Abstract
The use of coronary physiology to guide myocardial revascularisation was shown to improve clinical outcomes and reduce costs in patients with coronary artery disease. Fractional flow reserve (FFR) is the most commonly used pressure-derived physiological index for coronary lesion assessment, being supported by a body of compelling randomised evidence, but its uptake into clinical practice remains unacceptably low. The instantaneous wave-free ratio (iFR) is a novel adenosine-free pressure-derived index of coronary stenosis severity that was recently introduced to circumvent the limitations of existing hyperaemic pressure-derived indices with the aim of increasing the widespread adoption of coronary physiology assessment. Following the recent publication of two large-scale, randomised, patient outcome clinical trials, iFR has emerged as a simpler, safe and effective alternative to FFR to guide coronary revascularisation. This has led to renewed interest in the field of coronary physiology and challenges current paradigms supporting the need for pharmacologically-induced maximal hyperaemia as an essential requirement for coronary stenosis assessment. This review aims at addressing the physiological concepts and patient outcome evidence supporting the use of iFR and discuss the recent development of novel iFR-based applications allowing full integration of invasive coronary physiology in percutaneous coronary intervention planning strategy.
Introduction
Inducible myocardial ischaemia is considered to be a prerequisite for the clinical benefit of coronary revascularisation [1]. In this regard, the introduction of invasive pressure-derived physiological indices to guide myocardial revascularisation represented a major breakthrough in the treatment of patients with coronary artery disease (CAD), by moving the focus of coronary revascularisation from anatomy to physiology [2] (Table 1). The main premise of coronary physiology assessment is to determine the functional significance of individual stenoses at the time of clinical decision-making, providing an objective marker to identify ischaemic lesions, and therefore patients, most likely to benefit from coronary revascularisation [1].

Table 1.
Invasive physiological indices to assess the functional significance of coronary artery stenosis.
Fractional flow reserve (FFR) is the most widely used pressure-derived invasive physiological index for coronary lesion assessment in contemporary clinical practice. FFR is the ratio of the mean distal coronary pressure (Pd) to the mean proximal coronary pressure (Pa) across a stenosis during maximal hyperaemia, a condition that is commonly achieved by the intracoronary or intravenous administration of a potent vasodilator agent, such as adenosine [3,4,5]. Based on the results of landmark clinical trials [6,7,8,9,10,11] (Table 2), most recent guidelines recommend the use of FFR to identify haemodynamically significant coronary lesions in patients with stable CAD [1,12]. Despite this, the worldwide adoption of FFR into current clinical practice remains limited [13], accounting for less than 10% of coronary procedures in Switzerland [14]. Potential reasons for the low uptake of coronary physiology assessment include technical challenges related to FFR measurements, time consumption, inadequate or lack of reimbursement, physician preferences, patient-related discomfort, and contraindications to or costs associated with adenosine. Furthermore, adenosine is either not licensed nor unavailable in some healthcare systems.

Table 2.
Summary of FFR pivotal patient outcome trials.
The instantaneous wave-free ratio (iFR) is a novel pressure-based physiological index of coronary stenosis severity that is measured under resting conditions by making use of the unique properties of baseline coronary physiology and does not require the administration of vasodilator drugs, such as adenosine [15]. iFR has recently emerged as a simpler, safe and effective alternative to FFR to guide coronary revascularisation, contributing to a renewed interest in the field of coronary physiology and challenging current paradigms supporting the need of pharmacologically induced maximal hyperaemia as an essential requirement for coronary stenosis assessment. The purpose of the present review is to address the rationale, fundamentals and available patient outcome data supporting the use of iFR for physiological lesion assessment and discuss present and future applications of the iFR technology.
Fractional flow reserve
FFR is currently considered the gold standard for assessment of the functional significance of coronary stenosis, being supported by a large body of randomised evidence demonstrating its value in clinical decision making [6,7,8,9,10,11]. FFR is defined as the ratio of maximum achievable coronary blood flow (CBF) in the presence of an epicardial coronary stenosis and the theoretical maximum CBF in the hypothetical absence of the coronary stenosis during maximal pharmacological vasodilation [3].
Patient outcome trials
The use of FFR to guide coronary revascularisation is supported by several randomised patient outcome trials (Table 2). DEFER (Deferral versus performance of percutaneous transluminal coronary angioplasty (PTCA) in patients without documented ischaemia) was a prospective, randomised trial including 325 patients with stable CAD referred for elective percutaneous coronary intervention (PCI) who underwent FFR assessment of de novo intermediate coronary lesions [6]. Patients with FFR ≥0.75 were randomly assigned to deferral or PCI, whereas patients with FFR <0.75 underwent PCI as planned (reference group). The primary endpoint was the absence of major adverse cardiac events (MACE) during 24 months of follow-up. Eventfree survival was similar between deferred and treated patients (89 vs 83% at 24 months), but was significantly lower in the reference group (78% at 24 months) [6]. Moreover, the proportion of patients free from angina was similar in deferral and PCI groups (70 vs 51%) but was significantly higher in the reference group (80%) [6]. Subsequently, 5-year follow-up of the DEFER cohort confirmed that long-term outcomes of patients after deferral of PCI in intermediate coronary stenosis with FFR ≥0.75 were excellent [7].
FAME (Fractional Flow Reserve versus Angiography for Multivessel Evaluation) was a prospective, multicentre trial that randomly assigned 1005 patients with multivessel CAD to FFR-guided or to angiography alone-guided coronary revascularisation with drug-eluting stents [8]. The incidence of the primary endpoint of MACE, a composite of death, nonfatal myocardial infarction (MI) or repeat revascularisation at 1 year, was significantly lower in the FFR group compared with the angiography-alone group (13.2 vs 18.3%, respectively; relative risk 0.72, 95% confidence interval [CI] 0.54–0.96; p = 0.02) [8]. Furthermore, physiology-guided revascularisation using a FFR threshold >0.80 was associated with fewer stents, less contrast volume, and reduced costs compared with coronary revascularisation guided by visual assessment only.
In the prospective, multicentre, randomised FAME 2 trial, patients with angiographically documented stable CAD and candidates for PCI underwent FFR assessment to determine the haemodynamic severity of each indicated coronary stenosis [9]. Patients with an FFR ≤0.80 in at least one stenosis were randomly assigned to an FFR-guided PCI strategy plus optimal medical therapy (OMT) or OMT alone, whereas patients with an FFR >0.80 in all vessels with indicated coronary stenoses were enrolled in a registry and received OMT. The primary endpoint was a composite of death, MI, or unplanned hospitalisation leading to urgent revascularisation during the first 2 years. Recruitment was halted prematurely after enrolment of 1220 patients (median follow-up 7 months) owing to a large reduction in the primary composite endpoint in the FFR-guided PCI+OMT group compared with the OMT alone group (4.3 vs 12.7%, respectively; hazard ratio [HR] 0.32, 95% CI 0.19–0.53; p <0.001), driven by significantly lower rates of urgent revascularisation (1.6 vs 11.1%; HR 0.13, 95% CI 0.06–0.30; p <0.001) in the FFR-guided PCI arm. Notably, rates of death from any cause, cardiac death and MI were not statistically different between the two groups [9]. The longer-term follow-up of the FAME 2 trial demonstrated persistent lower rates of the primary composite endpoint in the FFR-guided PCI group, primarily as a result of lower rates of urgent revascularisation in the FFR-guided PCI arm, with no significant between-group differences in the rates of all-cause death, cardiac death, or MI, at 2- [10] and 3-year [11] follow-up.
Based on the results of these landmark studies, current European Society of Cardiology guidelines recommend the use of FFR to identify haemodynamically relevant coronary lesions in stable patients when evidence of myocardial ischaemia is not available (class of recommendation I, level of evidence A) and FFR-guided PCI in patients with multivessel disease (class of recommendation IIA, level of evidence B) [1]. However, despite being endorsed by strong clinical evidence, the use of FFR to guide coronary revascularisation in contemporary practice remains low.
Limitations of the hyperaemic pressure-derived physiological indices
The concept of FFR and hyperaemic pressure-derived indices of coronary stenosis severity depends on the fundamental physiological principle that coronary pressure is directly proportional to CBF when microvascular resistance is stable, a condition that is commonly achieved during the administration of hyperaemic agents, such as adenosine [3,16]. Under these conditions, the decrease in pressure across a coronary stenosis reflects the decrease in CBF to the amount of subtended myocardium. This assumption was translated into the paradigm that coronary pressure can only be considered as a surrogate to CBF during maximal hyperaemia. Nonetheless, the cornerstone of FFR is based on a simplified theoretical model of the coronary circulation, thereby potentially limiting the diagnostic accuracy of FFR in clinical practice.
The relationship between pressure and flow is indeed not linear but curvilinear. The pressure-flow correlation is straight in the physiological range of perfusion pressures (incremental-linear relationship) and curves towards the pressure axis at lower perfusion pressures (non-zero pressure intercept), owing to several conditions such as central venous pressure (deducted from both proximal and distal coronary pressure in the experimental validation of FFR, because considered as negligible), collateral flow, epicardial capacitance and intramyocardial compliance [17]. Furthermore, microcirculatory resistance, which is influenced by many factors including capacitive, inertial and resistive forces, or the complex effects of systolic contraction, fluctuates in a phasic pattern throughout the cardiac cycle even after administration of potent pharmacological agents [15]. These fluctuations reflect the close interaction between myocardium and microcirculation during systole (high intracoronary resistance, microvasculature compression) and diastole (lower intracoronary resistance, microvasculature decompression) [18]. To minimise these effects, the FFR is calculated during hyperaemia and time-averaged over several cardiac cycles to ensure constant intracoronary resistance. Importantly, the actual coronary microvascular resistance values are not routinely measured in clinical practice as they cannot be derived from pressure measurements alone; thus, coronary resistance is assumed to be constant (and minimal). This represents a potential source of error in the assessment of FFR, as any unaccounted variability in minimal microvascular resistance will influence FFR values. The impact of this variability is more relevant in lesions within the intermediate range of coronary stenosis severity than for minimally obstructed coronary arteries [17].
The achievement of maximal hyperaemia in clinical practice is less attainable than currently acknowledged. Adenosine is the most widely used vasodilatory pharmacological agent and represents the current gold standard to induce maximal hyperaemia during FFR measurements [19]. Nevertheless, the vasodilatory response to adenosine may be incomplete in some patients as a result of the complex physiological mediation of vascular tone, therefore precluding achievement of a true and predictable maximal hyperaemic state in all patients [17]. Accordingly, hyperaemic microvascular resistance during vasodilatation induced by adenosine is highly variable between patients, and between adjacent perfusion territories within the same patient, thus compromising the validity of the FFR concept [17]. Finally, adenosine is associated with significant adverse effects and patient discomfort such as dyspnoea, chest pain and headache, and is contraindicated in patients with documented allergy to adenosine or severe asthma.
Hyperaemia-free pressure-derived indices of coronary stenosis severity
Adenosine-free pressure-derived physiological indices were recently introduced to further simplify physiological coronary assessment. By negating the need for administration of pharmacological agents such as adenosine, saving time, and reducing costs and side effects, hyperaemia-free pressure-derived physiological indices were developed to increase adoption of physiology-guided coronary revascularisation into routine clinical practice. Pioneering studies performed more than 40 years ago demonstrated that, whereas hyperaemic CBF was affected only when the coronary lumen was reduced by at least 50%, resting CBF remained unaltered until the coronary lumen diameter was reduced by at least 85%, owing to the counteractive effects of coronary autoregulation [20]. With progressive narrowing of the coronary lumen, coronary autoregulation maintains a constant CBF through compensatory vasodilatation of the distal coronary resistance vessels. The stable baseline CBF conditions therefore provide an ideal environment for the development of resting pressure-based indices of coronary stenosis severity.
Instantaneous wave-free ratio
Fundamentals
iFR is a novel non-hyperaemic pressure-derived index of coronary stenosis severity, which is measured at rest by using the unique properties of baseline coronary physiology, and does not require administration of potent pharmacological vasodilator agents, such as adenosine. iFR is measured during a specific period of diastole, called the wave-free period (WFP), when CBF is intrinsically at its highest compared with the whole cardiac cycle [15]. By means of measurement during a higher flow velocity, the capacity to discriminate between stenosis severities at rest is amplified and greater than during any other phase of the cardiac cycle.
The WFP was originally isolated by application of wave-intensity analysis (WIA). Pioneering work using WIA demonstrated that the forces propagating from the proximal vessel (aorta and other systemic arteries) conflict with those travelling from the distal end (microcirculation) [18]. During the WFP, a specific diastolic period, no new waves are generated and competing waves affecting CBF are quiescent [15] (Figure 1). During this time window, coronary flow velocity is approximately 30% higher than whole-cycle resting flow velocity, intracoronary pressure and flow decline linearly and microcirculatory resistance is significantly more stable and lower than over the rest of cardiac cycle [15]. Importantly, this period of the cardiac cycle was found to have the lowest and most stable resistance attainable under resting conditions without the need for maximal pharmacological vasodilation [15]. Accordingly, the iFR is calculated as the ratio of distal coronary pressure to proximal aortic pressure during the WFP [15]. Notably, iFR can be calculated on a beat-by-beat basis without requiring several beats to be averaged, including during irregular heart rhythms, such as atrial fibrillation [15]. The IDEAL (Iberian-Dutch-English) study provided the physiological framework for iFR by analysing pressure-flow relationship in a wide range of stenosis severities under both resting and hyperaemic conditions [22]. The study demonstrates that pressure gradients across coronary stenosis at rest are predominantly determined by compensatory vasodilator changes in microvascular resistance due to coronary autoregulation [22]. These findings supported the translation of early coronary physiological concepts derived from animal models to CAD patients by suggesting that resting pressure-derived indices could be used to determine haemodynamic significance of coronary artery stenoses in clinical practice.
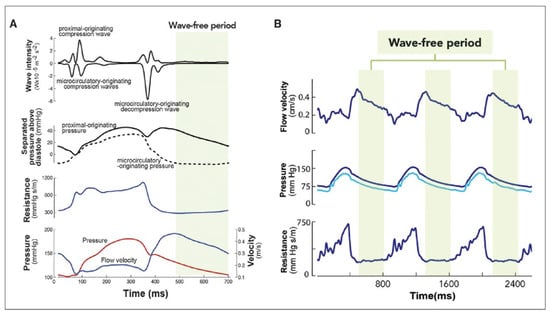
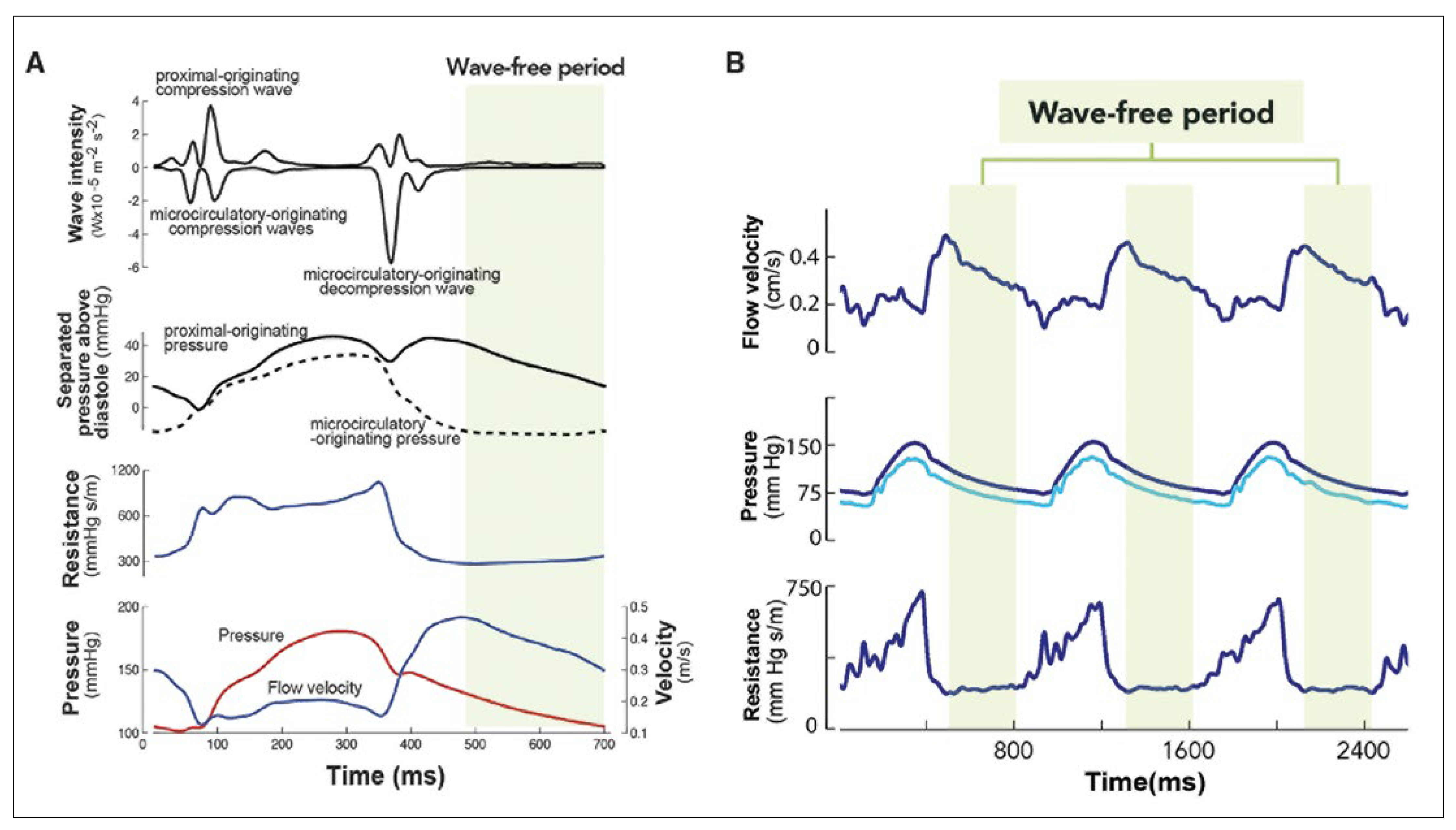
Figure 1.
Basic concepts of iFR. (A) Wave-intensity analysis demonstrates the proximal and distal (microcirculatory) originating waves generated during the cardiac cycle. A wave-free period is identified in diastole when no new waves are generated (green) corresponding to a time period in which there is minimal microcirculatory-originating pressure, minimal and constant resistance and a nearly constant rate of change in coronary flow velocity. (B) Coronary flow velocity, proximal and distal pressure traces and instantaneous resistance demonstrate the beat-to-beat stability of the wave-free period. Flow velocity over the wave-free period is higher than that over the whole cardiac cycle, allowing greater discrimination between stenosis severities than over the whole cycle at rest. Reprinted with permission from Nijjer SS, Sen S, Petraco R, Davies JE. Advances in coronary physiology. Circ J. 2015;79(6):1172–84.
Early validation studies
The ADVISE (Adenosine Vasodilator Independent Stenosis Evaluation) [15] and ADVISE registry [23] studies assessed the diagnostic accuracy of iFR compared with FFR. In the ADVISE validation study, iFR was found to correlate closely with FFR with excellent diagnostic accuracy (receiver-operating characteristic [ROC] area under the curve 93%, at FFR cut-off threshold of 0.80), specificity (91%), sensitivity (85%), negative (85%) and positive (91%) predictive values [15]. In a large-scale core laboratory-based analysis, the overall linear correlation between iFR and FFR was moderate with an overall diagnostic accuracy of ≈80% using the optimal ROC-determined iFR cut-off of 0.90 to predict a FFR ≤0.80, which can be improved to ≥90% in a subset of lesions [24]. In the international ADVISE registry including 312 patients with angiographically intermediate stenoses, a close classification agreement was found between iFR and FFR (area under ROC curve 86%). To match an FFR value of 0.80, the ROC curve identified an optimal iFR cut-off value of 0.89. Further validation studies showed that iFR with a cut-point of 0.89 had diagnostic accuracy that was at least as good as, and in some cases superior to, FFR when compared with hyperaemic stenosis resistance [25,26], myocardial perfusion studies [27] and positron emission tomography [28].
The iFR-FFR hybrid strategy
The high classification agreement between FFR and iFR outside of the intermediate zone provided the rationale for the use of a staged, hybrid iFR-FFR decision-making strategy, in which only patients within a certain range of intermediate iFR values (0.86–0.93) would require adenosine for FFR classification of lesions [29]. With an FFR cut-off value of 0.80, an iFR <0.86 was associated with a high positive predictive value (92%) to confirm treatment, whereas an iFR >0.93 was associated with a high negative predictive value (91%) to defer treatment. Limiting the use of adenosine to cases with iFR values between 0.86 to 0.93 obviated the need for a vasodilator drug in 57% of patients (76% in the FFR 0.75–0.80 range), while maintaining 95% agreement with an FFR-only strategy [29]. However, with the recent publication of randomised patient outcome trials comparing iFR using a single cut-off value with FFR to guide coronary revascularisation, the routine use of an iFR-FFR hybrid strategy is currently not recommended.
Patient outcome trials
Recently, two large-scale, randomised, controlled, patient outcome trials, DEFINE-FLAIR (Functional Lesion Assessment of Intermediate Stenosis to Guide Revascularisation) [30] and iFR-SWEDEHEART (Evaluation of iFR versus FFR in Stable Angina or Acute Coronary Syndrome) [31], addressed the question as to whether iFR was a safe and effective alternative to the established gold standard FFR to guide to coronary revascularisation in patients with CAD. The DEFINE-FLAIR and iFR-SWEDEHEART studies were designed similarly, with prespecified single thresholds for treatment (iFR ≤0.89, FFR ≤0.80) and deferral (iFR >0.89, FFR >0.80), and the primary endpoint was standardised as the 1-year risk of MACE, defined as a composite of all-cause death, nonfatal MI or unplanned revascularisation. The DEFINE-FLAIR and iFR-SWEDEHEART trials were designed to investigate the noninferiority of iFR to FFR with respective noninferiority margins of 3.4 and 3.2% for the difference in risk. Importantly, these noninferiority margins were more conservative than margins commonly used in studies evaluating medical devices or drugs [31,32]. Overall, the main results of DEFINE-FLAIR and iFR-SWEDEHEART trials were remarkably concordant in demonstrating that coronary revascularisation guided by iFR was noninferior to an FFR-guided strategy with respect to 1-year clinical outcomes. The DEFINE-FLAIR and iFR-SWEDEHEART studies represent a major step forward in the field of invasive coronary physiology assessment by expanding significantly the available randomised patient outcome data for physiology-guided coronary revascularisation (Table 3). Moreover, DEFINE-FLAIR and iFR-SWEDEHEART trials provide the first randomised evidence for iFR-guided decision making for coronary revascularisation and validated the use of a single iFR 0.89 cut-off value in clinical practice, thereby eliminating the need of a diagnostic grey zone or a hybrid approach.

Table 3.
Summary of pivotal iFR patient outcome trials.
DEFINE-FLAIR is the largest randomised trial to date assessing use of coronary physiology to guide myocardial revascularisation. DEFINE-FLAIR was a prospective, multicentre, international, double-blinded, randomised, noninferiority trial that randomly assigned 2492 patients with at least one intermediate coronary artery stenosis of questionable physiological severity in a 1:1 ratio to undergo either iFR-guided or FFR-guided coronary revascularisation [30]. Patients with stable CAD or with acute coronary syndrome (ACS) with bystander intermediate CAD in non-culprit vessels were included. Unlike the study populations included in the landmark DEFER and FAME trials (mean FFR values 0.71 and 0.75, respectively), the mean FFR value of patients included in DEFINE-FLAIR was 0.83 ± 0.09 (Table 3), emphasising that the majority of patients presented with lesions that truly fell in the intermediate severity range, and therefore that conclusions from the study are relevant for the patients whom iFR and FFR were originally designed to investigate. The primary endpoint was the 1-year risk of MACE, a composite of death from any cause, nonfatal MI, or unplanned revascularisation. At 1-year follow-up, coronary revascularisation guided by iFR was noninferior to revascularisation guided by FFR with respect to the risk of MACE (6.8 vs 7.0%; difference in risk 0.2 percentage points; 95% CI 2.3–1.8; p <0.001 for noninferiority; HR 0.95; 95% CI 0.68–1.33; p = 0.78). The incidence of individual components of the composite endpoint did not differ significantly between the two groups. Importantly, the number of patients who had adverse procedural symptoms and clinical signs was significantly lower (3.1 vs 30.8%, p <0.001) and the median procedural time was significantly shorter (40.5 vs. 45.0 minutes, p = 0.001) in the iFR group than in the FFR group.
iFR-SWEDEHEART was a multicentre, open-label, registry-based, randomised, controlled clinical trial that used the Swedish Coronary Angiography and Angioplasty Registry (SCAAR) for enrolment [31]. iFR-SWEDE-HEART randomly assigned 2037 participants with stable CAD or ACS with an intermediate stenosis in a non-culprit artery, and an indication for physiologically guided assessment of coronary artery stenosis in a 1:1 ratio to undergo revascularisation guided by either iFR or FFR. The primary endpoint was the rate of a composite of death from any cause, nonfatal MI infarction, or unplanned revascularisation at 12 months. At 1-year follow-up, the primary endpoint occurred similarly in the iFR and FFR groups (6.7 vs 6.1%, respectively; difference in risk 0.7%; 95% CI –1.5–2.8; p = 0.007 for noninferiority). There were no significant between-group differences in the risk of each component of the composite endpoint. The study results were consistent within major subgroups, and the rates of ischaemic endpoints, including MI, target-lesion revascularisation, in-stent restenosis and stent thrombosis, did not differ significantly between the two groups. Similarly to DEFINE-FLAIR, a significantly higher proportion of patients in the FFR group than in the iFR group reported chest discomfort during the procedure (68.3 vs 3.0%, respectively; p <0.001). Furthermore, the total number of lesions assessed was significantly greater in the iFR group than in the FFR group, which was possibly related to the fact that operators using FFR are unlikely to persist with additional lesion assessment in patients experiencing adenosine-related chest discomfort. These findings tend to support the central notion that iFR is a much more tolerable procedure and therefore permits an easier and a more complete assessment of coronary anatomy.
Pooled patient-level meta-analysis of DEFINE-FLAIR and iFR-SWEDEHEART
The pooled patient-level meta-analysis of DEFINE-FLAIR and iFR-SWEDEHEART studies yields the largest dataset of CAD patients managed with coronary physiology assessment in contemporary clinical practice and provides outcome data for a total of 4529 patients with intermediate coronary artery lesions undergoing physiology-guided coronary revascularisation. Overall, the patient-level meta-analysis confirmed the non-inferiority of iFR versus FFR to guide coronary revascularisation (HR 1.03, 95% CI 0.81–1.31; p = 0.81) [33].
Physiology-guided deferral of coronary revascularisation occurred more frequently in the pooled iFR group than in the pooled FFR group (50.0 vs 45.0%, respectively; p <0.01). Deferral of physiologically insignificant lesions was found to be safe with similarly low rates of MACE at 12 months, irrespective of iFR- or FFR-based deferral (4.12 vs 4.05%, respectively; HR 1.05, 95% CI 0.69–1.60; p = 0.82). These results suggest similar patient outcomes with iFR- and FFR-guided deferral despite coronary revascularisation being performed less frequently in the iFR arm, and highlight the fundamental physiological differences between iFR and FFR concepts. Particularly, iFR has been shown to be more closely linked to CBF than FFR [34], and a previous study demonstrated higher revascularisation rates associated with physiological assessment guided by FFR than by coronary flow rate (CFR) [35].
Finally, the combined patient-level analysis of DEFINE-FLAIR and iFR-SWEDEHEART trials provides unique randomised evidence comparing iFR with FFR for the physiological assessment of non-culprit coronary stenoses in a subgroup of 440 patients with ACS. FFR-guided deferral of intervention in ACS patients was associated with a significantly increased risk of MACE compared with FFR-guided deferral in patients with stable CAD (HR 0.52, 95% CI 0.27–1.00; p <0.05), whereas iFR-guided deferral was associated with similar rates of MACE, irrespective of the clinical presentation (HR 0.74, 95% CI 0.38–1.43; p = 0.37) [33]. These data suggest that FFR may be an inferior prognostic marker for deferring treatment of non-culprit lesions in ACS patients compared with iFR, probably because of a blunted response to hyperaemic agents in the stunned myocardium following ACS [33].
Limitations of the iFR concept
Despite being supported by robust preclinical studies and validated by randomised patient outcome trials, iFR has experienced significant scrutiny and sparked intense debate in the literature over recent years. By making use of baseline coronary physiology properties, the iFR concept undoubtedly has limitations [34,35,36] (Table 1). Furthermore, longer-term outcome results of the DEFINE-FLAIR trial are warranted, particularly with respect to deferred-intervention patients, on the assumption that the use of iFR may reduce referrals for coronary revascularisation compared with FFR. Randomised outcome data are also needed in higher-risk patient subgroups with more complex coronary lesions (left main or proximal coronary artery disease) and higher baseline cardiovascular risk (bystander coronary lesions in patients with ACS, including ST-elevation MI), where coronary revascularisation may result in survival benefit. Finally, randomised clinical studies are warranted to determine clinical outcomes in patients with discordant iFR and FFR values, particularly for iFR negative and FFR positive patients.
Novel iFR-based physiological applications
iFR pullback
Tandem lesions and diffusely diseased vessels represent a challenge to hyperaemic indices such as FFR, owing to the haemodynamic interdependence (“cross-communication”) between serial stenoses under hyperaemic conditions [38]. Hyperaemic flow across one coronary stenosis is limited by presence of another stenosis in the same coronary vessel and vice versa, thereby precluding the simple and accurate determination of FFR for each individual coronary stenosis. As a result, removal of one coronary stenosis by means of PCI increases hyperaemic flow, thereby changing the pressure gradient across the residual stenosis. The unique properties of baseline physiology assessment may overcome the intrinsic limitations of hyperaemic pressure-derived indices and offer a potential solution for the assessment of tandem and/or diffuse lesions [38]. Unlike hyperaemic flow, resting coronary flow is preserved across nearly the entire range of coronary stenosis severities until stenoses become critical or subtotally occluded [20]. Resting pressure changes along the vessel length as measured by iFR are therefore more consistent and predictable than hyperaemic pressure gradients. Resting pressure tracings can be generated on a beat-to-beat basis using iFR pullback, thus permitting haemodynamic significance of each individual coronary stenosis to be accurately mapped and quantified. Importantly, resting coronary flow is not altered by removing a coronary stenosis by the means of PCI, and iFR pressure gradients across any residual coronary stenosis in the same vessel remain therefore unchanged [38]. In a first-in-man pilot study, automated iFR pullback recordings were made in 29 patients with tandem and/or diffuse CAD [39]. A post-hoc iFR physiological map integrating pullback speed and physiological data, co-registered with the patient coronary angiogram, was generated using a dedicated software to calculate physiological stenosis severity, length, and pressure-drop intensity (ΔiFR/mm) across individual coronary stenoses to predict post-PCI iFR, which was ultimately compared with the observed post-PCI iFR (Figure 2). With use of computer-assisted simulations to model the haemodynamic impact of removing a coronary stenosis on the iFR pullback recording, virtual PCI was performed to estimate post-PCI iFR values (Figure 2). The iFR pullback was associated with a high degree of accuracy for predicting post-PCI iFR values, thereby offering a potential solution to facilitate PCI planning strategy in clinical practice [39]. Despite the promising results of this proof-of-concept study, the need for offline analysis and motorised pressure-wire pullback limited the subsequent clinical application of the technology.
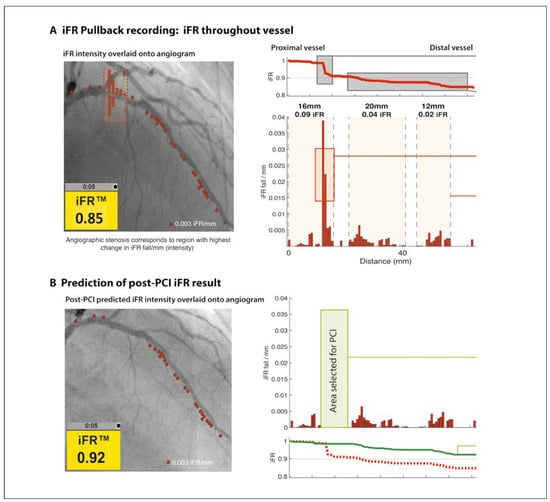
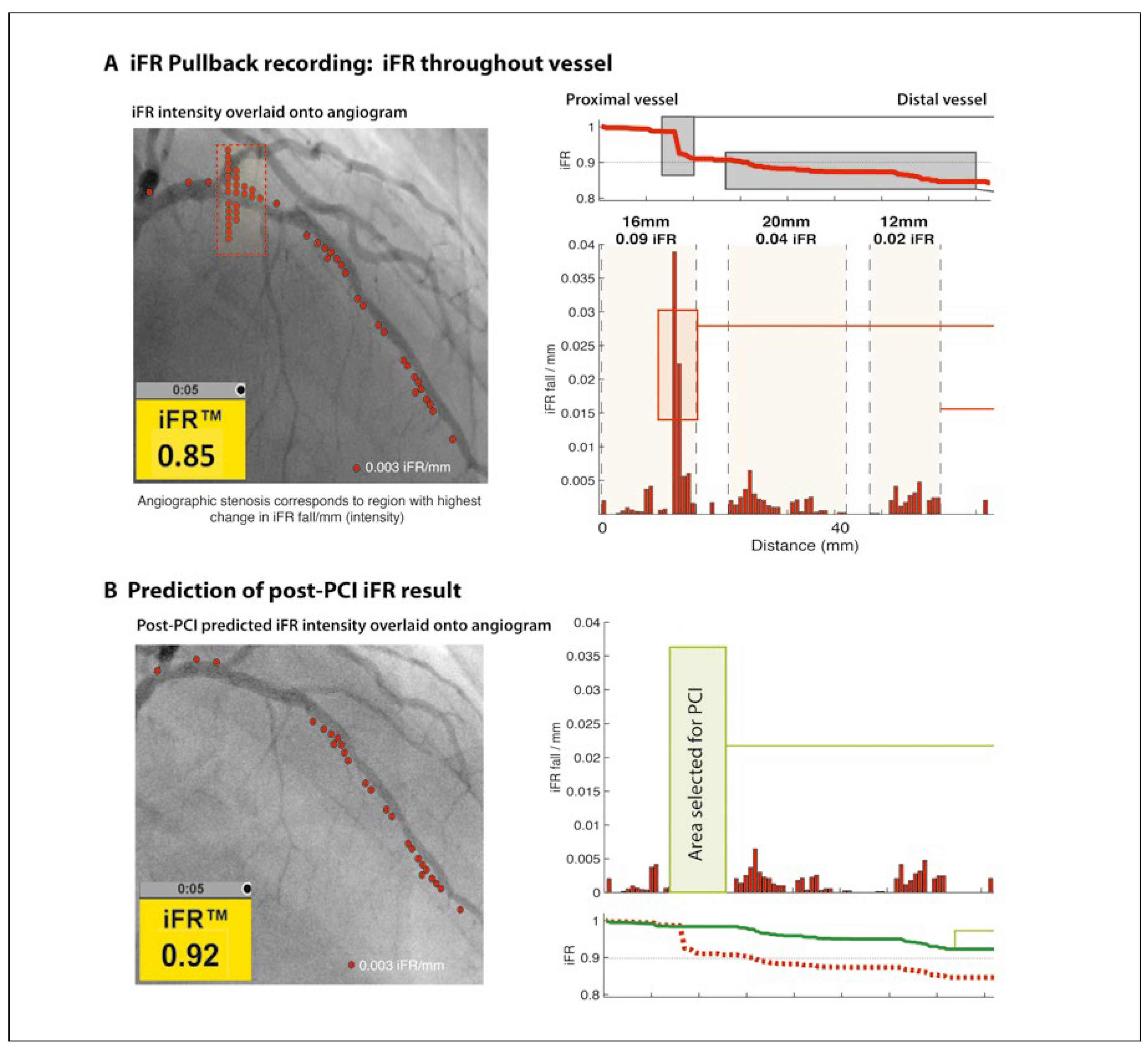
Figure 2.
iFR pullback. (A) iFR pullback recording throughout the coronary vessel. Post hoc co-registration of the iFR pullback trace with the coronary angiogram identifies pressure loss along the length of the vessel and distinguishes focal from diffuse disease. (B) Prediction of the post-PCI iFR result. Virtual PCI calculates the expected post-PCI iFR result for the area selected for PCI. LAD: left anterior descending artery; PCI: percutaneous coronary intervention. Reprinted with premission from Elsevier from Nijjer SS, Sen S, Petraco R, Escaned J, Echavarria-Pinto M, Broyd C, et al. Pre-angioplasty instantaneous wave-free ratio pullback provides virtual intervention and predicts hemodynamic outcome for serial lesions and diffuse coronary artery disease. JACC Cardiovasc Interv. 2014;7(12):1386–96.
iFR co-registration
Further developments of the iFR algorithm combined with real-time computer to track the pressure-wire movement progressively removed the remaining technical barriers to facilitate complete integration of the iFR pullback concept into clinical practice. The iFR co-registration technology uses a dedicated proprietary software to create a fully integrated real-time physiological map of the coronary vessel under manual pullback that is co-registered with the patient coronary angiogram (Figure 3). The iFR co-registration technology permits the instantaneous calculation of predicted post-PCI iFR values, thereby determining the potential physiological benefit of different treatment strategies. Revascularisation strategies that maximise the physiological benefit with a minimum of stents over more extensive PCI approaches may be planned to potentially improve patient outcomes. Contrariwise, the iFR co-registration may identify patients for whom greater numbers or longer stents are required in order to achieve haemodynamic improvement. Finally, the iFR co-registration technology enables accurate physiological documentation of angiographically diffuse CAD, thus contributing to the tailoring of treatment strategies at a patient level and the choice appropriate alternative approaches to PCI (medical therapy or surgical revascularisation) in selected patients.
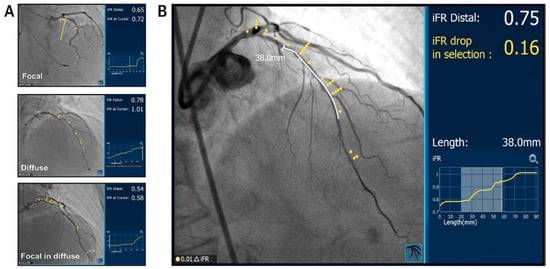
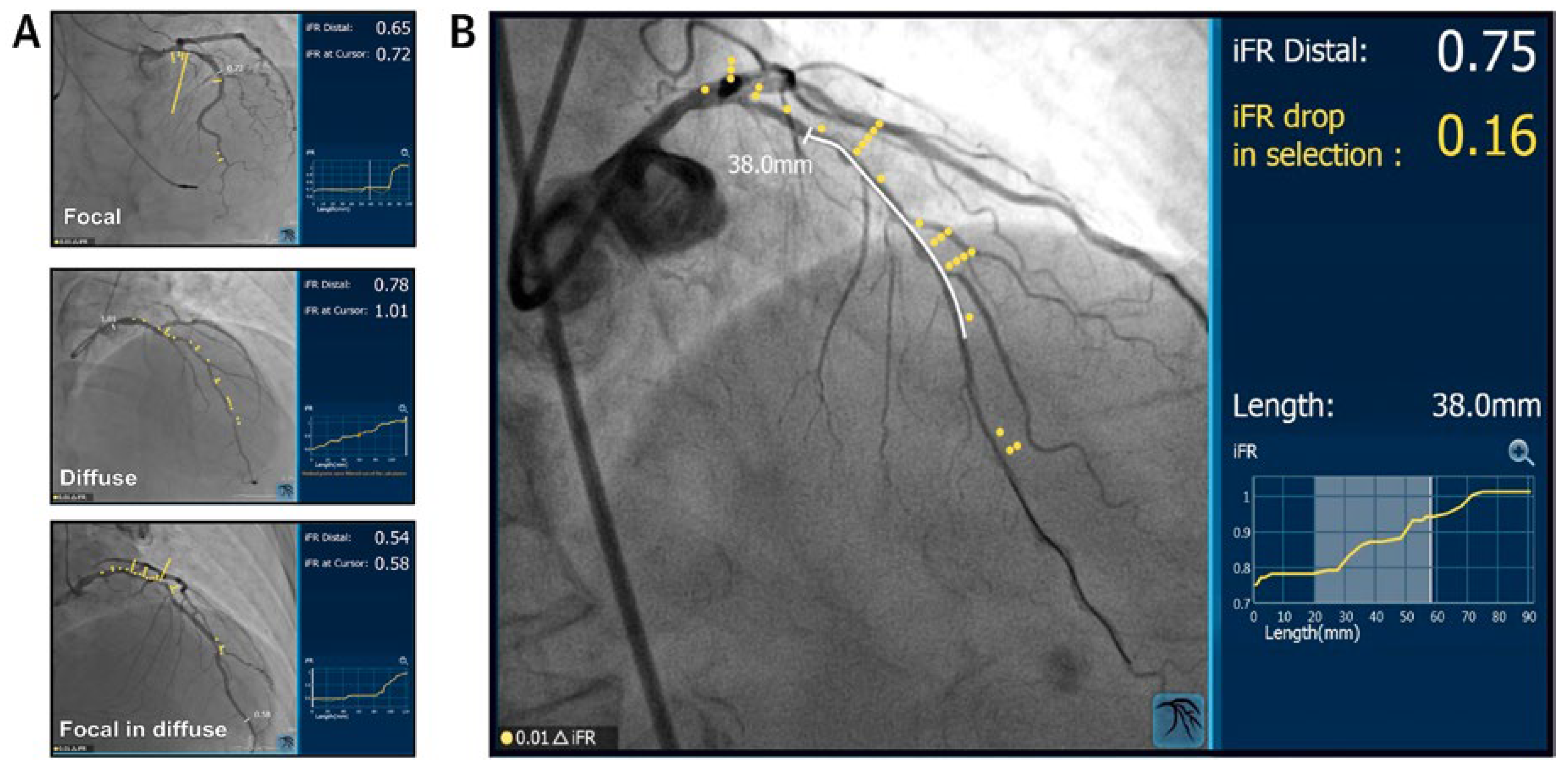
Figure 3.
iFR co-registration. (A) Co-registration of iFR pullback traces with corresponding coronary angiograms demonstrates three distinct patterns of pressure loss along the length of coronary vessels: focal stenosis, diffuse coronary disease, focal stenosis and diffuse coronary disease. (B) iFR co-registration allows virtual percutaneous coronary interventional (PCI) planning with real-time calculation of expected post-PCI iFR results. Reprinted with premission from Elsevier from Götberg M, Cook CM, Sen S, Nijjer S, Escaned J, Davies JE. The evolving future of instantaneous wave-free ratio and fractional flow reserve. J Am Coll Cardiol. 2017;70(11):1379–402.
Conclusions
iFR is a novel adenosine-independent pressure-derived physiological index that recently emerged as a safe and effective alternative to FFR for the invasive assessment of coronary stenosis severity with the potential to increase the widespread adoption of physiology-guided coronary revascularisation into routine clinical practice. By harnessing the unique properties of resting coronary physiology and addressing the drawbacks of pharmacologically-induced maximal hyperaemia, iFR challenges the paradigm of FFR as the reference standard for invasive assessment of coronary lesions. Emerging evidence suggests that iFR may be a superior prognostic marker compared with FFR for deferring intervention for non-culprit coronary lesions in patients with ACS. Finally, fully integrated virtual PCI planning using the promising real-time iFR co-registration technology is unveiling a new era in the field of coronary physiology by shifting the paradigm of coronary revascularisation from simply physiological justification towards precise guidance of coronary intervention at both vessel and lesion levels.
Funding / Potential Competing Interests
Juan F. Iglesias reports institutional education funding and hororaria/ speaker fees from Philips Volcano. SS Nijjer reports grants for physician educational events from Philips Volcano. Justin E. Davies is a consultant and has received research funding from Philips Volcano; additionally, he is co-inventor of iFR technology that is under license to Philips volcano from Imperial College London, UK.
References
- Windecker, S.; Kolh, P.; Alfonso, F.; Collet, J.P.; Cremer, J.; Falk, V.; et al. 2014 ESC/EACTS Guidelines on myocardial revascularization: The Task Force on Myocardial Revascularization of the European Society of Cardiology (ESC) and the European Association for Cardio-Thoracic Surgery (EACTS)Developed with the special contribution of the European Association of Percutaneous Cardiovascular Interventions (EAPCI). Eur Heart J 2014, 35, 2541–2619. [Google Scholar] [PubMed]
- Götberg, M.; Cook, C.M.; Sen, S.; Nijjer, S.; Escaned, J.; Davies, J.E. The Evolving Future of Instantaneous Wave-Free Ratio and Fractional Flow Reserve. J Am Coll Cardiol 2017, 70, 1379–1402. [Google Scholar] [CrossRef]
- Pijls, N.H.; van Son, J.A.; Kirkeeide, R.L.; De Bruyne, B.; Gould, K.L. Experimental basis of determining maximum coronary, myocardial, and collateral blood flow by pressure measurements for assessing functional stenosis severity before and after percutaneous transluminal coronary angioplasty. Circulation 1993, 87, 1354–1367. [Google Scholar] [CrossRef]
- Pijls, N.H.; Van Gelder, B.; Van der Voort, P.; Peels, K.; Bracke, F.A.; Bonnier, H.J.; et al. Fractional flow reserve. A useful index to evaluate the influence of an epicardial coronary stenosis on myocardial blood flow. Circulation 1995, 92, 3183–3193. [Google Scholar] [CrossRef]
- Pijls, N.H.; De Bruyne, B.; Peels, K.; Van Der Voort, P.H.; Bonnier, H.J.; Bartunek JKoolen, J.J.; et al. Measurement of fractional flow reserve to assess the functional severity of coronary-artery stenoses. N Engl J Med 1996, 334, 1703–1708. [Google Scholar] [CrossRef]
- Bech, G.J.; De Bruyne, B.; Pijls, N.H.; de Muinck, E.D.; Hoorntje, J.C.; Escaned, J.; et al. Fractional flow reserve to determine the appropriateness of angioplasty in moderate coronary stenosis: A randomized trial. Circulation 2001, 103, 2928–2934. [Google Scholar] [CrossRef] [PubMed]
- Pijls, N.H.J.; van Schaardenburgh, P.; Manoharan, G.; et al. Percutaneous Coronary Intervention of Functionally Nonsignificant Stenosis. 5-Year Follow-Up of the DEFER Study. J Am Coll Cardiol 2007, 49, 2105–2111. [Google Scholar] [CrossRef]
- Tonino, P.A.; De Bruyne, B.; Pijls, N.H.; Siebert, U.; Ikeno, F.; van ‘t Veer, M.; Klauss, V.; Manoharan, G.; Engstrm, T.; Oldroyd, K.G.; Ver Lee, P.N.; MacCarthy, P.A.; Fearon, W.F.; FAME Study Investigators. Fractional flow reserve versus angiography for guiding percutaneous coronary intervention. N Engl J Med 2009, 360, 213–224. [Google Scholar] [CrossRef] [PubMed]
- De Bruyne, B.; Pijls, N.H.; Kalesan, B.; Barbato, E.; Tonino, P.A.; Piroth, Z.; Jagic, N.; Möbius-Winkler, S.; Rioufol, G.; Witt, N.; Kala, P.; MacCarthy, P.; Engström, T.; Oldroyd, K.G.; Mavromatis, K.; Manoharan, G.; Verlee, P.; Frobert, O.; Curzen, N.; Johnson, J.B.; Jüni, P.; Fearon, W.F.; FAME 2 Trial Investigators. Fractional flow reserve-guided PCI versus medical therapy in stable coronary disease. N Engl J Med 2012, 367, 991–1001. [Google Scholar] [CrossRef]
- De Bruyne, B.; Fearon, W.F.; Pijls, N.H.; Barbato, E.; Tonino, P.; Piroth, Z.; et al. Fractional flow reserve-guided PCI for stable coronary artery disease. N Engl J Med 2014, 371, 1208–1217. [Google Scholar] [CrossRef]
- Fearon, W.F.; Nishi, T.; De Bruyne, B.; Boothroyd, D.B.; Barbato, E.; Tonino, P.; et al. Clinical Outcomes and Cost-Effectiveness of Fractional Flow Reserve-Guided Percutaneous Coronary Intervention in Patients With Stable Coronary Artery Disease: Three-Year Follow-Up of the FAME 2 Trial (Fractional Flow Reserve Versus Angiography for Multivessel Evaluation). Circulation 2018, 137, 480–487. [Google Scholar]
- Patel, M.R.; Calhoon, J.H.; Dehmer, G.J.; Grantham, J.A.; Maddox, T.M.; Maron, D.J.; Smith, P.K. ACC/AATS/AHA/ASE/ASNC/SCAI/SCCT/STS 2017 Appropriate Use Criteria for Coronary Revascularization in Patients With Stable Ischemic Heart Disease: A Report of the American College of Cardiology Appropriate Use Criteria Task Force, American Association for Thoracic Surgery, American Heart Association, American Society of Echocardiography, American Society of Nuclear Cardiology, Society for Cardiovascular Angiography and Interventions, Society of Cardiovascular Computed Tomography, and Society of Thoracic Surgeons. J Am Coll Cardiol 2017, 69, 2212–2241. [Google Scholar]
- Dattilo, P.B.; Prasad, A.; Honeycutt, E.; Wang, T.Y.; Messenger, J.C. Contemporary patterns of fractional flow reserve and intravascular ultrasound use among patients undergoing percutaneous coronary intervention in the United States: Insights from the National Cardiovascular Data Registry. J Am Coll Cardiol 2012, 60, 2337–2339. [Google Scholar] [CrossRef]
- Rigamonti, F.; Fahrni, G.; Maeder, M.; Cook, S.; Weilenmann, D.; Wenaweser, P.; et al. Switzerland: Coronary and structural heart interventions from 2010 to 2015. EuroIntervention 2017, 13, Z75–Z79. [Google Scholar] [CrossRef] [PubMed]
- Sen, S.; Escaned, J.; Malik, I.S.; Mikhail, G.W.; Foale, R.A.; Mila, R.; et al. Development and Validation of a New Adenosine-Independent Index of Stenosis Severity From Coronary Wave–Intensity Analysis Results of the ADVISE (ADenosine Vasodilator Independent Stenosis Evaluation) Study. J Am Coll Cardiol 2012, 59, 1392–1402. [Google Scholar] [CrossRef]
- Spaan, J.A.; Piek, J.J.; Hoffman, J.I.; Siebes, M. Physiological basis of clinically used coronary hemodynamic indices. Circulation 2006, 113, 446–455. [Google Scholar] [CrossRef] [PubMed]
- van de Hoef, T.P.; Meuwissen, M.; Escaned, J.; Davies, J.E.; Siebes, M.; Spaan, J.A.; et al. Fractional flow reserve as a surrogate for inducible myocardial ischaemia. Nat Rev Cardiol 2013, 10, 439–452. [Google Scholar] [CrossRef]
- Davies, J.E.; Whinnett, Z.I.; Francis, D.P.; Manisty, C.H.; Aguado-Sierra, J.; Willson, K.; et al. Evidence of a Dominant Backward-Propagating “Suction” Wave Responsible for Diastolic Coronary Filling in Humans, Attenuated in Left Ventricular Hypertrophy. Circulation 2006, 113, 1768–1778. [Google Scholar] [CrossRef]
- Vranckx, P.; Cutlip, D.E.; McFadden, E.P.; Kern, M.J.; Mehran, R.; Muller, O.; et al. Coronary pressure-derived fractional flow reserve measurements: Recommendations for standardization, recording, and reporting as a core laboratory technique: Proposals for integration in clinical trials. Circ Cardiovasc Interv 2012, 5, 312–317. [Google Scholar] [CrossRef] [PubMed]
- Gould, K.L.; Lipscomb, K.; Calvert, C. Compensatory changes of the distal coronary vascular bed during progressive coronary constriction. Circulation 1975, 51, 1085–1094. [Google Scholar] [CrossRef] [PubMed]
- Nijjer, S.S.; Sen, S.; Petraco, R.; Davies, J.E. Advances in coronary physiology. Circ J 2015, 79, 1172–1184. [Google Scholar] [CrossRef][Green Version]
- Nijjer, S.S.; de Waard, G.A.; Sen, S.; van de Hoef, T.P.; Petraco, R.; Echavarría-Pinto, M.; et al. Coronary pressure and flow relationships in humans: Phasic analysis of normal and pathological vessels and the implications for stenosis assessment: A report from the Iberian-Dutch-English (IDEAL) collaborators. Eur Heart J 2016, 37, 2069–2080. [Google Scholar] [CrossRef]
- Petraco, R.; Escaned, J.; Sen, S.; Nijjer, S.; Asrress, K.N.; Echavarria-Pinto, M.; et al. Classification performance of instantaneous wave-free ratio (iFR) and fractional flow reserve in a clinical population of intermediate coronary stenoses: Results of the ADVISE registry. EuroIntervention 2013, 9, 91–101. [Google Scholar] [CrossRef] [PubMed]
- Jeremias, A.; Maehara, A.; Généreux, P.; Asrress, K.N.; Berry, C.; De Bruyne, B.; et al. Multicenter core laboratory comparison of the instantaneous wave-free ratio and resting Pd/Pa with fractional flow reserve: The RESOLVE study. J Am Coll Cardiol 2014, 63, 1253–1261. [Google Scholar] [CrossRef]
- Sen, S.; Asrress, K.N.; Nijjer, S.; et al. Diagnostic Classification of the Instantaneous Wave-Free Ratio Is Equivalent to Fractional Flow Reserve and Is Not Improved With Adenosine Administration. J Am Coll Cardiol 2013, 61, 1409–1420. [Google Scholar] [CrossRef] [PubMed]
- Sen, S.; Nijjer, S.; Petraco, R.; Malik, I.S.; Francis, D.P.; Davies, J. Instantaneous wave-free ratio: Numerically different, but diagnostically superior to FFR? Is lower always better? J Am Coll Cardiol 2013, 62, 566. [Google Scholar] [CrossRef]
- van de Hoef, T.P.; Meuwissen, M.; Escaned, J.; et al. Head-to-head comparison of basal stenosis resistance index, instantaneous wave-free ratio, and fractional flow reserve: Diagnostic accuracy for stenosis-specific myocardial ischaemia. EuroIntervention 2015, 11, 914–925. [Google Scholar] [CrossRef] [PubMed]
- Hwang, D.; Jeon, K.-H.; Lee, J.M.; et al. Diagnostic Performance of Resting and Hyperemic Invasive Physiological Indices to Define Myocardial Ischemia: Validation With (13)N-Ammonia Positron Emission Tomography. JACC Cardiovasc Interv 2017, 10, 751–760. [Google Scholar] [CrossRef]
- Petraco, R.; Park, J.J.; Sen, S.; Nijjer, S.S.; Malik, I.S.; Echavarría-Pinto, M.; et al. Hybrid iFR-FFR decision-making strategy: Implications for enhancing universal adoption of physiology-guided coronary revascularisation. EuroIntervention 2013, 8, 1157–1165. [Google Scholar] [CrossRef]
- Davies, J.E.; Sen, S.; Dehbi, H.-M.; Al-Lamee, R.; Petraco, R.; Nijjer, S.S.; et al. Use of the Instantaneous Wave-free Ratio or Fractional Flow Reserve in PCI. N Engl J Med 2017, 376, 1824–1834. [Google Scholar] [CrossRef]
- Götberg, M.; Christiansen, E.H.; Gudmundsdottir, I.J.; Sandhall, L.; Danielewicz, M.; Jakobsen, L.; et al. Instantaneous Wave-free Ratio versus Fractional Flow Reserve to Guide PCI. N Engl J Med 2017, 376, 1813–1823. [Google Scholar] [CrossRef] [PubMed]
- Bhatt, D.L. Assessment of Stable Coronary Lesions. N Engl J Med 2017, 376, 1879–1881. [Google Scholar] [CrossRef] [PubMed]
- Escaned, J. Safety of coronary revascularisation deferral based on iFR and FFR measurements in stable angina and acute coronary syndromes. Oral Presentation, EuroPCR, Paris, France. 2017. [Google Scholar]
- Finet, G.; Rioufol, G. A new adenosine-independent index of stenosis severity: Why would one assess a coronary stenosis differently? J Am Coll Cardiol 2012, 59, 1915. [Google Scholar] [CrossRef] [PubMed]
- Pijls, N.H.; Van ‘t Veer, M.; Oldroyd, K.G.; Berry, C.; Fearon, W.F.; Kala, P.; et al. Instantaneous wave-free ratio or fractional flow reserve without hyperemia: Novelty or nonsense? J Am Coll Cardiol 2012, 59, 1916–1917. [Google Scholar] [CrossRef]
- Rudzinski, W.; Waller, A.H.; Kaluski, E. Instantaneous wave-free ratio and fractional flow reserve: Close, but not close enough! J Am Coll Cardiol 2012, 59, 1915–1916. [Google Scholar] [CrossRef]
- Berry, C.; McClure, J.D.; Oldroyd, K.G. Meta-Analysis of Death and Myocardial Infarction in the DEFINE-FLAIR and iFR-SWEDEHEART Trials. Circulation 2017, 136, 2389–2391. [Google Scholar] [CrossRef]
- Nijjer, S.S.; Sen, S.; Petraco, R.; Mayet, J.; Francis, D.P.; Davies, J.E.R. The Instantaneous wave-Free Ratio (iFR) pullback: A novel innovation using baseline physiology to optimise coronary angioplasty in tandem lesions. Cardiovasc Revascularization Med 2015, 16, 167–171. [Google Scholar] [CrossRef]
- Nijjer, S.S.; Sen, S.; Petraco, R.; Escaned, J.; Echavarria-Pinto, M.; Broyd, C.; et al. Pre-angioplasty instantaneous wave-free ratio pullback provides virtual intervention and predicts hemodynamic outcome for serial lesions and diffuse coronary artery disease. JACC Cardiovasc Interv 2014, 7, 1386–1396. [Google Scholar] [CrossRef]
© 2018 by the author. Attribution - Non-Commercial - NoDerivatives 4.0.