Abstract
The study aims to assess the usefulness of human T-cell leukemia virus type 1 (HTLV-1)-infected cell analysis using flow cytometry (HAS-Flow) as a monitoring method for adult T-cell leukemia (ATL) development in HTLV-1-positive patients with rheumatoid arthritis (RA) under treatment with antirheumatic therapies. A total of 13 HTLV-1-negative and 57 HTLV-1-positive RA patients participated in this study, which was used to collect clinical and laboratory data, including HAS-Flow and HTLV-1 proviral load (PVL), which were then compared between the two groups. CADM1 expression on CD4+ cells in peripheral blood (PB) was used to identify HTLV-1-infected cells. The population of CADM1+ CD4+ cells was significantly higher in HTLV-1-positive RA patients compared to HTLV-1-negative RA patients. The population of CADM1+ CD4+ cells was correlated with HTLV-1 PVL values. There were no antirheumatic therapies affecting both the expression of CADM1 on CD4+ cells and PVLs. Six HTLV-1-positive RA patients who indicated both high HTLV-1 PVL and a predominant pattern of CADM1+ CD7neg CD4+ cells in HAS-Flow can be classified as high-risk for ATL progression. HAS-Flow could be a useful method for monitoring high-risk HTLV-1-positive RA patients who are at risk of developing ATL during antirheumatic therapies.
1. Introduction
Standardization of antirheumatic therapies improves prognosis in patients with rheumatoid arthritis (RA). Several biologics and targeted-synthetic disease-modifying antirheumatic drugs (DMARDs) have transformed rheumatic disease treatment [1]. However, the risk of serious infections and malignancies in patients with RA from the use of biologics and synthetic DMARDs remains unknown [2,3].
Human T-cell leukemia virus type 1 (HTLV-1) is the causative agent of adult T-cell leukemia/lymphoma (ATL) and HTLV-1-associated myelopathy/tropical spastic paraparesis (HAM/TSP). There are approximately 1 million HTLV-1 carriers in Japan, making it endemic, [4] and it is estimated that at least 4000 new HTLV-1 infections occur yearly among adults and adolescents in Japan [5]. Furthermore, the number of HTLV-1 carriers has reportedly increased in urban regions of Japan, such as Chubu, Kanto, and Kinki. [5] Further, the incidence of RA is higher in women than in men; therefore, the prevalence of HTLV-1 infection in RA patients in Japan is expected to be high. Based on the prevalence of HTLV-1 infection and RA, the number of HTLV-1-positive patients with RA in Japan could range from 5000 to 10,000.
The CD4-positive T-cells are the main target of HTLV-1. The incidence rate of ATL was estimated at approximately 5% of HTLV-1 carriers. The risk factors for ATL development have been reported to be advanced age and higher HTLV-1 proviral load (PVL) values (>4.0 copies per 100 peripheral blood mononuclear cells (PBMCs)) in HTLV-1-asymptomatic carriers [6]. An increasing HTLV-1 PVL value, which reflects the oligo- or monoclonal expansion of HTLV-1-infected T-cells, was observed in HTLV-1-asymptomatic carriers before the emergence of ATL [7]. The serum concentration of soluble IL-2 receptor (sIL2-R) reflects the expansion of HTLV-1-infected T-cells [8]. However, quantitative polymerase chain reaction (PCR) measurement of HTLV-1 PVL value is not available in daily clinical practice of HTLV-1 carriers. Standardized quantitative PCR for evaluating HTLV-1 PVL has not yet been commercialized; it is only available for research purposes. Furthermore, using inverse-long PCR methods in clinical laboratory tests to assess clonal expansion of HTLV-1-infected T-lymphocytes is unrealistic. As a result, an uncomplicated and efficacious method for monitoring the dynamics of HTLV-1-infected T-lymphocytes is necessary.
HTLV-1-infected cell analysis system flow cytometry (HAS-Flow) was developed as a novel method for monitoring HTLV-1-infected cells, including ATL cells. The cell adhesion molecule 1 (CADM1) versus CD7 plot accurately reflects disease progression in HTLV-1 infection, and CADM1-positive cells with downregulated CD7 in HTLV-1-asymptomatic carriers have properties similar to those in indolent ATL [9]. For example, CADM1+ CD7-negative (CD7neg) cells have been reported to be enriched with clonally expanded cells and abnormal lymphocytes, which were suspected as ATL cells [9]. Several studies that used HAS-Flow analysis suggested an increased risk of developing ATL among participants who had >25% of CD4+ cells that were positive for CADM1 and >50% of CADM1+ cells that were negative for CD7 (CADM1+ CD7dim < CADM1+ CD7neg; CADM1+ CD7neg-dominant pattern) [9,10,11].
However, HAS-Flow has been established as an analysis system for HTLV-1-infected cells using PBMCsobtained from HTLV-1 carriers, including HTLV-1-associated disorders such as HAM/TSP and ATL [9,10,11]. Because no studies have indicated CADM1 expression in CD4 lymphocytes in chronic inflammatory diseases such as RA, it is unclear whether HAS-Flow is an adequate method to evaluate HTLV-1-infected cells and ATL development in HTLV-1-positive RA patients. In addition, it is yet to be elucidated whether antirheumatic therapies including immunosuppressants and biologics effect the expression of CADM1 in CD4 lymphocytes.
Therefore, this study aims to evaluate the usefulness of HAS-Flow in HTLV-1-positive RA patients receiving antirheumatic therapies. In addition, the correlation between HTLV-1 PVL values and the proportion of CADM1+ CD4+ T-lymphocytes in HTLV-1-positive RA patients was examined. The influence of RA disease activity and its antirheumatic therapies on the expression of CADM1 in CD4+ T-lymphocytes were also analyzed. The present study demonstrated that HAS-Flow may be an adequate and useful method for monitoring HTLV-1-infected cells and evaluating the high-risk cell population of ATL progression using HAS-Flow in HTLV-1-positive RA patients.
2. Materials and Methods
2.1. Study Design and Participants
The HTLV-1 RA Miyazaki registry was conducted from December 2017 at the University of Miyazaki Hospital and Miyazaki Zenjinkai Hospital in the Miyazaki Prefecture, Japan. This registry was started as inheritance research of the HTLV-1 RA Miyazaki Cohort Study [12]. The registry aimed to investigate the effect of HTLV-1 infection on the clinical features of RA patients and to clarify whether immunosuppressive therapies alter the risk factors associated with the development of ATL in HTLV-1-positive RA patients. All participants were diagnosed with RA on the basis of the 1987 diagnostic criteria of the American College of Rheumatology (ACR) and screened for HTLV-1 infection [13,14]. Accordingly, 85 HTLV-1-positive RA patients participated in this registry until April 2022. All RA patients were treated with antirheumatic drugs, such as methotrexate (MTX) and biologic agents, in accordance with RA treatment guidelines [15,16,17]. Written informed consent was obtained from all participants and they were expected to periodically visit the University of Miyazaki Hospital and Miyazaki Zenjinkai Hospitals (formerly named Zenjinkai shimin-no-Mori Hospital) for clinical assessment and sample collection [12].
This registry was used to choose the participants for the current investigation. The following are the study’s inclusion criteria: HTLV-1-positive RA participants who underwent HAS-Flow between April 2019 and December 2021 in this registry. Quantitative PCR was also used to determine HTLV-1 PVL levels. According to these inclusion criteria, 57 of 85 HTLV-1-positive RA patients were enrolled in this study. Furthermore, 13 HTLV-1-negative RA patients had performed HAS-Flow in this registry during the same observation period. All clinical data assessed, such as RA disease activity and antirheumatic regimen, was collected from the patient’s medical records. The study protocol was approved by the research ethics committees of the University of Miyazaki Hospital (approval no. O-0236) and Miyazaki Zenjinkai Hospital, and followed the Ethical Guidelines for Medical and Health Research Involving Human Subjects.
2.2. HAS-Flow
For HAS-Flow analysis, whole blood samples in EDTA tubes were obtained periodically from 57 participants with HTLV-1-positive RA and 13 participants with HTLV-1-negative RA. HAS-Flow analysis was performed to detect the expression levels of CADM1 and CD7 in CD4+ T-lymphocytes, according to previously reported methods [11]. An unlabelled CADM1 antibody (clone 3E1) was purchased from MBL (Tokyo, Japan) and subjected to primary amine biotinylation using biotin N-hydroxysuccinimide ester (Sigma Aldrich, St. Louis, MO, USA). All other antibodies were obtained from BioLegend (San Diego, CA, USA). Cells were stained using a combination of biotin-CADM1, allophycocyanin-CD7, and PE-Cy7-CD4. After washing, phycoerythrin (PE)-conjugated streptavidin was applied. A FACS Calibur instrument (BD Immunocytometry Systems, San Jose, CA, USA) was used for all multicolour flow cytometry. Data were analyzed using the FlowJo software (TreeStar, San Carlos, CA, USA).
2.3. The Measurement of HTLV-1 PVL
The current study used HTLV-1 PVL levels measured immediately before or after performing HAS-Flow. The HTLV-1 PVL was measured using PBMCs separated by Ficoll-based density gradient centrifugation; DNA was purified from PBMCs; and real-time PCR was performed using the Light Cycler 2.0 thermal cycler (Roche Diagnostics, Mannheim, Germany) to measure the HTLV-1 pX region and the human albumin gene [18]. The PVL levels of HTLV-1 in PBMCs were measured in duplicates.
2.4. Clinical Assessment of RA
Clinical information was collected during the observation period while performing HAS-Flow. According to the European League Against Rheumatism (EULAR) guidelines, the Disease Activity Score of 28 joints (DAS28) using the erythrocyte sedimentation rate, Simple Disease Activity Index (SDAI) and Clinical Disease Activity Index (CDAI) were used to evaluate RA disease activity [19]. Physical function was assessed using the Health Assessment Questionnaire-Disability Index (HAQ-DI).
2.5. Statistical Analysis
Statistical analyses were performed using EZR (Saitama Medical Centre, Jichi Medical University, Saitama, Japan). EZR is a modified version of R commander (version 2.4-2), which was designed to add statistical functions that are frequently used in biostatistics [20]. The median with interquartile range (IQR) and numbers and percentages were used to express continuous and categorical data, respectively. A group comparison between HTLV-1-negative and HTLV-1-positive RA participants was conducted using the Mann–Whitney U test for age, inflammatory biomarkers value, CDAI, SDAI, DAS28, HAQ–DI, corticosteroid dose, and MTX dose. Categorical variables, including sex, Steinbrocker’s stage and class, rheumatoid factor (RF), anti-citrullinated protein antibody (ACPA) positivity, and usage of corticosteroids and DMARDs such as MTX, tacrolimus and biologic agents, were compared between HTLV-1-negative and HTLV-1-positive RA participants using Fisher’s exact test. A group comparison between HTLV-1-negative and HTLV-1-positive RA participants was conducted using the Mann–Whitney U test for CADM1+ CD4 lymphocytes and the CADM1+ CD7neg CD4 lymphocyte population. The correlation between HTLV-1 PVL, CADM1+ CD4 lymphocytes and CADM1+ CD7neg CD4 lymphocyte population was conducted using Spearman’s test. A p-value of <0.05 was considered significant.
3. Results
3.1. Characteristics of HTLV-1-Negative and HTLV-1-Positive RA Participants
The clinical characteristics of the HTLV-1-negative and HTLV-1-positive RA participants who participated in this investigation are shown in Table 1. Treatment with DMARDs, including MTX and/or biologic agents, was effective in all RA participants, according to the ACR/EULAR guidelines [16]. There were no differences between the two groups in terms of median age, sex ratio, C-reactive protein and erythrocyte sedimentation rate values, or RF/ACPA seroprevalence. According to the EULAR improvement criteria, the CDAI, SDAI and DAS28 values of both groups indicated a low RA disease activity. The proportion of RA participants who received corticosteroids did not change between those who were HTLV-1-negative and those who were HTLV-1-positive. The rate of MTX use, median dosage of MTX and proportion of participants using tacrolimus and biologic agents did not differ between the groups. The number of persons with HTLV-1-associated illnesses such as HAM/TSP was four among HTLV-1-positive RA participants.

Table 1.
Characteristics of HTLV-1-negative and -positive participants with RA.
3.2. The Population of CADM1+ CD4+ Cells in HTLV-1-Negative and HTLV-1-Positive RA Participants
Figure 1 shows representative data of CADM1 versus CD7 plotted by HAS-Flow in HTLV-1-negative RA participants and HTLV-1-positive RA participants. For CD4+ cells, a CADM1 versus CD7 plot was constructed (Figure 1A). According to the previous report, the proportion of CADM1+ CD7dim and CADM1+ CD7neg was named D region (D) and N region (N), respectively [11] (Figure 1B). In HTLV-1-positive RA participants, the population of CADM1+ CD4+ cells (D + N) were higher than in HTLV-1-negative RA participants (15.2% vs. 8.9%, p = 0.002) (Figure 2A). Furthermore, the population of CADM1+ CD7neg CD4+ cells (N) in HTLV-1-positive RA participants was higher than that in HTLV-1-negative RA participants (4.3% vs. 2.5%, p = 0.006) (Figure 2B). The population of CADM1+ CD4+ cells was lower in HTLV-1-negative RA participants compared to those in HTLV-1-positive RA participants. The effect of antirheumatic therapies on CADM1 expression may be deemed minimal because there were no differences in antirheumatic therapy regimen between the two groups. In addition, there were no associations between the population of CADM1+ CD4+ cells and clinical features of RA, such as disease duration and inflammatory conditions. These findings show that CADM1+ CD4+ cells could be evaluated as HTLV-1-infected cells by HAS-Flow in HTLV-1-positive RA participants.
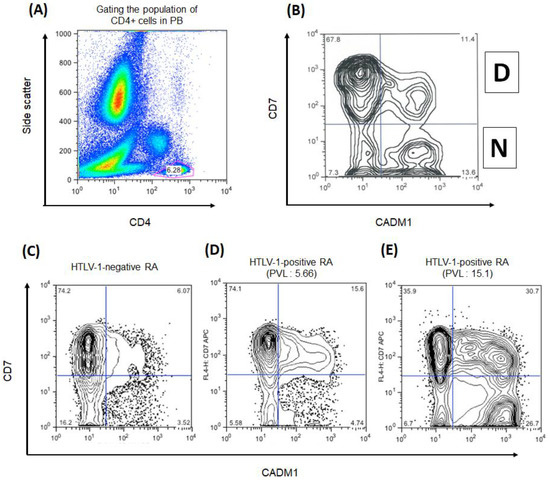
Figure 1.
The representative data of CADM1 versus CD7 plot in CD4+ cells in participants with rheumatoid arthritis (RA). (A) The gating of the CD4+ cell population in peripheral blood (PB). (B) CADM1 versus CD7 plot of CD4+ T-cell population. Upper-right and lower-right regions were named D and N, following previous study. The CD4+ T-cells in D and N region are human T-cell leukemia virus type 1 (HTLV-1)-infected cells. (C–E) The CADM1 versus CD7 plot in CD4+ cells in HTLV-1-negative RA patient, HTLV-1-positive RA participants with different proviral loads (PVLs). The HTLV-1 PVL were 5.66 and 15.1 copies/100 peripheral blood mononuclear cells, respectively.
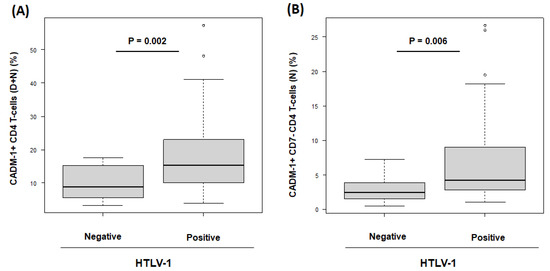
Figure 2.
The comparison of CADM1+ CD4+ T-cell populations between human T-cell leukemia virus type 1 HTLV-1-negative and -positive participants with rheumatoid arthritis (RA). (A) The box plot of the population of CADM1+ CD4+ T-cells, which present in D + N region, in HTLV-1-negative and -positive RA participants. (B) The box plot of the population of CADM1+ CD7neg CD4+ T-cells, which present in N region, in HTLV-1-negative and -positive RA participants.
3.3. The Correlation between Population of CADM1+ CD4+ Cells and HTLV-1 PVL in HTLV-1-Positive RA Participants
The median HTLV-1 PVL for the 57 HTLV-1-positive RA participants was 2.09 copies/100 PBMCs (IQR, 5.2). The population of CADM1+ CD4+ cells (D + N) was correlated with the HTLV-1 PVL values in RA participants receiving several antirheumatic therapies (R = 0.44, p = 0.0005) (Figure 3A). In addition, the population of CADM1+ CD7neg CD4+ cells (N) was also significantly correlated with the HTLV-1 PVL values (R = 0.6, p = 0.0000008) (Figure 3B). In the present study, four RA participants with HAM/TSP were enrolled (Figure 3, open red circles). One of four RA participants with HAM/TSP had a high HTLV-1 PVL of more than 4.0 copies/100PBMCs as well as an increase in the CADM1+ CD7neg CD4+ cell population.
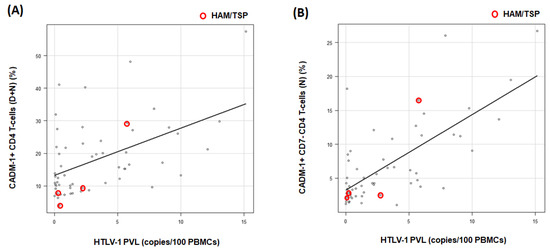
Figure 3.
Scatter plot of the human T-cell leukemia virus type 1 (HTLV-1) proviral load (PVL) versus the percentage of CADM1-positive cells from the CADM1 versus CD7 plot. (A), X- and Y-axis indicates HTLV-1 PVL and the population of CADM1+ CD4+ T-cells (D + N region), respectively (R = 0.44). (B), X- and Y-axis indicates HTLV-1 PVL and the population of CADM1+ CD7 neg CD4+ T-cells (N region), respectively (R = 0.6). The plot with red circles indicated RA participants with HTLV-1-associated myelopathy/tropical spastic paraparesis (HAM/TSP). PBMCs: peripheral blood mononuclear cells.
3.4. Assessment of High-Risk RA Participants for ATL Development Based on HAS-Flow Analysis and HTLV-1 PVL Values
Table 2 shows the HAS-Flow analysis results of 57 HTLV-1-positive RA participants. Out of the 57 participants, 13 participants (22.8%) had more than 25% of CD4+ cells positive for CADM1. These 13 participants were divided into two groups based on the population of CADM1+ CD7neg cells, with more than 50% among CADM1+ cells (Table 2, a and b). In our analysis, 7 of the 13 participants had an increased number of CADM1+ CD7neg cells (CADM1+ CD7neg dominant pattern) (Table 2, b). Nineteen of 57 participants had high HTLV-1 PVL of more than 4.0 copies/100PBMCs. A CADM1+ CD7neg dominant pattern of HAS-Flow was observed in six participants with high HTLV-1 PVL of more than 4.0 copies/100PBMCs. HTLV-1-positive RA participants with high HTLV-1 PVL and a CADM1+ CD7neg dominant pattern may be classified as high-risk participants with ATL development potential.

Table 2.
HAS-Flow results and proportion of HTLV-1-positive RA participants with high proviral load (PVL) values.
4. Discussion
This is the first study to show that HAS-Flow analysis may be used to assess HTLV-1-infected CD4+ cells in HTLV-1-positive RA patients under treatment with antirheumatic therapies.
Among CD4+ cells the population expressing CADM1 was higher in HTLV-1-positive RA patients compared to those in HTLV-1-negative RA patients. CADM1, which was previously discovered as a tumor suppressor in lung cancer [21], has been revealed to be highly and exclusively expressed in HTLV-1-infected cells in the peripheral blood (PB) regardless of the ATL subtype [22,23]. HTLV-1 clones can be highly purified in the CADM1-positive population of CD4+ cells in PB samples from HTLV-1 asymptomatic carriers as well as ATL patients [9,11]. However, there were no reports to clarify the population of CADM1+ CD4+ cells in the PB of RA patients. This study suggests that the population of CADM1+ CD4+ cells was lower in HTLV-1-negative RA patients compared to HTLV-1-positive RA patients. In addition, the percentage of the CADM1+ CD4+ cell population in PB correlated with the HTLV-1 PVL values in HTLV-1-positive RA patients. These HAS-Flow findings corroborated prior data from HTLV-1 carriers, including HAM/TSP patients [24,25]. The mechanisms of CADM1 expression in HTLV-1-infected CD4+ cells are yet unknown. Several studies have suggested that the HTLV-1-related protein Tax is responsible for the expression of CADM1 in HTLV-1-infected cells [24,25]. The Tax-NF-kB complex binds to the CADM1 promotor region [26]. As a result, CADM1 expression in CD4+ cells may be influenced by HTLV-1 Tax activity in both HTLV-1 carriers and HTLV-1-positive RA patients. In addition, our results suggest that antirheumatic therapies may not affect the expression of CADM1 on CD4+ cells in HTLV-1-positive RA patients. Therefore, HAS-Flow analysis may be useful to monitor HTLV-1-infected cells in RA patients receiving antirheumatic therapies.
The independent risk factors for the progression of ATL have been indicated as follows: a higher HTLV-1 PVL, advanced age, family history of ATL, and the first opportunity for HTLV-1 testing during treatment for other diseases [6]. In addition, an increase of more than 25% of CADM1+ CD4+ cells may be one of the risk factors of ATL development in patients with HTLV-1 carriers, including HAM/TSP patients [10,24]. As a result, HTLV-1-positive RA patients with a high PVL value and a significant population of CADM1+ CD4+ cells could be classified as having a high risk of developing ATL. In this study, 19 patients out of 57 HTLV-1-positive RA patients had both a high PVL value and a large population of CADM1+ CD4+ cells, more than 4.0 copies/100PBMCs, and more than 25%, respectively. CD7 downregulation has been reported as a predictive biomarker for progression to ATL [10,24]. The CADM1+ CD7neg dominant pattern of HAS-Flow may be an important finding as predictive ATL progression. In this study, six HTLV-1-positive RA patients showed high HTLV-1 PVL and a CADM1+ CD7neg dominant pattern. These six patients may need close follow-up as high-risk patients with ATL development during antirheumatic therapies. As a result, evaluating both PVL and HAS-Flow, not only for HTLV-1 carriers but also for HTLV-1-positive RA patients, may be a useful method to estimate the risk of ATL development.
A recent study developed and demonstrated the use of oligoclonality index (OCI)-Flow, which is another flow cytometry method to analyze HTLV-1-infected cells, based on the T-cell receptor (TCR) Vβ subunit diversity on T-cells infected with HTLV-1 (CD3+, CCR4+, and CD26− T cells) [27]. OCI-Flow appears to be more specific for identifying patients with ATL-like clones, compared with methods that evaluate CD7 downregulation to predict the development of ATL. Because CD7 downregulation in CD4+ cells increases with increasing PVLs, identification of an ATL-like clone based only on the levels of CD7 expression, such as HAS-Flow, may be limited. Compared with HAS-Flow, OCI-Flow may provide more information on the oligoclonality of HTLV-1-infected cells, however, the versatility and convenience of tests needs to be considered during assessment of the risk of developing ATL; therefore, stratification of these patients using a simple method, such as HAS-Flow, may be considered useful. In the future, a more sensitive and specific prediction algorithm to assess the risk of developing ATL will be developed by combining flow cytometry, such as OCI-Flow and HAS-Flow, next generation sequencing to evaluate gene mutations [10], and a method to track and analyze clonality by detecting transgene integration sites [28].
However, there are several limitations to the present study. Firstly, the sample size was small. Secondly, because this study has been performed as a cross-sectional observational study, there was no time-sequential evaluation of HAS-Flow in this study. Therefore, the impact of antirheumatic therapies on the population of CADM1+ CD4+ cells in patients with HTLV-1-positive RA is yet to be elucidated. It is necessary to investigate whether CADM1+ CD7neg dominant pattern is altered during antirheumatic therapies based on long-term observation. Thirdly, we used HAS-Flow and HTLV-1 PVL to assess the high-risk for ATL development in HTLV-1-positive RA patients; six patients were identified as high-risk in this study. However, whether these high-risk RA patients developed ATL is unknown. As a result, we intend to conduct a large-scale study in the future with prolonged follow-up periods to investigate the utility of HAS-Flow as a monitoring and/or predictive approach for ATL development in HTLV-1-positive RA patients.
5. Conclusions
In conclusion, the analysis of CADM1+ CD4+ cells by HAS-Flow may be a useful method to observe HTLV-1-infected cells in HTLV-1-positive RA patients. Antirheumatic therapies, including immunosuppressants and biologics, may have less effect on the expression of CADM1. Because CD7neg HTLV-1-infected cells have a significant potential of ATL progression, examining the CADM1+ CD7neg predominant pattern in HTLV-1-positive RA patients may be a predictive finding of ATL development. However, whether antirheumatic medications affect the progression of ATL in HTLV-1-positive RA patients is unknown. Future research into the time-sequential HAS-Flow study could provide insights into the role impact of antirheumatic drugs in ATL progression.
Author Contributions
The principal investigator of this project, K.U.; Conceptualization, K.U.; prepared the manuscript, figures, and tables, K.U., Y.H. (Yuki Hashikura) and S.M.; methodology, A.T., Y.H. (Yuki Hashikura) and K.U.; designed the study protocol, M.K. and K.U.; validation, K.K., M.K. and Y.H. (Yuki Hashikura); formal analysis, M.K., Y.H. (Yuki Hashikura), S.M., K.U., A.T., K.K. and M.K.; investigation, M.K. and K.U.; resources, K.U.; performed HAS-Flow analysis, M.K., Y.H. (Yuki Hashikura), A.T., K.K. and K.U.; performed the recruitment of participants, clinical assessment, data curation, and data collection, M.K., M.M., C.I., S.M., T.K., M.M., Y.H. (Yayoi Hashiba), S.M. and T.H.; writing—original draft preparation, K.U.; contributed to the statistical analysis; M.K. and K.U.; writing—review and editing, K.U.; visualization, K.U. and Y.H. (Yuki Hashikura); supervision, T.H.; project administration, K.U.; funding acquisition, K.U. All authors have read and agreed to the published version of the manuscript.
Funding
This study was supported by a grant from the Practical Research Project for Rare/Intractable Diseases of the Japan Agency for Medical Research and Development (Grant No. JP19ek0109356, 20ek0109356h0003, 21ek0109529h0001), a Health and Labour Sciences Research Grant on Rare and Intractable Diseases from the Ministry of Health, Labour and Welfare of Japan (Grant No. 19FC1007), Grants-in-Aid for Scientific Research (C) [KAKENHI] (Grant No. 20K08776) and a Grant-in-Aid for Clinical Research from Miyazaki University Hospital.
Institutional Review Board Statement
This study has been approved by the research ethics committee of University of Miyazaki Hospital (approved No. O-0236).
Informed Consent Statement
Informed consent was obtained from all subjects involved in this study.
Data Availability Statement
All data are available under request to the corresponding author.
Acknowledgments
We would like to thank Yuki Kaseda of the University of Miyazaki for her technical support in this work. We would also like to acknowledge Yumiko Kai at the Institute of Rheumatology, Miyazaki Zenjinkai Hospital, for her help in data management.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Burmester, G.R.; Pope, J.E. Novel treatment strategies in rheumatoid arthritis. Lancet 2017, 389, 2338–2348. [Google Scholar] [CrossRef] [PubMed]
- Singh, J.A.; Cameron, C.; Noorbaloochi, S.; Cullis, T.; Tucker, M.; Christensen, R.; Ghogomu, E.T.; Coyle, D.; Clifford, T.; Tugwell, P.; et al. Risk of serious infection in biological treatment of patients with rheumatoid arthritis: A systematic review and meta-analysis. Lancet 2015, 386, 258–265. [Google Scholar] [CrossRef] [PubMed]
- Sepriano, A.; Kerschbaumer, A.; Smolen, J.S.; van der Heijde, D.; Dougados, M.; van Vollenhoven, R.; McInnes, I.B.; Bijlsma, J.W.; Burmester, G.R.; de Wit, M.; et al. Safety of synthetic and biological DMARDs: A systematic literature review informing the 2019 update of the EULAR recommendations for the management of rheumatoid arthritis. Ann. Rheum. Dis. 2020, 79, 760–770. [Google Scholar] [CrossRef] [PubMed]
- Satake, M.; Yamaguchi, K.; Tadokoro, K. Current prevalence of HTLV-1 in Japan as determined by screening of blood donors. J. Med. Virol. 2012, 84, 327–335. [Google Scholar] [CrossRef] [PubMed]
- Satake, M.; Iwanaga, M.; Sagara, Y.; Watanabe, T.; Okuma, K.; Hamaguchi, I. Incidence of human T-lymphotropic virus 1 infection in adolescent and adult blood donors in Japan: A nationwide retrospective cohort analysis. Lancet Infect. Dis. 2016, 16, 1246–1254. [Google Scholar] [CrossRef]
- Iwanaga, M.; Watanabe, T.; Utsunomiya, A.; Okayama, A.; Uchimaru, K.; Koh, K.R.; Ogata, M.; Kikuchi, H.; Sagara, Y.; Uozumi, K.; et al. Joint Study on Predisposing Factors of ATL Development investigators. Human T-cell leukemia virus type I (HTLV-1) proviral load and disease progression in asymptomatic HTLV-1 carriers: A nationwide prospective study in Japan. Blood 2010, 116, 1211–1219. [Google Scholar] [CrossRef]
- Firouzi, S.; Farmanbar, A.; Nakai, K.; Iwanaga, M.; Uchimaru, K.; Utsunomiya, A.; Suzuki, Y.; Watanabe, T. Clonality of HTLV-1-infected T cells as a risk indicator for development and progression of adult T-cell leukemia. Blood Adv. 2017, 1, 1195–1205. [Google Scholar] [CrossRef]
- Arisaw, K.; Katamine, S.; Kamihira, S.; Kurokawa, K.; Sawada, T.; Soda, M.; Doi, H.; Saito, H.; Shirahama, S. A nested case-control study of risk factors for adult T-cell leukemia/lymphoma among human T-cell lymphotropic virus type-I carriers in Japan. Cancer Causes Control 2002, 13, 657–663. [Google Scholar] [CrossRef]
- Kobayashi, S.; Nakano, K.; Watanabe, E.; Ishigaki, T.; Ohno, N.; Yuji, K.; Oyaizu, N.; Asanuma, S.; Yamagishi, M.; Yamochi, T.; et al. CADM1 expression and stepwise downregulation of CD7 are closely associated with clonal expansion of HTLV-I-infected cells in adult T-cell leukemia/lymphoma. Clin. Cancer Res. 2014, 20, 2851–2861. [Google Scholar] [CrossRef]
- Nagasaka, M.; Yamagishi, M.; Yagishita, N.; Araya, N.; Kobayashi, S.; Makiyama, J.; Kubokawa, M.; Yamauchi, J.; Hasegawa, D.; Coler-Reilly, A.L.G.; et al. Mortality and risk of progression to adult T cell leukemia/lymphoma in HTLV-1-associated myelopathy/tropical spastic paraparesis. Proc. Natl. Acad. Sci. USA 2020, 117, 11685–11691. [Google Scholar] [CrossRef]
- Kobayashi, S.; Watanabe, E.; Ishigaki, T.; Ohno, N.; Yuji, K.; Nakano, K.; Yamochi, T.; Watanabe, N.; Tojo, A.; Watanabe, T.; et al. Advanced human T-cell leukemia virus type 1 carriers and early-stage indolent adult T-cell leukemia-lymphoma are indistinguishable based on CADM1 positivity in flow cytometry. Cancer Sci. 2015, 106, 598–603. [Google Scholar] [CrossRef]
- Umekita, K.; Hashiba, Y.; Kariya, Y.; Kubo, K.; Miyauchi, S.; Aizawa, A.; Umeki, K.; Nomura, H.; Kawaguchi, T.; Matsuda, M.; et al. The time-sequential changes of risk factors for adult T-cell leukemia development in human T-cell leukemia virus-positive patients with rheumatoid arthritis: A retrospective cohort study. Mod. Rheumatol. 2019, 29, 795–801. [Google Scholar] [CrossRef]
- Arnett, F.C.; Edworthy, S.M.; Bloch, D.A.; McShane, D.J.; Fries, J.F.; Cooper, N.S.; Healey, L.A.; Kaplan, S.R.; Liang, M.H.; Luthra, H.S.; et al. The American Rheumatism Association 1987 revised criteria for the classification of rheumatoid arthritis. Arthritis Rheum. Am. Rheum. Assoc. 1988, 31, 315–324. [Google Scholar] [CrossRef]
- Aletaha, D.; Neogi, T.; Silman, A.J.; Funovits, J.; Felson, D.T.; Bingham, O.C., 3rd; Birnbaum, N.S.; Burmester, G.R.; Bykerk, V.P.; Cohen, M.D.; et al. 2010 Rheumatoid arthritis classification criteria: An American College of Rheumatology/European League Against Rheumatism collaborative initiative. Arthritis Rheum. 2010, 62, 2569–2581. [Google Scholar] [CrossRef]
- Singh, J.A.; Saag, K.G.; Bridges, S.L.J.r.; Akl, E.A.; Bannuru, R.R.; Sullivan, M.C.; Vaysbrot, E.; McNaughton, C.; Osani, M.; Shmerling, R.H.; et al. 2015 American College of Rheumatology guideline for the Treatment of rheumatoid arthritis. Arthritis Care Res. 2016, 68, 1–25. [Google Scholar] [CrossRef]
- Smolen, J.S.; Landewé, R.; Bijlsma, J.; Burmester, G.; Chatzidionysiou, K.; Dougados, M.; Nam, J.; Ramiro, S.; Voshaar, M.; van Vollenhoven, R.; et al. EULAR recommendations for the management of rheumatoid arthritis with synthetic and biological disease-modifyingantirheumatic drugs: 2016 update. Ann. Rheum. Dis. 2017, 76, 960–977. [Google Scholar] [CrossRef]
- Smolen, J.S.; Landewé, R.B.M.; Bijlsma, J.W.J.; Burmester, G.R.; Dougados, M.; Kerschbaumer, A.; McInnes, I.B.; Sepriano, A.; van Vollenhoven, R.F.; de Wit, M.; et al. EULAR recommendations for the management of rheumatoid arthritis with synthetic and biological disease-modifyingantirheumatic drugs: 2019 update. Ann. Rheum. Dis. 2020, 79, 685–699. [Google Scholar] [CrossRef]
- Tanaka, G.; Okayama, A.; Watanabe, T.; Aizawa, S.; Stuver, S.; Mueller, N.; Hsieh, C.C.; Tsubouchi, H. The clonal expansion of human T lymphotropic virus type 1-infected T cells: A comparison between seroconverters and long-term carriers. J. Infect. Dis. 2005, 191, 1140–1147. [Google Scholar] [CrossRef]
- Anderson, J.K.; Zimmerman, L.; Caplan, L.; Michaud, K. Measures of rheumatoid arthritis disease activity: Patient (PtGA) and Provider (PrGA) Global Assessment of Disease Activity, Disease Activity Score (DAS) and Disease Activity Score with 28-Joint Counts (DAS28), simplified disease activity index (SDAI), Clinical Disease Activity Index (CDAI), Patient Activity Score (PAS) and Patient Activity Score-II (PASII), Routine Assessment of Patient Index Data (RAPID), Rheumatoid Arthritis Disease Activity Index (RADAI) and Rheumatoid Arthritis Disease Activity Index-5 (RADAI-5), Chronic Arthritis Systemic Index (CASI), Patient-Based Disease Activity Score with ESR (PDAS1) and Patient-Based Disease Activity Score without ESR (PDAS2), and Mean Overall Index for Rheumatoid Arthritis (MOI-RA). Arthritis Care Res. 2011, 63 (Suppl. S11), S14–S36. [Google Scholar]
- Kanda, Y. Investigation of the freely available easy-to-use software ‘EZR’ for medical statistics. Bone Marrow Transplant. 2013, 48, 452–458. [Google Scholar] [CrossRef]
- Kuramochi, M.; Fukuhara, H.; Nobukuni, T.; Kanbe, T.; Maruyama, T.; Ghosh, H.P.; Pletcher, M.; Isomura, M.; Onizuka, M.; Kitamura, T.; et al. TSLC1 is a tumor-suppressor gene in human non-small-cell lung cancer. Nat. Genet. 2001, 27, 427–430. [Google Scholar] [CrossRef] [PubMed]
- Sasaki, H.; Nishikata, I.; Shiraga, T.; Akamatsu, E.; Fukami, T.; Hidaka, T.; Kubuki, Y.; Okayama, A.; Hamada, K.; Okabe, H.; et al. Overexpression of a cell adhesion molecule, TSLC1, as a possible molecular marker for acute-type adult T-cell leukemia. Blood 2005, 105, 1204–1213. [Google Scholar] [CrossRef] [PubMed]
- Nakahata, S.; Saito, Y.; Marutsuka, K.; Hidaka, T.; Maeda, K.; Hatakeyama, K.; Shiraga, T.; Goto, A.; Takamatsu, N.; Asada, Y.; et al. Clinical significance of CADM1/TSLC1/IgSF4 expression in adult T-cell leukemia/lymphoma. Leukemia 2012, 26, 1238–1246. [Google Scholar] [CrossRef] [PubMed]
- Makiyama, J.; Kobayashi, S.; Watanabe, E.; Ishigaki, T.; Kawamata, T.; Nakashima, M.; Yamagishi, M.; Nakano, K.; Tojo, A.; Watanabe, T.; et al. CD4+ CADM1+ cell percentage predicts disease progression in HTLV-1 carriers and indolent adult T-cell leukemia/lymphoma. Cancer Sci. 2019, 110, 3746–3753. [Google Scholar] [CrossRef]
- Manivannan, K.; Rowan, A.G.; Tanaka, Y.; Taylor, G.P.; Bangham, C.R. CADM1/TSLC1 Identifies HTLV-1-Infected cells and determines their susceptibility to CTL-Mediated lysis. PLoS Pathog. 2016, 12, e1005560. [Google Scholar] [CrossRef]
- Sarkar, B.; Nishikata, I.; Nakahata, S.; Ichikawa, T.; Shiraga, T.; Saha, H.R.; Fujii, M.; Tanaka, Y.; Shimoda, K.; Morishita, K. Degradation of p47 by autophagy contributes to CADM1 overexpression in ATLL cells through the activation of NF-κB. Sci. Rep. 2019, 9, 3491. [Google Scholar] [CrossRef]
- Wolf, S.N.; Haddow, J.; Greiller, C.; Taylor, G.P.; Cook, L.B.M.; Rowan, A.G. Quantification of T cell clonality in human T cell leukaemia virus type-1 carriers can detect the development of adult T cell leukaemia early. Blood Cancer J. 2021, 11, 66. [Google Scholar] [CrossRef]
- Wada, Y.; Sato, T.; Hasegawa, H.; Matsudaira, T.; Nao, N.; Coler-Reilly, A.L.G.; Tasaka, T.; Yamauchi, S.; Okagawa, T.; Momose, H.; et al. RAISING is a high-performance method for identifying random transgene integration sites. Commun. Biol. 2022, 5, 535. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).