Reducing pulmonary artery pressure with the IASD may be a new therapeutic option to treat symptomatic heart failure patients with preserved or moderately reduced ejection fraction.
Introduction
Heart failure with preserved ejection fraction (HFpEF) is a frequent disease with a prevalence of 1.1–5.5% in the general population in Europe [1]. From a pathophysiological point of view, symptoms and a prognosis may depend on lack of stroke volume reserve and/or elevated pulmonary artery pressure [2,3]. In fact, it was shown that left atrial pressure as a major determinant of pulmonary venous and pulmonary artery pressure correlates with symptoms and prognosis [4]. Accordingly, reduction of left atrial pressure may be a promising therapeutic strategy. Consequently, devices have been developed to reduce left atrial pressure through creation of a shunt between the left and right atria [5,6]. While the V-Wave device (V-Wave. Caesarea, Israel) has been studied in a small number of patients with HFrEF (heart failure with reduced ejection fraction), the Corvia-device (IASD, Corvia Medical Inc., Tewksbury, MA, USA) has been evaluated in a larger number of patients with HFpEF and HFmrEF (heart failure with mid-range ejection fraction).
Findings
In the REDUCE LAP-HF-Trial, the IASD was studied in 64 patients with HFpEF and HFmrEF in a multicentre, open-label, single-arm, phase I trial [5]. Patients were included if they had evidence of functional class II, III or IV heart failure, an ejection fraction ≥40% and a pulmonary capillary wedge pressure (PCWP) ≥15 mm Hg at rest or ≥25 mm Hg during supine bike exercise.
As a prerequisite for a left atrial to right atrial pressure gradient on the one hand, and to exclude right ventricular failure on the other, central venous pressure (CVP) had to be lower than 14 mm Hg, and tricuspid annular plain systolic excursion (TAPSE) had to be above 14 mm.
Patients had an average age of 69 years, 66% were female, 72% were in New York Heart Association class III, 81% suffered from hypertension and 33% from diabetes. Patients underwent right heart catheterisation at rest and during supine bicycle exercise, both at baseline and 6 months after device implantation. The latter was performed percutaneously via the femoral vein, and the device was positioned using a transseptal puncture of the interatrial septum. IASD placement was successful in 64/66 patients. In two patients, implantation of the device was abandoned without any further consequences for the patients.
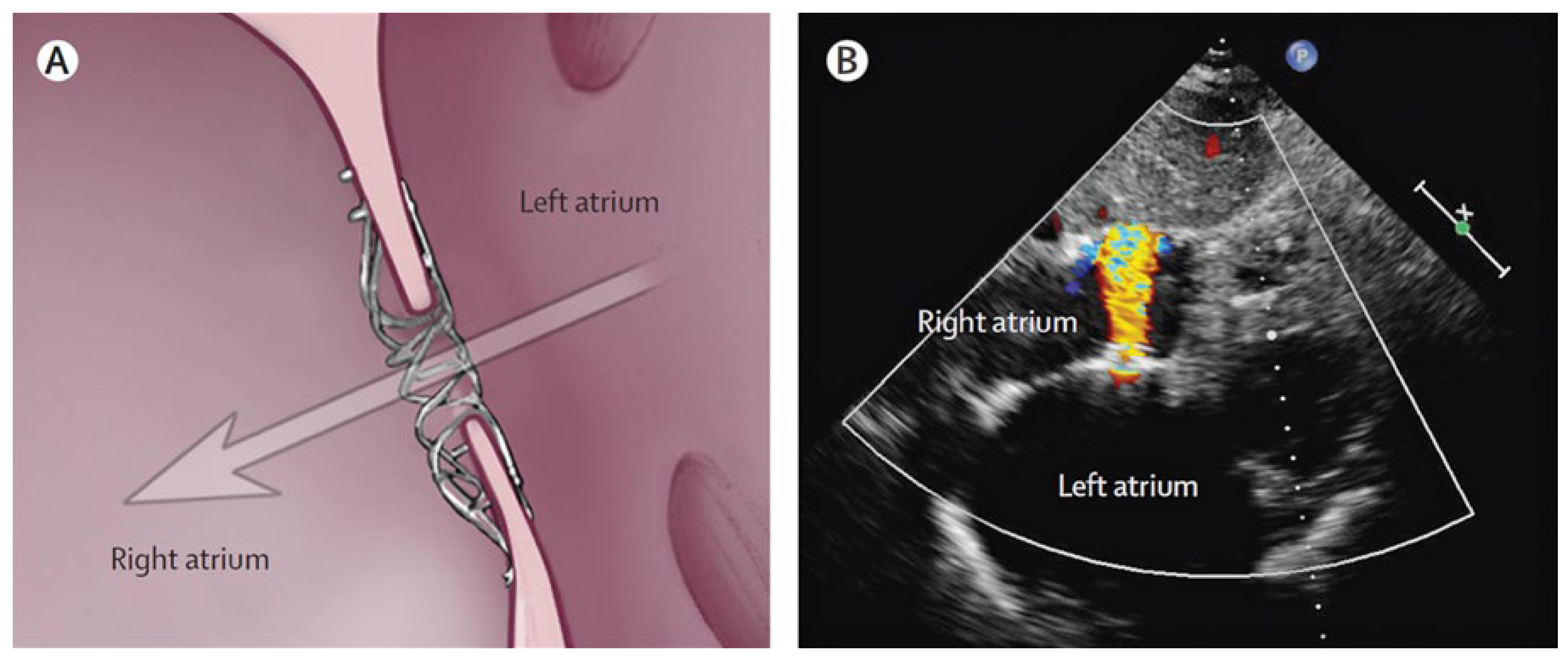
No patient had a major adverse cardiac or cerebrovascular event or a need for cardiac surgical intervention for a device-related complication during 6 months of follow-up. Accordingly, no patient met the primary safety endpoint. The IASD resulted in a pulmonary to systemic flow ratio (Qp/Qs) of 1.27 at 6 months as compared to 1.06 at baseline (p = 0.0004). All patients with adequate echocardiographic image quality at 6 months (n = 50) had evidence of left to right flow through the device on colour flow Doppler echocardiography without any right to left flow (Figure 1).
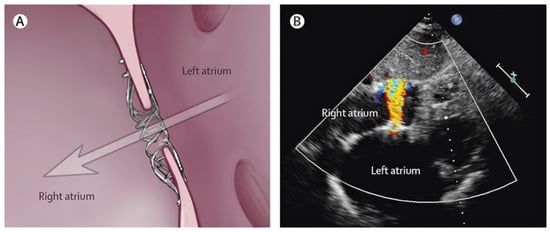
Figure 1.
Interatrial shunt device (IASD). A: Device placement in the interatrial septum, arrow indicates right to left atrial blood flow. B: Echocardiographic image showing colour flow from the left to the right atrium. (Reproduced with permission from Hasenfuss et al. 2016 [5]).
Exercise haemodynamic measurements before device implantation showed significant rises in PCWP from 17 ± 5 to 35 ± 8 mm Hg, and in RA from 9 ± 4 to 11 ± 5 mm Hg from rest to peak exercise. The shunt driving pressure (PCWP–CVP) increased from rest to exercise from 8 ± 4 to 17 ± 8 mm Hg. The mean exercise time before device implantation was 7.3 ± 3.1 min at a work load of 43 ± 18 W.
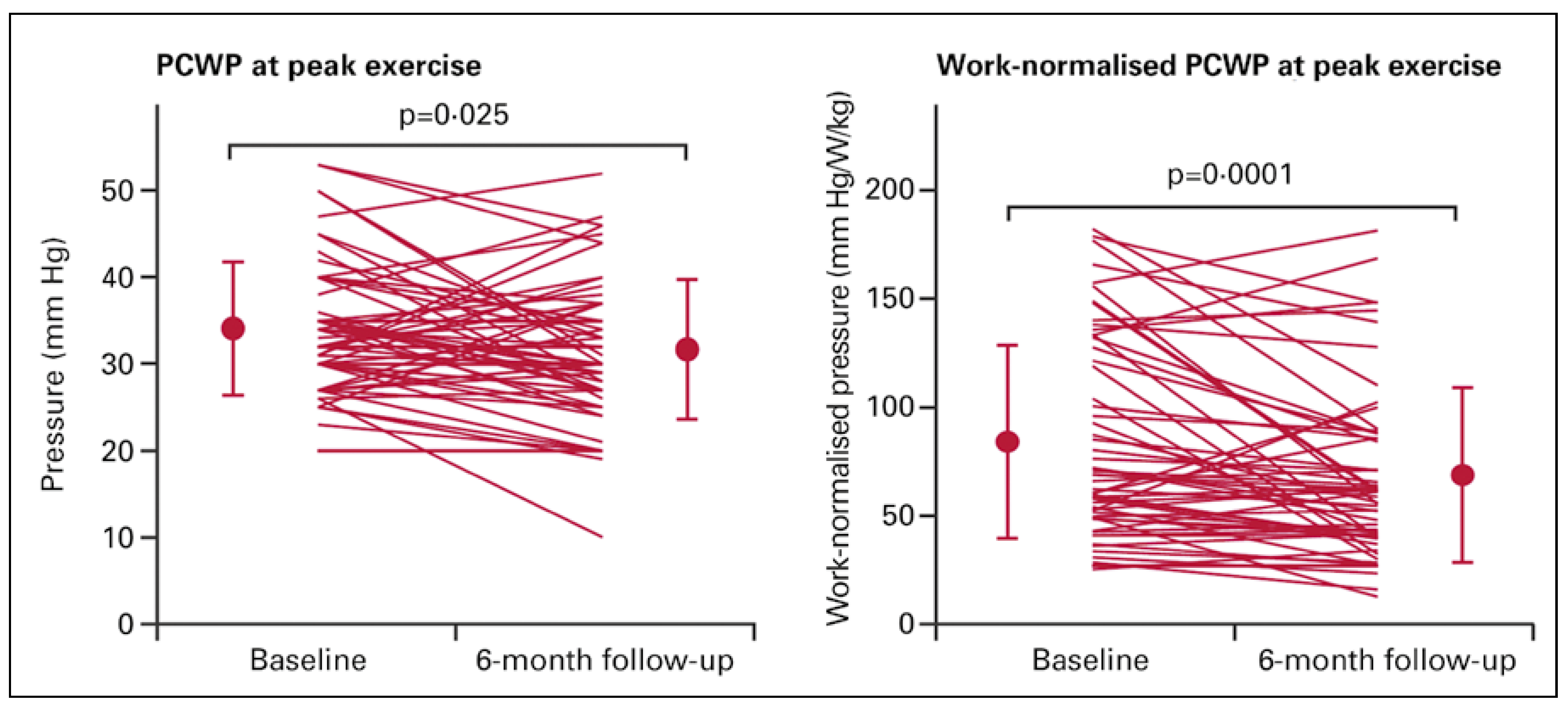
Exercise time increased to 8.2 min ± 3.4 (p = 0.0275) and work load increased to 49 ± 20 W at 6 months after IASD implantation. These favourable changes were associated with a reduction of peak exercise PCWP from 34 ± 8 to 32 ± 8 mm Hg (p = 0.00255) (Figure 2). The reduction in PCWP should be interpreted relative to the increased exercise duration at a higher work load. Consequently, workload- and weight-normalised PCWP (PCWP/W/kg) may most appropriately assess the impact of IASD on exercise performance. Workload- and weight-normalised PCWP at peak exercise was reduced from 84 ± 45 to 69 ± 40 mm Hg/W/kg (p = 0.0001).
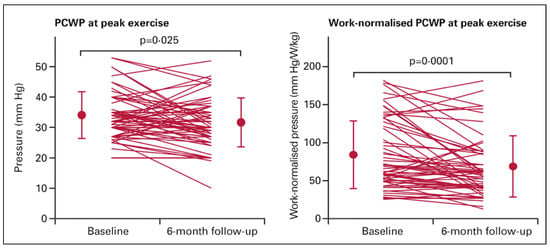
Figure 2.
Haemodynamic effects of an interatrial shunt device (IASD) before and 6 months after implantation. Left: pulmonary capillary wedge pressure (PCWP) at peak exercise. Right: workload- and weight-normalised PCWP. (Reproduced with permission from Hasenfuss et al. 2016 [5].).
At 6 months, resting right atrial pressure had increased slightly compared with baseline, from 9 ± 4 to 11 ± 5 mm Hg (p = 0.0270). Pulmonary vascular resistance was unchanged. Right ventricular diastolic volume index increased from 22 ± 9 to 27 ± 11 ml/m² (p <0.0001) and right atrial volume index increased from 35 ± 17 to 40 ± 22 ml/ m² (p <0.0145). Left ventricular diastolic volume index decreased from 68 ± 13 to 62 ± 17 ml/m² (p = 0.0004), and left atrial volume index did not significantly change. TAPSE was not influenced by the IASD (20 ± 4 mm before and after implantation of the device).
The favourable haemodynamic effects of IASD observed in the open-label single-arm study were confirmed in a double blind randomised sham-controlled trial (REDUCE LAP-HF I Trial). The inclusion criteria were similare to those of the REDUCE LAP-HF-Trial. Twenty-two patients were randomised to IASD implantation and 22 to a control sham procedure. The latter included femoral venous access with intracardiac echocardiography, but no IASD placement. Haemodynamics during rest and exercise at baseline and at 1 month after randomisation were compared. There were no periprocedural or 1-month major adverse cardiovascular, cerebrovascular and renal events in the IASD group. The primary performance endpoint, exercise PCWP at 1 month, decreased significantly in the IASD-treated group compared with the sham control group. The secondary endpoints − exercise duration, peak exercise workload, and workload- and weight-corrected PCWP − all improved in the IASD treatment group compared with the control group, although the differences did not achieve statistical significance as the trial was not powered to demonstrate effectiveness in these endpoints [7].
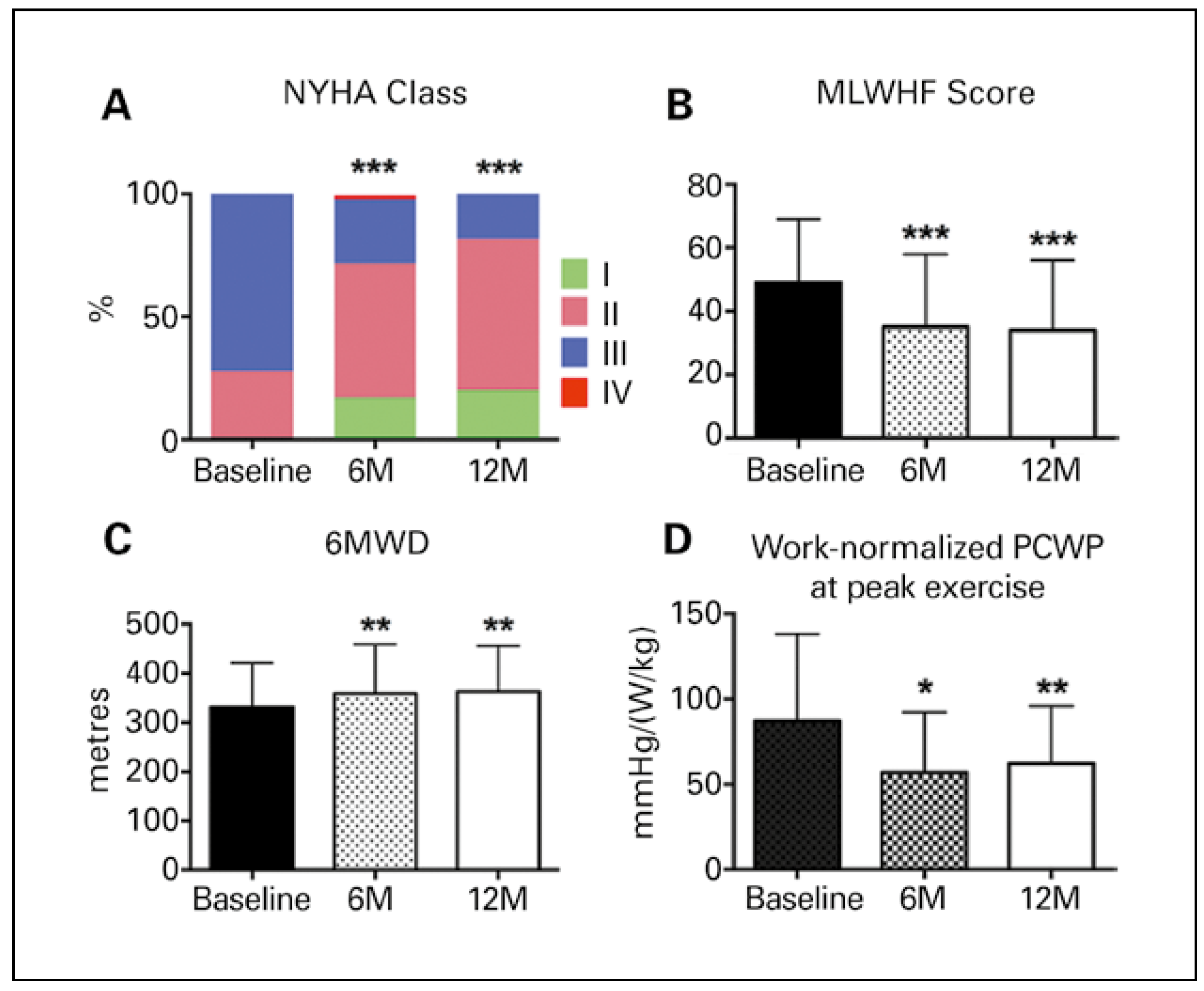
Favourable haemodynamic changes with the IASD explain the symptomatic and functional improvement of the patients after 6 and 12 months of follow-up [8]. Patients in the REDUCE LAP-HF-Trial showed significant improvements in NYHA functional class, Minnesota living with heart failure questionnaire and 6-minute walk distance. The latter was 313 ± 105 m at baseline, 345 ± 106 m at 6 months and 363 ± 93 m at 12 months (Figure 3).
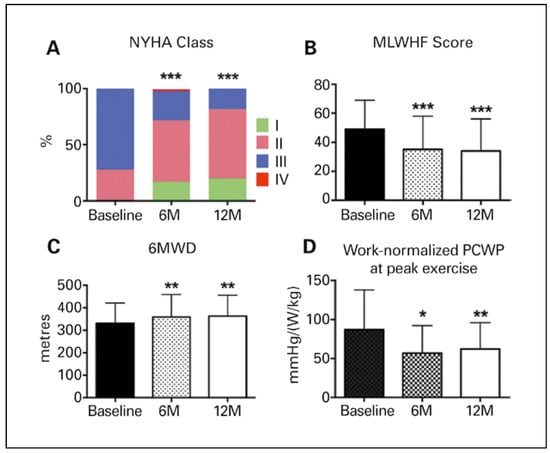
Figure 3.
Symptomatic and functional improvement after intra-atrial shunt device (IASD over 12 months). A: NYHA class = New York Heart Association Functional Class; B: MLWHF score = Minnesota Living With Heart Failure Questionnaire; C: 6MWD = 6-minute walking distance; D: Work-normalised PCWP at peak exercise = work- and weight-normalised pulmonary capillary wedge pressure at peak exercise. (Reproduced with permission from Kaye et al. 2016 [8].).
Haemodynamic findings at 12 months in a subset of patients were comparable to those at 6 months with a persisting improvement in workload- and weight-normalised PCWP (Figure 3). Importantly, there was no haemodynamic or echocardiographic evidence of shunt-induced pulmonary hypertension or right ventricular failure.
Discussion
The studies show that the IASD is safe, reduces PCWP and functions properly through 12 months of follow-up. The persistent left to right shunt reduces exercise PCWP without any adverse effects on right heart function and pulmonary circulation. Beneficial haemodynamic effects are associated with symptomatic and functional improvement of patients with HFpEF and HFmrEF.
The data available from the IASD studies support the hypothesis that elevated left atrial pressure (as indicated by PCWP) inducing post-capillary pulmonary hypertension significantly contributes to the symptoms of patients with “diastolic heart failure” and that reducing left atrial pressure may represent a new therapeutic approach in these patients. This conclusion is consistent with previous work indicating that pulmonary artery pressure is of key pathophysiological relevance in patients with HFpEF [9]. Moreover, there is considerable evidence that pulmonary artery pressures are predictors of mortality in these patients [4,10].
Pulmonary artery pressure can be reduced by vasodilators and diuretics, and it has been shown that medical therapy guided by pressure monitoring reduces heart failure hospitalisation, whereas no other therapeutic approach (with the exception of exercise training) has yet shown to be effective in this group of patients [9]. These data, together with the available date from the IASD creates much enthusiasm that reducing pulmonary artery pressure by a persistent shunt may be a new therapeutic option in patients with HFpEF and HFmrEF, and perhaps also in HFrEF.
The IASD approach critically depends on the left to right pressure gradient to drive the shunt and the size of the hole in the atrial septum. As an inclusion criterion in the IASD studies, PCWP had to be above 15 mm Hg, and CVP below 14 mm Hg. These inclusion criteria resulted in an average PCWP–CVP difference of 8 mm Hg at rest and 17 mm Hg at peak exercise. The ISAD device creates a septal defect of 8 mm cross-section, which in turn results in a Qp/Qs of 1.27. This communication appears to be large enough for continuous shunting and long-term patency without any evidence of paradoxical embolisation. Moreover, in these patients without right heart failure before device implantation (TAPSE >14 mm) the shunt did not result in impaired right ventricular function or increased pulmonary vascular resistance. The latter is consistent with previous recommendations that an atrial septal defect needs no therapeutic closure below a Qp/Qs of 1.5.
Finally, the haemodynamic findings support previous recommendations that HFpEF (or HFmrEF) may require haemodynamic testing during exercise [2,11]. In all IASD-studies, 30% of patients would not have met the inclusion criteria at rest, but showed clearly elevated pulmonary artery pressures during exercise.
In conclusion, reducing pulmonary artery pressure with the IASD may be a new therapeutic option to treat symptomatic HFpEF and HFmrEF patients.
Disclosure Statement
No financial support and no other potential conflict of interest relevant to this article was reported. G. Hasenfuss and D. M. Kaye have been PIs of reported IASD trials.
References
- Lam, C.S.; Donal, E.; Kraigher-Krainer, E.; Vasan, R.S. Epidemiology and clinical course of heart failure with preserved ejection fraction. Eur J Heart Fail. 2011, 13, 18–28. [Google Scholar] [CrossRef] [PubMed]
- Borlaug, B.A.; Kane, G.C.; Melenovsky, V.; Olson, T.P. Abnomral right ventricular-pulmonary artery coupling with exercise in heart failure with preserved ejection fraction. Eur Heart J. 2016, 37, 3293–3302. [Google Scholar] [CrossRef] [PubMed]
- Burkhoff, D.; Maurer, M.S.; Packer, M. Heart failure with a normal ejection fraction: Is it really a disorder of diastolic function? Circulation 2003, 107, 656–658. [Google Scholar] [CrossRef] [PubMed]
- Dorfs, S.; Zeh, W.; Hochholzer, W.; Jander, N.; Kienzle, R.P.; Pieske, B.; et al. Pulmonary capillary wedge pressure during exercise and long-term mortality in patients with suspected heart failure with preserved ejection fraction. Eur Heart J. 2014, 35, 3103–3112. [Google Scholar] [CrossRef] [PubMed]
- Hasenfuß, G.; Hayward, C.; Burkhoff, D.; Silvestry, F.E.; McKenzie, S.; Gustafsson, F.; et al. A transcatheter intracardiac shunt device for heart failure with preserved ejection fraction (REDUCE LAP-HF): A multicenter, open-label, single-arm, phase 1 trial. Lancet 2016, 387, 1298–1304. [Google Scholar] [CrossRef] [PubMed]
- Del Trigo, M.; Bergeron, S.; Bernier, M.; Amat-Santos, I.J.; Puri, R.; Campelo-Parada, F.; et al. Unidirectional left-to-right interatrial shunting for treatment of patients with heart failure with reduced ejection fraction: A safety and proof-of-principle cohort study. Lancet 2016, 387, 1290–1297. [Google Scholar] [CrossRef] [PubMed]
- Feldman, T.; Mauri, L.; Kahwash, R.; Litwin, S.; Ricciardi, M.J.; van der Harst, P.; et al. A transcatheter interatrial shunt device for the treatment of heart failure with preserved ejection fraction (REDUCE LAP-HF I): A phase 2, Randomized, Sham-controlled trial. Circulation 2018, 137, 364–375. [Google Scholar] [CrossRef] [PubMed]
- Kaye, D.M.; Hasenfuß, G.; Neuzil, P.; Post, M.C.; Doughty, R.; Trochu, J.-N.; et al. One-Year Outcomes After Transcatheter Insertion of an Interatrial Shunt Device for the Management of Heart Failure With Preserved Ejection Fraction. Circ Heart Fail. 2016, 9, e003662. [Google Scholar] [CrossRef] [PubMed]
- Adamson, P.B.; Abraham, W.T.; Bourge, R.C.; Costanzo, M.R.; Hasan, A.; Yadav, C.; et al. Wireless pulmonary artery pressure monitoring ruides management to reduce decompensation in heart failure with preserved ejection fraction. Circ Heart Fail. 2014, 7, 935–944. [Google Scholar] [CrossRef] [PubMed]
- Zile, M.R.; Bennett, T.D.; El Hajj, S.; Kueffer, F.J.; Baicu, C.F.; Abraham, W.T.; et al. Intracardiac Pressures Measured Using an Implantable Hemodynamic Monitor: Relationship to Mortality in Patients With Chronic Heart Failure. Circ Heart Fail. 2017, 10, e003594. [Google Scholar] [CrossRef] [PubMed]
- Borlaug, B.A.; Nishimura, R.A.; Sorajja, P.; Lam Carolyn, S.P.; Redfield, M. Exercise hemodynamics enhance diagnosis of early heart failure with preserved ejection fraction. Circ Heart Fail. 2010, 3, 588–595. [Google Scholar] [CrossRef] [PubMed]
© 2018 by the author. Attribution - Non-Commercial - NoDerivatives 4.0.