A New Approach to Breast Specimen Orientation: Avoiding Pitfalls with the Specimen Plate Concept
Abstract
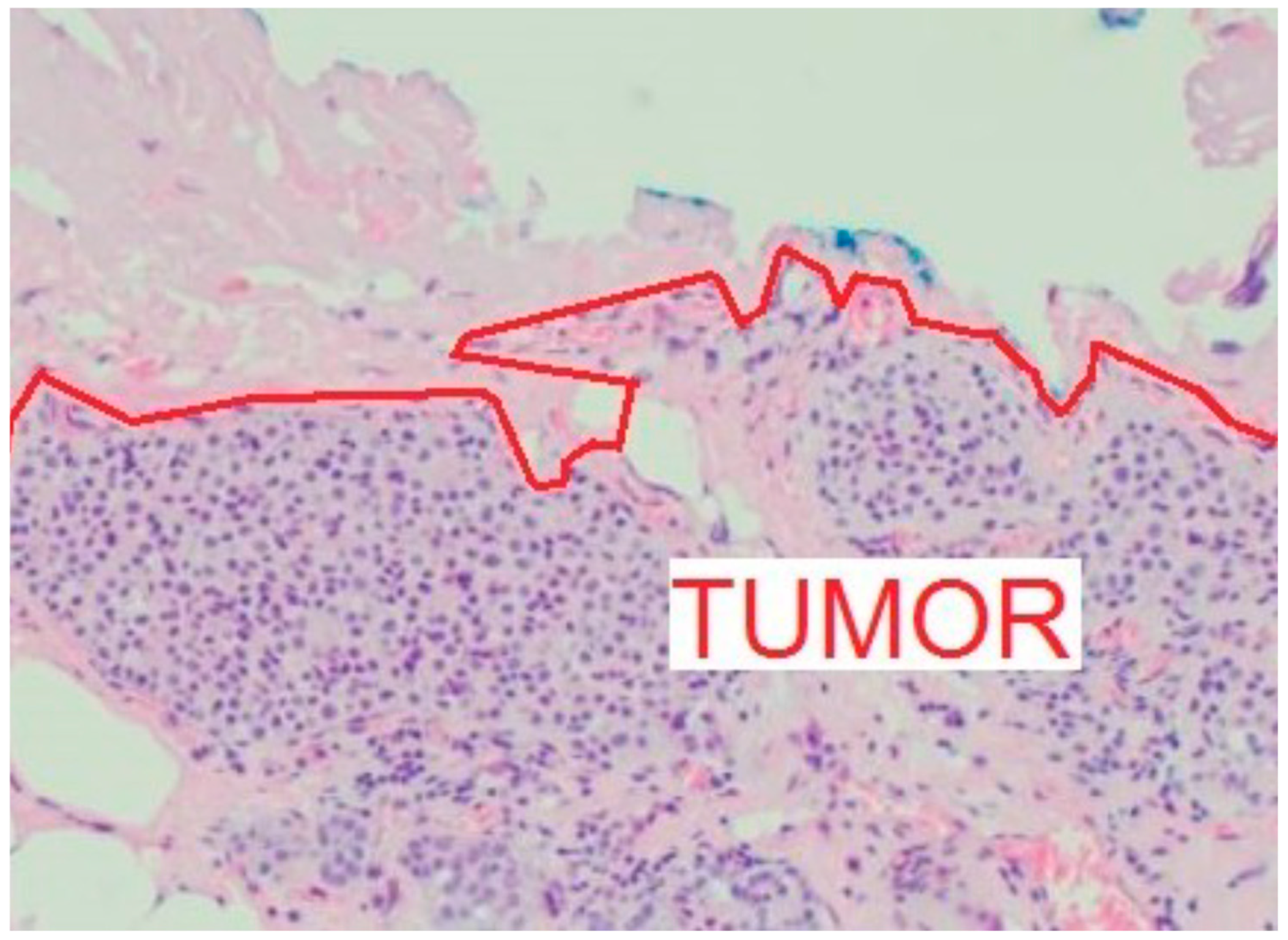
1. Introduction
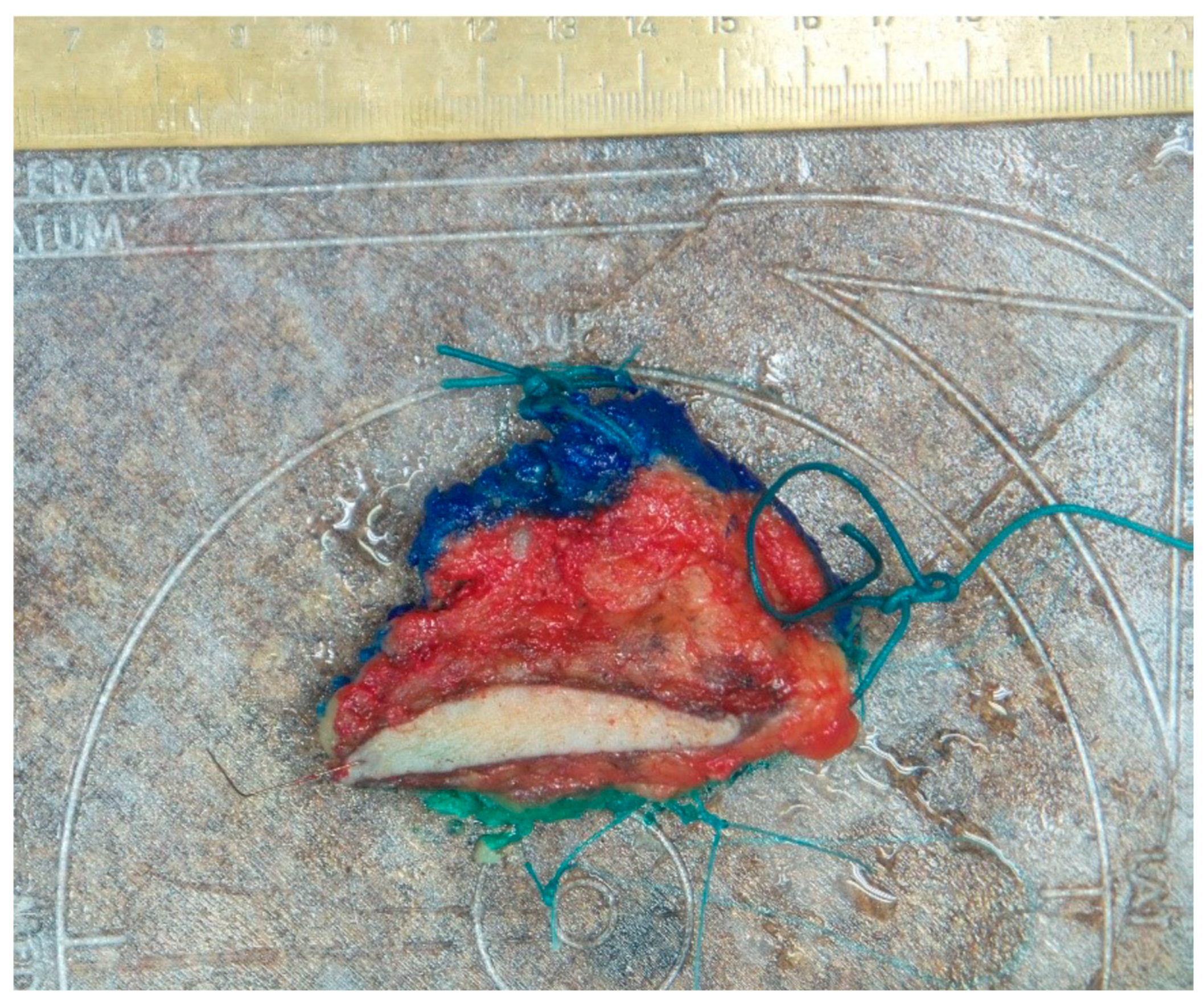
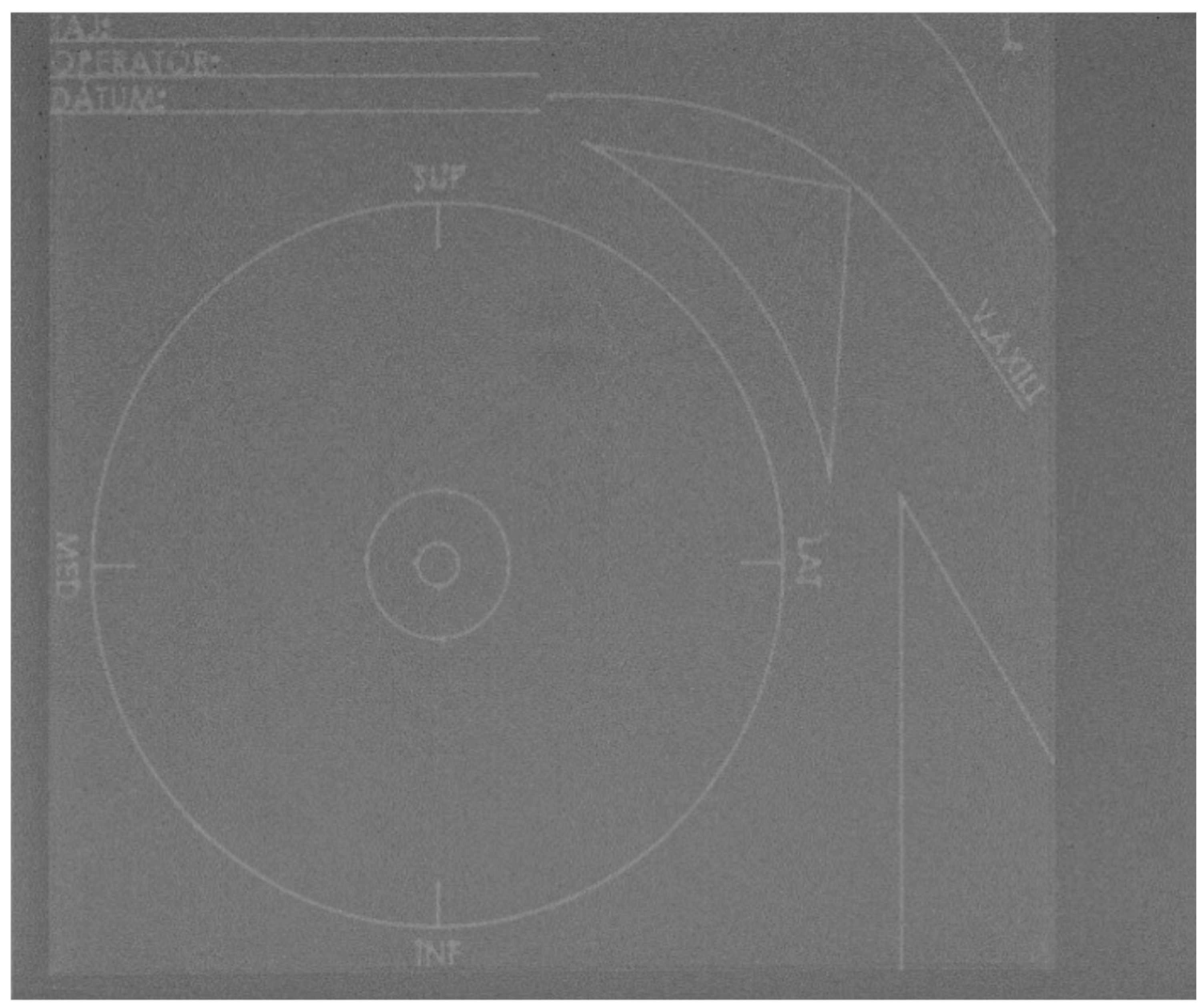
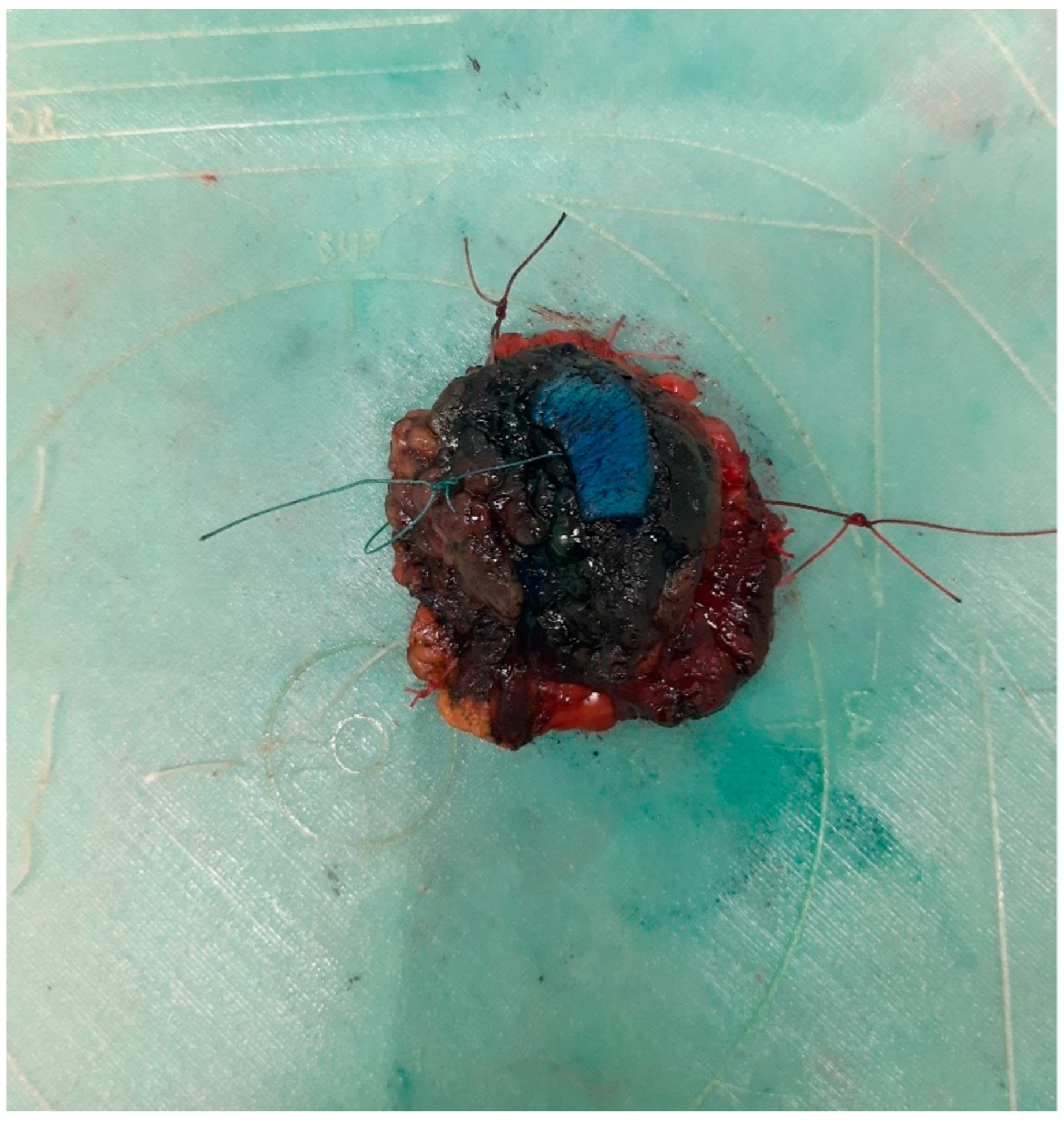
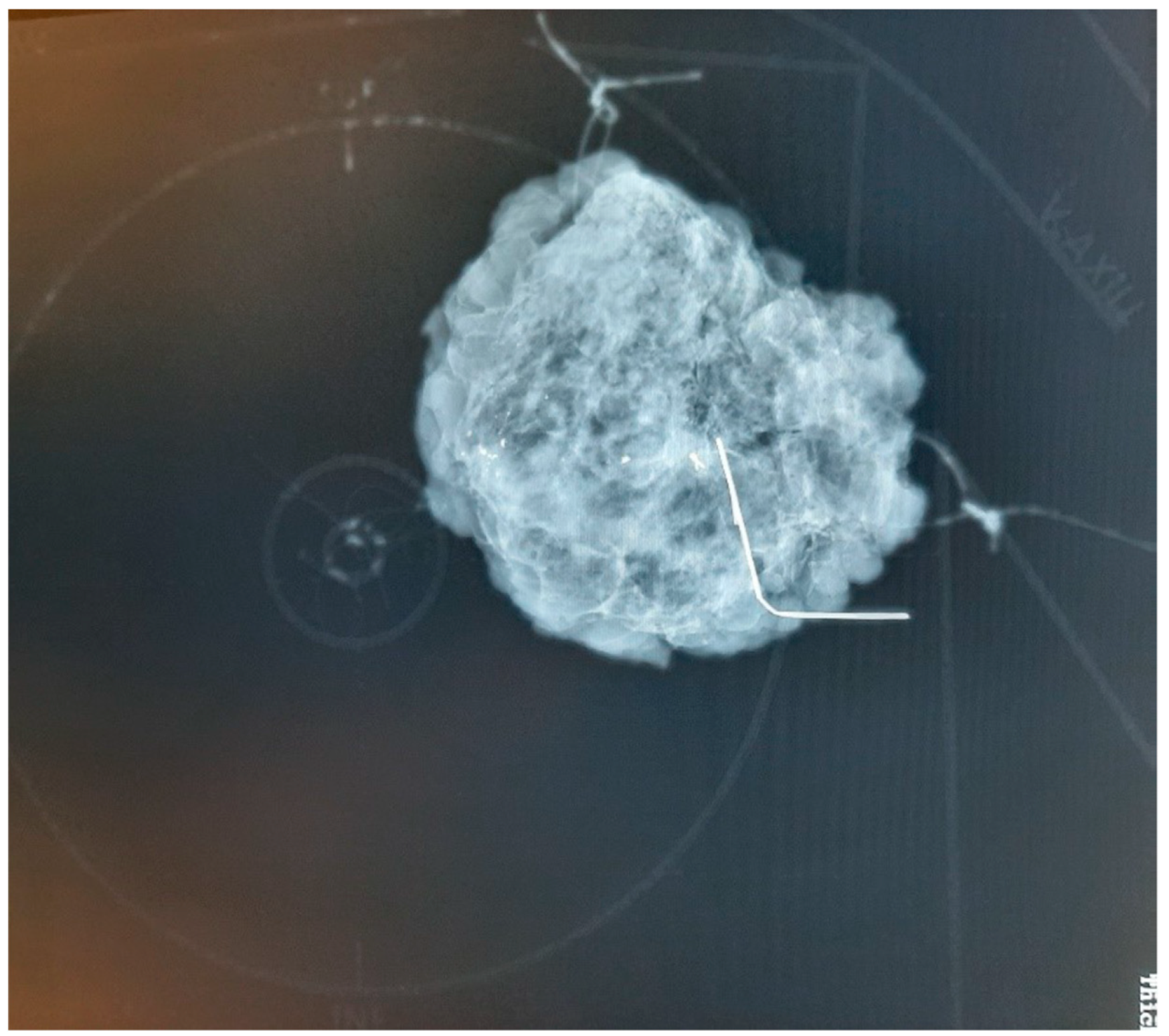
2. Materials and Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
Appendix A. 3D Printing Details
- The plate is made using a Creality Ender 5 3D printer (Creality, Shenzhen, China)
- A layer thickness of 0.1 mm was used to create a solid yet braided structure. This allows the material to be shaped like a textile but be more flexible.
- The material is TPU A95 synthetic resin. This material holds the stitches used to attach the specimen securely, maintaining proper tensile strength even if only a small bit of the plate is occupied by the stitch.
- Printing parameters:
- Print speed: 30 mm/s
- Printing temperature: 240 °C
- Nozzle diameter: 0.6 mm
References
- Curigliano, G.; Burstein, H.J.; Gnant, M.; Loibl, S.; Cameron, D.; Regan, M.; St Gallen Consensus Conference Panelists. Understanding breast cancer complexity to improve patient outcomes: The St Gallen International Consensus Conference for the Primary Therapy of Individuals with Early Breast Cancer 2023. Ann. Oncol. 2023, 34, 970–986. [Google Scholar] [CrossRef] [PubMed]
- Molnar, T.F. A new device for the identification of lymph nodes at lung cancer surgery. Eur. J. Cardiothorac. Surg. 2007, 31, 311–312. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Kurniasih, D.A.A.; Setiawati, E.P.; Pradipta, I.S.; Subarnas, A. Patients’ Perspectives of Interprofessional Collaboration in Breast Cancer Unit. Healthcare 2023, 11, 332. [Google Scholar] [CrossRef]
- Houssami, N.; Macaskill, P.; Marinovich, M.L.; Dixon, J.M.; Irwig, L.; Brennan, M.E.; Solin, L.J. Meta-analysis of the impact of surgical margins on local recurrence in women with early-stage invasive breast cancer treated with breast-conserving therapy. Eur. J. Cancer 2010, 46, 3219–3232. [Google Scholar] [CrossRef] [PubMed]
- Lázár, G.; Kelemen, P.; Kósa, C.; Maráz, R.; Paszt, A.; Pavlovics, G.; Sávolt, Á.; Simonka, Z.; Tóth, D.; Mátrai, Z. IV. Emlőrák Konszenzus Konferencia–Az emlőrák korszerű sebészi kezelése. Magy. Onkol. (In Hungarian). 2020, 64, 329–346. [Google Scholar] [PubMed]
- Kiss, Z.; Kocsis, J.; Nikolényi, A.; Horváth, Z.; Knollmajer, K.; Benedek, A.; Varnai, M.; Polanyi, Z.; Kovacs, K.A.; Berta, A.; et al. Opposite trends in incidence of breast cancer in young and old female cohorts in Hungary and the impact of the COVID-19 pandemic: A nationwide study between 2011–2020. Front. Oncol. 2023, 13, 1182170. [Google Scholar] [CrossRef] [PubMed]
- Benjamin, M.A.; Sinnott, C.; Bawa, S.; Kaufman, D.I.; Guarino, K.; Addona, T. Re-excision rate after partial mastectomy in oncoplastic breast-conserving surgery: A single-institutional experience and review of the literature. Ann. Plast. Surg. 2019, 82, S170–S172. [Google Scholar] [CrossRef] [PubMed]
- Nanda, A.; Hu, J.; Hodgkinson, S.; Ali, S.; Rainsbury, R.; Roy, P.G. Oncoplastic breast-conserving surgery for women with primary breast cancer. Cochrane Database Syst. Rev. 2021, 10, CD013658. [Google Scholar] [CrossRef] [PubMed]
- McCahill, L.E.; Single, R.M.; Aiello Bowles, E.J.; Feigelson, H.S.; James, T.A.; Barney, T.; Engel, J.M.; Onitilo, A.A. Variability in reexcision following breast conservation surgery. JAMA 2012, 307, 467–475. [Google Scholar] [CrossRef]
- Morrow, M.; Jagsi, R.; Alderman, A.K.; Griggs, J.J.; Hawley, S.T.; Hamilton, A.S.; Graff, J.J.; Katz, S.J. Surgeon recommendations and receipt of mastectomy for treatment of breast cancer. JAMA 2009, 302, 1551–1556. [Google Scholar] [CrossRef]
- Kong, J.; Bandyopadhyay, S.; Chen, W.; Al-Mufarrej, F.; Choi, L.; Kosir, M.A. Improved Rate of Negative Margins for Inflammatory Breast Cancer Using Intraoperative Frozen Section Analysis. Cancers 2023, 15, 4597. [Google Scholar] [CrossRef] [PubMed]
- Ohtake, T.; Yasuda, M.; Ito, J.; Watanabe, K.; Gonda, K.; Abe, N.; Ishii, M.; Sato, Y.; Momma, T.; Takenoshita, S. Pathological aspects of the intraductal spread of breast cancer. Breast Cancer 2013, 20, 34–40. [Google Scholar] [CrossRef]
- Carter, D. Margins of “lumpectomy” for breast cancer. Hum. Pathol. 1986, 17, 330–332. [Google Scholar] [CrossRef]
- Pilewskie, M.; Morrow, M. Margins in Breast Cancer: How Much Is Enough? Cancer 2018, 124, 1335–1341. [Google Scholar] [CrossRef] [PubMed]
- Ikeda, T.; Akiyama, F.; Hiraoka, M.; Inaji, H.; Ohuchi, N.; Takatsuka, Y.; Yoshimoto, M. Surgical Margin Status as a Cause of Local Failure after Breast Conserving Therapy. Breast Cancer 1999, 6, 93–97. [Google Scholar] [CrossRef] [PubMed]
- Maishman, T.; Cutress, R.I.; Hernandez, A.; Gerty, S.; Copson, E.R.; Durcan, L.; Eccles, D.M. Local Recurrence and Breast Oncological Surgery in Young Women with Breast Cancer: The POSH Observational Cohort Study. Ann. Surg. 2017, 266, 165–172. [Google Scholar] [CrossRef] [PubMed]
- Beriwal, S.; Schwartz, G.F.; Komarnicky, L.; Garcia-Young, J.A. Breast-conserving therapy after neoadjuvant chemotherapy: Long-term results. Breast J. 2006, 12, 159–164. [Google Scholar] [CrossRef] [PubMed]
- Massat, N.J.; Dibden, A.; Parmar, D.; Cuzick, J.; Sasieni, P.D.; Duffy, S.W. Impact of screening on breast cancer mortality: The UK program 20 years on. Cancer Epidemiol. Biomark. Prev. 2016, 25, 455–462. [Google Scholar] [CrossRef] [PubMed]
- Banys-Paluchowski, M.; Kühn, T.; Masannat, Y.; Rubio, I.; de Boniface, J.; Ditsch, N.; Karadeniz Cakmak, G.; Karakatsanis, A.; Dave, R.; Hahn, M.; et al. Localization techniques for non-palpable breast lesions: Current status, knowledge gaps, and rationale for the MELODY study (EUBREAST-4/iBRA-NET, NCT 05559411). Cancers 2023, 15, 1173. [Google Scholar] [CrossRef]
- Parisi, S.; Gambardella, C.; Santoriello, A.; Ruggiero, R.; Iovino, F.; Fisone, F.; Mongardini, F.M.; Lucido, F.S.; Tolone, S.; Docimo, L. Early breast cancer: Could combined LOCalizer™ and ultrasound localization replace the metallic wire? A multicentric study. J. Clin. Med. 2024, 13, 1713. [Google Scholar] [CrossRef]
- Elzohery, Y.H.; Gomaa, M.M.; Mohamed, G.; Fadlalla, W.M.; Taha, S.N.; Ibraheem, M.H. Comparison of wire-guided localization (WGL) and radio-guided occult lesion localization (ROLL) in localization of non-palpable breast lesions. World J. Surg. Oncol. 2023, 21, 266. [Google Scholar] [CrossRef] [PubMed]
- Patel, J.; Jenkins, S. A technique for marking oncological breast tissue specimens. Ann. Med. Surg. 2016, 7, 7–8. [Google Scholar] [CrossRef] [PubMed]
- Gibson, G.R.; Lesnikoski, B.A.; Yoo, J.; Mott, L.A.; Cady, B.; Barth, R.J., Jr. A comparison of ink-directed and traditional whole-cavity re-excision for breast lumpectomy specimens with positive margins. Ann. Surg. Oncol. 2001, 8, 693–704. [Google Scholar] [CrossRef] [PubMed]
- Volleamere, A.J.; Kirwan, C.C. National survey of breast cancer specimen orientation marking systems. Eur. J. Surg. Oncol. 2013, 39, 255–259. [Google Scholar] [CrossRef] [PubMed]
|
|
| Questions 1 | Answers | Responder Groups | ||
|---|---|---|---|---|
| Pathologists | Surgeons | Radiologists | ||
| 1. Marking methods used for specimen orientation | Suture markings 2 | 100% | 100% | 100% |
| Clip markings | 11.1% | 8.3% | 0% | |
| Orientation drawings/schematics | 22.2% | 25% | 16.7% | |
| Other Methods (including various types of thread markings and schematic drawings) | 11.1% | 8.3% | 0% | |
| 2. Use of specimen mammograms for pathological assessment in case of non-palpable tumors | Yes No | 77.8% 22.2% | n/a | n/a |
| 3. Specimen mammography clarity | Unambiguous | 25% | 41.7% | 100% |
| Ambiguous | 75% | 58.3% | 0% | |
| 4. Percentage of ambiguity in specimen mammograms where it exists (for surgeons)/percentage of ambiguity in specimen orientation (for radiologists and pathologists) | <10% | 71.4% | 50% | 66.7% |
| 10–50% | 28.6% | 50% | 33.3% | |
| >50% | 0% | 0% | 0% | |
| 5. Common causes of misunderstanding (for radiologists and pathologists) | Unclear Directions of Markings | 50% | n/a | 80% |
| Ambiguous marking methods | 50% | 20% | ||
| 6. Imaging directions | Two-Directional (cranio-caudal and medio-lateral) | 100% | 100% | 100% |
| Antero-Posterior (A-P) Direction (coronal plane) | 0% | 0% | 0% | |
| 7. Additional coronal plane imaging utility | Beneficial | 83.3% | 75% | n/a |
| Not beneficial | 16.6% | 25% | ||
| 8. Significant factor in determining the direction of a re-excision for non-palpable tumors | Mammographic image for the surgeon | n/a | 25% | n/a |
| Consultation with the radiologist | 75% | |||
| 9. Intraoperative photographs | Beneficial | 66.7% | 66.7% | n/a |
| Not beneficial | 33.3% | 33.3% | ||
| 10. Standardization of protocol exists | Yes | 75% | 75% | 75% |
| No | 25% | 25% | 25% | |
| 11. Usefulness of standardized protocol (in the absence of standardization) | Found useful | 87.5% | 66.7% | n/a |
| Not found useful | 12.5% | 33.3% | ||
| 12. Nationwide standardization | Found useful | 87.5% | 66.7% | n/a |
| Not found useful | 12.5% | 33.3% | ||
| 13. Types of suture markings used (open-ended answer) | The suture marking method for orientation of breast-conserving surgical specimens primarily involved the use of sutures of varying lengths and placement to indicate different anatomical directions. The commonly reported marking scheme included Short (superior): Two short sutures indicating the superior (upper) margin of the specimen. Long (lateral): One long suture marking the lateral (outer) margin. Medium (medial): One short suture denoting the medial (inner) margin. Different colors for Mammillary-Central, as indicated by various methods depending on the institution, often involving different colored sutures. It was noted that some institutions employed variations in their marking techniques. These variations included the use of either multiple or single sutures to differentiate the oriented sides of the specimen. | |||
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Drozgyik, A.; Szabó, T.; Kovács, G.; Kollár, D.; Molnár, T.F. A New Approach to Breast Specimen Orientation: Avoiding Pitfalls with the Specimen Plate Concept. Curr. Oncol. 2024, 31, 4589-4598. https://doi.org/10.3390/curroncol31080342
Drozgyik A, Szabó T, Kovács G, Kollár D, Molnár TF. A New Approach to Breast Specimen Orientation: Avoiding Pitfalls with the Specimen Plate Concept. Current Oncology. 2024; 31(8):4589-4598. https://doi.org/10.3390/curroncol31080342
Chicago/Turabian StyleDrozgyik, András, Tamás Szabó, György Kovács, Dániel Kollár, and Tamás F. Molnár. 2024. "A New Approach to Breast Specimen Orientation: Avoiding Pitfalls with the Specimen Plate Concept" Current Oncology 31, no. 8: 4589-4598. https://doi.org/10.3390/curroncol31080342
APA StyleDrozgyik, A., Szabó, T., Kovács, G., Kollár, D., & Molnár, T. F. (2024). A New Approach to Breast Specimen Orientation: Avoiding Pitfalls with the Specimen Plate Concept. Current Oncology, 31(8), 4589-4598. https://doi.org/10.3390/curroncol31080342






