Abstract
In the latter part of the 20th century, three developments intersected: skin-to-artery catheterization, percutaneous tracheostomy, and market introduction of video-chip camera-tipped endoscopes. By the millennium, every vessel within the body could be visualized radiographically, and percutaneous tracheostomy (with tracheal-ring “dilation,” flawless high-resolution intratracheal video-imagery, and tracheal intubation) could consistently be achieved at the patient’s bedside. Initiated through the skin and abetted by guide-wire insertion, these procedures are the lasting gifts of Sven-Ivar Seldinger (1921–1998) of Mora, Sweden, and Pasquale Ciaglia (1912–2000) of Utica, New York. Physicians and surgeons managing intracranial, craniofacial, and maxillofacial injury are among those honoring the Seldinger–Ciaglia “collaboration.”
Sven-Ivar Seldinger (1921–1998) (Figure 1a) is acknowledged worldwide to have pioneered percutaneous angiography over a guide wire, a profound foundation for current-day interventional radiography and interventional cardiology. By the time of Seldinger’s demise at the age of 76, all vessels of the body were deemed to be readily within the reach of sufficient radiographic contrast and detailed display, using his technique.
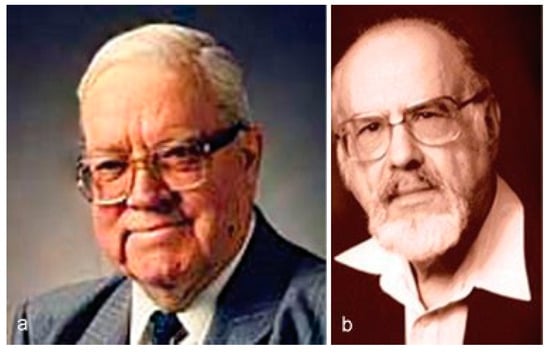
Figure 1.
(a) Sven-Ivar Seldinger (1921–1998). (b) Pasquale (“Pat”) Ciaglia (1912–2000).
Similarly but with less fanfare, when Pasquale Ciaglia (1912–2000) (Figure 1b) died at the age of 88, he was acknowledged to have pioneered percutaneous tracheostomy over a guide wire, at the patient’s bedside. The Ciaglia procedure reached new levels of efficiency after video-chip and camera-tipped endoscopes became available, and the technique gained broad popularity when controlled studies documented better pulmonary toilet, reduced mortality, shortened mechanical ventilation, and an abridged length of hospital stay.
The two pioneers cast a wide swath of innovation across multiple specialties, but their contributions are no more evident than in the management of cranial, craniofacial, and maxillofacial injury. Outcomes today reflect the diuturnity of the Seldinger and Ciaglia’s contributions, first offered in the latter half of the 20th century.
Percutaneous Angiography
During the early industrialization of Sweden in the 18th century, Mechanical Workshops (niduses for economic development) were formed to utilize Sweden’s natural resources, such as water, ore, and carding wool. Often vetted by on-site English engineers with firsthand experience of the prior industrialization of Britain, the incubators birthed enterprises in mining, manufacture of steel, shipbuilding, and creation of woven textiles in metropolitan Stockholm (Figure 2).
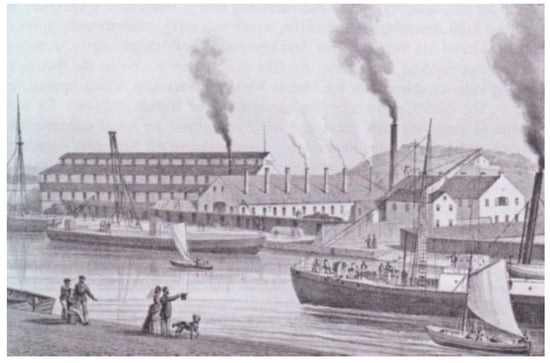
Figure 2.
Motala Verkstad (M. V.), founded in 1822, delivered the first steamship (the Motala) to the Swedish Post Office in 1831; G. Pabst in this lithograph portrays the M. V. Mechanical Workshop and adjacent foundries assembled by the 1870s. The Company gained renown worldwide in ensuing decades by building ships, bridges, locomotives, and kitchen sinks. [1 of 48 lithographs in Pabst G. Sveriges Industriella Etablissementer. Forsta Serien. Stockholm, Kjellberg and Astrom, 1872; image courtesy of Gustaf Pabst and the National Library of Sweden].
In 1840, the Swedish federal government abandoned craft guilds and sponsored the right of all citizens to start an enterprise. Creation of Mechanical Workshops sprang to life throughout southern and central Sweden. In Eskilstuna alone, 70 miles west of Stockholm, 180 Workshops were germinated to produce “light, high-quality knives and scythe blades; locks and fittings; hand-tools such as chisels and files; and precision weapons” [].
In the backwater, further southwest and northwest, the urban experience was repeated on a smaller, yet equally successful, scale: small-town entrepreneurs were encouraged to field products for local and national markets. The cottage industry maintained Stockholm-like quality controls, largely shielded from the trauma of the World Wars, and citizen pioneers over the ensuing 150 years learned skill-sets in precision machinery and fine instrumentation. The widespread mini-industrialization meant jobs, quality outcomes, and protracted economic prowess.
The Mechanical Workshop in Mora, in the Dalarna area, some 200 miles northwest of Stockholm, between the northern shore of Lake Siljan and the southern shore of Lake Orsasjon, reached notable success. Members in Mora designed and manufactured hardy clocks and watches, domestic sewing machines, wellhoned knives, and precision water faucets (Wikipedia; Greitz; Whonamedit). Their provincial prowess was celebrated annually during the summer solstice, when collections of Dalhast wooden horses (Figure 3a,b), folk costumes, and centuries-old dance around a maypole went on display (Figure 4).
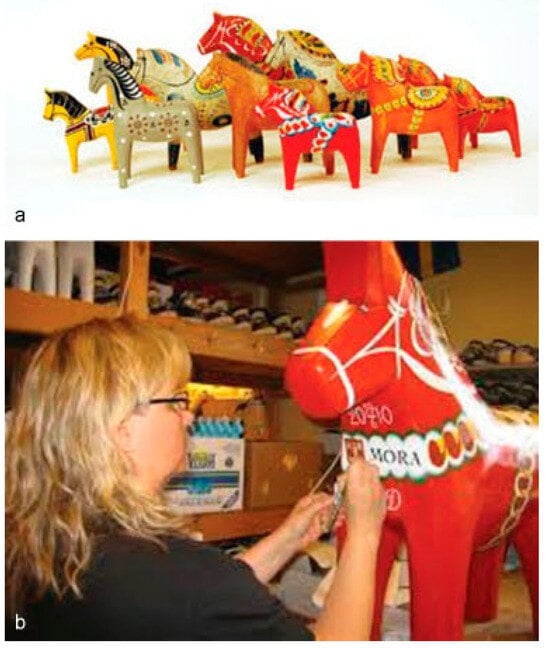
Figure 3.
(a,b) Dalhast wooden horses, each carved and identifiably painted by artists of the villages in the parish of Mora [photographs courtesy of Itdalarna.se and mora.se].
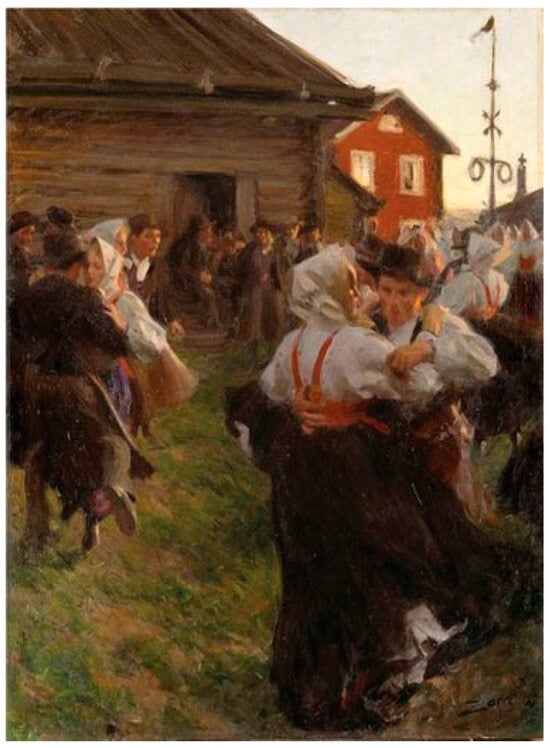
Figure 4.
The celebration of the 1897 solstice is depicted in Midsummer Dance, painted by Mora artist, Anders Zorn (1860–1920) [photograph of painting, courtesy of the Swedish Museum of Fine Arts, Stockholm].
For several generations, relatives on the maternal side of the Seldinger family had been elected to head the Mora Workshop. During adolescence, Sven-Ivar Seldinger and his five siblings, each an issue of the marriage of Ivar Swenson and Signe Vilhelmina Matson, would visit their maternal grandfather, to witness local engineering prowess and problem solving. From an early age, the youngsters gained a solid work ethic and serial exposure to innovation.
Sven-Ivar attended local public schools and the University of Uppsala, as a prelude to completing medical training at the Uppsala School of Medicine, in 1948. During a first year of a Residency in Radiology, he completed a series of deputyships in the Department of Surgery, at Karolinska Hospital. (Figure 5) Seldinger remained at Karolinska after the residency in radiology for two decades [,].

Figure 5.
Karolinska Kommun (Karolinska Hospital).
Attempts during the first half of the 20th century, in France, Cuba, Germany, Sweden, and the United States, to radiographically demonstrate the finer details of many visceral arteries, let alone the thoracic and ascending aorta and the aortic arch, had failed [,,,,,,,,,,,,]. Clinical successes had been limited:
- To visualization of the temporal and aortic vessels, after direct needle stick and an injection of contrast (1931) []
- To insertion of catheters into the aorta through a trocar in the surgically exposed temporal artery (1941 and 1946) [,]
- To proposals for catheterization of the right atrium, right ventricle, and pulmonary artery, based on the insights of Nobel Prize winners Werner Forssmann, Andre Cournand, and Dickinson Richards []
- To insertion of catheters into the radial artery (1948) [] and into the common carotid (1949) []
- To introduction of sheaths into the aorta, using a blunt silver thread as a guide (1949) []
- To direct injection of contrast material into the right and the left ventricles by percutaneous puncture (1951) []
- To percutaneous insertion of an inherently rigid nonradiopaque, polyethylene tube into the femoral artery, through a hollow needle (1951) []
Still, a percutaneous approach to angiography was needed (to avoid a “cut-down”) and use of large, soft catheters had long been sought, so large volumes of contrast medium could be injected to counter the volume and high velocity of aortic blood [].
Seldinger resolved the issues in a single session in the anatomy laboratory, during his radiology residency.
- First, he cut a side hole in a catheter, placed a cutting needle in the hole, and positioned the needle such that it was 1 to 2 mm beyond the end of the catheter; yet advancing the bulky aggregate within a vessel lumen proved awkward [,,].
- Second, he reduced the inherent mass of the combined needle–catheter by withdrawing the needle (from the catheter), then replaced the needle with a guidewire [,,]; the sequence (needle > catheter > guide wire) proved inept.
- Finally, “with three items in hand,” he elected a more favorable sequence (needle > guide wire > catheter) [,] (Figure 6):
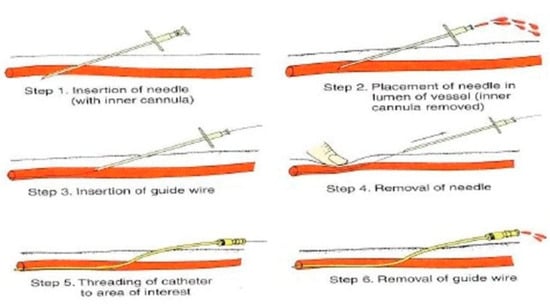 Figure 6. Modified illustration of the six steps of the Seldinger technique, courtesy of Shah R and www.slideshare.net.
Figure 6. Modified illustration of the six steps of the Seldinger technique, courtesy of Shah R and www.slideshare.net.
The first clinical angiography soon followed: after cubital, percutaneous puncture of the brachial artery and placement of a guide wire, Seldinger advanced a catheter to the level of the inferior thyroid artery, injected contrast material, and took a single, radiographic exposure. The X-ray revealed an occult, mediastinal parathyroid adenoma, the location of which had been skirted during prior operative exploration.
Numerous radiologists within and outside Sweden (notably P. Odman of Stockholm) soon corroborated Seldinger’s inaugural experience [,,,,,].
The details of an array of vessels, previously hidden from radiographic view, became known. The intricate, radiographic features of intracerebral arteries, the branches of the external carotid artery, the thoracic and ascending aorta, and the aortic arch, by example, were soon revealed. Numerous awards and recognition followed as the immensity of Seldinger’s seminal work was recognized [,,,,].
In 1967, at the age of 47 and after two decades of service at Karolinska Hospital, Doctor Seldinger left to join the Department of Radiology at Mora Hospital, in his hometown (Figure 7). He served as the Head of the Department from 1968 to 1986, where his photograph is still featured.
Figure 7.
Mora Kommun (Mora Hospital) [aerial photograph, courtesy of Wikipedia and Julia Svechnikova].
Sven-Ivar Seldinger died in 1998 and was survived by his wife, Britt-Liss, a noted painter, until her subsequent death. Their remains are together at Mora Kyrka. Sven-Ivar and BrittLiss are survived by daughters Mari, Nina, and Mona.
Percutaneous Tracheostomy
Pasquale (“Pat”) Ciaglia (1912–2000) was the sole issue of Clementine Perrillo (of New York) and Egidio (“Jerry”) Ciaglia of Buccino, a town in the southeast coastal province of Salerno, Italy []. Pat’s early adolescence was spent in Manhattan in the Italian “ghetto” on Second Avenue, characterized by cramped conditions and the searing passage of trolleys and elevated railroad cars (Figure 8).
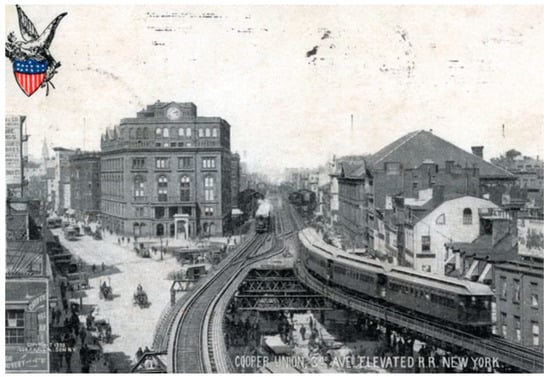
Figure 8.
Cooper Union, trolley lined 3rd Avenue, and the elevated railroad of Manhattan, New York City, at the turn of the 20th century. www. maggieblank.com Accessed 03–13–2015. [postcard posted 1904, courtesy collection of Maggie Land Blalock and the Library of Congress].
At the age of 10, the family moved (“escaped,” in Ciaglia’s words []) to Utica, NY, a town bordering the Erie Canal, in the Mohawk Valley and some 175 miles to the north–northwest of New York City (Figure 9). Centered in Oneida County around the parishes of St. Mary of Mount Carmel and St. Anthony of Padua, Utica was traversed by a ravine from north to south, such that the eastern section of the town was often referred to as East Utica. Known locally as “the gulf,” the natural fault was progressively filled, reaching lower East Utica by the time the Ciaglias arrived in 1921 [].
Figure 9.
1909 panoramic view of Utica, NY [photograph, courtesy of familypedia.wikia.com].
Arrivals to Utica often first sought employment in local textile mills, brickyards, lumber yards, and road construction companies. Entrepreneurs in their midst would initiate small businesses, choosing to be olive oil merchants, block-ice delivery men, haberdashers, musicians who provided background music for silent movies played at local theaters, bankers, insurance agents, wholesale or retail grocers, pasticciotta and sfogliatelle pastry bakers, purveyors of steamship tickets, or even speculators in the purchase and sale of real estate. Pasquale’s parents became part of this entrepreneurial mix, founding the Utica Drug Company at 906 Bleecker Street (Figure 10), the busy thoroughfare of East Utica, characterized by graceful elms, an ice cream shop, shoe repair, barber shop, and a family restaurant. Adolescents, often in the form of push-cart peddlers (Figure 11), were perceived to be developing skill sets to become champions of local and regional commerce [,]. In the early 1900s, Frank Inserra and Frank Longo entered the wholesale fruit business (Figure 12), and in 1916, the four Bonomo brothers (all from Villabate, Sicily) founded a pasta factory on Whitesboro Street that would later be couched as the largest macaroni enterprise in Upstate New York (Figure 13).
Figure 10.
The intersection of Bleecker Street and Kossuth Avenue, Utica, NY, looking east in the 1920s and 1930s; Egidio (“Jerry”) Ciaglia, a pharmacy school graduate of the State University of New York (SUNY), founded the Utica Drug Company at 906 Bleecker Street; Ciaglia was ably assisted for years by employee Ralph Vendetti [photograph, courtesy of the Oneida County Historical Society and the Utica Observer-Dispatch, June 3, 2001, issue].
Figure 11.
Adolescent push-cart peddlers in the Italian section of East Utica [photograph, courtesy of Philip A. Bean and the Utica Saturday Globe].
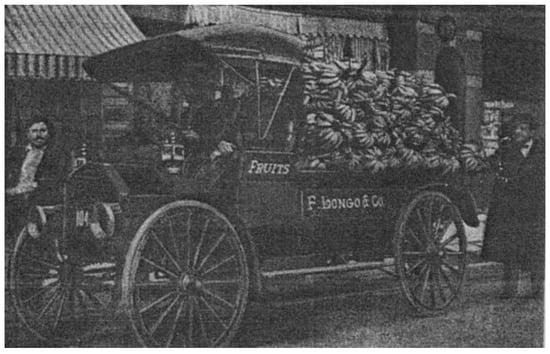
Figure 12.
Longo and Company fruit truck on Bleecker Street, East Utica, NY, in 1925 (photograph, courtesy of Philip A. Bean and the Utica Public Library).
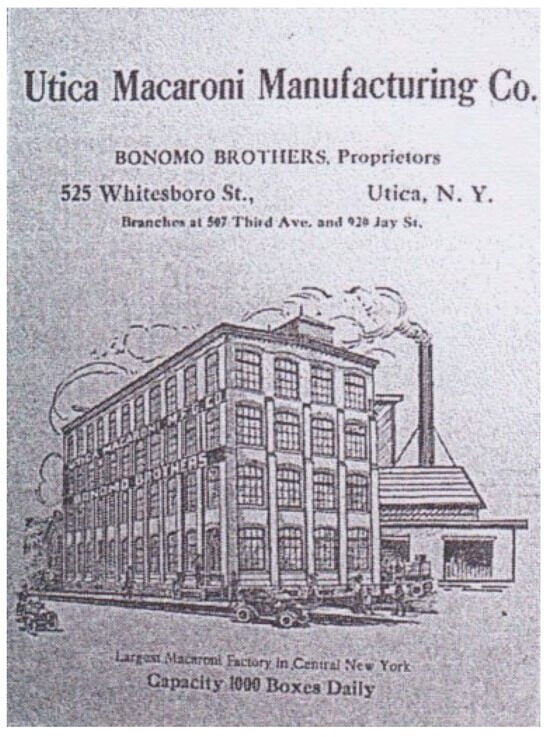
Figure 13.
The pasta factory on Whitesboro Street founded by Joseph, Frank, Vincent, and Salvatore Bonomo, at peak production produced 1,000 boxes of pasta daily [photograph, courtesy of the Oneida County Historical Society].
The newspapers II Pensiero Italiano, La Luce, and II Messagero dell’ Ordine set print in Italian; old-style feste (particularly the festa of Saints Cosmo and Damiano, at Saint Anthony of Padua Church) were frequently offered; traditional neighborhood evening strolls (la passeggiata) were encouraged; and not-so-secret mutual-aid societies ensured a sense of community, reminiscent of the Italian and Sicilian homeland [,,,].
Pat Ciaglia attended Utica Free Academy and the local Edmund A. Wetmore School, and by the time he went to high school (Figure 14), Italians were often elected to office; they had formed an effective political slate of prominent candidates that gained wide acceptance. Italian immigrants and their 20,000 children and grandchildren by 1929 constituted about a quarter of the population [].
Figure 14.
Pasquale Ciaglia, 1929, upon graduation from the Wetmore School [photograph, courtesy of The Academician and the Oneida County Historical Society].
In 1929, Pat Ciaglia matriculated at nearby Hamilton College, less than 10 miles from home (Figure 15). A school for boys at the time, it had been founded in 1793 by the Presbyterian Church as the Hamilton-Oneida Academy. Ciaglia (pronounced chal-ya) graduated in 1933, with, in his words, “a degree of anonymity.” Medical school at New York Medical College, in Valhalla, NY, preceded an internship at Crouse Irving Hospital (Figure 16) in Syracuse and a residency in Chest Medicine and Surgery at Sea View Hospital (Figure 17), on Staten Island [].
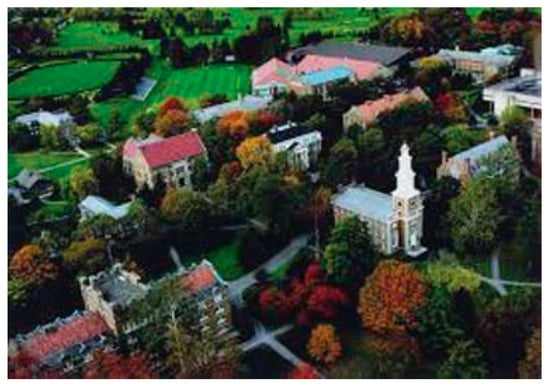
Figure 15.
Hamilton College, f.k.a. HamiltonOneida Academy.
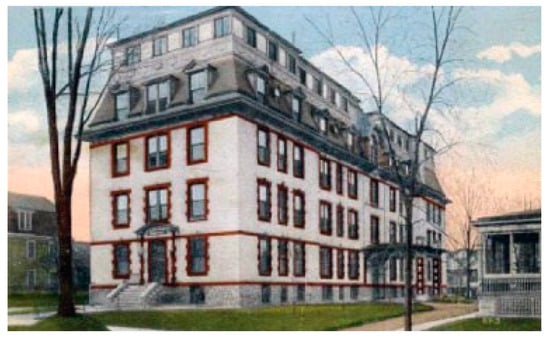
Figure 16.
Crouse Irving Hospital, Syracuse, NY.

Figure 17.
Sea View Hospital, New York City.
Immediately after thoracic residency training, Pat entered the United States Army and served for a total of 3.5 years during World War II. He was first sent to the Women’s Army Corp Training Center in Daytona, FL, then reassigned to the Medical Corp of the 48th General Hospital, as it embarked to Glasgow, Scotland, and the Borough of Swindon. In 1944, after 6 months in Swindon, 70 miles west of London, Ciaglia was transferred to the Department of Thoracic Surgery at the Lariboisière Hospital (Figure 18), in Paris, France. His assignment at Lariboisière lasted 2 years.

Figure 18.
48th Army General Hospital (Hôpital Lariboisière), Paris.
At a Parisian get together, Pat met Jacqueline Chicault, a French social worker, and the two married in August 18, 1945. The couple returned to the United States at War-end. Doctor Ciaglia arrived in Utica in 1946 to practice thoracic surgery (Figure 19) and, with Jacqueline, to raise their daughter Patricia Francine. Jacqueline’s mother joined them in 1947. Ciaglia joined the staff of four local hospitals, including St. Elizabeth (Figure 20) and Oneida County, where he practiced for 45 years, before retirement in 1994 (Figure 21).
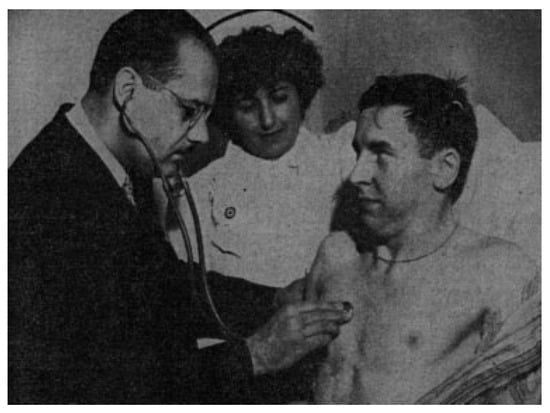
Figure 19.
Pasquale Ciaglia and nurse Josephine Talerico examine a postoperative patient at Oneida County Hospital [photograph, courtesy of Utica Observer and the Oneida County Historical Society].

Figure 20.
Saint Elizabeth Hospital, Utica, NY.
Figure 21.
Doctor and Mrs. Ciaglia [photograph, courtesy of Cook Medical, Bloomington, IN; Available at: remembering-dr-pat-ciaglia-atchest/2014; accessed October 20, 2015].
The subcutaneous position of the trachea had invited early attempts at percutaneous intubation, but the proposed techniques were labeled as “awkward” and “dangerous,” in great part because of a large number of fatalities. Then in 1984, Ciaglia by chance witnessed the ease with which a radiologist and urologist were able to consummate percutaneous removal of a kidney stone, using an Amplatz Renal Dilator set and the Seldinger technique.
Ciaglia quickly recognized its potential for tracheostomy. Cadaver dissections in Utica confirmed its applicability, and a foreshortened tracheostomy tube was created (Figure 22) to ensure intubation well above the carina. Thirty-four consecutive clinical cases of percutaneous tracheostomy free of complications soon followed, as reported in the journal Chest, in 1985 []. Other surgeons confirmed the inaugural effort of Ciaglia and his colleagues, and over the ensuing 15 years, multiple centers documented improved pulmonary toilet, reduced mortality, shortened mechanical ventilation, and an abridged length of stay following the percutaneous procedure [,,,,]. Industry facilitated clinical acceptance of the procedure by developing coiled J-shaped, guide-wire delivery systems, poised for single-handed advancement of the guide wire into the tracheal lumen. Various commercial embodiments followed, including the recent Blue Rhino kits distributed by Cook Medical of Bloomington, IN. Early designs of video-chip and camera-tipped endoscopes by Olympus (Olympus Corp., Center Valley, PA) and by Karl Storz Endoscopy (Karl Storz Endoscopy, El Segundo, CA) strategically entered the market.
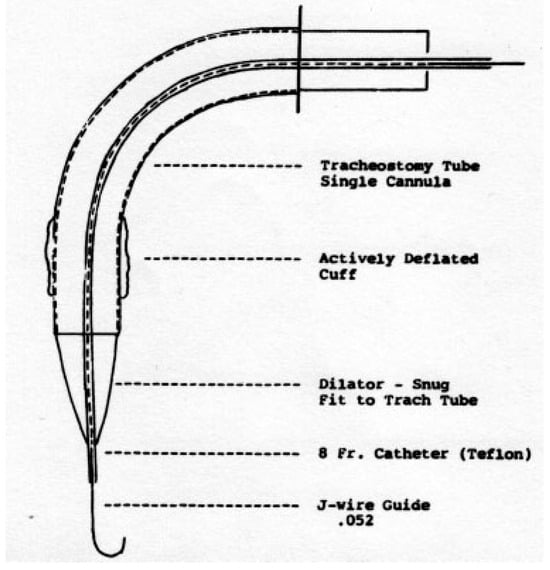
Figure 22.
Inaugural foreshortened tube used in percutaneous tracheostomy [illustration, courtesy of Pasquale Ciaglia, Rita Firsching, Cynthia Syniec, Chest, and the American College of Chest Physicians].
Percutaneous tracheostomy at the intensive care unit bedside, with virtual endoscopy, real-time video display (Figure 23), now features a rather standardized sequence.
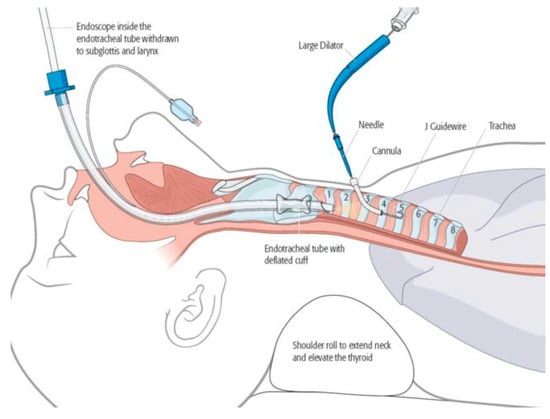
Figure 23.
Illustration and algorithm of percutaneous tracheostomy. An endoscope is passed through the endotracheal tube, to reach the upper trachea the cuff of the endotracheal tube is deflated, and the tube is withdrawn to the level of the subglottis needle-and-canula are inserted percutaneously into the trachea needle is removed J-guide-wire is inserted (through the lumen of the canula) primary and secondary dilators are placed on the guide wire, to dilate the tracheal ring interspace, then removed tracheostomy tube is placed on the guide wire and advanced into the trachea guide wire is removed tracheostomy tube collar is secured with 4-point fixation sutures.
Discussion
Tracheostomy was first attempted in Ancient India, Egypt, and Rome. The procedure was used only sporadically and sparingly over ensuing centuries, chosen only for upper airway obstruction caused by hematoma, abscess, tumor, or supraglottitis. A gibbous flare occurred in the 17th and 18th centuries, when epidemics of diphtheria were common [] (Figure 24). Then Armand Trousseau (1801–1867), a pupil of Pierre Bretonneau, introduced a tracheal spreader, popularized the anatomy and refinement of the tracheal procedure [], and introduced thoracentesis (1843) and endotracheal intubation to the Academy of Medicine of Paris in 1851 (Figure 25). Over the ensuing 150 years, tracheostomy has been made available in cases of upper and lower airway obstruction, when prolonged mechanical ventilation is required.

Figure 24.
Depiction of tracheostomy by Scultetus, J. Armamentarium chirurgicum. Ulm, Kuhnen, 1653.

Figure 25.
Armand Trousseau (1801–1867) popularized tracheostomy and introduced thoracentesis (1843) and endotracheal intubation (1851) to members of the Academy of Medicine of Paris [photograph, courtesy of Garrison FH. An Introduction to the History of Medicine with Medical Chronology, Suggestions for Study, and Bibliographic Data. Philadelphia, PA: WB Saunders Company; 1913].
Management of airway has been of particular interest to neurosurgeons (caring for those with stroke and other central, cranial compromise) [] and to surgeons managing craniofacial and maxillofacial trauma [,,,]. High-velocity pancraniomaxillofacial injuries are characterized by widely applied force equilibrium circuits, complex fracture lines, and wholesale instability. These patients require attentive airway management, and tracheostomy (after guide-wire intubation) is often prerequisite to first neurosurgical procedures and then, at the same setting, craniofacial and maxillofacial restoration [].
Despite the current ease with which percutaneous tracheostomy can be achieved, a cohort of patients is best exempted from the procedure at the bedside, and “controlled,” open tracheostomy is best undertaken in the presence of a posteriorly directed trachea; a foreshortened (substernal) trachea; a deviated trachea; obscured palpable landmarks, particularly a nonpalpable cricoid; a palpable, anomalous, right innominate artery; an extremely enlarged thyroid or lobe by palpation; morbid obesity; and a short or “bull” neck. Other conditions (anticoagulation; thrombocytopenia, when extreme; coagulopathy; and prior tracheostomy) may also provoke open, surgical tracheostomy.
Technical finesse of percutaneous tracheostomy is enhanced in the author’s experience by use of the following:
- Thoracic roll to extend the neck and elevate the thyroid gland
- Thorough local anesthetic with epinephrine infiltration of the subcutaneous and pretracheal soft tissue, with a 5- to 10-minute waiting period
- Preparation of skin with chlorhexidine (to avoid tracheal mucosal exposure to povidone)
- Use of a split-thyroid sheet to avoid encumbered access
- Surgical markings (thyroid notch, cricoid, midline, level of horizontal incision, suprasternal notch)
- Horizontal incision, with efficient dissection of the subcutaneous fat and Scarpa fascia
- Vertical dissection between the strap muscles and incision of the pretracheal fascia with needle electrocautery
- The needle-and-cannula, after entering the trachea between the second and third “rings” or the third and fourth “rings,” is directed downwardly, toward the carina, to avoid the soft, membranous posterior wall of the trachea and the underlying anterior wall of the esophagus
- Dilators “expand” the inter-ring space, to favor untethered entry of the tracheostomy tube, into the trachea. Cartilage is neither incised nor excised; every effort is made to ensure it remains intact and is not fractured.
Potential complications include punctured esophagus/retropharyngeal abscess []; subcutaneous atelectasis; airway compromise and desaturation; and postoperative bleeding from wound margins and/or erosion of thyroid vessels.
The safety, efficiency, and cost-effectiveness of percutaneous tracheostomy have been increasingly documented by surgeons, critical care physicians, and interventional pulmonologists, who now perform a majority of the procedures [,,].
Tracheostomy abetted by Seldinger guide-wire insertion has inarguably enhanced the status of medicine and surgery in general and the repair of craniofacial and maxillofacial injury in particular, in the 21st century.
Acknowledgments
Thanks to Lena Freijs, Omradessamordnare, Mora Hospital, Mora, Sweden, and notably Janice Reilly, Research Volunteer, Oneida County Historical Society, Utica, NY, for their help with seminal documents and references, enriching this article.
References
- Schon, L. An Economic History of Modern Sweden; Routledge: Abingdon, 2012. [Google Scholar]
- Doby, T. Development of Angiography and Cardiovascular Catheterization; John Wright: Littleton, CO, 1976. [Google Scholar]
- Doby, T. A tribute to Sven-Ivar Seldinger. AJR Am J Roentgenol 1984, 142, 1–4. [Google Scholar]
- Dos Santos, R.; Lamas, A.C.; Caldas, J.P. Arteriographie des Membres et de l’aorte Abdominale; Masson et Cie: Paris, 1931. [Google Scholar]
- Farinas, P.L. A new technique for the arteriographic examination if the abdominal aorta and its branches. AJR 1941, 46, 641–645. [Google Scholar]
- Farinas, P.L. Retrograde abdominal aortography; a contribution to the study of the abdominal aorta and iliac arteries. Radiology 1946, 47, 344–348. [Google Scholar] [CrossRef]
- Sourkes, T.L. Nobel Prize Winners in Medicine and Physiology; Abelard-Schuman: London, 1966; [Forrsmann, Cournand, and Richards won the Nobel Prize in 1956 for their work concerning ‘heart catheterization and pathological changes in the circulatory system.’]. [Google Scholar]
- Radner, S. Thoracic aortography by catheterization. Acta Radiol (Stockh) 1948, 29, 179–180. [Google Scholar]
- Freeman, N.E.; Miller, E.R. Retrograde arteriography in the diagnosis of cardiovascular lesions; visualization of aneurysms and peripheral arteries. Ann Intern Med 1949, 30, 330–342. [Google Scholar]
- Jonsson, G. Thoracic aortography by means of a cannula inserted percutaneously into the common carotid artery. Acta Radiol 1949, 31, 376–386. [Google Scholar] [CrossRef]
- Euler, H.E. Die peroesophagale Aortenpunktion. Arch Ohren Nassen Kehlk 1949, 155, 536–567. [Google Scholar] [CrossRef]
- Helmsworth, J.A.; McGuire, J.; Felson, B. Arteriography of the aorta and its branches by means of the polyethylene catheter. Am J Roentgenol Radium Ther 1950, 64, 196–213. [Google Scholar]
- Goodwin, W.E.; Scardino, P.L.; Scott, W.W. Translumbar aortic puncture and retrograde catheterization of the aorta in aortography and renal arteriography. Ann Surg 1950, 132, 944–958. [Google Scholar]
- Ponsdomenech, E.R.; Beato Nunez, V. Heart puncture in man for Diodrast visualization of the ventricular chambers and great arteries. Am Heart J 1951, 41, 643–650. [Google Scholar]
- Peirce, E.C., II. Percutaneous femoral artery catheterization in man with special reference to aortography. Surg Gynecol Obstet 1951, 93, 56–74. [Google Scholar]
- Seldinger, S.I. A leaf out of the history of angiography. In Pioneers in Angiography; Silvestre, M.E., Abecasis, F., Veiga-Pires, J.A., Eds.; Excerpta Medica (Elsevier): New York, 1987. [Google Scholar]
- Seldinger, S.I.; Edholm, P. Principles of percutaneous selective angiography. In Vascular Roentgenology; Schobinger, R.A., Ruzicka, F.F., Eds.; Macmillan: New York, 1964; pp. 41–45. [Google Scholar]
- Thomas, C.; O’Leary, J.P. Sven Ivar Seldinger. Am Surg 1996, 62, 783–784. [Google Scholar]
- Higgs, Z.C.; Macafee, D.A.; Braithwaite, B.D.; Maxwell-Armstrong, C.A. The Seldinger technique: 50 years on. Lancet 2005, 366, 1407–1409. [Google Scholar]
- Seldinger, S.I. Catheter replacement of the needle in percutaneous arteriography; a new technique. Acta Radiol 1953, 39, 368–376. [Google Scholar]
- Seldinger, S.I. Localization of parathyroid adenomata by arteriography. Acta Radiol 1954, 42, 353–366. [Google Scholar]
- Edholm, P.; Seldinger, S.I. Percutaneous catheterization of the renal artery. Acta Radiol 1956, 45, 15–20. [Google Scholar]
- Seldinger, S.I. Visualization of aortic and arterial occlusion by percutaneous puncture or catheterization of peripheral arteries. Angiology 1957, 8, 73–86. [Google Scholar]
- Seldinger, S.I. A simple method of catheterization of the spleen and liver. Acta Radiol 1957, 48, 93–96. [Google Scholar]
- Odman, P. Percutaneous selective angiography of the main branches of the aorta. Acta Radiol 1956, 45, 1–14. [Google Scholar]
- Cunningham, J.J.; Thurber, B. The abdominal aortogram: an historic perspective. Am J Roentgenol Radium Ther Nucl Med 1972, 116, 441–444. [Google Scholar]
- Flodmark, O.; Greitz, T. Obituary. Sven-Ivar Seldinger. Interv Neuroradiol 1999, 5, 9–10. [Google Scholar]
- Egidio Ciaglia Dies, Was Local Pharmacist; Utica Daily Press, 1966.
- Nates, J. Obitulogy: Pasquale Ciaglia, M.D., F.A.C.S. Internet J Emerg Intensive Care Med 2001, 52, 1–3, [written by Doctor Ciaglia; the date of death was postdated]. [Google Scholar]
- Clarke, T.W. Utica: For a Century and a Half, Widtman Press: Utica, 1952.
- Cardarelli, M.J. East Utica: Macchiata d’Amore; Ikon: Utica, NY, 2005. [Google Scholar]
- Bean, P.A. La Colonia: Italian Life and Politics in Utica, NY, 1860–1985; Syracuse University Press: Syracuse, NY, 2005. [Google Scholar]
- Ciaglia, P.; Firshing, R.; Syniec, C. Elective percutaneous dilational tracheostomy, a new simple beside procedure: preliminary report. Chest 1985, 87, 815–819. [Google Scholar]
- Shelden, C.H.; Pudenz, R.H.; Freshwater, D.B.; Crue, B.L. A new method for tracheotomy. J Neurosurg 1955, 12, 428–431. [Google Scholar] [PubMed]
- Toy, F.J.; Weinstein, J.D. A percutaneous tracheostomy device. Surgery 1969, 65, 384–389. [Google Scholar]
- Smith, V.M. Perforation of trachea during tracheotomy performed with Sheldon tracheotome. J Am Med Assoc 1957, 165, 2074–2076. [Google Scholar]
- Byhahn, C.; Wilke, H.J.; Halbig, S.; Lischke, V.; Westphal, K. Percutaneous tracheostomy: Ciaglia blue rhino versus the basic Ciaglia technique of percutaneous dilational tracheostomy. Anesth Analg 2000, 91, 882–886. [Google Scholar]
- Bowen, C.P.; Whitney, L.R.; Truwit, J.D.; Durbin, C.G.; Moore, M.M. Comparison of safety and cost of percutaneous versus surgical tracheostomy. Am Surg 2001, 67, 54–60. [Google Scholar]
- Scultetus, J. Armamentarium Chirugicum; Kuhnen: Ulm, Germany, 1653. [Google Scholar]
- Trousseau, A. Memoire sur un cas de tracheotomie pratiquee dans la periode extreme de croup. J des Connaissance Medico-Chirurgicales. 1833, 1, 41. [Google Scholar]
- Browd, S.R.; MacDonald, J.D. Percutaneous dilational tracheostomy in neurosurgical patients. Neurocrit Care 2005, 2, 268–273. [Google Scholar]
- Pollock, R.A.; Dingman, R.O. Management and reconstruction of athletic injuries of the face, anterior neck and upper respiratory tract. In Sports Injuries: Mechanism, Prevention, and Treatment; Schneider, R.C., Kennedy, J.C., Plant, M., Fleming, W., Eds.; Williams & Wilkins Publishing Co: Baltimore, MD, 1985. [Google Scholar]
- Manson, P.N.; Clark, N.; Robertson, B.; Crawley, W.A. Comprehensive management of pan-facial fractures. J Craniomaxillofac Trauma 1995, 1, 43–56. [Google Scholar] [PubMed]
- Marcus, J.; Erdmann, D.; Rodriguez, E.D. Essentials of Craniomaxillofacial Trauma; Quality Medical: St. Louis, MO, 2012. [Google Scholar]
- Pollock, R.A. Craniomaxillofacial Buttresses: Anatomy and Operative Repair, Thieme Medical Publishing: New York, 2012.
- Pollock, R.A.; Purvis, J.M.; Apple DFJr Murray, H.H. Esophageal and hypopharyngeal injuries in patients with cervical spine trauma. Ann Otol Rhinol Laryngol 1981, 90 Pt 1, 323–327. [Google Scholar] [CrossRef] [PubMed]
- Yarmus, L.; Pandian, V.; Gilbert, C.; et al. Safety and efficiency of interventional pulmonologists performing percutaneous tracheostomy. Respiration 2012, 84, 123–127. [Google Scholar] [CrossRef] [PubMed]
- Patel, H.H.; Siltumens, A.; Bess, L.; Camacho, F.; Goldenberg, D. The decline of tracheotomy among otolaryngologists: a 14-year review. Otolaryngol Head Neck Surg 2015, 152, 465–469. [Google Scholar] [CrossRef]
© 2016 by the author. The Author(s) 2016.