Abstract
There is a lack of consensus regarding preferred implant materials for orbital floor fracture reconstruction, leading to surgeon- and institution-dependent preferences. A variety of implants are used for orbital floor fracture reconstruction, each with their own complication profile. Knowledge of different implant materials is critical to identifying complications when they present. We report a delayed periorbital abscess 5 years after orbital floor reconstruction using a silicone implant.
Orbital floor fractures are a common result of blunt trauma to the periorbital region []. Presenting signs and symptoms include periorbital edema and ecchymosis, enophthalmos, diplopia, subconjunctival hemorrhage, and facial deformity []. The highest risk group is men aged between 20 and 40 years [,]. Common mechanisms of injury include motor vehicle collisions, physical assault, and falls, with regional and demographic differences influencing the prevalence of each mechanism [].
Management of orbital floor fractures has been the subject of debate. Some authors have developed guidelines for observation versus surgical repair based on the presence of extraocular muscle entrapment, oculocardiac reflex, degree of diplopia or enophthalmos, and size of fracture and resulting defect []. However, specific parameters for signs and symptoms remain surgeon and institution dependent []. The primary goals of surgical reconstruction of orbital floor fractures are to restore orbital volume, reduce extraocular muscle entrapment, and prevent long-term enophthalmos and/or diplopia. If surgical reduction is indicated, orbital floor is reconstructed with autologous bone grafts, resorbable materials, or permanent implants []. Newer alloplastic implant materials (porous polyethylene and titanium) are used more frequently due to their safety and availability []. Knowledge of different materials used in reconstruction is essential when presented with implant-related complications. In this case report, we present a delayed implant-related periorbital abscess 5 years after orbital floor reconstruction with silicone.
Case Report
A 35-year-old man presented in February 2012 with a 2-day history of worsening left lower eyelid edema, erythema, and pain. He had previously suffered a traumatic left orbital floor fracture in 2005 for which he underwent surgical repair at an outside hospital. The operative details of the repair were not immediately available. The patient reported blurred vision in the left eye, but denied diplopia. On examination, his left lower eyelid was indurated, edematous, and erythematous (Figure 1). Visual acuity and extraocular movements were grossly intact, but proptosis and superior globe displacement was noted.

Figure 1.
Preoperative exam demonstrating erythema and edema of the left lower eyelid.
A CT sinus with contrast revealed a left-sided, rim-enhancing 1.9 × 0.9 cm mass consistent with an abscess just superior to previous surgical hardware (Figure 2). Superior displacement of the globe and medial displacement of the inferior rectus muscle were noted (Figure 2a). The patient was taken for a transconjunctival approach to the orbital floor. Drainage of the abscess revealed a mobile titanium screw. The floor implant made of a silicone sheet was partially secured by an additional retained screw (Figure 3). After drainage of the abscess cavity and removal of all infected hardware, the capsule surrounding the infected implant was gently debrided. The scar tissue from the prior repair appeared to support the orbital floor and no implant was replaced in the infected cavity.
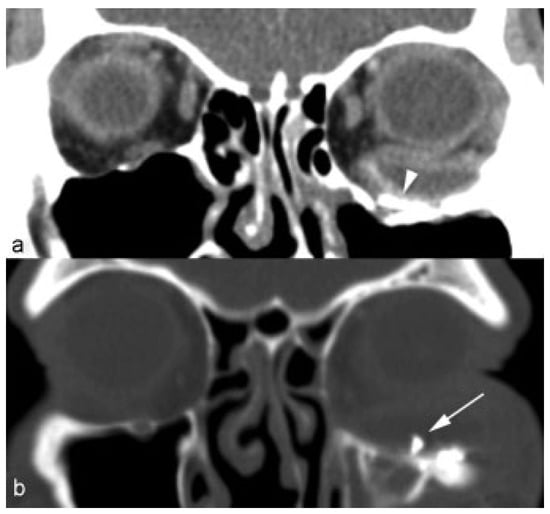
Figure 2.
Preoperative CT of face coronal sections with (a) soft-tissue window demonstrating periorbital abscess associated with a radiopaque implant (arrowhead) on the orbital floor. (b) Bone window demonstrates loose screw (arrow) within the abscess cavity.
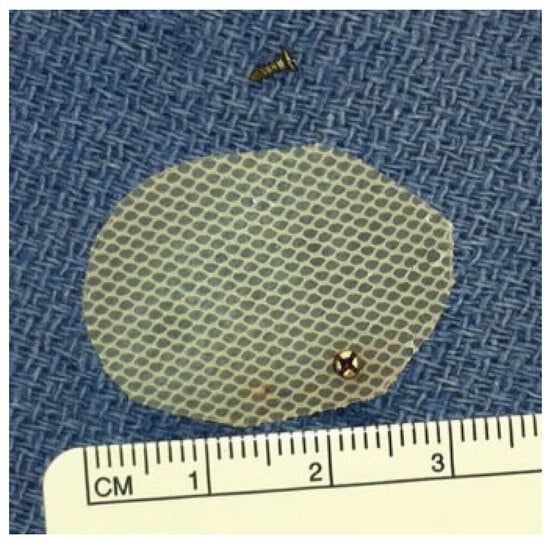
Figure 3.
Intraoperative image of removed silicone sheet and titanium screw.
Wound cultures revealed methicillin-sensitive Staphylococcus aureus, which was treated with intravenous (IV) clindamycin and IV ceftriaxone. Periorbital edema, erythema, and blurry vision resolved after a week of outpatient antibiotics. At 1-year follow-up, the patient reports no diplopia and demonstrates no gross asymmetry of the orbital position.
Discussion
Surgeons managing orbital floor fractures should be aware of the complication and risks of any material that they may prefer for floor reconstruction. There is a lack of consensus regarding the ideal material to be used []. Prospective, comparative studies in orbital floor fracture management are lacking due to lack of consensus on indications, timing, and materials to be used []. These different treatment paradigms create some controversy in orbital floor fracture management and the potential for delayed complications from materials such as silicone.
This report is consistent with and expands upon other publications reporting delayed infections due to silicone implant materials used on the orbital floor [,,,,]. Poor implant fixation, as demonstrated by the loose screw, can be problematic with any implant material. When orbital cellulitis or abscess is suspected, the authors suggest obtaining a history of prior orbital surgery (diagnosis, approach, and materials used). As seen in this case, removal of an infected silicone implant may leave adequate scar and implant capsule to obviate the need for revision orbital floor reconstruction. Patients should be counseled to comply with long-term follow-up focusing on orbital floor support, orbital volumes, and diplopia.
Complications from orbital floor implants may be identified more readily if the surgeon is familiar with the historical and current trends. Autologous grafts (e.g., calvarial bone or ear cartilage grafts) are less often chosen due to potential donor site morbidity [,,]. Allogenic materials such as lyophilized dura have the potential for disease transmission, while demineralized bone has shown high resorption rates [,].
There is an extensive list of implant options, but fewer materials are commonly used in practice. Both permanent (e.g., porous polyethylene, titanium) and resorbable (e.g., gel film, polydioxanone, poly L-lactide) materials are named in a recent study of members of the Canadian Society of Plastic Surgeons []. High-density porous polyethylene and/or titanium implants (or a composite of both) were preferred by 83% of surgeons. Only 5% preferred autologous bone or cartilage grafts. Silicone implants were used by only 4% []. A survey of oculoplastic surgeons from 14 countries in the Asia-Pacific region similarly found that porous polyethylene was the most preferred implant material [].
Surgeons have chosen to transition to porous polyethylene and titanium due to their readily availability, safety, and efficacy [,]. Vascular and tissue ingrowth into the pores (average size: 150 µm) of porous polyethylene implants may stabilize the implant and reduce infection rates [,]. Titanium mesh also has low infection rates and stability. A reported downside for both of these materials is the potential for scar adherence to periorbital tissues, which has been theorized to induce diplopia by limiting extraocular motion []. In contrast, silicone implants induce a fibrous capsule secondary to a foreign body reaction, and are prone to cysts, abscess formation, and extrusion due to contraction of the fibrous capsule [,].
The first reported use of silicone implants for orbital floor fracture repair was in 1963 by Lipshutz and Ardizone []. Numerous reports of silicone implant complications have led to a decline in its use. Morrison et al reported that 12% (n = 311) of silicone orbital implants required removal due to infection, implant migration or extrusion, and persistent edema []. Similarly, Laxenaire et al. expounded on the findings that lead to a 13.8% removal rate (n = 137), reasons for which included infection, implant migration, dacryocystitis, cutaneous fistulas, and persistent diplopia [].
Despite these findings, some reports describe success with silicone implants. Prowse et al published a comparative retrospective review of all orbital floor reconstructions (n = 81) at their hospital over a 12-year period []. Among patients with orbital floor fractures, those treated with silicone implants, compared with those treated with nonsilicone materials, had fewer palpable implants, patient complaints, and implant-related revision surgery []. The limitations of this study are striking, leading to weak generalizability. The non-silicone comparative group did not include porous polyethylene and include only four cases of titanium mesh. Additionally, the mean follow-up in the study was on average of 3.5 months, which would not identify the delayed complications of silicone implants [,,,,,].
Conclusion
Silicone implants used in orbital floor reconstruction can cause infection, implant migration, and abscess. While exposure of silicone implants to the maxillary sinus microbiome may contribute to infectious complications, this theory is less likely due to most infections occurring in a delayed fashion. In cases of orbital cellulitis or abscess, obtaining a history of prior orbital reconstruction is critical in identifying implantrelated infection. Practitioners should be knowledgeable in geographic patterns of the implant preferences for orbital floor reconstruction. After removal of an infected implant, additional reconstruction of the orbital floor may not be necessary, but at least a year of follow-up is recommended.
Note
No financial disclosures.
Conflicts of Interest
None.
References
- Converse, J.M.; Smith, B.; Obear, M.F.; Wood-Smith, D. Orbital blowout fractures: A ten-year survey. Plast Reconstr Surg 1967, 39, 20–36. [Google Scholar] [CrossRef] [PubMed]
- Gart, M.S.; Gosain, A.K. Evidence-based medicine: Orbital floor fractures. Plast Reconstr Surg 2014, 134, 1345–1355. [Google Scholar] [CrossRef]
- Ellis, E.I.I.I.; El-Attar, A.; Moos, K.F. An analysis of 2,067 cases of zygomatico-orbital fracture. J Oral Maxillofac Surg 1985, 43, 417–428. [Google Scholar] [CrossRef]
- Tong, L.; Bauer, R.J.; Buchman, S.R. A current 10-year retrospective survey of 199 surgically treated orbital floor fractures in a nonurban tertiary care center. Plast Reconstr Surg 2001, 108, 612–621. [Google Scholar] [CrossRef] [PubMed]
- Burnstine, M.A. Clinical recommendations for repair of orbital facial fractures. Curr Opin Ophthalmol 2003, 14, 236–240. [Google Scholar] [CrossRef] [PubMed]
- Alinasab, B.; Ryott, M.; Stjärne, P. Still no reliable consensus in management of blow-out fracture. Injury 2014, 45, 197–202. [Google Scholar] [CrossRef]
- Gunarajah, D.R.; Samman, N. Biomaterials for repair of orbital floor blowout fractures: A systematic review. J Oral Maxillofac Surg 2013, 71, 550–570. [Google Scholar] [CrossRef]
- Aldekhayel, S.; Aljaaly, H.; Fouda-Neel, O.; Shararah, A.W.; Zaid, W.S.; Gilardino, M. Evolving trends in the management of orbital floor fractures. J Craniofac Surg 2014, 25, 258–261. [Google Scholar] [CrossRef]
- Avashia, Y.J.; Sastry, A.; Fan, K.L.; Mir, H.S.; Thaller, S.R. Materials used for reconstruction after orbital floor fracture. J Craniofac Surg 2012, 23, 1991–1997. [Google Scholar] [CrossRef]
- Dougherty, W.R.; Wellisz, T. The natural history of alloplastic implants in orbital floor reconstruction: An animal model. J Craniofac Surg 1994, 5, 26–32, discussion 33. [Google Scholar] [CrossRef]
- Brown, A.E.; Banks, P. Late extrusion of alloplastic orbital floor implants. Br J Oral Maxillofac Surg 1993, 31, 154–157. [Google Scholar] [CrossRef]
- Lipshutz, H.; Ardizone, R.A. The use of silicone rubber in the immediate reconstruction of fractures of the floor of the orbit. J Trauma 1963, 3, 563–568. [Google Scholar] [CrossRef]
- Morrison, A.D.; Sanderson, R.C.; Moos, K.F. The use of Silastic as an orbital implant for reconstruction of orbital wall defects: Review of 311 cases treated over 20 years. J Oral Maxillofac Surg 1995, 53, 412–417. [Google Scholar] [CrossRef]
- Laxenaire, A.; Lévy, J.; Blanchard, P.; Lerondeau, J.C.; Tesnier, F.; Scheffer, P. Complications of Silastic implants used in orbital repair [in French]. Rev Stomatol Chir Maxillofac 1997, 98 (Suppl. S1), 96–99. [Google Scholar]
- Mok, D.; Lessard, L.; Cordoba, C.; Harris, P.G.; Nikolis, A. A review of materials currently used in orbital floor reconstruction. Can J Plast Surg 2004, 12, 134–140. [Google Scholar] [CrossRef] [PubMed]
- Koh, V.; Chiam, N.; Sundar, G. Survey of common practices among oculofacial surgeons in the Asia-Pacific region: Management of orbital floor blowout fractures. Craniomaxillofac Trauma Reconstr 2014, 7, 197–202. [Google Scholar] [CrossRef]
- Gear, A.J.; Lokeh, A.; Aldridge, J.H.; Migliori, M.R.; Benjamin, C.I.; Schubert, W. Safety of titanium mesh for orbital reconstruction. Ann Plast Surg 2002, 48, 1–7, discussion 7–9. [Google Scholar] [CrossRef] [PubMed]
- Lee., S.; Maronian, N.; Most, S.P.; et al. Porous high-density polyethylene for orbital reconstruction. Arch Otolaryngol Head Neck Surg 2005, 131, 446–450. [Google Scholar] [CrossRef]
- Prowse, S.J.; Hold, P.M.; Gilmour, R.F.; Pratap, U.; Mah, E.; Kimble, F.W. Orbital floor reconstruction: A case for silicone. A 12 year experience. J Plast Reconstr Aesthet Surg 2010, 63, 1105–1109. [Google Scholar] [CrossRef]
- Aboh, I.V.; Chisci, G.; Gennaro, P.; et al. Complications of orbital floor repair with silastic sheet: The skin fistula. J Craniofac Surg 2013, 24, 1288–1291. [Google Scholar] [CrossRef]
- Awan, M.A.; Cheung, C.M.; Sandramouli, S.; Mathews, J. An unusual late complication of orbital floor fracture repair. Eye (Lond) 2006, 20, 1454–1455. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Bourgault, S.; Bordua-Robert, M.F.; Molgat, Y.M. Recurrent orbital cyst as a late complication of silastic implant for orbital floor fracture repair. Can J Ophthalmol 2011, 46, 368–369. [Google Scholar] [CrossRef] [PubMed]
- Lee, D.H.; Joo, Y.E.; Lim, S.C. Migrated orbital Silastic sheet implant mimicking bilateral sinusitis. J Craniofac Surg 2011, 22, 2158–2159. [Google Scholar] [CrossRef]
- Warrier, S.; Prabhakaran, V.C.; Davis, G.; Selva, D. Delayed complications of silicone implants used in orbital fracture repairs. Orbit 2008, 27, 147–151. [Google Scholar] [CrossRef] [PubMed]
- Verma, S.; Garg, A.; Nastri, A. Orbitomaxillary mass after repair of the orbital floor. Br J Oral Maxillofac Surg 2014, 52, 977–979. [Google Scholar] [CrossRef]
© 2015 by the author. The Author(s) 2015.