Review on Polymer, Ceramic and Composite Materials for CAD/CAM Indirect Restorations in Dentistry—Application, Mechanical Characteristics and Comparison
Abstract
1. Introduction
2. Materials and Methods
3. Historical Outlook on CAD/CAM
4. Advantages of CAD/CAM
5. Limitations and Handling of the System
6. Currently Used Dental CAD/CAM Systems
7. Computer-Aided Design
8. Materials for CAD/CAM
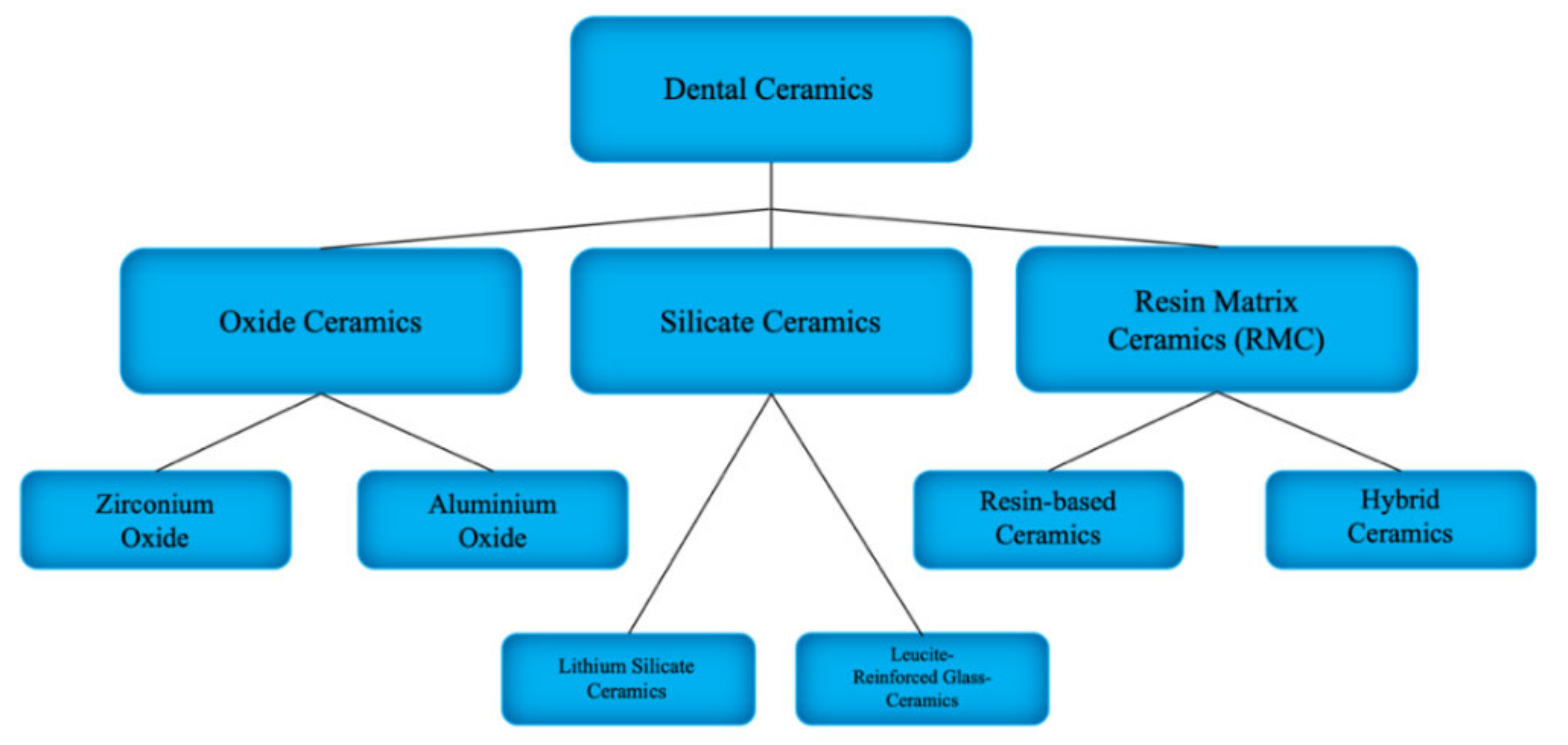
8.1. Dental Ceramics
8.1.1. Resin Matrix Ceramics
8.1.2. Silicate Ceramics
8.1.3. Leucite-Reinforced Glass Ceramics
8.1.4. Lithium Silicate Ceramics
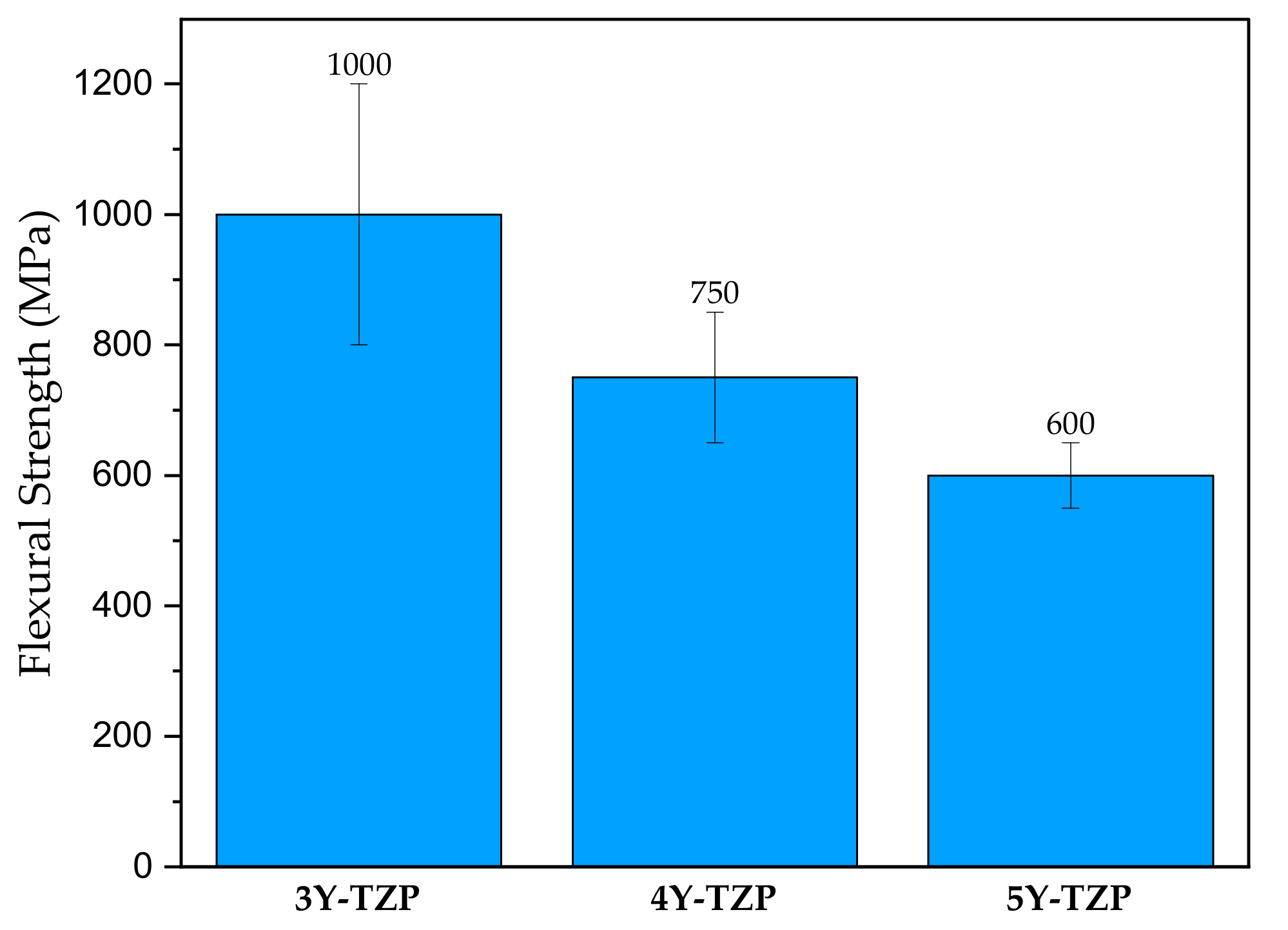
8.1.5. Oxide Ceramics
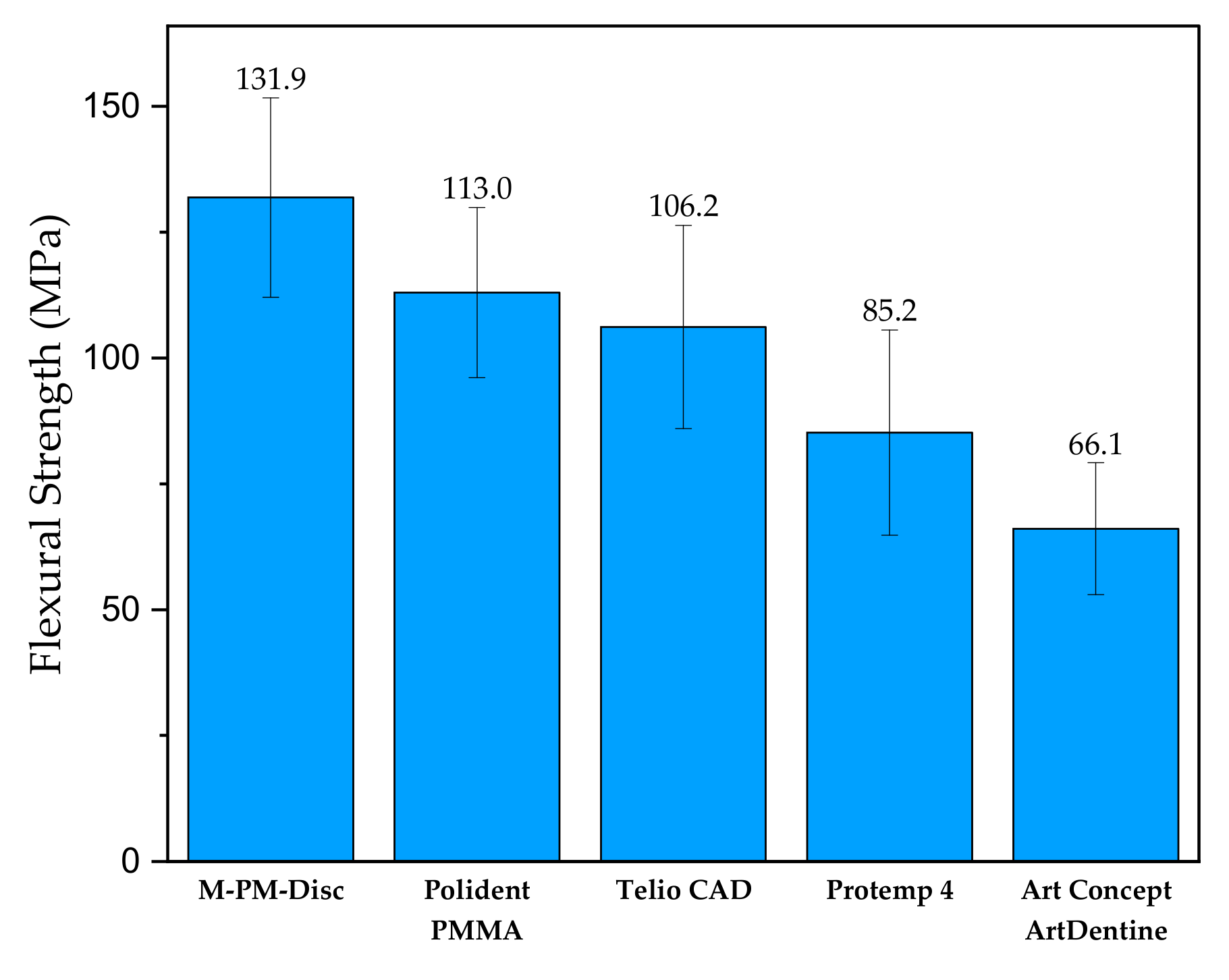
8.2. Polymer-Based Materials
8.3. Composites
9. Nanoscale Aspect of CAD/CAM Materials
10. Comparison of CAD/CAM Materials
| Material Type | Product, Manufacturer | Flexural Strength (MPa) | Hardness (HV) | Elastic Modulus (GPa) | Composition | References |
|---|---|---|---|---|---|---|
| Composites | VITA CAD-Temp, Vita Zahnfabrik | 80 | n/a | 2.8 | Acrylate polymer with microparticle filler | [44,95] |
| Aluminium oxide ceramics | VITA In-Ceram ALUMINA, Vita Zahnfabrik | 419 | 2035 | 410 | Al2O3 (82 wt.%), La2O3 (12 wt.%), SiO2 (4.5 wt.%), CaO (0.8 wt.%), other oxides (0.7 wt.%) | [96] |
| Zirconium oxide ceramics | IPS e.max zirCAD, Ivoclar Vivadent | 1200 | n/a | 206.3 | 3 mol% Yttria-stabilized tetragonal zirconia polycrystals (3Y-TZP) | [93,97] |
| Lithium silicate ceramics | IPS e.max CAD, Ivoclar Vivadent | 353.1 | 617 | 102.7 | SiO2, Li2O, K2O, P2O5, SiO2, ZnO | [85,91,98,99] |
| Leucite-Reinforced Glass Ceramics | IPS Empress CAD, Ivoclar Vivadent | 160 | 632.2 | 62 | SiO2 (60–65 wt.%), Al2O3 (16–20 wt.%) K2O (10–14 wt.%) Na2O (3.5–6.5 wt.%), other oxides (0.5 wt.%), pigments | [100] |
| Resin-based ceramics | Lava Ultimate, 3M | 200 | 96 | 12 | Polymerizable resin, dispersed nanometric colloidal silica, ZrO2 spherical particles | [48,85,93,101] |
| PMMA | Polident PMMA, Polident | 114 | 26 | 2.77 | PMMA, pigment | [102] |
| Hybrid cermics | VITA ENAMIC, Vita Zahnfabrik | 150–160 | 200 | 30 | SiO2, Al2O3, Na2O, K2O, B2O3, ZrO2, CaO, urethane dimethylacrylate, triethylene glycol dimethylacrylate | [50,85] |
| PEEK | PEEK-OPTIMA™, Invibio | 165 | n/a | 3.70 | PEEK | [103,104,105] |
11. Adhesion–Bonding of CAD/CAM Restoration
12. User Experience of CAD/CAM Hybrid Materials
13. Surface Finishing and Disguise of CAD/CAM Restorations.
14. Biocompatibility and Cytotoxicity of CAD/CAM Materials
15. Current Demand for the CAD/CAM Restorations
16. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Boboulos, M.A. CAD-CAM & Rapid Prototyping Application Evaluation; Bookboon: London, UK, 2010; ISBN 9788776816766. [Google Scholar]
- Davidowitz, G.; Kotick, P.G. The Use of CAD/CAM in Dentistry. Dent. Clin. N. Am. 2011, 55, 559–570. [Google Scholar] [CrossRef]
- Okoński, P.; Lasek, K.; Mierzwińska-Nastalska, E. Kliniczne zastosowanie wybranych materiałów ceramicznych. Protet. Stomatol. 2012, 62, 181–189. [Google Scholar]
- Duret, F.; Blouin, J.L.; Duret, B. CAD-CAM in dentistry. J. Am. Dent. Assoc. 1988, 117, 715–720. [Google Scholar] [CrossRef]
- Fasbinder, D.J. Materials for chairside CAD/CAM restorations. Compend. Contin. Educ. Dent. 2010, 31, 702–710. [Google Scholar] [PubMed]
- Mörmann, W.H. The evolution of the CEREC system. J. Am. Dent. Assoc. 2006, 137, 7–13. [Google Scholar] [CrossRef]
- Rekow, D. Computer-aided design and manufacturing in dentistry: A review of the state of the art. J. Prosthet. Dent. 1987, 58, 512–516. [Google Scholar] [CrossRef]
- Zaruba, M.; Mehl, A. Chairside systems: A current review Chairside-Systeme: Eine aktuelle Übersicht. Int. J. Comput. Dent. 2017, 20, 123–149. [Google Scholar]
- Joda, T.; Brägger, U. Patient-centered outcomes comparing digital and conventional implant impression procedures: A randomized crossover trial. Clin. Oral Implant. Res. 2016, 27, e185–e189. [Google Scholar] [CrossRef] [PubMed]
- Gjelvold, B.; Chrcanovic, B.R.; Korduner, E.K.; Collin-Bagewitz, I.; Kisch, J. Intraoral Digital Impression Technique Compared to Conventional Impression Technique. A Randomized Clinical Trial. J. Prosthodont. 2016, 25, 282–287. [Google Scholar] [CrossRef]
- Yuzbasioglu, E.; Kurt, H.; Turunc, R.; Bilir, H. Comparison of digital and conventional impression techniques: Evaluation of patients’ perception, treatment comfort, effectiveness and clinical outcomes. BMC Oral Health 2014, 14, 1–7. [Google Scholar] [CrossRef]
- Giordano, R. Materials for chairside CAD/CAM-produced restorations. J. Am. Dent. Assoc. 2006, 137, 14S–21S. [Google Scholar] [CrossRef]
- Li, R.W.K.; Chow, T.W.; Matinlinna, J.P. Ceramic dental biomaterials and CAD/CAM technology: State of the art. J. Prosthodont. Res. 2014, 58, 208–216. [Google Scholar] [CrossRef] [PubMed]
- Papadiochou, S.; Pissiotis, A.L. Marginal adaptation and CAD-CAM technology: A systematic review of restorative material and fabrication techniques. J. Prosthet. Dent. 2018, 119, 545–551. [Google Scholar] [CrossRef] [PubMed]
- Abdullah, A.O.; Pollington, S.; Liu, Y. Comparison between direct chairside and digitally fabricated temporary crowns. Dent. Mater. J. 2018, 37, 957–963. [Google Scholar] [CrossRef]
- Ahmed, K.E. We’re Going Digital: The Current State of CAD/CAM Dentistry in Prosthodontics. Prim. Dent. J. 2018, 7, 30–35. [Google Scholar] [CrossRef] [PubMed]
- Kuźniar-Folwarczny, A.; Sulewski, M.; Błaszczyk, A.; Sulewska, A.; Kosior, P.; Dobrzyński, M. Charakterystyka ceramicznych materiałów stomatologicznych stosowanych w gabinetowych systemach CAD/CAM, 2019, 8, 479–487. Inż. Fiz. Med. 2019, 8, 479–487. [Google Scholar]
- Miyazaki, T.; Hotta, Y.; Kunii, J.; Kuriyama, S.; Tamaki, Y. A review of dental CAD/CAM: Current status and future perspectives from 20 years of experience. Dent. Mater. J. 2009, 28, 44–56. [Google Scholar] [CrossRef] [PubMed]
- Otto, T.; Dent, M. Case series Clinical Results from a Long Term Case Series using Chairside CEREC CAD-CAM Inlays and Onlays. Int. J. Prosthodont. 2008, 21, 53–59. [Google Scholar]
- Sjögren, G.; Molin, M.; Van Dijken, J.W.V. A 5-year clinical evaluation of ceramic inlays (Cerec) cemented with a dual-cured or chemically cured resin composite luting agent. Acta Odontol. Scand. 1998, 56, 263–267. [Google Scholar] [CrossRef]
- Zimmermann, M.; Koller, C.; Reymus, M.; Mehl, A.; Hickel, R. Clinical Evaluation of Indirect Particle-Filled Composite Resin CAD/CAM Partial Crowns after 24 Months. J. Prosthodont. 2018, 27, 694–699. [Google Scholar] [CrossRef]
- Tunac, A.T.; Celik, E.U.; Yasa, B. Two-year performance of CAD/CAM fabricated resin composite inlay restorations: A randomized controlled clinical trial. J. Esthet. Restor. Dent. 2019, 31, 627–638. [Google Scholar] [CrossRef] [PubMed]
- Alghazzawi, T.F. Advancements in CAD/CAM technology: Options for practical implementation. J. Prosthodont. Res. 2016, 60, 72–84. [Google Scholar] [CrossRef] [PubMed]
- Rahim Hussain, D. CAD CAM In Restorative Dentistry, College of Dentistry. Maser’s Thesis, University of Baghdad, Baghdad, Iraq, 2018. [Google Scholar]
- Jia-Mahasap, W. Comparative Assessment of Conventional vs. CAD/CAM Complete Denture Fabrication Techniques on Patient Satisfaction, Quality of Life and Prosthesis Biofilm. Master’s Thesis, University of Iowa, Iowa City, IA, USA, 2017. [Google Scholar]
- Bilgin, M.S.; Baytaroğlu, E.N.; Erdem, A.; Dilber, E. A review of computer-aided design/computer-aided manufacture techniques for removable denture fabrication. Eur. J. Dent. 2016, 10, 286–291. [Google Scholar] [CrossRef] [PubMed]
- Saponaro, P.C.; Yilmaz, B.; Heshmati, R.H.; McGlumphy, E.A. Clinical performance of CAD-CAM-fabricated complete dentures: A cross-sectional study. J. Prosthet. Dent. 2016, 116, 431–435. [Google Scholar] [CrossRef] [PubMed]
- Vecsei, B.; Joós-Kovács, G.; Borbély, J.; Hermann, P. Comparison of the accuracy of direct and indirect three-dimensional digitizing processes for CAD/CAM systems—An In Vitro study. J. Prosthodont. Res. 2017, 61, 177–184. [Google Scholar] [CrossRef]
- Pallesen, U.; Van Dijken, J.W.V. An 8-year evaluation of sintered ceramic and glass ceramic inlays processed by the Cerec CAD/CAM system. Eur. J. Oral Sci. 2000, 108, 239–246. [Google Scholar] [CrossRef] [PubMed]
- Sjögren, G.; Molin, M.; van Dijken, J.W. A 10-year prospective evaluation of CAD/CAM-manufactured (Cerec) ceramic inlays cemented with a chemically cured or dual-cured resin composite. Int. J. Prosthodont. 2004, 17, 241–246. [Google Scholar]
- Zimmer, S.; Göhlich, O.; Rüttermann, S.; Lang, H.; Raab, W.H.M.; Barthel, C.R. Long-term survival of cerec restorations: A 10-year study. Oper. Dent. 2008, 33, 484–487. [Google Scholar] [CrossRef]
- Awada, A.; Nathanson, D. Mechanical properties of resin-ceramic CAD/CAM restorative materials Presented at the American Association of Dental Research/Canadian Association of Dental Research Annual Meeting, Charlotte, NC, March 2014. J. Prosthet. Dent. 2015, 114, 587–593. [Google Scholar] [CrossRef]
- Popa, D.; Bordea, I.R.; Burde, A.V.; Crişan, B.; Câmpian, R.S.; Constantiniuc, M. Surface modification of zirconia after laser irradiation. Optoelectron. Adv. Mater. Rapid Commun. 2016, 10, 785–788. [Google Scholar]
- Romanyk, D.L.; Martinez, Y.T.; Veldhuis, S.; Rae, N.; Guo, Y.; Sirovica, S.; Fleming, G.J.P.; Addison, O. Strength-limiting damage in lithium silicate glass-ceramics associated with CAD–CAM. Dent. Mater. 2019, 35, 98–104. [Google Scholar] [CrossRef]
- Uzun, G. An overview of dental cad/cam systems. Biotechnol. Biotechnol. Equip. 2008, 22, 530–535. [Google Scholar] [CrossRef][Green Version]
- Blatz, M.B.; Conejo, J. The Current State of Chairside Digital Dentistry and Materials. Dent. Clin. N. Am. 2019, 63, 175–197. [Google Scholar] [CrossRef] [PubMed]
- Steinmassl, P.-A.; Klaunzer, F.; Steinmassl, O.; Dumfahrt, H.; Grunert, I. Evaluation of Currently Available CAD/CAM Denture Systems. Int. J. Prosthodont. 2017, 30, 116–122. [Google Scholar] [CrossRef]
- Hategan, S.I.; Ionel, T.F.; Goguta, L.; Gavrilovici, A.; Negrutiu, M.L.; Jivanescu, A. Powder and Powder-Free Intra-Oral Scanners: Digital Impression Accuracy. Prim. Dent. J. 2018, 7, 40–43. [Google Scholar] [CrossRef] [PubMed]
- Abdullah, A.; Muhammed, F.; Zheng, B.; Liu, Y. An Overview of Computer Aided Design/Computer Aided Manufacturing (CAD/CAM) in Restorative Dentistry. J. Dent. Mater. Tech. 2018, 7, 1–10. [Google Scholar] [CrossRef]
- Ender, A.; Mehl, A. In-Vitro evaluation of the accuracy of conventional and digital methods of obtaining full-arch dental impressions. Quintessence Int. 2015, 46, 9–17. [Google Scholar] [CrossRef]
- Beuer, F.; Schweiger, J.; Edelhoff, D. Digital dentistry: An overview of recent developments for CAD/CAM generated restorations. Br. Dent. J. 2008, 204, 505–511. [Google Scholar] [CrossRef] [PubMed]
- Lambert, H.; Durand, J.C.; Jacquot, B.; Fages, M. Dental biomaterials for chairside CAD/CAM: State of the art. J. Adv. Prosthodont. 2017, 9, 486–495. [Google Scholar] [CrossRef]
- Ruse, N.D.; Sadoun, M.J. Resin-composite blocks for dental CAD/CAM applications. J. Dent. Res. 2014, 93, 1232–1234. [Google Scholar] [CrossRef] [PubMed]
- Rogula, J.; Kuźniar-Folwarczny, A.; Sulewski, M.; Błaszczyk, A. Charakterystyka kompozytowych materiałów stomatologicznych stosowanych w gabinetowych systemach CAD/CAM. Inżynier i Fizyk Medyczny 2020, 9, 57–61. [Google Scholar]
- Charlton, D.G.; Roberts, H.W.; Tiba, A. Measurement of select physical and mechanical properties of 3 machinable ceramic materials. Quintessence Int. 2008, 39, 573–579. [Google Scholar]
- Kelly, J.R.; Nishimura, I.; Campbell, S.D. Ceramics in dentistry: Historical roots and current perspectives. J. Prosthet. Dent. 1996, 75, 18–32. [Google Scholar] [CrossRef]
- Datla, S.R.; Alla, R.K.; Alluri, V.R.; Babu, J.P.; Konakanchi, A. Dental Ceramics: Part II–Recent Advances in Dental Ceramics. Am. J. Mater. Eng. Technol. 2015, 3, 19–26. [Google Scholar] [CrossRef]
- Spitznagel, F.A.; Boldt, J.; Gierthmuehlen, P.C. CAD/CAM Ceramic Restorative Materials for Natural Teeth. J. Dent. Res. 2018, 97, 1082–1091. [Google Scholar] [CrossRef]
- 3M. LavaTM Ultimate CAD/CAM Restorative for CEREC. Available online: .https://www.3m.com/3M/en_US/company-us/all-3m-products/~/lava-ultimate-cerec-3M-Lava-Ultimate-CAD-CAM-Restorative-for-CEREC-/?N=5002385+3294768924&rt=rud (accessed on 14 March 2021).
- Vita Zahnfabrik. Vita Enamic -Technical and Scientific Documentation. 2019. Available online: https://www.vita-zahnfabrik.com/en/VITA-ENAMIC-17427.html (accessed on 14 March 2021).
- Thurmond, J.W.; Barkmeier, W.W.; Wilwerding, T.M. Effect of porcelain surface treatments on bond strengths of composite resin bonded to porcelain. J. Prosthet. Dent. 1994, 72, 355–359. [Google Scholar] [CrossRef]
- Kurtulmus-Yilmaz, S.; Cengiz, E.; Ongun, S.; Karakaya, I. The Effect of Surface Treatments on the Mechanical and Optical Behaviors of CAD/CAM Restorative Materials. J. Prosthodont. 2019, 28, e496–e503. [Google Scholar] [CrossRef] [PubMed]
- Klosa, K.; Boesch, I.; Kern, M. Long-term bond of glass ceramic and resin cement: Evaluation of titanium tetrafluoride as an alternative etching agent for lithium disilicate ceramics. J. Adhes. Dent. 2013, 15, 377–37783. [Google Scholar] [CrossRef]
- El-Mowafy, O.; Brochu, J.F. Longevity and clinical performance of IPS-Empress ceramic restorations—A literature review. J. Can. Dent. Assoc. 2002, 68, 233–237. [Google Scholar] [PubMed]
- Mayinger, F.; Lümkemann, N.; Musik, M.; Eichberger, M.; Stawarczyk, B. Comparison of mechanical properties of different reinforced glass-ceramics. J. Prosthet. Dent. 2020, 1–8. [Google Scholar] [CrossRef]
- Tysowsky, G.W. The science behind lithium disilicate: A metal-free alternative. Dent. Today 2009, 28, 112–113. [Google Scholar] [PubMed]
- Pieger, S.; Salman, A.; Bidra, A.S. Clinical outcomes of lithium disilicate single crowns and partial fixed dental prostheses: A systematic review. J. Prosthet. Dent. 2014, 112, 22–30. [Google Scholar] [CrossRef] [PubMed]
- Schultheis, S.; Strub, J.R.; Gerds, T.A.; Guess, P.C. Monolithic and bi-layer CAD/CAM lithium-disilicate versus metal-ceramic fixed dental prostheses: Comparison of fracture loads and failure modes after fatigue. Clin. Oral Investig. 2013, 17, 1407–1413. [Google Scholar] [CrossRef]
- Reich, S.; Endres, L.; Weber, C.; Wiedhahn, K.; Neumann, P.; Schneider, O.; Rafai, N.; Wolfart, S. Three-unit CAD/CAM-generated lithium disilicate FDPs after a mean observation time of 46 months. Clin. Oral Investig. 2014, 18, 2171–2178. [Google Scholar] [CrossRef] [PubMed]
- Eldwakhly, E.; Ahmed, D.R.M.; Soliman, M.; Abbas, M.M.; Badrawy, W. Color and translucency stability of novel restorative CAD/CAM materials. Dent. Med. Probl. 2019, 56, 349–356. [Google Scholar] [CrossRef]
- Conejo, J.; Nueesch, R.; Vonderheide, M.; Blatz, M.B. Clinical Performance of All-Ceramic Dental Restorations. Curr. Oral Heal. Reports 2017, 4, 112–123. [Google Scholar] [CrossRef]
- Raigrodski, A.J. Clinical and laboratory considerations for the use of CAD/CAM Y-TZP-based restorations. Pract. Proced. Aesthet. Dent. 2003, 15, 469–476; quiz 477. [Google Scholar]
- Kelly, P.M.; Rose, L.R.F. The martensitic transformation in ceramics - Its role in transformation toughening. Prog. Mater. Sci. 2002, 47, 463–557. [Google Scholar] [CrossRef]
- Gebhardr, A.; Todd, J.C. IPS e.max ZirCAD - Scientific Documentation. Available online: https://asia.ivoclarvivadent.com/zoolu-website/media/document/42081/IPS+e-max+ZirCAD (accessed on 5 November 2020).
- Rojas Vizcaya, F. Retrospective 2- to 7-Year Follow-Up Study of 20 Double Full-Arch Implant-Supported Monolithic Zirconia Fixed Prostheses: Measurements and Recommendations for Optimal Design. J. Prosthodont. 2018, 27, 501–508. [Google Scholar] [CrossRef] [PubMed]
- Mallineni, S.K.; Nuvvula, S.; Matinlinna, J.P.; Yiu, C.K.; King, N.M. Biocompatibility of various dental materials in contemporary dentistry: A narrative insight. J. Investig. Clin. Dent. 2013, 4, 9–19. [Google Scholar] [CrossRef]
- Alt, V.; Hannig, M.; Wöstmann, B.; Balkenhol, M. Fracture strength of temporary fixed partial dentures: CAD/CAM versus directly fabricated restorations. Dent. Mater. 2011, 27, 339–347. [Google Scholar] [CrossRef] [PubMed]
- Alp, G.; Murat, S.; Yilmaz, B. Comparison of Flexural Strength of Different CAD/CAM PMMA-Based Polymers. J. Prosthodont. 2019, 28, e491–e495. [Google Scholar] [CrossRef]
- Güth, J.F.; e Silva, J.S.A.; Beuer, F.; Edelhoff, D. Enhancing the predictability of complex rehabilitation with a removable CAD/CAM-fabricated long-term provisional prosthesis: A clinical report. J. Prosthet. Dent. 2012, 107, 1–6. [Google Scholar] [CrossRef]
- Rodriguez, F.; Cohen, C.; Ober, C.K.; Archer, L. Principles of Polymer Systems; CRC Press: Boca Raton, FL, USA, 2014. [Google Scholar]
- Matarasso, S.; Rasperini, G.; Iorio Siciliano, V.; Salvi, G.E.; Lang, N.P.; Aglietta, M. A 10-year retrospective analysis of radiographic bone-level changes of implants supporting single-unit crowns in periodontally compromised vs. periodontally healthy patients. Clin. Oral Implant. Res. 2010, 21, 898–903. [Google Scholar] [CrossRef]
- Taufall, S.; Eichberger, M.; Schmidlin, P.R.; Stawarczyk, B. Fracture load and failure types of different veneered polyetheretherketone fixed dental prostheses. Clin. Oral Investig. 2016, 20, 2493–2500. [Google Scholar] [CrossRef]
- Tekin, S.; Cangül, S.; Adıgüzel, Ö.; Değer, Y. Areas for use of PEEK material in dentistry. Int. Dent. Res. 2018, 8, 84–92. [Google Scholar] [CrossRef]
- Güth, J.F.; Almeida E Silva, J.S.; Ramberger, M.; Beuer, F.; Edelhoff, D. Treatment concept with CAD/CAM-fabricated high-density polymer temporary restorations. J. Esthet. Restor. Dent. 2012, 24, 310–318. [Google Scholar] [CrossRef] [PubMed]
- Bähr, N.; Keul, C.; Edelhoff, D.; Eichberger, M.; Roos, M.; Gernet, W.; Stawarczyk, B. Effect of different adhesives combined with two resin composite cements on shear bond strength to polymeric CAD/CAM materials. Dent. Mater. J. 2013, 32, 492–501. [Google Scholar] [CrossRef]
- Stawarczyk, B.; Liebermann, A.; Eichberger, M.; Güth, J.F. Evaluation of mechanical and optical behavior of current esthetic dental restorative CAD/CAM composites. J. Mech. Behav. Biomed. Mater. 2016, 55, 1–11. [Google Scholar] [CrossRef]
- Ardelean, L.C.; Bortun, C.M.; Podariu, A.C.; Rusu, L.C. Acrylates and Their Alternatives in Dental Applications. Acrylic Polym. Healthc. 2017. [Google Scholar] [CrossRef]
- Alamoush, R.A.; Kushnerev, E.; Yates, J.M.; Satterthwaite, J.D.; Silikas, N. Response of two gingival cell lines to CAD/CAM composite blocks. Dent. Mater. 2020, 36, 1214–1225. [Google Scholar] [CrossRef]
- Okada, R.; Asakura, M.; Ando, A.; Kumano, H.; Ban, S.; Kawai, T.; Takebe, J. Fracture strength testing of crowns made of CAD/CAM composite resins. J. Prosthodont. Res. 2018, 62, 287–292. [Google Scholar] [CrossRef]
- Bapat, R.A.; Joshi, C.P.; Bapat, P.; Chaubal, T.V.; Pandurangappa, R.; Jnanendrappa, N.; Gorain, B.; Khurana, S.; Kesharwani, P. The use of nanoparticles as biomaterials in dentistry. Drug Discov. Today 2019, 24, 85–98. [Google Scholar] [CrossRef] [PubMed]
- Mitra, S.B.; Wu, D.; Holmes, B.N. An application of nanotechnology in advanced dental materials. J. Am. Dent. Assoc. 2003, 134, 1382–1390. [Google Scholar] [CrossRef] [PubMed]
- Schmalz, G.; Hickel, R.; van Landuyt, K.L.; Reichl, F.X. Nanoparticles in dentistry. Dent. Mater. 2017, 33, 1298–1314. [Google Scholar] [CrossRef] [PubMed]
- Suh, W.H.; Suslick, K.S.; Stucky, G.D.; Suh, Y.H. Nanotechnology, nanotoxicology, and neuroscience. Prog. Neurobiol. 2009, 87, 133–170. [Google Scholar] [CrossRef]
- Ai, J.; Biazar, E.; Jafarpour, M.; Montazeri, M.; Majdi, A.; Aminifard, S.; Zafari, M.; Akbari, H.R.; Rad, H.G. Nanotoxicology and nanoparticle safety in biomedical designs. Int. J. Nanomed. 2011, 6, 1117. [Google Scholar] [CrossRef]
- Ludovichetti, F.S.; Trindade, F.Z.; Werner, A.; Kleverlaan, C.J.; Fonseca, R.G. Wear resistance and abrasiveness of CAD-CAM monolithic materials. J. Prosthet. Dent. 2018, 120, 318–e1. [Google Scholar] [CrossRef]
- Lee, Y.K. Influence of scattering/absorption characteristics on the color of resin composites. Dent. Mater. 2007, 23, 124–131. [Google Scholar] [CrossRef]
- AlKahtani, R.N. The implications and applications of nanotechnology in dentistry: A review. Saudi Dent. J. 2018, 30, 107–116. [Google Scholar] [CrossRef] [PubMed]
- Thompson, G.A.; Luo, Q. Contribution of postpolymerization conditioning and storage environments to the mechanical properties of three interim restorative materials. J. Prosthet. Dent. 2014, 112, 638–648. [Google Scholar] [CrossRef]
- Naveen, K.S.; Singh, J.P.; Viswambaran, C.M.; Dhiman, R.K. Evaluation of flexural strength of resin interim restorations impregnated with various types of silane treated and untreated glass fibres. Med. J. Armed Forces India 2015, 71, S293–S298. [Google Scholar] [CrossRef] [PubMed]
- Chun, K.J.; Lee, J.Y. Comparative study of mechanical properties of dental restorative materials and dental hard tissues in compressive loads. J. Dent. Biomech. 2014, 5. [Google Scholar] [CrossRef] [PubMed]
- Wendler, M.; Belli, R.; Petschelt, A.; Mevec, D.; Harrer, W.; Lube, T.; Danzer, R.; Lohbauer, U. Chairside CAD/CAM materials. Part 2: Flexural strength testing. Dent. Mater. 2017, 33, 99–109. [Google Scholar] [CrossRef] [PubMed]
- VITA IN-CERAM. Available online: http://www.cerec.co.il/downloads/vita_in_ceram.pdf (accessed on 5 November 2020).
- Belli, R.; Wendler, M.; de Ligny, D.; Cicconi, M.R.; Petschelt, A.; Peterlik, H.; Lohbauer, U. Chairside CAD/CAM materials. Part 1: Measurement of elastic constants and microstructural characterization. Dent. Mater. 2017, 33, 84–98. [Google Scholar] [CrossRef] [PubMed]
- Wendler, M.; Belli, R.; Valladares, D.; Petschelt, A.; Lohbauer, U. Chairside CAD/CAM materials. Part 3: Cyclic fatigue parameters and lifetime predictions. Dent. Mater. 2018, 34, 910–921. [Google Scholar] [CrossRef]
- VITA CAD-Temp. Available online: https://erp.somuden.es/instrucciones/804-6.pdf (accessed on 5 November 2020).
- Osorio, E.; Toledano, M.; da Silveira, B.L.; Osorio, R. Effect of different surface treatments on In-Ceram Alumina roughness. An AFM study. J. Dent. 2010, 38, 118–122. [Google Scholar] [CrossRef]
- ZirCAD. The Innovative Zirconium Oxide. Available online: https://www.ivoclarvivadent.com/en/p/all/products/all-ceramics/ips-emax-technicians/ips-emax-zircad (accessed on 5 November 2020).
- Mainjot, A.K.; Dupont, N.M.; Oudkerk, J.C.; Dewael, T.Y.; Sadoun, M.J. From Artisanal to CAD-CAM Blocks: State of the Art of Indirect Composites. J. Dent. Res. 2016, 95, 487–495. [Google Scholar] [CrossRef] [PubMed]
- Dobrzynski, M.; Pajaczkowska, M.; Nowicka, J.; Jaworski, A.; Kosior, P.; Szymonowicz, M.; Kuropka, P.; Rybak, Z.; Bogucki, Z.A.; Filipiak, J.; et al. Study of Surface Structure Changes for Selected Ceramics Used in the CAD/CAM System on the Degree of Microbial Colonization, In Vitro Tests. Biomed Res. Int. 2019, 2019. [Google Scholar] [CrossRef]
- IPS Empress CAD. Available online: https://www.ivoclarvivadent.com/en/productcategories/ips-empress-system-technicians/ips-empress-cad (accessed on 5 November 2020).
- Lava Ultimate: Technical Product Profile. Available online: http://www.d-way.cz/data/product/13/23/files/Lava_Ult_TPP.pdf (accessed on 4 November 2020).
- Polident CAD/CAM Discs. Available online: https://www.polident.si/en/products/cad-cam-discs/2019071510431758 (accessed on 5 November 2020).
- Toth, J.M.; Wang, M.; Estes, B.T.; Scifert, J.L.; Seim, H.B.; Turner, A.S. Polyetheretherketone as a biomaterial for spinal applications. Biomaterials 2006, 27, 324–334. [Google Scholar] [CrossRef]
- Ferguson, S.J.; Visser, J.M.A.; Polikeit, A. The long-term mechanical integrity of non-reinforced PEEK-OPTIMA polymer for demanding spinal applications: Experimental and finite-element analysis. Eur. Spine J. 2006, 15, 149–156. [Google Scholar] [CrossRef]
- PEEK OPTIMA Natural–Invibio. Available online: https://invibio.com/materials/peek-optima-natural (accessed on 4 November 2020).
- Mine, A.; Kabetani, T.; Kawaguchi-Uemura, A.; Higashi, M.; Tajiri, Y.; Hagino, R.; Imai, D.; Yumitate, M.; Ban, S.; Matsumoto, M.; et al. Effectiveness of current adhesive systems when bonding to CAD/CAM indirect resin materials: A review of 32 publications. Jpn. Dent. Sci. Rev. 2019, 55, 41–50. [Google Scholar] [CrossRef]
- El Zohairy, A.A.; De Gee, A.J.; Mohsen, M.M.; Feilzer, A.J. Microtensile bond strength testing of luting cements to prefabricated CAD/CAM ceramic and composite blocks. Dent. Mater. 2003, 19, 575–583. [Google Scholar] [CrossRef]
- Blatz, M.B.; Vonderheide, M.; Conejo, J. The Effect of Resin Bonding on Long-Term Success of High-Strength Ceramics. J. Dent. Res. 2018, 97, 132–139. [Google Scholar] [CrossRef]
- Furtado de Mendonca, A.; Shahmoradi, M.; de Gouvêa, C.V.D.; De Souza, G.M.; Ellakwa, A. Microstructural and Mechanical Characterization of CAD/CAM Materials for Monolithic Dental Restorations. J. Prosthodont. 2019, 28, e587–e594. [Google Scholar] [CrossRef] [PubMed]
- Sonmez, N.; Gultekin, P.; Turp, V.; Akgungor, G.; Sen, D.; Mijiritsky, E. Evaluation of five CAD/CAM materials by microstructural characterization and mechanical tests: A comparative In Vitro study. BMC Oral Health 2018, 18, 1–13. [Google Scholar] [CrossRef] [PubMed]
- Queiroz, J.R.C.; Fissmer, S.F.; Koga-Ito, C.Y.; Salvia, A.C.R.D.; Massi, M.; Sobrinho, A.S.d.S.; Júnior, L.N. Effect of diamond-like carbon thin film coated acrylic resin on candida albicans biofilm formation. J. Prosthodont. 2013, 22, 451–455. [Google Scholar] [CrossRef] [PubMed]
- Haralur, S.B. Evaluation of efficiency of manual polishing over autoglazed and overglazed porcelain and its effect on plaque accumulation. J. Adv. Prosthodont. 2012, 4, 179–186. [Google Scholar] [CrossRef]
- Kanat-Ertürk, B. Color Stability of CAD/CAM Ceramics Prepared with Different Surface Finishing Procedures. J. Prosthodont. 2020, 29, 166–172. [Google Scholar] [CrossRef] [PubMed]
- Stawarczyk, B.; Sener, B.; Trottmann, A.; Roos, M.; Özcan, M.; Hämmerle, C.H.F. Discoloration of manually fabricated resins and industrially fabricated CAD/CAM blocks versus glass-ceramic: Effect of storage media, duration, and subsequent polishing. Dent. Mater. J. 2012, 31, 377–383. [Google Scholar] [CrossRef]
- De Jager, N.; Feilzer, A.J.; Davidson, C.L. The influence of surface roughness on porcelain strength. Dent. Mater. 2000, 16, 381–388. [Google Scholar] [CrossRef]
- Mota, E.G.; Smidt, L.N.; Fracasso, L.M.; Burnett, L.H.; Spohr, A.M. The effect of milling and postmilling procedures on the surface roughness of CAD/CAM materials. J. Esthet. Restor. Dent. 2017, 29, 450–458. [Google Scholar] [CrossRef]
- Ivoclar Vivadent AG IPS, e.max CAD Glaze—Advanced Characterization. Available online: https://www.youtube.com/watch?v=_pMPUyfnZNA (accessed on 14 October 2020).
- Tekçe, N.; Fidan, S.; Tuncer, S.; Kara, D.; Demirci, M. The effect of glazing and aging on the surface properties of CAD/CAM resin blocks. J. Adv. Prosthodont. 2018, 10, 50–57. [Google Scholar] [CrossRef] [PubMed]
- Vichi, A.; Fabian Fonzar, R.; Goracci, C.; Carrabba, M.; Ferrari, M. Effect of finishing and polishing on roughness and gloss of lithium disilicate and lithium silicate zirconia reinforced glass ceramic for CAD/CAM systems. Oper. Dent. 2018, 43, 90–100. [Google Scholar] [CrossRef]
- Ekici, M.A.; Egilmez, F.; Cekic-Nagas, I.; Ergun, G. Physical characteristics of ceramic/glasspolymer based CAD/CAM materials: Effect of finishing and polishing techniques. J. Adv. Prosthodont. 2019, 11, 128–137. [Google Scholar] [CrossRef]
- Marrelli, M.; Maletta, C.; Inchingolo, F.; Alfano, M.; Tatullo, M. Three-point bending tests of zirconia core/veneer ceramics for dental restorations. Int. J. Dent. 2013, 2013. [Google Scholar] [CrossRef] [PubMed]
- D’Argenio, V.; Salvatore, F. The role of the gut microbiome in the healthy adult status. Clin. Chim. Acta 2015, 451, 97–102. [Google Scholar] [CrossRef] [PubMed]
- Rizo-Gorrita, M.; Herráez-Galindo, C.; Torres-Lagares, D.; Serrera-Figallo, M.Á.; Gutiérre-Pérez, J.L. Biocompatibility of Polymer and Ceramic CAD/CAM Materials with Human Gingival Fibroblasts (HGFs). Polymers 2019, 11, 1446. [Google Scholar] [CrossRef] [PubMed]
- Wenz, L.M.; Merritt, K.; Brown, S.A.; Moet, A.; Steffee, A.D. In Vitro biocompatibility of polyetheretherketone and polysulfone composites. J. Biomed. Mater. Res. 1990, 24, 207–215. [Google Scholar] [CrossRef]
- Hussain, B.; Le Thieu, M.K.; Johnsen, G.F.; Reseland, J.E.; Haugen, H.J. Can CAD/CAM resin blocks be considered as substitute for conventional resins? Dent. Mater. 2017, 33, 1362–1370. [Google Scholar] [CrossRef]
- Shim, J.; Kim, H.; Park, S.; Yun, H.; Ryu, J. Comparison of Various Implant Provisional Resin Materials for Cytotoxicity and Attachment to Human Gingival Fibroblasts. Int. J. Oral Maxillofac. Implants 2019, 34, 390–396. [Google Scholar] [CrossRef] [PubMed]
- Daguano, J.K.M.B.; Milesi, M.T.B.; Rodas, A.C.D.; Weber, A.F.; Sarkis, J.E.S.; Hortellani, M.A.; Zanotto, E.D. In Vitro biocompatibility of new bioactive lithia-silica glass-ceramics. Mater. Sci. Eng. C 2019, 94, 117–125. [Google Scholar] [CrossRef] [PubMed]
- Reference Offices. Available online: https://www.amadar.pl/sprzet/system-cadcam/poznaj-system-cerec/gabinety-referencyjne/ (accessed on 18 November 2020).
- Joda, T.; Bragger, U.; Zitzmann, N.U. CAD/CAM implant crowns in a digital workflow: Five-year follow-up of a prospective clinical trial. Clin. Implant Dent. Relat. Res. 2019, 21, 169–174. [Google Scholar] [CrossRef] [PubMed]
- Aslan, Y.U.; Coskun, E.; Ozkan, Y.; Dard, M. Clinical Evaluation of Three Types of CAD/CAM Inlay/Onlay Materials after 1-Year Clinical Follow Up. Eur. J. Prosthodont. Restor. Dent. 2019, 27, 131–140. [Google Scholar] [CrossRef] [PubMed]



| Type of Ceramics | Brand, Manufacturer | Clinical Application |
|---|---|---|
| Resin Matrix Ceramics | Lava Ultimate, 3M-ESPE VITA Enamic, VITA-Zahnfabrik Cerasmart, GC | Onlays, inlays, veneers, single crowns, implant crowns |
| Lithium Silicate Ceramics | IPS e.max CAD, Ivoclar Vivadent VITA Suprinity PC, VITA Zahnfabrik Celtra Duo, Dentsply Sirona | Inlays, onlays, veneers, crowns |
| Leucite-Reinforced Glass Ceramics | IPS Empress CAD, Ivoclar Vivadent | Veneers, inlays, onlays, crowns |
| Zirconium Oxide Ceramics | NobelProcera Zirconia, Nobel Biocare | Single crowns, bridges, prosthetic restorations covering the entire dental arches, mainly posterior segment |
| Aluminium Oxide Ceramics | InCeram Alumina, VITA Zahnfabrik | Single crowns, bridges |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Skorulska, A.; Piszko, P.; Rybak, Z.; Szymonowicz, M.; Dobrzyński, M. Review on Polymer, Ceramic and Composite Materials for CAD/CAM Indirect Restorations in Dentistry—Application, Mechanical Characteristics and Comparison. Materials 2021, 14, 1592. https://doi.org/10.3390/ma14071592
Skorulska A, Piszko P, Rybak Z, Szymonowicz M, Dobrzyński M. Review on Polymer, Ceramic and Composite Materials for CAD/CAM Indirect Restorations in Dentistry—Application, Mechanical Characteristics and Comparison. Materials. 2021; 14(7):1592. https://doi.org/10.3390/ma14071592
Chicago/Turabian StyleSkorulska, Aleksandra, Paweł Piszko, Zbigniew Rybak, Maria Szymonowicz, and Maciej Dobrzyński. 2021. "Review on Polymer, Ceramic and Composite Materials for CAD/CAM Indirect Restorations in Dentistry—Application, Mechanical Characteristics and Comparison" Materials 14, no. 7: 1592. https://doi.org/10.3390/ma14071592
APA StyleSkorulska, A., Piszko, P., Rybak, Z., Szymonowicz, M., & Dobrzyński, M. (2021). Review on Polymer, Ceramic and Composite Materials for CAD/CAM Indirect Restorations in Dentistry—Application, Mechanical Characteristics and Comparison. Materials, 14(7), 1592. https://doi.org/10.3390/ma14071592









