Abstract
Recently published studies have shown that cardiac complications are not uncommon in patients with coronavirus 2019 (COVID-19) disease. We describe the case of a 55-year-old female presenting with chest pain after having had influenza-like symptoms. Chest computed tomography showed a circumferential pericardial effusion, confirmed by transthoracic echocardiography with a normal left ventricular ejection fraction. The nasopharyngeal swab was negative, but the use of a rapid test identified COVID-19 antibodies, revealing the infectious cause of the pericarditis.
Case description
A 55-year-old female presented to the outpatient clinic because of pleuritic chest pain 1 month after experiencing influenza-like symptoms. She described myalgia, headache, fatigue and cough. She was previously in good health; she was an occasional smoker and had a history of dyslipidaemia.
On physical examination, the patient was afebrile and presented a friction rub. A 12-lead electrocardiogram (ECG) was normal. Cardiac troponin I and creatine kinase concentrations were within the reference range. Blood inflammatory markers showed a slight increase in C-reactive protein levels of 9 mg/l (reference range <5 mg/l) and normal blood cell counts. D-dimer levels were 1605 ng/ml (reference range <500 ng/ml). Chest computed tomography did not show lung involvement, but there was a circumferential pericardial effusion up to 15 mm (Figure 1A). Transthoracic echocardiography confirmed the pericardial effusion (Figure 1B) with a dilated non-collapsing inferior vena cava and a left ventricular ejection fraction of 70%. Additional tests for common causes of pericarditis – including enterovirus, coxsackievirus, adenovirus and Epstein-Barr virus – were negative. Connective tissue disorders such as systemic lupus erythematosus were also excluded by laboratory testing. Based on the clinical history and the coronavirus disease 2019 (COVID-19) outbreak, COVID-19 was deemed possible. A single nasopharyngeal swab was performed with a negative result for severe acute respiratory syndrome coronavirus 2 (SARS-Cov-2) according to polymerase chain reaction (PCR) method. Finally, we performed a rapid IgM/IgG antibody test to screen for previous coronavirus 2019 infection, which identified IgG antibodies to COVID-19. IgM antibodies were negative. Although an idiopathic origin cannot be ruled out, we assumed that SARS-CoV-2 infection was the most likely cause of our patient’s pericarditis.
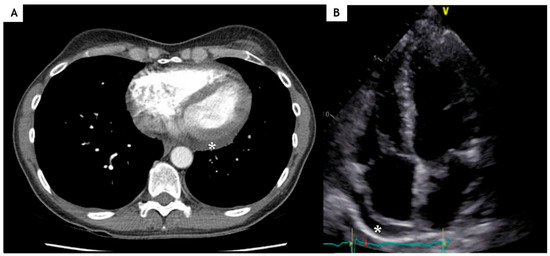
Figure 1.
A. Computed tomography of the chest and B. echocardiography showing pericardial effusion (*).
We prescribed non-steroidal anti-inflammatory drugs (NSAIDs) and colchicine according to European society for Cardiology (ESC) guidelines [1]. One month later, the patient reported improvement in symptoms and repeated echocardiography showed regression of the pericardial effusion.
Discussion
This report highlights a case of pericarditis associated with COVID-19 disease, in a patient with mild symptoms, no signs of interstitial pneumonia and a negative nasopharyngeal swab test. The presence of antibodies to the coronavirus in the blood seemed adequate evidence to relate this virus to the pericarditis.
Although PCR has become the standard method for the diagnosis of COVID-19, there are many reasons for a negative nasopharyngeal swab, including poor quality of the specimen, little patient material, testing on a single swab or collection in a late stage of the infection [2]. Recently, several rapid antibody test kits have been developed, which permit qualitative detection of IgG and IgM antibodies. For the present report, we selected the SARS-CoV-2 IgM/IgG antibody Rapid Test (Sure Biotech Ltd. Hong Kong) with a sensitivity and specificity of 82% and 96%, respectively, for IgM and 93% and 98%, respectively for IgG [3]. Thanks to its characteristics, the rapid test allows immediate diagnosis and requires minimal training. However, the test must be performed at least 7 to 10 days after a potential infection in order to detect IgM and IgG antibodies. Certainly, this test cannot confirm presence of the virus as it provides evidence of recent infection only.
The exact pathogenesis of pericarditis in SARS-CoV-2 re-mains uncertain [4]. Pericarditis could result from direct infection of the pericardium by the virus spreading from the respiratory tract. However, no virus RNA could be isolated in a cardiac biopsy to date. Alternatively, SARS-CoV-2 could trigger secondary immune-mediated inflammation of the pericardium.
This report highlights the ability of the rapid antibody test to detect COVID-19 disease after symptom onset. We believe that recognition of the association between COVID-19 and pericarditis is helpful in guiding the investigations and planning a strict clinical follow-up of these patients.
Funding
The case report was supported by an unrestricted grant from the Fonds Scientifique Cardiovasculaire (Fribourg, Switzerland).
Informed Consent Statement
The authors confirm that written consent for submission and publication of this case report, including images and associated text, has been obtained from the patient in line with COPE guidance.
Conflicts of Interest
The authors have no conflicts of interest to disclose.
References
- Adler, Y.; Charron, P.; Imazio, M.; Badano, L.; Barón-Esquivias, G.; Bogaert, J.; et al. ESC Scientific Document Group. 2015 ESC Guidelines for the diagnosis and management of pericardial diseases: The Task Force for the Diagnosis and Management of Pericardial Diseases of the European Society of Cardiology (ESC) Endorsed by: The European Association for Cardio-Thoracic Surgery (EACTS). Eur Heart J. 2015, 36, 2921–2964. [Google Scholar] [CrossRef] [PubMed]
- Marty, F.M.; Chen, K.; Verrill, K.A. How to Obtain a Nasopharyngeal Swab Specimen. N Engl J Med. 2020, 382. [Google Scholar] [CrossRef] [PubMed]
- Coronavirus (COVID-19) Rapid Test | Your Reliable Supplier of IVD Products. 2020. Available online: https://www.surebiotech.com/rapid-test/ coronavirus-covid-19-rapid-test/.
- Inciardi, R.M.; Lupi, L.; Zaccone, G.; Italia, L.; Raffo, M.; Tomasoni, D.; et al. Cardiac Involvement in a Patient With Coronavirus Disease 2019 (COVID-19). JAMA Cardiol. 2020. [Google Scholar] [CrossRef] [PubMed]
© 2020 by the author. Attribution - Non-Commercial - NoDerivatives 4.0.