Case report
A 25-year-old Caucasian woman presented to our hospital in April 2005, complaining of exertional dyspnoea, palpitations and fatigue since three weeks. She underwent a mitral and tricuspid valve replacement with two mechanical prostheses in 1999 in Serbia for rheumatic mitral and tricuspid stenosis and was reoperated in 2003 for a subacute tricuspid prosthesis obstruction with implantation of a 31 mm bi-leaflet St. Jude valve. On physical examination she was an alert young woman without clinical signs of left or right heart failure. Cardiac auscultation revealed a large splitting of S1 associated to a 3/6 holosystolic murmur and 3/6 diastolic rumble on the left parasternal and apical regions. A transthoracic echocardiography (TTE) was performed and showed a normal left ventricular systolic function with a mild post-operative septal hypokinesia, a mildly dilated left atrium and a normally functioning mitral prosthetic valve. The right atrium was dilated and assumed a round shape with bulging of the interatrial septum to the left. There was a dilatation of the inferior vena cava and the sub-hepatic veins. The right ventricle was mildly dilated with a normal right ventricular systolic function. The posterior leaflet of the tricuspid prosthetis was jammed in a close position and there was an incomplete excursion of the anterior leaflet with a significant valvular leak. The mean transprosthetic gradient varied between 7 and 9 mm Hg (Figure 1, Figure 2 and Figure 3).
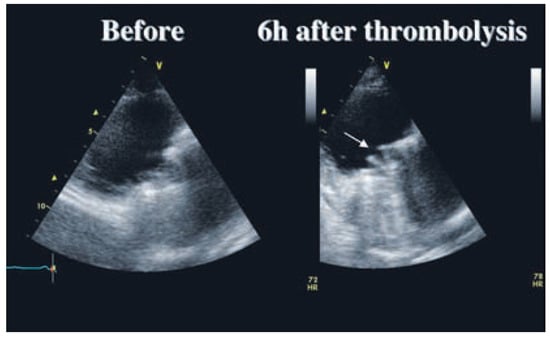
Figure 1.
End-diastolic parasternal long axis view of the right ventricle centered on the prosthetic tricuspid valve. Before thrombolysis, there is no visible leaflets movement. After thrombolysis, the two leaflets are opening symmetrically (arrow).
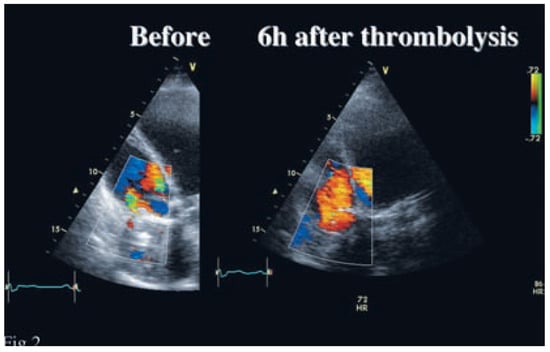
Figure 2.
End-diastolic apical four chamber view of the right ventricle centered on the prosthetic tricuspid valve. Before thrombolysis, two small high velocity jets are visible on the lateral aspects of the valve. After thrombolysis, a normal pattern of low velocity jet through the entire valve is demonstrated.
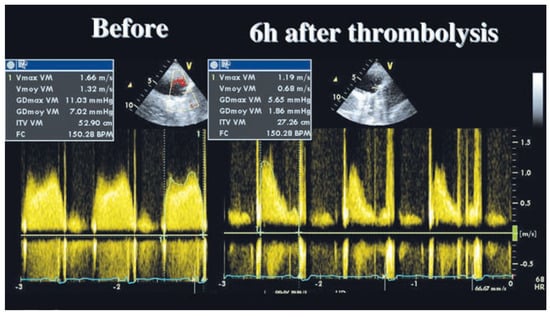
Figure 3.
Continuous Doppler recordings of the tricuspid prosthesis in parasternal long axis view of the right ventricle. The mean gradient went down from 7 mm Hg before to 1.9 mm Hg after thrombolysis.
A diagnosis of a subacute thrombosis of the tricuspid St. Jude valve was made and an intravenous thrombolysis was started. We administered a recombinant tissue plasminogen activator (rt-PA; Actilyse®, Boehringer Ingelheim, Germany) with a loading dose of 10 mg IV, followed by 90 mg IV for 90 min. Heparin 5000 U bolus IV was administered 2 hours after the loading dose, followed with 30 000 U/ 24 h IV. One hour after the end of the thrombolysis, the diastolic rumble had disappeared. A transthoracic examination, 6 hours after the beginning of the fibrinolysis, showed a complete excursion of the two leaflets with a mean transprosthetic gradient of 2 mm Hg (Figure 1, Figure 2 and Figure 3).
The patient left the hospital with the treatment of phenprocoumone targeted to an INR between 3.0 and 3.5 and acetylsalicylic acid 100 mg/d. In November 2007, a routine TTE examination showed once again a partial thrombosis of the tricuspid prosthesis with a mean gradient of 9 mm Hg. Anticoagulation had been shortly interrupted for the ablation of a nasal polyp. A new thrombolysis following the same protocol was undertaken during a single day overnight hospitalisation with comparable success.
Discussion
The incidence of prosthetic valve thrombosis (PVT) may be as high as 13% in the first year or 20% overall in patients with tricuspid valve prostheses, mostly because of an inadequate anticoagulation []. Cases of thrombolysis of right-sided PVT are uncommon in the medical literature [,,].The largest cohort comes from Tong et al. [] who report 15 cases of tricuspid valve thrombosis in a group of 107 patients with PVT. A complete haemodynamic success (ie return of the transvalvular gradient to normal range) after thrombolysis was reported in 14/15 patients and a partial haemodynamic success (ie partial improvement in gradient without complete normalisation) in 1/15. The clinical success, defined as haemodynamic success without clinical complication, was 100%, which was statistically higher than the success rate of left-sided valves thrombolysis. No apparent clinical complications, including minor or major bleedings, were described in the tricuspid valve group, but computed tomography scans or ventilated/perfused lung scintigraphies were not performed to document subclinical pulmonary embolism.
Conclusions
In view of its excellent results and few complications, thrombolysis of right-sided PVT is the treatment of choice for the great majority of patients. Surgical valvular replacement has to be considered only after failure of several successive thrombolysis. Anticoagulation according to the standard recommendations and addition of acetylsalicylic acid are essential to prevent recurrent thrombosis after a successful thrombolysis.
References
- Cannegieter, S.C.; Rosendaqal, F.R. Thrombolembolic and bleeding complications in patients with mechanical heart valve prostheses. Circulation. 1994, 89, 635–641. [Google Scholar] [CrossRef] [PubMed]
- Özkan, M.; Kaymaz, C.; Kirma, C.; et al. Intravenous thrombolytic treatment of mechanical prosthetic valve thrombosis: a study using serial transesophageal echocardiography. J Am Coll Cardiol. 2000, 35, 1881–1889. [Google Scholar] [CrossRef] [PubMed]
- Roudaut, R.; Lafitte, S.; Roudaut, M.F.; et al. Fibrinolysis of mechanical prosthetic valve thrombosis. J Am Coll Cardiol. 2003, 41, 653–658. [Google Scholar] [CrossRef] [PubMed]
- Gupta, D.; Kothara, S.S.; Bahl, V.K.; et al. Thrombolytic therapy for prosthetic valve thrombosis; shortand long-term results. Am Heart J. 2000, 140, 906–916. [Google Scholar] [CrossRef] [PubMed]
- Tong, A.; Roudaut, R.; Özkan, M.; et al. Transesophageal echocardiography improves risk assessment of thrombolysis of prosthetic valve thrombosis: results of the international PROTEE registry. J Am Coll Cardiol. 2004, 43, 77–84. [Google Scholar] [CrossRef] [PubMed]
© 2008 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).