Abstract
Background: The global increase in the population older than 80 years has led to a paradigm shift centered in the hospital environment, with the inclusion of domiciliary oral health actions improving quality of life. This review evaluates the effects of domiciliary dental care and oral health promotion in nursing homes of older adults. Methods: Seven databases were searched without date restrictions from 15 September to 21 November 2024. A manual search was also performed in the reference lists of the included articles. This research included studies evaluating older adults aged ≥80 years, regardless of sex, who received domiciliary dental care associated or not with oral health promotion, evaluating periodontal condition, dental caries, and the dental and denture plaque index. Regarding data collection and analysis, a risk of bias assessment was performed using RoB 2.0 and RoB 1.0, according to the study design. The level of evidence was assessed using the GRADE tool. Results: Of the 2415 studies found, 5 met the eligibility criteria. After quality assessment, one randomized clinical trial presented a moderate risk of bias, and one presented a low risk. Also, two non-randomized studies presented a high risk and one a low risk. The certainty of evidence was classified as low for all outcomes assessed. One study demonstrated a reduction in the caries level of participants. Regarding periodontal and gingival conditions, although the occurrence of deep pockets (greater than 3.5 mm) decreased over time, there was no significant difference between the control and intervention groups. The level of dental and denture plaque showed a slight reduction. Conclusion: There is limited evidence that domiciliary dental care in nursing homes for older adults can lead to a reduction in caries levels and that oral health programs can reduce dental and denture plaque in evaluations conducted over periods of up to two years. Although the results show a limited magnitude, this does not diminish the importance of promoting domiciliary oral health care.
1. Introduction
The current trend of population aging has brought the need for a paradigm shift related to health and social systems. Amid a major demographic transition, the World Health Organization [1] estimates that by 2030, one in six people worldwide will be 60 years or older, with this population increasing from 1 billion in 2020 to 1.4 billion in 2030 and 2.1 billion by 2050. This projection highlights the need for expanded primary and long-term health care services to ensure longevity and a healthy life [2]. In this context, oral health enables essential functions such as eating and speaking, which are linked to self-confidence, well-being, social interaction, and participation in daily activities [2,3]. However, older adults often face compromised oral health [4] due to issues such as edentulism, difficulties with dental prostheses, periodontal diseases, residual roots, and carious lesions [5,6]. This scenario underscores the vulnerability of older adults in accessing dental care, exacerbated by reduced cognitive function, lack of autonomy, depression, and the absence of caregiver guidance on proper oral hygiene [6,7].
In this context, oral health promotion in nursing homes emerges as a viable option. It is a health care service that plays preventive and educational roles in the oral health of older adults [8]. When associated with domiciliary dental care, treatments performed by dentists, this approach ensures equal access to oral care, providing personalized and specialized treatment [9] and promoting better quality of life for functional and healthy older adults [6,10]. Studies suggest that older adults living in nursing homes often have poor oral-health-related quality of life [10,11] and that one in four seniors prefers domiciliary dental consultations due to access barriers such as functional impairments and cognitive decline [9]. This highlights the significant need for domiciliary dental care, which is often overlooked when assessing the demand for general home health care services [9,12]. Neglecting oral health issues disregards their impact not only on overall health but also on the quality of life and daily well-being of this population [13].
Oral conditions such as the need for dentures, tooth loss, and the use of ill-fitting prostheses—with consequent impairments in masticatory function, aesthetics, and speech—affect not only physical health but also psychological and social well-being, directly impacting the quality of life of older individuals [13]. In response to this issue, domiciliary dental care in nursing homes provides older adults with greater comfort and attention by offering preventive, curative, and educational measures. Additionally, it promotes coordination between health care professionals and family members, allowing for the implementation of a treatment plan tailored to older adults’ needs, ultimately aiming to improve their quality of life [8]. However, there are still few studies addressing the emerging need for implementing domiciliary oral health programs in nursing homes within the context of comprehensive older adult care, considering their oral and general health conditions as well as their quality of life. Therefore, this study aims to assess the effectiveness of domiciliary dental care and oral health promotion in nursing homes. The objective is to demonstrate to caregivers, nurses, dentists, patients, and family members the need to implement this service by qualified professionals trained to work in this field.
2. Materials and Methods
2.1. Protocol and Registration
This review was conducted in accordance with Cochrane guidelines, and the report was described following the PRISMA framework. This study was registered in the International Prospective Register of Systematic Reviews (PROSPERO) under the ID number CRD42024586468 and performed according to PRISMA guidelines (Preferred Reporting Items for Systematic Reviews and Meta-Analyses Protocol) [14] (Supplementary Table S1).
2.2. Research Question
The following PICOS question was investigated: “In older adults aged 80 and over, receiving domiciliary dental care associated or not to oral health programs in nursing homes, what are the effects on oral health, considering the level of caries, plaque and periodontal disease?”
2.3. Eligibility Criteria
The selection followed the criteria of the PICOS acronym, being the following: population (P), older adults aged 80 and over, regardless of sex, living in nursing homes; intervention (I), oral health preventive measures provided by nurses and caregivers, whether associated with dental care provided by dentists or not; comparison (C), individuals who did not receive oral health programs or individuals evaluated before the intervention; outcome (O), level of caries, periodontal condition, and amount of bacterial plaque on teeth and dentures; and study type (S), randomized or controlled clinical trials. The search excluded studies conducted on populations under 80 years of age who did not receive oral health prevention at nursing homes by caregivers or dentists or who did not present data regarding the assessment of the level of caries, dental and denture plaque, or periodontal disease.
2.4. Information Sources
The research was conducted on the databases Embase, Latin American Literature in Health Sciences (LILACS), PubMed/MEDLINE, Scopus, and Web of Science. Gray literature was included, searched in Google Scholar and ProQuest, with manual searches of references from the included studies and consultation with experts. There were no restrictions regarding the publication date or language of studies. Comprehensive searches were made from 15 to 21 September 2024.
2.5. Search Strategy and Selection Process
The search strategy was created using MeSH terms, keywords, and Boolean operators (“OR” and “AND”) to cover the PICOS acronym (Supplementary Table S1). References were exported to the RAYYAN reference manager [15], where duplicate files were removed. Two independent reviewers (C.S. and K.T.) selected the included articles in two phases. First (Phase 1), both reviewers assessed the titles and abstracts according to the eligibility criteria; second (Phase 2), they examined the full texts of the articles included in Phase 1, selecting the articles using the same criteria as in Phase 1 and then verifying all information found. In cases of discrepancies, a third reviewer (B.L.) was involved before making the final decision in both phases. If important data for the review were missing or unclear, an attempt to contact the corresponding author of the study was made to resolve or clarify the issue.
2.6. Data Collection Process
Two independent reviewers (C.S. and K.T.) collected the data from the selected articles. Once selected, they verified the recovered information with the third reviewer (B.L.). The collected information included author, study type, year of publication, country, patient characteristics (sample size, sex, and age), clinical characteristics (central tendency measures referring to oral health indices, including caries prevalence, plaque, and periodontal disease), nursing home characteristics, and key conclusions. Any discrepancies were discussed among the three reviewers.
2.7. Study Risk of Bias Assessment
Both Risk of Bias 2 (RoB 2) [16] and 1 (RoB 1.0) [17] are methods utilized to assess the risk of bias in randomized clinical trials, with the goal of ensuring the reliability and quality of evidence in systematic reviews. RoB 1 evaluates seven key domains of bias, categorizing each as low, unclear, or high risk based on the available information and the methodology employed in the assessed study. In contrast, RoB 2 offers a more structured and standardized approach, focusing on five key domains that are classified as low risk, some risk, or high risk of bias. This structure facilitates a more objective evaluation. The assessment was conducted by two reviewers, and any discrepancies were resolved by the third reviewer.
2.8. Certainty Assessment
Two intervention comparisons (amount of plaque on the teeth and plaque on the dentures) were assessed in this review according to the GRADE tool (Grading of Recommendations Assessment, Development and Evaluation approach) [18]. The narrative GRADE was classified as not serious, serious, or very serious issues in each one of the five domains evaluated: study design, risk of bias, inconsistency, indirectness, and imprecision. The final classification was rated as high, moderate, low, or very low.
3. Results
3.1. Identification and Selection of Studies
The search in electronic and manual databases retrieved 2858 studies distributed among the following sources: PubMed (402), Web of Science (293), Scopus (422), Cochrane Library (1.702), Embase (35), Livivo (0), Lilacs (0), and gray literature (4). These records were organized in a flowchart illustrated in Figure 1. After removing 439 duplicate records, 2419 studies remained for screening. In the initial analysis, based on titles and abstracts, 2409 articles were excluded because they did not meet the pre-established inclusion criteria. Thus, after this screening, 10 potentially relevant articles were selected for full reading. However, three of them were excluded because they did not answer the review question [10,19,20] and two were cross-sectional studies [21,22]. At completion of the process, five studies were included in the final analysis [23,24,25,26,27]. Additionally, a manual search was performed in the reference lists of the selected articles, but no additional studies were identified.
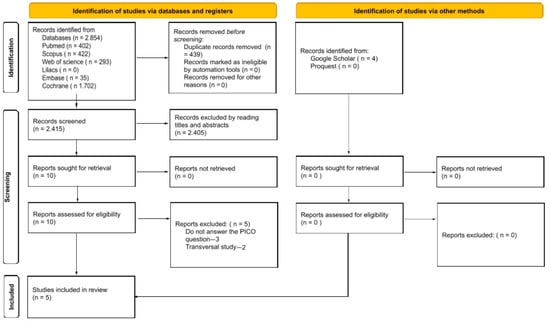
Figure 1.
Flow diagram of study identification.
3.2. Assessment of the Methodological Quality of Included Studies
Analysis of the methodological quality of the included studies revealed that the risk of bias was classified as “low” in two studies [23,24], “moderate” in one study [25] and “high” in two studies [26,27], as illustrated in Figure 2 and Figure 3. Concerning random sequence generation, all five studies had a low risk of bias. In two studies the interventions were not described clearly enough [25,27], and another two studies were compromised by missing data [25,26]. One study presented losses throughout the evaluation due to the death of some participants and deviation from intended intervention due to changes in care dependency during the study period [26] The clarity of outcome measurement was considered insufficient in two studies [26,27]. Regarding the inclusion and exclusion criteria, all studies demonstrated a low risk of bias, indicating a robust process of participant selection.
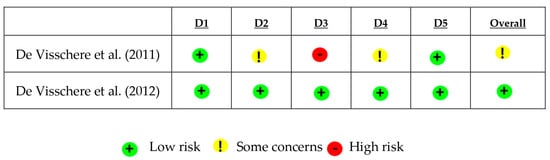
Figure 2.
Risk of bias domains among randomized trials, divided into risks of bias: arising from the randomization process (D1); due to deviations from intended interventions (D2); due to missing outcome data; in outcome measurement (D4); and in selection of the reported result (D5) (ROB-2) [23,25].
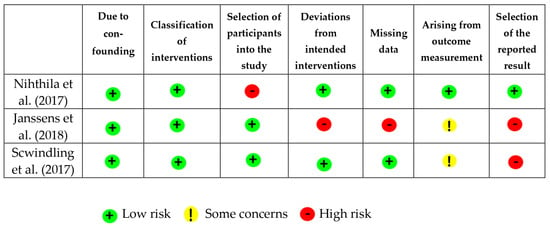
Figure 3.
Graph of risk of bias in the reviewer’s judgement about each risk of bias domain across included studies (ROB-I) [24,26,27].
3.3. Data Extraction and Characteristics of Selected Studies
Data extraction from the selected studies is described in Table 1. Two studies were classified as randomized clinical trials, two as controlled clinical trials, and one as an observational cohort trial, involving samples of 269 to 1987 patients of both sexes. Four of the selected studies analyzed the level of dental plaque and the presence of plaque on dentures [23,24,25,27]. Regarding the presence of caries, one study performed this evaluation [24]. The follow-up period varied, with annual assessments performed in some studies [21,22], while others described biannual follow-ups, including regular visits [23] and reassessments after the initial consultation [24]. Participants were assessed based on protocols that included oral health instructions, oral hygiene practices, and personalized interventions [23,24,25,26,27,28]. The articles employed different statistical methods, such as mixed model analysis [23,25,27], t-test and chi-square [25,27], a generalized linear model [24,25], a generalized mixed model [27], and the Wilcoxon test [25,26]. Only one study used ANOVA [27], the McNemar test [26], and a generalized linear model [23]. In addition, two studies used logistic regression [24,26]. In total, four studies demonstrated statistically significant results related to the interventions performed, with emphasis on the reduction of dental plaque and the presence of plaque on dental prostheses [24,25,26,27].

Table 1.
Characteristics of included studies.
3.4. Synthesis of Results
A meta-analysis was not feasible in this systematic review due to clinical, methodological, and statistical heterogeneities. The included studies used different protocols of intervention, follow-up periods, measurement methods, and could not be compared by a meta-analysis.
3.5. Level of Evidence
According to GRADE, the evaluation of the certainty of evidence is described in Table 2. The certainty of evidence was classified as low. This was mainly due to limitations such as intervention heterogeneity, different assessed methods, and the risk of bias results. Therefore, confidence in the estimate of effects is limited.

Table 2.
Quality assessment of included studies.
4. Discussion
Concerning the oral health condition of older adults, an analysis of comorbidities, cognitive impairments, and their consequent impact on quality of life highlights the importance of having trained professionals in the nursing home environment attentive to the individual’s needs [28]. Therefore, it is reasonable to assume that the implementation of domiciliary dental care and oral health programs in nursing homes for older adults would improve oral health indicators. However, the studies evaluated in this systematic review show only low evidence of slight improvements in the oral health of older adults who received domiciliary oral health programs in nursing homes or minimal dental intervention by dentists [23,24,25,26,27].
One study with considerable risk of bias assessed the reduction from 70.5% to 36.5% regarding the caries levels in older adults, who received oral health preventive measures at nursing homes [26]. The domiciliary dental care performed by dentists through restorative procedures plays a fundamental role in reducing the level of caries. The presence of a dentist in the nursing home to provide curative care is essential to ensure greater access to dental care and promote better oral health indices. Regarding the periodontal condition, which involves more extensive interventions such as scaling or even surgeries, it was predictable that merely providing oral health education programs at nursing homes would not be sufficient to promote significant improvements. Although one study with considerable risk of bias [27] showed a reduction in periodontal pockets of approximately 3 mm in depth, this finding does not reflect significant differences between the intervention and control groups after 12 and 24 months, respectively (p = 0.62–0.69; 95% CI = −15.6 to 11.8).
Even though there was a slight improvement in oral health, it is essential to also consider the emotional health and well-being of older adults, which typically show low levels of quality of life at the onset of domiciliary dental care [10,11] and which are improved after interventions [29]. In this regard, since the need for treatment and the costs increase with age [19], as well as the degree of dependence [30], oral health preventive measures should be offered at least semiannually and involve all key participants, including caregivers, nurses, family members, and the older adults themselves.
In relation to dental plaque levels, three studies [23,24,25] showed an average reduction in dental plaque indices ranging from 1.4 (32.4) [27] to 1.7 (8.05) [24], a small magnitude associated with a large variability observed in the standard deviation, which makes its clinical significance less representative. The loss of manual dexterity and functional capacity along with the presence of cognitive difficulties and other psychomotor limitations [31] has a significant impact on the ability to perform oral hygiene actions [32], increasing the need for home assistance from a qualified professional [24]. Conversely, professionals without dental training [23,24,25], those who do not practice oral health care themselves, or even those who received oral health information infrequently [27] may not adequately assist the older adults in maintaining oral health. It is undeniable that there are various difficulties faced by nurses and caregivers, including patient resistance to adopting new hygiene habits and varying degrees of dementia, depression, anxiety, and other cognitive and functional limitations [23]. It is also important to consider the work routine of the caregiver, the number of working hours, the number of patients assisted, and pressures faced by family members and managers, among other factors.
Concerning the level of denture plaque, two short-term studies [23,27] demonstrated an improvement in the indices, yet without significant differences between the control and experimental groups. This result is like the evaluation of plaque levels on natural teeth, although there is greater ease in cleaning dentures compared to natural teeth [24]. The use of auxiliary instruments, such as ultrasonic devices for denture cleaning or electric toothbrushes, could help control oral hygiene in older adults; however, these resources require financial investment. Thus, socioeconomic factors can impact oral health conditions, particularly in older adults with fewer financial resources or those residing in institutions that routinely receive little governmental financial support for oral health measures despite the legal obligation to allocate such investment [33].
A deeper understanding of the results of this systematic review should consider not only aspects related to patient limitations but also those of dental professionals. There is a need for specific training to qualify domiciliary dental care for patients with special needs, such as older adults. However, there are few professional courses available, and the demand for this dental specialty remains low despite its growing need. It is essential to encourage dental students, starting from their undergraduate studies, to learn about and engage with this increasingly present reality.
It is also important to consider the need for adequate remuneration for professionals, corresponding to the complexity of care provided, as significant financial investments are required for mobile dental treatment units, consumable materials, and the professional transportation to perform the service [34]. For populations in economically underprivileged regions, this service should be offered by public health systems and promoted by governmental health organizations. Finally, the presence of specialized dental professionals in nursing homes—not only for preventive measures but also for curative actions—working in collaboration with other multidisciplinary professionals at the facility, with a reasonable frequency, can lead to better oral health outcomes for the older adults, improving their quality of life [27].
Limitations
The greatest difficulties of this systematic review are associated with the lack of studies related to the oral health of older adults receiving domiciliary dental care associated or not with oral health programs in nursing homes. In addition, the literature currently available is quite heterogeneous and has problems related to methodological quality. Thus, the evidence generated by this review is limited. The absence of the control group was a limitation presented by one study in this review [26]. The samples evaluated had varying degrees of dependence, which led to inconsistency and imprecision in the results. Randomization had limitations in some studies and was not sufficient to eliminate confounding factors [23,25]. Thus, the level of evidence generated by the GRADE tool for the evaluations of the plaque levels on both teeth and dentures was considered low due to the considerable risk of bias in the included studies [23,24,25,27]; the inconsistency and imprecision [23,24,25,27] of the results; the different effect estimates used, measured by professionals with different technical backgrounds [23,25,27]; uncontrolled confounding factors, such as systemic medications [27]; and the impact of random error presented in the statistical analysis of studies. However, it is important to highlight that, despite the methodological limitations, the studies indicate an improvement, albeit modest, in the oral health condition of older adults receiving nursing home care, a finding that can be reinforced by new randomized, multicenter clinical studies, where domiciliary dental interventions and evaluations are conducted by dentists at least semiannually, and which control for confounding factors such as the level of dependence, systemic comorbidities, and cognitive difficulties. Among the strengths of our review, we emphasize the transparency of the project, which was conducted in accordance with its registration on the Prospero platform, as well as the methodological rigor applied in its execution and reporting, adhering to the PRISMA guidelines. Additionally, the absence of restrictions in the search for primary studies helps to minimize potential publication bias.
5. Conclusions
There is limited evidence that domiciliary dental care in nursing homes for older adults can lead to a reduction in caries levels. Also, oral health programs can reduce dental and denture plaque, with no significant effect on periodontal health, in evaluations conducted over periods of up to two years. Although the results show a limited magnitude, this does not diminish the importance of promoting domiciliary oral health care. Additionally, it is essential to expand the domiciliary dental care, especially for older adults, whose demand has been increasing over the years.
Supplementary Materials
The following supporting information can be downloaded at https://www.mdpi.com/article/10.3390/ijerph22050683/s1, Table S1: Database search strategy.
Author Contributions
C.C.O.d.S.: data curation; formal analysis, investigation; validation; methodology; formal analysis; writing—original draft; I.M.L.M.: investigation; formal analysis; methodology; writing—review and editing; K.T.: data curation; investigation; methodology; writing—review and editing; K.R.S.: data curation; investigation; writing—review and editing; L.S.A.: formal analysis; investigation; methodology; writing—review and editing; F.S.C.: investigation; validation; methodology; writing—review and editing; B.L.S.P.: conceptualization; formal analysis; project administration; supervision; writing—review and editing. All authors have read and agreed to the published version of the manuscript.
Funding
This study was financed in part by the Coordination for the Improvement of Higher Education Personnel—Brazil (Coordenação de Aperfeiçoamento de Pessoal de Nível Superior—CAPES)—Financing Code 001 and by and by Fundação de Amparo à Pesquisa do Estado do Rio de Janeiro—FAPERJ: 260003/000577/2023.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
No new data were created or analyzed in this study. Data sharing is not applicable to this article.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- World Health Organization. Ageing; WHO: Geneva, Switzerland, 2024; Available online: https://www.who.int/health-topics/ageing#tab=tab_1 (accessed on 8 November 2024).
- World Health Organization. Oral Health; WHO: Geneva, Switzerland, 2024; Available online: https://www.who.int/health-topics/oral-health/#tab=tab_1 (accessed on 8 November 2024).
- Badewy, R.; Singh, H.; Quiñonez, C.; Singhal, S. Impact of poor oral health on community-dwelling seniors: A scoping review. Health Serv. Insights 2021, 14, 1–19. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Czwikla, J.; Herzberg, A.; Kapp, S.; Kloep, S.; Schmidt, A.; Rothgang, H.; Schwendicke, F.; Hoffmann, F. Home care recipients have poorer oral health than nursing home residents: Results from two German studies. J. Dent. 2021, 107, 103607. [Google Scholar] [CrossRef] [PubMed]
- Barbosa, K.G.N. Condições de saúde bucal em idosos: Uma revisão da realidade brasileira. Odontol. Clín.-Cient. 2011, 10, 221–225. [Google Scholar]
- Oliveira, T.F.S.; Embaló, B.; Pereira, M.C.; Borges, S.C.; Mello, A.L.S.F. Saúde bucal de pessoas idosas domiciliadas acompanhadas na atenção primária: Estudo transversal. Rev. Bras. Geriatr. Gerontol. 2021, 24, e220038. [Google Scholar] [CrossRef]
- Koyama, S.; Aida, J.; Kondo, K.; Yamamoto, T.; Saito, M.; Ohtsuka, R.; Nakade, M.; Osaka, K. Does poor dental health predict becoming homebound among older Japanese? BMC Oral Health 2016, 16, 51. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Miranda, A.F.; Rodrigues, J.S.; Franco, E.J. A necessidade da odontologia domiciliar e cuidados bucais em idosos dependentes. Rev. Ciênc. Odontol. 2018, 2, 33–38. [Google Scholar]
- Komulainen, K.; Ylöstalo, P.; Syrjälä, A.M.; Ruoppi, P.; Knuuttila, M.; Sulkava, R.; Hartikainen, S. Preference for dentist’s home visits among older people. Community Dent. Oral Epidemiol. 2012, 40, 89–95. [Google Scholar] [CrossRef]
- Salmi, R.; Närhi, T.; Suominen, A.; Suominen, A.L.; Lahti, S. Oral health-related quality of life among home-dwelling older people with and without domiciliary care. Gerodontology 2023, 40, 340–347. [Google Scholar] [CrossRef] [PubMed]
- Henni, S.H.; Skudutyte-Rysstad, R.; Ansteinsson, V.; Helleso, R.; Hovden, E.A.S. Oral health and oral health-related quality of life among older adults receiving home health care services: A scoping review. Gerodontology 2023, 40, 161–171. [Google Scholar] [CrossRef] [PubMed]
- Salmi, R.; Lahti, S.; Tolvanen, M.; Suhonen, R.; Närhi, T. Oral health assessment in domiciliary care service planning of older people. Spec. Care Dent. 2019, 39, 485–490. [Google Scholar] [CrossRef] [PubMed]
- Bronzato, P.C. O Impacto da Saúde Bucal na Qualidade de Vida dos Idosos. Bachelor’s thesis, Faculdade de Odontologia de Araçatuba, Universidade Estadual Paulista Júlio de Mesquita Filho, Araçatuba, Brazil, 2014. [Google Scholar]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Ouzzani, M.; Hammady, H.; Fedorowicz, Z.; Elmagarmid, A. Rayyan—A Web and Mobile App for Systematic Reviews. Syst. Rev. 2016, 5, 210 . [Google Scholar] [CrossRef] [PubMed]
- Sterne, J.A.C.; Savović, J.; Page, M.J.; Elbers, R.G.; Blencowe, N.S.; Boutron, I.; Cates, C.J.; Cheng, H.Y.; Corbett, M.S.; Eldridge, S.M.; et al. RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ 2019, 366, l4898. [Google Scholar] [CrossRef] [PubMed]
- Higgins, J.P.T.; Green, S. Cochrane Handbook for Systematic Reviews of Interventions; Version 5.1.0 [Updated March 2011]; The Cochrane Collaboration: London, UK, 2011; Available online: www.handbook.cochrane.org (accessed on 5 January 2022).
- Atkins, D.; Best, D.; Briss, P.A.; Eccles, M.; Falck-Ytter, Y.; Flottorp, S.; Guyatt, G.H.; Harbour, R.T.; Haugh, M.C.; Henry, D.; et al. GRADE Working Group. Grading quality of evidence and strength of recommendations. BMJ 2004, 328, 1490–1494. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Tuuliainen, E.; Nihtilä, A.; Komulainen, K.; Nykänen, I.; Hartikainen, S.; Tiihonen, M.; Suominen, A.L. Use of oral health care services among older home care clients in the context of an intervention study. Scand. J. Caring Sci. 2024, 38, 426–437. [Google Scholar] [CrossRef] [PubMed]
- Komulainen, K.; Ylöstalo, P.; Syrjälä, A.M.; Ruoppi, P.; Knuuttila, M.; Sulkava, R.; Hartikainen, S. Oral health intervention among community-dwelling older people: A randomized 2-year intervention study. Gerodontology 2015, 32, 62–72. [Google Scholar] [CrossRef]
- Fukuyama, Y.; Komiyama, T.; Ohi, T.; Hattori, Y. Association between oral health and nutritional status among older patients requiring long-term care who received home-visit dental care. J. Oral Sci. 2024, 66, 130–133. [Google Scholar] [CrossRef]
- Strömberg, E.; Hagman-Gustafsson, M.L.; Holmén, A.; Wårdh, I.; Gabre, P. Oral status, oral hygiene habits and caries risk factors in home-dwelling elderly dependent on moderate or substantial supportive care for daily living. Community Dent. Oral Epidemiol. 2012, 40, 221–229. [Google Scholar] [CrossRef]
- De Visschere, L.; Schols, J.; van der Putten, G.J.; de Baat, C.; Vanobbergen, J. Effect evaluation of a supervised versus non-supervised implementation of an oral health care guideline in nursing homes: A cluster randomised controlled clinical trial. Gerodontology 2012, 29, e96–e106. [Google Scholar] [CrossRef] [PubMed]
- Nihtilä, A.; Tuuliainen, E.; Komulainen, K.; Autonen-Honkonen, K.; Nykänen, I.; Hartikainen, S.; Ahonen, R.; Tiihonen, M.; Suominen, A.L. Preventive oral health intervention among old home care clients. Age Ageing 2017, 46, 846–851. [Google Scholar] [CrossRef] [PubMed]
- De Visschere, L.; de Baat, C.; Schols, J.M.; Deschepper, E.; Vanobbergen, J. Evaluation of the implementation of an ’oral hygiene protocol’ in nursing homes: A 5-year longitudinal study. Community Dent. Oral Epidemiol. 2011, 39, 416–425. [Google Scholar] [CrossRef] [PubMed]
- Janssens, B.; Vanobbergen, J.; Petrovic, M.; Jacquet, W.; Schols, J.M.; De Visschere, L. The impact of a preventive and curative oral healthcare program on the prevalence and incidence of oral health problems in nursing home residents. PLoS ONE 2018, 13, e0198910. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Schwindling, F.S.; Krisam, J.; Hassel, A.J.; Rammelsberg, P.; Zenthöfer, A. Long-term success of oral health intervention among care-dependent institutionalized seniors: Findings from a controlled clinical trial. Community Dent. Oral Epidemiol. 2017, 46, 109–117. [Google Scholar] [CrossRef] [PubMed]
- Riggs, S.; Blue, C.; Golden, J. The oral health quality of life for seniors in residential facilities who have direct access to care as compared to those without access. Geriatr. Nurs. 2020, 41, 406–410. [Google Scholar] [CrossRef] [PubMed]
- Pearson, N.K.; Gibson, B.J.; Davis, D.M.; Gelbier, S.; Robinson, P.G. The effect of a domiciliary denture service on oral health related quality of life: A randomised controlled trial. Br. Dent. J. 2007, 203, E3–E101. [Google Scholar] [CrossRef]
- Zenthöfer, A.; Rammelsberg, P.; Cabrera, T.; Hassel, A.J. Increasing dependency of older people in nursing homes is associated with need for dental treatments. Neuropsychiatr. Dis. Treat. 2014, 10, 2285–2290. [Google Scholar] [CrossRef]
- Tuuliainen, E.; Autonen-Honkonen, K.; Nihtilä, A.; Komulainen, K.; Nykänen, I.; Hartikainen, S.; Ahonen, R.; Tiihonen, M.; Suominen, A.L. Oral Health and Hygiene and Association of Functional Ability: A Cross-Sectional Study Among Old Home Care Clients. Oral Health Prev. Dent. 2020, 18, 253–262. [Google Scholar] [CrossRef]
- Tuuliainen, E.; Nihtilä, A.; Komulainen, K.; Nykänen, I.; Hartikainen, S.; Tiihonen, M.; Suominen, A.L. The association of frailty with oral cleaning habits and oral hygiene among elderly home care clients. Scand. J. Caring Sci. 2020, 34, 938–947. [Google Scholar] [CrossRef]
- Genaro, L.E.; Aurelio, T.G.; Pereira Areias, C.M.F.G.; Valsecki Júnior, A.; Saliba, T.A.; Lopez Rosell, F. The Role of the Dentist in Home Care for the Older People: A Narrative Review of the Literature. J. Dent. 2024, 12, 27–32. [Google Scholar] [CrossRef]
- Göstemeyer, G.; Baker, S.R.; Schwendicke, F. Barriers and facilitators for provision of oral health care in dependent older people: A systematic review. Clin. Oral Investig. 2019, 23, 979–993. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).