Validity and Reliability of Short-Term Heart Rate Variability Parameters in Older People in Response to Physical Exercise
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Participants
2.3. Procedures
2.4. Assessments
2.4.1. Morphological Measures
2.4.2. Cardiovascular Parameters
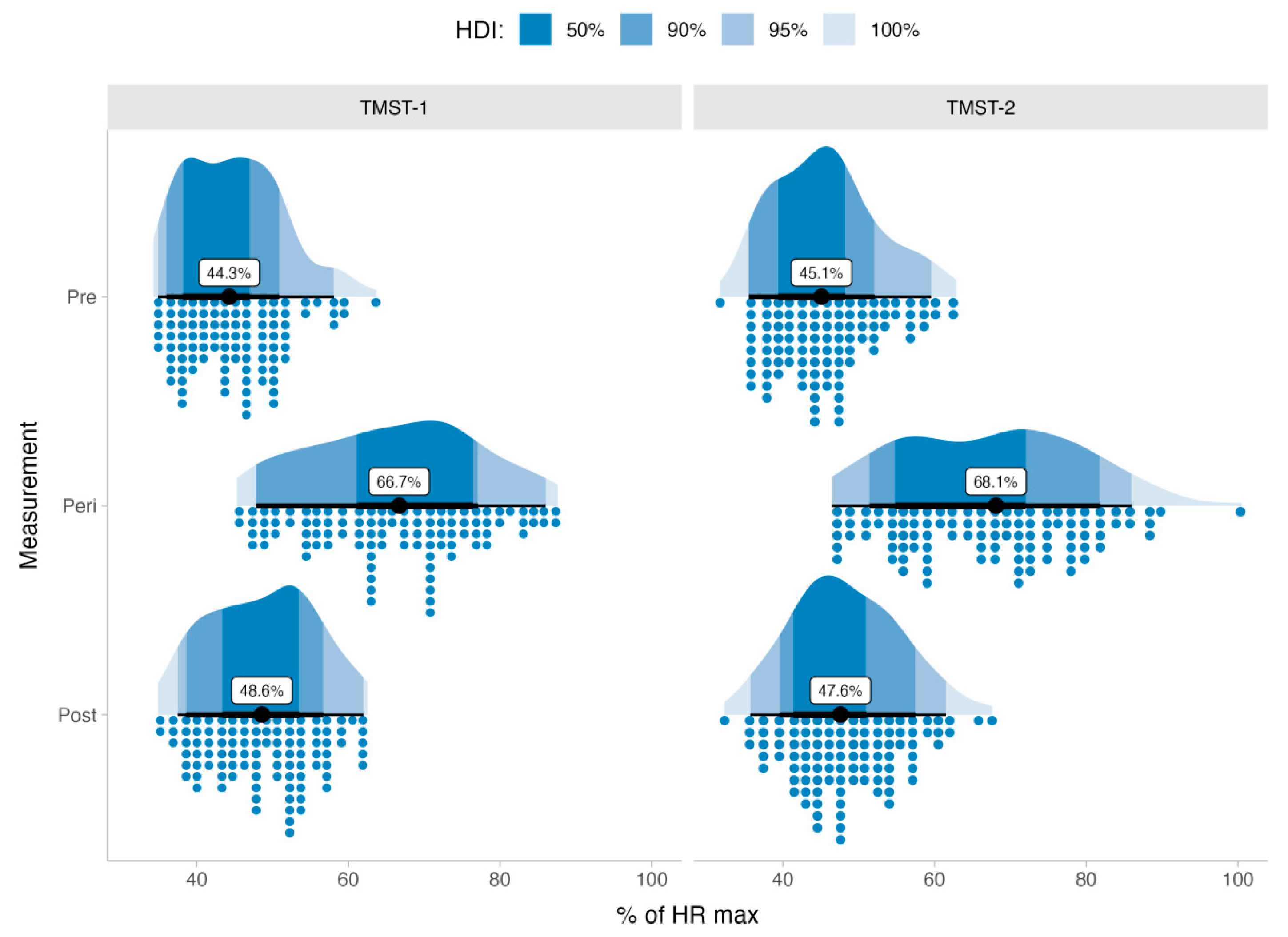
2.4.3. 2-Minute Step Test
2.5. Statistical Analysis
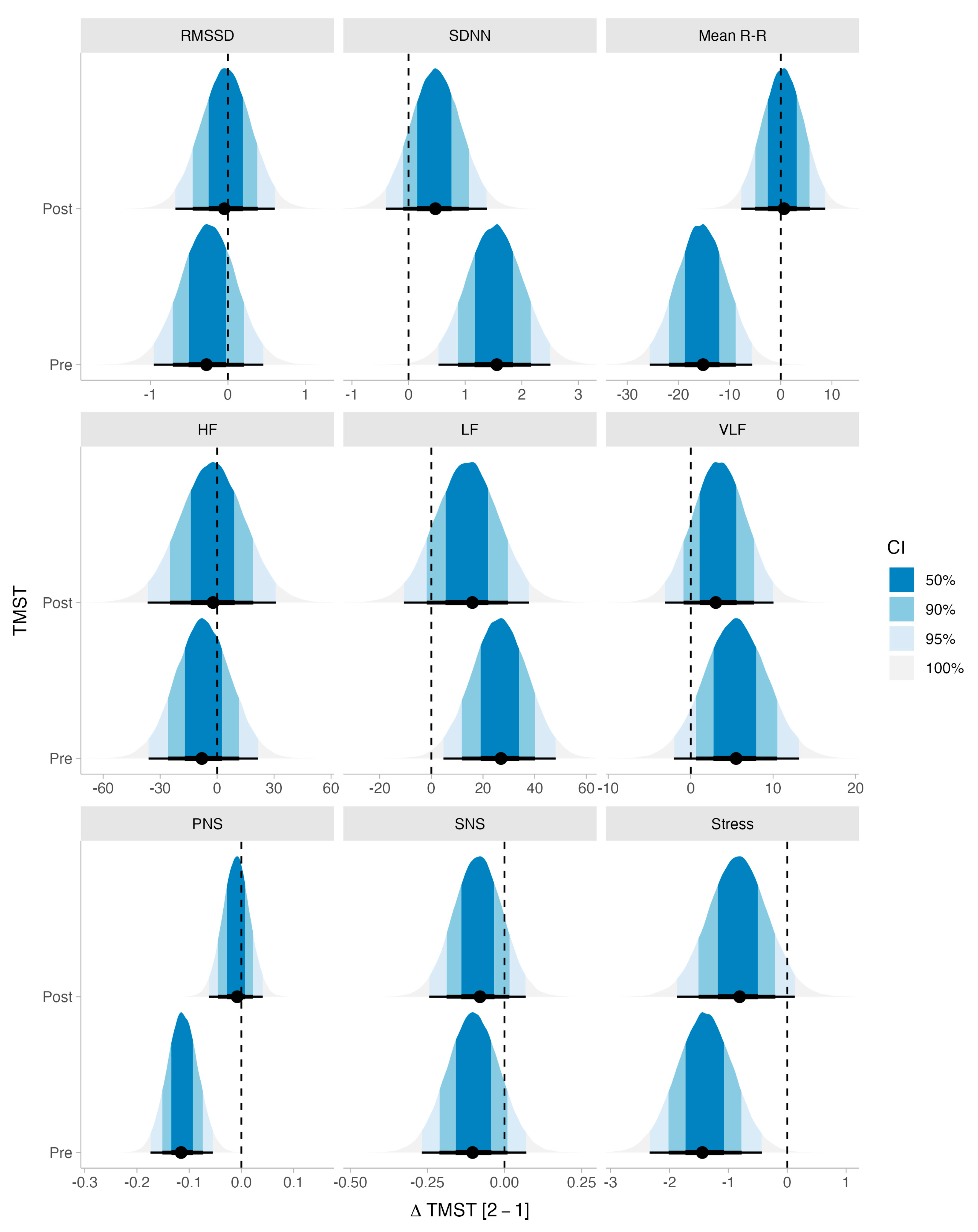
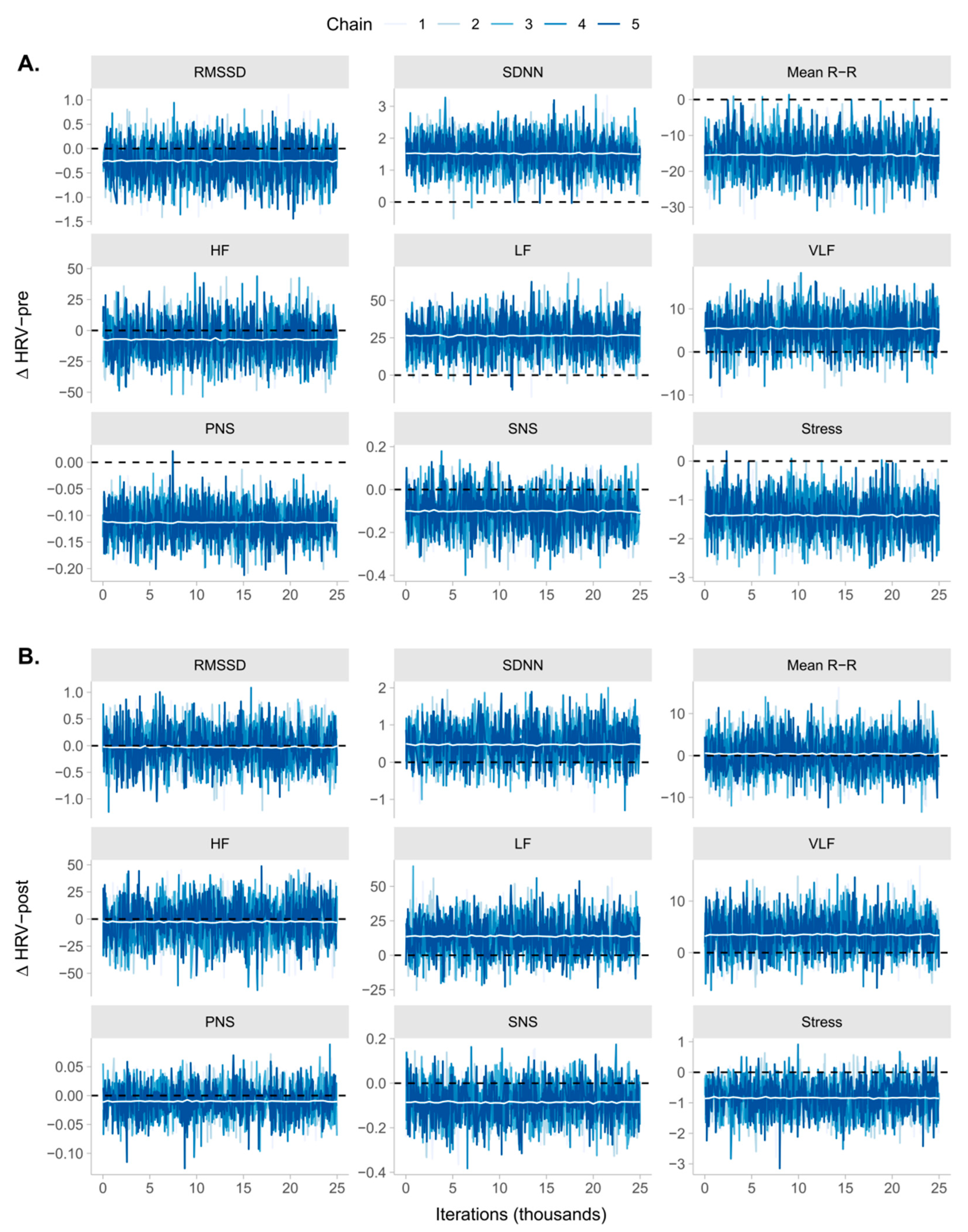
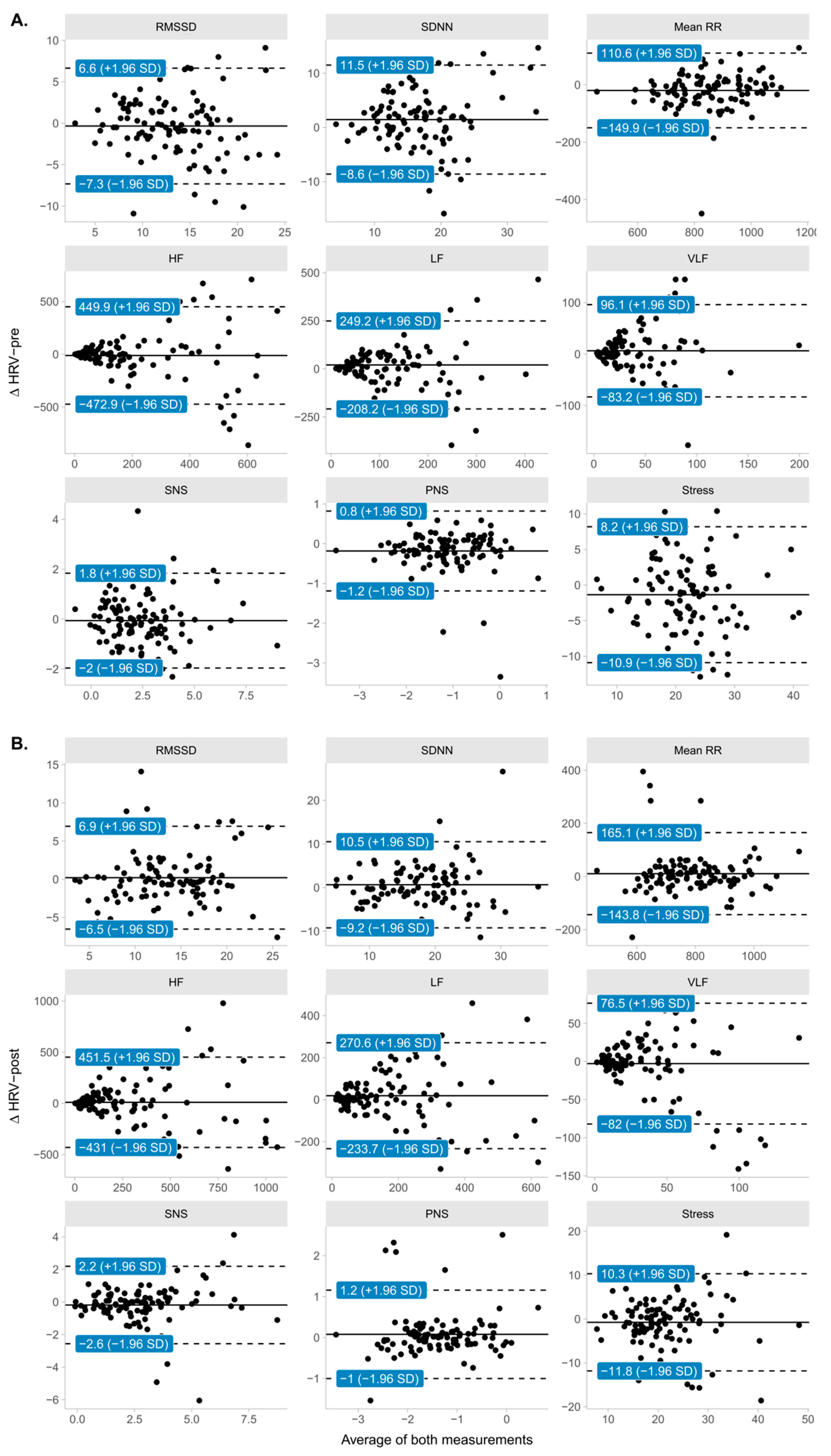
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
| Measure | Prior | ||
|---|---|---|---|
| Distribution | Location | Scale | |
| ∆HRV-pre | |||
| RMSSD | normal | 0 | 9.113 |
| SDNN | normal | 0 | 12.776 |
| Mean R-R | normal | 0 | 128.778 |
| HF | normal | 0 | 343.377 |
| LF | normal | 0 | 266.465 |
| VLF | normal | 0 | 93.548 |
| PNS | normal | 0 | 0.756 |
| SNS | normal | 0 | 2.175 |
| Stress | normal | 0 | 12.178 |
| ∆HRV-post | |||
| RMSSD | normal | 0 | 8.261 |
| SDNN | normal | 0 | 11.298 |
| Mean R-R | normal | 0 | 103.483 |
| HF | normal | 0 | 420.373 |
| LF | normal | 0 | 303.097 |
| VLF | normal | 0 | 81.326 |
| PNS | normal | 0 | 0.645 |
| SNS | normal | 0 | 1.964 |
| Stress | normal | 0 | 12.629 |
References
- Raffin, J.; Barthélémy, J.-C.; Dupré, C.; Pichot, V.; Berger, M.; Féasson, L.; Busso, T.; Da Costa, A.; Colvez, A.; Montuy-Coquard, C.; et al. Exercise Frequency Determines Heart Rate Variability Gains in Older People: A Meta-Analysis and Meta-Regression. Sports Med. 2019, 49, 719–729. [Google Scholar] [CrossRef] [PubMed]
- Manser, P.; Thalmann, M.; Adcock, M.; Knols, R.H.; de Bruin, E.D. Can Reactivity of Heart Rate Variability Be a Potential Biomarker and Monitoring Tool to Promote Healthy Aging? A Systematic Review with Meta-Analyses. Front. Physiol. 2021, 12, 686129. [Google Scholar] [CrossRef] [PubMed]
- Laborde, S.; Mosley, E.; Thayer, J.F. Heart Rate Variability and Cardiac Vagal Tone in Psychophysiological Research–Recommendations for Experiment Planning, Data Analysis, and Data Reporting. Front. Psychol. 2017, 8, 213. [Google Scholar] [CrossRef] [PubMed]
- Task Force of the European Society of Cardiology. Heart Rate Variability: Standards of Measurement, Physiological Interpretation and Clinical Use. Circulation 1996, 93, 1043–1065. [Google Scholar] [CrossRef]
- Souza, H.C.D.; Philbois, S.V.; Veiga, A.C.; Aguilar, B.A. Heart Rate Variability and Cardiovascular Fitness: What We Know so Far. Vasc. Health Risk Manag. 2021, 17, 701. [Google Scholar] [CrossRef]
- Figueiredo, T.d.G.; de Souza, H.C.M.; Neves, V.R.; do Rêgo Barros, A.E.V.; Dornelas de Andrade, A.d.F.; Brandão, D.C. Effects of Physical Exercise on the Autonomic Nervous System in Patients with Coronary Artery Disease: A Systematic Review. Expert Rev. Cardiovasc. Ther. 2020, 18, 749–759. [Google Scholar] [CrossRef]
- Ikura, H.; Katsumata, Y.; Seki, Y.; Ryuzaki, T.; Shiraishi, Y.; Miura, K.; Sato, K.; Fukuda, K. Real-Time Analysis of Heart Rate Variability during Aerobic Exercise in Patients with Cardiovascular Disease. Int. J. Cardiol. Heart Vasc. 2022, 43, 101147. [Google Scholar] [CrossRef]
- Batouli-Santos, D.; Reis-Silva, A.; Guimarães-Lourenço, G.; Mendonça-Guimarães, R.; Moreira-Marconi, E.; Sonza, S.; Bernardo-Filho, M.; Sá-Caputo, D.C. Acute Effect of Whole Body-Vibration Exercise and Osteopathic Manipulative Treatment on the Heart Rate Variability in Individuals with Metabolic Syndrome: Randomized Cross-Study Protocol. Int. J. Osteopath. Med. 2022, 45, 41–47. [Google Scholar] [CrossRef]
- Casanova-Lizón, A.; Manresa-Rocamora, A.; Flatt, A.A.; Sarabia, J.M.; Moya-Ramón, M. Does Exercise Training Improve Cardiac-Parasympathetic Nervous System Activity in Sedentary People? A Systematic Review with Meta-Analysis. Int. J. Environ. Res. Public Health 2022, 19, 13899. [Google Scholar] [CrossRef]
- Schaffarczyk, M.; Rogers, B.; Reer, R.; Gronwald, T. Validation of a Non-Linear Index of Heart Rate Variability to Determine Aerobic and Anaerobic Thresholds during Incremental Cycling Exercise in Women. Eur. J. Appl. Physiol. 2022, 123, 299–309. [Google Scholar] [CrossRef]
- Thoma, S.F.; Pérez-Riera, A.R.; Silva, E.A.C.; Costa, E.L.C.O.; Ferreira, A.N.; Belfort, E.E.T.; Leite, J.C.; Zangirolami-Raimundo, J.; Raimundo, R.D. Evaluation of Autonomic Cardiac Modulation and Body Composition in Elderly Submitted to the Protocol of Exercise and the Gametherapy: A Clinical Trial Protocol (SPIRIT Compliant). Medicine 2022, 101, e31236. [Google Scholar] [CrossRef]
- Lin, L.L.; Chen, Y.J.; Lin, T.Y.; Weng, T.C. Effects of Resistance Training Intensity on Heart Rate Variability at Rest and in Response to Orthostasis in Middle-Aged and Older Adults. Int. J. Environ. Res. Public Health 2022, 19, 10579. [Google Scholar] [CrossRef] [PubMed]
- Marôco, J.L.; Pinto, M.; Laranjo, S.; Santa-Clara, H.; Fernhall, B.; Melo, X. Cardiovagal Modulation in Young and Older Male Adults Following Acute Aerobic Exercise. Int. J. Sports Med. 2022, 43, 931–940. [Google Scholar] [CrossRef] [PubMed]
- D’Agosto, T.; Peçanha, T.; Bartels, R.; Moreira, D.; Silva, L.; Nóbrega, A.; Lima, J. Cardiac Autonomic Responses at Onset of Exercise: Effects of Aerobic Fitness. Int. J. Sports Med. 2014, 35, 879–885. [Google Scholar] [CrossRef] [PubMed]
- Silvestrini, N. Psychological and Neural Mechanisms Associated with Effort-Related Cardiovascular Reactivity and Cognitive Control: An Integrative Approach. Int. J. Psychophysiol. 2017, 119, 11–18. [Google Scholar] [CrossRef]
- Castillo-Aguilar, M.; Valdés-Badilla, P.; Herrera-Valenzuela, T.; Guzmán-Muñoz, E.; Delgado-Floody, P.; Andrade, D.C.; Moraes, M.M.; Arantes, R.M.E.; Núñez-Espinosa, C. Cardiac Autonomic Modulation in Response to Muscle Fatigue and Sex Differences During Consecutive Competition Periods in Young Swimmers: A Longitudinal Study. Front. Physiol. 2021, 12, 1989. [Google Scholar] [CrossRef]
- Porges, S.W. The Polyvagal Perspective. Biol. Psychol. 2007, 74, 116–143. [Google Scholar] [CrossRef]
- Thayer, J.F.; Hansen, A.L.; Saus-Rose, E.; Johnsen, B.H. Heart Rate Variability, Prefrontal Neural Function, and Cognitive Performance: The Neurovisceral Integration Perspective on Self-Regulation, Adaptation, and Health. Ann. Behav. Med. 2009, 37, 141–153. [Google Scholar] [CrossRef]
- McCraty, R.; Shaffer, F. Heart Rate Variability: New Perspectives on Physiological Mechanisms, Assessment of Self-Regulatory Capacity, and Health Risk. Glob. Adv. Health Med. 2015, 4, 46–61. [Google Scholar] [CrossRef]
- Niu, Z.; Liu, F.; Li, B.; Li, N.; Yu, H.; Wang, Y.; Tang, H.; Chen, X.; Lu, Y.; Cheng, Z.; et al. Acute Effect of Ambient Fine Particulate Matter on Heart Rate Variability: An Updated Systematic Review and Meta-Analysis of Panel Studies. Environ. Health Prev. Med. 2020, 25, 77. [Google Scholar] [CrossRef]
- Sessa, F.; Anna, V.; Messina, G.; Cibelli, G.; Monda, V.; Marsala, G.; Ruberto, M.; Biondi, A.; Cascio, O.; Bertozzi, G.; et al. Heart Rate Variability as Predictive Factor for Sudden Cardiac Death. Aging 2018, 10, 166. [Google Scholar] [CrossRef] [PubMed]
- Seals, D.R.; Monahan, K.D.; Bell, C.; Tanaka, H.; Jones, P.P. The Aging Cardiovascular System: Changes in Autonomic Function at Rest and in Response to Exercise. Int. J. Sport Nutr. Exerc. Metab. 2001, 11, S189–S195. [Google Scholar] [CrossRef] [PubMed]
- Álvarez-Millán, L.; Lerma, C.; Castillo-Castillo, D.; Quispe-Siccha, R.M.; Pérez-Pacheco, A.; Rivera-Sánchez, J.; Fossion, R. Chronotropic Response and Heart Rate Variability Before and After a 160 m Walking Test in Young, Middle-Aged, Frail, and Non-Frail Older Adults. Int. J. Environ. Res. Public Health 2022, 19, 8413. [Google Scholar] [CrossRef] [PubMed]
- Katayama, P.L.; Dias, D.P.M.; Silva, L.E.V.; Virtuoso-Junior, J.S.; Marocolo, M. Cardiac Autonomic Modulation in Non-Frail, Pre-Frail and Frail Elderly Women: A Pilot Study. Aging Clin. Exp. Res. 2015, 27, 621–629. [Google Scholar] [CrossRef] [PubMed]
- Toosizadeh, N.; Ehsani, H.; Parthasarathy, S.; Carpenter, B.; Ruberto, K.; Mohler, J.; Parvaneh, S. Frailty and Heart Response to Physical Activity. Arch. Gerontol. Geriatr. 2021, 93, 104323. [Google Scholar] [CrossRef]
- Yu, X.; Antink, C.H.; Leonhardt, S.; Bollheimer, L.C.; Laurentius, T. Non-Contact Measurement of Heart Rate Variability in Frail Geriatric Patients: Response to Early Geriatric Rehabilitation and Comparison with Healthy Old Community-Dwelling Individuals–a Pilot Study. Gerontology 2022, 68, 707–719. [Google Scholar] [CrossRef]
- Michael, S.; Jay, O.; Halaki, M.; Graham, K.; Davis, G.M. Submaximal Exercise Intensity Modulates Acute Post-Exercise Heart Rate Variability. European J. Appl. Physiol. 2016, 116, 697–706. [Google Scholar] [CrossRef]
- Rikli, R.E.; Jones, C.J. Senior Fitness Test Manual; Human Kinetics: Champaign, IL, USA, 2013. [Google Scholar]
- Gifford, R.M.; Boos, C.J.; Reynolds, R.M.; Woods, D.R. Recovery Time and Heart Rate Variability Following Extreme Endurance Exercise in Healthy Women. Physiol. Rep. 2018, 6, e13905. [Google Scholar] [CrossRef]
- Mialich, M.; Martinez, E.Z.; Jordão, A., Jr. Comparative Study of Instruments for the Analysis of Body Composition in a Sample of the Brazilian Population. Int. J. Body Compos. Res. 2011, 9, 19–24. [Google Scholar]
- Calderón, T.M.L.; Rodriguez-Hernandez, M. Efecto de Un Programa de 18 Semanas de Actividad física Sobre La Capacidad Aeróbica, La Fuerza y La Composición Corporal En Personas Adultas Mayores. Pensam. Actual 2018, 18, 125–135. [Google Scholar]
- Malik, M. Heart Rate Variability: Standards of Measurement, Physiological Interpretation, and Clinical Use: Task Force of the European Society of Cardiology and the North American Society for Pacing and Electrophysiology. Ann. Noninvasive Electrocardiol. 1996, 1, 151–181. [Google Scholar] [CrossRef]
- Buchheit, M.; Chivot, A.; Parouty, J.; Mercier, D.; Al Haddad, H.; Laursen, P.; Ahmaidi, S. Monitoring Endurance Running Performance Using Cardiac Parasympathetic Function. Eur. J. Appl. Physiol. 2010, 108, 1153–1167. [Google Scholar] [CrossRef] [PubMed]
- Berntson, G.G.; Thomas Bigger, J., Jr.; Eckberg, D.L.; Grossman, P.; Kaufmann, P.G.; Malik, M.; Nagaraja, H.N.; Porges, S.W.; Saul, J.P.; Stone, P.H.; et al. Heart Rate Variability: Origins, Methods, and Interpretive Caveats. Psychophysiology 1997, 34, 623–648. [Google Scholar] [CrossRef] [PubMed]
- Buchheit, M.; Gindre, C. Cardiac Parasympathetic Regulation: Respective Associations with Cardiorespiratory Fitness and Training Load. Am. J. Physiol.-Heart Circ. Physiol. 2006, 291, H451–H458. [Google Scholar] [CrossRef]
- Akselrod, S.; Gordon, D.; Ubel, F.A.; Shannon, D.C.; Berger, A.C.; Cohen, R.J. Power Spectrum Analysis of Heart Rate Fluctuation: A Quantitative Probe of Beat-to-Beat Cardiovascular Control. Science 1981, 213, 220–222. [Google Scholar] [CrossRef]
- Goldstein, D.S.; Bentho, O.; Park, M.-Y.; Sharabi, Y. Low-Frequency Power of Heart Rate Variability Is Not a Measure of Cardiac Sympathetic Tone but May Be a Measure of Modulation of Cardiac Autonomic Outflows by Baroreflexes. Exp. Physiol. 2011, 96, 1255–1261. [Google Scholar] [CrossRef]
- Fisher, A.; Groves, D.; Eleuteri, A.; Mesum, P.; Patterson, D.; Taggart, P. Heart Rate Variability at Limiting Stationarity: Evidence of Neuro-Cardiac Control Mechanisms Operating at Ultra-Low Frequencies. Physiol. Meas. 2014, 35, 309. [Google Scholar] [CrossRef]
- Rajendra Acharya, U.; Paul Joseph, K.; Kannathal, N.; Lim, C.M.; Suri, J.S. Heart Rate Variability: A Review. Med. Biol. Eng. Comput. 2006, 44, 1031–1051. [Google Scholar] [CrossRef]
- Yoo, H.H.; Yune, S.J.; Im, S.J.; Kam, B.S.; Lee, S.Y. Heart Rate Variability-Measured Stress and Academic Achievement in Medical Students. Med. Princ. Pract. 2021, 30, 193–200. [Google Scholar] [CrossRef]
- Baevsky, R.; Berseneva, A. Methodical Recommendations Use Kardivar System for Determination of the Stress Level and Estimation of the Body Adaptability Standards of Measurements and Physiological Interpretation. 2008. Available online: https://www.academia.edu/35296847/Methodical_recommendations_USE_KARDiVAR_SYSTEM_FOR_DETERMINATION_OF_THE_STRESS_LEVEL_AND_ESTIMATION_OF_THE_BODY_ADAPTABILITY_Standards_of_measurements_and_physiological_interpretation_Moscow_Prague_2008 (accessed on 20 October 2022).
- Rikli, R.E.; Jones, C.J. Functional Fitness Normative Scores for Community-Residing Older Adults, Ages 60–94. J. Aging Phys. Act. 1999, 7, 162–181. [Google Scholar] [CrossRef]
- Feng, D. agRee: Various Methods for Measuring Agreement. 2020. Available online: https://CRAN.R-project.org/package=agRee (accessed on 20 October 2022).
- Evans, J.D. Straightforward Statistics for the Behavioral Sciences; Thomson Brooks/Cole Publishing Co.: Belmont, CA, USA, 1996. [Google Scholar]
- Hackenberger, B.K. Bayes or Not Bayes, Is This the Question? Croat. Med. J. 2019, 60, 50. [Google Scholar] [CrossRef] [PubMed]
- Ashby, D. Bayesian Statistics in Medicine: A 25 Year Review. Stat. Med. 2006, 25, 3589–3631. [Google Scholar] [CrossRef] [PubMed]
- Makowski, D.; Ben-Shachar, M.S.; Chen, S.A.; Lüdecke, D. Indices of Effect Existence and Significance in the Bayesian Framework. Front. Psychol. 2019, 10, 2767. [Google Scholar] [CrossRef] [PubMed]
- Heck, D.W. A Caveat on the Savage–Dickey Density Ratio: The Case of Computing Bayes Factors for Regression Parameters. Br. J. Math. Stat. Psychol. 2019, 72, 316–333. [Google Scholar] [CrossRef]
- Jeffreys, H. The Theory of Probability; OUP Oxford: Oxford, UK, 1998. [Google Scholar]
- Vehtari, A.; Gelman, A.; Simpson, D.; Carpenter, B.; Bürkner, P.-C. Rank-Normalization, Folding, and Localization: An Improved r for Assessing Convergence of MCMC. arXiv 2019, arXiv:1903.08008. preprint. [Google Scholar] [CrossRef]
- Bürkner, P.-C. Brms: An r Package for Bayesian Multilevel Models Using Stan. J. Stat. Softw. 2017, 80, 1–28. [Google Scholar] [CrossRef]
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2021. [Google Scholar]
- Goodrich, B.; Gabry, J.; Ali, I.; Brilleman, S. Rstanarm: Bayesian Applied Regression Modeling via Stan. 2022. Available online: https://mc-stan.org/rstanarm (accessed on 20 October 2022).
- Makowski, D.; Ben-Shachar, M.S.; Lüdecke, D. bayestestR: Describing Effects and Their Uncertainty, Existence and Significance Within the Bayesian Framework. J. Open Source Softw. 2019, 4, 1541. [Google Scholar] [CrossRef]
- Ben-Shachar, M.S.; Lüdecke, D.; Makowski, D. effectsize: Estimation of Effect Size Indices and Standardized Parameters. J. Open Source Softw. 2020, 5, 2815. [Google Scholar] [CrossRef]
- Pfadt, J.M.; van den Bergh, D.; Goosen, J. Bayesrel: Bayesian Reliability Estimation. 2022. Available online: https://CRAN.R-project.org/package=Bayesrel (accessed on 20 October 2022).
- Kim, H.-G.; Cheon, E.-J.; Bai, D.-S.; Lee, Y.H.; Koo, B.-H. Stress and Heart Rate Variability: A Meta-Analysis and Review of the Literature. Psychiatry Investig. 2018, 15, 235. [Google Scholar] [CrossRef]
- Tiwari, R.; Kumar, R.; Malik, S.; Raj, T.; Kumar, P. Analysis of Heart Rate Variability and Implication of Different Factors on Heart Rate Variability. Curr. Cardiol. Rev. 2021, 17, 74–83. [Google Scholar] [CrossRef]
- Cygankiewicz, I.; Zareba, W. Heart Rate Variability. Handb. Clin. Neurol. 2013, 117, 379–393. [Google Scholar] [PubMed]
- Nicolini, P.; Ciulla, M.M.; Asmundis, C.D.; Magrini, F.; Brugada, P. The Prognostic Value of Heart Rate Variability in the Elderly, Changing the Perspective: From Sympathovagal Balance to Chaos Theory. Pacing Clin. Electrophysiol. 2012, 35, 621–637. [Google Scholar] [CrossRef] [PubMed]
- Lu, W.-C.; Tzeng, N.-S.; Kao, Y.-C.; Yeh, C.-B.; Kuo, T.B.; Chang, C.-C.; Chang, H.-A. Correlation Between Health-Related Quality of Life in the Physical Domain and Heart Rate Variability in Asymptomatic Adults. Health Qual. Life Outcomes 2016, 14, 149. [Google Scholar] [CrossRef] [PubMed]
- Colcombe, S.; Kramer, A.F. Fitness Effects on the Cognitive Function of Older Adults: A Meta-Analytic Study. Psychol. Sci. 2003, 14, 125–130. [Google Scholar] [CrossRef]
- Seals, D.R.; Desouza, C.A.; Donato, A.J.; Tanaka, H. Habitual Exercise and Vascular Aging. J. Appl. Physiol. 2008, 105, 1323–1332. [Google Scholar] [CrossRef]
| Characteristic | Overall, N = 105 1 | Sex | Comparison | ||
|---|---|---|---|---|---|
| Female, N = 82 1 | Male, N = 23 1 | Difference 2 | 95% CI 2,3 | ||
| Age (years) | 70.9 ± 5.9 | 70.3 ± 6.0 | 73.2 ± 5.0 | −0.54 | −1.0, −0.07 |
| Body mass (kg) | 74 ± 14 | 74 ± 15 | 77 ± 10 | −0.24 | −0.71, 0.22 |
| Height (cm) | 155 ± 8 | 153 ± 6 | 164 ± 7 | −1.7 | −2.2, −1.1 |
| Body fat (%) | 38 ± 9 | 41 ± 6 | 25 ± 6 | 2.8 | 2.2, 3.4 |
| Body water (%) | 47 ± 6 | 45 ± 4 | 55 ± 5 | −2.3 | −2.9, −1.8 |
| Bone mass (%) | 2.74 ± 4.17 | 2.70 ± 4.73 | 2.87 ± 0.28 | −0.05 | −0.51, 0.41 |
| Muscle mass (%) | 44 ± 8 | 41 ± 5 | 54 ± 6 | −2.5 | −3.1, −1.9 |
| Measure | Median | CI 95% 1 | pd 3 | ROPE 2 | R-hat 4 | ESS 5 | BF 6 | |||
|---|---|---|---|---|---|---|---|---|---|---|
| CI Low | CI High | Low | High | % Inside | ||||||
| ∆HRV-pre | ||||||||||
| RMSSD | −0.25 | −0.959 | 0.458 | 75.8% | −0.365 | 0.365 | 58% | 1.000 | 83,974 | 0.050 |
| SDNN | 1.52 | 0.529 | 2.506 | 99.8% | −0.511 | 0.511 | 2.3% | 1.000 | 84,522 | 3.617 |
| Mean R-R | −15.47 | −25.602 | −5.593 | 99.8% | −5.151 | 5.151 | 2.1% | 1.000 | 84,462 | 3.838 |
| HF | −7.38 | −36.091 | 21.513 | 69.3% | −13.735 | 13.735 | 59.6% | 1.000 | 83,517 | 0.048 |
| LF | 26.44 | 4.661 | 48.151 | 99.1% | −10.659 | 10.659 | 7.6% | 1.000 | 80,397 | 0.720 |
| VLF | 5.45 | −2.030 | 13.162 | 92.2% | −3.742 | 3.742 | 31.9% | 1.000 | 80,128 | 0.112 |
| PNS | −0.11 | −0.174 | −0.055 | 100% | −0.030 | 0.030 | 0.3% | 1.000 | 84,078 | 32.902 |
| SNS | −0.10 | −0.268 | 0.071 | 88% | −0.087 | 0.087 | 42.1% | 1.000 | 82,412 | 0.079 |
| Stress | −1.40 | −2.336 | −0.430 | 99.8% | −0.487 | 0.487 | 3.1% | 1.000 | 82,470 | 2.526 |
| ∆HRV-post | ||||||||||
| RMSSD | −0.03 | −0.679 | 0.605 | 53.3% | −0.330 | 0.330 | 68.5% | 1.000 | 85,628 | 0.040 |
| SDNN | 0.48 | −0.403 | 1.382 | 85.5% | −0.452 | 0.452 | 45.5% | 1.000 | 84,183 | 0.070 |
| Mean R-R | 0.41 | −7.730 | 8.686 | 53.9% | −4.139 | 4.139 | 67.5% | 1.000 | 85,178 | 0.040 |
| HF | −2.62 | −36.558 | 30.969 | 56.2% | −16.815 | 16.815 | 66.8% | 1.000 | 83,878 | 0.041 |
| LF | 13.92 | −10.604 | 37.828 | 87% | −12.124 | 12.124 | 42.5% | 1.000 | 81,263 | 0.077 |
| VLF | 3.46 | −3.116 | 10.053 | 85.1% | −3.253 | 3.253 | 45.4% | 1.000 | 85,824 | 0.070 |
| PNS | −0.01 | −0.062 | 0.041 | 65.1% | −0.026 | 0.026 | 64.3% | 1.000 | 82,840 | 0.044 |
| SNS | −0.09 | −0.244 | 0.069 | 86.1% | −0.079 | 0.079 | 44.4% | 1.000 | 80,284 | 0.072 |
| Stress | −0.84 | −1.871 | 0.128 | 95.1% | −0.505 | 0.505 | 24.9% | 1.000 | 81,326 | 0.158 |
| Parameter | CCC 2 | Interpretation 3 | CI 95% 1 | |
|---|---|---|---|---|
| Low | High | |||
| ∆HRV-pre | ||||
| RMSSD | 0.722 | Strong | 0.624 | 0.808 |
| SDNN | 0.651 | Strong | 0.534 | 0.751 |
| Mean RR | 0.866 | Very Strong | 0.817 | 0.911 |
| HF | 0.449 | Moderate | 0.285 | 0.601 |
| LF | 0.376 | Weak | 0.201 | 0.540 |
| VLF | 0.335 | Weak | 0.159 | 0.502 |
| SNS | 0.839 | Very Strong | 0.778 | 0.893 |
| PNS | 0.769 | Strong | 0.687 | 0.840 |
| Stress | 0.716 | Strong | 0.614 | 0.800 |
| ∆HRV-post | ||||
| RMSSD | 0.755 | Strong | 0.666 | 0.832 |
| SDNN | 0.712 | Strong | 0.608 | 0.801 |
| Mean RR | 0.824 | Very Strong | 0.758 | 0.881 |
| HF | 0.703 | Strong | 0.599 | 0.794 |
| LF | 0.656 | Strong | 0.538 | 0.761 |
| VLF | 0.361 | Weak | 0.199 | 0.520 |
| SNS | 0.780 | Strong | 0.698 | 0.849 |
| PNS | 0.755 | Strong | 0.669 | 0.832 |
| Stress | 0.726 | Strong | 0.628 | 0.811 |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Castillo-Aguilar, M.; Mabe Castro, M.; Mabe Castro, D.; Valdés-Badilla, P.; Herrera-Valenzuela, T.; Guzmán-Muñoz, E.; Lang, M.; Niño Méndez, O.; Núñez-Espinosa, C. Validity and Reliability of Short-Term Heart Rate Variability Parameters in Older People in Response to Physical Exercise. Int. J. Environ. Res. Public Health 2023, 20, 4456. https://doi.org/10.3390/ijerph20054456
Castillo-Aguilar M, Mabe Castro M, Mabe Castro D, Valdés-Badilla P, Herrera-Valenzuela T, Guzmán-Muñoz E, Lang M, Niño Méndez O, Núñez-Espinosa C. Validity and Reliability of Short-Term Heart Rate Variability Parameters in Older People in Response to Physical Exercise. International Journal of Environmental Research and Public Health. 2023; 20(5):4456. https://doi.org/10.3390/ijerph20054456
Chicago/Turabian StyleCastillo-Aguilar, Matías, Matías Mabe Castro, Diego Mabe Castro, Pablo Valdés-Badilla, Tomás Herrera-Valenzuela, Eduardo Guzmán-Muñoz, Morin Lang, Oscar Niño Méndez, and Cristian Núñez-Espinosa. 2023. "Validity and Reliability of Short-Term Heart Rate Variability Parameters in Older People in Response to Physical Exercise" International Journal of Environmental Research and Public Health 20, no. 5: 4456. https://doi.org/10.3390/ijerph20054456
APA StyleCastillo-Aguilar, M., Mabe Castro, M., Mabe Castro, D., Valdés-Badilla, P., Herrera-Valenzuela, T., Guzmán-Muñoz, E., Lang, M., Niño Méndez, O., & Núñez-Espinosa, C. (2023). Validity and Reliability of Short-Term Heart Rate Variability Parameters in Older People in Response to Physical Exercise. International Journal of Environmental Research and Public Health, 20(5), 4456. https://doi.org/10.3390/ijerph20054456












