The inferior palpebral (IP) nerve is the smallest branch of the infraorbital nerve (ION) and supplies cutaneous innervation to the inferior eyelid and the conjunctiva [
1]. It normally branches within the infraorbital canal before emerging through the infraorbital foramen (IOF) [
2,
3]. It then courses superolaterally in relation to the IOF to its region of distribution [
4].
Reported variations of the IP nerve include partial innervation of the inferior eyelid, emergence through accessory IOF, and bifid anatomy [
5]. The frequencies of occurrence of some of these variations are unknown.
As part of the entire ION complex, IP nerve is often involved in pain syndromes of the face [
6]. Traumatic injuries to this nerve may be occasioned by orbitozygomatic complex fracture [
7] or deep lacerations whereas iatrogenic injuries may occur during maxillofacial surgery [
8]. The aim of this study was to describe the precise pattern and distribution of the nerve to highlight the aberrations that may influence the outcome of clinical interventions.
Materials and Methods
This study was performed on 84 IP nerves by dissection of the faces of 42 formalin-fixed cadavers from the laboratory of topographic anatomy, Department of Human Anatomy, University of Nairobi, Kenya. These included cadavers without facial malformations, injury, or evidence of surgical operation in the midface.
The point of emergence of the ION was determined by dissection and its branches were exposed. The course of the IP nerve was defined through meticulous dissection. The position of emergence of the IP nerve was recorded as either infraorbital and accessory infraorbital or other foramina. If the nerve emerged other than from the IOF, its relationship with the IOF was determined followed by the course toward its termination. When the nerve emerged from an accessory foramen the bone was drilled to confirm that it branched from the ION within the infraorbital canal. All instances of aberrant emergence were investigated further through wide dissection to confirm the branching point and exclude the possibility of the nerve being absent. Other features of the IP nerve investigated were its relationship with the other branches of the ION including common trunks and postemergence fusion.
Results
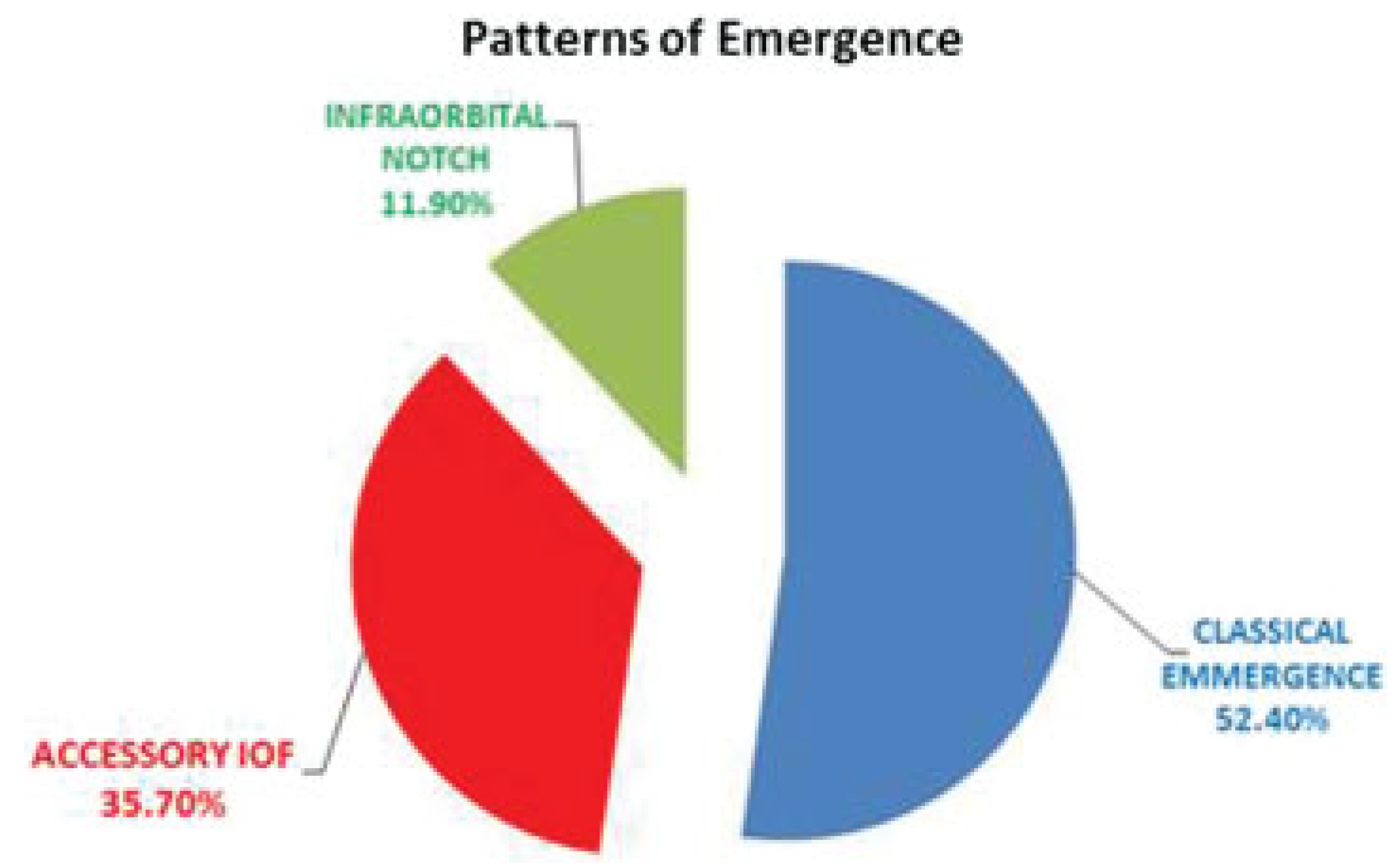
The normal course superolaterally relative to the IOF was noted in 34 nerves (40.48%). The classical emergence from the IOF occurred in 44 nerves (52.4%), while the rest emerged from an accessory IOF, and a few from an infraorbital notch (►
Figure 1). Variations encountered were categorized into those involving its emergence, course, or a complete absence of the nerve.
Variation in Emergence
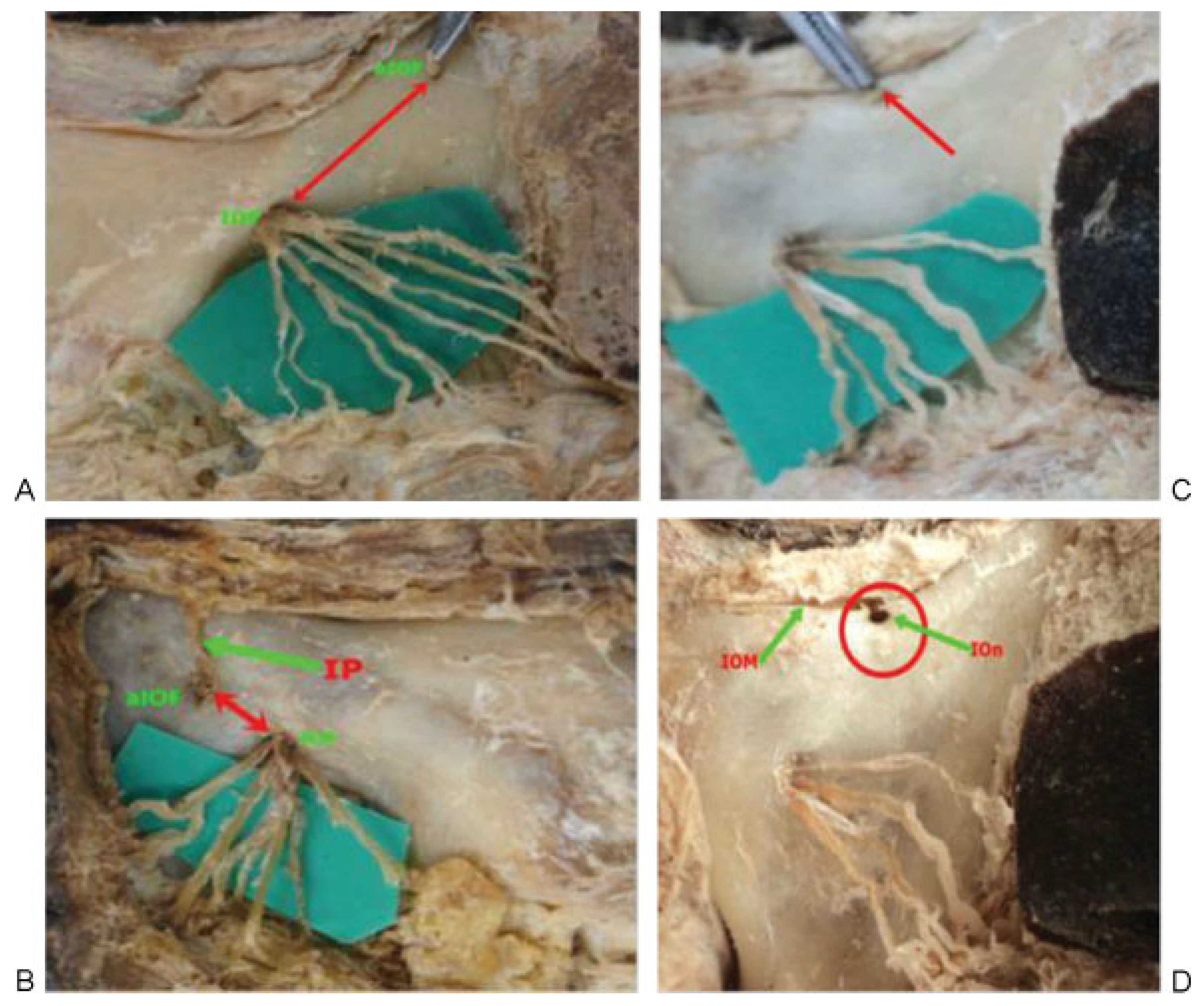
Emergence from an accessory IOF was noted in 30 (35.71%) nerves. All nerves from an accessory foramen were superomedial to the IOF and as such entered into the inferior eyelid medially. Their distance from the IOF was highly variable (►
Figure 2A,B).
Emergence from an infraorbital notch was noted in 10 (11.9%) nerves (►
Figure 2C,D). These had a brief short extraosseous course before entering the inferior eyelid. Some of these nerves were noted to course in the orbital floor before emerging through a notch in the elevation of the infraorbital rim (margin). The ends of the notch were connected by fibrous tissue which ran over the nerve. In keeping with the emergence from accessory infraorbital foramina, the nerves traversing the notch all lay superomedial to the IOF.
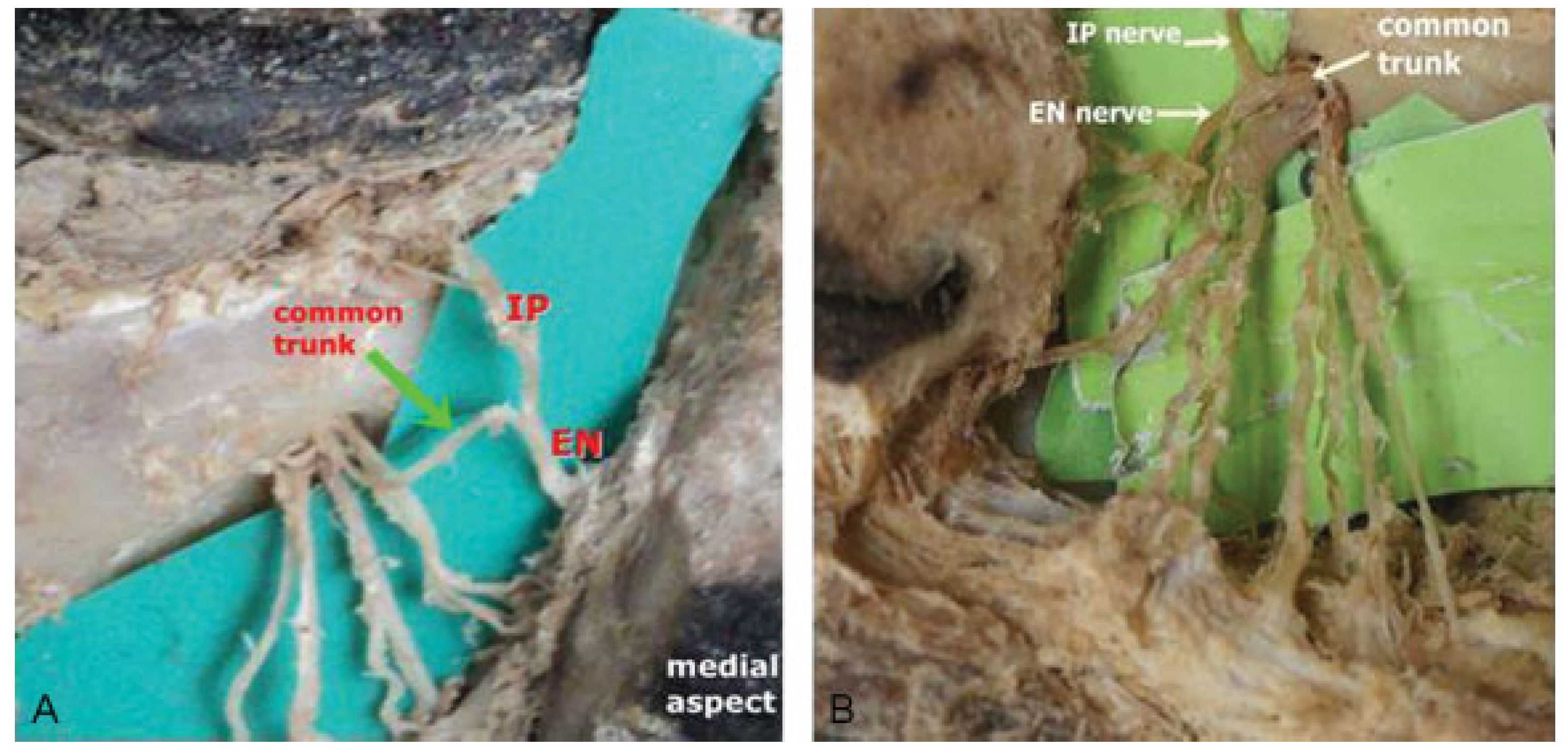
A further variation in emergence was a common trunk with the external nasal nerve which occurred in 4.76% (►
Figure 3). This trunk ran medially for approximately 8 to 9 mm from the IOF before bifurcating into the IP nerve running superiorly to the inferior eyelid and the external nasal nerve which had a short oblique course before entering the ala of the nose. There were no cases of multiple IP nerves.
Variations in the Course
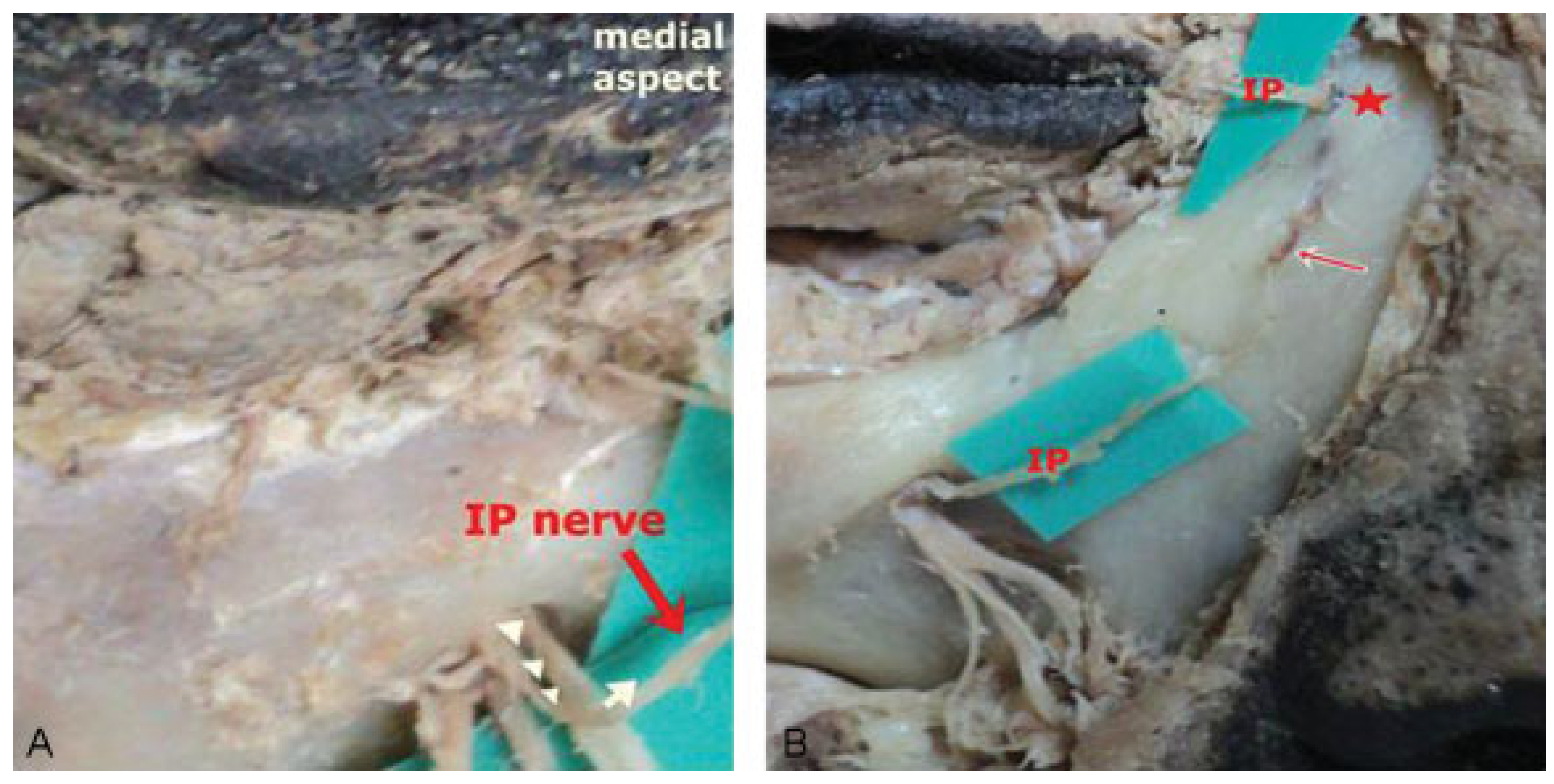
A variant superomedial course of the IP nerve relative to the IOF (►
Figure 4A,B) was noted in the majority of nerves (59.52%). Twenty (23.8%) nerves emerged from the IOF while the rest emerged from the accessory foramen or the infraorbital notch.
Intraosseous Canal
In two cases, the nerve had a short superomedial course before entering an osseous canal from which it emerged via a foramen just medial to the medial canthus to penetrate into the IP (►
Figure 4B).
Discussion
Reports on studies on dry skulls show that accessory IOF are a common occurrence [
9]. Results from this study has shown that the IP nerve may commonly traverse one of these accessory foramina. It is noteworthy that despite the presence of multiple accessory IOF, there were no cases of multiple or even bifid IP nerves unlike previously reported [
5]. This study has also revealed the existence of an infraorbital notch, a hitherto unreported finding. These aberrant patterns of emergence may significantly reduce the success of ION block in the area of distribution of the nerve. These findings may suggest that the consideration of a separate IP nerve block be made in procedures exclusive to the inferior eyelid such as blepharoplasty. If this were to be done, extreme caution is recommended in view of the variable distance from the IOF and the close proximity to the orbit. An important observation is that all the variant positions of emergence occurred medial to the IOF and this was in keeping with previous reports indicating tendency of the nerve to be located more medially [
5]. This and in addition to the present findings may imply that the area lateral to the IOF may be a safer point for surgical incision than the medial side.
While fusion of the nasal nerves has been described [
5], a common emergence between the inferior eyelid and external nasal nerves has not. Majority of the nerves in this study exhibited a variant superomedial course. This occurred when the nerve had a classical emergence from the IOF and in all cases of aberrant emergence from an accessory foramen or infraorbital notch. A superomedially coursing IP nerve has been reported [
5] but with a much lower frequency. While the higher frequency observed in this study may be a result of the sample size, there exists a possibility that this variation is the predominant pattern in the general population. Maxillofacial surgeons need to be aware of this variant course as the nerve is at increased risk of injury during surgery as medial incisions including the Weber Ferguson are done more frequently to avoid injuring the IP and zygomaticofacial nerves on the lateral aspect [
10].
Conclusion
This study has demonstrated that the IP nerve has a high anatomical variability that may account for the difficulties and complications encountered in clinical interventions. It is believed that this information will improve clinical management of conditions affecting the region of distribution nerve of the IP nerve as well as in surgical interventions.