Abstract
This paper describes the course of treatment of a severely diplaced bilateral mandibular body fracture, where the first osteosynthesis failed. The subject developed an open bite due to a posterior rotation of the distal part of the mandible and anterior rotation of the proximal parts of the mandible. This situation was evaluated with CBCT and the facial skeleton was segmented using computer software. Correct occlusion was virtually established by bilateral virtual osteotomies in the fracture areas of the mandible. After segmentation, the mandible was virtually rotated back into position and the open bite was closed. A patient specific mandibular reconstruction plate was outlined and fabricated from the new virtual situation and the plate was thereafter installed utilizing the preoperative plan. Osteotomy- and drill-guides was used and thus simplified the surgery resulting in uneventful healing. Virtual planning and patient specific implants and guides were valuable in this case of secondary reconstructive trauma surgery.
Bilateral mandibular body fractures may at times result in severely displaced fragments of the mandibular bone and occlusion derangements due to the muscular forces that act upon the jaw. Treatment of these fractures may, if the fracture pattern is considered as ”unfavorable,” require very rigid internal fixation [1]. Intraoral application of this type of osteosynthesis may at times be challenging and result in inadequate fixation. This paper describes such a situation in a case where revision surgery was virtually planned and executed with the help of computer software and fabrication of a patient specific implant (PSI).
Case Report
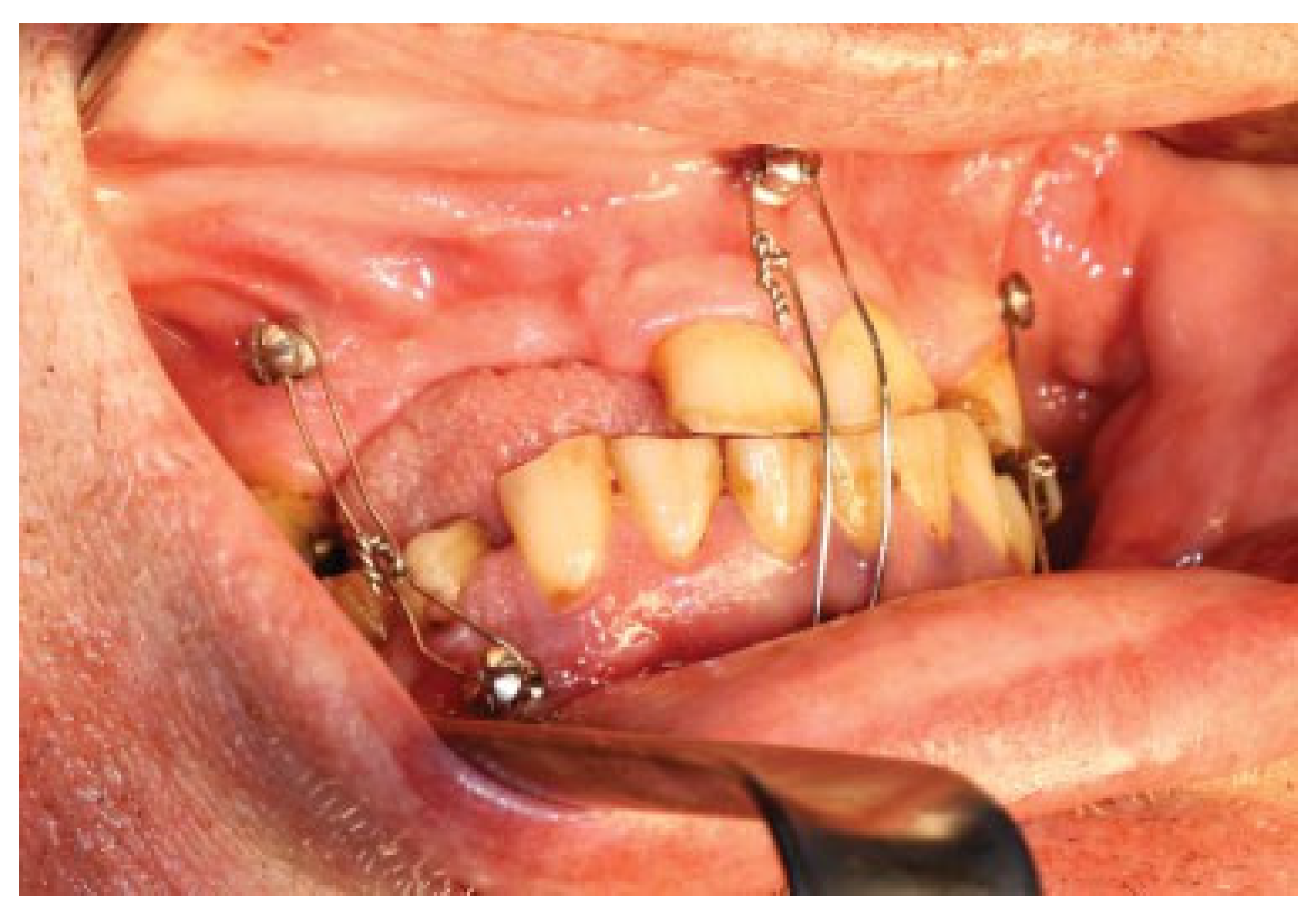
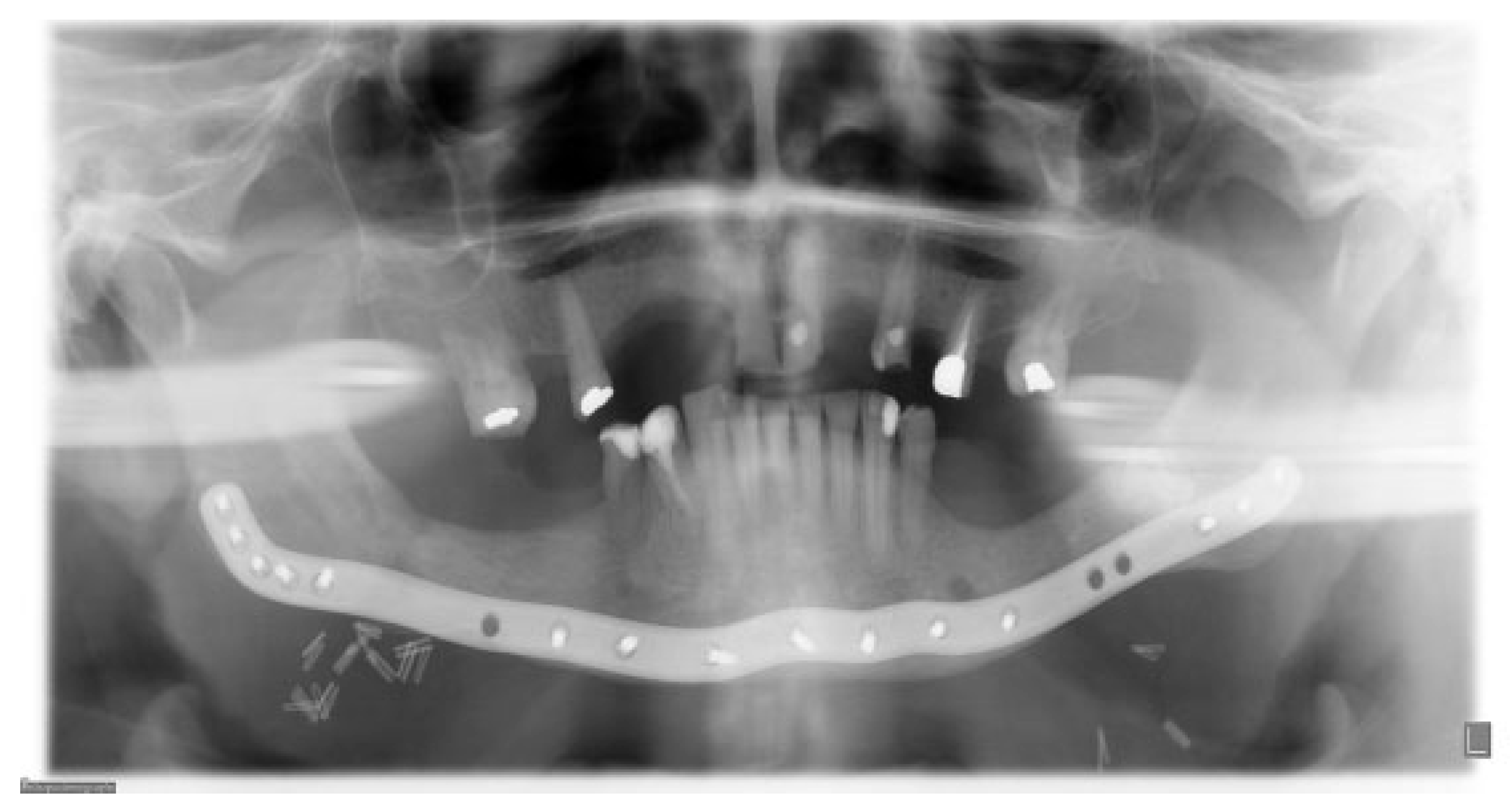
A 57-year-old man sustained a bilateral mandibular body comminute fracture due to a horse-kick trauma to his lower jaw. The subject was obese but otherwise healthy and due to the trauma omitted to the Uppsala University Hospital, Department of Oral & Maxillofacial Surgery. The anterior part of the mandible was severely displaced with a clinical open bite and the subject was taken from the Intensive care unit (ICU) to the Operating room (OR) after one night of monitoring. Partial edentulism was seen in both jaws (Figure 1). Open reduction and fixation of the fractures were performed via an intra-oral route. Noticeable was the difficulty in using a trocar due to the subjects’ constitution with abundance of soft tissue. Two mandibular plates were placed on each side and post-operative situation was evaluated with cone beam computed tomography (CBCT) (Figure 2). Initial healing was uneventful and the patient was not held in maxillo-mandibular fixation (MMF). At the two-week follow-up intraoral fistulas were found in the area of fractures and instability of the osteosynthesis occurred with opening of the bite as a result. The subject was scheduled for secondary surgery and meanwhile oral antibiotics (phenoxymethyl penicillin and metronidazole) were prescribed.
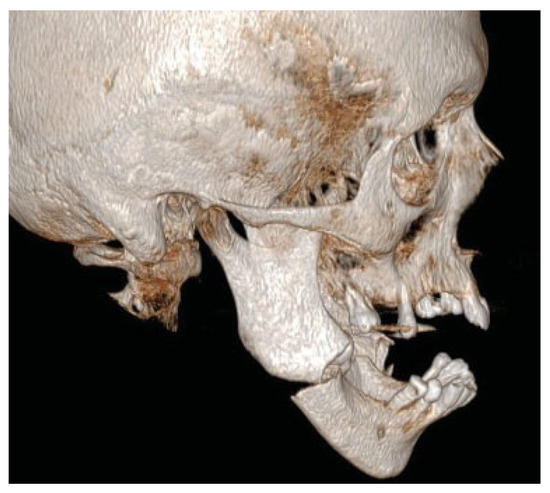
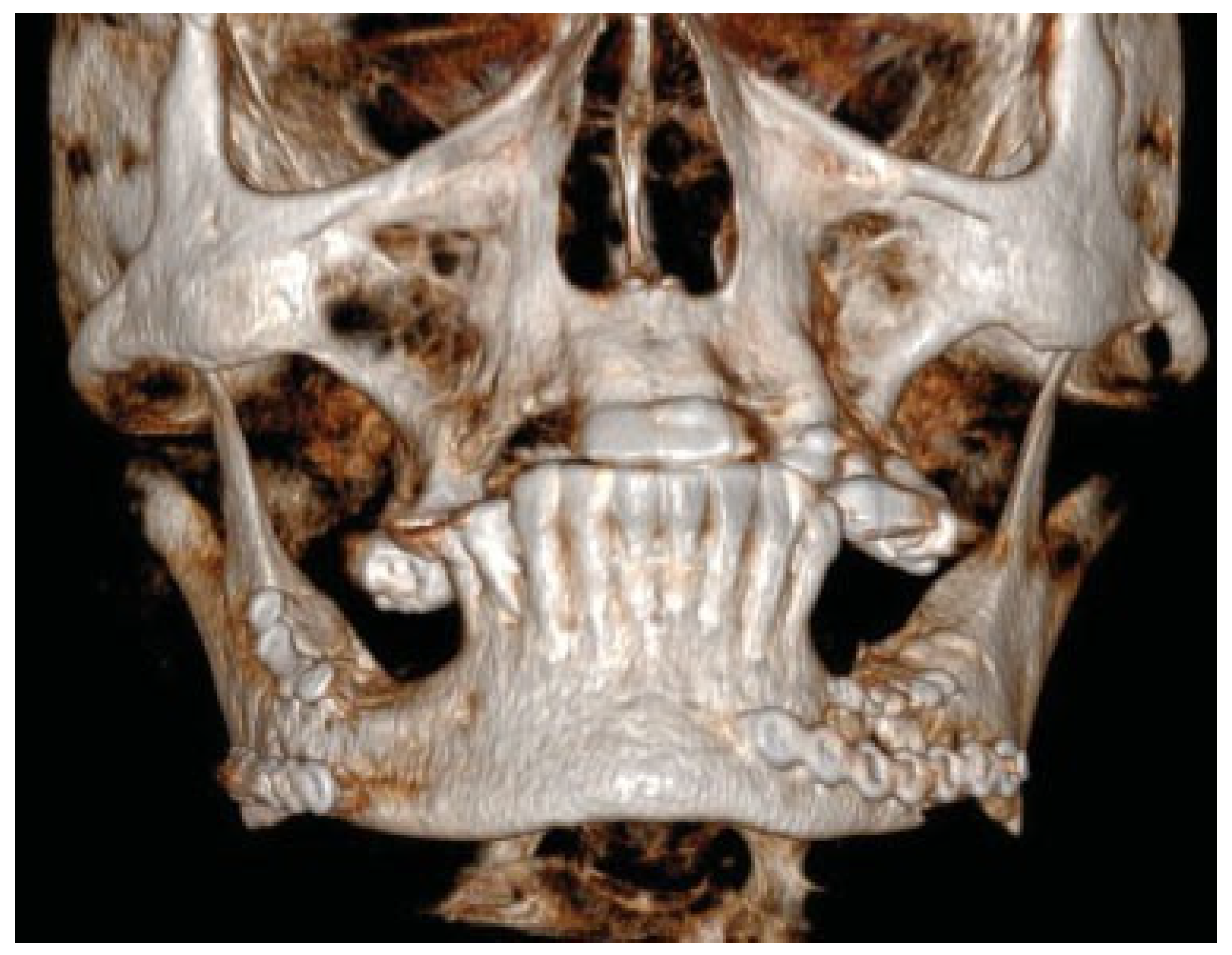
Figure 1.
Preoperative situation. Displaced bilateral mandibular body fracture after trauma by a horse-kick.
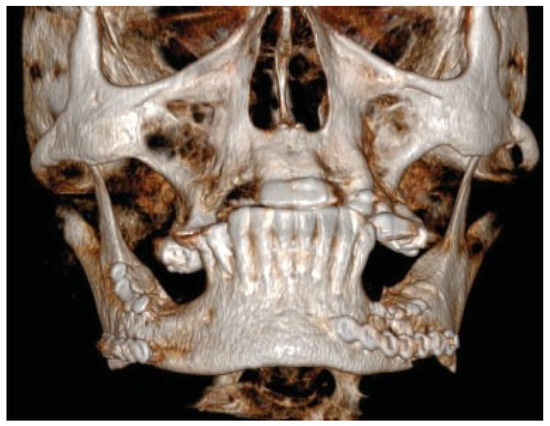
Figure 2.
Post-operative situation after bilateral intraoral plate fixation and placements of basal screws via trocar.
Imaging and Virtual Planning
New imaging of the lower face and maxilla was performed (Figure 3). Digital Imaging and Communications in Medicine (DICOM) data was uploaded and the case was planned in the computer software PRO Plan CMF (Materialise Inc., Leuven, Belgium). The facial skeleton was segmented and the dislocated parts of the mandible could thereafter be corrected by virtual surgery. Existing plates and screws were removed in the computer software and osteotomies were performed in the areas of the non-healing bilateral fracture sites. The proximal two ramus fragments were posteriorly rotated 4 degrees backward and the distal tooth-bearing segment was anteriorly rotated to reach its original occlusion and close the bite (Figure 4). The planned outcome was decided and finalized in a web-videoconference between the responsible surgeon in Sweden and the medical engineer at Materialise in Belgium.

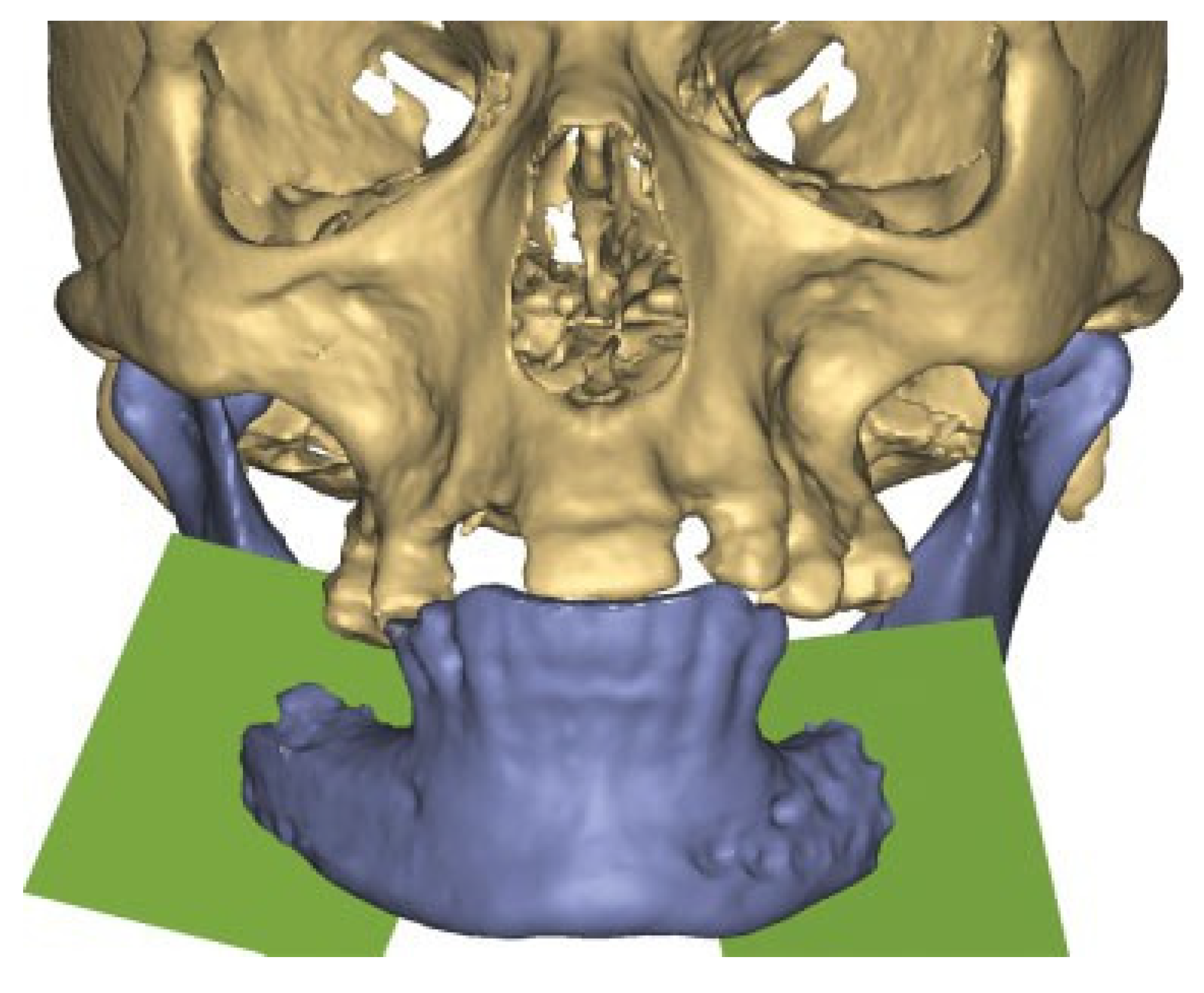
Figure 3.
Patient developed infections with oral mucosal fistulas in the fracture areas and an open bite. CBCT displays obvious anterior rotation of proximal segments and posterior rotation of the dentate part of mandible. Considerable muscle action creates new dislocation and is not counteracted by the inadequate osteosynthesis of the fractures.
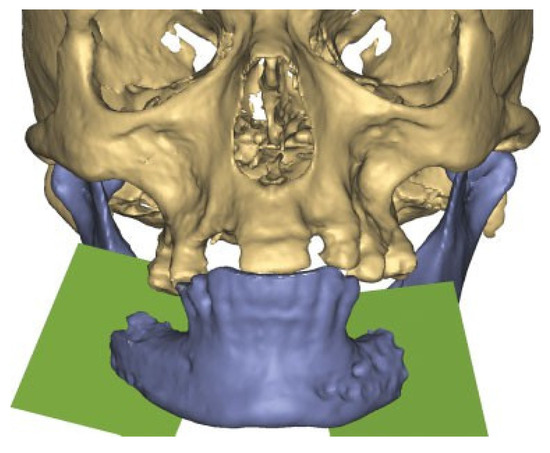
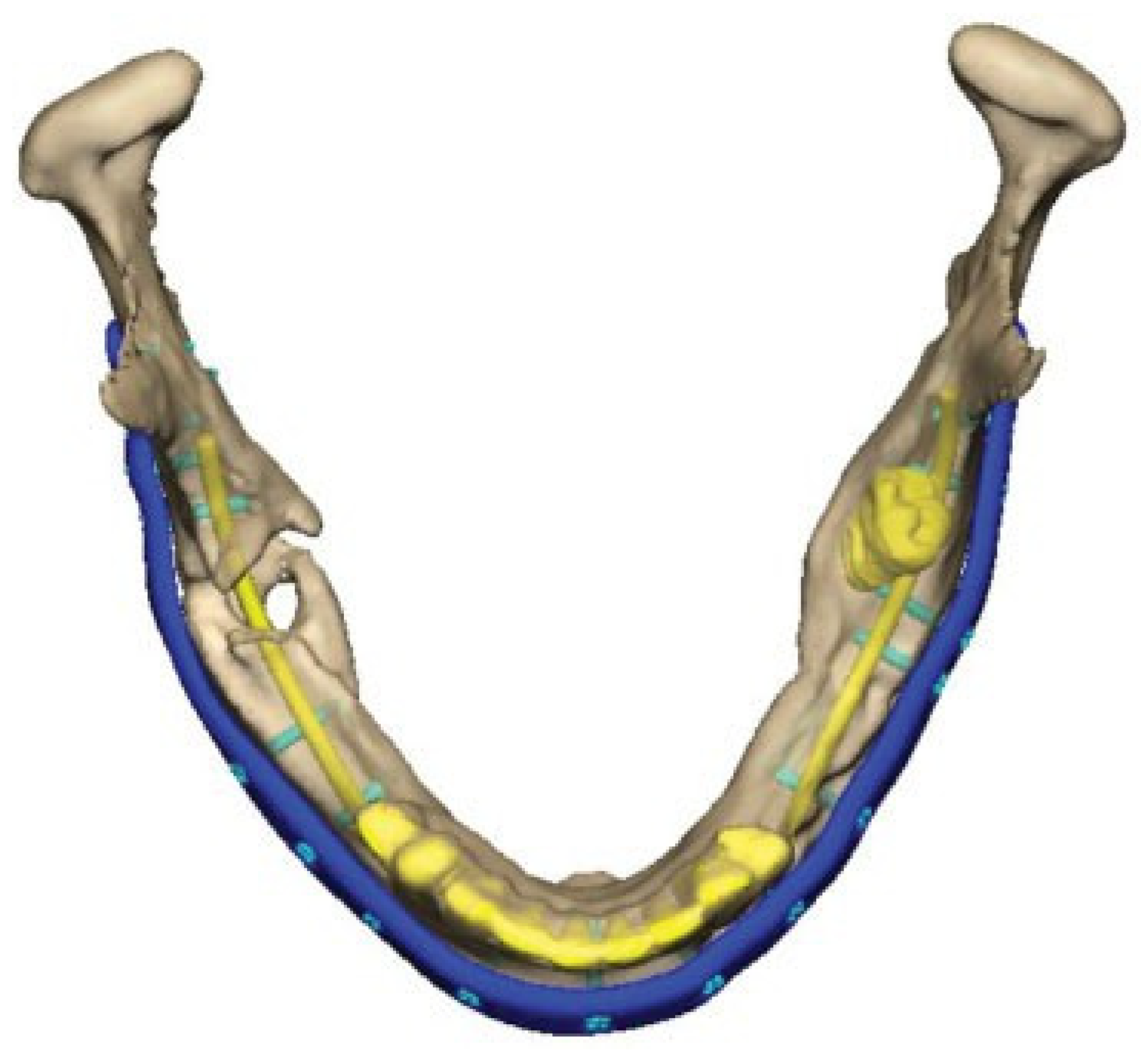
Figure 4.
After plate removal in the software, osteotomies in the fracture areas and corrective rotation of displaced fragments was performed to close the open bite and restore the occlusion in the virtual plan.
Implant and Corrective Surgery
A Patient Specific Implant (PSI), an angle-to-angle mandibular reconstruction plate, was designed and outlined along the mandibular border. Plate holes with locking function for screws were outlined. The dimension of the plate was 2.5 mm thick and 8 mm wide. A total of 18 screw-holes were placed with care taken to avoid the fracture areas, teeth and nerves. (Figure 5) Simultaneously, a combined cutting- and drill guide was produced for osteotomies and drill holes virtually planned in the mandible. (Figure 6) The plate was then manufactured by milling from a titanium block (TRUMATCH® CMF, DePuy Synthes GmbH, Oberdorf, Switzerland) after the surgeon had approved its final form.
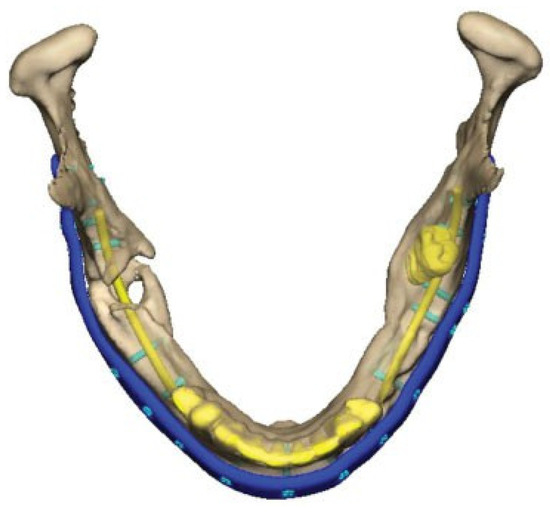
Figure 5.
Virtual design of plate and planning of holes and screw locations. Note the screws in the posterior left mandible avoiding the mandibular nerve and molar inside the bone.
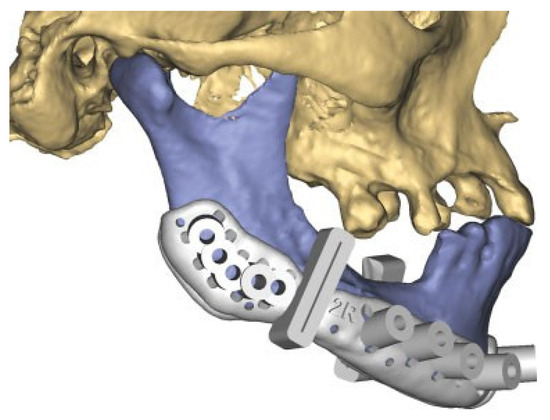
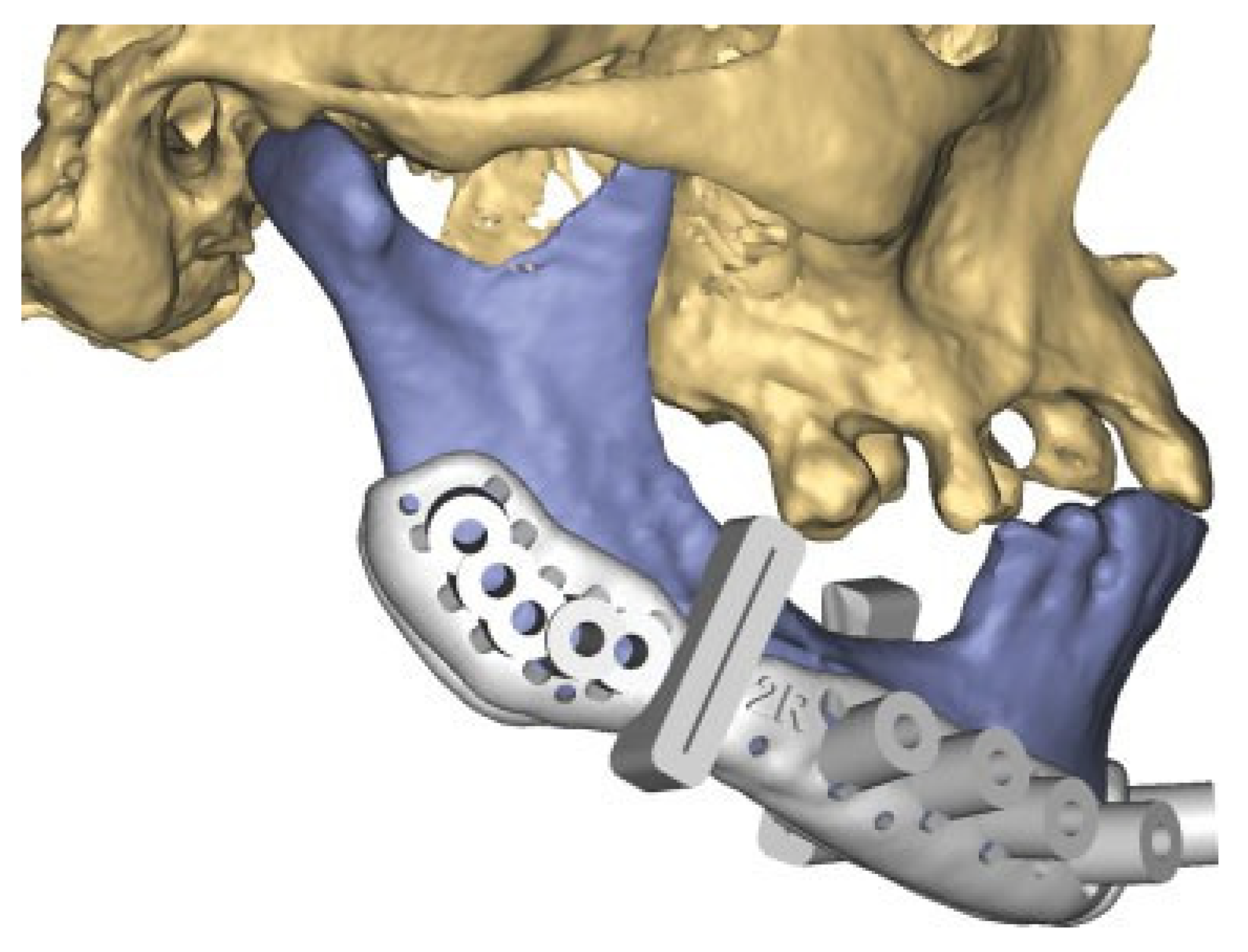
Figure 6.
Guide for osteotomies and screw holes (right side).
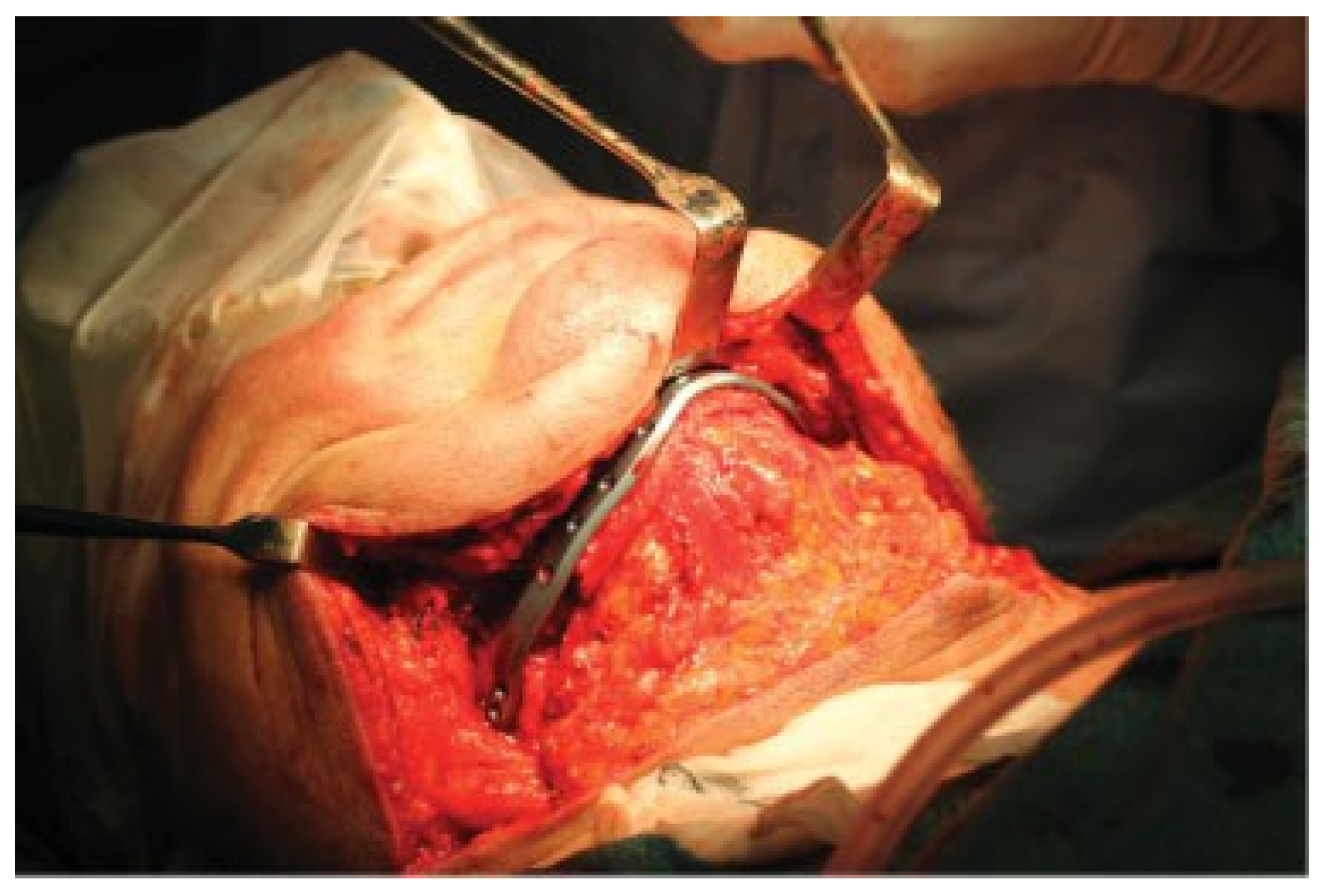
The secondary correction was performed via an extra-oral, wide exposure of the mandible (Figure 7). The failing osteosynthesis material was removed. The area of osteotomies (not needed to perform cuts due to bone resorption from infection) and screw-holes were outlined and placed with the help of the previously virtually planned surgical guides (Figure 8). The subject was placed in MMF with screws (Figure 9). The necrotic tissue was cleared out from the area of the fractures bilaterally. The open bite was corrected by the pre-planned rotations of the segments in the area of the virtual osteotomies and proper occlusion was established. By placing the subject in MMF, the rotations of the displaced segments were enhanced, these included 4 degrees posterior rotation of the two proximal segments and anterior rotation of the anterior segment to alignment of the mandibular border. The mandibular position was secured by the installation of the PSI-plate, displaying an exact fit to the mandibular border, and the already drilled holes and by placing the screws of planned length (Figure 5). In this way, holes and screws worked together as multiple guides in moving the segments into their planned correct position along a perfect match under the plate (Figure 10). An iliac-crest graft of cortico-cancellous bone was harvested and placed into the bilateral defects. Oral fistulas were closed and the wide flap over the neck was repositioned in layers using resorbable sutures in the sub-cutaneous tissue and with staples in the skin. MMF was removed and occlusion found in order as planned. Healing was thereafter uneventful and a stable situation and a good occlusion have been seen on all follow-ups until the latest at 10 months post-op (Figure 11, Figure 12 and Figure 13).

Figure 7.
Wide extra-oral exposure of the mandible, removal of plates and granular tissue in the fracture areas. Outcome model and PSI is displayed.

Figure 8.
3-D printed surgical guide for drilling holes and indicating area for osteotomies placed onto the bone on the right side of the mandible (repeated on the left side with the left surgical guide).
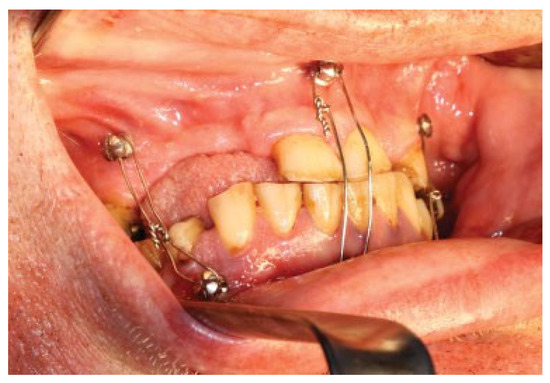
Figure 9.
The patient was placed in MMF during the procedure, enhancing the planned virtual rotations of segments in real life (posterior rotations of the proximal segments 4 degrees and anterior rotation of the distal segment of the mandible).
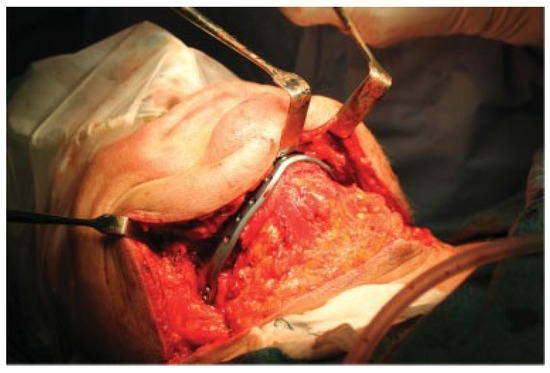
Figure 10.
After drilling holes with the help of the guide, the plate was easily attached in the planned position to the mandible.

Figure 11.
Immediate postoperative situation captured with CBCT.
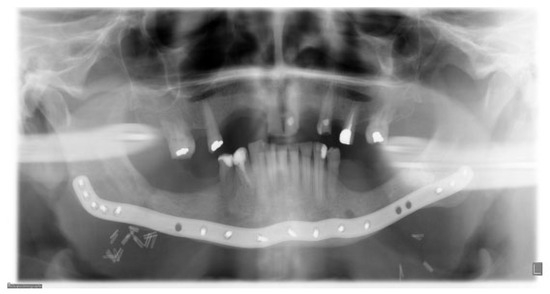
Figure 12.
Six months follow-up. Clinical and radiological healing is seen in the previous fracture areas in the region of the first molar on both sides of the mandible.

Figure 13.
Occlusion at 6 months follow-up.
Discussion
This paper describes and exemplifies the simplicity and advantages seen with virtual surgical planning in an elective case of a mandible fracture needing revision surgery. The final clinical outcome was appropriate and the surgical procedure facilitated and shortened. In the literature today, Virtual surgical planning (VSP) is commonly described [2,3,4], but the fabrication of PSI for this indication has so far not often been described [5].
The time elapsing from the moment of trauma until surgery is an important issue in maxillofacial trauma surgery. In many centres, the trauma-service and available resources do not allow for immediate surgical treatment of incoming cases with facial fractures. Other injuries and comorbidities in the subject may also necessitate a delay in repair of the facial fractures, creating a time-window and enabling possibility for manufacturing patient specific implants for fixation.
Previously, bending of reconstruction plates was always done by hand; either preoperatively on a stereolithographic model, or during surgery after reduction of the segments [6].
Our experience with VSP goes back to 2008, when we first started planning and attaining cutting guides for free fibula flaps in tumor reconstructive cases with the use of VSP [7]. In that sense, we have through these years and many cases of mandibular and TMJ reconstructive cases learned to trust this technology. The workflow for fabrication of a PSI starts with attaining DICOM-files for loading into the planning software. CBCT, as a complement to computed tomography (CT), has for the last decade been a useful tool in diagnosis and follow-up of facial fractures at our institution [8]. For this case we used a commercially available partner for the virtual planning. After a data-file with the plan and the virtual implant has been created, the next step is to find a manufacturer for the implant. To continuously hold this resource available is demanding and costly, with difficulties in estimating the amount of cases over a certain period of time. This fact may be illustrated in the partnership of Materialise and DePuy Synthes responsible for manufacturing the implant described here.
Over the years, the evolution of the software has been fast and the interface where engineering meets surgical expertise has also become more sophisticated. Surgeons can now choose to focus on the plan and less on technical issues such as difficult segmentation and computer associ- ated matters. The availability and cost for this workflow is of course a problem and puts limits to its use in certain parts of the world. To increase the use of PSI:s, the workflow would favorably be aimed at keeping the software and engineering support in-house in the hospital close to the patients. This means that centres must either have a large volume of cases and/or involve many specialties (e.g., maxillofacial-, plastic-, orthopaedic-, neuro- and hand surgery) that will use the system and contribute with resources. Additive manufacturing (AM) of various surgical implants is therefore an interesting area of research and development in craniofacial reconstructive surgery [9,10,11]. With the fast evolution of imaging and linking to 3-D printing the future for this area is promising [12].
In this paper, the implant was cut out from a solid piece of titanium. This milling technique is time consuming and costly, but the result was in this case striking with a very exact fit to the bone of both the surgical guides and of the implant. Even though this described case had a substantial number of missing teeth in both jaws, the central incisors and the remaining teeth were sufficient indicators of correct occlusion during surgery and for evaluating a good outcome at follow-up as seen in the illustrations. Making of cuts through the slots in the surgical guides were not needed as the infection had taken care of this step. This fact does not alter the advantage of planning the surgery virtually and to prefabricate a plate for realignment of the mandible and performing a very rigid and anatomically favorable osteosynthesis in the revision surgery.
In other areas of reconstructive maxillofacial surgery, e.g., allogeneic total joint reconstructions (TJR), implants are often custom-made with the obvious advantage of the implant being shaped for the patient, but still with the large disadvantage of very high costs [13]. Orthognathic surgery is another area that have come to use VSP routinely in many centres [14]. In an elective setting for surgical intervention with meticulous preoperative planning that represents this surgical field, fabrication of cutting guides and fabrication of implants for fixation must be a favorable path for successful and predictable procedures [15,16]. And ultimately, the need for VSP in facial transplantation surgery, or vascularized composite allotrans-plantation (VCA), has been clearly emphasized in reports from several centres [17,18,19].
Indeed, there remain some areas of refinement to this technique, e.g., the problem with artifacts from dental fillings in CT/CBCTscans. Intraoral laser scanning of the occlusion and the segmentation of data files from scanning and DICOM-data into a 3-D computer model of the craniofacial area may offer a solution to this problem and an area where research is undertaken at the moment [20].
Conclusion
Surgical revision in the case described in this report was facilitated by the use of preoperative virtual surgical planning, virtual osteotomies, adjustment of displaced segments and the fabrication of a patient specific implant for fixation of a bilateral mandibular body fracture.
Acknowledgments
The author wishes to thank Maria Isabel Osorio Garcia, Clinical Engineer, Materialise, Leuven, Belgium, for assisting in planning of the case and for help with illustrations.
References
- Rudderman, R.H.; Mullen, R.L.; Phillips, J.H. The biophysics of mandibular fractures: An evolution toward understanding. Plast Reconstr Surg 2008, 121, 596–607. [Google Scholar] [CrossRef] [PubMed]
- Bai, S.; Shang, H.; Liu, Y.; Zhao, J.; Zhao, Y. Computer-aided design and computer-aided manufacturing locating guides accompanied with prebent titanium plates in orthognathic surgery. J Oral Maxillofac Surg 2012, 70, 2419–2426. [Google Scholar] [CrossRef] [PubMed]
- Hirsch, D.L.; Garfein, E.S.; Christensen, A.M.; Weimer, K.A.; Saddeh, P.B.; Levine, J.P. Use of computer-aided design and computer-aided manufacturing to produce orthognathically ideal surgical outcomes: A paradigm shift in head and neck reconstruction. J Oral Maxillofac Surg 2009, 67, 2115–2122. [Google Scholar] [CrossRef] [PubMed]
- Juergens, P.; Krol, Z.; Zeilhofer, H.F.; et al. Computer simulation and rapid prototyping for the reconstruction of the mandible. J Oral Maxillofac Surg 2009, 67, 2167–2170. [Google Scholar] [CrossRef] [PubMed]
- Tepper, O.M.; Sorice, S.; Hershman, G.N.; Saadeh, P.; Levine, J.P.; Hirsch, D. Use of virtual 3-dimensional surgery in post-traumatic craniomaxillofacial reconstruction. J Oral Maxillofac Surg 2011, 69, 733–741. [Google Scholar] [CrossRef]
- Kernan, B.T.; Wimsatt, J.A.I.I.I. Use of a stereolithography model for accurate, preoperative adaptation of a reconstruction plate. J Oral Maxillofac Surg 2000, 58, 349–351. [Google Scholar] [CrossRef]
- Leiggener, C.; Messo, E.; Thor, A.; Zeilhofer, H.F.; Hirsch, J.M. A stereolithography (SLA) guide for transferring a virtual plan to real time surgery in composite mandibular reconstruction with free fibula osseous flaps. Int J Oral Maxillofac Surg 2009, 38, 187–192. [Google Scholar] [CrossRef]
- Palomo, L.; Palomo, J.M. Cone beam CT for diagnosis and treatment planning in trauma cases. Dent Clin North Am 2009, 53, 717–727, vi–vii. [Google Scholar] [CrossRef] [PubMed]
- Lethaus, B.; Poort, L.; Böckmann, R.; Smeets, R.; Tolba, R.; Kessler, P. Additive manufacturing for microvascular reconstruction of the mandible in 20 patients. J Craniomaxillofac Surg 2012, 40, 43–46. [Google Scholar] [CrossRef] [PubMed]
- Mangano C, Mangano F, Shibli JA; et al. Prospective clinical evaluation of 201 direct laser metal forming implants: Results from a 1-year multicenter study. Lasers Med Sci 2012, 27, 181–189. [Google Scholar] [CrossRef] [PubMed]
- Mangano F, Macchi A, Shibli JA; et al. Maxillary ridge augmentation with custom-made CAD/CAM scaffolds. A 1-year prospective study on 10 patients. J Oral Implantol 2014, 40, 561–569. [Google Scholar] [CrossRef]
- Tevlin R, Atashroo D, Duscher D; et al. Impact of surgical innovation on tissue repair in the surgical patient. Br J Surg 2015, 102, e41–e55. [Google Scholar] [CrossRef]
- Aagaard, E.; Thygesen, T. A prospective, single-centre study on patient outcomes following temporomandibular joint replacement using a custom-made Biomet TMJ prosthesis. Int J Oral Maxillofac Surg 2014, 43, 1229–1235. [Google Scholar] [CrossRef] [PubMed]
- Stokbro, K.; Aagaard, E.; Torkov, P.; Bell, R.B.; Thygesen, T. Virtual planning in orthognathic surgery. Int J Oral Maxillofac Surg 2014, 43, 957–965. [Google Scholar] [CrossRef] [PubMed]
- Levine, J.P.; Patel, A.; Saadeh, P.B.; Hirsch, D.L. Computer-aided design and manufacturing in craniomaxillofacial surgery: The new state of the art. J Craniofac Surg 2012, 23, 288–293. [Google Scholar] [CrossRef]
- Aboul-Hosn Centenero, S.; Hernández-Alfaro, F. 3D planning in orthognathic surgery: CAD/CAM surgical splints and prediction of the soft and hard tissues results—Our experience in 16 cases. J Craniomaxillofac Surg 2012, 40, 162–168. [Google Scholar] [CrossRef] [PubMed]
- Bojovic B, Dorafshar AH, Brown EN; et al. Total face, double jaw, and tongue transplant research procurement: An educational model. Plast Reconstr Surg 2012, 130, 824–834. [Google Scholar] [CrossRef]
- Roche NA, Vermeersch HF, Stillaert FB; et al. Complex facial reconstruction by vascularized composite allotransplantation: The first Belgian case. J Plast Reconstr Aesthet Surg 2015, 68, 362–371. [Google Scholar] [CrossRef] [PubMed]
- Fernandez-Alvarez, J.A.; Infante-Cossio, P.; Barrera-Pulido, F.; et al. Virtual reality AYRA software for preoperative planning in facial allotransplantation. J Craniofac Surg 2014, 25, 1805–1809. [Google Scholar] [CrossRef] [PubMed]
- Nilsson, J.; Thor, A.; Kamer, L. Development of workflow for recording virtual bite in the planning of orthognathic operations. Br J Oral Maxillofac Surg 2015, 53, 384–386. [Google Scholar] [CrossRef] [PubMed]
© 2016 by the author. The Author(s) 2016.