Abstract
Teledentistry offers possibilities for improving efficiency and quality of care and supporting cost-effective healthcare systems. This umbrella review aims to synthesize existing systematic reviews on teledentistry and provide a summary of evidence of its clinical- and cost-effectiveness. A comprehensive search strategy involving various teledentistry-related terms, across seven databases, was conducted. Articles published until 24 April 2023 were considered. Two researchers independently reviewed titles, abstracts and full-text articles. The quality of the included reviews was critically appraised with the AMSTAR-2 checklist. Out of 749 studies identified, 10 were included in this umbrella review. Two reviews focusing on oral-health outcomes revealed that, despite positive findings, there is not yet enough evidence for the long-term clinical effectiveness of teledentistry. Ten reviews reported on economic evaluations or costs, indicating that teledentistry is cost-saving. However, these conclusions were based on assumptions due to insufficient evidence on cost-effectiveness. The main limitation of our umbrella review was the critically low quality of the included reviews according to AMSTAR-2 criteria, with many of these reviews basing their conclusions on low-quality studies. This highlights the need for high-quality experimental studies (e.g., RCTs, factorial designs, stepped-wedge designs, SMARTs and MRTs) to assess teledentistry’s clinical- and cost-effectiveness.
1. Introduction
1.1. The Need for Cost-Effective Care
Due to an expanding and aging population, the global healthcare sector faces major public health challenges, such as an increase in non-communicable diseases (NCDs), a higher demand for care, healthcare workforce shortages, a lack of access to care and long waiting lists [1,2]. These challenges require a transformation of the healthcare system, as healthcare costs continue to rise, and the current healthcare system seems unsustainable in the long term [2,3]. There is a need for cost-effective innovations that increase efficiency, reduce pressure on healthcare systems and maintain the quality of care. Digital technologies offer possibilities for improving the efficiency and quality of care and supporting healthcare systems to provide cost-effective care [4,5,6].
1.2. Telehealth
The onset of the COVID-19 pandemic has increased the use of digital technologies, as the world transitioned to telehealth services to provide healthcare to patients remotely, while staying safe [4]. Telemedicine is a branch of telehealth, referring to the provision of healthcare services through the use of information and communication technologies in situations where a health provider and a patient (or another health provider) are not in the same location [7]. Examples of telemedicine are continuous home monitoring, involving the transfer of patient health data, and teleconsultations for remote practitioner–patient consultations.
In a recent systematic umbrella review on telemedicine, Eze and co-authors found that telemedicine interventions were at least as effective as face-to-face care [8]. Nevertheless, the authors concluded that caution is warranted, since in certain disease and specialty areas, telemedicine may be a less effective way to deliver care [8].
1.3. Definition of Teledentistry and Related Terms
Teledentistry is a subfield of telehealth, along with telemedicine, that is specifically dedicated to oral healthcare. The term teledentistry is often incorrectly used interchangeably for the umbrella term telehealth, which encompasses both remote healthcare delivery and the delivery of distance learning and training of healthcare providers [7]. Published dental articles have reported multiple definitions of teledentistry and related terms, and used several definitions interchangeably, like m-health, teledentistry, tele-oral medicine and telehealth.
To define teledentistry and its related definitions, the first author organized a meeting with the e-oral health network of the International Association of Dental Research (IADR) and other experts in this field [7]. According to the terminology consensus report, teledentistry was defined as follows:
“Teledentistry represents the uses of information and telecommunication technology to provide oral healthcare services between an oral healthcare provider and a patient/recipient or other health care providers, who are separated by distance.”
The prefix “tele” to common dental clinical disciplines describes the application of teledentistry to dental specialties, e.g., “teleperiodontology”, “teleorthodontics” and “telepaedodontics” [9]. Like telemedicine, teledentistry encompasses subunits such as tele-triage, tele-consultation, tele-assistance, tele-diagnosis and tele-monitoring [7].
1.4. The Current Study
The growing use of teledentistry has led to many studies investigating teledentistry applications in different settings. With the increasing number of literature reviews on teledentistry available, the next step in providing policy makers, academics and healthcare providers with evidence is to conduct a review of the existing systematic reviews, i.e., an umbrella review [10]. An umbrella review also helps to identify areas in which research is currently lacking, and to formulate recommendations for practice and for future research [10]. Consequently, the aim of this umbrella review is to synthesize existing systematic reviews on teledentistry and provide a summary of the evidence on its clinical and cost-effectiveness.
2. Materials and Methods
This umbrella review is consistent with the Preferred Reporting Items for Systematic Reviews and Meta Analyses (PRISMA) guidelines [11] and the umbrella review methodology described by Arosmatis and colleagues [12]. In accordance with the PRISMA guidelines, the protocol for this systematic umbrella review was registered in the International Prospective Register of Systematic Reviews (PROSPERO) on 17 May 2023 (PROSPERO 2023 CRD42023363204) with no deviation from it.
2.1. Data Sources and Search Strategy
Seven databases were searched from inception to 24 April 2023: (1) PubMed/MEDLINE (National Library of Medicine); (2) EMBASE; (3) Cumulative Index of Nursing and Allied Health Literature (CINAHL); (4) ISI/Web of Science; (5) Scopus, (6) Cochrane Database of Systematic Reviews (CDSR) and (7) National Health Service Economic Evaluations Database & Health Technology Assessment (NHSEED & HTA). Other sources included the major repositories of systematic reviews, including the JBI Database of Systematic Reviews and Implementation Reports, the Database of Abstracts of Reviews of Effects and the PROSPERO register. A comprehensive search strategy was designed in collaboration with a librarian. Various search terms (including synonyms and closely related words) for teledentistry/telemedicine and oral health/dentistry terms were chosen and used as Medical Subject Headings (MeSH) or free-text words in PubMed. Consequently, the search strategy was adapted and optimized for all consulted databases (See Table S1 in the Supplementary Materials for final search strategies). In addition, manual cross-referencing of the bibliographies of all included studies was carried out. Also, this review utilized indexing sources to retrieve subsequent relevant articles that cited the included publications. EndNote reference manager was used to store retrieved references. The search was not limited to the English language in order to maximize its sensitivity, and to identify the number of publications in other languages.
2.2. Eligibility Criteria
Reviews that measured the costs and oral-health outcomes of teledentistry, compared to traditional alternatives or in addition to usual care, both interventional or observational studies, were included.
2.2.1. Design
We included only peer-reviewed published systematic reviews of primary studies that included a description of search terms and conducted their searches in Medline or PubMed and at least one other international scientific database. Furthermore, position papers, editorial letters, opinion pieces and books chapters were excluded due to the high risk of bias in these publications.
2.2.2. Teledentistry Interventions
Irrespective of the terms used in the reviews, we included reviews in which the original studies measured the effect of teledentistry interventions that met the teledentistry definition published by the e-oral health network (see Introduction [7]). Reviews that focused on the delivery of training to oral health professionals were excluded (as this is not teledentistry, but part of telehealth). A review was included if it consisted of teledentistry interventions involving oral healthcare delivery through telecommunication systems that included either synchronous (real-time) or asynchronous (independent of time) communication between a patient (or caregiver) and their healthcare provider, or between healthcare providers, who are separated by distance.
Therefore, reviews focusing on interventions with no direct interaction with a healthcare provider, or on interventions with unidirectional communication, were excluded. For example, reviews that focused on automated text-message reminders to improve adherence were excluded (e.g., Lima et al. [13]). Also, we excluded reviews if it was unclear whether the studies included contained interventions with unidirectional or directional communication, or if the effects of these unidirectional or directional interventions were not reported separately (e.g., Al-Moghrabi et al. (2022) [14] and Fernandez et al. (2021) [15]). If a review included studies that measured the effect of oral-health or e-health interventions, besides teledentistry interventions, but the results of the effectiveness on teledentistry interventions were not reported separately, then the review was excluded [16,17].
2.2.3. Population and Setting
The review consisted of studies carried out on humans, i.e., patients, healthcare providers and caregivers of any age or condition. In this review, healthcare providers (such as dentists, dental hygienists, nutritionists or nurses) are those who deliver oral healthcare. Reviews were included if the original studies utilized teledentistry within dental practice in general, specialist dental settings, a healthcare setting (such as acute care, primary or community healthcare) or home care.
2.2.4. Outcomes
Reviews were included if they provided adequate information on oral-health outcomes and costs. Outputs included measures of oral health, oral hygiene levels, periodontal status, oral-health-related behaviours and oral-health-related quality of life. We excluded the psychosocial factors of oral-health behaviour (such as attitude), as these outcomes are less closely related to (better) oral health. Reviews reporting on multiple health outcomes, but separately reporting results on oral health, were included. Additionally, outcomes regarding costs included measures of economic evaluations, direct costs and indirect costs (e.g., reduced waiting lists, hours per patient, number of referrals, mean waiting times, inappropriate referrals and travel time). These outcomes were selected to reflect one of the main goals of teledentistry, which is to increase access to oral-health services while minimizing the costs and improving the quality of care. If an economic evaluation did not compare the costs and outcomes of two or more alternatives, it falls under the category of partial economic evaluation. Partial economic evaluations encompass studies focusing on (1) cost description, (2) cost-consequence description and (3) cost analysis [18]. Reviews of partial economic evaluations were also selected.
2.2.5. Language
Manuscripts swritten in English, Dutch, Spanish or German were included, as the first author and one of the co-authors could understand scientific articles written in those languages.
2.3. Study Selection
The study selection was performed in two stages after removing the duplicates and inserting the studies into Rayyan software [19]. Deduplication was performed semi-automatically, using the deduplication capabilities in Endnote [20] and a manual check for the author and title by a medical-information specialist. In the first stage, two authors (JS and AQ) independently read the titles and abstracts of potentially relevant articles against the eligibility criteria. Disagreements were discussed and all were easily resolved through discussion. In the second stage, the full-text of the selected articles was obtained and the same two persons independently applied the eligibility criteria to confirm the final selection. Citations were coded in Rayyan as ‘included’, ‘excluded’ or ‘maybe’, as appropriate. All disagreements (indicated as ‘conflicts’ (n = 7) and ‘maybe’ (n = 37)) were resolved through discussion. If necessary (n = 10), a third reviewer (RM) was consulted to reach consensus.
2.4. Data Extraction
The first author extracted the data from the full-text articles. Other reviewing authors (AQ, BV, LS, BvM and RM) verified the extracted data. Information was extracted from each included study on the following: (1) citation details (authors’ names and year of publication); (2) objectives of the included reviews; (3) type of review; (4) participant details; (5) setting and context; (6) number of databases sourced and searched; (7) date range of database searching; (8) publication date range of studies included in the review that informed each outcome of interest; (9) number of studies, types of studies and country of origin of studies included in each review; (10) instrument used to appraise the primary studies and the rating of their quality; (11) outcomes reported that were relevant to the umbrella-review question; (12) method of synthesis/analysis employed to synthesize the evidence. The extracted data are presented in the tables and text.
2.5. Quality Assessment of the Selected Studies
The first author and co-authors assessed the methodological quality (critical ap-praisal) of the included studies using the validated measurement tool to assess system-atic reviews (AMSTAR 2) [21] (See File S1 in the Supplementary Materials for the AMSTAR 2 checklist). According to AMSTAR 2, reviews are graded according to methodological flaws in seven critical and nine non-critical domains. AMSTAR 2 was chosen for its content validity and its ability to assess systematic reviews of both ran-domized and non-randomized studies. Before rating the included systematic reviews, each rater reviewed the AMSTAR 2 comprehensive user guide (See File S2 in the Supplementary Materials for the user guide). An overall rating of each systematic review was calculated using the AMSTAR 2 online form [21]. Discrepancies among assessors were resolved via discussion until reaching consensus.
2.6. Data Analysis
According to the methodological approach for umbrella reviews that was reported by Aromataris et al. (2015), the analytical unit is the literature review, not the included primary studies (except when an outcome is only informed by one included study) [12]. However, we conducted thorough investigations into the original references identified by the systematic reviews. The overlap of original articles was taken into account when interpreting the data. In the results, we explicitly stated which references measured the outcomes of interests and reported whether there was any overlap. The results are presented narratively and with tables and figures for illustration. No attempt was made to compare teledentistry interventions across reviews or across review populations, and a meta-analysis was precluded due to the heterogeneity of teledentistry interventions, population and outcomes.
3. Results
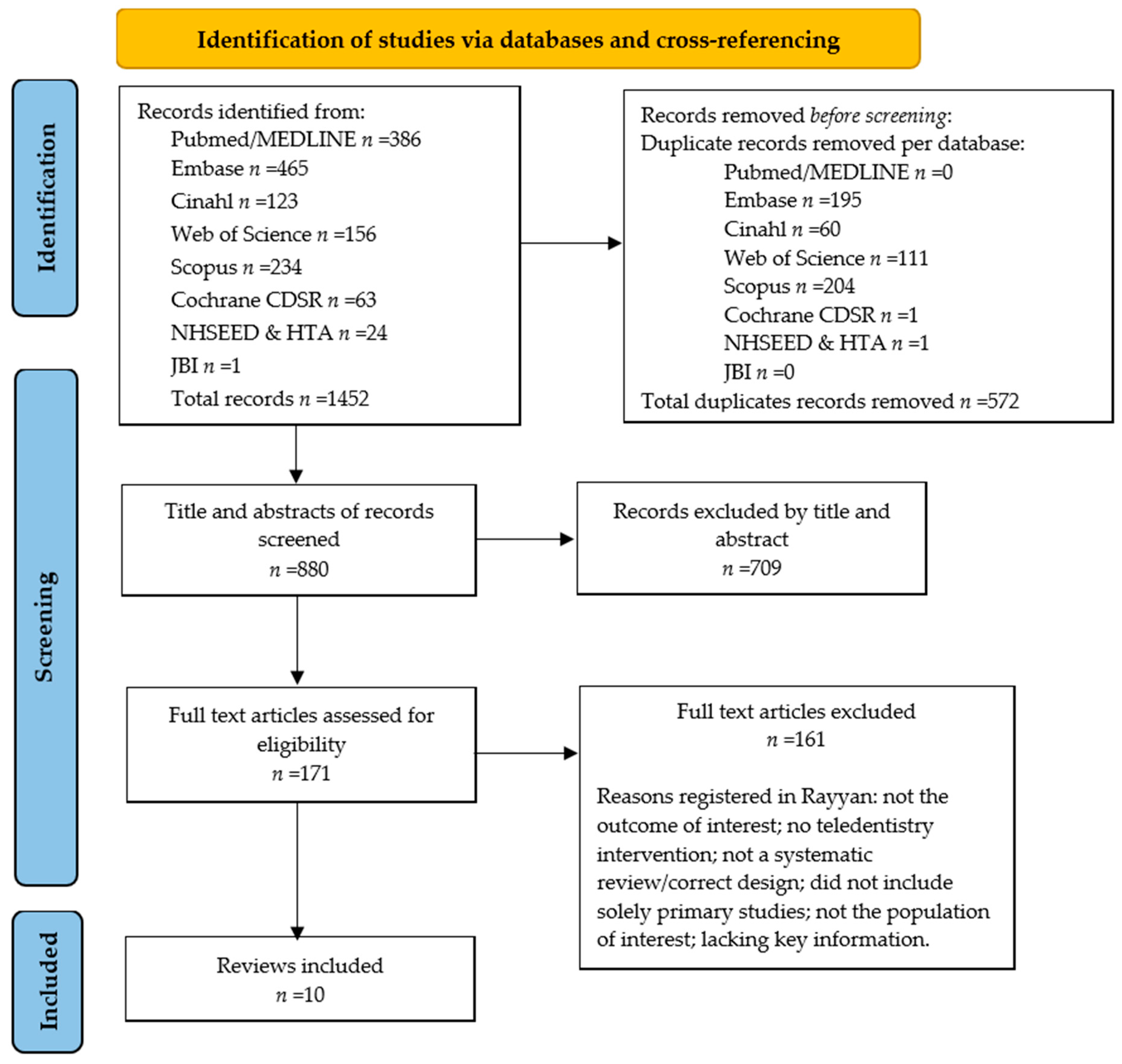
Figure 1 presents the umbrella-review selection process in a PRISMA flow diagram. After removing duplications, the combined searches yielded 880 articles. Based on the screening of titles and abstracts, 171 full-text articles were obtained and evaluated for the preset eligibility criteria. During the full-text screening process, we excluded reviews in which we were unable to judge whether the review met the eligibility criteria due to lacking key information, i.e., important details on the design, intervention or if the outcome measures of the included studies were not clear or missing [9,22,23,24,25,26,27,28,29]. One review’s conclusion about the costs was in contrast with the conclusion stated in the original article and was therefore excluded during the data-selection process [30]. In total, 10 reviews were included in this umbrella review [31,32,33,34,35,36,37,38,39,40].
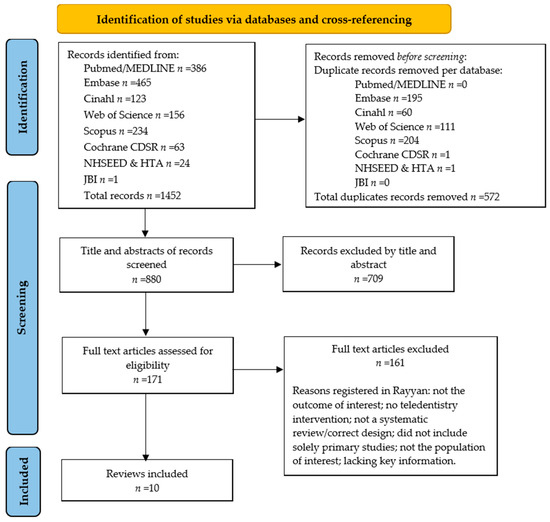
Figure 1.
A PRISMA flow diagram of the umbrella review.
Table 1 presents an overall description of the included reviews characteristics and findings. All included reviews employed qualitative analysis to synthesize the evidence. In only one study, the primary research aim aligned with our study aim and thus exclusively addressed the outcome of interest [37]. Conversely, the remaining studies covered multiple outcomes and the outcomes of interest were reported as secondary outcome measures.

Table 1.
Included review characteristics and findings.
The modality of the teledentistry intervention, i.e., as synchronous (real-time) or asynchronous (store-and-forward) interactions [7], was only reported in two included reviews [31,39], of which tele-consultation was a common real-time interaction. Aquilanti et al. 2020 [31] stated that the asynchronous (store-and-forward) model was always the less costly one, followed by the real-time model and face-to-face dental visits. Also, Joshi et al., 2020 [39], stated that real-time consultation had better outcomes concerning costs.
3.1. An Overview of the Outcomes Reported by the Teledentistry Reviews
3.1.1. Oral-Health Outcomes
Two reviews assessed the effectiveness of teledentistry on oral-health outcomes compared to traditional alternatives [32,37].
The review by Ben-Omran et al. (2021) [32] reported that there was no significant difference between intervention and control groups in terms of Geriatric Oral Health Assessment Index scores, measuring the oral-health-related quality of life. Despite positive findings, Ben-Omran and his colleagues concluded that there was insufficient evidence to firmly advocate for the long-term clinical effectiveness of teledentistry.
The review by Estai et al. (2018) [37] included nine articles considering various clinical outcomes, of which three studies specifically addressed the clinical outcome of interest, i.e., DFS scores, periodontal indices and oral hygiene scores. Despite the diverse objectives, methodologies and outcome measures employed across the included studies, teledentistry interventions were comparable to, or had advantages over, non-telemedicine approaches. However, Estai and his colleagues’ overall conclusion was that there is not yet enough conclusive evidence of the effectiveness and long-term use of teledentistry.
3.1.2. Economic Evaluations and Costs
Ten reviews focused on outcomes with regard to costs and economic evaluations; of these, only five [31,32,35,36,37] provide reports on costs as outcomes of interest in their reviews and included a review of studies of true economic evaluation as defined by Drummond and collaborators (2005) [18]. The review conducted by Aquilanti and collaborators [31] included three studies reporting economic evaluations. Estai and collaborators’ [37] review also included three studies reporting economic evaluations. Those two reviews used the Drummond and collaborators’ checklist [18] to evaluate the quality of the economic evaluations. Interestingly, although these two reviews were conducted in different years, they included different studies and only one overlapped. Moreover, for the overlapping study, despite employing an identical assessment tool (Drummond et al.’s), each review yielded disparate scores.
A more recent review by Emami and collaborators [36] identified seven studies which include some elements of economic evaluation and used the level of evidence according to the Oxford Centre for Evidence-Based Medicine [41]. On the other hand, Daniel and collaborators [35] and Ben-Omran and collaborators [32] included two studies each that were found to be economic evaluations, but no evaluation tool was mentioned to facilitate the quality-evaluation task.
Interestingly, overall, these ten reviews encompassed a total of five different studies that incorporated some form of economic evaluation. These evaluations included a range of economic impacts and study designs; cost descriptions; cost analysis; cost-minimization analysis; and even time-effectiveness, which is not typically considered a form of economic evaluation on its own.
The remaining four reviews [34,38,39,40] did not report on true economic evaluations, but summarized information on costs. This information mentioned costs, mostly as the reduction of costs by using teledentistry in terms of the reduction of travel and waiting times, and of other features of telehealth that are related to costs (e.g., reduced loss of productivity, less unnecessary travel, fewer accommodation expenses and reduced time for services). Furthermore, these reviews included studies on the reduction of cost, but were not related to any health outcomes, and found that teledentistry is likely to be a cost-effective or a cost-saving alternative compared to the standard practice of face-to-face consultation. Two of those reviews [38,39] mentioned that the cost-effectiveness of teledentistry was an assumption based on the reduction of cost, but without providing any evidence of studies that substantiated claims regarding cost-effectiveness. Conversely, another study [35] emphasized the need for further economic evaluation in teledentistry to support any contention on cost-effectiveness. The review conducted by Estai and collaborators [37] indicated that cost-minimization was said to be conducted in two studies; however, a closer examination of the original studies does not support that statement. Instead, the economic analyses in the original studies were more like cost-analysis studies. Furthermore, the review by Estai et al. concluded that none of the studies included considered cost–benefit, cost-effectiveness, cost–utility or incremental economic analyses.
3.2. Results of Quality Appraisal
According to the AMSTAR-2 quality-assessment tool, all reviews were of critically low or low quality (see Table 2). The most common weakness across the reviews was a poor description of the original studies (e.g., missing important information on outcomes, study design or intervention). According to the authors of the included reviews, the original articles were descriptive in nature and provided a poor quality of evidence, which in turn contributed to the poor reporting quality of the reviews. The absence of good-quality economic studies in teledentistry has also been cited in the included reviews (e.g., [35,37]).

Table 2.
Methodological quality of included systematic reviews.
For the majority of reviews, the AMSTAR-2 quality scores were low for the following domains: Q3 (reviews did not explain the selection of the study design), Q7 (reviews did not justify the reasons for exclusions or search limitations), Q8 (reviews did not describe the studies sufficiently), Q13 (reviews did not take into consideration the risk of bias in the interpretation of the results) and Q14 (reviews did not explain how heterogeneity across studies may have impacted the results). None of the included reviews reported on the sources of funding for primary studies (Q10).
4. Discussion
The aim of this umbrella review was to synthesize the existing systematic reviews on teledentistry and provide a summary of evidence of teledentistry’s effects on oral-health outcomes and costs.
4.1. Main Findings
In this umbrella review, ten articles were selected. While most reviews described positive effects of teledentistry on oral-health outcomes, it is important to interpret these findings cautiously, due to their overall critically low quality, according to AMSTAR-2 criteria. The benefits of teledentistry and piloting teledentistry have been explored widely; however, studies focusing on the clinical effectiveness of the use of teledentistry and immediate clinical implications are limited.
Teledentistry is commonly perceived to be cost-saving and cost effective; however, this is often only based on assumptions. Although some reviews explored the health economic implications related to teledentistry, most of them based their conclusions on low-quality observational studies without clear methodologies or with small sample sizes, or on self-reports or the subjective opinions of participants. These designs do not allow for evidence-based conclusions on their cost-effectiveness. Clinical trials, particularly RCTs and other quasi-experimental designs, are in general best suited for assessing the efficacy and cost-effectiveness of an intervention, and thus allow for strong evidence-based conclusions. However, digital health interventions are complex interventions and some evaluation methods, for example, RCTs, may not be the most effective way of evaluating digital technology deployments in healthcare [42]. While RCTs provide valuable data on the clinical efficacy and safety of a particular intervention, they may not capture its economic implications and long-term outcomes. When assessing cost-effectiveness, effectiveness trials may be more suitable as they provide insights into the real-world performance of the intervention.
Hrynyschyn et al. (2022) conducted a scoping review to identify alternatives to RCT’s as potentially more appropriate evaluation methods of digital health interventions [42]. According to the authors, factorial designs were mostly used to evaluate digital health interventions, followed by stepped-wedge designs, sequential multiple assignment randomised trials (SMARTs), and micro randomised trials (MRTs) [42]. Some of these methods allow for the adaptation of interventions (e.g., SMART or MRT) and the evaluation of specific components of interventions (e.g., factorial designs) [42].
Economic evaluations are essential for informing policymakers and dental practitioners about the feasibility, benefits and challenges of integrating teledentistry into healthcare systems. Researchers and healthcare professionals increasingly acknowledge the importance of assessing the cost effectiveness, return on investment, and overall economic viability of teledentistry. The growing interest in teledentistry emphasizes the need for economic evaluations to comprehend its financial implications and benefits when integrated into oral-healthcare systems [9,35]. Nonetheless, Mariño et al.’s (2013) [9] assertion remains relevant: there is still a scarcity of studies that adequately address the issue of the economic evaluation of teledentistry. Our research demonstrated a comparatively restricted number of cost-analyses and economic assessments specifically targeting teledentistry (n = 10) when compared to other sectors of telemedicine. To illustrate, Bergmo’s systematic review spanning 1990–2007 identified only 33 economic evaluations within telemedicine [43]. Importantly, the economic evaluations in teledentistry have shown low adherence to Drummond’s standards [18]. This observation aligns with the quality assessments found in reviews of telemedicine.
To the best of our knowledge, this study is the first ever umbrella review to focus on the effects of teledentistry on costs and oral-health outcomes. Our findings are consistent with similar reviews conducted on both the clinical outcomes and cost-effectiveness of telemedicine [8]. Eze et al. [8] reported in their umbrella review on telemedicine that 92% of the included systematic reviews were of a low to critically low quality, measured with the same quality-measurement assessment tool as used in our umbrella review (AMSTAR). They reported that telemedicine can be cost-effective and can improve clinical outcomes, such as glycaemic control in diabetic patients and improving patients’ diet quality and nutrition. However, they found that generalizability was also hindered by poor quality and reporting standards.
4.2. Quality Assessment of the Included Reviews
To assess the quality of the included reviews, we used the AMSTAR2 quality-assessment tool. All the included systematic reviews were of “low” or “critically low” quality, resulting in a high risk of bias for our findings. The low quality of reviews available in the literature was mostly caused by poor reporting quality or unavailable data (e.g., missing details on the outcomes, interventions or study designs of the included studies).
Selection bias may have occurred when we had to exclude a great number of reviews (n = 9) that lacked key information, such as when the description of the studies was too poor and data extraction was not possible to perform. This was mostly the case when the primary research aim of that study had a different focus than our study aim. The majority of the included reviews stated that most of the original articles included in the reviews were also poorly reported. To improve the quality of future research, researchers could use the guidelines for reporting research that can be found on the website of ‘Enhancing the QUAlity and Transparency Of health Research’ (EQUATOR network) to ensure that they report all key information.
4.3. Strengths, Limitations and Recommendations
An advantage of an umbrella review is that it identifies gaps in a specific research field and can inform future research [44]. A disadvantage of an umbrella review is that the validity of the findings depends on the quality of the eligible systematic reviews and meta-analyses. A limitation of our umbrella review was the low quality of the included reviews according the AMSTAR2 assessment, which influences the validity of the findings of this umbrella review. Although AMSTAR2 is a validated tool, some modifications could improve its validity. For example, this assessment tool does not consider the study designs of the original studies included in the systematic reviews. However, the quality of the review can be influenced by the study designs and the robustness of the results.
Studies have reported multiple definitions on e-health and used several definitions interchangeably, such as m-health, teledentistry, tele-oral medicine, and telehealth. Another strength of this review is that we used the definition of teledentistry defined by the e-oral health network of the IADR and used this terminology to label the intervention in the reviews, rather than the terms stated in the article [7]. This is important because although the authors employed a wide search in seven databases to include all articles using alternative terms for teledentistry, it is possible that we missed articles employing alternative terminology. A recommendation arising from this review is therefore the use of universal terminology to label interventions in future research, as it would prevent different uses of terminology in future studies, increasing the homogeneity of studies and preventing publication bias. The use of terminology proposed by the e-oral health network [7] could help in achieving this objective.
Teledentistry interventions are highly diverse in both context and applications. Given the heterogeneity of primary study samples, interventions and design, and the lack of key information on the content of the teledentistry interventions and outcomes, subgroup analyses and meta-analyses were not possible, limiting the findings. Nevertheless, we have provided a narrative review by outlining the current evidence on the effectiveness of teledentistry and highlighting the research gaps for future studies. Categorizing interventions in future studies by the types of teledentistry applications [7] and their modalities (store-forward or real-time) can be useful to provide a better overview and compare the results across studies in the future.
A high prevalence of oral diseases and a high level of unmet oral health needs are common among people living with disabilities and mental health illnesses, and among institutionalized/hospitalized people and older people [45]. Moreover, poor oral-health status is a marker of adverse health outcomes and health inequalities, indicating that enhancing access to dental care is crucial in these patient groups, for example, people with poor access to care [45].
Oral-health professionals could remotely assist other healthcare professionals to provide oral-health care in people with poor access to care. These people could greatly benefit from teledentistry applications, like teleconsultation with small cameras. However, our umbrella review shows that teledentistry has rarely been applied, and no experimental study on the effectiveness have been performed on these groups of the population with special healthcare needs [40]. Thus, especially these populations, there is a need for more high-quality experimental studies measuring the effects of teledentistry on oral-health-related outcomes and costs.
Artificial intelligence (AI) has evolved tremendously in recent years, and the application of AI in teledentistry has the potential to revolutionize remote dental care [46]. Machine learning, including deep learning-based algorithms, has been developed to create predictive models of risk assessment and diagnostic services for oral health, which can enable teledentistry to better its remote screening, diagnoses, record keeping, triaging, and monitoring of dental diseases [7,46]. We, therefore, assume that in the future, teledentistry with the integration of AI can play a bigger role in improving efficiency and quality of care, and to support healthcare systems providing cost-effective care. To reach this objective, research will also need to be stepped up in this AI area so that cost-effective interventions can be implemented.
5. Conclusions
Ten reviews researched the promising potential of teledentistry; however, evaluations on cost and oral-health outcomes are scarce. Only five studies incorporated some form of economic evaluation. These evaluations included a range of economic impacts and study designs; cost descriptions, cost analysis, cost-minimization analysis, and even time-effectiveness, which is not typically considered a form of economic evaluation on its own. Thus, there is insufficient qualitative evidence to support conclusions on the cost-effectiveness or long-term effectiveness of teledentistry.
The main limitation of our review stems from the low or critically low quality of the included reviews, as per the AMSTAR-2 criteria. Many of these reviews drew conclusions from studies of low quality with poor design reporting and a descriptive nature, thereby contributing to the overall poor reporting quality within the included reviews.
Therefore, high-quality experimental studies (e.g., RCT’s, factorial designs, stepped-wedge designs, SMARTs and MRTs) on the clinical- and cost-effectiveness of teledentistry are needed to increase the body of evidence regarding the digitalization of oral care.
A recommendation for future research is the universal use of terminology on teledentistry and its related terms. Using the terminology created by the e-oral health network and used in this study will help to standardize approaches and compare results across studies.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/ijerph21040407/s1, Table S1: The final search strategy adapted and optimized for all consulted databases; File S1: File AMSTAR checklist; File S2: AMSTAR guided document.
Author Contributions
J.F.M.S. was responsible for the conceptualization, methodology, investigation and wrote the original draft. J.F.M.S. and A.H.Q. selected the studies independently. J.F.M.S. and R.M. contributed to the acquisition of the data and analysis, and edited the results. A.H.Q., B.V., L.S., B.v.M. and R.M. verified the data extraction and quality assessment. All authors (J.F.M.S., A.H.Q., B.V., L.S., H.B., N.G., B.v.M. and R.M.) contributed to the conceptualization, interpretation of the results and have reviewed the final manuscript. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by Regieorgaan SIA RAAK part of the Netherlands Organisation for Scientific Research (NWO); grant number: HBOPD.2018.05.016. The funder had no role in study design, data collection, data analysis, data interpretation, or the article’s writing.
Acknowledgments
The authors sincerely thank Caroline Planting, a librarian of VU Medical Centre, for her input and help with creating a search protocol and a comprehensive search strategy, and performing the search in all databases.
Conflicts of Interest
The authors declare no conflicts of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript; or in the decision to publish the results. The authors are solely responsible for the views expressed in this publication, and these views do not necessarily represent the perspectives, decisions or policies of the author’s employer, institution or organization.
References
- Deml, M.J.; Jungo, K.T.; Maessen, M.; Martani, A.; Ulyte, A. Megatrends in Healthcare: Review for the Swiss National Science Foundation’s National Research Programme 74 (NRP74) “Smarter Health Care”. Public Health Rev. 2022, 43, 1604434. [Google Scholar] [CrossRef] [PubMed]
- Ernst and Young. Health Reimagined: A New Participatory Health Paradigm. 2015. Available online: https://eysweeney.com.au/Documents/EYHealthReimagined2016.pdf (accessed on 22 December 2022).
- Day, G.E. Is our health workforce prepared for future health megatrends? Aust. Health Rev. 2015, 39, 487–488. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. Global Strategy on Digital Health 2020–2025; Licence: CC BY-NC-SA 3.0 IGO; World Health Organization: Geneva, Switzerland, 2021. [Google Scholar]
- Butcher, C.J.; Hussain, W. Digital healthcare: The future. Future Healthc. J. 2022, 9, 113–117. [Google Scholar] [CrossRef] [PubMed]
- Gentili, A.; Failla, G.; Melnyk, A.; Puleo, V.; Tanna, G.L.D.; Ricciardi, W.; Cascini, F. The cost-effectiveness of digital health interventions: A systematic review of the literature. Front. Public Health 2022, 10, 787135. [Google Scholar] [CrossRef] [PubMed]
- Mariño, R.J.; Uribe, S.E.; Chen, R.; Schwendicke, F.; Giraudeau, N.; Scheerman, J.F.M. Terminology of e-Oral Health: Consensus Report of the IADR’s e-Oral Health Network Terminology Task Force. BMC Oral Health 2024, 24, 280. [Google Scholar] [CrossRef] [PubMed]
- Eze, N.D.; Mateus, C.; Cravo Oliveira Hashiguchi, T. Telemedicine in the OECD: An umbrella review of clinical and cost-effectiveness, patient experience and implementation. PLoS ONE 2020, 15, e0237585. [Google Scholar] [CrossRef] [PubMed]
- Mariño, R.; Ghanim, A. Teledentistry: A systematic review of the literature. J. Telemed. Telecare 2013, 19, 179–183. [Google Scholar] [CrossRef] [PubMed]
- Grant, M.J.; Booth, A. A typology of reviews: An analysis of 14 review types and associated methodologies. Health Inf. Libr. J. 2009, 26, 91–108. [Google Scholar] [CrossRef]
- Moher, D.; Shamseer, L.; Clarke, M.; Ghersi, D.; Liberati, A.; Petticrew, M.; Shekelle, P.; Stewart, L.A.; PRISMA-P Group. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015 statement. Syst. Rev. 2015, 4, 1. [Google Scholar] [CrossRef] [PubMed]
- Aromataris, E.; Fernandez, R.; Godfrey, C.M.; Holly, C.; Khalil, H.; Tungpunkom, P. Summarizing systematic reviews: Methodological development, conduct and reporting of an umbrella review approach. Int. J. Evid. Based Health 2015, 13, 132–140. [Google Scholar] [CrossRef]
- Lima, I.F.P.; de Andrade Vieira, W.; de Macedo Bernardino, I.; Costa, P.A.; Lima, A.P.B.; Pithon, M.M.; Paranhos, L.R. Influence of reminder therapy for controlling bacterial plaque in patients undergoing orthodontic treatment: A systematic review and meta-analysis. Angle Orthod. 2018, 88, 483–493. [Google Scholar] [CrossRef] [PubMed]
- Al-Moghrabi, D.; Alkadhimi, A.; Tsichlaki, A.; Pandis, N.; Fleming, P.S. The influence of mobile applications and social media-based interventions in producing behavior change among orthodontic patients: A systematic review and meta-analysis. Am. J. Orthod. Dentofac. Orthop. 2022, 161, 338–354. [Google Scholar] [CrossRef] [PubMed]
- Fernandez, C.E.; Maturana, C.A.; Coloma, S.I.; Carrasco-Labra, A.; Giacaman, R.A. Teledentistry and mHealth for Promotion and Prevention of Oral Health: A Systematic Review and Meta-analysis. J. Dent. Res. 2021, 100, 914–927. [Google Scholar] [CrossRef]
- Hofmann, U.K.; Hildebrand, F.; Mederake, M.; Migliorini, F. Telemedicine in orthopaedics and trauma surgery during the first year of COVID pandemic: A systematic review. BMC Musculoskelet. Disord. 2023, 24, 101. [Google Scholar] [CrossRef] [PubMed]
- Van den Bosch, S.C.; van de Voort, N.E.M.; Xi, T.; Kool, R.B.; Bergé, S.J.; Faber, M.J. Oral & Maxillofacial surgery is ready for patient-centred eHealth interventions − the outcomes of a scoping review. Int. J. Oral Maxillofac. Surg. 2019, 48, 830–840. [Google Scholar]
- Drummond, M.F.; Sculpher, M.J.; Claxton, K.; Stoddart, G.L.; Torrance, G.W. Methods for the Economic Evaluation of Health Care Programmes; Oxford University Press: Oxford, UK, 2015; ISBN 978-0-19-164358-3. [Google Scholar]
- Ouzzani, M.; Hammady, H.; Fedorowicz, Z.; Elmagarmid, A. Rayyan-a web and mobile app for systematic reviews. Syst. Rev. 2016, 5, 210. [Google Scholar] [CrossRef] [PubMed]
- Bramer, W.M.; Giustini, D.; de Jonge, G.B.; Holland, L.; Bekhuis, T. De-duplication of database search results for systematic reviews in EndNote. J. Med. Libr. Assoc. 2016, 104, 240–243. [Google Scholar] [CrossRef] [PubMed]
- Shea, B.J.; Reeves, B.C.; Wells, G.; Thuku, M.; Hamel, C.; Moran, J.; Moher, D.; Tugwell, P.; Welch, V.; Kristjansson, E.; et al. AMSTAR 2: A critical appraisal tool for systematic reviews that include randomised or non-randomised studies of healthcare interventions, or both. BMJ 2017, 358, j4008. [Google Scholar] [CrossRef] [PubMed]
- Al-Shammery, D.; Alqhtani, N.; Alotaibi, A.N.; AlSharidah, M.; AlShehri, K.; AlShamrani, A. Contributions and Concerns about the Use of Teledentistry in Clinical Orthodontics. Oral Health Prev. Dent. 2021, 19, 465–469. [Google Scholar]
- Dailah, H.G. Mobile Health (mHealth) Technology in Early Detection and Diagnosis of Oral Cancer-A Scoping Review of the Current Scenario and Feasibility. J. Health Eng. 2022, 2022, 4383303. [Google Scholar] [CrossRef] [PubMed]
- Da Silva, H.E.C.; Santos, G.N.M.; Ferreira Leite, A.; Mesquita, C.R.M.; de Souza Figueiredo, P.T.; Miron Stefani, C.; de Santos Melo, N. The feasibility of telehealth in the monitoring of head and neck cancer patients: A systematic review on remote technology, user adherence, user satisfaction, and quality of life. Support. Care Cancer 2022, 30, 8391–8404. [Google Scholar] [CrossRef] [PubMed]
- Kirkwood, B. Development of Military Teledentistry. Med. J. 2021, 33–39. [Google Scholar]
- Minervini, G.; Russo, D.; Herford, A.S.; Gorassini, F.; Meto, A.; D’Amico, C.; Cervino, G.; Cicciù, M.; Fiorillo, L. Teledentistry in the Management of Patients with Dental and Temporomandibular Disorders. BioMed Res. Int. 2022, 2022, 7091153. [Google Scholar] [CrossRef] [PubMed]
- Poirier, B.; Jensen, E.; Sethi, S. The evolution of the teledentistry landscape in Australia: A scoping review. Aust. J. Rural Health 2022, 30, 434–441. [Google Scholar] [CrossRef] [PubMed]
- Saccomanno, S.; Quinzi, V.; Albani, A.; D’Andrea, N.; Marzo, G.; Macchiarelli, G. Utility of Teleorthodontics in Orthodontic Emergencies during the COVID-19 Pandemic: A Systematic Review. Healthcare 2022, 10, 1108. [Google Scholar] [CrossRef] [PubMed]
- Soegyanto, A.I.; Siregar, K.N.; Maharani, D.A.; Wimardhani, Y.S. Teledentistry for Improving Oral Medicine Diagnosis: A Systematic Review. J. Int. Dent. Med. Res. 2022, 15, 365–369. [Google Scholar]
- Aljohani, M.A.B.; Alanazi, A.; Alotaibi, G. Effect of Teledentistry and Outcome for Dental Professionals at Saudi Arabia: A Systematic scoping Review. J. Res. Med. Dent. Sci. 2021, 9, 157–162. [Google Scholar]
- Aquilanti, L.; Santarelli, A.; Mascitti, M.; Procaccini, M.; Rappelli, G. Dental Care Access and the Elderly: What Is the Role of Teledentistry? A Systematic Review. Int. J. Environ. Res. Public Health 2020, 17, 9053. [Google Scholar] [CrossRef] [PubMed]
- Ben-Omran, M.O.; Livinski, A.A.; Kopycka-Kedzierawski, D.T.; Boroumand, S.; Williams, D.; Weatherspoon, D.J.; Iafolla, T.J.; Fontelo, P.; Dye, B.A. The use of teledentistry in facilitating oral health for older adults: A scoping review. J. Am. Dent. Assoc. 2021, 152, 998–1011.e17. [Google Scholar] [CrossRef] [PubMed]
- Costa, C.; Peralta, F.; Mello, A. How Has Teledentistry Been Applied in Public Dental Health Services? An Integrative Review. Telemed. e-Health 2020, 26, 945–954. [Google Scholar] [CrossRef] [PubMed]
- Flores, A.; Lazaro, S.; Molina-Bastos, C.; Guattini, V.; Umpierre, R.; Goncalves, M.; Carrard, V.C. Teledentistry in the diagnosis of oral lesions: A systematic review of the literature. J. Am. Med. Inform. Assoc. JAMIA 2020, 27, 1166–1172. [Google Scholar] [CrossRef] [PubMed]
- Daniel, S.; Wu, L.; Kumar, S. Teledentistry: A systematic review of clinical outcomes, utilization and costs. J. Dent. Hyg. JDH/Am. Dent. Hyg. Assoc. 2013, 87, 345–352. [Google Scholar]
- Emami, E.; Harnagea, H.; Shrivastava, R.; Ahmadi, M.; Giraudeau, N. Patient satisfaction with e-oral health care in rural and remote settings: A systematic review. Syst. Rev. 2022, 11, 234. [Google Scholar] [CrossRef] [PubMed]
- Estai, M.; Kanagasingam, Y.; Tennant, M.; Bunt, S. A systematic review of the research evidence for the benefits of teledentistry. J. Telemed. Telecare 2018, 24, 147–156. [Google Scholar] [CrossRef] [PubMed]
- Irving, M.; Stewart, R.; Spallek, H.; Blinkhorn, A. Using teledentistry in clinical practice, an enabler to improve access to oral health care: A qualitative systematic review. J. Telemed. Telecare 2018, 24, 129–146. [Google Scholar] [CrossRef] [PubMed]
- Joshi, V.; Bhardwaj, P.; Joshi, N.; Singh, K.; Bajaj, K.; Suthar, P. A Scoping review of challenges, scope and assessment approaches of teledentistry: An Indian perspective. Indian J. Community Health 2021, 33, 559–567. [Google Scholar] [CrossRef]
- Uhrin, E.; Domokos, Z.; Czumbel, L.; Kói, T.; Hegyi, P.; Hermann, P.; Borbély, J.; Cavalcante, B.G.N.; Németh, O. Teledentistry: A Future Solution in the Diagnosis of Oral Lesions: Diagnostic Meta-Analysis and Systematic Review. Telemed. J. E Health 2023, 29, 1591–1600. [Google Scholar] [CrossRef] [PubMed]
- Oxford Centre for Evidence-Based Medicine. Levels of Evidence; Oxford Centre for Evidence-Based Medicine: Oxford, UK, 2009; Available online: https://ec.europa.eu/health/scientific_committees/scheer/docs/sunbeds_co241_en.pdf (accessed on 22 December 2023).
- Hrynyschyn, R.; Prediger, C.; Stock, C.; Helmer, S.M. Evaluation Methods Applied to Digital Health Interventions: What Is Being Used beyond Randomised Controlled Trials?—A Scoping Review. Int. J. Environ. Res. Public Health 2022, 19, 5221. [Google Scholar] [CrossRef] [PubMed]
- Bergmo, T.S. Can economic evaluation in telemedicine be trusted? A systematic review of the literature. Cost Eff. Resour. Alloc. 2009, 7, 18. [Google Scholar] [CrossRef] [PubMed]
- Belbasis, L.; Bellou, V.; Ioannidis, J. Conducting umbrella reviews. BMJ Med. 2022, 1, e000071. [Google Scholar] [CrossRef] [PubMed]
- Council of Australian Governments; Oral Health Monitoring Group. Healthy Mouths, Healthy Lives: Australia’s National Oral Health Plan 2015–2024; COAG: Canberra, Australia, 2015. Available online: http://www.coaghealthcouncil.gov.au/Publications/Reports/ArtMID/514/ArticleID/81/Australias-National-Oral-Health-Plan-2015-2024 (accessed on 22 December 2023).
- Batra, P.; Tagra, H.; Katyal, S. Artificial Intelligence in Teledentistry. Discoveries 2022, 10, 153. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2024 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).