Animal Models for Crimean-Congo Hemorrhagic Fever Human Disease
Abstract
1. CCHFV as an Endemic and Emerging Pathogen
2. Virus Strain Genetic Diversity
3. Human Crimean-Congo Hemorrhagic Fever
3.1. Transmission
3.2. Phases of Disease
3.3. Hematology and Coagulopathy
3.4. Innate Immunity and Hyper-Inflammatory Cytokine Responses
3.5. Adaptive Immune Response
3.6. Organ Specific Pathogenesis
3.6.1. Liver Pathogenesis
3.6.2. Neuropathogenesis
3.6.3. Cardiac and Respiratory Disease
4. Small Animal Models
4.1. History of Murine Model Development
4.2. Routes of Infection
4.3. Hematology and Coagulopathy
4.4. Hyper-Inflammatory Cytokine Response
4.5. Adaptive Immune Response
4.6. Organ Specific Pathogenesis
4.6.1. Liver Pathogenesis
4.6.2. Neuropathogenesis
4.6.3. Cardiac and Respiratory Disease
5. Tick-Transmission Models
6. Non-Human Primate Models
7. Countermeasure Development
7.1. MCMs Use in Humans
7.2. Evaluation of MCMs in Animal Models
7.2.1. Vaccines
7.2.2. Immunotherapeutics
7.2.3. Small Molecule Inhibitors
7.3. The Impact of Strain Heterogeneity on MCM Protection
7.4. Down-Selection of CCHFV Murine Models for MCM Evaluation
8. BSL2 and BSL3 Surrogate Models
9. Conclusions
Author Contributions
Funding
Acknowledgments
Conflicts of Interest
References
- Whitehouse, C.A. Crimean-Congo hemorrhagic fever. Antiviral Res. 2004, 64, 145–160. [Google Scholar] [CrossRef] [PubMed]
- Hoogstraal, H. The epidemiology of tick-borne Crimean-Congo hemorrhagic fever in Asia, Europe, and Africa. J. Med. Entomol. 1979, 15, 307–417. [Google Scholar] [CrossRef] [PubMed]
- Bente, D.A.; Forrester, N.L.; Watts, D.M.; McAuley, A.J.; Whitehouse, C.A.; Bray, M. Crimean-Congo hemorrhagic fever: History, epidemiology, pathogenesis, clinical syndrome and genetic diversity. Antiviral Res. 2013, 100, 159–189. [Google Scholar] [CrossRef] [PubMed]
- Spengler, J.R.; Bergeron, E.; Spiropoulou, C.F. Crimean-Congo hemorrhagic fever and expansion from endemic regions. Curr. Opin. Virol. 2019, 34, 70–78. [Google Scholar] [CrossRef]
- Negredo, A.; de la Calle-Prieto, F.; Palencia-Herrejon, E.; Mora-Rillo, M.; Astray-Mochales, J.; Sanchez-Seco, M.P.; Bermejo Lopez, E.; Menarguez, J.; Fernandez-Cruz, A.; Sanchez-Artola, B.; et al. Autochthonous Crimean-Congo Hemorrhagic Fever in Spain. N. Engl. J. Med. 2017, 377, 154–161. [Google Scholar] [CrossRef] [PubMed]
- Estrada-Pena, A.; Jameson, L.; Medlock, J.; Vatansever, Z.; Tishkova, F. Unraveling the ecological complexities of tick-associated Crimean-Congo hemorrhagic fever virus transmission: A gap analysis for the western Palearctic. Vector Borne Zoonotic Dis. 2012, 12, 743–752. [Google Scholar] [CrossRef]
- Spengler, J.R.; Estrada-Pena, A.; Garrison, A.R.; Schmaljohn, C.; Spiropoulou, C.F.; Bergeron, E.; Bente, D.A. A chronological review of experimental infection studies of the role of wild animals and livestock in the maintenance and transmission of Crimean-Congo hemorrhagic fever virus. Antivir. Res. 2016, 135, 31–47. [Google Scholar] [CrossRef]
- Shepherd, A.J.; Leman, P.A.; Swanepoel, R. Viremia and antibody response of small African and laboratory animals to Crimean-Congo hemorrhagic fever virus infection. Am. J. Trop. Med. Hyg. 1989, 40, 541–547. [Google Scholar] [CrossRef]
- Ergonul, O. Crimean-Congo haemorrhagic fever. Lancet Infect. Dis. 2006, 6, 203–214. [Google Scholar] [CrossRef]
- Ergonul, O. Crimean-Congo hemorrhagic fever virus: New outbreaks, new discoveries. Curr. Opin. Virol. 2012, 2, 215–220. [Google Scholar] [CrossRef]
- Schmaljohn, C.S.; Nichol, S.T. Bunyaviridae. In Fields Virology, 5th ed.; Knipe, D.M., Howley, P.M., Eds.; Lippincott Williams & Wilkins: Philadelphia, PA, USA, 2007; pp. 1741–1789. [Google Scholar]
- Zivcec, M.; Scholte, F.E.; Spiropoulou, C.F.; Spengler, J.R.; Bergeron, E. Molecular Insights into Crimean-Congo Hemorrhagic Fever Virus. Viruses 2016, 8, 106. [Google Scholar] [CrossRef] [PubMed]
- Atkinson, B.; Latham, J.; Chamberlain, J.; Logue, C.; O’Donoghue, L.; Osborne, J.; Carson, G.; Brooks, T.; Carroll, M.; Jacobs, M.; et al. Sequencing and phylogenetic characterisation of a fatal Crimean–Congo haemorrhagic fever case imported into the United Kingdom, October 2012. Euro Surveill 2012, 17, 20327. [Google Scholar]
- Carroll, S.A.; Bird, B.H.; Rollin, P.E.; Nichol, S.T. Ancient common ancestry of Crimean-Congo hemorrhagic fever virus. Mol. Phylogenet Evol. 2010, 55, 1103–1110. [Google Scholar] [CrossRef] [PubMed]
- Deyde, V.M.; Khristova, M.L.; Rollin, P.E.; Ksiazek, T.G.; Nichol, S.T. Crimean-Congo hemorrhagic fever virus genomics and global diversity. J. Virol. 2006, 80, 8834–8842. [Google Scholar] [CrossRef] [PubMed]
- Mild, M.; Simon, M.; Albert, J.; Mirazimi, A. Towards an understanding of the migration of Crimean-Congo hemorrhagic fever virus. J. Gen. Virol. 2010, 91, 199–207. [Google Scholar] [CrossRef] [PubMed]
- Engin, A.; Arslan, S.; Kizildag, S.; Ozturk, H.; Elaldi, N.; Dokmetas, I.; Bakir, M. Toll-like receptor 8 and 9 polymorphisms in Crimean-Congo hemorrhagic fever. Microbes Infect. 2010, 12, 1071–1078. [Google Scholar] [CrossRef] [PubMed]
- Engin, A.; Arslan, S.; Ozbilum, N.; Bakir, M. Is there any relationship between Toll-like receptor 3 c.1377C/T and -7C/A polymorphisms and susceptibility to Crimean Congo hemorrhagic fever? J. Med. Virol. 2016, 88, 1690–1696. [Google Scholar] [CrossRef] [PubMed]
- Akinci, E.; Bodur, H.; Musabak, U.; Sagkan, R.I. The relationship between the human leukocyte antigen system and Crimean-Congo hemorrhagic fever in the Turkish population. Int. J. Infect. Dis. 2013, 17, e1038–e1041. [Google Scholar] [CrossRef][Green Version]
- Aytekin, F.Y.; Barut, H.S.; Rustemoglu, A.; Atay, A.; Gunal, O.; Duygu, F. Factors related to fatalities and clinical progression of Crimean-Congo hemorrhagic fever patients and the effects of IL 28-B gene polymorphism. Arch. Virol. 2019, 164, 547–557. [Google Scholar] [CrossRef]
- Midilli, K.; Gargili, A.; Ergonul, O.; Elevli, M.; Ergin, S.; Turan, N.; Sengoz, G.; Ozturk, R.; Bakar, M. The first clinical case due to AP92 like strain of Crimean-Congo Hemorrhagic Fever virus and a field survey. BMC Infect. Dis. 2009, 9, 90. [Google Scholar] [CrossRef]
- Salehi-Vaziri, M.; Baniasadi, V.; Jalali, T.; Mirghiasi, S.M.; Azad-Manjiri, S.; Zarandi, R.; Mohammadi, T.; Khakifirouz, S.; Fazlalipour, M. The First Fatal Case of Crimean-Congo Hemorrhagic Fever Caused by the AP92-Like Strain of the Crimean-Congo Hemorrhagic Fever Virus. Jpn. J. Infect. Dis. 2016, 69, 344–346. [Google Scholar] [CrossRef] [PubMed]
- Papa, A.; Chaligiannis, I.; Kontana, N.; Sourba, T.; Tsioka, K.; Tsatsaris, A.; Sotiraki, S. A novel AP92-like Crimean-Congo hemorrhagic fever virus strain, Greece. Ticks Tick Borne Dis. 2014, 5, 590–593. [Google Scholar] [CrossRef] [PubMed]
- Yen, Y.C.; Kong, L.X.; Lee, L.; Zhang, Y.Q.; Li, F.; Cai, B.J.; Gao, S.Y. Characteristics of Crimean-Congo hemorrhagic fever virus (Xinjiang strain) in China. Am. J. Trop. Med. Hyg. 1985, 34, 1179–1182. [Google Scholar] [PubMed]
- Smirnova, S.E. A comparative study of the Crimean hemorrhagic fever-Congo group of viruses. Arch. Virol. 1979, 62, 137–143. [Google Scholar] [CrossRef] [PubMed]
- Burney, M.I.; Ghafoor, A.; Saleen, M.; Webb, P.A.; Casals, J. Nosocomial outbreak of viral hemorrhagic fever caused by Crimean Hemorrhagic fever-Congo virus in Pakistan, January 1976. Am. J. Trop. Med. Hyg. 1980, 29, 941–947. [Google Scholar] [CrossRef] [PubMed]
- Conger, N.G.; Paolino, K.M.; Osborn, E.C.; Rusnak, J.M.; Gunther, S.; Pool, J.; Rollin, P.E.; Allan, P.F.; Schmidt-Chanasit, J.; Rieger, T.; et al. Health care response to CCHF in US soldier and nosocomial transmission to health care providers, Germany, 2009. Emerg. Infect. Dis. 2015, 21, 23–31. [Google Scholar] [CrossRef] [PubMed]
- Pshenichnaya, N.Y.; Nenadskaya, S.A. Probable Crimean-Congo hemorrhagic fever virus transmission occurred after aerosol-generating medical procedures in Russia: Nosocomial cluster. Int. J. Infect. Dis. 2015, 33, 120–122. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Tezer, H.; Sucakli, I.A.; Sayli, T.R.; Celikel, E.; Yakut, I.; Kara, A.; Tunc, B.; Ergonul, O. Crimean-Congo hemorrhagic fever in children. J. Clin. Virol. 2010, 48, 184–186. [Google Scholar] [CrossRef] [PubMed]
- Cevik, M.A.; Erbay, A.; Bodur, H.; Eren, S.S.; Akinci, E.; Sener, K.; Onguru, P.; Kubar, A. Viral load as a predictor of outcome in Crimean-Congo hemorrhagic fever. Clin. Infect. Dis. 2007, 45, e96–e100. [Google Scholar] [CrossRef] [PubMed]
- Cevik, M.A.; Erbay, A.; Bodur, H.; Gulderen, E.; Bastug, A.; Kubar, A.; Akinci, E. Clinical and laboratory features of Crimean-Congo hemorrhagic fever: Predictors of fatality. Int. J. Infect. Dis. 2008, 12, 374–379. [Google Scholar] [CrossRef] [PubMed]
- Swanepoel, R.; Gill, D.E.; Shepherd, A.J.; Leman, P.A.; Mynhardt, J.H.; Harvey, S. The clinical pathology of Crimean-Congo hemorrhagic fever. Rev. Infect. Dis. 1989, 11, S794–S800. [Google Scholar] [CrossRef] [PubMed]
- Maltezou, H.C.; Papa, A. Crimean-Congo hemorrhagic fever: Epidemiological trends and controversies in treatment. BMC Med. 2011, 9, 131. [Google Scholar] [CrossRef] [PubMed]
- Jamieson, D.J.; Theiler, R.N.; Rasmussen, S.A. Emerging infections and pregnancy. Emerg. Infect. Dis. 2006, 12, 1638–1643. [Google Scholar] [CrossRef] [PubMed]
- Pshenichnaya, N.Y.; Leblebicioglu, H.; Bozkurt, I.; Sannikova, I.V.; Abuova, G.N.; Zhuravlev, A.S.; Barut, S.; Shermetova, M.B.; Fletcher, T.E. Crimean-Congo hemorrhagic fever in pregnancy: A systematic review and case series from Russia, Kazakhstan and Turkey. Int. J. Infect. Dis. 2017, 58, 58–64. [Google Scholar] [CrossRef] [PubMed]
- Aslani, D.; Salehi-Vaziri, M.; Baniasadi, V.; Jalali, T.; Azad-Manjiri, S.; Mohammadi, T.; Khakifirouz, S.; Fazlalipour, M. Crimean-Congo hemorrhagic fever among children in Iran. Arch. Virol. 2017, 162, 721–725. [Google Scholar] [CrossRef]
- Stepanova, N.A.; Tabakina, T.E.; Krasovskii, V.A.; Oleinikova Ia, V.; Pogrebova, T.K.; Smirnova, S.E.; Tkachenko, B.A.; Karpovich, S.V. The characteristics of the action of nondepolarizing myorelaxants during operations on children with thermal injuries. Anesteziol Reanimatol 1998, 1, 27–30. [Google Scholar]
- Ergonul, O.; Tuncbilek, S.; Baykam, N.; Celikbas, A.; Dokuzoguz, B. Evaluation of serum levels of interleukin (IL)-6, IL-10, and tumor necrosis factor-alpha in patients with Crimean-Congo hemorrhagic fever. J. Infect. Dis. 2006, 193, 941–944. [Google Scholar] [CrossRef]
- Duru, F.; Fisgin, T. Hematological aspects of Crimean-Congo hemorrhagic fever. Turk. J. Haematol 2009, 26, 161–166. [Google Scholar]
- Onguru, P.; Akgul, E.O.; Akinci, E.; Yaman, H.; Kurt, Y.G.; Erbay, A.; Bayazit, F.N.; Bodur, H.; Erbil, K.; Acikel, C.H.; et al. High serum levels of neopterin in patients with Crimean-Congo hemorrhagic fever and its relation with mortality. J. Infect. 2008, 56, 366–370. [Google Scholar] [CrossRef]
- Ozkurt, Z.; Ozden, K.; Kiki, I.; Usanmaz, M. Prognostic significance of antithrombin activity in patients with crimean-congo hemorrhagic Fever. Eurasian J. Med. 2011, 43, 83–86. [Google Scholar] [CrossRef]
- Yau, J.W.; Teoh, H.; Verma, S. Endothelial cell control of thrombosis. BMC Cardiovasc. Disord 2015, 15, 130. [Google Scholar] [CrossRef] [PubMed]
- Turner, M.D.; Nedjai, B.; Hurst, T.; Pennington, D.J. Cytokines and chemokines: At the crossroads of cell signalling and inflammatory disease. Biochim. Biophys. Acta 2014, 1843, 2563–2582. [Google Scholar] [CrossRef] [PubMed]
- Ergonul, O.; Seref, C.; Eren, S.; Celikbas, A.; Baykam, N.; Dokuzoguz, B.; Gonen, M.; Can, F. Cytokine response in crimean-congo hemorrhagic fever virus infection. J. Med. Virol. 2017, 89, 1707–1713. [Google Scholar] [CrossRef] [PubMed]
- Papa, A.; Bino, S.; Velo, E.; Harxhi, A.; Kota, M.; Antoniadis, A. Cytokine levels in Crimean-Congo hemorrhagic fever. J. Clin. Virol. 2006, 36, 272–276. [Google Scholar] [CrossRef] [PubMed]
- Altay, F.A.; Elaldi, N.; Senturk, G.C.; Altin, N.; Gozel, M.G.; Albayrak, Y.; Sencan, I. Serum sTREM-1 level is quite higher in Crimean Congo Hemorrhagic Fever, a viral infection. J. Med. Virol. 2016, 88, 1473–1478. [Google Scholar] [CrossRef] [PubMed]
- Medvedev, A.E. Toll-like receptor polymorphisms, inflammatory and infectious diseases, allergies, and cancer. J. Interferon Cytokine Res. 2013, 33, 467–484. [Google Scholar] [CrossRef] [PubMed]
- Golden, J.W.; Shoemaker, C.J.; Lindquist, M.L.; Zeng, X.; Daye, S.P.; Williams, J.A.; Liu, J.; Coffin, K.M.; Olshner, S.; Flusin, O.; et al. GP38-targeting monoclonal antibodies protect adult mice against lethal Crimean-Congo hemorrhagic fever virus infection. Sci. Adv. 2019, (in press).
- Fritzen, A.; Risinger, C.; Korukluoglu, G.; Christova, I.; Corli Hitzeroth, A.; Viljoen, N.; Burt, F.J.; Mirazimi, A.; Blixt, O. Epitope-mapping of the glycoprotein from Crimean-Congo hemorrhagic fever virus using a microarray approach. PLoS Negl. Trop. Dis. 2018, 12, e0006598. [Google Scholar] [CrossRef]
- Emmerich, P.; Mika, A.; von Possel, R.; Rackow, A.; Liu, Y.; Schmitz, H.; Günther, S.; Sherifi, K.; Halili, B.; Jakupi, X.; et al. Sensitive and specific detection of Crimean-Congo Hemorrhagic Fever Virus (CCHFV)—Specific IgM and IgG antibodies in human sera using recombinant CCHFV nucleoprotein as antigen in μ-capture and IgG immune complex (IC) ELISA tests. PLOS Negl. Trop. Dis. 2018, 12, e0006366. [Google Scholar] [CrossRef]
- Bertolotti-Ciarlet, A.; Smith, J.; Strecker, K.; Paragas, J.; Altamura, L.A.; McFalls, J.M.; Frias-Staheli, N.; Garcia-Sastre, A.; Schmaljohn, C.S.; Doms, R.W. Cellular localization and antigenic characterization of crimean-congo hemorrhagic fever virus glycoproteins. J. Virol. 2005, 79, 6152–6161. [Google Scholar] [CrossRef]
- Burt, F.J.; Leman, P.A.; Abbott, J.C.; Swanepoel, R. Serodiagnosis of Crimean-Congo haemorrhagic fever. Epidemiol. Infect. 1994, 113, 551–562. [Google Scholar] [CrossRef] [PubMed]
- Yadav, P.D.; Pardeshi, P.G.; Patil, D.Y.; Shete, A.M.; Mourya, D.T. Persistence of IgG antibodies in survivors of Crimean Congo hemorrhagic fever virus infection, India. J. Infect. Public Health 2019. [Google Scholar] [CrossRef] [PubMed]
- Goedhals, D.; Paweska, J.T.; Burt, F.J. Long-lived CD8+ T cell responses following Crimean-Congo haemorrhagic fever virus infection. PLoS Negl. Trop. Dis. 2017, 11, e0006149. [Google Scholar] [CrossRef] [PubMed]
- Vassilenko, S.M.; Vassilev, T.L.; Bozadjiev, L.G.; Bineva, I.L.; Kazarov, G.Z. Specific intravenous immunoglobulin for Crimean-Congo haemorrhagic fever. Lancet 1990, 335, 791–792. [Google Scholar] [CrossRef]
- Ergonul, O.; Celikbas, A.; Baykam, N.; Eren, S.; Dokuzoguz, B. Analysis of risk-factors among patients with Crimean-Congo haemorrhagic fever virus infection: Severity criteria revisited. Clin. Microbiol. Infect. 2006, 12, 551–554. [Google Scholar] [CrossRef] [PubMed]
- Burt, F.J.; Swanepoel, R.; Shieh, W.J.; Smith, J.F.; Leman, P.A.; Greer, P.W.; Coffield, L.M.; Rollin, P.E.; Ksiazek, T.G.; Peters, C.J.; et al. Immunohistochemical and in situ localization of Crimean-Congo hemorrhagic fever (CCHF) virus in human tissues and implications for CCHF pathogenesis. Arch. Pathol. Lab. Med. 1997, 121, 839–846. [Google Scholar] [PubMed]
- Baskerville, A.; Satti, A.; Murphy, F.A.; Simpson, D.I. Congo-Crimean haemorrhagic fever in Dubai: Histopathological studies. J. Clin. Pathol. 1981, 34, 871–874. [Google Scholar] [CrossRef] [PubMed]
- Rodrigues, R.; Paranhos-Baccala, G.; Vernet, G.; Peyrefitte, C.N. Crimean-Congo hemorrhagic fever virus-infected hepatocytes induce ER-stress and apoptosis crosstalk. PLoS ONE 2012, 7, e29712. [Google Scholar] [CrossRef]
- Dufour, J.; Clavien, P.-A. Signaling Pathways in Liver Diseases, 3rd ed.; Dufour, J., Clavien, P., Eds.; John Wiley & Sons, Ltd.: Hoboken, NJ, USA, 2015. [Google Scholar]
- Kleib, A.S.; Salihy, S.M.; Ghaber, S.M.; Sidiel, B.W.; Sidiya, K.C.; Bettar, E.S. Crimean-Congo Hemorrhagic Fever with Acute Subdural Hematoma, Mauritania, 2012. Emerg. Infect. Dis. 2016, 22, 1305–1306. [Google Scholar] [CrossRef]
- Butenko, A.M. Data from studying etiology, laboratory diagnosis, and immunology of Crimean hemorrhagic fever; questions of ecology of the viral agent [in Russian] (in English: NAMRU3-T1152). Avtoref Diss. Soisk Uchen Step Dokt Biol. Nauk. Inst. Poliomiel Virus Enceph. Acad Med. Nauk. SSSR, Mosc, (in Russian) (in English, NAMRU3-T-1152). 1971. [Google Scholar]
- Smorodintsev, A.; Kazkintsev, L.; Chaudakov, V. Virus hemorrhagic fevers (in Russian). Isreal Progam Sci. Transl. Jerus. 1963, 2–156. [Google Scholar]
- Neklyudov, M. A case of hemorrhagic fever (Crimea) (in Russian) (in English: NAMRU3-T1514). Suvrem Med. Sof. 1952, 5, 92–95. [Google Scholar]
- Oztoprak, B.; Oztoprak, I.; Engin, A. Is the brain spared in Crimean-Congo haemorrhagic fever? An MR-SWI study to reveal CNS involvement. Eur. Radiol. 2018, 28, 3893–3901. [Google Scholar] [CrossRef] [PubMed]
- Muco, E.; Como, N.; Bino, S.; Harxhi, A.; Pipero, P.; Kota, M.; Mehmeti, J.; Kushi, A.; Kraja, D. Crimean-Congo hemorrhagic fever with hepatic impairment and vaginal hemorrhage: A case report. J. Med. Case Rep. 2018, 12, 118. [Google Scholar] [CrossRef] [PubMed]
- Dogan, O.T.; Engin, A.; Salk, I.; Epozturk, K.; Eren, S.H.; Elaldi, N.; Bakir, M.; Dokmetas, I.; Akkurt, I. Evaluation of Respiratory Findings in Crimean-Congo Hemorrhagic Fever. Southeast. Asian J. Trop. Med. Public Health 2011, 42, 1100–1105. [Google Scholar] [PubMed]
- Bilgin, G.; Ataman Hatipoglu, C.; Altun, S.; Bulut, C.; Kinikli, S.; Demiroz, A.P. An investigation of pulmonary findings of Crimean-Congo haemorrhagic fever patients. Turk. J. Med. Sci. 2014, 44, 162–167. [Google Scholar] [CrossRef] [PubMed]
- Engin, A.; Yilmaz, M.B.; Elaldi, N.; Erdem, A.; Yalta, K.; Tandogan, I.; Kaya, S.; Bakir, M.; Dokmetas, I. Crimean-Congo hemorrhagic fever: Does it involve the heart? Int. J. Infect. Dis. 2009, 13, 369–373. [Google Scholar] [CrossRef] [PubMed]
- Sannikova, I.V.; Pacechnikov, V.D.; Maleev, V.V. Respiratory lesions in Congo-Crimean hemorrhagic fever. Ter. Arkh. 2007, 79, 20–23. [Google Scholar] [PubMed]
- Aktas, T.; Aktas, F.; Ozmen, Z.; Kaya, T. Does Crimean-Congo Hemorrhagic Fever Cause a Vasculitic Reaction with Pulmonary Artery Enlargement and Acute Pulmonary Hypertension? Lung 2016, 194, 807–812. [Google Scholar] [CrossRef]
- Aktas, T.; Aktas, F.; Ozmen, Z.; Altunkas, A.; Kaya, T.; Demir, O. Thorax CT findings in patients with Crimean-Congo hemorrhagic fever (CCHF). Springerplus 2016, 5, 1823. [Google Scholar] [CrossRef]
- Aktas, F.; Aktas, T. The pulmonary findings of Crimean-Congo hemorrhagic fever patients with chest X-ray assessments. Radiol. Med. 2019. [Google Scholar] [CrossRef]
- Zeller, H.G.; Cornet, J.P.; Camicas, J.L. Experimental transmission of Crimean-Congo hemorrhagic fever virus by west African wild ground-feeding birds to Hyalomma marginatum rufipes ticks. Am. J. Trop. Med. Hyg. 1994, 50, 676–681. [Google Scholar] [CrossRef] [PubMed]
- Chumakov, M.P.; Butenko, A.M.; Shalunova, N.V.; Mart’ianova, L.I.; Smirnova, S.E.; Bashkirtsev Iu, N.; Zavodova, T.I.; Rubin, S.G.; Tkachenko, E.A.; Karmysheva, V.; et al. New data on the viral agent of Crimean hemorrhagic fever. Vopr. Virusol. 1968, 13, 377. [Google Scholar] [PubMed]
- Bereczky, S.; Lindegren, G.; Karlberg, H.; Akerstrom, S.; Klingstrom, J.; Mirazimi, A. Crimean-Congo hemorrhagic fever virus infection is lethal for adult type I interferon receptor-knockout mice. J. Gen. Virol. 2010, 91, 1473–1477. [Google Scholar] [CrossRef] [PubMed]
- Zivcec, M.; Safronetz, D.; Scott, D.; Robertson, S.; Ebihara, H.; Feldmann, H. Lethal Crimean-Congo hemorrhagic fever virus infection in interferon alpha/beta receptor knockout mice is associated with high viral loads, proinflammatory responses, and coagulopathy. J. Infect. Dis. 2013, 207, 1909–1921. [Google Scholar] [CrossRef] [PubMed]
- Bente, D.A.; Alimonti, J.B.; Shieh, W.J.; Camus, G.; Stroher, U.; Zaki, S.; Jones, S.M. Pathogenesis and immune response of Crimean-Congo hemorrhagic fever virus in a STAT-1 knockout mouse model. J. Virol. 2010, 84, 11089–11100. [Google Scholar] [CrossRef]
- Aligholipour Farzani, T.; Foldes, K.; Hanifehnezhad, A.; Yener Ilce, B.; Bilge Dagalp, S.; Amirzadeh Khiabani, N.; Ergunay, K.; Alkan, F.; Karaoglu, T.; Bodur, H.; et al. Bovine Herpesvirus Type 4 (BoHV-4) Vector Delivering Nucleocapsid Protein of Crimean-Congo Hemorrhagic Fever Virus Induces Comparable Protective Immunity against Lethal Challenge in IFNalpha/beta/gammaR−/− Mice Models. Viruses 2019, 11. [Google Scholar] [CrossRef] [PubMed]
- Sheehan, K.C.; Lai, K.S.; Dunn, G.P.; Bruce, A.T.; Diamond, M.S.; Heutel, J.D.; Dungo-Arthur, C.; Carrero, J.A.; White, J.M.; Hertzog, P.J.; et al. Blocking monoclonal antibodies specific for mouse IFN-alpha/beta receptor subunit 1 (IFNAR-1) from mice immunized by in vivo hydrodynamic transfection. J. Interferon Cytokine Res. 2006, 26, 804–819. [Google Scholar] [CrossRef]
- Pinto, A.K.; Daffis, S.; Brien, J.D.; Gainey, M.D.; Yokoyama, W.M.; Sheehan, K.C.; Murphy, K.M.; Schreiber, R.D.; Diamond, M.S. A temporal role of type I interferon signaling in CD8+ T cell maturation during acute West Nile virus infection. PLoS Pathog. 2011, 7, e1002407. [Google Scholar] [CrossRef]
- Garrison, A.R.; Shoemaker, C.J.; Golden, J.W.; Fitzpatrick, C.J.; Suschak, J.J.; Richards, M.J.; Badger, C.V.; Six, C.M.; Martin, J.D.; Hannaman, D.; et al. A DNA vaccine for Crimean-Congo hemorrhagic fever protects against disease and death in two lethal mouse models. PLoS Negl. Trop. Dis. 2017, 11, e0005908. [Google Scholar] [CrossRef]
- Lindquist, M.E.; Zeng, X.; Altamura, L.A.; Daye, S.P.; Delp, K.L.; Blancett, C.; Coffin, K.M.; Koehler, J.W.; Coyne, S.; Shoemaker, C.J.; et al. Exploring Crimean-Congo hemorrhagic fever virus-induced hepatic injury using antibody-mediated type I interferon blockade in mice. J. Virol. 2018. [Google Scholar] [CrossRef]
- Spengler, J.R.; Kelly Keating, M.; McElroy, A.K.; Zivcec, M.; Coleman-McCray, J.D.; Harmon, J.R.; Bollweg, B.C.; Goldsmith, C.S.; Bergeron, E.; Keck, J.G.; et al. Crimean-Congo Hemorrhagic Fever in Humanized Mice Reveals Glial Cells as Primary Targets of Neurological Infection. J. Infect. Dis. 2017, 216, 1386–1397. [Google Scholar] [CrossRef] [PubMed]
- Tignor, G.H.; Hanham, C.A. Ribavirin efficacy in an in vivo model of Crimean-Congo hemorrhagic fever virus (CCHF) infection. Antivir. Res. 1993, 22, 309–325. [Google Scholar] [CrossRef]
- Rodriguez, S.E.; Cross, R.W.; Fenton, K.A.; Bente, D.A.; Mire, C.E.; Geisbert, T.W. Vesicular Stomatitis Virus-Based Vaccine Protects Mice against Crimean-Congo Hemorrhagic Fever. Sci. Rep. 2019, 9, 7755. [Google Scholar] [CrossRef] [PubMed]
- Hawman, D.W.; Haddock, E.; Meade-White, K.; Williamson, B.; Hanley, P.W.; Rosenke, K.; Komeno, T.; Furuta, Y.; Gowen, B.B.; Feldmann, H. Favipiravir (T-705) but not ribavirin is effective against two distinct strains of Crimean-Congo hemorrhagic fever virus in mice. Antivir. Res. 2018, 157, 18–26. [Google Scholar] [CrossRef] [PubMed]
- Haddock, E.; Feldmann, F.; Hawman, D.W.; Zivcec, M.; Hanley, P.W.; Saturday, G.; Scott, D.P.; Thomas, T.; Korva, M.; Avsic-Zupanc, T.; et al. A cynomolgus macaque model for Crimean-Congo haemorrhagic fever. Nat. Microbiol. 2018. [Google Scholar] [CrossRef] [PubMed]
- Smith, D.R.; Shoemaker, C.J.; Zeng, X.; Garrison, A.R.; Golden, J.W.; Schellhase, C.; Pratt, D.W.; Rossi, F.D.; Fitzpatrick, C.J.; Shamblin, J.D.; et al. Persistent Crimean-Congo Hemorrhagic Fever Virus Infection in the Testes and within Granulomas of Nonhuman Primates with Latent Tuberculosis (under review).
- Causey, O.R.; Kemp, G.E.; Madbouly, M.H.; David-West, T.S. Congo virus from domestic livestock, African hedgehog, and arthropods in Nigeria. Am. J. Trop. Med. Hyg. 1970, 19, 846–850. [Google Scholar] [CrossRef]
- Olschlager, S.; Gabriel, M.; Schmidt-Chanasit, J.; Meyer, M.; Osborn, E.; Conger, N.G.; Allan, P.F.; Gunther, S. Complete sequence and phylogenetic characterisation of Crimean-Congo hemorrhagic fever virus from Afghanistan. J. Clin. Virol. 2011, 50, 90–92. [Google Scholar] [CrossRef]
- Duh, D.; Nichol, S.T.; Khristova, M.L.; Saksida, A.; Hafner-Bratkovic, I.; Petrovec, M.; Dedushaj, I.; Ahmeti, S.; Avsic-Zupanc, T. The complete genome sequence of a Crimean-Congo hemorrhagic fever virus isolated from an endemic region in Kosovo. Virol. J. 2008, 5. [Google Scholar] [CrossRef]
- Begum, F.; Wisseman, C.L., Jr.; Casals, J. Tick-borne viruses of West Pakistan. II. Hazara virus, a new agent isolated from Ixodes redikorzevi ticks from the Kaghan Valley, W. Pakistan. Am. J. Epidemiol 1970, 92, 192–194. [Google Scholar] [CrossRef]
- Anonymous, Hazara (HAZ) strain. JC 280. Am. J. Trop. Med. Hyg. 1970, 19, 1095–1096. [Google Scholar] [CrossRef]
- Shimada, S.; Aoki, K.; Nabeshima, T.; Fuxun, Y.; Kurosaki, Y.; Shiogama, K.; Onouchi, T.; Sakaguchi, M.; Fuchigami, T.; Ono, H.; et al. Tofla virus: A newly identified Nairovirus of the Crimean-Congo hemorrhagic fever group isolated from ticks in Japan. Sci. Rep. 2016, 6, 20213. [Google Scholar] [CrossRef] [PubMed]
- Causey, O.R. In supplement to the catalogue of Arthopod-borne viruses, No 226. Am. J. Trop. Med. Hyg. 1970, 19, 1123–1124. [Google Scholar]
- Cash, P. Polypeptide synthesis of Dugbe virus, a member of the Nairovirus genus of the Bunyaviridae. J. Gen. Virol. 1985, 66, 141–148. [Google Scholar] [CrossRef] [PubMed]
- Sweet, C.; Coates, D.M. Studies of the pathogenesis of Dugbe virus in normal and in immunosuppressed mice. In Hemorrhagic Fever with Renal Syndrome, Tick-and Mosquito-Borne Viruses; Springer: Vienna, Austria, 1990; Volume 1, pp. 181–195. [Google Scholar]
- Golden, J.W. Infection studies of Crimean-Congo hemorrhagic fever virus in wild-type and transgenic mice. (in preparation)
- Dowall, S.D.; Graham, V.A.; Rayner, E.; Hunter, L.; Watson, R.; Taylor, I.; Rule, A.; Carroll, M.W.; Hewson, R. Protective effects of a Modified Vaccinia Ankara-based vaccine candidate against Crimean-Congo Haemorrhagic Fever virus require both cellular and humoral responses. PLoS ONE 2016, 11, e0156637. [Google Scholar] [CrossRef]
- Burt, F.J.; Spencer, D.C.; Leman, P.A.; Patterson, B.; Swanepoel, R. Investigation of tick-borne viruses as pathogens of humans in South Africa and evidence of Dugbe virus infection in a patient with prolonged thrombocytopenia. Epidemiol Infect. 1996, 116, 353–361. [Google Scholar] [CrossRef]
- Eguchi, A.; Wree, A.; Feldstein, A.E. Biomarkers of liver cell death. J. Hepatol. 2014, 60, 1063–1074. [Google Scholar] [CrossRef]
- Wang, X.; Ning, Q. Immune mediated liver failure. EXCLI J. 2014, 13, 1131–1144. [Google Scholar]
- Ogasawara, J.; Watanabe-Fukunaga, R.; Adachi, M.; Matsuzawa, A.; Kasugai, T.; Kitamura, Y.; Itoh, N.; Suda, T.; Nagata, S. Lethal effect of the anti-Fas antibody in mice. Nature 1993, 364, 806–809. [Google Scholar] [CrossRef]
- Schwabe, R.F.; Brenner, D.A. Mechanisms of Liver Injury. I. TNF-alpha-induced liver injury: Role of IKK, JNK, and ROS pathways. Am. J. Physiol. Gastrointest Liver Physiol. 2006, 290, G583–G589. [Google Scholar] [CrossRef]
- Huys, L.; van Hauwermeiren, F.; Dejager, L.; Dejonckheere, E.; Lienenklaus, S.; Weiss, S.; Leclercq, G.; Libert, C. Type I interferon drives tumor necrosis factor-induced lethal shock. J. Exp. Med. 2009, 206, 1873–1882. [Google Scholar] [CrossRef]
- Buttigieg, K.R.; Dowall, S.D.; Findlay-Wilson, S.; Miloszewska, A.; Rayner, E.; Hewson, R.; Carroll, M.W. A novel vaccine against Crimean-Congo Haemorrhagic Fever protects 100% of animals against lethal challenge in a mouse model. PLoS ONE 2014, 9, e91516. [Google Scholar] [CrossRef] [PubMed]
- Hinkula, J.; Devignot, S.; Akerstrom, S.; Karlberg, H.; Wattrang, E.; Bereczky, S.; Mousavi-Jazi, M.; Risinger, C.; Lindegren, G.; Vernersson, C.; et al. Immunization with DNA Plasmids Coding for Crimean-Congo Hemorrhagic Fever Virus Capsid and Envelope Proteins and/or Virus-Like Particles Induces Protection and Survival in Challenged Mice. J. Virol. 2017. [Google Scholar] [CrossRef] [PubMed]
- Scholte, F.E.M.; Spengler, J.R.; Welch, S.R.; Harmon, J.R.; Coleman-McCray, J.D.; Freitas, B.T.; Kainulainen, M.H.; Pegan, S.D.; Nichol, S.T.; Bergeron, E.; et al. Single-dose replicon particle vaccine provides complete protection against Crimean-Congo hemorrhagic fever virus in mice. Emerg. Microbes Infect. 2019, 8, 575–578. [Google Scholar] [CrossRef] [PubMed]
- Dowall, S.D.; Buttigieg, K.R.; Findlay-Wilson, S.J.; Rayner, E.; Pearson, G.; Miloszewska, A.; Graham, V.A.; Carroll, M.W.; Hewson, R. A Crimean-Congo hemorrhagic fever (CCHF) viral vaccine expressing nucleoprotein is immunogenic but fails to confer protection against lethal disease. Hum. Vaccin. Immunother. 2016, 12, 519–527. [Google Scholar] [CrossRef]
- Kortekaas, J.; Vloet, R.P.; McAuley, A.J.; Shen, X.; Bosch, B.J.; de Vries, L.; Moormann, R.J.; Bente, D.A. Crimean-Congo Hemorrhagic Fever Virus Subunit Vaccines Induce High Levels of Neutralizing Antibodies But No Protection in STAT1 Knockout Mice. Vector Borne Zoonotic Dis. 2015, 15, 759–764. [Google Scholar] [CrossRef]
- Canakoglu, N.; Berber, E.; Tonbak, S.; Ertek, M.; Sozdutmaz, I.; Aktas, M.; Kalkan, A.; Ozdarendeli, A. Immunization of knock-out alpha/beta interferon receptor mice against high lethal dose of Crimean-Congo hemorrhagic fever virus with a cell culture based vaccine. PLoS Negl. Trop. Dis. 2015, 9, e0003579. [Google Scholar] [CrossRef]
- Zivcec, M.; Safronetz, D.; Scott, D.P.; Robertson, S.; Feldmann, H. Nucleocapsid protein-based vaccine provides protection in mice against lethal Crimean-Congo hemorrhagic fever virus challenge. PLoS Negl. Trop. Dis. 2018, 12, e0006628. [Google Scholar] [CrossRef]
- Mousavi-Jazi, M.; Karlberg, H.; Papa, A.; Christova, I.; Mirazimi, A. Healthy individuals’ immune response to the Bulgarian Crimean-Congo hemorrhagic fever virus vaccine. Vaccine 2012, 30, 6225–6229. [Google Scholar] [CrossRef]
- Gargili, A.; Estrada-Pena, A.; Spengler, J.R.; Lukashev, A.; Nuttall, P.A.; Bente, D.A. The role of ticks in the maintenance and transmission of Crimean-Congo hemorrhagic fever virus: A review of published field and laboratory studies. Antivir. Res. 2017, 144, 93–119. [Google Scholar] [CrossRef]
- Xia, H.; Beck, A.S.; Gargili, A.; Forrester, N.; Barrett, A.D.; Bente, D.A. Transstadial Transmission and Long-term Association of Crimean-Congo Hemorrhagic Fever Virus in Ticks Shapes Genome Plasticity. Sci. Rep. 2016, 6, 35819. [Google Scholar] [CrossRef] [PubMed]
- Levi, V.; Vasilenko, S. Study on the Crimean hemorrhagic fever (CHF) virus transmission mechansim in Hyalomma pl. plumbeum ticks. Epidemiol. Mikrobiol. Infekts. Boles. 1972, 9, 182–185. [Google Scholar]
- Gargili, A.; Thangamani, S.; Bente, D. Influence of laboratory animal hosts on the life cycle of Hyalomma marginatum and implications for an in vivo transmission model for Crimean-Congo hemorrhagic fever virus. Front. Cell Infect. Microbiol. 2013, 3, 39. [Google Scholar] [CrossRef] [PubMed]
- Berezin, V.V. Investigation of the ecology of arboviruses in river deltas of the Caspian and Azov Sea basins (In English: NAMRU3-T1160). Avtoref Diss. Soisk Uchen Step Dokt. Biol. Nauk Inst. Polio Virus Entsef Akad Med. Nauk SSSR 1971, 37. [Google Scholar]
- Shepherd, A.J.; Swanepoel, R.; Cornel, A.J.; Mathee, O. Experimental studies on the replication and transmission of Crimean-Congo hemorrhagic fever virus in some African tick species. Am. J. Trop. medicine Hyg. 1989, 40, 326–331. [Google Scholar] [CrossRef] [PubMed]
- Rodriguez, S.E.; McAuley, A.J.; Gargili, A.; Bente, D.A. Interactions of Human Dermal Dendritic Cells and Langerhans Cells Treated with Hyalomma Tick Saliva with Crimean-Congo Hemorrhagic Fever Virus. Viruses 2018, 10. [Google Scholar] [CrossRef] [PubMed]
- Fagbami, A.H.; Tomori, O.; Fabiyi, A.; Isoun, T.T. Experimantal Congo virus (Ib -AN 7620) infection in primates. Virologie 1975, 26, 33–37. [Google Scholar] [PubMed]
- Pratt, W.D.; Gibbs, P.; Pitt, M.L.; Schmaljohn, A.L. Use of telemetry to assess vaccine-induced protection against parenteral and aerosol infections of Venezuelan equine encephalitis virus in non-human primates. Vaccine 1998, 16, 1056–1064. [Google Scholar] [CrossRef]
- Rossi, S.L.; Russell-Lodrigue, K.E.; Killeen, S.Z.; Wang, E.; Leal, G.; Bergren, N.A.; Vinet-Oliphant, H.; Weaver, S.C.; Roy, C.J. IRES-Containing VEEV Vaccine Protects Cynomolgus Macaques from IE Venezuelan Equine Encephalitis Virus Aerosol Challenge. PLoS Negl. Trop. Dis. 2015, 9, e0003797. [Google Scholar] [CrossRef]
- Papa, A.; Papadimitriou, E.; Christova, I. The Bulgarian vaccine Crimean-Congo haemorrhagic fever virus strain. Scand. J. Infect. Dis. 2010, 43, 225–229. [Google Scholar] [CrossRef]
- Bodur, H.; Erbay, A.; Akinci, E.; Onguru, P.; Bayazit, N.; Eren, S.S.; Kubar, A. Effect of oral ribavirin treatment on the viral load and disease progression in Crimean-Congo hemorrhagic fever. Int. J. Infect. Dis. 2011, 15, e44–e47. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Ceylan, B.; Calica, A.; Ak, O.; Akkoyunlu, Y.; Turhan, V. Ribavirin is not effective against Crimean-Congo hemorrhagic fever: Observations from the Turkish experience. Int. J. Infect. Dis. 2013, 17, e799–e801. [Google Scholar] [CrossRef] [PubMed]
- Dokuzoguz, B.; Celikbas, A.K.; Gok, S.E.; Baykam, N.; Eroglu, M.N.; Ergonul, O. Severity scoring index for Crimean-Congo hemorrhagic fever and the impact of ribavirin and corticosteroids on fatality. Clin. Infect. Dis. 2013, 57, 1270–1274. [Google Scholar] [CrossRef] [PubMed]
- Keshtkar-Jahromi, M.; Sajadi, M.M.; Ansari, H.; Mardani, M.; Holakouie-Naieni, K. Crimean-Congo hemorrhagic fever in Iran. Antiviral Res. 2013, 100, 20–28. [Google Scholar] [CrossRef]
- Koksal, I.; Yilmaz, G.; Aksoy, F.; Aydin, H.; Yavuz, I.; Iskender, S.; Akcay, K.; Erensoy, S.; Caylan, R.; Aydin, K. The efficacy of ribavirin in the treatment of Crimean-Congo hemorrhagic fever in Eastern Black Sea region in Turkey. J. Clin. Virol. 2010, 47, 65–68. [Google Scholar] [CrossRef]
- Mardani, M.; Jahromi, M.K.; Naieni, K.H.; Zeinali, M. The efficacy of oral ribavirin in the treatment of crimean-congo hemorrhagic fever in Iran. Clin. Infect. Dis. 2003, 36, 1613–1618. [Google Scholar] [CrossRef]
- Sharifi-Mood, B.; Alavi-Naini, R.; Metanat, M.; Mohammadi, M.; Shakeri, A.; Amjadi, A. Efficacy of high-dose methylprednisolone in patients with Crimean-Congo haemorrhagic fever and severe thrombocytopenia. Trop. Doct. 2013, 43, 49–53. [Google Scholar] [CrossRef]
- Soares-Weiser, K.; Thomas, S.; Thomson, G.; Garner, P. Ribavirin for Crimean-Congo hemorrhagic fever: Systematic review and meta-analysis. BMC Infect. Dis. 2010, 10, 207. [Google Scholar] [CrossRef]
- Jabbari, A.; Besharat, S.; Abbasi, A.; Moradi, A.; Kalavi, K. Crimean-Congo hemorrhagic fever: Case series from a medical center in Golestan province, Northeast of Iran (2004). Indian J. Med. Sci. 2006, 60, 327–329. [Google Scholar] [CrossRef]
- Keshtkar-Jahromi, M.; Kuhn, J.H.; Christova, I.; Bradfute, S.B.; Jahrling, P.B.; Bavari, S. Crimean-Congo hemorrhagic fever: Current and future prospects of vaccines and therapies. Antiviral Res. 2011, 90, 85–92. [Google Scholar] [CrossRef]
- Suleiman, M.N.; Muscat-Baron, J.M.; Harries, J.R.; Satti, A.G.; Platt, G.S.; Bowen, E.T.; Simpson, D.I. Congo/Crimean haemorrhagic fever in Dubai. An outbreak at the Rashid Hospital. Lancet 1980, 2, 939–941. [Google Scholar] [CrossRef]
- Fisher-Hoch, S.P.; Khan, J.A.; Rehman, S.; Mirza, S.; Khurshid, M.; McCormick, J.B. Crimean Congo-haemorrhagic fever treated with oral ribavirin. Lancet 1995, 346, 472–475. [Google Scholar] [PubMed]
- Cevik, M.A.; Elaldi, N.; Akinci, E.; Onguru, P.; Erbay, A.; Buzgan, T.; Uzun, R.; Kubar, A.; Bodur, H. A preliminary study to evaluate the effect of intravenous ribavirin treatment on survival rates in Crimean-Congo hemorrhagic fever. J. Infect. 2008, 57, 350–351. [Google Scholar] [CrossRef] [PubMed]
- Ergonul, O. Evidence supports ribavirin use in Crimean-Congo hemorrhagic fever. Int. J. Infect. Dis. 2014, 29, 296. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Oestereich, L.; Rieger, T.; Neumann, M.; Bernreuther, C.; Lehmann, M.; Krasemann, S.; Wurr, S.; Emmerich, P.; de Lamballerie, X.; Olschlager, S.; et al. Evaluation of antiviral efficacy of ribavirin, arbidol, and T-705 (favipiravir) in a mouse model for Crimean-Congo hemorrhagic fever. PLoS Negl. Trop. Dis. 2014, 8, e2804. [Google Scholar] [CrossRef] [PubMed]
- Dowall, S.D.; Carroll, M.W.; Hewson, R. Development of vaccines against Crimean-Congo haemorrhagic fever virus. Vaccine 2017, 35, 6015–6023. [Google Scholar] [CrossRef] [PubMed]
- Papa, A.; Mirazimi, A.; Koksal, I.; Estrada-Pena, A.; Feldmann, H. Recent advances in research on Crimean-Congo hemorrhagic fever. J. Clin. Virol. 2015, 64, 137–143. [Google Scholar] [CrossRef]
- Hawman, D.W.; Feldmann, H. Recent advances in understanding Crimean-Congo hemorrhagic fever virus. F1000Res 2018, 7. [Google Scholar] [CrossRef]
- Suschak, J.J.; Wang, S.; Fitzgerald, K.A.; Lu, S. A cGAS-Independent STING/IRF7 Pathway Mediates the Immunogenicity of DNA Vaccines. J. Immunol. 2016, 196, 310–316. [Google Scholar] [CrossRef]
- Han, N.; Rayner, S. Epidemiology and mutational analysis of global strains of Crimean-Congo haemorrhagic fever virus. Virol. Sin. 2011, 26, 229–244. [Google Scholar] [CrossRef]
- Zivcec, M.; Guerrero, L.I.W.; Albarino, C.G.; Bergeron, E.; Nichol, S.T.; Spiropoulou, C.F. Identification of broadly neutralizing monoclonal antibodies against Crimean-Congo hemorrhagic fever virus. Antivir. Res. 2017, 146, 112–120. [Google Scholar] [CrossRef] [PubMed]
- Ahmed, A.A.; McFalls, J.M.; Hoffmann, C.; Filone, C.M.; Stewart, S.M.; Paragas, J.; Khodjaev, S.; Shermukhamedova, D.; Schmaljohn, C.S.; Doms, R.W.; et al. Presence of broadly reactive and group-specific neutralizing epitopes on newly described isolates of Crimean-Congo hemorrhagic fever virus. J. Gen. Virol. 2005, 86, 3327–3336. [Google Scholar] [CrossRef] [PubMed]
- Dowall, S.D.; Findlay-Wilson, S.; Rayner, E.; Pearson, G.; Pickersgill, J.; Rule, A.; Merredew, N.; Smith, H.; Chamberlain, J.; Hewson, R. Hazara virus infection is lethal for adult type I interferon receptor-knockout mice and may act as a surrogate for infection with the human-pathogenic Crimean-Congo hemorrhagic fever virus. J. Gen. Virol. 2012, 93, 560–564. [Google Scholar] [CrossRef] [PubMed]
- Smirnova, S.E.; Shestopalova, N.M.; Reingold, V.N.; Zubri, G.L.; Chumakov, M.P. Experimental Hazara Virus infection in mice. Acta Virol. 1977, 21, 128–132. [Google Scholar] [PubMed]
- Coates, D.M.; Sweet, C. Studies on the pathogenicity of a nairovirus, Dugbe virus, in normal and immunosuppressed mice. J. Gen. Virol. 1990, 71, 325–332. [Google Scholar] [CrossRef] [PubMed]
- Boyd, A.; Fazakerley, J.K.; Bridgen, A. Pathogenesis of Dugbe virus infection in wild-type and interferon-deficient mice. J. Gen. Virol. 2006, 87, 2005–2009. [Google Scholar] [CrossRef]
- David-West, T.S. Dugbe virus: A new tick-borne arbovirus from Nigeria. Trans. R. Soc. Tro.p Med. Hyg. 1973, 67, 438. [Google Scholar] [CrossRef]
- David-West, T.S.; Cooke, A.R.; David-West, A.S. A serological survey of Dugbe virus antibodies in Nigerians. Trans. R. Soc. Trop. Med. Hyg. 1975, 69, 358. [Google Scholar] [CrossRef]
- Hansford, K.M.; Carter, D.; Gillingham, E.L.; Hernandez-Triana, L.M.; Chamberlain, J.; Cull, B.; McGinley, L.; Paul Phipps, L.; Medlock, J.M. Hyalomma rufipes on an untraveled horse: Is this the first evidence of Hyalomma nymphs successfully moulting in the United Kingdom? Ticks Tick Borne Dis. 2019, 10, 704–708. [Google Scholar] [CrossRef]
- Bartolini, B.; Gruber, C.E.; Koopmans, M.; Avsic, T.; Bino, S.; Christova, I.; Grunow, R.; Hewson, R.; Korukluoglu, G.; Lemos, C.M.; et al. Laboratory management of Crimean-Congo haemorrhagic fever virus infections: Perspectives from two European networks. Euro Surveill. 2019, 24. [Google Scholar] [CrossRef]
- Papa, A. Diagnostic approaches for Crimean-Congo hemorrhagic fever virus. Expert Rev. Mol. Diagn. 2019, 19, 531–536. [Google Scholar] [CrossRef] [PubMed]
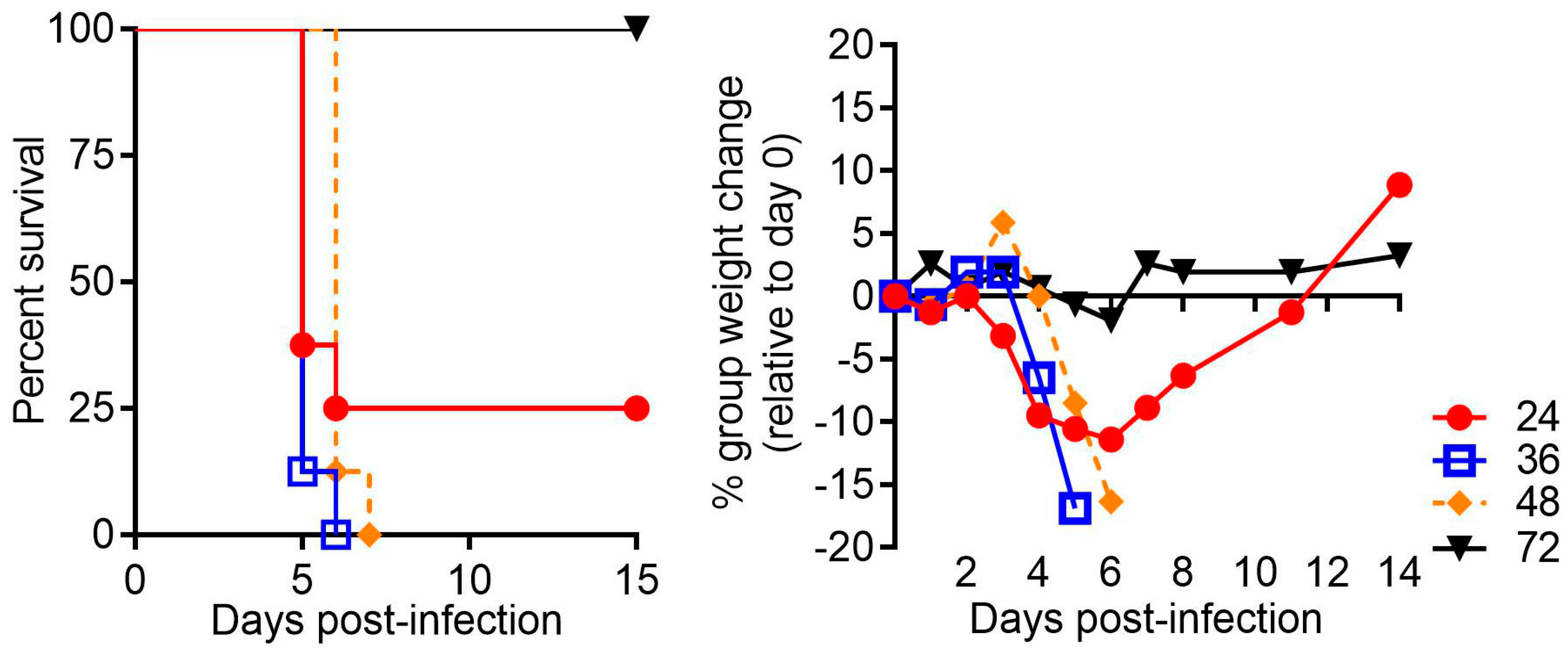
| Animal Model | Virus Strain(s) | Virus Dose | Route(s) of Infection | % lethality | Time to Death [days] | Salient Features | REF |
|---|---|---|---|---|---|---|---|
| Neonatal mice | IbAr 10200 | 100 Lethal-dose units | IP | 100 | 3 d | Do not predict immunotherapeutic protection behavior in adult rodents, Ribavirin protects against lethality | [85] |
| STAT-1−/− mice | IbAr 10200, Turkey-2004 | 10-1000 PFU | SC, IP | 20–100 | 3–6 d | hepatic injury, subunit vaccines may not protect well in this model. 10 PFUtick dose is only 20% lethal, higher doses uniformly lethal | [78,86] |
| IFNAR−/− mice | IbAr 10200, Afg09-2990, Hoti | 10-10,000 TCID50 or PFU | SC, IP, IN, IM | >90 | 4–8 d | Prototypical rodent model for CCHFV, C57BL/6 or 129 background develop severe disease. Strain Hoti has a reduced MTD | [76,77,82,87] |
| IFNAR−/−, IFNAGR−/− mice | Ank-2 | 100 TCID50 | IP | 100 | 4–6 d | Used to evaluate N subunit vaccines | [79] |
| C57BL/6, BALB/c, B6:129 | IbAr 10200, Afg09-2990, Hoti | 100 PFU | SC, IP | >90 (IFN-I blockade) | 5 d | No disease ensues unless IFN-I signaling is blocked by antibody (MAR1-5A3) | [48,83] |
| Rag2−/− mice | Afg09-2990, Hoti | 100 PFU | IP | 100 | 4–5 d after disruption of IFN-I signaling | Hepatitis in mice with active IFN-I signaling, disruption of IFN-I signaling results in 100% lethality similar to normal mice | [83] |
| SGM3 Humanized mice | Turkey-2004, Oman-199809166 | 1 × 104 TCID50 | IP | 0 or 100 | 15–23 d | Neurological disease ensues absent of systemic (visceral) disease. Only strain Turkey produced severe disease and lethality. Oman is not lethal | [84] |
| Cynomolgus Macaques | Hoti, Afg09-2990 | 5log10 TCID50 and 1 × 106 PFU | IV, SC and IV/SC combo | 0–60 | 6–7 d | Disease model with fever, increased liver enzymes, thrombocytopenia, leukocytopenia. In some studies animals meet euthanasia criteria | [88,89] |
| Virus | Strain | Origin | Passage History | Animal Model | REF |
|---|---|---|---|---|---|
| CCHFV | IbAr 10200 | 1966, tick-isolate (Hyalomma excavatum), Nigeria | 9× SMB 1, 3× HepG2 2 | Mice | [90] |
| Afg09-2990 | 2009, human-isolate, fatal case, Afghanistan | 3× Vero 2, 2× Huh7 2 | Mice, NHP | [91] | |
| Kosova Hoti | 2001, human isolate, fatal case, Kosovo | 2× VeroE6 2 | Mice, NHP | [92] | |
| Oman-199809166 | 1998, human-isolate, outcome unknown, Oman | 2× VeroE6, 1× SW13 2 | Mice | [84] | |
| Turkey-200406546 | 2004, human-isolate, outcome unknown, Turkey | 1× SMB, 1× SW13 | Mice | [84] | |
| Ank-2 | 2012, human-isolate, outcome unknown, Turkey | 3× SW13 | Mice | [79] | |
| HAZV | JC280 | 1964, tick-isolate (Ixodes redikorzevi), Pakistan | SMB | Mice | [93,94] |
| TOFV | Tok-Hfla-2013 | 2013, tick-isolate (H. formosensis), Japan | Not passaged, homogenized ticks used | Mice | [95] |
| DUGV | IbAr 1792 | 1964, tick-isolate (Amblyomma variegatum), Nigeria | SMB | Mice | [96] |
| KT281/75 | 1975, tick-isolate (Amblyomma variegatum), Nigeria | 5× BSC-1 2, 2× SMB | Mice | [97] | |
| IbH11480 | 1966, human-isolate, Nigeria | 5× SMB | Mice | [98] |
| Vaccine. | Treatment Regimen | Route of Vaccination | Animal Species/Strain | % Protection | Target(s) | Mechanism of Protection | Human Efficacy Data | REF |
|---|---|---|---|---|---|---|---|---|
| MVA-GP | 1 × 107 PFU/dose, 2 doses | IM | IFNAR−/−(A129) | 100 | M-segment glycoproteins | antibody appeared irrelevant | N | [107] |
| M-segment DNA vaccine | 25 µg DNA, three doses | IM electroporation | IFNAR−/−(C57BL/6), or C57BL/6 (mAb 5A3 treated upon challenge) | 60–70 | M-segment glycoproteins | neutralizing and total antibody titers do not correlate with protection | N | [82] |
| rVSV expressing M-segment ORF | 1 or 2 doses of 107 PFU/dose | IP | STAT-1 | 100 | M-segment glycoproteins | antibody against glycoproteins, and neutralizing antibody titers but mechanism is unclear | N | [86] |
| GN/GC and N DNA vaccine and/or VLPs | 50 µg DNA; 1 × 106 VLPs, three doses varying combinations | intradermal electroporation (DNA), IP (VLP) | IFNAR−/−(A129) | 100 | GN, GC and N | unknown | N | [108] |
| Bovine Herpesvirus N subunit vaccine | 100 TCID50, two doses | IM | IFNAGR−/− | 100 | N | unknown | N | [79] |
| CCHF virus-like replicon particle with M-segment | 1 dose of 105 TCID50 or 103 TCID50 | SC | IFNAR−/− | 103 TCID50 (80%), 105 TCID50 (100%) | M-segment glycoproteins | unknown | N | [109] |
| MVA-NP | 1 or 2 doses of 107 PFU/dose | IM | IFNAR−/−(A129) | 0 | N | not protective | N | [110] |
| GN ectodomain or GC ectodomain subunit vaccines | 2 doses 7.5 µg GC or 15 µg GN | IP | STAT-1 | 0 + | GN or GC | not protective | N | [111] |
| Formalin inactivated cell culture derived CCHFV mixed with alum | 3 doses of 5, 20, or 40 µg | IP | IFNAR−/− | 5 µg dose (60%), 20 and 40 µg (80%) | Whole virus | antibody against glycoproteins, and neutralizing antibody titers but mechanism is unclear | N | [112] |
| Adenovirus N subunit vaccine | 1.25 × 107 IFU | IM | IFNAR−/−(C57BL/6) | 33–78 | N | prime/boost more protective | N | [113] |
| Mouse brain-derived chloroform and heat inactivated CCHFV strain V42/81 # adsorbed on Al(OH)3 | 1 mL doses (day 0 and 30, 1 y and every 5 y thereafter (given March-April) | SC | humans | Unknown | Whole virus | antibody against glycoproteins and N, and T-cell response to N but mechanism is unclear | Y | [114] |
| Class | MCM | Treatment Regimen | Route of Delivery | Animal Species/Strain | Post-Exposure Protection | % Protection | Target(s) | Mechanism of Protection | Human Efficacy Data | REF |
|---|---|---|---|---|---|---|---|---|---|---|
| Immunotherapeutic | CCHF-bulin # | 3–9 mL, 1–5 d or longer | IM | humans | Y | >60(human) | antibody targets unidentified | human convalescent plasma | Y | [55] |
| CCHF-venin# | 30 mL combined with 30 mL of CCHF-Bulin | IV | humans | Y | 100(human) | antibody targets unidentified | human convalescent plasma | Y | [55] | |
| mAb-13G8 | 1 mg/dose, two doses | SC, IP | IFNAR−/−, mAb 5A3 treated C57BL/6 mice | Y | 70–100 | GP38 | may involve complement | N | [48] | |
| Small-molecule | Ribavirin # | 500 mg (oral), 30 mg/kg–7.5 mg/kg IV | oral, SC #, IV #, IP ^ | humans, mice (STAT-1 and IFNAR−/−) | Y | 20–80 Mice Unclear * (Human) | Nucleoside-analog | targets viral RNA synthesis | Y * | [78,85,87,131,137,138,139] |
| Favipiravir | 300 mg/kg | IP | IFNAR−/−mice | Y | 100 | Nucleoside-analog | targets viral RNA synthesis | N | [87,140] |
| Virus | Animal Model | Virus Strain(s) | Virus Dose | Route(s) of Infection | % Lethality | Time to Death [days] | Salient Features | REF |
|---|---|---|---|---|---|---|---|---|
| HAZV | Neonatal mice | JC280 | 103–104 LD50 | IC | 100 | 2.5–3 d | neuronal destruction, viremia and high titers in liver | [149] |
| IFNAR−/− mice (A129) | JC280 | 40000, 1000 and 10 PFU | ID | 70–100 | 4–7 d | liver damage, histopathological changes in spleen and lymph nodes | [148] | |
| TOFV | IFNAR−/− mice (A129) | Tok-Hfla-2013 | 10-3–103 FFU | SC | 0, 25 or 100 | 3–6 d | gastrointestinal disorder, 10−3 FFU dose not lethal, 10−2 FFU 25% lethality, higher doses are uniformly lethal | [95] |
| DUGV | Neonatal mice | KT281/75 | 0.3-1522 PFU | IN | 100 | 3–6 d | highest titers in brain | [150] |
| CD-1 mice + cyclophosphamide | KT281/75 | >4.2 × 104 PFU | SC, IN | 0–80 | < 40 d | respiratory and neurological disease ensues in cyclophosphamide treated mice but only after IN challenge. SC challenge is not lethal | [150] | |
| IFNAR−/− mice (A129) | IbAr 1792 | 100-1000 PFU | IC, IP | 100 | 2–5 d | Neurological disease | [151] | |
| CD-1 mice | Ib11480 | 2488 PFU | IN | Not specified | Not specified | neurological disease, did not require immunosuppression | [98] |
© 2019 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Garrison, A.R.; Smith, D.R.; Golden, J.W. Animal Models for Crimean-Congo Hemorrhagic Fever Human Disease. Viruses 2019, 11, 590. https://doi.org/10.3390/v11070590
Garrison AR, Smith DR, Golden JW. Animal Models for Crimean-Congo Hemorrhagic Fever Human Disease. Viruses. 2019; 11(7):590. https://doi.org/10.3390/v11070590
Chicago/Turabian StyleGarrison, Aura R., Darci R. Smith, and Joseph W. Golden. 2019. "Animal Models for Crimean-Congo Hemorrhagic Fever Human Disease" Viruses 11, no. 7: 590. https://doi.org/10.3390/v11070590
APA StyleGarrison, A. R., Smith, D. R., & Golden, J. W. (2019). Animal Models for Crimean-Congo Hemorrhagic Fever Human Disease. Viruses, 11(7), 590. https://doi.org/10.3390/v11070590





