Abstract
The authors present a case of acute coronary syndrome caused by a covered rupture of the aorta compressing the left main coronary artery. The cause of the rupture was later revealed to be a giant cell aortitis in a patient who had no other symptoms and was not known for giant cell arteritis.
Case description
A 78-year-old man, known to have hypertension, presented to the emergency department with stabbing, transfixing chest pain, evolving over the past 2 days. On examination, blood pressure was elevated at 171/96 mm Hg and there was a holosystolic murmur on cardiac auscultation. The electrocardiogram showed ST-segment elevation in aVR combined with ST-segment depression of >1 mm on infero-lateral leads V4–V6 and DI, DII and aVL suggestive of left main coronary artery stenosis (Figure 1) and ultra-sensitive troponin was elevated at 876 ng/l (reference range <18 ng/l).
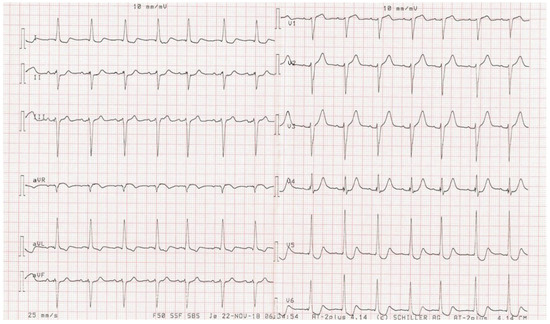
Figure 1.
ECG showing a left main coronary artery stenosis pattern.
The patient was diagnosed with an acute coronary syndrome and transferred for urgent angiography. Coronary angiography confirmed a critical stenosis of the left main coronary artery (Figure 2– panel A) but when the interventional cardiologist tried to reposition the catheter in the left main coronary artery for stenting, an injection of contrast revealed an adjacent structure. At this point the operator proceeded to aortography, which showed this structure to be an aneurysm of the ascending aorta compressing the left main coronary artery (Figure 2 – panel B) and responsible for the identified stenosis.
Figure 2.
Coronary angiography showing left main coronary artery stenosis (panel A) and aortic aneurysm compressing the origin of the left main coronary artery (panel B).
The patient was taken immediately into surgery. Sternotomy exposed a covered rupture of the aorta compressing the left main coronary artery, as well as a haemopericardium.
A Bentall procedure with hemiarch replacement was performed and the patient’s aorta was sent for analysis. Histology of the patient’s aorta was compatible with a giant cell aortitis (Figure 3 – panels C and D).
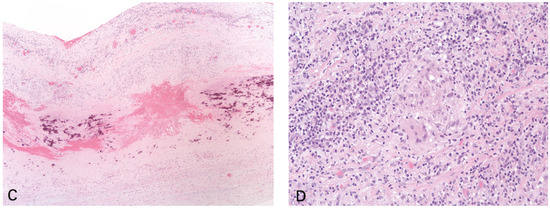
Figure 3.
Aortic wall with haematoxylin and eosin stain at 40× magnification (panel C) and 200× magnification (Panel D) showing lymphoplasmocytic chronic inflammation in the external media and the adventitia associated with a histiocyte and giant cell infiltrate that delimits necrosis areas in the media.
The patient had no history suggestive of giant cell arteritis and presented no other symptoms of the disease. A full vascular work-up with magnetic resonance imaging angiography and ophthalmological examination revealed no other affected arteries. He progressed well under treatment with corticosteroids.
Discussion
Giant cell arteritis is a systemic vasculitis that can affect large- and medium-sized arteries with an incidence of 15–33 cases per 100,000 persons aged >50 years [1].
The incidence of aortic involvement has been described to be between 20% and 40% [2,3] and only 1% to 6% will present with aortic dissection or rupture [1,4].
Our patient was not known to have giant cell arteritis and the initial presentation was in the form of aortic rupture. Patients with large artery complications often have few of the usual symptoms of giant cell arteritis, causing the diagnosis to be overlooked, as was the case with our patient. Furthermore, aneurysm size has been shown not to predict aortic dissection or rupture [5].
In conclusion, this case describes a giant cell aortitis presenting as a covered rupture of the aorta diagnosed at coronary angiography. The patient's anamnesis and clinical findings were suggestive of aortic disease, but an urgent coronary angiography was performed owing to an ECG suggestive of high-risk acute coronary syndrome and elevated cardiac enzymes. This illustrates the need to correctly identify the patients in whom immediate primary percutaneous coronary intervention is needed, and those who would benefit from previous screening with echocardiography and/or computed tomography (CT). If echocardiography and/or CT scan are not available or were not performed in the emergency department, ventriculography before the coronary intervention can also provide useful information for the differential diagnosis.
Disclosure statement
No financial support and no other potential conflict of interest relevant to this article was reported.
References
- Nuenninghoff, D.M.; Hunder, G.G.; Christianson, T.J.; McClelland, R.L.; Matteson, E.L. Incidence and predictors of large-artery complication (aortic aneurysm, aortic dissection, and/or large-artery stenosis) in patients with giant cell arteritis: a population-based study over 50 years. Arthritis Rheum. 2003, 48, 3522–31. [Google Scholar] [CrossRef] [PubMed]
- Bossert, M.; Prati, C.; Balblanc, J.C.; Lohse, A.; Wendling, D. Aortic involvement in giant cell arteritis: current data. Joint Bone Spine. 2011, 78, 246–51. [Google Scholar] [CrossRef] [PubMed]
- Berthod, P.E.; Aho-Glélé, S.; Ornetti, P.; Chevallier, O.; Devilliers, H.; Ricolfi, F.; et al. CT analysis of the aorta in giant-cell arteritis: a case-control study. Eur Radiol. 2018, 28, 3676–84. [Google Scholar] [CrossRef] [PubMed]
- Gawinecka, J.; Schönrath, F.; von Eckardstein, A. Acute aortic dissection: pathogenesis, risk factors and diagnosis. Swiss Med Wkly. 2017 Aug;147:w14489.
- Kermani, T.A.; Warrington, K.J.; Crowson, C.S.; Hunder, G.G.; Ytterberg, S.R.; Gabriel, S.E.; et al. Predictors of Dissection in Aortic Aneurysms From Giant Cell Arteritis. J Clin Rheumatol. 2016, 22, 184–7. [Google Scholar] [CrossRef] [PubMed]
© 2021 by the author. Attribution - Non-Commercial - NoDerivatives 4.0.