Septal perforations affect around 1% of the general population. They may arise from numerous etiologies, including idiopathic, infectious, traumatic, inflammatory, or drug induced and are most commonly iatrogenic in nature. Symptomatic patients may present with complaints associated with disruption of laminar nasal airflow, such as mucosal crusting and desiccation, epistaxis, whistling, and nasal airway obstruction depending on the size and location of the perforation [
1]. Asymptomatic perforations are commonly untreated.
Treatment of a symptomatic perforation ranges from conservative treatment with moisturizing agents, placement of a prosthetic button, to surgical management. The goal of surgical treatment is to restore functional laminar flow in the nasal airway by reconstructing the perforation using local pedicled mucosal flaps with or without free interpositional grafts [
2]. Surgical management of septal perforations remains challenging for otolaryngologists. Multiple techniques have been described, with reproducibility of outcomes depending on both patient factors and experience of the surgeon. Perforations larger than 2 cm have been associated with increased rates of failures [
3].
The pericranium provides a robust source of native vascularized tissue that is commonly used in the reconstruction of the anterior skull base. Paloma et al previously described the use of a pericranial flap for repair of a single, large, anterior septal perforation [
4]. The aim of our study was to present our experience with this technique and furthermore to describe our use of intraoperative angiography using laser-assisted indocyanine green imaging to confirm flap perfusion.
Case Report
A 31-year-old man presented to the senior author’s (S.M.) clinic for repair of a septal perforation. He had previously undergone an attempted surgical repair by an outside surgeon which was unsuccessful. His past medical history was significant only for a history of allergic rhinitis treated with nasal steroid sprays, and he denied any illicit drug use. An autoimmune workup had been completed previously and was unremarkable.
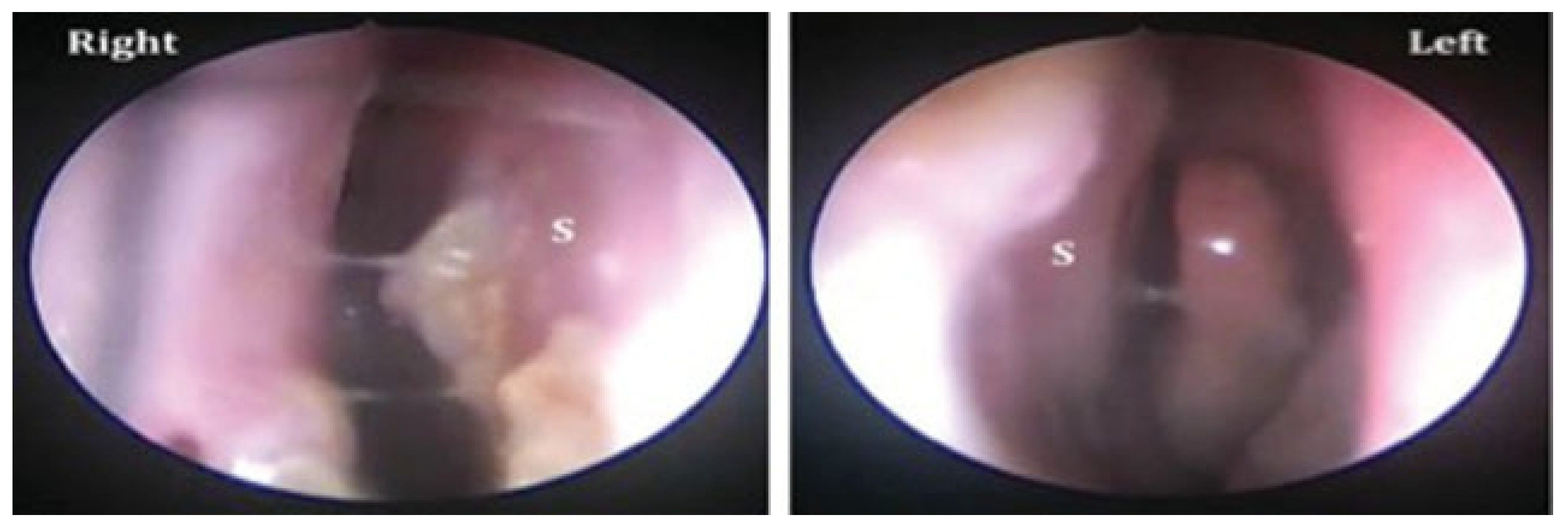
On examination, the perforation was noted to be anterior in location, measuring 1.7 cm × 1.7 cm (
Figure 1). The patient was taken to the operating room and a septal perforation repair was performed using a combination of a standard external rhinoplasty approach and a tunneled pericranial flap harvested through a coronal incision (see section “Surgical Technique” for details). Intraoperatively, the viability of the pericranial flap was confirmed using intraoperative laser angiography using the SPY system. The patient was admitted for pain control and wound management. He was discharged on postoperative day 5. Intranasal Silastic splints were left in place for 21 days postoperatively. Nasal endoscopy performed at 3 months follow-up demonstrated complete closure of perforation with mild mucosal crusting (
Figure 1). Follow up at 1, 3, and 10 weeks confirmed a stable repair with well-healed mucosa and no evidence of recurrent perforation. Follow up at 5 years revealed a completely healed repair.
Surgical Technique
The septum is first exposed using a left-sided hemitransfixion incision and a left submucoperichondrial flap is elevated releasing the edges of the perforation circumferentially. This dissection is then carried around the anterocaudal septum, and elevation of the contralateral submucoperichondrial flap is performed in the same plane. A standard external rhinoplasty approach is then performed using transcolumellar and marginal incisions for maximum exposure. The upper lateral cartilages are then released from the dorsal septum, allowing the surgeon access to the septum and septal perforation from above. A coronal incision is then performed and carried down to the deep temporal fascia laterally and superficial to the pericranium in the central compartment. The scalp is then elevated anteriorly toward the orbital rim, sharply dividing the conjoint tendon and staying deep to the frontal branch of the facial nerve.
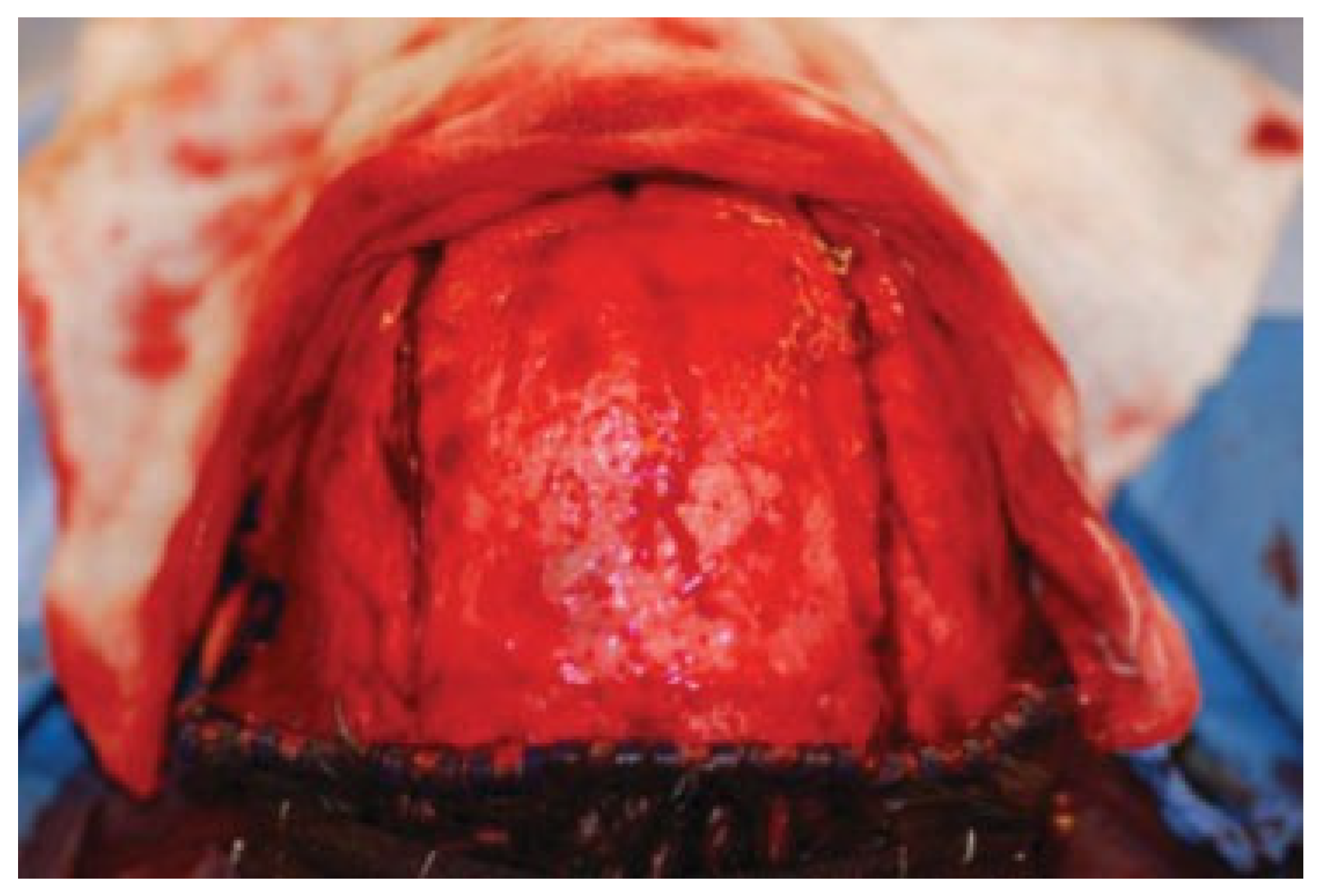
A rectangular pericranial flap pedicled on the supratrochlear vessels is designed (
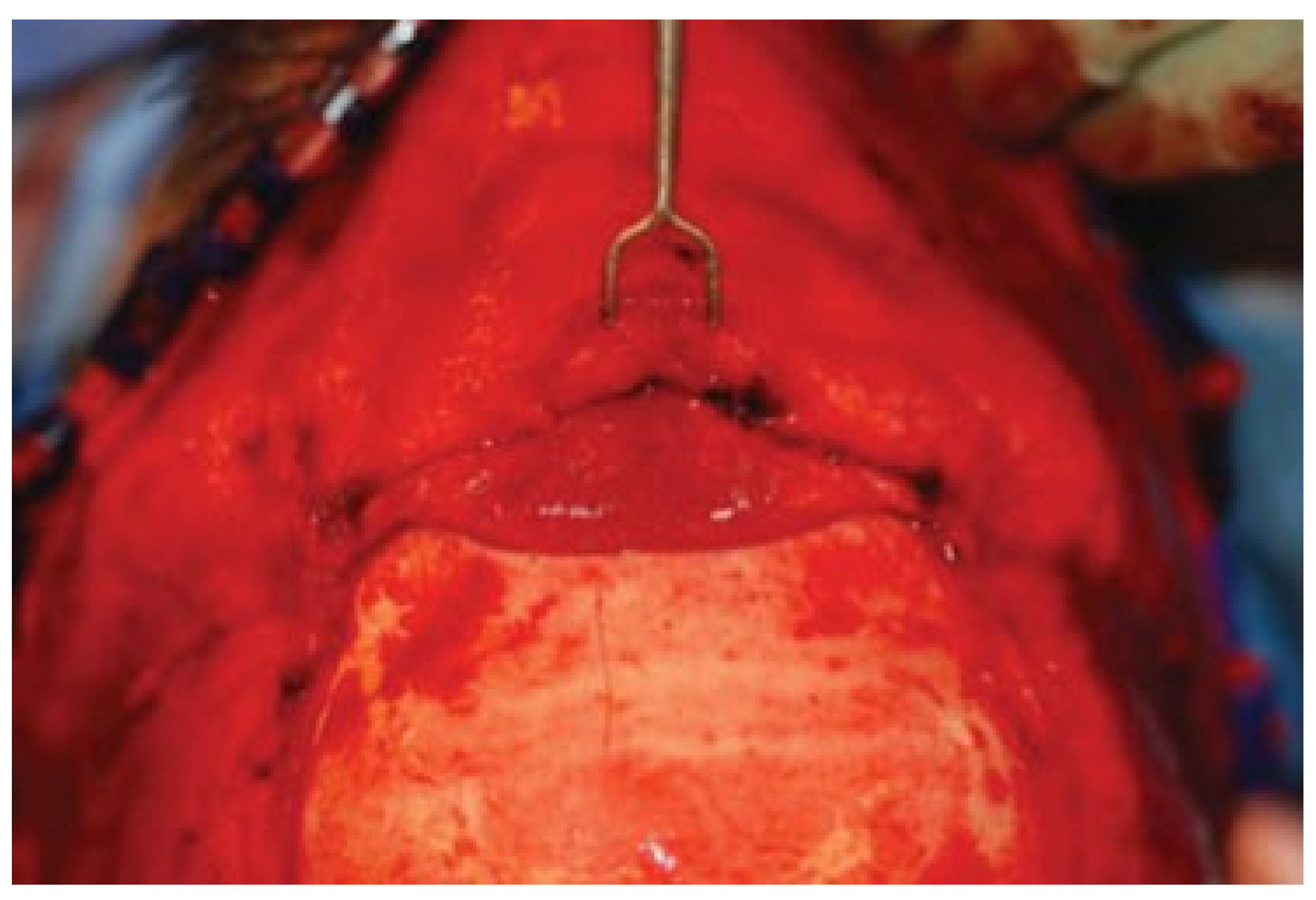
Figure 3) and incised with electrocautery, followed by elevation with a Cottle elevator. Through the external rhinoplasty approach, the nasal skin and soft-tissue envelope is then elevated superiorly in the subcutaneous plane and connected to the superior dissection. The tunnel is widened to 3 cm at the nasofrontal area appropriately and the flap passed through this into the nasal cavity (
Figure 4 and
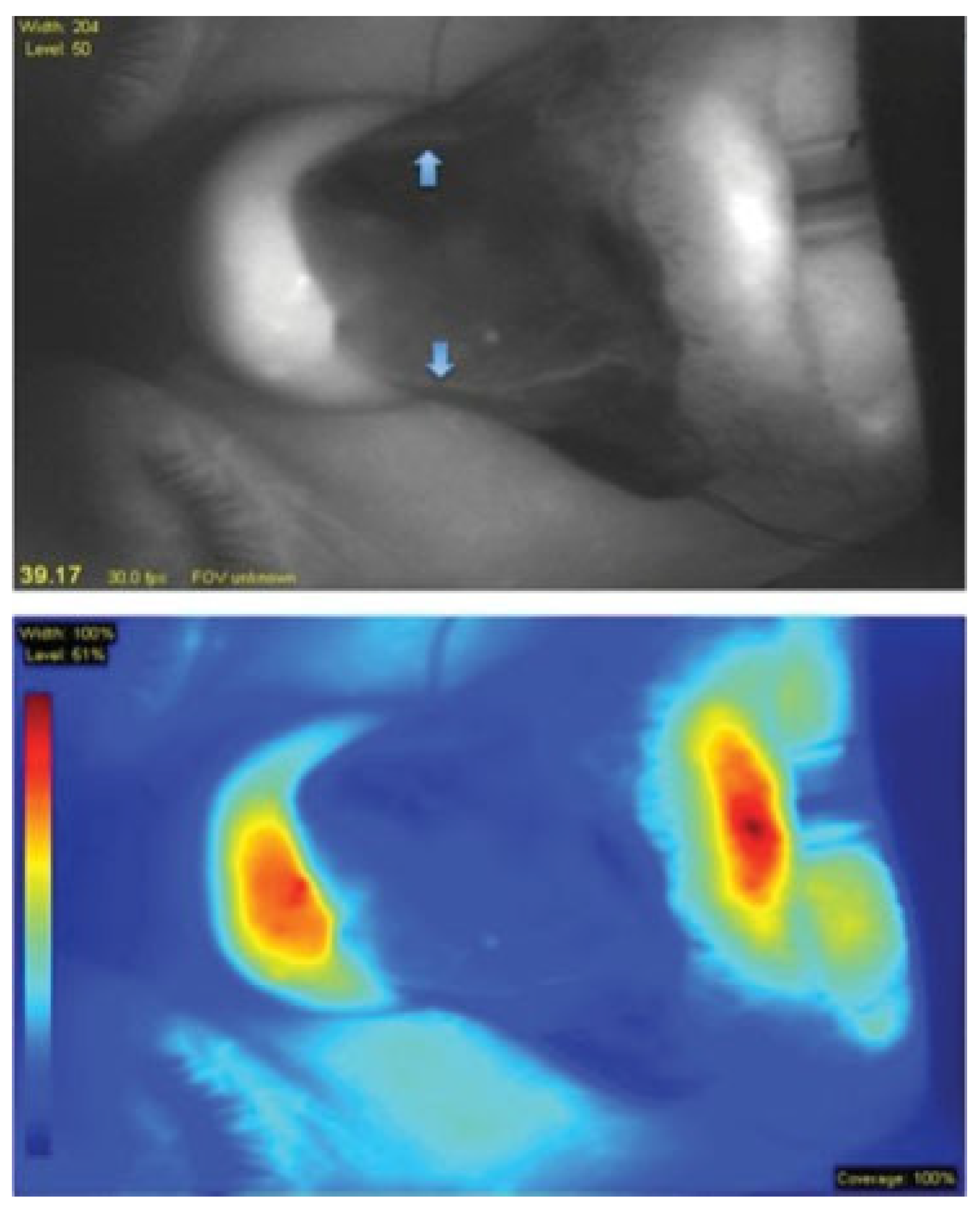
Figure 5). The narrowest point is at the nasal dorsum at approximately 2 cm. Intra-operative laser angiography with the SPY system is performed to verify distal perfusion of the flap (
Figure 6).
The central septal perforation was elevated along all of its edges and onto the floor. The flap is then placed over the perforation and its edges are tucked underneath the elevated mucoperichondrium on both sides providing complete coverage of the septal perforation in a double layer. The pericranial flap is then sutured in place using interrupted 5–0 chromic gut sutures as well as a 4–0 plain gut mattress suture. The hemitransfixion, margin, columellar, and coronal incisions are then closed in standard fashion. Bilateral Doyle splints are placed taking care not to disrupt the pericranial flap, and sutured securely to the septum using a 4–0 nylon suture.
Discussion
The repair of septal perforations is a challenging endeavor, as the treating physician must take into account the etiology, location, size, patient considerations, and availability of reconstructive options when formulating a treatment plan. Complicating this is the lack of standardization in operative techniques, in particular for larger perforations. Varying rates of successful closure have been reported. A recent systematic review of the literature demonstrated that use of local mucosal advancement flaps in combination with an interpositional graft demonstrated overall higher rates of successful perforation closure when compared with local mucosal flaps alone. However, this conclusion was tempered by the quality of the current literature as no level 1, 2, or 3 studies have been published to date [
5]. In addition, size of perforation has been demonstrated to be predictive of a higher rate of failure, with perforations >2 cm in maximal diameter being at higher risk for persistent septal perforation following surgery [
3].
Given the elevated risk of failure with larger perforations approaching or exceeding 2 cm in maximal dimension, vascularized flaps may provide additional benefits over free interpositional grafts. The pericranial flap provides a well-vascularized tissue that may be used to cover bone or cartilage. Deep branches from the supraorbital and supratrochlear arteries provide a robust, proximal vascular supply [
6]. The location of the supratrochlear arteries is consistent making selection of this flap reliable [
7]. Importantly, the use of a pedicled vascularized flap allows for immediate intraoperative assessment of flap perfusion and viability using laser angiography. This ensures a robustly vascularized interpositional flap and eliminates the uncertain viability associated with use of large free grafts by providing real-time quantitative information [
8,
9]. A low perfusion index may predict likelihood of postoperative failure. This additional information may lead surgeons to alter intraoperative plans for reconstruction or counsel patients on the need for revision surgery in the future. In the cases for treatment of septal perforations, this would be an invaluable tool to ensure the highest likelihood of successful perforation closure. Use of this flap for nasal reconstructions offers the additional advantages of a large volume flap to cover larger septal defects as well as use of autologous tissue with decreased infection rates [
4].
Excellent results were achieved with use of the pericranial flap. The external rhinoplasty approach provided a wide field of exposure and no aesthetic deformities were noted. In our experience, the keys to success in management of septal perforations are consideration of flap design, surgical approach, and incorporation of a tension-free graft. This case represents our experience with the pericranial flap via an external rhinoplasty approach and provides another tool in the arsenal for repair of large perforations. Selection of this flap should be made at the discretion of the operating surgeon after consideration of reconstructive options.