Biofilm on Toothbrushes of Children with Cystic Fibrosis: A Potential Source of Lung Re-Infection after Antibiotic Treatment?
Abstract
:1. Introduction
2. Materials and Methods
2.1. Bacterial Species Identification from Sputum Samples
2.2. Toothbrush Collection and Sample Processing
2.3. Biofilm Bacterial Culture and Identification
2.4. Confocal Laser Scanning Microscopy
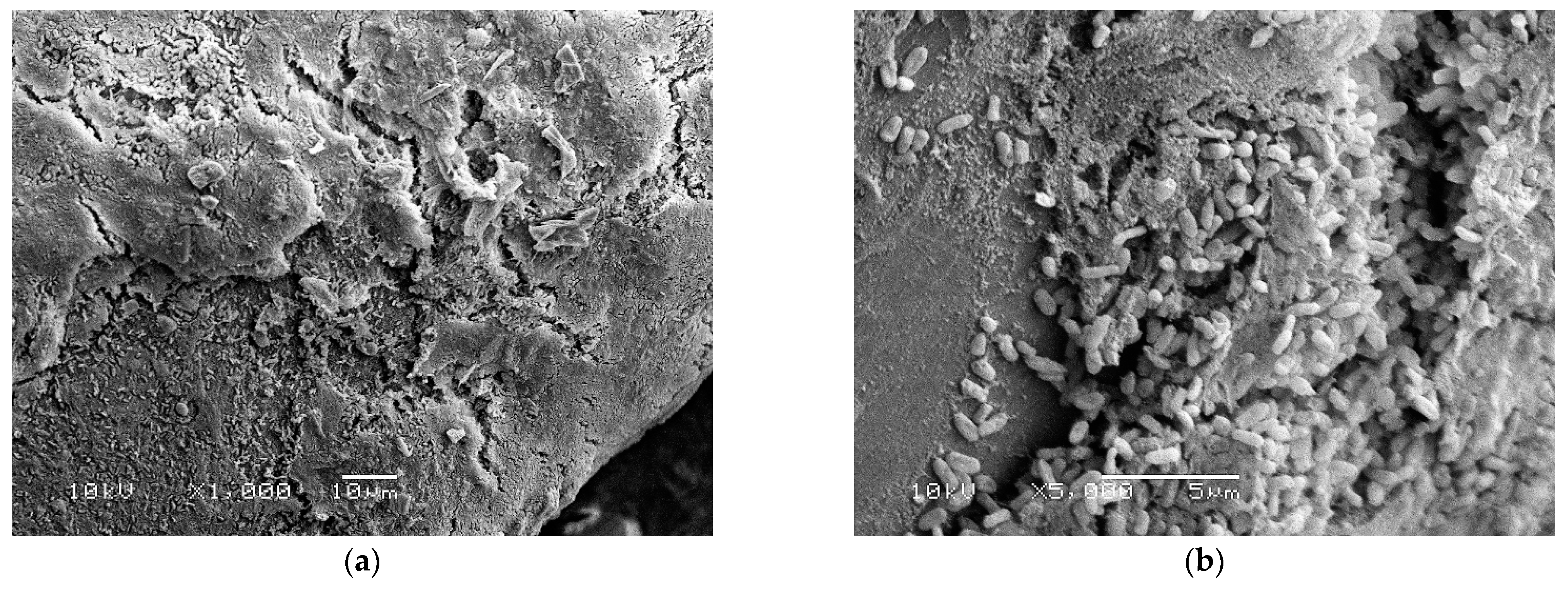
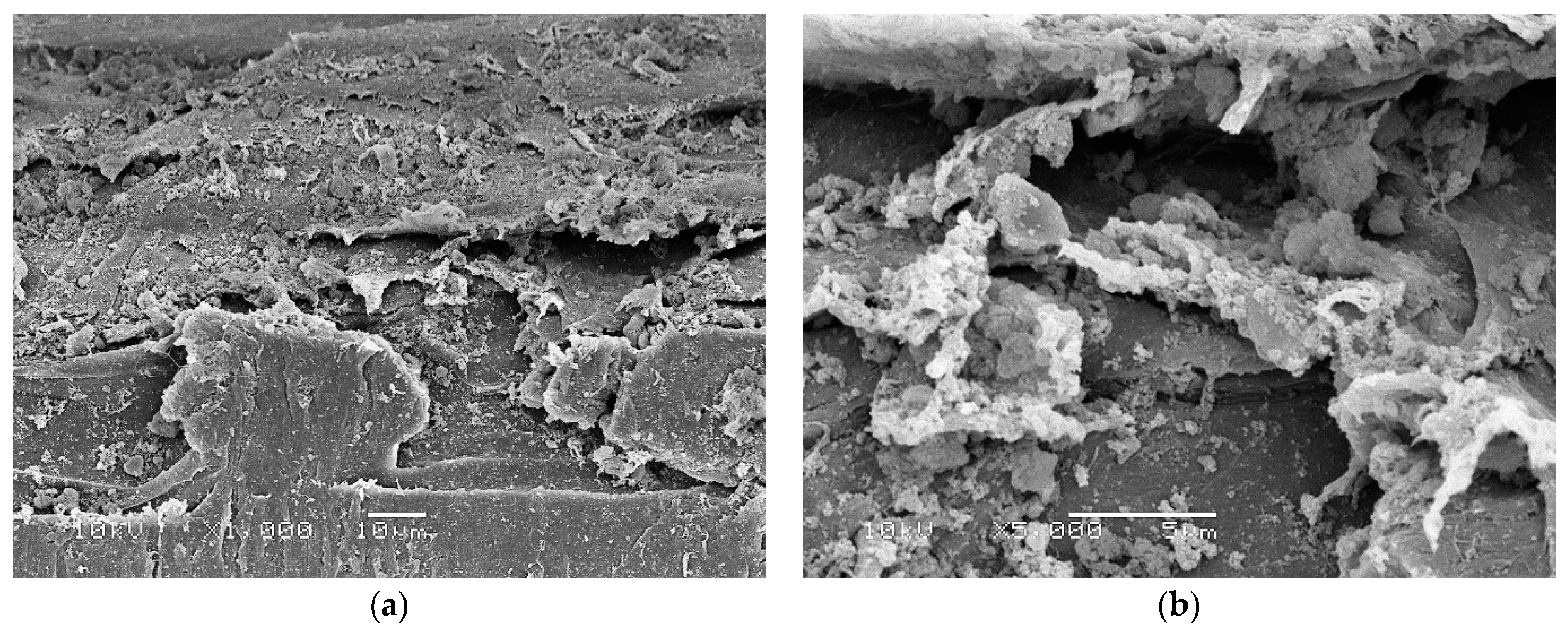
2.5. Scanning Electron Microscopy
2.6. Statistical Analysis
3. Results
3.1. Bacterial Species from Sputum Samples
3.2. Bacterial Number and Species from Toothbrushes
3.3. Confocal Laser Scanning Microscopy
3.4. Scanning Electron Microscopy
4. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Cantin, A.M.; Hartl, D.; Konstan, M.W.; Chmiel, J.F. Inflammation in cystic fibrosis lung disease: Pathogenesis and therapy. J. Cyst. Fibros. 2015, 14, 419–430. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ranganathan, S.C.; Hall, G.L.; Sly, P.D.; Stick, S.M.; Douglas, T.A.; Australian Respiratory Early Surveillance Team for Cystic Fibrosis (AREST-CF). Early Lung Disease in Infants and Preschool Children with Cystic Fibrosis. What Have We Learned and What Should We Do about It? Am. J. Respir. Crit. Care Med. 2017, 195, 1567–1575. [Google Scholar] [CrossRef] [PubMed]
- Harrison, F. Microbial ecology of the cystic fibrosis lung. Microbiology 2007, 153, 917–923. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lyczak, J.B.; Cannon, C.L.; Pier, G.B. Lung infections associated with cystic fibrosis. Clin. Microbiol. Rev. 2002, 15, 194–222. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Murray, T.S.; Egan, M.; Kazmierczak, B.I. Pseudomonas aeruginosa chronic colonization in cystic fibrosis patients. Curr. Opin. Pediatr. 2007, 19, 83–88. [Google Scholar] [CrossRef] [PubMed]
- Mah, T.F. Biofilm-specific antibiotic resistance. Future Microbiol. 2012, 7, 1061–1072. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Schelstraete, P.; De Boeck, K.; Proesmans, M.; Lebecque, P.; Leclercq-Foucart, J.; Malfroot, A.; Vaneechoutte, M.; De Baets, F. Pseudomonas aeruginosa in the home environment of newly infected cystic fibrosis patients. Eur. Respir. J. 2008, 31, 822–829. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hu, H.; Harmer, C.; Anuj, S.; Wainwright, C.E.; Manos, J.; Cheney, J.; Harbour, C.; Zablotska, I.; Turnbull, L.; Whitchurch, C.B.; et al. Type 3 secretion system effector genotype and secretion phenotype of longitudinally collected Pseudomonas aeruginosa isolates from young children diagnosed with cystic fibrosis following newborn screening. Clin. Microbiol. Infect. 2013, 19, 266–272. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Passarelli, M.R.; Sandri, A.; Boaretti, M.; Grilli, A.; Volpi, S.; Melotti, P.; Burlacchini, G.; Lleò, M.M.; Signoretto, C. Toothbrushes may convey bacteria to the cystic fibrosis lower airways. J. Oral Microbiol. 2019, 11, 1647036. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kidd, T.J.; Ramsay, K.A.; Hu, H.; Bye, P.T.; Elkins, M.R.; Grimwood, K.; Harbour, C.; Marks, G.B.; Nissen, M.D.; Robinson, P.J.; et al. Low rates of Pseudomonas aeruginosa misidentification in isolates from cystic fibrosis patients. J. Clin. Microbiol. 2009, 47, 1503–1509. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Genevois, A.; Roques, C.; Segonds, C.; Cavalié, L.; Brémont, F.; Maubisson, L.; Mas, E.; Mittaine, M. Bacterial colonization status of cystic fibrosis children’s toothbrushes: A pilot study. Arch. Pédiatrie 2015, 22, 1240–1246. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Pittman, J.E.; Calloway, E.H.; Kiser, M.; Yeatts, J.; Davis, S.D.; Drumm, M.L.; Schechter, M.S.; Leigh, M.W.; Emond, M.; Van Rie, A.; et al. Age of Pseudomonas aeruginosa acquisition and subsequent severity of cystic fibrosis lung disease. Pediatr. Pulmonol. 2011, 46, 497–504. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Netuschil, L.; Auschill, T.M.; Sculean, A.; Arweiler, N.B. Confusion over live/dead stainings for the detection of vital microorganisms in oral biofilms—Which stain is suitable? BMC Oral Health 2014, 14, 2. [Google Scholar] [CrossRef] [PubMed] [Green Version]

| Child ID | Bacterial Species in Sputum Sample | Toothbrush Collection Point | P. aeruginosa Number | S. aureus Number | Bacteria Species in Toothbrush Sample |
|---|---|---|---|---|---|
| 1 | P. aeruginosa | Before antibiotic treatment | 4.87 × 105 ± 4.03 × 104 | 0 | P. aeruginosa Streptococcus mitis Enterobacter cloacae |
| 2 | S. aureus P. aeruginosa | Before antibiotic treatment | 2.76 × 105 ± 3.96 × 104 | 3.85 × 104 ± 2.33 × 103 | P. aeruginosa S. aureus Klebsiella oxytoca |
| 3 | P. aeruginosa Haemophilus influenzae | Two weeks from starting antibiotic treatment | 2.33 × 103 ± 4.61 × 102 | 0 | P. aeruginosa Micrococcus luteus Brachybacterium spp. |
| 4 | P. aeruginosa | Three weeks from starting antibiotic treatment | 3.64 × 103 ± 5.07 × 102 | 0 | P. aeruginosa S. epidermidis S. hominis Enterobacter cloacae Enterococcus faecium |
| 5 | S. aureus P. aeruginosa | Three months after antibiotic treatment | 0 | 0 | Kocuria spp. Streptococcus mutans |
| 6 | Stenotrophomonas maltophilia | Seven months after antibiotic treatment | 0 | 0 | Streptococcus sanguinis |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Hu, H.; Clothier, N.; Jacombs, A.; Mckay, K.; Deva, A.K.; Vickery, K. Biofilm on Toothbrushes of Children with Cystic Fibrosis: A Potential Source of Lung Re-Infection after Antibiotic Treatment? Materials 2022, 15, 2139. https://doi.org/10.3390/ma15062139
Hu H, Clothier N, Jacombs A, Mckay K, Deva AK, Vickery K. Biofilm on Toothbrushes of Children with Cystic Fibrosis: A Potential Source of Lung Re-Infection after Antibiotic Treatment? Materials. 2022; 15(6):2139. https://doi.org/10.3390/ma15062139
Chicago/Turabian StyleHu, Honghua, Nicole Clothier, Anita Jacombs, Karen Mckay, Anand K. Deva, and Karen Vickery. 2022. "Biofilm on Toothbrushes of Children with Cystic Fibrosis: A Potential Source of Lung Re-Infection after Antibiotic Treatment?" Materials 15, no. 6: 2139. https://doi.org/10.3390/ma15062139
APA StyleHu, H., Clothier, N., Jacombs, A., Mckay, K., Deva, A. K., & Vickery, K. (2022). Biofilm on Toothbrushes of Children with Cystic Fibrosis: A Potential Source of Lung Re-Infection after Antibiotic Treatment? Materials, 15(6), 2139. https://doi.org/10.3390/ma15062139








