Effect of Gamma Radiation on the Wear Potential of Hybrid Ceramic to Tooth Enamel
Abstract
1. Introduction
2. Materials and Methods
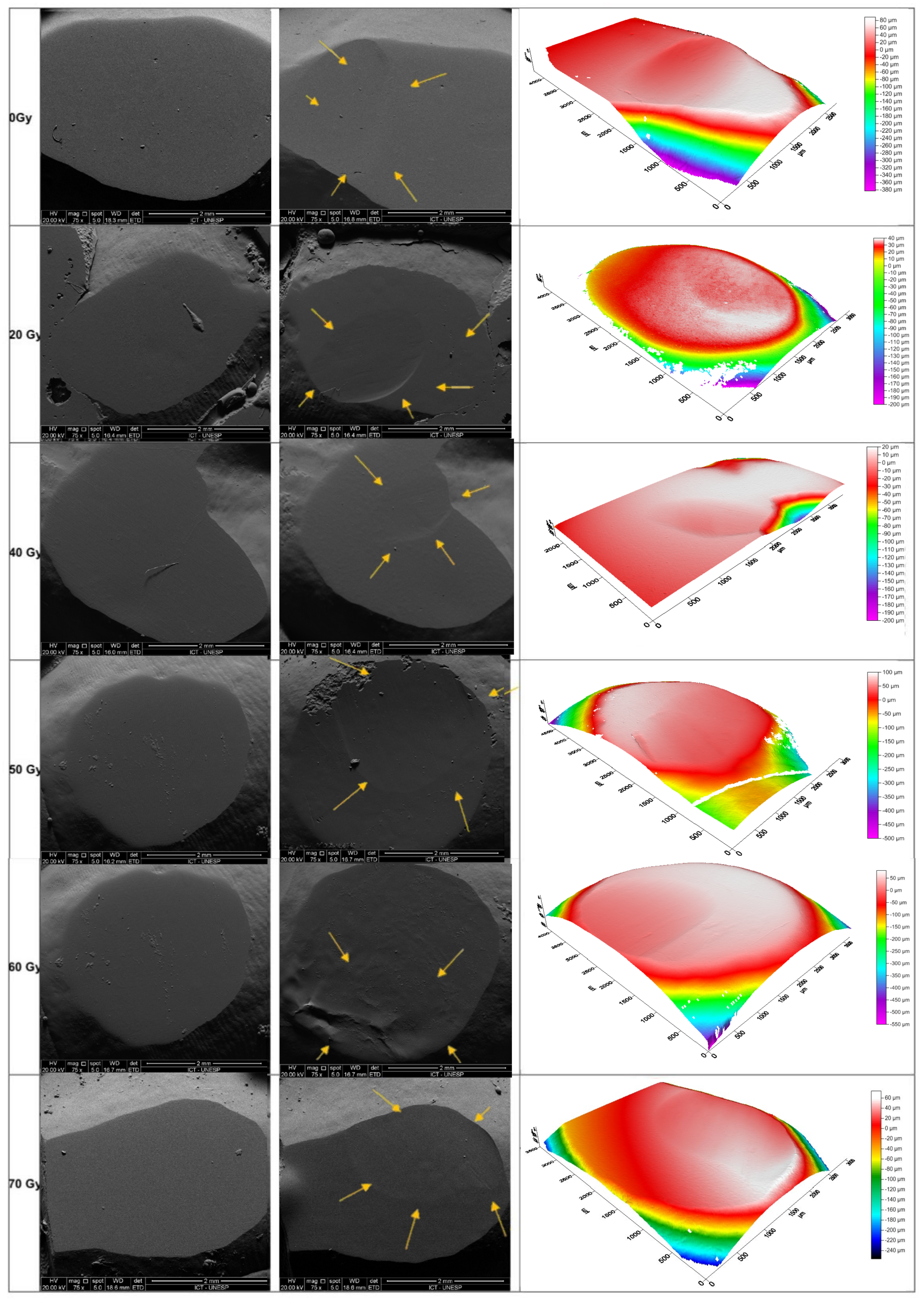
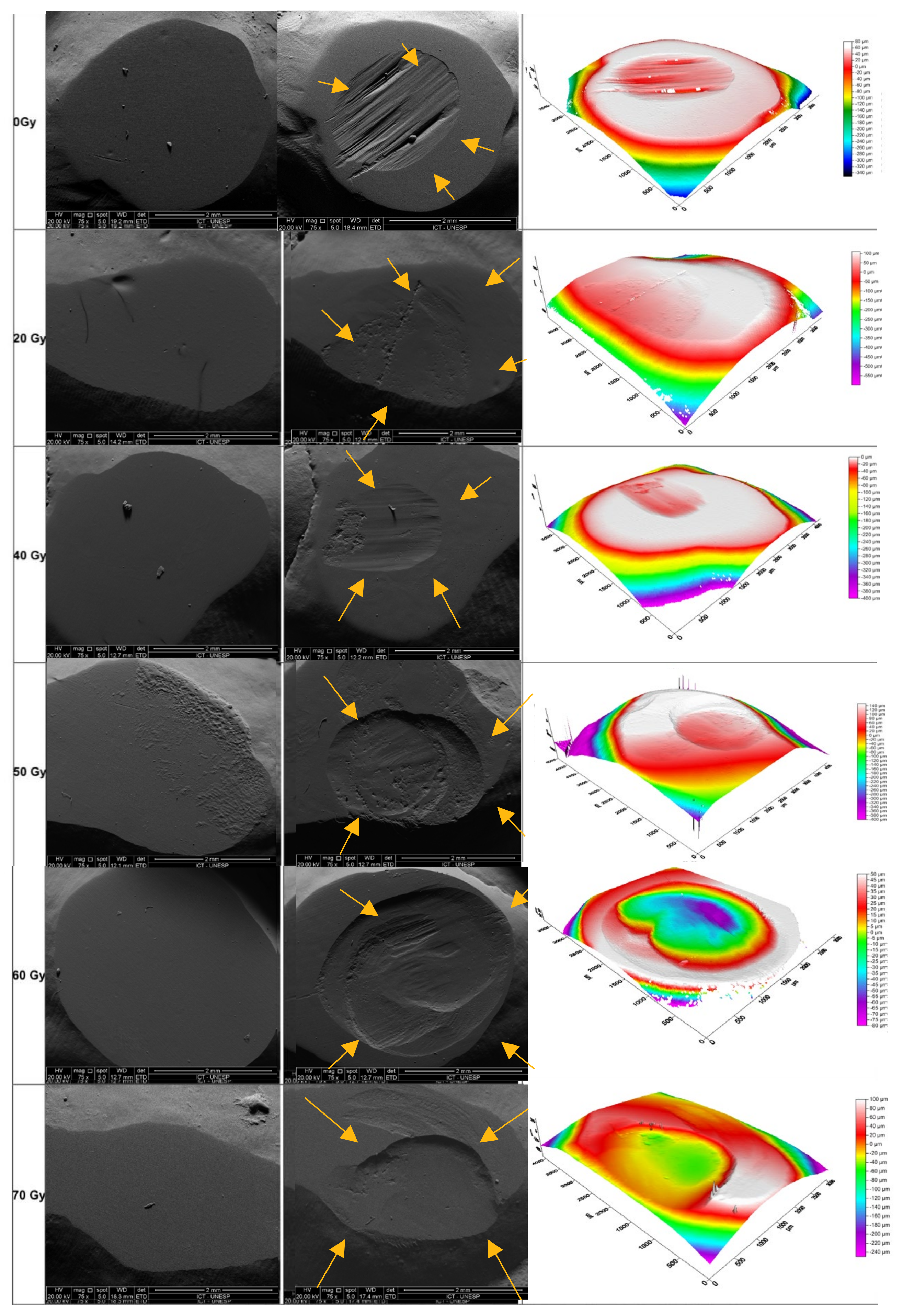
2.1. Chewing Simulation
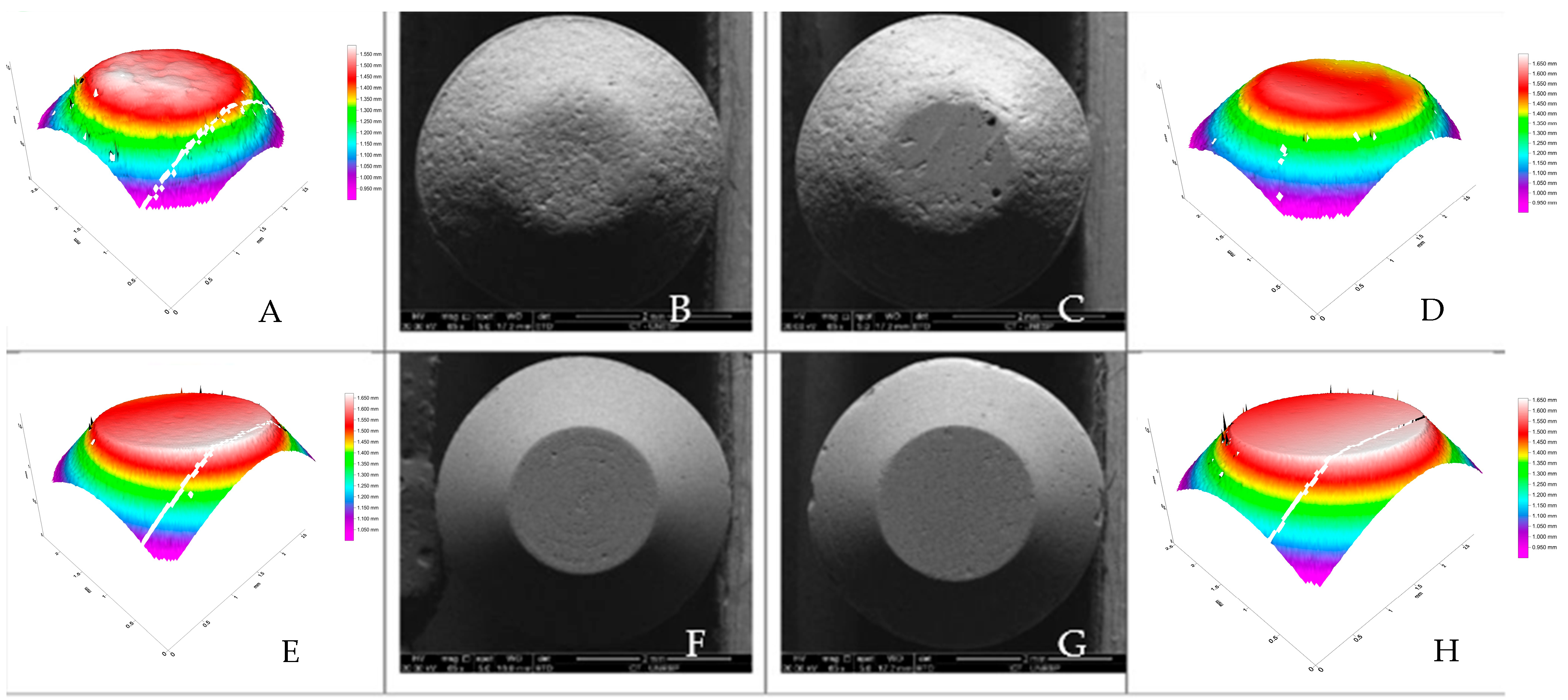
2.2. Optical Profilometry
2.3. Production of Ceramic Discs and Tests
2.4. Biaxial Flexural Strength Test
2.5. Hardness and Elastic Moduli
2.6. FT-IR
2.7. Statistical Analysis
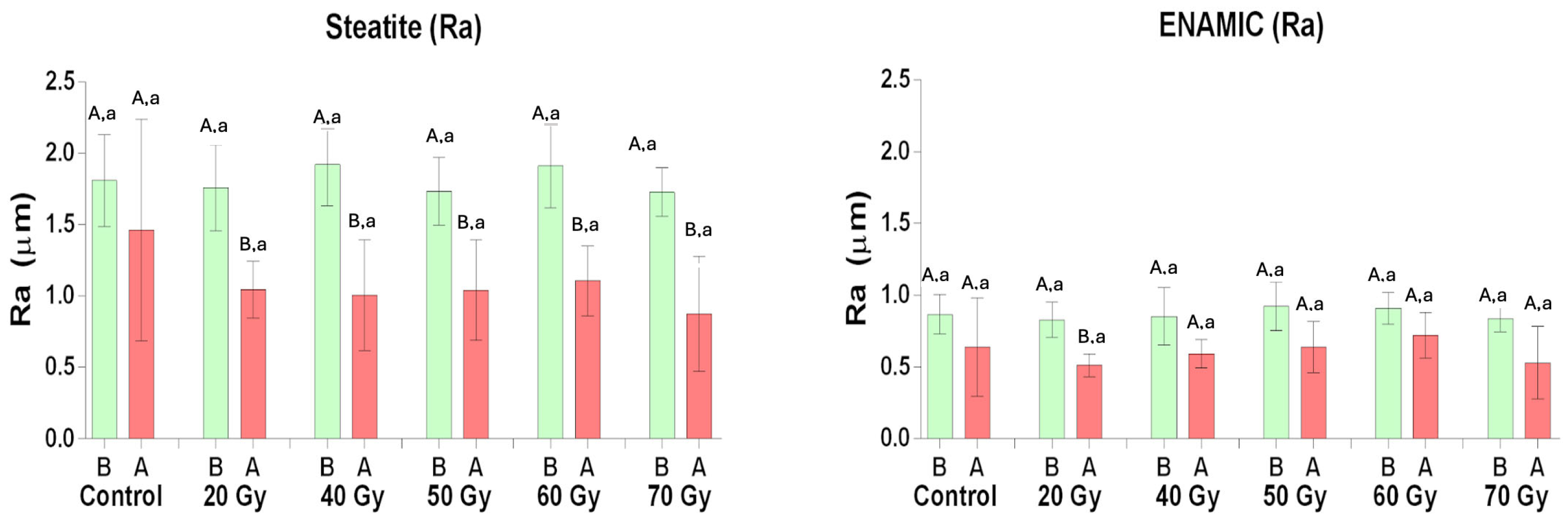
3. Results
4. Discussion
5. Conclusions
- The mechanical and chemical properties of the Enamic remained unchanged after exposure to gamma radiation, even at doses as high as 70 Gy;
- Enamic demonstrated a lower wear resistance and a reduced capacity to wear the antagonist tooth enamel compared to steatite, across various doses of gamma radiation.
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Chin, D.W.; Treister, N.; Friedland, B.; Cormack, R.A.; Tishler, R.B.; Makrigiorgos, G.M.; Court, L.E. Effect of dental restorations and prostheses on radiotherapy dose distribution: A Monte Carlo study. J. Appl. Clin. Med. Phys. 2009, 10, 2853. [Google Scholar] [CrossRef] [PubMed]
- Meldrum, A.; Boatner, L.A.; Ewing, R.C. Size effects in the irradiation-induced crystalline-to-amorphous transformation. Nucl. Instrum. Meth 2003, 207, 28–35. [Google Scholar] [CrossRef]
- Coldea, A.; Swain, M.V.; Thiel, N. Mechanical properties of polymer-infiltrated-ceramic-network materials. Dent. Mater. 2013, 29, 419–426. [Google Scholar] [CrossRef]
- Ramos, N.C.; Campos, T.M.; Paz, I.S.; Machado, J.P.; Bottino, M.A.; Cesar, P.F.; de Melo, R.M. Microstructure characterization and SCG of newly engineerde dental ceramics. Dent. Mater. 2016, 32, 870–878. [Google Scholar] [CrossRef] [PubMed]
- Leung, B.T.; Tsoi, J.K.; Matinlinna, J.P.; Pow, E.H. Comparison of mechanical properties of three machinable ceramics with an experimental fluorophlogopite glass ceramic. J. Prosthet. Dent. 2015, 114, 440–446. [Google Scholar] [CrossRef]
- He, L.H.; Purton, D.; Swain, M. A novel polymer infiltrated ceramic for dental simulation. J. Mater. Sci. Mater. Med. 2011, 22, 1639–1643. [Google Scholar] [CrossRef]
- He, L.H.; Swain, M. A novel polymer infiltrated ceramic dental material. Dent. Mater. 2011, 27, 527–534. [Google Scholar] [CrossRef]
- Lawson, N.C.; Bansal, R.; Burgess, J.O. Wear, strength, modulus and hardness of CAD/CAM restorative materials. Dent. Mater. 2016, 32, e275–e283. [Google Scholar] [CrossRef]
- Mao, Z.; Beuer, F.; Hey, J.; Schmidt, F.; Sorensen, J.A.; Prause, E. Antagonist enamel tooth wear produced by different dental ceramic systems: A systematic review and network meta-analysis of controlled clinical trials. J. Dent. 2024, 142, 104832. [Google Scholar] [CrossRef]
- Zhi, L.; Bortolotto, T.; Krejci, I. Comparative in vitro wear resistance of CAD/CAM composite resin and ceramic materials. J. Prosthet. Dent. 2016, 115, 199–202. [Google Scholar] [CrossRef]
- Xu, Z.; Yu, P.; Arola, D.D.; Min, J.; Gao, S. A comparative study on the wear behavior of a polymer infiltrated ceramic network (PICN) material and tooth enamel. Dent. Mater. 2017, 33, 1351–1361. [Google Scholar] [CrossRef] [PubMed]
- Dejak, B.D.; Langot, C.; Krasowski, M.; Klich, M. Evaluation of Hardness and Wear of Conventional and Transparent Zirconia Ceramics, Feldspathic Ceramic, Glaze, and Enamel. Materials 2024, 17, 3518. [Google Scholar] [CrossRef] [PubMed]
- Della Bona, A.; Corazza, P.H.; Zhang, Y. Characterization of a polymer-infiltrated ceramic-network material. Dent. Mater. 2014, 30, 564–569. [Google Scholar] [CrossRef] [PubMed]
- Tu, Y.; Hao, L.; Ding, Y.; Zhong, Y.; Hua, C.; Jiang, L. The influence of different radiotherapy doses on the mechanical properties and microstructure of the enamel and dentin of human premolar teeth. Strahlenther. Onkol. 2024, 200, 1047–1056. [Google Scholar] [CrossRef] [PubMed]
- Qing, P.; Huang, S.; Gao, S.S.; Qian, L.M.; Yu, H.Y. Effect of gamma irradiation on the wear behavior of human tooth enamel. Sci. Rep. 2015, 5, 11568. [Google Scholar] [CrossRef]
- de Barros da Cunha, S.R.; Fonseca, F.P.; Ramos, P.A.M.M.; Haddad, C.M.K.; Fregnani, E.R.; Aranha, A.C.C. Effects of different radiation doses on the microhardness, superficial morphology, and mineral components of human enamel. Arch. Oral. Biol. 2017, 80, 130–135. [Google Scholar] [CrossRef]
- Pioch, T.; Golfels, D.; Staehle, H.J. An experimental study of the stability of irradiated teeth in the region of the dentinoenamel junction. Endod. Dent. Traumatol. 1992, 8, 241–244. [Google Scholar] [CrossRef]
- Soares, C.J.; Castro, C.G.; Neiva, N.A.; Soares, P.V.; Santos-Filho, P.C.; Naves, L.Z.; Pereira, P.N.R. Effect of gamma irradiation on ultimate tensile strength of enamel and dentin. J. Dent. Res. 2010, 89, 159–164. [Google Scholar] [CrossRef]
- Bozan, P.Ö.; Kavak, A.; Aslan, M.; Çanakçi, H.; Demiryürek, A. Effects of ionizing radiation on mechanical proprieties of restorative materials and enamel in upper molars: An in-vitro study. J. Stoma 2023, 76, 31–36. [Google Scholar] [CrossRef]
- Kudkuli, J.; Agrawal, A.; Gurjar, O.P.; Sharma, S.D.; Rekha, P.D.; Manzoor, M.A.P.; Singh, B.; Rao, B.S.; Abdulla, R. Demineralization of tooth enamel following radiation therapy; An in vitro microstructure and microhardness analysis. J. Cancer Res. Ther. 2020, 16, 612–618. [Google Scholar] [CrossRef]
- Miranda, R.R.; Ribeiro, T.E.; Silva, E.L.C.D.; Simamoto Júnior, P.C.; Soares, C.J.; Novais, V.R. Effects of fractionation and ionizing radiation dose on the chemical composition and microhardness of enamel. Arch. Oral. Biol. 2021, 121, 104959. [Google Scholar] [CrossRef] [PubMed]
- Muñoz, M.A.; Garín-Correa, C.; González-Arriagada, W.; Quintela Davila, X.; Häberle, P.; Bedran-Russo, A.; Luque-Martínez, I. The adverse effects of radiotherapy on the structure of dental hard tissues and longevity of dental restoration. Int. J. Radiat. Biol. 2020, 96, 910–918. [Google Scholar] [CrossRef] [PubMed]
- Duruk, G.; Acar, B.; Temelli, Ö. Effect of different doses of radiation on morphogical, mechanical and chemical properties of primary and permanent teeth-an in vitro study. BMC Oral. Health 2020, 20, 242. [Google Scholar] [CrossRef] [PubMed]
- Mörmann, W.H.; Stawarczyk, B.; Ender, A.; Sener, B.; Attin, T.; Mehl, A. Wear characteristics of current aesthetic dental restorative CAD/CAM materials: Two-body wear, gloss retention, roughness and Martens hardness. J. Mech. Behav. Biomed. Mater. 2013, 20, 113–125. [Google Scholar] [CrossRef]
- ISO 6872; Dentistry—Guidance on Color Measurement. ISO: Geneva, Switzerland, 2015.
- Tikku, A.P.; Bhatt, M.L.; Painuly, N.K.; Bharti, R.; Bains, R.; Misra, S. Shear bond strength analysis and marginal gap evaluation of restoration–tooth interface of aesthetic restorations after simulated Co-60 gamma irradiation. J. Radiot Prac. 2023, 22, e13. [Google Scholar]
- Cruz, A.D.; Sinhoreti, M.A.; Ambrosano, G.M.; Rastelli, A.N.; Bagnato, V.S.; Boscolo, F.N. Effect of therapeutic dose X rays on mechanical and chemical properties of esthetic dental materials. J. Mater. Res. 2008, 11, 313–318. [Google Scholar]
- Papynov, E.K.; Shichalin, O.O.; Apansevich, V.I.; Nikiforova, N.O.; Belov, A.A.; Buravlev, I.Y.; Azon, S.A.; Buravleva, A.A.; Gnilyak, E.A.; Pankratov, I.V.; et al. Production of X-ray absorbing ceramics and products based on them for radiotherapy of the periorbital eye region. Ceram. Inter. 2024, 50, 41581–41589. [Google Scholar]
- Eggmann, F.; Hwang, J.D.; Ayub, J.M.; Mante, F.K. Impact of Irradiation on the Adhesive Performance of Resin-Based Dental Biomaterials: A Systematic Review of Laboratory Studies. Materials 2023, 16, 2580. [Google Scholar] [CrossRef]
- Preis, V.; Grumser, K.; Schneider-Feyrer, S.; Behr, M.; Rosentritt, M. Cycle-dependent in vitro wear performance of dental ceramics after clinical surface treatments. J. Mech. Behav. Biomed. Mater. 2016, 53, 49–58. [Google Scholar] [CrossRef]
- Stawarczyk, B.; Liebermann, A.; Eichberger, M.; Güth, J.F. Evaluation of mechanical and optical behavior of current esthetic dental restorative CAD/CAM composites. J. Mech. Behav. Biomed. Mater. 2015, 55, 1–11. [Google Scholar] [CrossRef]
- Choi, J.W.; Song, E.J.; Shin, J.H.; Jeong, T.S.; Huh, J.B. In Vitro Investigation of Wear of CAD/CAM Polymeric Materials Against Primary Teeth. Materials 2017, 10, 1410. [Google Scholar] [CrossRef] [PubMed]
- Ludovichetti, F.S.; Trindade, F.Z.; Werner, A.; Kleverlaan, C.J.; Fonseca, R.G. Wear resistance and abrasiveness of CAD-CAM monolithic materials. J. Prosthet. Dent. 2018, 120, 318.e1–318.e8. [Google Scholar] [CrossRef] [PubMed]
- Zurek, A.D.; Alfaro, M.F.; Wee, A.G.; Yuan, J.C.; Barao, V.A.; Mathew, M.T.; Sukotjo, C. Wear Characteristics and Volume Loss of CAD/CAM Ceramic Materials. J. Prosthodont. 2018, 6, e510–e518. [Google Scholar]
- Bottino, M.A.; Campos, F.; Ramos, N.C.; Rippe, M.P.; Valandro, L.F.; Melo, R.M. Inlays made from a hybrid material: Adaptation and bond strengths. Oper. Dent. 2015, 40, E83–E91. [Google Scholar]
- Pells, G. Radiation Effects in Ceramics. MRS Bull. 1997, 22, 22–28. [Google Scholar] [CrossRef]
- Dietrich, A.; Heimann, R.B.; Willmann, G. The colour of medical-grade zirconia (Y-TZP). J. Mater. Sci. Mater. Med. 1996, 7, 559–565. [Google Scholar]
- Hobbs, L.W.; Clinard, F.W., Jr.; Zinkle, S.J.; Ewing, R.C. Radiation effects in ceramics. J. Nucl. Mater. 1994, 216, 291–321. [Google Scholar] [CrossRef]
- Catelan, A.; Padilha, A.C.; Salzedas, L.M.; Coclete, G.A.; Santos, P.H. Effect of radiotherapy on the radiopacity and flexural strength of a composite resin. Acta Odontol. Latinoam. 2008, 21, 159–162. [Google Scholar]
- Von Fraunhofer, J.A.; Curtis, P., Jr.; Sharma, S.; Farman, A.G. The effects of gamma radiation on the properties of composite restorative resins. J. Dent. 1989, 17, 177–183. [Google Scholar] [CrossRef]
- Zhu, X.; Xie, Y.; Wang, X. Effect of crystallite size and microstrain on X-ray diffraction peak broadening in polycrystalline materials. J. Mater. Sci. 2010, 45, 573–579. [Google Scholar]
| Material | Radiation | Mean/Standard Deviation |
|---|---|---|
| Enamic | 70 Gy | 0.08 ± 0.03 C |
| 60 Gy | 0.06 ± 0.04 C | |
| 50 Gy | 0.05 ± 0.03 C | |
| 40 Gy | 0.04 ± 0.01 C | |
| 20 Gy | 0.05 ± 0.01 C | |
| 0 Gy | 0.05 ± 0.02 C | |
| Steatite | 70 Gy | 0.77 ± 0.24 A |
| 60 Gy | 0.74 ± 0.51 A | |
| 50 Gy | 0.41 ± 0.23 B | |
| 40 Gy | 0.25 ± 0.06 BC | |
| 20 Gy | 0.23 ± 0.17 BC | |
| 0 Gy | 0.23 ± 0.14 BC |
| Material | Mean/Standard Deviation |
|---|---|
| Enamic | 0.36 ± 0.19 A |
| Steatite | 0.04 ± 0.02 B |
| Material | Baseline Roughness | Upon Chewing Roughness | Nano Hardness | Modulus of Elasticity |
|---|---|---|---|---|
| Enamic Steatite | 0.8 ± 0.1 A 1.8 ± 0.2 B | 0.3 ± 0.2 A 0.7 ± 0.3 B | 413.7 ± 125.7 913.5 ± 96.4 | 37.049 ± 4.3 95.61 ± 15.5 |
| Dose | Flexural Strength (MPa) | Hardness (VHN) |
|---|---|---|
| Control (0 Gy) | 108.82 ± 12.68 A | 413.73 ± 125.70 A |
| 20 Gy | 107.90 ± 10.65 A | 408.04 ± 134.62 A |
| 40 Gy | 104.81 ± 11.76 A | 426.85 ± 122.54 A |
| 70 Gy | 102.43 ± 14.92 A | 417.51 ± 191.45 A |
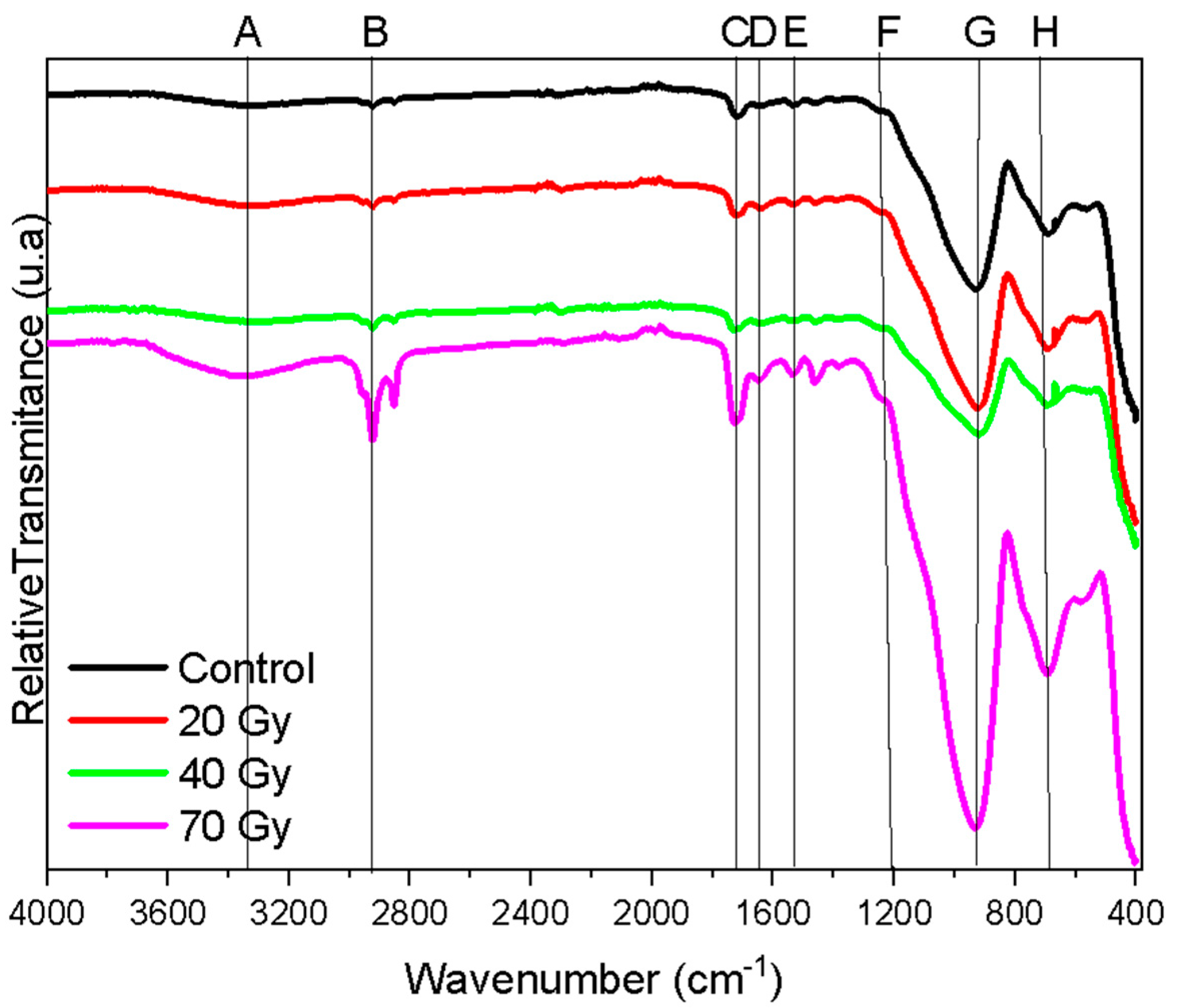
| Frequencies (cm−1) | Assignment | Band Set | Reference |
|---|---|---|---|
| ≈3432 | NH/-OH | A | Ramos et al., 2016 [4] |
| ≈2912 | C-H | B | Ramos et al., 2016 [4] |
| 1730 | C=O | C | Ramos et al., 2016 [4] |
| 1617 | C=O | D | Ramos et al., 2016 [4] |
| 1530 | Amide | E | Ramos et al., 2016 [4] |
| 1070 | Si-O-Si/Si-O-Al | F | Ramos et al., 2016 [4] |
| 1058 | Si-O-Si/Si-O-Al | G | Ramos et al., 2016 [4] |
| 792 | Al-O | H | Ramos et al., 2016 [4] |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
da Silva, P.N.F.; Costa, F.C.; Silva, C.d.S.; Barcellos, M.C.; Manea, S.; Gonçalez, O.L.; Jardim, V.R.; Martins, G.V.; Lima, N.; Found, A.A.; et al. Effect of Gamma Radiation on the Wear Potential of Hybrid Ceramic to Tooth Enamel. Materials 2025, 18, 702. https://doi.org/10.3390/ma18030702
da Silva PNF, Costa FC, Silva CdS, Barcellos MC, Manea S, Gonçalez OL, Jardim VR, Martins GV, Lima N, Found AA, et al. Effect of Gamma Radiation on the Wear Potential of Hybrid Ceramic to Tooth Enamel. Materials. 2025; 18(3):702. https://doi.org/10.3390/ma18030702
Chicago/Turabian Styleda Silva, Pollyanna Nogueira Ferreira, Fernanda Calvo Costa, Célio dos Santos Silva, Maria Carolina Barcellos, Sílvio Manea, Odair Lellis Gonçalez, Vitor Ribeiro Jardim, Gislene Valdete Martins, Nelson Lima, Anelyse Arata Found, and et al. 2025. "Effect of Gamma Radiation on the Wear Potential of Hybrid Ceramic to Tooth Enamel" Materials 18, no. 3: 702. https://doi.org/10.3390/ma18030702
APA Styleda Silva, P. N. F., Costa, F. C., Silva, C. d. S., Barcellos, M. C., Manea, S., Gonçalez, O. L., Jardim, V. R., Martins, G. V., Lima, N., Found, A. A., De Souza, G. M., & Tango, R. N. (2025). Effect of Gamma Radiation on the Wear Potential of Hybrid Ceramic to Tooth Enamel. Materials, 18(3), 702. https://doi.org/10.3390/ma18030702






