Abstract
Although there is a worldwide increase in maxillofacial trauma incidence; the pattern and etiology of these injuries varies from one country to another depending on socioeconomic, cultural, and environmental factors. This study aims to realize the epidemiological characteristics of maxillofacial fractures in our department. A retrospective cross-sectional study of all facial trauma patients admitted to our department during 2009 to 2012. Patients’ data including gender, age, etiology of trauma, the pattern and demographic distribution of fractures of maxillofacial skeleton, and associated injuries were analyzed and compared with previously published data. The chi-square test was used with a p value of less than 0.05, which was considered statistically significant. There is a significant increase in maxillofacial fractures incidence in the past 2 years than former ones. There is a male predominance with highest incidence in the age group of 20 to 40 years. Road traffic accident is the most common etiological factor followed by violence. There is increase in mandibular fracture incidence compared with midface. The significant increased incidence of maxillofacial fracture due to motor car accidents and assaults in the past 2 years reflects a behavioral change within the community.
Facial fractures are the result of various types of trauma to the face, and may occur in isolation or combined with other injuries [1]. The epidemiological assessment of maxillofacial fractures represents a special interest to identify the potential trend of their frequency, age, gender, and anatomic distribution especially when comparison of these patterns is done over time periods.
The incidence of maxillofacial fractures varies widely between different countries depending on local demographic and socioeconomic status [2,3]. Generally, the incidence is higher in males than in females with peak incidence between 20 and 30 years [4]. Many causes had been incriminated in the etiology of facial fractures; however, the main causes worldwide are traffic accidents, assaults, falls, and sport injuries [5,6]. Motor car accidents (MCA) have always been the most frequent cause of facial fractures worldwide; however, recent studies have shown that assaults are now the most common cause in many developed countries.
Our hospital is serving more than 4 million people living in the eastern region of Cairo besides draining areas of the country side near this region. The presence of our plastic surgery department with surgeons specializing in maxillofacial surgery and the lack of public hospitals specializing in this field in the surrounding region has led it to act as a tertiary care center and have increased the number of injuries likely to be referred and treated in this hospital, thus offers a model that could be a sign of our community.
In this article, we intend to assess the epidemiological features of maxillofacial fractures treated at our department for the period from January 2009 to December 2012.
Patients and Methods
A total of 330 patients suffering from facial trauma and suspected facial bone fractures including the nose, frontal bone, maxilla, zygoma, and mandible were presented to the emergency room in our hospital in the period between 2009 and 2012. Of these, only 215 patients were confirmed to have facial fractures necessitating surgical intervention by computed tomography (axial and coronal slices + three-dimensional reconstructed images) and so admitted to our department and operated upon.
We retrospectively analyzed their medical records and data were collected concerning sex, age, cause of injury, type of fracture, treatment modality, and postoperative complications. Patients were divided into seven age groups: 0 to 10-year-old, 11 to 20-year-old, 21 to 30-year-old, 31 to 40-year-old, 41 to 50-year-old, 51 to 60-year-old, and >60-year-old groups. The following analyses were conducted for each age group: causes of injury (e.g., motor vehicle accidents, falling, violence, and gunshot) and fracture type (e.g., nasal bone, zygoma, maxilla, mandible, and frontal bone fractures) and clinical outcomes.
Statistical Analysis
Patient characteristics were analyzed using descriptive statistics; qualitative variables (absolute and relative frequencies) and quantitative variables (means and standard deviation [SD]). The chi-square test was used to evaluate the association between gender, cause of facial fractures, and region affected. A p value of less than 0.05 was considered statistically significant.
Results
Patients’ Data
A total of 215 patients were evaluated for the study in which 183 were males and 32 were females. There was a vast male predominance in all age groups with an overall male-to-female ratio of 5.7:1. The age group 21 to 30 years accounted largest in both sexes (in males and in females) followed by patients in the age group 31 to 40 years (Figure 1).
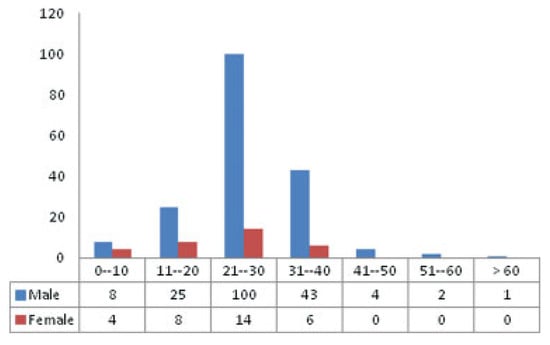
Figure 1.
Age and gender distribution of patients.
The annual distribution of patients based on the number and gender of patients is shown in Table 1. There was no statistical difference among the individual years.

Table 1.
Annual distribution of fractures based on gender difference.
The age of the patients ranged from 2 to 62 years with a mean age 25.7256 years (SD, 9.16842 years). The highest mean was in 2009 (28.8462) whereas the least was in 2010 (22.9592) with no statistical difference between the 4 years of study (Figure 2).
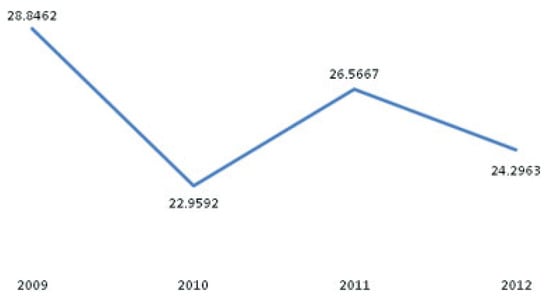
Figure 2.
Mean age distribution of patients.
Among these, the third and fourth decade age groups were significantly more likely to sustain facial fractures (75.3%) with a peak incidence of maxillofacial trauma observed at 25 years (p < 0.05). A decreasing trend was seen with age proceeding to both the extremes (Figure 3).
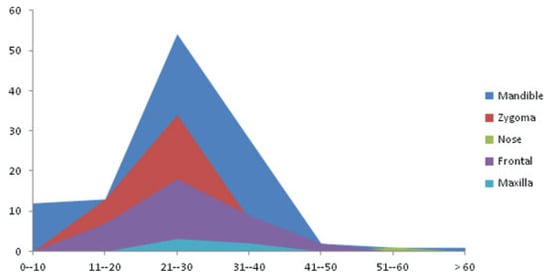
Figure 3.
Fracture site distribution based on age group.
Trauma Type
The most common cause of injury throughout the study was violence and MCA, followed by gunshot and fall from height. The mean age of the patients involved in violence was 27.6364 years (SD, 6.94176 years), whereas the mean age of those who were not involved in violence was 20.5866 years (Table 2).

Table 2.
Cause of fracture distribution of patients.
The annual distribution of patients based on cause of injury showed that MCA was statistically significantly higher in 2009 and 2010 (p < 0.05); however, a shift occurred in 2011 and 2012 leading to statistically significant increase in the rate of violence than the other causes of injury in the previous 2 years (p < 0.05) as shown in Figure 4.
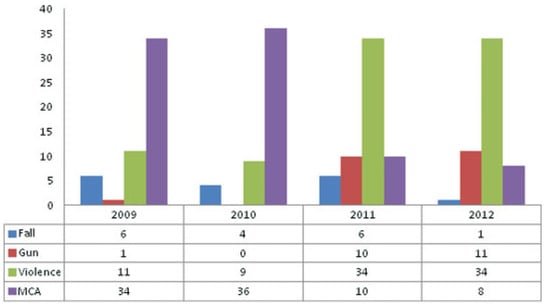
Figure 4.
Cause of fracture distribution based on year.
Almost all patients involved in gunshot injuries and approximately 85% of the patients involved in violence and MCA were males (Figure 5).
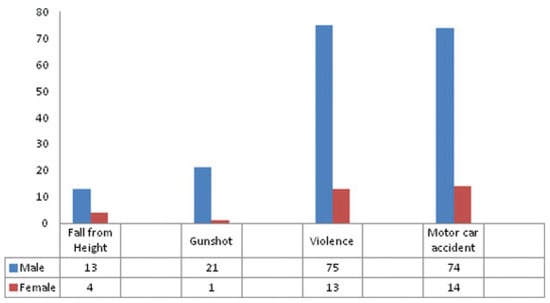
Figure 5.
Cause of fracture distribution based on gender.
In all the age groups, violence and MCA constituted the main causes of fractures with a significant higher difference than other causes (p < 0.05). In patients younger than 10 years, the fractures were mostly due to fall from height.
Falling was a common cause of injury in children younger than 15 years. Violence was more common in those older than 27 years whereas firearms were common in those older than 26 years (Table 3).

Table 3.
Cause of fracture distribution based on age group.
Pattern and Site of Fracture
There were 179 (83.2%) simple facial fractures and 36 (16.7%) multiple facial fractures. Significantly, mandibular fractures were the most common among all facial bone fractures, accounting for 51.6% of all fractures (p < 0.05), zygomaticomaxillary fractures (25.6%) and nasal fractures (16.7%) were the next most common (Figure 6).
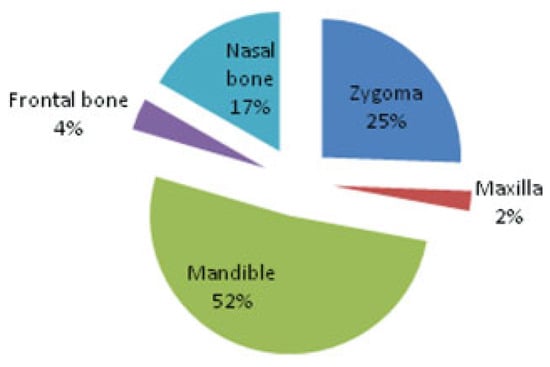
Figure 6.
Site of facial fractures distribution in patients.
In all age groups, fractures of the mandible and zygoma constituted the foremost locations of fractures with a significant higher difference than other locations (p < 0.05) (Table 4).

Table 4.
Site of fracture distribution based on age group.
The site of fracture distribution based on gender differences showed that fractures were mainly affecting the mandible and zygoma with higher percentage of mandible and nasal bone affection within the male sex group than within the female sex group but with no significant statistical difference (Table 5).

Table 5.
Site of fracture distribution based on gender.
Fracture mandible showed significantly statistical higher incidence than other sites based on the cause of injury (p < 0.05) except for the MCA where fracture zygoma was higher but with no statistical difference (Figure 7).
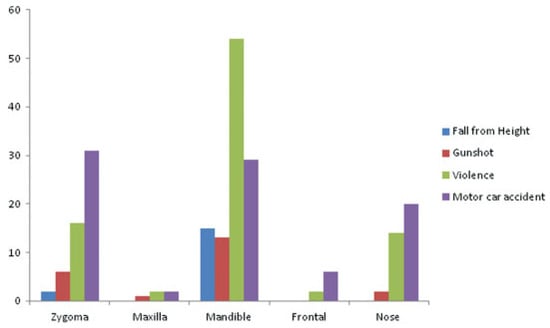
Figure 7.
Site of fracture distribution based on cause of fracture.
The annual distribution of patients based on the site of fracture is shown in Table 6.There was no statistical difference among the individual years.

Table 6.
Site of fracture distribution of fractures based on year.
Treatment Modalities
Surgical treatment was performed on the majority of the patients throughout the 4 years. A total of 215 operations were done with open reduction and internal fixation showed the higher frequency (90.7%) with no significant statistical difference among the individual years. The annual distribution of procedures done for the patients is shown in Table 7. There was no statistical difference among the individual years.

Table 7.
Procedure distribution of fractures based on year.
The procedure distribution of patients based on age is shown in Table 8. There was no statistical difference among the different age groups.

Table 8.
Procedure distribution based on age group.
Over 90% of patients involved in gunshot injuries, violence, and MCA necessitated open reduction and internal fixation, whereas patients involved in falls were treated almost equally by open reduction and internal fixation and mandibulomaxillary fixation (Figure 8).
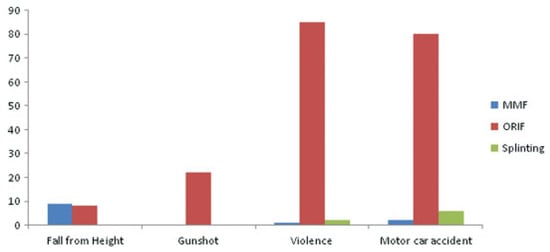
Figure 8.
Procedure distribution based on cause of fracture.
All zygomaticomaxillary complex, frontal bone, and 89.2% of mandibular fractures needed open reduction and internal fixation, whereas all nasal bone fractures were treated only with splinting (Figure 9).
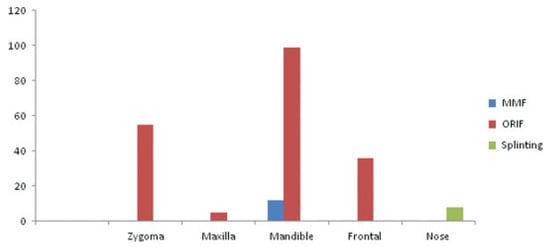
Figure 9.
Procedure distribution based on site of fracture.
Postsurgical Complications
The postoperative complications included infection, paresthesia, diplopia, ectropion, and malocclusion (Table 9).

Table 9.
Postoperative complications.
Discussion
Many studies all over the world had been conducted to study the epidemiology and characteristics of maxillofacial trauma in a single medical center [7,8,9,10,11,12]; however, there are very few studies regarding the Egyptian population [13].
This study was done to review the different epidemiological features of maxillofacial fractures as the incidence, cause, and site of fracture and patients’ data as age, sex, and also surgical procedures and postoperative complications and to correlate these different features with each other within the years of study.
In this study, an overall male-to-female ratio was observed as 5.7:1, this is similar to findings from other studies [12,14] and higher than other studies [15,16,17]. This male dominance reflects cultural and/or employment differences in our eastern community and express the probability of exposure of male to high risk jobs and outdoor daily life risks that could lead to facial injuries.
In agreement with many other studies [18,19,20], the third and fourth decade groups of age in both sexes with mean age of 25.7 years were significantly more likely to sustain facial fractures. That is because it is the energetic period of life where an individual takes part in hazardous sports, fast driving, and more likely to be involved in violence acts. In all age groups, violence and MCA constituted the main causes of fractures in concordance with other studies [21,22]. The maxillofacial fracture in the patient over 60 years was due to fall and this matches with other studies stating that falls are the main cause of facial injury in elderly patients [23].
As most of the studies stated, the etiology of injuries varied considerably between countries as regard to the socioeconomic status [2,3]. The main causes of maxillofacial fractures all over the world are road accidents, assaults, fall, and sports-related injuries [5,6]. In our study, the percentage of maxillofacial fractures due to MCA in 2009 and 2010 were 65.4 and 73.5%, respectively, and constituted the main cause of injury. These findings are in agreement with other studies from developing countries [24,25]. This increase is not in concordance with regular and frequent stress on the use of seat belts and helmets, in addition to many new well-constructed highways with regular maintenance. We think that this is because of a behavioral deficit of some individuals showing ignorance of traffic rules and regulations.
However, this had significantly decreased in comparison to 2011 and 2012 (16.7 and 14.8%, respectively) with a great increase in the frequency of interpersonal violence accounting for more than 55% of the injuries. This is similar to findings from other studies [26,27].
Violence was significantly more common in males than in females (5.8:1) as results from other studies [16], and also the rate of incidence was much higher in those older than 27 years than all other age groups which was also similar to other studies [3].
The significant increase in the usage of firearms in the past 2 years of the study reflects a change in some cultural habits and necessitates the implication of new preventive measures to control this increase that pose unexpected consequences.
In our study, mandibular fractures were the most common among all other sites accounting for 51.6% of all fractures as mentioned in many other studies [12,14]; however, this is not corresponding with other studies that found that nasal bones and zygomaticomaxillary complex the most common site of injury due to their prominent position within the facial skeleton [10,28].
Concerning the site of fracture in relation to cause of injury, mandibular fractures were likely to occur with violence and this agrees with the common thought that assaults are significant predictors for isolated mandible fractures [1]. On the contrary, all other sites were more likely in MCA.
Because of the high variability in the maxillofacial fracture patterns; many treatment modalities have been proposed depending on the own features of each fracture and also surgeons’ experience and that is why standardization of a surgical technique is not possible and combination of different methods are preferred.
In our study, open reduction and internal fixation with titanium plates was the most commonly used method with the usage of bone grafts in old fractures only while mandibulomaxillary fixation alone and splinting were used in less than 10% of cases.
The most frequent postoperative complications after treatment of maxillofacial fractures are malocclusion, infection, and nonunion [29]. We had a complication rate of 9.3% (n = 20); the most common complication was infection (35%) treated conservatively with broad spectrum antibiotics and also local wound care. Malocclusion took place in five patients; all of them needed a second surgery.
The significant increased incidence of maxillofacial fracture due to MCA and assaults in the past 2 years reflects a behavioral change within the community and showed the necessity for a national plan that should be headed to prevention and treatment.
References
- Erdmann, D.; Follmar, K.E.; Debruijn, M.; et al. A retrospective analysis of facial fracture etiologies. Ann Plast Surg 2008, 60, 398–403. [Google Scholar] [CrossRef]
- Kruger, E.; Smith, K.; Tennant, M. Jaw fractures in the indigenous and non-indigenous populations of Western Australia: 1999–2003. Int J Oral Maxillofac Surg 2006, 35, 658–662. [Google Scholar] [CrossRef] [PubMed]
- van den Bergh, B.; Karagozoglu, K.H.; Heymans, M.W.; Forouzanfar, T. Aetiology and incidence of maxillofacial trauma in Amsterdam: a retrospective analysis of 579 patients. J Craniomaxillofac Surg 2012, 40, e165–e169. [Google Scholar] [CrossRef]
- Paes, J.V.; de Sá Paes, F.L.; Valiati, R.; de Oliveira, M.G.; Pagnoncelli, R.M. Retrospective study of prevalence of face fractures in southern Brazil. Indian J Dent Res 2012, 23, 80–86. [Google Scholar] [PubMed]
- Ellis, E., III; Moos, K.F.; el-Attar, A. Ten years of mandibular fractures: an analysis of 2,137 cases. Oral Surg Oral Med Oral Pathol 1985, 59, 120–129. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.H.; Cho, B.K.; Park, W.J. A 4-year retrospective study of facial fractures on Jeju, Korea. J Craniomaxillofac Surg 2010, 38, 192–196. [Google Scholar] [CrossRef]
- Gassner, R.; Tuli, T.; Hächl, O.; Rudisch, A.; Ulmer, H. Cranio-maxillofacial trauma: a 10 year review of 9,543 cases with 21,067 injuries. J Craniomaxillofac Surg 2003, 31, 51–61. [Google Scholar] [CrossRef]
- Motamedi, M.H. An assessment of maxillofacial fractures: a 5-year study of 237 patients. J Oral Maxillofac Surg 2003, 61, 61–64. [Google Scholar] [CrossRef]
- Ozkaya, O.; Turgut, G.; Kayali, M.U.; Uğurlu, K.; Kuran, I.; Baş, L. A retrospective study on the epidemiology and treatment of maxillofacial fractures. Ulus Travma Acil Cerrahi Derg 2009, 15, 262–266. [Google Scholar]
- Leles, J.L.; dos Santos, E.J.; Jorge, F.D.; da Silva, E.T.; Leles, C.R. Risk factors for maxillofacial injuries in a Brazilian emergency hospital sample. J Appl Oral Sci 2010, 18, 23–29. [Google Scholar] [CrossRef]
- Zix, J.A.; Schaller, B.; Lieger, O.; Saulacic, N.; Thorén, H.; Iizuka, T. Incidence, aetiology and pattern of mandibular fractures in central Switzerland. Swiss Med Wkly 2011, 141, w13207. [Google Scholar] [CrossRef] [PubMed]
- Kapoor, P.; Kalra, N. A retrospective analysis of maxillofacial injuries in patients reporting to a tertiary care hospital in East Delhi. Int J Crit Illn Inj Sci 2012, 2, 6–10. [Google Scholar] [CrossRef] [PubMed]
- Sakr, K.; Farag, I.A.; Zeitoun, I.M. Review of 509 mandibular fractures treated at the University Hospital, Alexandria, Egypt. Br J Oral Maxillofac Surg 2006, 44, 107–111. [Google Scholar] [CrossRef]
- Pombo, M.; Luaces-Rey, R.; Pértega, S.; et al. Review of 793 facial fractures treated from 2001 to 2008 in a coruña university hospital: types and etiology. Craniomaxillofac Trauma Reconstr 2010, 3, 49–54. [Google Scholar] [CrossRef]
- Chandra Shekar, B.R.; Reddy, C. A five-year retrospective statistical analysis of maxillofacial injuries in patients admitted and treated at two hospitals of Mysore city. Indian J Dent Res 2008, 19, 304–308. [Google Scholar] [CrossRef]
- Ravindran, V.; Ravindran Nair, K.S. Metaanalysis of maxillofacial trauma in the northern districts of Kerala: one year prospective study. J Maxillofac Oral Surg 2011, 10, 321–327. [Google Scholar] [CrossRef] [PubMed]
- Momeni, H.; Shahnaseri, S.; Hamzeheil, Z. Distribution assessment of maxillofacial fractures in trauma admitted patients in Yazd hospitals: an epidemiologic study. Dent Res J (Isfahan) 2011, 8 (Suppl. S1), S80–S83. [Google Scholar]
- Cheema, S.A.; Amin, F. Incidence and causes of maxillofacial skeletal injuries at the Mayo Hospital in Lahore, Pakistan. Br J Oral Maxillofac Surg 2006, 44, 232–234. [Google Scholar] [CrossRef]
- Oginni, F.O.; Ajike, S.O.; Obuekwe, O.N.; Fasola, O. A prospective multicenter study of injury profile, severity and risk factors in 221 motorcycle-injured Nigerian maxillofacial patients. Traffic Inj Prev 2009, 10, 70–75. [Google Scholar] [CrossRef]
- Al Ahmed, H.E.; Jaber, M.A.; Abu Fanas, S.H.; Karas, M. The pattern of maxillofacial fractures in Sharjah, United Arab Emirates: a review of 230 cases. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2004, 98, 166–170. [Google Scholar] [CrossRef]
- Adebayo, E.T.; Ajike, O.S.; Adekeye, E.O. Analysis of the pattern of maxillofacial fractures in Kaduna, Nigeria. Br J Oral Maxillofac Surg 2003, 41, 396–400. [Google Scholar] [CrossRef] [PubMed]
- Bakardjiev, A.; Pechalova, P. Maxillofacial fractures in Southern Bulgaria—a retrospective study of 1706 cases. J Craniomaxillofac Surg 2007, 35, 147–150. [Google Scholar] [CrossRef] [PubMed]
- Iida, S.; Kogo, M.; Sugiura, T.; Mima, T.; Matsuya, T. Retrospective analysis of 1502 patients with facial fractures. Int J Oral Maxillofac Surg 2001, 30, 286–290. [Google Scholar] [CrossRef] [PubMed]
- Fasola, A.O.; Lawoyin, J.O.; Obiechina, A.E.; Arotiba, J.T. Inner city maxillofacial fractures due to road traffic accidents. Dent Traumatol 2003, 19, 2–5. [Google Scholar] [CrossRef] [PubMed]
- Ansari, M.H. Maxillofacial fractures in Hamedan province, Iran: a retrospective study (1987–2001). J Craniomaxillofac Surg 2004, 32, 28–34. [Google Scholar] [CrossRef]
- Depprich, R.; Handschel, J.; Hornung, J.; Meyer, U.; Kübler, N.R. Causation, therapy and complications of treating mandibular fractures—a retrospective analysis of 10 years [in German]. Mund Kiefer Gesichtschir 2007, 11, 19–26. [Google Scholar] [CrossRef]
- Lee, K.H. Epidemiology of mandibular fractures in a tertiary trauma centre. Emerg Med J 2008, 25, 565–568. [Google Scholar] [CrossRef]
- Eggensperger, N.; Smolka, K.; Scheidegger, B.; Zimmermann, H.; Iizuka, T. A 3-year survey of assault-related maxillofacial fractures in central Switzerland. J Craniomaxillofac Surg 2007, 35, 161–167. [Google Scholar] [CrossRef]
- Güven, O. Stabilisation of the delayed zygomatic arch fracture. Int J Oral Maxillofac Surg 1987, 16, 445–447. [Google Scholar] [CrossRef]
© 2014 by the author. The Author(s) 2014.