determining cell fate and behavioral choices [165,166]. Under the complex interaction of the TME, reversible transformation can be achieved between tumorigenic and non-tumorigenic cells. This is the reason why it is difficult to completely remove CSCs [167]. Cancer-associated fibroblasts (CAFs) play a significant positive role in the development and transfer of CR-CSCs [168]. A tumor is an entity composed of multiple heterogeneous cells. Different subtypes of CSCs may have different resistance mechanisms, and therefore, each cancer subtype may require unique therapies [169]. The plethora of contributing factors in cancer and the complex regulatory network make it difficult to eradicate cancer via a single therapeutic intervention.
Fortunately, researchers never give up. In order to achieve effective treatment, more extensive and in-depth research has been conducted to examine molecular and cellular aspects, including the synergistic targeting of CR-CSCs and TME in cancer treatment. Fibroblast activation protein (FAP) is a type II membrane-bound glycoprotein that is overexpressed in CAFs and activated fibroblasts at wound healing/inflammatory sites. FAP inhibitor has been developed to target CAFs to improve TME [170]. In response to the problem of tumor stem cell heterogeneity, anti CSC drugs with diverse targets have been or are currently being developed. Many of them have been incorporated into clinical or preclinical trials. In the face of the differing responses of different patients to therapeutic approaches, prognosis prediction and personalized treatment are the best solutions. Single cell omics and organoid technology can assist in achieving this goal. Using large-scale omics technologies, we can subtype cancers and build predictive models for treatment response [35,55]. In vitro culture of patient derived tumor organoids can enable prediction of drug sensitivity and resistance, and achieve precision treatment [171]. In summary, in the face of differing treatment responses in patients, the heterogeneity of cancer stem cells and the complex regulatory mechanisms of cancer, researchers have been struggling to decipher them.
5. Conclusions
CR-CSCs are a small group of stem cells in colon cancer that have unlimited proliferation, self-renewal and differentiation ability, playing an important role in drug resistance, metastasis and recurrence. CSCs are like cancer seeds, which cannot be ignored in cancer treatment. The advancement of modern medical technology has given us a certain level of understanding of colon cancer stem cells, but we have not yet fully understood them. Regarding the current situation of CR-CSCs targeted inhibitors, it is important to strengthen the synergistic effect between drugs. By combining drugs targeting CR-CSCs with other treatment methods, we can prevent cancer metastasis and recurrence while reducing the occurrence of drug resistance, which will improve the effectiveness of current CRC treatment. Cancer and the tissue involved are integrated, and treatment should adopt a systematic approach, striving to completely eliminate the seeds to prevent metastasis and recurrence. Targeted inhibitors of CRCSCs are an emerging treatment method for CRC. Although there are still many unclear mechanisms to be discovered, it can be expected that in the future, these drugs will play an undeniable role in preventing colon cancer metastasis and recurrence. Certainly, a complete cancer treatment requires not only targeted treatment for CR-CSCs, but also targeted combination therapy for non-CR-CSCs and TME, as well as the entire tumor. In order to benefit all patients, personalized therapy is the ultimate goal. Single-cell omics technology and organoid technology have contributed to a deeper understanding of the different aspects of cancer stem cells and to the development of more effective treatments for cancer. Achieving this goal still requires considerable efforts and collaboration from researchers.
Author Contributions
X.B. proposed the theme of the manuscript. H.Z. and R.H. searched, consulted the literature, and wrote the manuscript, while Z.W. and J.X. revised the manuscript. H.Z. and R.H. made the same contribution to the manuscript. All authors have read and agreed to the published version of the manuscript.
Funding
This research was supported by Shenzhen Science and Technology Program (JCYJ20210324133602007), Construction Funds of Key Medical Disciplines in Longhua District, Shenzhen (MKD202007090211), Inflammation and Immune Mediated Diseases Laboratory of Anhui Province Open Project (IMMDL20220009) and Special project of medical research of Medical Association of Longhua District, Shenzhen (2023LHMA03).
Institutional Review Board Statement
Not Applicable.
Informed Consent Statement
Not Applicable.
Data Availability Statement
Not Applicable.
Acknowledgments
We acknowledge Zhifu Zhang for assistance, support and significant contributions during the revisions of the paper. We would like to thank the Support from the Shenzhen “Healthcare San Ming Project”.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Lapidot, T.; Sirard, C.; Vormoor, J.; Murdoch, B.; Hoang, T.; Caceres-Cortes, J.; Minden, M.; Paterson, B.; Caligiuri, M.A.; Dick, J.E. A cell initiating human acute myeloid leukaemia after transplantation into SCID mice. Nature 1994, 367, 645–648. [Google Scholar] [CrossRef] [PubMed]
- Dontu, G.; Al-Hajj, M.; Abdallah, W.M.; Clarke, M.F.; Wicha, M.S. Stem cells in normal breast development and breast cancer. Cell Prolif. 2003, 36 (Suppl. 1), 59–72. [Google Scholar] [CrossRef] [PubMed]
- Singh, S.K.; Clarke, I.D.; Terasaki, M.; Bonn, V.E.; Hawkins, C.; Squire, J.; Dirks, P.B. Identification of a cancer stem cell in human brain tumors. Cancer Res. 2003, 63, 5821–5828. [Google Scholar] [PubMed]
- Maitland, N.J.; Collins, A. A tumour stem cell hypothesis for the origins of prostate cancer. BJU Int. 2005, 96, 1219–1223. [Google Scholar] [CrossRef] [PubMed]
- Lam, J.S.; Yamashiro, J.; Shintaku, I.P.; Vessella, R.L.; Jenkins, R.B.; Horvath, S.; Said, J.W.; Reiter, R.E. Prostate stem cell antigen is overexpressed in prostate cancer metastases. Clin. Cancer Res. 2005, 11, 2591–2596. [Google Scholar] [CrossRef]
- O’Brien, C.A.; Pollett, A.; Gallinger, S.; Dick, J.E. A human colon cancer cell capable of initiating tumour growth in immunodeficient mice. Nature 2007, 445, 106–110. [Google Scholar] [CrossRef] [PubMed]
- Boman, B.M.; Wicha, M.S. Cancer stem cells: A step toward the cure. J. Clin. Oncol. 2008, 26, 2795–2799. [Google Scholar] [CrossRef] [PubMed]
- Reya, T.; Morrison, S.J.; Clarke, M.F.; Weissman, I.L. Stem cells, cancer, and cancer stem cells. Nature 2001, 414, 105–111. [Google Scholar] [CrossRef]
- Chen, K.; Huang, Y.H.; Chen, J.L. Understanding and targeting cancer stem cells: Therapeutic implications and challenges. Acta Pharmacol. Sin. 2013, 34, 732–740. [Google Scholar] [CrossRef]
- Chaffer, C.L.; Brueckmann, I.; Scheel, C.; Kaestli, A.J.; Wiggins, P.A.; Rodrigues, L.O.; Brooks, M.; Reinhardt, F.; Su, Y.; Polyak, K.; et al. Normal and neoplastic nonstem cells can spontaneously convert to a stem-like state. Proc. Natl. Acad. Sci. USA 2011, 108, 7950–7955. [Google Scholar] [CrossRef]
- Prasetyanti, P.R.; Medema, J.P. Intra-tumor heterogeneity from a cancer stem cell perspective. Mol. Cancer 2017, 16, 41. [Google Scholar] [CrossRef] [PubMed]
- Bütof, R.; Dubrovska, A.; Baumann, M. Clinical perspectives of cancer stem cell research in radiation oncology. Radiother. Oncol. 2013, 108, 388–396. [Google Scholar] [CrossRef] [PubMed]
- Rich, J.N. Cancer stem cells in radiation resistance. Cancer Res. 2007, 67, 8980–8984. [Google Scholar] [CrossRef] [PubMed]
- Hermann, P.C.; Huber, S.L.; Herrler, T.; Aicher, A.; Ellwart, J.W.; Guba, M.; Bruns, C.J.; Heeschen, C. Distinct populations of cancer stem cells determine tumor growth and metastatic activity in human pancreatic cancer. Cell Stem Cell 2007, 1, 313–323. [Google Scholar] [CrossRef] [PubMed]
- Oskarsson, T.; Batlle, E.; Massagué, J. Metastatic stem cells: Sources, niches, and vital pathways. Cell Stem Cell 2014, 14, 306–321. [Google Scholar] [CrossRef] [PubMed]
- Abdullah, L.N.; Chow, E.K. Mechanisms of chemoresistance in cancer stem cells. Clin. Transl. Med. 2013, 2, 3. [Google Scholar] [CrossRef]
- Yao, J.; Liu, Y.; Yang, J.; Li, M.; Li, S.; Zhang, B.; Yang, R.; Zhang, Y.; Cui, X.; Feng, C. Single-Cell Sequencing Reveals that DBI is the Key Gene and Potential Therapeutic Target in Quiescent Bladder Cancer Stem Cells. Front. Genet. 2022, 13, 904536. [Google Scholar] [CrossRef]
- Antonica, F.; Santomaso, L.; Pernici, D.; Petrucci, L.; Aiello, G.; Cutarelli, A.; Conti, L.; Romanel, A.; Miele, E.; Tebaldi, T.; et al. A slow-cycling/quiescent cells subpopulation is involved in glioma invasiveness. Nat. Commun. 2022, 13, 4767. [Google Scholar] [CrossRef]
- Sung, H.; Ferlay, J.; Siegel, R.L.; Laversanne, M.; Soerjomataram, I.; Jemal, A.; Bray, F. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J. Clin. 2021, 71, 209–249. [Google Scholar] [CrossRef]
- Marhaba, R.; Klingbeil, P.; Nuebel, T.; Nazarenko, I.; Buechler, M.W.; Zoeller, M. CD44 and EpCAM: Cancer-initiating cell markers. Curr. Mol. Med. 2008, 8, 784–804. [Google Scholar] [CrossRef]
- Gaiser, M.R.; Lämmermann, T.; Feng, X.; Igyarto, B.Z.; Kaplan, D.H.; Tessarollo, L.; Germain, R.N.; Udey, M.C. Cancer-associated epithelial cell adhesion molecule (EpCAM; CD326) enables epidermal Langerhans cell motility and migration in vivo. Proc. Natl. Acad. Sci. USA 2012, 109, E889–E897. [Google Scholar] [CrossRef] [PubMed]
- Cheung, P.; Xiol, J.; Dill, M.T.; Yuan, W.C.; Panero, R.; Roper, J.; Osorio, F.G.; Maglic, D.; Li, Q.; Gurung, B.; et al. Regenerative Reprogramming of the Intestinal Stem Cell State via Hippo Signaling Suppresses Metastatic Colorectal Cancer. Cell Stem Cell 2020, 27, 590–604.e9. [Google Scholar] [CrossRef] [PubMed]
- Shimokawa, M.; Ohta, Y.; Nishikori, S.; Matano, M.; Takano, A.; Fujii, M.; Date, S.; Sugimoto, S.; Kanai, T.; Sato, T. Visualization and targeting of LGR5(+) human colon cancer stem cells. Nature 2017, 545, 187–192. [Google Scholar] [CrossRef] [PubMed]
- de Sousa e Melo, F.; Kurtova, A.V.; Harnoss, J.M.; Kljavin, N.; Hoeck, J.D.; Hung, J.; Anderson, J.E.; Storm, E.E.; Modrusan, Z.; Koeppen, H.; et al. A distinct role for Lgr5(+) stem cells in primary and metastatic colon cancer. Nature 2017, 543, 676–680. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.; Gong, P.; Chen, T.; Gao, S.; Wu, Z.; Wang, X.; Li, J.; Marjani, S.L.; Costa, J.; Weissman, S.M.; et al. Colorectal Cancer Stem Cell States Uncovered by Simultaneous Single-Cell Analysis of Transcriptome and Telomeres. Adv. Sci. 2021, 8, 2004320. [Google Scholar] [CrossRef] [PubMed]
- Ohta, Y.; Fujii, M.; Takahashi, S.; Takano, A.; Nanki, K.; Matano, M.; Hanyu, H.; Saito, M.; Shimokawa, M.; Nishikori, S.; et al. Cell-matrix interface regulates dormancy in human colon cancer stem cells. Nature 2022, 608, 784–794. [Google Scholar] [CrossRef] [PubMed]
- Perekatt, A.O.; Shah, P.P.; Cheung, S.; Jariwala, N.; Wu, A.; Gandhi, V.; Kumar, N.; Feng, Q.; Patel, N.; Chen, L.; et al. SMAD4 Suppresses WNT-Driven Dedifferentiation and Oncogenesis in the Differentiated Gut Epithelium. Cancer Res. 2018, 78, 4878–4890. [Google Scholar] [CrossRef]
- Mani, S.A.; Guo, W.; Liao, M.J.; Eaton, E.N.; Ayyanan, A.; Zhou, A.Y.; Brooks, M.; Reinhard, F.; Zhang, C.C.; Shipitsin, M.; et al. The epithelial-mesenchymal transition generates cells with properties of stem cells. Cell 2008, 133, 704–715. [Google Scholar] [CrossRef]
- Barker, N.; van Es, J.H.; Kuipers, J.; Kujala, P.; van den Born, M.; Cozijnsen, M.; Haegebarth, A.; Korving, J.; Begthel, H.; Peters, P.J.; et al. Identification of stem cells in small intestine and colon by marker gene Lgr5. Nature 2007, 449, 1003–1007. [Google Scholar] [CrossRef]
- Barker, N.; Ridgway, R.A.; van Es, J.H.; van de Wetering, M.; Begthel, H.; van den Born, M.; Danenberg, E.; Clarke, A.R.; Sansom, O.J.; Clevers, H. Crypt stem cells as the cells-of-origin of intestinal cancer. Nature 2009, 457, 608–611. [Google Scholar] [CrossRef]
- Llado, V.; Nakanishi, Y.; Duran, A.; Reina-Campos, M.; Shelton, P.M.; Linares, J.F.; Yajima, T.; Campos, A.; Aza-Blanc, P.; Leitges, M.; et al. Repression of Intestinal Stem Cell Function and Tumorigenesis through Direct Phosphorylation of β-Catenin and Yap by PKCζ. Cell Rep. 2015, 10, 740–754. [Google Scholar] [CrossRef] [PubMed]
- Fumagalli, A.; Oost, K.C.; Kester, L.; Morgner, J.; Bornes, L.; Bruens, L.; Spaargaren, L.; Azkanaz, M.; Schelfhorst, T.; Beerling, E.; et al. Plasticity of Lgr5-Negative Cancer Cells Drives Metastasis in Colorectal Cancer. Cell Stem Cell 2020, 26, 569–578.e7. [Google Scholar] [CrossRef]
- Morral, C.; Stanisavljevic, J.; Hernando-Momblona, X.; Mereu, E.; Álvarez-Varela, A.; Cortina, C.; Stork, D.; Slebe, F.; Turon, G.; Whissell, G.; et al. Zonation of Ribosomal DNA Transcription Defines a Stem Cell Hierarchy in Colorectal Cancer. Cell Stem Cell 2020, 26, 845–861.e12. [Google Scholar] [CrossRef] [PubMed]
- Han, T.; Goswami, S.; Hu, Y.; Tang, F.; Zafra, M.P.; Murphy, C.; Cao, Z.; Poirier, J.T.; Khurana, E.; Elemento, O.; et al. Lineage Reversion Drives WNT Independence in Intestinal Cancer. Cancer Discov. 2020, 10, 1590–1609. [Google Scholar] [CrossRef] [PubMed]
- Vasquez, E.G.; Nasreddin, N.; Valbuena, G.N.; Mulholland, E.J.; Belnoue-Davis, H.L.; Eggington, H.R.; Schenck, R.O.; Wouters, V.M.; Wirapati, P.; Gilroy, K.; et al. Dynamic and adaptive cancer stem cell population admixture in colorectal neoplasia. Cell Stem Cell 2022, 29, 1213–1228.e8. [Google Scholar] [CrossRef] [PubMed]
- Makena, M.R.; Ranjan, A.; Thirumala, V.; Reddy, A.P. Cancer stem cells: Road to therapeutic resistance and strategies to overcome resistance. Biochim. Biophys. Acta Mol. Basis Dis. 2020, 1866, 165339. [Google Scholar] [CrossRef]
- Sato, T.; Vries, R.G.; Snippert, H.J.; van de Wetering, M.; Barker, N.; Stange, D.E.; van Es, J.H.; Abo, A.; Kujala, P.; Peters, P.J.; et al. Single Lgr5 stem cells build crypt-villus structures in vitro without a mesenchymal niche. Nature 2009, 459, 262–265. [Google Scholar] [CrossRef]
- Ricci-Vitiani, L.; Lombardi, D.G.; Pilozzi, E.; Biffoni, M.; Todaro, M.; Peschle, C.; De Maria, R. Identification and expansion of human colon-cancer-initiating cells. Nature 2007, 445, 111–115. [Google Scholar] [CrossRef]
- Li, G.; Liu, C.; Yuan, J.; Xiao, X.; Tang, N.; Hao, J.; Wang, H.; Bian, X.; Deng, Y.; Ding, Y. CD133(+) single cell-derived progenies of colorectal cancer cell line SW480 with different invasive and metastatic potential. Clin. Exp. Metastasis 2010, 27, 517–527. [Google Scholar] [CrossRef]
- Greve, B.; Kelsch, R.; Spaniol, K.; Eich, H.T.; Götte, M. Flow cytometry in cancer stem cell analysis and separation. Cytom. Part A 2012, 81, 284–293. [Google Scholar] [CrossRef]
- Pang, R.; Law, W.L.; Chu, A.C.; Poon, J.T.; Lam, C.S.; Chow, A.K.; Ng, L.; Cheung, L.W.; Lan, X.R.; Lan, H.Y.; et al. A subpopulation of CD26+ cancer stem cells with metastatic capacity in human colorectal cancer. Cell Stem Cell 2010, 6, 603–615. [Google Scholar] [CrossRef]
- Choi, D.; Lee, H.W.; Hur, K.Y.; Kim, J.J.; Park, G.S.; Jang, S.H.; Song, Y.S.; Jang, K.S.; Paik, S.S. Cancer stem cell markers CD133 and CD24 correlate with invasiveness and differentiation in colorectal adenocarcinoma. World J. Gastroenterol. 2009, 15, 2258–2264. [Google Scholar] [CrossRef]
- Fujimoto, K.; Beauchamp, R.D.; Whitehead, R.H. Identification and isolation of candidate human colonic clonogenic cells based on cell surface integrin expression. Gastroenterology 2002, 123, 1941–1948. [Google Scholar] [CrossRef] [PubMed]
- Dalerba, P.; Dylla, S.J.; Park, I.K.; Liu, R.; Wang, X.; Cho, R.W.; Hoey, T.; Gurney, A.; Huang, E.H.; Simeone, D.M.; et al. Phenotypic characterization of human colorectal cancer stem cells. Proc. Natl. Acad. Sci. USA 2007, 104, 10158–10163. [Google Scholar] [CrossRef] [PubMed]
- Munz, M.; Baeuerle, P.A.; Gires, O. The emerging role of EpCAM in cancer and stem cell signaling. Cancer Res. 2009, 69, 5627–5629. [Google Scholar] [CrossRef]
- Huang, E.H.; Hynes, M.J.; Zhang, T.; Ginestier, C.; Dontu, G.; Appelman, H.; Fields, J.Z.; Wicha, M.S.; Boman, B.M. Aldehyde dehydrogenase 1 is a marker for normal and malignant human colonic stem cells (SC) and tracks SC overpopulation during colon tumorigenesis. Cancer Res. 2009, 69, 3382–3389. [Google Scholar] [CrossRef]
- Chen, Y.C.; Hsu, H.S.; Chen, Y.W.; Tsai, T.H.; How, C.K.; Wang, C.Y.; Hung, S.C.; Chang, Y.L.; Tsai, M.L.; Lee, Y.Y.; et al. Oct-4 expression maintained cancer stem-like properties in lung cancer-derived CD133-positive cells. PLoS ONE 2008, 3, e2637. [Google Scholar] [CrossRef] [PubMed]
- Tang, Q.; Chen, J.; Di, Z.; Yuan, W.; Zhou, Z.; Liu, Z.; Han, S.; Liu, Y.; Ying, G.; Shu, X.; et al. TM4SF1 promotes EMT and cancer stemness via the Wnt/β-catenin/SOX2 pathway in colorectal cancer. J. Exp. Clin. Cancer Res. 2020, 39, 232. [Google Scholar] [CrossRef]
- Yao, C.; Su, L.; Shan, J.; Zhu, C.; Liu, L.; Liu, C.; Xu, Y.; Yang, Z.; Bian, X.; Shao, J.; et al. IGF/STAT3/NANOG/Slug Signaling Axis Simultaneously Controls Epithelial-Mesenchymal Transition and Stemness Maintenance in Colorectal Cancer. Stem Cells 2016, 34, 820–831. [Google Scholar] [CrossRef]
- Wu, A.; Oh, S.; Wiesner, S.M.; Ericson, K.; Chen, L.; Hall, W.A.; Champoux, P.E.; Low, W.C.; Ohlfest, J.R. Persistence of CD133+ cells in human and mouse glioma cell lines: Detailed characterization of GL261 glioma cells with cancer stem cell-like properties. Stem Cells Dev. 2008, 17, 173–184. [Google Scholar] [CrossRef]
- Elkashty, O.A.; Abu Elghanam, G.; Su, X.; Liu, Y.; Chauvin, P.J.; Tran, S.D. Cancer stem cells enrichment with surface markers CD271 and CD44 in human head and neck squamous cell carcinomas. Carcinogenesis 2020, 41, 458–466. [Google Scholar] [CrossRef]
- Liu, L.; Borlak, J. Advances in Liver Cancer Stem Cell Isolation and their Characterization. Stem Cell Rev. Rep. 2021, 17, 1215–1238. [Google Scholar] [CrossRef] [PubMed]
- Kharchenko, P.V. The triumphs and limitations of computational methods for scRNA-seq. Nat. Methods 2021, 18, 723–732. [Google Scholar] [CrossRef] [PubMed]
- Frank, M.H.; Wilson, B.J.; Gold, J.S.; Frank, N.Y. Clinical Implications of Colorectal Cancer Stem Cells in the Age of Single-Cell Omics and Targeted Therapies. Gastroenterology 2021, 160, 1947–1960. [Google Scholar] [CrossRef] [PubMed]
- Zheng, H.; Liu, H.; Li, H.; Dou, W.; Wang, J.; Zhang, J.; Liu, T.; Wu, Y.; Liu, Y.; Wang, X. Characterization of stem cell landscape and identification of stemness-relevant prognostic gene signature to aid immunotherapy in colorectal cancer. Stem Cell Res. Ther. 2022, 13, 244. [Google Scholar] [CrossRef] [PubMed]
- Chen, S.F.; Chang, Y.C.; Nieh, S.; Liu, C.L.; Yang, C.Y.; Lin, Y.S. Nonadhesive culture system as a model of rapid sphere formation with cancer stem cell properties. PLoS ONE 2012, 7, e31864. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.; Zhang, Y.; Cheng, L.; Li, C.; Dai, L.; Zhang, H.; Yan, F.; Shi, H.; Dong, G.; Ning, Z.; et al. Enrichment and characterization of cancer stem-like cells in ultra-low concentration of serum and non-adhesive culture system. Am. J. Transl. Res. 2018, 10, 1552–1561. [Google Scholar]
- Chaicharoenaudomrung, N.; Kunhorm, P.; Noisa, P. Three-dimensional cell culture systems as an in vitro platform for cancer and stem cell modeling. World J. Stem Cells 2019, 11, 1065–1083. [Google Scholar] [CrossRef]
- Hoarau-Véchot, J.; Rafii, A.; Touboul, C.; Pasquier, J. Halfway between 2D and Animal Models: Are 3D Cultures the Ideal Tool to Study Cancer-Microenvironment Interactions? Int. J. Mol. Sci. 2018, 19, 181. [Google Scholar] [CrossRef]
- Guo, X.; Chen, Y.; Ji, W.; Chen, X.; Li, C.; Ge, R. Enrichment of cancer stem cells by agarose multi-well dishes and 3D spheroid culture. Cell Tissue Res. 2019, 375, 397–408. [Google Scholar] [CrossRef]
- Gjorevski, N.; Sachs, N.; Manfrin, A.; Giger, S.; Bragina, M.E.; Ordóñez-Morán, P.; Clevers, H.; Lutolf, M.P. Designer matrices for intestinal stem cell and organoid culture. Nature 2016, 539, 560–564. [Google Scholar] [CrossRef] [PubMed]
- Clevers, H. Modeling Development and Disease with Organoids. Cell 2016, 165, 1586–1597. [Google Scholar] [CrossRef]
- Huang, L.; Holtzinger, A.; Jagan, I.; BeGora, M.; Lohse, I.; Ngai, N.; Nostro, C.; Wang, R.; Muthuswamy, L.B.; Crawford, H.C.; et al. Ductal pancreatic cancer modeling and drug screening using human pluripotent stem cell- and patient-derived tumor organoids. Nat. Med. 2015, 21, 1364–1371. [Google Scholar] [CrossRef] [PubMed]
- Herpers, B.; Eppink, B.; James, M.I.; Cortina, C.; Cañellas-Socias, A.; Boj, S.F.; Hernando-Momblona, X.; Glodzik, D.; Roovers, R.C.; van de Wetering, M.; et al. Functional patient-derived organoid screenings identify MCLA-158 as a therapeutic EGFR × LGR5 bispecific antibody with efficacy in epithelial tumors. Nat. Cancer 2022, 3, 418–436. [Google Scholar] [CrossRef] [PubMed]
- Frampton, J.E. Catumaxomab: In malignant ascites. Drugs 2012, 72, 1399–1410. [Google Scholar] [CrossRef]
- Bezan, A.; Hohla, F.; Meissnitzer, T.; Greil, R. Systemic effect of catumaxomab in a patient with metastasized colorectal cancer: A case report. BMC Cancer 2013, 13, 618. [Google Scholar] [CrossRef]
- Ströhlein, M.A.; Lordick, F.; Rüttinger, D.; Grützner, K.U.; Schemanski, O.C.; Jäger, M.; Lindhofer, H.; Hennig, M.; Jauch, K.W.; Peschel, C.; et al. Immunotherapy of peritoneal carcinomatosis with the antibody catumaxomab in colon, gastric, or pancreatic cancer: An open-label, multicenter, phase I/II trial. Onkologie 2011, 34, 101–108. [Google Scholar] [CrossRef]
- Bellone, S.; Black, J.; English, D.P.; Schwab, C.L.; Lopez, S.; Cocco, E.; Bonazzoli, E.; Predolini, F.; Ferrari, F.; Ratner, E.; et al. Solitomab, an EpCAM/CD3 bispecific antibody construct (BiTE), is highly active against primary uterine serous papillary carcinoma cell lines in vitro. Am. J. Obstet. Gynecol. 2016, 214, 99.e1–99.e8. [Google Scholar] [CrossRef]
- Herrmann, I.; Baeuerle, P.A.; Friedrich, M.; Murr, A.; Filusch, S.; Rüttinger, D.; Majdoub, M.W.; Sharma, S.; Kufer, P.; Raum, T.; et al. Highly efficient elimination of colorectal tumor-initiating cells by an EpCAM/CD3-bispecific antibody engaging human T cells. PLoS ONE 2010, 5, e13474. [Google Scholar] [CrossRef]
- Wang, Y.; Chen, M.; Wu, Z.; Tong, C.; Dai, H.; Guo, Y.; Liu, Y.; Huang, J.; Lv, H.; Luo, C.; et al. CD133-directed CAR T cells for advanced metastasis malignancies: A phase I trial. Oncoimmunology 2018, 7, e1440169. [Google Scholar] [CrossRef]
- Silva Galbiatti-Dias, A.L.; Fernandes, G.M.M.; Castanhole-Nunes, M.M.U.; Hidalgo, L.F.; Nascimento Filho, C.H.V.; Kawasaki-Oyama, R.S.; Ferreira, L.A.M.; Biselli-Chicote, P.M.; Pavarino, É.C.; Goloni-Bertollo, E.M. Relationship between CD44(high)/CD133(high)/CD117(high) cancer stem cells phenotype and Cetuximab and Paclitaxel treatment response in head and neck cancer cell lines. Am. J. Cancer Res. 2018, 8, 1633–1641. [Google Scholar] [PubMed]
- Yaeger, R.; Weiss, J.; Pelster, M.S.; Spira, A.I.; Barve, M.; Ou, S.I.; Leal, T.A.; Bekaii-Saab, T.S.; Paweletz, C.P.; Heavey, G.A.; et al. Adagrasib with or without Cetuximab in Colorectal Cancer with Mutated KRAS G12C. N. Engl. J. Med. 2023, 388, 44–54. [Google Scholar] [CrossRef]
- Tabernero, J.; Grothey, A.; Van Cutsem, E.; Yaeger, R.; Wasan, H.; Yoshino, T.; Desai, J.; Ciardiello, F.; Loupakis, F.; Hong, Y.S.; et al. Encorafenib Plus Cetuximab as a New Standard of Care for Previously Treated BRAF V600E-Mutant Metastatic Colorectal Cancer: Updated Survival Results and Subgroup Analyses from the BEACON Study. J. Clin. Oncol. 2021, 39, 273–284. [Google Scholar] [CrossRef] [PubMed]
- Sato-Dahlman, M.; Miura, Y.; Huang, J.L.; Hajeri, P.; Jacobsen, K.; Davydova, J.; Yamamoto, M. CD133-targeted oncolytic adenovirus demonstrates anti-tumor effect in colorectal cancer. Oncotarget 2017, 8, 76044–76056. [Google Scholar] [CrossRef] [PubMed]
- Masuda, M.; Uno, Y.; Ohbayashi, N.; Ohata, H.; Mimata, A.; Kukimoto-Niino, M.; Moriyama, H.; Kashimoto, S.; Inoue, T.; Goto, N.; et al. TNIK inhibition abrogates colorectal cancer stemness. Nat. Commun. 2016, 7, 12586. [Google Scholar] [CrossRef]
- Chen, Y.; Wang, X.Q.; Zhang, Q.; Zhu, J.Y.; Li, Y.; Xie, C.F.; Li, X.T.; Wu, J.S.; Geng, S.S.; Zhong, C.Y.; et al. (-)-Epigallocatechin-3-Gallate Inhibits Colorectal Cancer Stem Cells by Suppressing Wnt/β-Catenin Pathway. Nutrients 2017, 9, 572. [Google Scholar] [CrossRef] [PubMed]
- Toden, S.; Tran, H.M.; Tovar-Camargo, O.A.; Okugawa, Y.; Goel, A. Epigallocatechin-3-gallate targets cancer stem-like cells and enhances 5-fluorouracil chemosensitivity in colorectal cancer. Oncotarget 2016, 7, 16158–16171. [Google Scholar] [CrossRef]
- Wu, X.; Luo, F.; Li, J.; Zhong, X.; Liu, K. Tankyrase 1 inhibitior XAV939 increases chemosensitivity in colon cancer cell lines via inhibition of the Wnt signaling pathway. Int. J. Oncol. 2016, 48, 1333–1340. [Google Scholar] [CrossRef]
- Chen, Y.; Wang, M.H.; Zhu, J.Y.; Xie, C.F.; Li, X.T.; Wu, J.S.; Geng, S.S.; Han, H.Y.; Zhong, C.Y. TAp63α targeting of Lgr5 mediates colorectal cancer stem cell properties and sulforaphane inhibition. Oncogenesis 2020, 9, 89. [Google Scholar] [CrossRef]
- Chen, Y.; Li, Y.; Wang, X.Q.; Meng, Y.; Zhang, Q.; Zhu, J.Y.; Chen, J.Q.; Cao, W.S.; Wang, X.Q.; Xie, C.F.; et al. Phenethyl isothiocyanate inhibits colorectal cancer stem cells by suppressing Wnt/β-catenin pathway. Phytother. Res. PTR 2018, 32, 2447–2455. [Google Scholar] [CrossRef]
- Alumkal, J.J.; Slottke, R.; Schwartzman, J.; Cherala, G.; Munar, M.; Graff, J.N.; Beer, T.M.; Ryan, C.W.; Koop, D.R.; Gibbs, A.; et al. A phase II study of sulforaphane-rich broccoli sprout extracts in men with recurrent prostate cancer. Investig. New Drugs 2015, 33, 480–489. [Google Scholar] [CrossRef]
- Wang, Z.; Zhou, L.; Xiong, Y.; Yu, S.; Li, H.; Fan, J.; Li, F.; Su, Z.; Song, J.; Sun, Q.; et al. Salinomycin exerts anti-colorectal cancer activity by targeting the β-catenin/T-cell factor complex. Br. J. Pharmacol. 2019, 176, 3390–3406. [Google Scholar] [CrossRef] [PubMed]
- Wang, L.; Chang, J.; Varghese, D.; Dellinger, M.; Kumar, S.; Best, A.M.; Ruiz, J.; Bruick, R.; Peña-Llopis, S.; Xu, J.; et al. A small molecule modulates Jumonji histone demethylase activity and selectively inhibits cancer growth. Nat. Commun. 2013, 4, 2035. [Google Scholar] [CrossRef] [PubMed]
- Hsu, H.C.; Liu, Y.S.; Tseng, K.C.; Yang, T.S.; Yeh, C.Y.; You, J.F.; Hung, H.Y.; Chen, S.J.; Chen, H.C. CBB1003, a lysine-specific demethylase 1 inhibitor, suppresses colorectal cancer cells growth through down-regulation of leucine-rich repeat-containing G-protein-coupled receptor 5 expression. J. Cancer Res. Clin. Oncol. 2015, 141, 11–21. [Google Scholar] [CrossRef] [PubMed]
- Yang, W.; Li, Y.; Ai, Y.; Obianom, O.N.; Guo, D.; Yang, H.; Sakamuru, S.; Xia, M.; Shu, Y.; Xue, F. Pyrazole-4-Carboxamide (YW2065): A Therapeutic Candidate for Colorectal Cancer via Dual Activities of Wnt/β-Catenin Signaling Inhibition and AMP-Activated Protein Kinase (AMPK) Activation. J. Med. Chem. 2019, 62, 11151–11164. [Google Scholar] [CrossRef]
- Fang, L.; Zhu, Q.; Neuenschwander, M.; Specker, E.; Wulf-Goldenberg, A.; Weis, W.I.; von Kries, J.P.; Birchmeier, W. A Small-Molecule Antagonist of the β-Catenin/TCF4 Interaction Blocks the Self-Renewal of Cancer Stem Cells and Suppresses Tumorigenesis. Cancer Res. 2016, 76, 891–901. [Google Scholar] [CrossRef]
- Shin, J.H.; Jeong, J.; Choi, J.; Lim, J.; Dinesh, R.K.; Braverman, J.; Hong, J.Y.; Maher, S.E.; Amezcua Vesely, M.C.; Kim, W.; et al. Dickkopf-2 regulates the stem cell marker LGR5 in colorectal cancer via HNF4α1. iScience 2021, 24, 102411. [Google Scholar] [CrossRef] [PubMed]
- Roy, S.; Zhao, Y.; Yuan, Y.C.; Goel, A. Metformin and ICG-001 Act Synergistically to Abrogate Cancer Stem Cells-Mediated Chemoresistance in Colorectal Cancer by Promoting Apoptosis and Autophagy. Cancers 2022, 14, 1281. [Google Scholar] [CrossRef] [PubMed]
- Bamodu, O.A.; Yang, C.K.; Cheng, W.H.; Tzeng, D.T.W.; Kuo, K.T.; Huang, C.C.; Deng, L.; Hsiao, M.; Lee, W.H.; Yeh, C.T. 4-Acetyl-Antroquinonol B Suppresses SOD2-Enhanced Cancer Stem Cell-Like Phenotypes and Chemoresistance of Colorectal Cancer Cells by Inducing hsa-miR-324 re-Expression. Cancers 2018, 10, 269. [Google Scholar] [CrossRef]
- Chang, T.C.; Yeh, C.T.; Adebayo, B.O.; Lin, Y.C.; Deng, L.; Rao, Y.K.; Huang, C.C.; Lee, W.H.; Wu, A.T.; Hsiao, M.; et al. 4-Acetylantroquinonol B inhibits colorectal cancer tumorigenesis and suppresses cancer stem-like phenotype. Toxicol. Appl. Pharmacol. 2015, 288, 258–268. [Google Scholar] [CrossRef]
- Zhang, Q.; Li, X.T.; Chen, Y.; Chen, J.Q.; Zhu, J.Y.; Meng, Y.; Wang, X.Q.; Li, Y.; Geng, S.S.; Xie, C.F.; et al. Wnt/β-catenin signaling mediates the suppressive effects of diallyl trisulfide on colorectal cancer stem cells. Cancer Chemother. Pharmacol. 2018, 81, 969–977. [Google Scholar] [CrossRef]
- Kumar, B.; Ahmad, R.; Sharma, S.; Gowrikumar, S.; Primeaux, M.; Rana, S.; Natarajan, A.; Oupicky, D.; Hopkins, C.R.; Dhawan, P.; et al. PIK3C3 Inhibition Promotes Sensitivity to Colon Cancer Therapy by Inhibiting Cancer Stem Cells. Cancers 2021, 13, 2168. [Google Scholar] [CrossRef]
- Kim, H.; Yu, Y.; Choi, S.; Lee, H.; Yu, J.; Lee, J.H.; Kim, W.Y. Evodiamine Eliminates Colon Cancer Stem Cells via Suppressing Notch and Wnt Signaling. Molecules 2019, 24, 4520. [Google Scholar] [CrossRef]
- Husain, K.; Coppola, D.; Yang, C.S.; Malafa, M.P. Farnesyl dimethyl chromanol targets colon cancer stem cells and prevents colorectal cancer metastasis. Sci. Rep. 2021, 11, 2185. [Google Scholar] [CrossRef]
- Chen, Y.; Rao, X.; Huang, K.; Jiang, X.; Wang, H.; Teng, L. FH535 Inhibits Proliferation and Motility of Colon Cancer Cells by Targeting Wnt/β-catenin Signaling Pathway. J. Cancer 2017, 8, 3142–3153. [Google Scholar] [CrossRef]
- Lin, D.; Shen, Y.; Liang, T. Oncolytic virotherapy: Basic principles, recent advances and future directions. Signal Transduct. Target. Ther. 2023, 8, 156. [Google Scholar] [CrossRef]
- Zhao, F.; Zhang, R.; Wang, J.; Wu, D.; Pan, M.; Li, M.; Guo, M.; Dou, J. Effective tumor immunity to melanoma mediated by B16F10 cancer stem cell vaccine. Int. Immunopharmacol. 2017, 52, 238–244. [Google Scholar] [CrossRef] [PubMed]
- Hubbard, J.M.; Tőke, E.R.; Moretto, R.; Graham, R.P.; Youssoufian, H.; Lőrincz, O.; Molnár, L.; Csiszovszki, Z.; Mitchell, J.L.; Wessling, J.; et al. Safety and Activity of PolyPEPI1018 Combined with Maintenance Therapy in Metastatic Colorectal Cancer: An Open-Label, Multicenter, Phase Ib Study. Clin. Cancer Res. 2022, 28, 2818–2829. [Google Scholar] [CrossRef] [PubMed]
- Katoh, M. Canonical and non-canonical WNT signaling in cancer stem cells and their niches: Cellular heterogeneity, omics reprogramming, targeted therapy and tumor plasticity (Review). Int. J. Oncol. 2017, 51, 1357–1369. [Google Scholar] [CrossRef] [PubMed]
- Silva, V.R.; Santos, L.S.; Dias, R.B.; Quadros, C.A.; Bezerra, D.P. Emerging agents that target signaling pathways to eradicate colorectal cancer stem cells. Cancer Commun. 2021, 41, 1275–1313. [Google Scholar] [CrossRef]
- Sun, X.; Song, J.; Li, E.; Geng, H.; Li, Y.; Yu, D.; Zhong, C. (-)-Epigallocatechin-3-gallate inhibits bladder cancer stem cells via suppression of sonic hedgehog pathway. Oncol. Rep. 2019, 42, 425–435. [Google Scholar] [CrossRef] [PubMed]
- Jiang, P.; Xu, C.; Zhang, P.; Ren, J.; Mageed, F.; Wu, X.; Chen, L.; Zeb, F.; Feng, Q.; Li, S. Epigallocatechin-3-gallate inhibits self-renewal ability of lung cancer stem-like cells through inhibition of CLOCK. Int. J. Mol. Med. 2020, 46, 2216–2224. [Google Scholar] [CrossRef]
- Wang, D.; Upadhyaya, B.; Liu, Y.; Knudsen, D.; Dey, M. Phenethyl isothiocyanate upregulates death receptors 4 and 5 and inhibits proliferation in human cancer stem-like cells. BMC Cancer 2014, 14, 591. [Google Scholar] [CrossRef] [PubMed]
- Dong, T.T.; Zhou, H.M.; Wang, L.L.; Feng, B.; Lv, B.; Zheng, M.H. Salinomycin selectively targets ‘CD133+’ cell subpopulations and decreases malignant traits in colorectal cancer lines. Ann. Surg. Oncol. 2011, 18, 1797–1804. [Google Scholar] [CrossRef]
- Zhang, C.; Tian, Y.; Song, F.; Fu, C.; Han, B.; Wang, Y. Salinomycin inhibits the growth of colorectal carcinoma by targeting tumor stem cells. Oncol. Rep. 2015, 34, 2469–2476. [Google Scholar] [CrossRef]
- Takebe, N.; Miele, L.; Harris, P.J.; Jeong, W.; Bando, H.; Kahn, M.; Yang, S.X.; Ivy, S.P. Targeting Notch, Hedgehog, and Wnt pathways in cancer stem cells: Clinical update. Nat. Rev. Clin. Oncol. 2015, 12, 445–464. [Google Scholar] [CrossRef] [PubMed]
- Varjosalo, M.; Taipale, J. Hedgehog: Functions and mechanisms. Genes Dev. 2008, 22, 2454–2472. [Google Scholar] [CrossRef]
- Cochrane, C.R.; Szczepny, A.; Watkins, D.N.; Cain, J.E. Hedgehog Signaling in the Maintenance of Cancer Stem Cells. Cancers 2015, 7, 1554–1585. [Google Scholar] [CrossRef]
- Frampton, J.E.; Basset-Séguin, N. Vismodegib: A Review in Advanced Basal Cell Carcinoma. Drugs 2018, 78, 1145–1156. [Google Scholar] [CrossRef]
- Wu, C.; Hu, S.; Cheng, J.; Wang, G.; Tao, K. Smoothened antagonist GDC-0449 (Vismodegib) inhibits proliferation and triggers apoptosis in colon cancer cell lines. Exp. Ther. Med. 2017, 13, 2529–2536. [Google Scholar] [CrossRef]
- Batsaikhan, B.E.; Yoshikawa, K.; Kurita, N.; Iwata, T.; Takasu, C.; Kashihara, H.; Shimada, M. Cyclopamine decreased the expression of Sonic Hedgehog and its downstream genes in colon cancer stem cells. Anticancer Res. 2014, 34, 6339–6344. [Google Scholar]
- Smith, D.C.; Eisenberg, P.D.; Manikhas, G.; Chugh, R.; Gubens, M.A.; Stagg, R.J.; Kapoun, A.M.; Xu, L.; Dupont, J.; Sikic, B. A phase I dose escalation and expansion study of the anticancer stem cell agent demcizumab (anti-DLL4) in patients with previously treated solid tumors. Clin. Cancer Res. 2014, 20, 6295–6303. [Google Scholar] [CrossRef]
- Strosberg, J.R.; Yeatman, T.; Weber, J.; Coppola, D.; Schell, M.J.; Han, G.; Almhanna, K.; Kim, R.; Valone, T.; Jump, H.; et al. A phase II study of RO4929097 in metastatic colorectal cancer. Eur. J. Cancer 2012, 48, 997–1003. [Google Scholar] [CrossRef]
- Fischer, M.; Yen, W.C.; Kapoun, A.M.; Wang, M.; O’Young, G.; Lewicki, J.; Gurney, A.; Hoey, T. Anti-DLL4 inhibits growth and reduces tumor-initiating cell frequency in colorectal tumors with oncogenic KRAS mutations. Cancer Res. 2011, 71, 1520–1525. [Google Scholar] [CrossRef]
- Ponnurangam, S.; Mammen, J.M.; Ramalingam, S.; He, Z.; Zhang, Y.; Umar, S.; Subramaniam, D.; Anant, S. Honokiol in combination with radiation targets notch signaling to inhibit colon cancer stem cells. Mol. Cancer Ther. 2012, 11, 963–972. [Google Scholar] [CrossRef]
- Li, Y.; Wang, Z.; Jin, J.; Zhu, S.X.; He, G.Q.; Li, S.H.; Wang, J.; Cai, Y. Quercetin pretreatment enhances the radiosensitivity of colon cancer cells by targeting Notch-1 pathway. Biochem. Biophys. Res. Commun. 2020, 523, 947–953. [Google Scholar] [CrossRef]
- Chandra Boinpelly, V.; Verma, R.K.; Srivastav, S.; Srivastava, R.K.; Shankar, S. α-Mangostin-encapsulated PLGA nanoparticles inhibit colorectal cancer growth by inhibiting Notch pathway. J. Cell. Mol. Med. 2020, 24, 11343–11354. [Google Scholar] [CrossRef] [PubMed]
- Chen, J.; Shao, R.; Li, F.; Monteiro, M.; Liu, J.P.; Xu, Z.P.; Gu, W. PI3K/Akt/mTOR pathway dual inhibitor BEZ235 suppresses the stemness of colon cancer stem cells. Clin. Exp. Pharmacol. Physiol. 2015, 42, 1317–1326. [Google Scholar] [CrossRef]
- Wise-Draper, T.M.; Moorthy, G.; Salkeni, M.A.; Karim, N.A.; Thomas, H.E.; Mercer, C.A.; Beg, M.S.; O’Gara, S.; Olowokure, O.; Fathallah, H.; et al. A Phase Ib Study of the Dual PI3K/mTOR Inhibitor Dactolisib (BEZ235) Combined with Everolimus in Patients with Advanced Solid Malignancies. Target. Oncol. 2017, 12, 323–332. [Google Scholar] [CrossRef] [PubMed]
- Peng, Y.C.; Lu, S.D.; Zhong, J.H.; Xie, Z.B.; You, X.M.; Peng, N.F.; Li, L.Q. Combination of 5-fluorouracil and 2-morphilino-8-phenyl-4H-chromen-4-one may inhibit liver cancer stem cell activity. Tumour Biol. 2016, 37, 10943–10958. [Google Scholar] [CrossRef] [PubMed]
- Tanaka, G.; Inoue, K.; Shimizu, T.; Akimoto, K.; Kubota, K. Dual pharmacological inhibition of glutathione and thioredoxin systems synergizes to kill colorectal carcinoma stem cells. Cancer Med. 2016, 5, 2544–2557. [Google Scholar] [CrossRef]
- Kumar, S.; Agnihotri, N. Piperlongumine, a piper alkaloid targets Ras/PI3K/Akt/mTOR signaling axis to inhibit tumor cell growth and proliferation in DMH/DSS induced experimental colon cancer. Biomed. Pharmacother. 2019, 109, 1462–1477. [Google Scholar] [CrossRef]
- Cai, Z.; Ke, J.; He, X.; Yuan, R.; Chen, Y.; Wu, X.; Wang, L.; Wang, J.; Lan, P.; Wu, X. Significance of mTOR signaling and its inhibitor against cancer stem-like cells in colorectal cancer. Ann. Surg. Oncol. 2014, 21, 179–188. [Google Scholar] [CrossRef]
- Ji, N.; Mukherjee, N.; Reyes, R.M.; Gelfond, J.; Javors, M.; Meeks, J.J.; McConkey, D.J.; Shu, Z.J.; Ramamurthy, C.; Dennett, R.; et al. Rapamycin enhances BCG-specific γδ T cells during intravesical BCG therapy for non-muscle invasive bladder cancer: A randomized, double-blind study. J. Immunother. Cancer 2021, 9, e001941. [Google Scholar] [CrossRef]
- Seo, Y.; Kim, J.; Park, S.J.; Park, J.J.; Cheon, J.H.; Kim, W.H.; Kim, T.I. Metformin Suppresses Cancer Stem Cells through AMPK Activation and Inhibition of Protein Prenylation of the Mevalonate Pathway in Colorectal Cancer. Cancers 2020, 12, 2554. [Google Scholar] [CrossRef]
- Wang, K.; Huang, W.; Sang, X.; Wu, X.; Shan, Q.; Tang, D.; Xu, X.; Cao, G. Atractylenolide I inhibits colorectal cancer cell proliferation by affecting metabolism and stemness via AKT/mTOR signaling. Phytomedicine Int. J. Phytother. Phytopharm. 2020, 68, 153191. [Google Scholar] [CrossRef]
- Francipane, M.G.; Lagasse, E. Selective targeting of human colon cancer stem-like cells by the mTOR inhibitor Torin-1. Oncotarget 2013, 4, 1948–1962. [Google Scholar] [CrossRef] [PubMed]
- Mangiapane, L.R.; Nicotra, A.; Turdo, A.; Gaggianesi, M.; Bianca, P.; Di Franco, S.; Sardina, D.S.; Veschi, V.; Signore, M.; Beyes, S.; et al. PI3K-driven HER2 expression is a potential therapeutic target in colorectal cancer stem cells. Gut 2022, 71, 119–128. [Google Scholar] [CrossRef] [PubMed]
- Goodwin, R.; Jonker, D.; Chen, E.; Kennecke, H.; Cabanero, M.; Tsao, M.S.; Vickers, M.; Bohemier, C.; Lim, H.; Ritter, H.; et al. A phase Ib study of a PI3Kinase inhibitor BKM120 in combination with panitumumab in patients with KRAS wild-type advanced colorectal cancer. Invest. New Drugs 2020, 38, 1077–1084. [Google Scholar] [CrossRef] [PubMed]
- Malkomes, P.; Lunger, I.; Luetticke, A.; Oppermann, E.; Haetscher, N.; Serve, H.; Holzer, K.; Bechstein, W.O.; Rieger, M.A. Selective AKT Inhibition by MK-2206 Represses Colorectal Cancer-Initiating Stem Cells. Ann. Surg. Oncol. 2016, 23, 2849–2857. [Google Scholar] [CrossRef] [PubMed]
- Do, K.; Speranza, G.; Bishop, R.; Khin, S.; Rubinstein, L.; Kinders, R.J.; Datiles, M.; Eugeni, M.; Lam, M.H.; Doyle, L.A.; et al. Biomarker-driven phase 2 study of MK-2206 and selumetinib (AZD6244, ARRY-142886) in patients with colorectal cancer. Investig. New Drugs 2015, 33, 720–728. [Google Scholar] [CrossRef] [PubMed]
- Lin, L.; Liu, Y.; Li, H.; Li, P.K.; Fuchs, J.; Shibata, H.; Iwabuchi, Y.; Lin, J. Targeting colon cancer stem cells using a new curcumin analogue, GO-Y030. Br. J. Cancer 2011, 105, 212–220. [Google Scholar] [CrossRef] [PubMed]
- Jonker, D.J.; Nott, L.; Yoshino, T.; Gill, S.; Shapiro, J.; Ohtsu, A.; Zalcberg, J.; Vickers, M.M.; Wei, A.C.; Gao, Y.; et al. Napabucasin versus placebo in refractory advanced colorectal cancer: A randomised phase 3 trial. Lancet Gastroenterol. Hepatol. 2018, 3, 263–270. [Google Scholar] [CrossRef] [PubMed]
- Yuan, X.; Wu, H.; Xu, H.; Xiong, H.; Chu, Q.; Yu, S.; Wu, G.S.; Wu, K. Notch signaling: An emerging therapeutic target for cancer treatment. Cancer Lett. 2015, 369, 20–27. [Google Scholar] [CrossRef]
- Bray, S.J. Notch signalling in context. Nat. Rev. Mol. Cell Biol. 2016, 17, 722–735. [Google Scholar] [CrossRef] [PubMed]
- BeLow, M.; Osipo, C. Notch Signaling in Breast Cancer: A Role in Drug Resistance. Cells 2020, 9, 2204. [Google Scholar] [CrossRef]
- Hoey, T.; Yen, W.C.; Axelrod, F.; Basi, J.; Donigian, L.; Dylla, S.; Fitch-Bruhns, M.; Lazetic, S.; Park, I.K.; Sato, A.; et al. DLL4 blockade inhibits tumor growth and reduces tumor-initiating cell frequency. Cell Stem Cell 2009, 5, 168–177. [Google Scholar] [CrossRef]
- Polivka, J., Jr.; Janku, F. Molecular targets for cancer therapy in the PI3K/AKT/mTOR pathway. Pharmacol. Ther. 2014, 142, 164–175. [Google Scholar] [CrossRef]
- Chen, S.; Fisher, R.C.; Signs, S.; Molina, L.A.; Shenoy, A.K.; Lopez, M.C.; Baker, H.V.; Koomen, J.M.; Chen, Y.; Gittleman, H.; et al. Inhibition of PI3K/Akt/mTOR signaling in PI3KR2-overexpressing colon cancer stem cells reduces tumor growth due to apoptosis. Oncotarget 2017, 8, 50476–50488. [Google Scholar] [CrossRef]
- Pei, S.; Minhajuddin, M.; Callahan, K.P.; Balys, M.; Ashton, J.M.; Neering, S.J.; Lagadinou, E.D.; Corbett, C.; Ye, H.; Liesveld, J.L.; et al. Targeting aberrant glutathione metabolism to eradicate human acute myelogenous leukemia cells. J. Biol. Chem. 2013, 288, 33542–33558. [Google Scholar] [CrossRef]
- Song, C.W.; Lee, H.; Dings, R.P.; Williams, B.; Powers, J.; Santos, T.D.; Choi, B.H.; Park, H.J. Metformin kills and radiosensitizes cancer cells and preferentially kills cancer stem cells. Sci. Rep. 2012, 2, 362. [Google Scholar] [CrossRef]
- Saif, M.W.; Rajagopal, S.; Caplain, J.; Goodman, M.D.; Popowich, D.; Orkin, B.A.; Tsichlis, P.N.; Martell, R. The First Study Evaluating the Safety of Pre-Surgery Administration of Metformin in Patients with Colorectal and other Gastrointestinal Cancers and Effect on Cancer Stem Cells. Cancer Med. J. 2021, 4 (Suppl. 4), 1–10. [Google Scholar]
- Brooks, A.J.; Putoczki, T. JAK-STAT Signalling Pathway in Cancer. Cancers 2020, 12, 1971. [Google Scholar] [CrossRef] [PubMed]
- Quintás-Cardama, A.; Verstovsek, S. Molecular pathways: Jak/STAT pathway: Mutations, inhibitors, and resistance. Clin. Cancer Res. 2013, 19, 1933–1940. [Google Scholar] [CrossRef] [PubMed]
- Park, S.Y.; Lee, C.J.; Choi, J.H.; Kim, J.H.; Kim, J.W.; Kim, J.Y.; Nam, J.S. The JAK2/STAT3/CCND2 Axis promotes colorectal Cancer stem cell persistence and radioresistance. J. Exp. Clin. Cancer Res. 2019, 38, 399. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Rogoff, H.A.; Keates, S.; Gao, Y.; Murikipudi, S.; Mikule, K.; Leggett, D.; Li, W.; Pardee, A.B.; Li, C.J. Suppression of cancer relapse and metastasis by inhibiting cancer stemness. Proc. Natl. Acad. Sci. USA 2015, 112, 1839–1844. [Google Scholar] [CrossRef] [PubMed]
- Li, Y.; Han, Q.; Zhao, H.; Guo, Q.; Zhang, J. Napabucasin Reduces Cancer Stem Cell Characteristics in Hepatocellular Carcinoma. Front. Pharmacol. 2020, 11, 597520. [Google Scholar] [CrossRef] [PubMed]
- Yang, B.; Bai, H.; Sa, Y.; Zhu, P.; Liu, P. Inhibiting EMT, stemness and cell cycle involved in baicalin-induced growth inhibition and apoptosis in colorectal cancer cells. J. Cancer 2020, 11, 2303–2317. [Google Scholar] [CrossRef]
- Song, L.; Li, Z.Y.; Liu, W.P.; Zhao, M.R. Crosstalk between Wnt/β-catenin and Hedgehog/Gli signaling pathways in colon cancer and implications for therapy. Cancer Biol. Ther. 2015, 16, 1–7. [Google Scholar] [CrossRef]
- van den Brink, G.R.; Hardwick, J.C. Hedgehog Wnteraction in colorectal cancer. Gut 2006, 55, 912–914. [Google Scholar] [CrossRef]
- Ahmed, M.; Jinks, N.; Babaei-Jadidi, R.; Kashfi, H.; Castellanos-Uribe, M.; May, S.T.; Mukherjee, A.; Nateri, A.S. Repurposing Antibacterial AM404 as a Potential Anticancer Drug for Targeting Colorectal Cancer Stem-Like Cells. Cancers 2019, 12, 106. [Google Scholar] [CrossRef]
- Manic, G.; Signore, M.; Sistigu, A.; Russo, G.; Corradi, F.; Siteni, S.; Musella, M.; Vitale, S.; De Angelis, M.L.; Pallocca, M.; et al. CHK1-targeted therapy to deplete DNA replication-stressed, p53-deficient, hyperdiploid colorectal cancer stem cells. Gut 2018, 67, 903–917. [Google Scholar] [CrossRef]
- Narayan, S.; Ramisetti, S.; Jaiswal, A.S.; Law, B.K.; Singh-Pillay, A.; Singh, P.; Amin, S.; Sharma, A.K. ASR352, A potent anticancer agent: Synthesis, preliminary SAR, and biological activities against colorectal cancer bulk, 5-fluorouracil/oxaliplatin resistant and stem cells. Eur. J. Med. Chem. 2019, 161, 456–467. [Google Scholar] [CrossRef] [PubMed]
- Narayan, S.; Jaiswal, A.S.; Sharma, R.; Nawab, A.; Duckworth, L.V.; Law, B.K.; Zajac-Kaye, M.; George, T.J.; Sharma, J.; Sharma, A.K.; et al. NSC30049 inhibits Chk1 pathway in 5-FU-resistant CRC bulk and stem cell populations. Oncotarget 2017, 8, 57246–57264. [Google Scholar] [CrossRef] [PubMed]
- Takeda, M.; Koseki, J.; Takahashi, H.; Miyoshi, N.; Nishida, N.; Nishimura, J.; Hata, T.; Matsuda, C.; Mizushima, T.; Yamamoto, H.; et al. Disruption of Endolysosomal RAB5/7 Efficiently Eliminates Colorectal Cancer Stem Cells. Cancer Res. 2019, 79, 1426–1437. [Google Scholar] [CrossRef] [PubMed]
- Zhang, Z.Y.; Zheng, S.H.; Yang, W.G.; Yang, C.; Yuan, W.T. Targeting colon cancer stem cells with novel blood cholesterol drug pitavastatin. Eur. Rev. Med. Pharmacol. Sci. 2017, 21, 1226–1233. [Google Scholar]
- Huang, T.H.; Wu, S.Y.; Huang, Y.J.; Wei, P.L.; Wu, A.T.; Chao, T.Y. The identification and validation of Trichosstatin A as a potential inhibitor of colon tumorigenesis and colon cancer stem-like cells. Am. J. Cancer Res. 2017, 7, 1227–1237. [Google Scholar] [PubMed]
- Bogachek, M.V.; Park, J.M.; De Andrade, J.P.; Lorenzen, A.W.; Kulak, M.V.; White, J.R.; Gu, V.W.; Wu, V.T.; Weigel, R.J. Inhibiting the SUMO Pathway Represses the Cancer Stem Cell Population in Breast and Colorectal Carcinomas. Stem Cell Rep. 2016, 7, 1140–1151. [Google Scholar] [CrossRef]
- Konstantinopoulos, P.A.; Lee, J.M.; Gao, B.; Miller, R.; Lee, J.Y.; Colombo, N.; Vergote, I.; Credille, K.M.; Young, S.R.; McNeely, S.; et al. A Phase 2 study of prexasertib (LY2606368) in platinum resistant or refractory recurrent ovarian cancer. Gynecol. Oncol. 2022, 167, 213–225. [Google Scholar] [CrossRef]
- Wu, Z.; Huang, M.; Gong, Y.; Lin, C.; Guo, W. BRAF and EGFR inhibitors synergize to increase cytotoxic effects and decrease stem cell capacities in BRAF(V600E)-mutant colorectal cancer cells. Acta Biochim. Biophys. Sin. 2018, 50, 355–361. [Google Scholar] [CrossRef]
- Quarni, W.; Dutta, R.; Green, R.; Katiri, S.; Patel, B.; Mohapatra, S.S.; Mohapatra, S. Mithramycin A Inhibits Colorectal Cancer Growth by Targeting Cancer Stem Cells. Sci. Rep. 2019, 9, 15202. [Google Scholar] [CrossRef] [PubMed]
- Zhang, S.; Ju, X.; Yang, Q.; Zhu, Y.; Fan, D.; Su, G.; Kong, L.; Li, Y. USP47 maintains the stemness of colorectal cancer cells and is inhibited by parthenolide. Biochem. Biophys. Res. Commun. 2021, 562, 21–28. [Google Scholar] [CrossRef] [PubMed]
- Wei, F.; Zhang, T.; Yang, Z.; Wei, J.C.; Shen, H.F.; Xiao, D.; Wang, Q.; Yang, P.; Chen, H.C.; Hu, H.J.C.P. Biochemistry, Gambogic Acid Efficiently Kills Stem-Like Colorectal Cancer Cells by Upregulating ZFP36 Expression. Cell. Physiol. Biochem. 2018, 46, 829–846. [Google Scholar] [CrossRef] [PubMed]
- Chi, Y.; Zhan, X.K.; Yu, H.; Xie, G.R.; Wang, Z.Z.; Xiao, W.; Wang, Y.G.; Xiong, F.X.; Hu, J.F.; Yang, L.; et al. An open-labeled, randomized, multicenter phase IIa study of gambogic acid injection for advanced malignant tumors. Chin. Med. J. Engl. 2013, 126, 1642–1646. [Google Scholar]
- Ferguson, L.P.; Diaz, E.; Reya, T. The Role of the Microenvironment and Immune System in Regulating Stem Cell Fate in Cancer. Trends Cancer 2021, 7, 624–634. [Google Scholar] [CrossRef]
- Antonio, N.; Bønnelykke-Behrndtz, M.L.; Ward, L.C.; Collin, J.; Christensen, I.J.; Steiniche, T.; Schmidt, H.; Feng, Y.; Martin, P. The wound inflammatory response exacerbates growth of pre-neoplastic cells and progression to cancer. EMBO J. 2015, 34, 2219–2236. [Google Scholar] [CrossRef]
- Meacham, C.E.; Morrison, S.J. Tumour heterogeneity and cancer cell plasticity. Nature 2013, 501, 328–337. [Google Scholar] [CrossRef]
- Kobayashi, H.; Gieniec, K.A.; Lannagan, T.R.M.; Wang, T.; Asai, N.; Mizutani, Y.; Iida, T.; Ando, R.; Thomas, E.M.; Sakai, A.; et al. The Origin and Contribution of Cancer-Associated Fibroblasts in Colorectal Carcinogenesis. Gastroenterology 2022, 162, 890–906. [Google Scholar] [CrossRef] [PubMed]
- Kozovska, Z.; Gabrisova, V.; Kucerova, L. Colon cancer: Cancer stem cells markers, drug resistance and treatment. Biomed. Pharmacother. 2014, 68, 911–916. [Google Scholar] [CrossRef]
- Li, M.; Younis, M.H.; Zhang, Y.; Cai, W.; Lan, X. Clinical summary of fibroblast activation protein inhibitor-based radiopharmaceuticals: Cancer and beyond. Eur. J. Nucl. Med. Mol. Imaging 2022, 49, 2844–2868. [Google Scholar] [CrossRef] [PubMed]
- Drost, J.; van Jaarsveld, R.H.; Ponsioen, B.; Zimberlin, C.; van Boxtel, R.; Buijs, A.; Sachs, N.; Overmeer, R.M.; Offerhaus, G.J.; Begthel, H.; et al. Sequential cancer mutations in cultured human intestinal stem cells. Nature 2015, 521, 43–47. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).