Abstract
Mindfulness-, compassion-, and acceptance-based (i.e., “third wave”) psychotherapies are effective for treating chronic pain conditions. Many of these programs require that patients engage in the systematic home practice of meditation experiences so they can develop meditation skills. This systematic review aimed at evaluating the frequency, duration, and effects of home practice in patients with chronic pain undergoing a “third wave” psychotherapy. A comprehensive database search for quantitative studies was conducted in PubMed, Embase, and Web of Sciences Core Collection; 31 studies fulfilled the inclusion criteria. The reviewed studies tended to indicate a pattern of moderately frequent practice (around four days/week), with very high variability in terms of time invested; most studies observed significant associations between the amount of practice and positive health outcomes. Mindfulness-Based Stress Reduction and Mindfulness-Based Cognitive Therapy were the most common interventions and presented low levels of adherence to home practice (39.6% of the recommended time). Some studies were conducted on samples of adolescents, who practiced very few minutes, and a few tested eHealth interventions with heterogeneous adherence levels. In conclusion, some adaptations may be required so that patients with chronic pain can engage more easily and, thus, effectively in home meditation practices.
1. Introduction
The International Association for the Study of Pain (IASP) defines chronic pain as pain that lasts or recurs for longer than three months, regardless of if it is experienced in one or more than one anatomical regions [1]. In some cases, chronic pain is linked to other diseases as the underlying cause (i.e., secondary chronic pain, as in cancer, post-surgical, posttraumatic, and neuropathic pain, among others), while in other cases, it is a disease of its own (i.e., primarily chronic pain: fibromyalgia, migraines, irritable bowel syndrome, and low back pain, among others) [2,3]. Chronic pain conditions very often have a significant negative impact on the individual’s functionality, and a notable majority of these patients present with anxiety and depression; all in all, chronic pain is a leading source of human suffering and disability [4].
Different therapeutic approaches are used for treating chronic pain conditions: pharmacotherapies (e.g., analgesics, tricyclic antidepressants, and opioids, among others) have resulted in mixed results for safety and effectiveness for managing chronic pain [5,6,7,8,9]. For some chronic pain conditions, different evidence-based guidelines do not agree on first-line recommendations of only pharmacotherapy, and some even give a higher ranking to cognitive-behavioral therapy (CBT) and multi-component treatments (i.e., interventions that include different strategies, such as psychoeducation, relaxation, physical exercise, etc.) [10,11]. Classic CBT for chronic pain has focused on changing negative thoughts and maladaptive behaviors about pain to improve function and coping [12]; although it has proved to be effective, the impact of CBT on chronic pain conditions has generally been small [13].
In the last decades, different programs based on CBT have been developed, although in this case, they are focused on promoting mindfulness, i.e., nonjudgmental, present-focused attention, and other related constructs, such as compassion and acceptance. These interventions are not primarily focused on symptom relief but, instead, on the promotion of well-being. This is accomplished through the cultivation of psychological flexibility (i.e., a wide range of abilities, such as recognizing and adapting to situational demands, shifting mindsets or behavioral repertoires when these strategies compromise personal or social functioning, maintaining a balance between life domains, and being aware, open, and committed to behaviors that are congruent with deeply held values) [14,15]. Meditation practices play a central role in these programs since they train the patient to interact with their thoughts and feelings in a more detached manner.
Such interventions have been categorized under the term “third wave” CBT psychotherapies; Mindfulness-Based Stress Reduction (MBSR) [16], Mindfulness-Based Cognitive Therapy (MBCT) [17], and Acceptance and Commitment Therapy (ACT) [18] are some examples. Previous studies have concluded that these interventions’ effects on reducing pain interference are achieved through enhancing pain acceptance and psychological flexibility [19], as well as reducing fear of pain, pain-related anxiety, and fear-avoidance beliefs [20]. These changes play a significant role in improving functional impairment, anxiety, depression, and psychological distress in chronic pain conditions [21,22,23,24,25]. Some studies report higher effects of “third wave” psychotherapies than multicomponent interventions [26], although the superiority of these interventions compared to classic CBT is still unclear [27].
In “third wave” psychotherapies, mindfulness is cultivated through meditations that are first experienced by the patient in live group-based sessions and intended to be practiced at home alone between sessions and beyond. Structured programs, such as MBSR or MBCT, which consist of a weekly 2–2.5 h session during 8 consecutive weeks, ask participants to engage in “formal” practices (i.e., guided meditations, such as body scan, Awareness of Breath meditation, and mindful movement with suggestions to posture, attitude, and how attention is directed) 6 days a week at home, investing around 45 min per practice [16,17], in addition to the normally brief and unstructured “informal” practices (i.e., applying mindfulness to everyday activities such as mindful eating or showering). Home practices are reviewed and discussed in the next session with the instructor. These autonomous home practices are assumed to be critical to therapeutic change: the meta-analysis conducted by Parsons et al. [28] observed a significant association between the extent of formal mindfulness practice and positive intervention outcomes for a wide range of conditions, such as depression, anxiety, or insomnia. However, despite the importance of home practice, there is great heterogeneity in the instructions and resources provided to the participants and the methodology used to monitor home practice, as well as in the recommended duration of the practices, in the scientific studies [29].
The present systematic review focuses on chronic pain conditions. These chronic conditions require an ongoing need for self-management skills, such as mindfulness, to have a long-term impact on the physiology of the brain and overall health, which requires systematic and frequent home practice. Parsons et al. [28] observed that across 43 studies (N = 1427), the pooled estimate for participants’ home practice was 64% of the assigned amount, equating to about 30 min per day, six days per week [95% CI 60–69%]. The amount of home practice could be substantially different when considering patients with chronic pain for various reasons, such as physical discomfort (e.g., people with fibromyalgia may have difficulties with long durations of standing or sitting, which is often required in formal meditations) or cognitive impairment that is often associated with some chronic pain syndromes [30,31]. These could represent potential barriers to engaging in home practices, which might hinder the intervention’s effectiveness. Thus, the present work will systematically review quantitative studies conducted on samples of patients with chronic pain conditions who underwent a “third wave” psychotherapy to determine the frequency and duration of home practice of mindfulness and/or other related skills. When reported, the impact of such practice on main symptoms will be discussed, and certain variables (e.g., type of chronic pain, type of intervention, age group) will be granted special attention.
2. Materials and Methods
2.1. Design
A systematic review of quantitative studies, including randomized controlled trials (RCTs), non-RCTs, open trials with pre-post analysis, and pilot studies, was conducted. This systematic review was registered in the PROSPERO database (Registration number: CRD42022351572) and was implemented in accordance with the standards of Preferred Reporting Items for Systematic Reviews and Meta-analysis (PRISMA) guidelines [32] (checklist can be found in Supplementary Materials).
2.2. Data Sources and Search Strategy
A search strategy using PubMed, Embase, and Web of Sciences Core Collection databases was performed between September and October 2022. Only studies published in English were included, and no restrictions regarding publication dates were considered. Specific search terms (e.g., MeSH terms) were combined and adapted to each database and are detailed in the Supplementary Materials.
Also, relevant studies were sought from reference lists of included studies. The titles and abstracts of all potentially eligible studies identified from the search were reviewed against the inclusion and exclusion criteria by three reviewers. The full texts of all potential studies were then independently screened by three reviewers, and disagreements were resolved through discussion with a fourth reviewer.
2.3. Elegibility Criteria
The following inclusion and exclusion criteria were guided by the evidence-based medicine PICOS framework or strategy [33]:
- Participants: Patients who suffer from chronic pain conditions, both primary (e.g., fibromyalgia, irritable bowel syndrome, migraines, etc.) and secondary chronic pain (e.g., post-surgical pain, rheumatoid arthritis, chronic pain associated with a medical condition, etc.);
- Interventions and comparisons: The interventions included in this review were those constituted under the epigraph of “third wave” CBT (based on the practice of mindfulness, compassion, acceptance, etc.) and which prescribe the continued practice of the exercises at home by the participants. Interventions could be individual or group-based and could be conducted either in person or online. Blended interventions (i.e., a combination of online and in-person sessions) were also included. The duration of the intervention could vary. There were no inclusion/exclusion criteria regarding comparators/controls;
- Outcomes: Home practice frequency (i.e., number of days) and amount of practice (i.e., minutes per day) were the main outcomes of the systematic review. When reported, the relationship between practice and the study variables (e.g., pain, functionality, depression, anxiety, etc.) was also presented as an outcome. Information on home practice time had to cover the duration of the course and/or a post-intervention follow-up time. When detailed, practice time was reported for both so-called formal and informal practices. Barriers to or facilitators of maintaining the habit of practicing at home were included as secondary outcomes.
- Study design: We included randomized controlled trials (RCTs), non-RCTs, and open trials with pre-post analysis. Pilot studies were also included as long as they followed one of the previous study designs. Studies published in peer-reviewed journals as well as pre-print papers, were included. On the other hand, cross-sectional studies, qualitative studies, study protocols, reviews, clinical cases, conference proceedings, letters, commentaries, and case studies were excluded.
2.4. Search Outcomes
Initially, 9102 articles were retrieved from the databases PubMed, Embase, and Web of Sciences Core Collection; in addition, one article was identified from the citation search. Once duplicates were removed, a total of 5297 articles were identified and screened by three reviewers (A.B.-S., S.F.-M., and A.P.-A.); the full-text manuscripts for 157 studies were then sought for retrieval and assessed, of which 31 met the inclusion criteria (Figure 1).
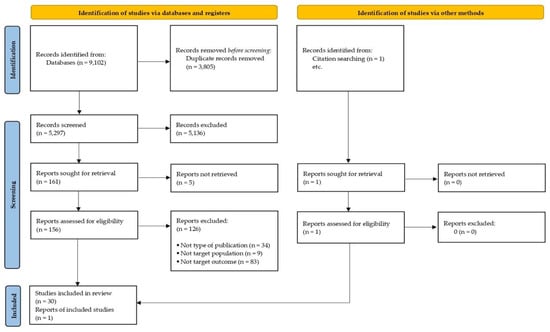
Figure 1.
PRISMA diagram of study flow.
2.5. Quality Appraisal
To assess the quality of the studies, we used the assessment tool developed by National Heart, Lung, and Blood Institute, one for controlled intervention studies and one for single-arm studies. This allowed the included studies, both controlled intervention studies, and single-arm studies, to be evaluated for risk of bias.
Two reviewers (A.M.-B. and A.B.-S.) conducted such a quality assessment of the included studies, and disagreements were resolved through discussion between the researchers and in consultation with a third author (A.P.-A.). The quality assessment is provided in the Supplementary Materials (Tables S1 and S2) along with a link to the assessment tools and their items.
2.6. Data Abstraction
Selection and coding were performed independently by three authors (A.B.-S., S.F.-M., and A.P.-A.). All detected articles were screened according to the established inclusion criteria; then, abstracts and titles were reviewed to identify those relevant to the research question. When too little information was available to determine eligibility, full articles were reviewed. Relevant articles were subsequently selected by cross-examination of articles. Disagreements between authors were resolved by consensus, and when in doubt, the final decision was made in consultation with a fourth author (H.M.-S.). A data extraction form was developed based on Centre for Reviews and Dissemination templates. Data collected included information on authors, date of publication, country of study, study design, sample characteristics (e.g., sample size, chronic pain condition, age), intervention type (i.e., MBSR, MBCT, ACT, etc.) and its duration, intervention format (e.g., face-to-face, online, blended), home practice details (frequency in days and time in minutes), and primary and secondary outcomes measured.
3. Results
3.1. Summary of the Findings
Table 1 provides a summary of the 31 studies included in this systematic review. The years of publication of the studies ranged between 2007 and 2022. Of the included studies, eight (26%) were conducted in Europe (United Kingdom, Spain, Denmark, and The Netherlands), twenty (65%) in America (United States of America and Canada), two (6%) in Oceania (Australia), and one (3%) in Asia (Hong Kong). Regarding the study design, twenty-four (78%) were RCTs, two (6%) non-RCTs, four (13%) were single-arm studies, and one (3%) was a secondary analysis of a previous RCT. With respect to the type of demographics included in the studies, four (13%) were carried out with a population that was 18 years old or younger, and twenty-seven (87%) with an adult population. Additionally, in four (13%) studies, the sample was made up only of the female population; in twenty-three (74%), it was made up of both men and women, and in four (13%), this information was not reported.
The most prevalent types of chronic pain conditions included fibromyalgia, irritable bowel syndrome, chronic low back pain, migraine, and medical conditions with chronic pain as a symptom (i.e., secondary chronic pain) (Table 1). Among the interventions studied, fourteen studies used standardized MBSR or MBCT programs. The other interventions combined mindfulness with other elements, such as acceptance, CBT techniques, and yoga exercises, among others. Despite the heterogeneity between the interventions, twenty-seven (88%) studies tested interventions with a duration of eight weeks. The duration of the remaining interventions ranged between 3 and 12 weeks.
An aspect of interest in this type of study is the way in which home practices are assigned. On the one hand, studies that used the Internet as a resource to facilitate audio or video with guided practices stand out, such as through YouTube [34], email [35], web pages developed specifically for the study [36,37], and download platforms [38]. On the other hand, some studies used physical books, CDs, and DVDs, and in which the practices that the participants had to carry out at home were compiled [26,39,40,41,42,43,44,45,46,47]. However, despite the relevance of this aspect, some studies did not specify how the participants received the instructions and resources to practice between sessions [48,49,50,51,52,53,54,55,56,57,58].
The way in which the frequency of home practice was recorded varies between the included studies. Only one study used both daily (during the intervention) and weekly (during follow-up) recordings of the home practice [41]. Fourteen studies used daily logs, of which two studies specified doing so online [35,52]; another two studies used pen and paper [55,59]; one study used both depending on the resources of the participants [42]; the others did not specify how they collected information [26,34,43,44,49,53,56,60,61]. Three studies used the weekly logs as a strategy to collect practice time at home [39,40,48]. On the other hand, some studies used other strategies to collect home practice but without specifying the timing. One study collected the information through a qualitative interview once the intervention had finished [62]; two studies created an ad hoc item for home practice time that was included as part of a post-intervention questionnaire [37,54]; one study used a logbook created specifically for the study but without specifying its characteristics [57]; and another study obtained the information from the number of logs turned in [50]. Finally, eight studies did not specify any information regarding the methodology used to collect the information [36,38,45,46,47,51,58,63].

Table 1.
Description of the studies reviewed.
Table 1.
Description of the studies reviewed.
| Authors (Year) | Design | Sample | Chronic Pain Condition | Intervention (Duration) |
|---|---|---|---|---|
| Ali et al. (2017) [62] | Single-arm study (3 cohorts) | N = 18 (11 females) Age: 14.80 (range: 10–18) | Functional somatic syndromes | MBSR (8 weeks) |
| Carson et al. (2010) [42] | RCT (2 arms: Yoga of Awareness Program vs. wait-list control) | NYoga-Awareness = 25 (all females) Age: 51.40 (SD = 13.17) | Fibromyalgia | Yoga of Awareness program (8 weeks) |
| Cebolla et al. (2021) [37] | Non-randomized controlled trial (2 arms: MBI vs. standard medical therapy) | NMBI = 45 (43 females) Age: 45.41 (SD = 10.46) | Inflammatory Bowel Disease | Blended MBI (8 weeks) |
| Chadi et al. (2016) [57] | RCT (2 arms: MBI vs. wait-list control) | NMBI = 19 (all females) Age: 15.80 (SD = 1.10) | Chronic pain as a result of a medical condition | Adapted MBI (8 weeks) |
| Chadi et al. (2018) [54] | RCT (2 arms: online MARS-A vs. in person MARS-A) | N = 18 (14 females) Age: 15.30 (range 13–18) | Medical condition that implies chronic pain or headaches | MARS-A Program (8 weeks) |
| Cooperman et al. (2021) [49] | RCT (2 arms: MORE vs. TAU) | NMORE = 15 (8 females) Age: 47.90 (SD = 8.70) | Patients with opioid use disorder and primary chronic pain | MORE (8 weeks) |
| Day et al. (2014) [58] | RCT (2 arms: MBCT vs. TAU) | NMBCT = 19 (17 females) Age: 43.10 (SD = 11.20) | Primary headache pain (and other comorbid chronic pain conditions) | MBCT (8 weeks) |
| Day et al. (2016) [52] | Secondary analysis of Day et al. (2014) | N = 21 (20 females) Age: 42.80 (SD = 12.50) | Primary headache pain (and other comorbid chronic pain conditions) | MBCT (8 weeks) |
| Day et al. (2020) [55] | RCT (3 arms: CT vs. MM vs. MBCT) | NMM+MBCT = 56 (sex n.r.) Age: 50.74 (SD = 14.43) | Chronic low back pain | MBCT (8 weeks) |
| Donnino et al. (2021) [48] | RCT (3 arms: MBSR vs. PSRT vs. TAU) | NMBSR = 12 (6 females) Age: 39.30 (SD = 14.40) | Chronic back pain | MBSR (8 weeks) |
| Gardiner et al. (2020) [36] | Single arm study (2 cohorts) | N = 43 (39 females) Age: 50.40 (SD = 12.60) | Chronic pain (as a symptom) | Our Whole Lives for Chronic Pain (9 weeks) |
| Garland et al. (2014) [45] | RCT (2 arms: MORE vs. support group) | NMORE = 57 (sex n.r.) Age: 48 (SD = 14) | Patients with opioid use disorder and chronic pain | MORE (8 weeks) |
| Greenberg et al. (2019) [50] | Non-randomized controlled trial (2 arms: 3RP + GetActive vs. 3RP + GetActive with Fitbit) | N = 13 (10 females) Age: 44 (SD = 14.31) | Different chronic pain conditions | 3RP (8 weeks) |
| Hearn and Finlay (2018) [63] | RCT (2 arms: online MBI vs. online psychoeducation) | NMBI = 36 (19 females) Age: 43.80 (SD = 8.70) | Patients with chronic pain after spinal cord injury | Online MBI (8 weeks) |
| Hesse et al. (2015) [59] | Single arm study | N = 20 (all females) Age: 14.15 (SD = 1.60) | Recurrent headaches | Adapted Mindful School Curriculum for Adolescents (8 weeks) |
| Howarth et al. (2019) [60] | RCT (2 arms: Brief MBI vs. active control) | NMBI = 37 (24 females) Age: 54.70 (SD = 12.50) | Persistent pain (as a symptom) | Brief MBI (4 weeks) |
| Johannsen et al. (2018) [51] | RCT (2 arms: MBCT vs. wait-list control) | NMBCT = 67 (all females) Age: 56.80 (SD = 9.99) | Persistent pain (as a symptom of breast cancer) | MBCT (8 weeks) |
| Mittal et al. (2022) [35] | RCT (2 arms: MBCT vs. TAU) | NMBCT = 22 (15 females) Age: 54.20 (SD = 12.80) | Persistent chest pain (non-cardiac cause) | MBCT (8 weeks) |
| Morone et al. (2008) [43] | RCT (2 arms: MBSR vs. wait-list control) | NMBSR = 19 (10 females) Age: 74.10 (SD = 6.10) | Chronic low-back pain | MBSR (8 weeks) |
| Pérez-Aranda et al. (2019) [26] | RCT (3 arms: MBSR vs. FibroQoL vs. TAU) | NMBSR = 75 (73 females) Age: 52.96 (SD = 7.98) | Fibromyalgia | MBSR (8 weeks) |
| Pradhan et al. (2007) [61] | RCT (2 arms: MBSR vs. TAU) | NMBSR = 31 (26 females) Age: 56 (SD = 9) | Rheumatoid arthritis | MBSR (8 weeks) |
| Rae et al. (2020) [46] | RCT (2 arms: MBI + yoga vs. stretching class) | NMBI = 10 (2 females) Age: 51.70 (SD = 14.90) | Chronic low-back pain | MBI + yoga (8 sessions) |
| Rosenzweig et al. (2010) [44] | Single-arm study | N = 133 (111 females) Age: 52.96 (SD = 7.98) | Different chronic pain conditions (mostly primary chronic pain) | MBSR (8 weeks) |
| Seng et al. (2019) [56] | RCT (2 arms: MBCT vs. TAU/wait-list control) | N = 31 (29 females) Age: 36.20 (SD = 10.60) | Migraine | MBCT (8 weeks) |
| Trompetter et al. (2014) [38] | RCT (3 arms: online ACT vs. online expressing writing vs. wait-list control) | NACT = 82 (63 females) Age: 52.90 (SD = 13.30) | Chronic pain (as a symptom) | Online ACT (9–12 weeks) |
| Van Gordon et al. (2017) [47] | RCT (2 arms: MAT vs. CBT) | NMAT = 74 (61 females) Age: 46.41 (SD = 9.06) | Fibromyalgia | MAT (8 weeks) |
| Wong et al. (2011) [39] | RCT (2 arms: MBSR vs. MPI) | NMBSR = 51 (sex n.r.) Age: 48.70 (SD = 7.84) | Chronic pain (as a symptom) | MBSR (8 weeks) |
| Zanca et al. (2022) [34] | RCT (2 arms: CMI vs. active control) | NCMI = 11 (2 females) Age: 50 (range 37–65) | Patients with chronic pain after spinal cord injury | CMI (4 weeks) |
| Zernicke et al. (2012) [40] | RCT (2 arms: MBSR vs. wait-list control) | NMBSR = 43 (40 females) Age: 45 (SD = 12.40) | Irritable bowel syndrome | MBSR (8 weeks) |
| Zgierska et al. (2016) [41] | RCT (2 arms: MBI vs. TAU) | NMBI = 21 (15 females) Age: 52.70 (SD = 10.50) | Chronic low back pain | MBI (8 weeks) |
| Zgierska et al. (2016) [53] | RCT (2 arms: MM + CBT vs. TAU) | NMM+CBT = 21 (sex n.r.) Age: 51.80 (SD = 9.70) | Patients with opioid-treated chronic low back pain | MM + CBT (8 weeks) |
Abbreviations: CMI = Clinical Meditation and Imagery; CT = Cognitive Therapy; MARS-A = Mindful Awareness and Resilience Skills for Adolescents; MAT = Meditation awareness training; MM = Mindfulness Meditation; MM + CBT = Mindfulness Meditation and Cognitive Behavioral Therapy; MORE = Mindfulness-Oriented Recovery Enhancement; MPI = Multidisciplinary Pain Intervention; PSRT = Psychophysiologic Symptom Relief Therapy; TAU = Treatment As Usual; 3RP = Mind–body Relaxation Response Resiliency Program; n.r. = “not reported”.
3.2. Study Quality
The overall quality of the 31 included studies was rated as fair. Only 10 (32%) included studies (10/27 controlled studies) were rated as good, while 12 (39%) (9/27 controlled studies and 3/4 single-arm studies) were rated as poor. For controlled studies, the risk of bias was mainly due to lack of blinding, the differences between groups at baseline, the high dropout rate at the endpoint (>20%), or the lack of sample size/power calculation. For the single-arm studies, the risk of bias was related to the lack of information on the sample’s representativeness, the non-inclusion of all the participants who met the inclusion/exclusion criteria, no sample size calculation, lack of blindness of people assessing outcomes, and the lack of follow-up measures.
3.3. Frequency of Home Practice
Table 2 displays the information on each reviewed study. Sixteen studies (51.6%) reported the number of days that patients with chronic pain practiced meditation at home during the intervention: on average, participants engaged in home practices for 4.27 days per week (SD = 1.40). In addition, twenty-four studies (77.4%) reported the minutes of practice: 26.78 min per day (SD = 21.10) during the intervention. Only four studies [48,53,56,60] reported the frequency of practice in follow-up assessments (1 to 4 months), finding an average frequency of 3.49 days per week (SD = 1.05) and 32.23 min per day (SD = 16.73).

Table 2.
Frequency of home practice during the intervention.
3.4. Impact of Home Practice on Main Symptoms
Nine studies explored the impact of the amount of practice on health outcomes, and seven of them found significant effects: Ali et al. [62] and Carson et al. [42] found that frequency of practice was significantly associated with improvement in functionality, fatigue, and relaxation. Day et al. [58] found that MBCT completers improved significantly on pain catastrophizing, pain acceptance, and self-efficacy compared to TAU and, similarly, Zgierska et al. [41] observed that “consistent meditators” had a greater decrease in pain ratings when compared with controls. In the same vein, Johannsen et al. [51] found that more work practice during the intervention predicted increases in mindfulness non-reactivity but not in pain catastrophizing (and no effects in the follow-up were observed). Rosenzweig et al. [44] reported a significant impact of the amount of home meditation practices on psychological distress, somatization symptoms, and self-rated general health. Similarly, Van Gordon et al. [47] also found that the number of minutes of meditation was significantly related to functionality, pain, psychological distress, sleep quality, and non-attachment.
On the other hand, two studies did not find any significant impact of the frequency of practice on the study outcomes: Day et al. [55] observed medium, yet not statistically significant, effects on pain interference and pain intensity, and Pradhan et al. [61] found that neither the overall sum of practice time nor the sum of time spent on a specific practice predicted change in any measure by two months, although each one-day increase in practice was associated with improvement in depressive symptoms and in psychological distress.
4. Discussion
Home meditation practice is considered a key part of “third wave” CBT psychotherapies, and it could be particularly relevant in the case of patients who experience chronic conditions, such as chronic pain, since they need to turn the trained skills into habits so these can have a meaningful impact on their health. The present systematic review has observed a moderate frequency of home practice during the interventions (around four days per week), although, in terms of time invested, a very high variability has been detected. Despite the high degree of heterogeneity of the studies included in this review, it seems clear that the amount of home practice has a significant impact on different outcomes related to chronic pain since most studies that explored this effect found significant results [41,42,44,47,51,58,62]. This goes in line with a previous systematic review which observed significant effects of home-practice frequency (MBSR or MBCT programs) on different mental health outcomes [28].
When comparing studies conducted on samples with primary and secondary chronic pain, following the IASP categorization [2], it was observed that, on average, the number of days of practice per week was higher in samples with secondary chronic pain (MSecondary = 5.63, SD = 1.11 vs. MPrimary = 4.16, SD = 1.25), while patients with primary chronic pain conditions invested more minutes per day (MPrimary = 27.37, SD = 13.56 vs. MSecondary = 15.16, SD = 17.69). Although some hypotheses related to the nature of the chronic pain condition and its impact on adherence to meditation exercises could be drawn, it is considered that more studies are needed, not only because of the heterogeneity of samples and interventions but also due to the amount of home practice in primary chronic pain conditions was reported in 18 studies, while only 6 studies were focused on secondary chronic pain, which hinders a precise comparison.
It is worth mentioning that four studies were conducted on samples of adolescents: Ali et al. [62] and Hesse et al. [59] studied a sample of adolescents with primary chronic pain conditions, and Chadi et al. [54,57] tested the effects of an MBI on samples of teenagers with chronic pain as a result of a medical condition. The adherence to home practice in these studies was notable in terms of days per week (ranging from 4 to 6.5 on average), but the amount of time invested each day was generally very low (ranging between 4 and 8 min per day on average). Although the studies reported significant effects of the interventions on treatment outcomes, such as functionality, anxiety, depression, and pain coping, the small sample sizes and some other methodological shortcomings need to be considered when interpreting these results. The review conducted by Lin et al. [64] considered that MBIs could lead to improvement in the overall quality of life for adolescents suffering from chronic pain, but a systematic review [65] concluded that the evidence was inconsistent. Some authors have pointed out that learning mindfulness might require meta-cognitive skills that many adolescents may not have developed yet [66,67], in addition to discipline and consistency regarding meditation practice, which are also uncommon among teenagers. Thus, it is suggested that before implementing “third wave” CBT psychotherapies for adolescents with chronic pain, previous steps addressed at promoting the required basic skills should be taken.
The MBSR and MBCT programs were the most common “third wave” psychotherapies in the reviewed studies (eight and six studies, respectively). In these programs, practicing 6 days a week for approximately 45 min per practice is recommended [16,17]. Four of the reviewed studies using MBCT or MBSR reported both the frequency of practice and the minutes invested per day [26,43,44,58], and none of them reached the recommended adherence; on average, patients practiced 39.6% of the recommended time. This is considerably lower than the result reported in the systematic review conducted by Parsons et al. [28], in which patients with different mental health conditions undergoing MBSR or MBCT practiced around 64% of the recommended time. With due caution, since our finding is based on very few studies—other studies only reported the minutes of practice but not its frequency, it could be hypothesized that patients with chronic pain may present some difficulties in engaging in home meditation practices that should be acknowledged when implementing programs such as MBSR and MBCT: adaptations to posture may be required (e.g., laying down and standing yoga might be too strenuous for patients with pain), as well as shortening the duration of some practices or sessions—as some studies have already tested for other “third wave” psychotherapies [68]—and offering adapted audio guides and other resources to help patients to focus their attention on the exercise when they practice at home. Reducing perceived barriers is key to the individuals engaging in meditation practices in the long term [69], and previous studies conducted on different samples found that “pragmatic barriers” (e.g., being unable to sit for long periods of time, not having enough time or the optimal environment to meditate, difficulty lying on the floor) are common concerns among people with chronic pain who start practicing [70,71], which suggests that the abovementioned adaptations could be useful for other populations besides chronic pain patients.
Among the interventions tested in the reviewed studies, three of them [38,54,63] were eHealth programs, i.e., health services delivered or enhanced through the Internet and related technologies (e.g., telehealth, mobile apps, etc.) [72,73,74]. These studies reported frequent home practice but of short duration: Chadi et al. [54] reported that patients using the eHealth intervention practiced around 6 days per week only for a total of 30 min per week (i.e., an average of 5 min per day), although this was equivalent to the amount of practice reported by the group who received the MBI in face-to-face sessions; Hearn and Finlay [63] observed that most patients (72.2%) adhered to the autonomous practices in their MBI (i.e., 10 min, 6 days a week); and Trompetter et al. [38] reported that the majority of the participants practiced 3 days per week, around 15–20 min per day.
While eHealth may offer patients with chronic pain a number of advantages (e.g., geographic adaptability, schedule flexibility, easy accessibility), some studies using eHealth programs, particularly those without any guidance, highlight the difficulties in achieving adequate adherence rates [75]. Learning how to meditate, as with any other skill, requires at first some guidance on how to perform the practice; moreover, difficulties and doubts are often presented while practicing, for which some external support is considered adequate, at least initially. Some of the reviewed studies have observed a significant association between session attendance, session engagement, and frequency of autonomous practice [52,58], which suggests that a certain degree of guidance may be needed to engage in practices. In addition, a previous systematic review found that, in Internet-delivered psychotherapies, the existence of guidance is associated with better outcomes [76]. Therefore, blended interventions, i.e., a combination of eHealth with face-to-face sessions [77], might have the potential to maintain the advantages of eHealth while offering guidance to patients. A blended MBI was studied by Cebolla et al. [37], who observed that, on average, patients with irritable bowel syndrome practiced around 30 days during the 8-week blended intervention (i.e., around 55% of days), and they invested approximately 15 min per day. Remarkably, half of the surveyed participants reported practicing regularly (between five–seven days per week), which could be considered a notable degree of adherence. In any case, new studies testing the adherence to autonomous practices in blended interventions and their impact on health outcomes are required to discuss their therapeutic potential in chronic pain conditions.
Finally, for what concerns formal vs. informal meditation, two of the three studies which compared them found that informal practices were more common [37,57]. These practices refer to applying mindfulness to day-to-day activities, such as eating or walking, without the need to use guidance or presenting a certain posture, and some studies have observed that this type of practice is associated with improvements in different health outcomes, even more than formal practices [78,79]. These latter practices are considered basic exercises to start developing the “mindful state”, i.e., the ability to observe thoughts and feelings in a non-judgmental, non-attached manner. While some programs, such as MBCT or MBSR, recommend 45 min of formal practices throughout the program, they intertwine these exercises with informal practices from the very first sessions. For patients with chronic pain, who, according to the present systematic review, tend to present with a pattern of moderately frequent low-duration meditations, it could be suitable to shorten the requirements of formal practices while finding ways to potentiate informal practices.
Limitations and Future Research Directions
The main strengths of this review are that the searches for articles were carried out in different scientific databases and trial registries, verified the selection decisions by three reviewers, and assessed the quality of the study by peers. It is also highlighted that the criteria included RCTs, randomized uncontrolled trials, open trials with pre-post analysis, as well as pilot studies, as long as they followed one of the above study designs, so the risk of not including studies relevant to the objective of the review was. Finally, both primary and secondary chronic pain have been included, following the classification carried out by the IASP [2]. However, there are certain limitations in the present review that should be considered. First, due to the variability of methods in which home practice was recorded and the heterogeneity of how its frequency was reported, it has not been possible to perform a meta-analysis. Moreover, it needs to be noted that the frequency and duration of home practices were mostly self-reported, with the associated inevitable bias. Second, a low risk of bias was concluded in only 10 studies (out of 31), making it necessary to state that higher-quality studies are needed. Third, data on follow-up assessments were only reported in four studies [48,53,56,60], which hindered the extraction of conclusions about the tendency to adhere to home practice once the interventions end. Finally, only studies published in English have been included, which may have implied the loss of articles relevant to the objective of the review.
For future studies, it is considered essential to systematically establish the way in which participants should record what type of practices and the frequency they perform at home (i.e., number of days per week) as well as the duration of each practice. In this regard, clear indications on the recommended amount of home practice should be presented to patients; most studies conducted on this topic do not report presenting such indications [80], and those which do either are based solely on the MBSR and MBCT protocols (6 days per week, 45 min per practice) or establish arbitrary ranges [34,41,42,43,49,53,59,63]. While it seems clear that higher doses of practice are related to better health outcomes, it has not been established which is the adequate nor the minimum amount of home practice associated with improvements. Probably, individual differences play an important role in this regard, but future studies should explore these aspects so that empirically-based recommendations can be offered to patients.
In another vein, new technologies offer the possibility to improve the assessment of home practice: wearable technologies, smartphone apps, text message reminders to fill in practice diaries, or online portals may be used to enhance adherence to home practice and facilitate its evaluation [28,81]; these could be complemented with some biometric variables (e.g., heart rate variability, respiration rate) to achieve a more objective measure of meditation [82], although informal practices will probably remain hard to assess with precision. On the other hand, due to the risk of abandoning the practices once the intervention program has finished, it is essential to include follow-up sessions that favor a higher rate of maintenance and analyze their impact on long-term clinical variables. Another important point is the need to improve the quality and rigor of research designs in future studies; it is indispensable to work with properly calculated sample sizes that favor a better quality of statistical analyses as well as to perform both intention-to-treat and per-protocol analyses. Finally, it should be noted that it is highly relevant to delve into the factors involved in adherence to home practice in “third wave” CBT psychotherapies and, thus, increase the rates of practice time in general [83].
5. Conclusions
The present systematic review has observed that patients with chronic pain present a pattern of moderately frequent—around four days per week—the autonomous practice of mediation while undergoing “third wave” psychotherapies, with a high degree of variability in terms of duration (i.e., minutes per practice). The reviewed studies support the relationship between the amount of practice and the treatment outcomes. The MBSR and MBCT programs were the most common interventions, and although data on practice at home was incomplete in many studies, it seems that patients with chronic pain practice significantly less than what is recommended in these programs (i.e., 6 days a week, 45 min per day), maybe due to some difficulties (e.g., maintaining a posture or focusing attention for long periods of time) that could justify some adaptations in the way that home practices are prescribed and supported. In a similar line, adolescents with chronic pain, who usually engage in very short practices, may require some previous development of meta-cognitive skills so that they can adhere properly to MBIs. In this review, a few eHealth interventions were included, with heterogeneous adherence rates to home practice; it is considered that alternatives that include guidance (e.g., blended interventions) could be more suitable for chronic pain patients, also considering some adaptations, such as shortening or reducing formal practices during the intervention in favor of informal practices which seem to be more easily implemented and even more impactful.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/ijerph20054438/s1, Table S1: Risk of bias for controlled intervention studies based on the Heart, Lung, and Blood Institute assessment tool; Table S2: Risk of bias for single-arm studies based on the Heart, Lung, and Blood Institute assessment tool. References [32,84] are cited in the Supplementary Materials.
Author Contributions
Conceptualization, A.P.-A., A.B.-S. and S.F.-M.; methodology, S.F.-M.; software, A.B.-S., A.P.-A. and S.F.-M.; validation, A.M.-B. and H.M.-S.; formal analysis, A.B.-S., A.P.-A., A.M.-B. and H.M.-S.; investigation, A.P.-A.; writing—original draft preparation, A.B.-S., A.M.-B. and A.P.-A.; writing—review and editing, P.G., M.J.C., Y.L.-d.-H. and J.G.-C.; visualization, A.B.-S.; supervision, A.P.-A. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Acknowledgments
A.P-A. has a postdoctoral “Sara Borrell” contract from the Instituto de Salud Carlos III (Spanish Ministry of Science and Innovation, CD20/00181). A.M.-B. gratefully acknowledges the support of Margarita Salas’ postdoctoral fellowship at the University of Zaragoza, funded by the European Union-NextGenerationEU.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Treede, R.D.; Rief, W.; Barke, A.; Aziz, Q.; Bennett, M.I.; Benoliel, R.; Cohen, M.; Evers, S.; Finnerup, N.B.; First, M.B.; et al. A Classification of Chronic Pain for ICD-11. Pain 2015, 156, 1003–1007. [Google Scholar] [CrossRef]
- Treede, R.D.; Rief, W.; Barke, A.; Aziz, Q.; Bennett, M.I.; Benoliel, R.; Cohen, M.; Evers, S.; Finnerup, N.B.; First, M.B.; et al. Chronic Pain as a Symptom or a Disease: The IASP Classification of Chronic Pain for the International Classification of Diseases (ICD-11). Pain 2019, 160, 19–27. [Google Scholar] [CrossRef]
- Nicholas, M.; Vlaeyen, J.W.S.; Rief, W.; Barke, A.; Aziz, Q.; Benoliel, R.; Cohen, M.; Evers, S.; Giamberardino, M.A.; Goebel, A.; et al. The IASP Classification of Chronic Pain for ICD-11: Chronic Primary Pain. Pain 2019, 160, 28–37. [Google Scholar] [CrossRef]
- Goldberg, D.S.; McGee, S.J. Pain as a Global Public Health Priority. BMC Public Health 2011, 11, 770. [Google Scholar] [CrossRef]
- Kroenke, K.; Krebs, E.E.; Bair, M.J. Pharmacotherapy of Chronic Pain: A Synthesis of Recommendations from Systematic Reviews. Gen. Hosp. Psychiatry 2009, 31, 206–219. [Google Scholar] [CrossRef]
- Mcpherson, S.; Smith, C.L.; Dobscha, S.K.; Morasco, B.J.; Demidenko, M.I.; Meath, T.H.A.; Lovejoy, T.I. Changes in Pain Intensity after Discontinuation of Long-Term Opioid Therapy for Chronic Noncancer Pain. Pain 2018, 159, 2097–2104. [Google Scholar] [CrossRef]
- Feise, R.J.; Mathieson, S.; Kessler, R.S.; Witenko, C.; Zaina, F.; Brown, B.T. Benefits and Harms of Treatments for Chronic Non-Specific Low Back Pain without Radiculopathy: Systematic Review and Meta-Analysis. Spine J. 2022. [Google Scholar] [CrossRef]
- Abdel Shaheed, C.; Awal, W.; Zhang, G.; Gilbert, S.E.; Gallacher, D.; McLachlan, A.; Day, R.O.; Ferreira, G.E.; Jones, C.M.P.; Ahedi, H.; et al. Efficacy, Safety, and Dose-Dependence of the Analgesic Effects of Opioid Therapy for People with Osteoarthritis: Systematic Review and Meta-Analysis. Med. J. Aust. 2022, 216, 305–311. [Google Scholar] [CrossRef]
- Hamilton, M.; Kwok, W.S.; Hsu, A.; Mathieson, S.; Gnjidic, D.; Deyo, R.; Ballantyne, J.; Von Korff, M.; Blyth, F.; Lin, C.-W.C. Opioid Deprescribing in Patients with Chronic Noncancer Pain: A Systematic Review of International Guidelines. Pain 2022, 164, 485–493. [Google Scholar] [CrossRef]
- Thieme, K.; Mathys, M.; Turk, D.C. Evidenced-Based Guidelines on the Treatment of Fibromyalgia Patients: Are They Consistent and If Not, Why Not? Have Effective Psychological Treatments Been Overlooked? J. Pain 2017, 18, 747–756. [Google Scholar] [CrossRef]
- Dowell, D.; Ragan, K.R.; Jones, C.M.; Baldwin, G.T.; Chou, R. CDC Clinical Practice Guideline for Prescribing Opioids for Pain—United States, 2022. MMWR Recomm. Rep. 2022, 71, 1–95. [Google Scholar] [CrossRef]
- Pérez-Aranda, A.; Barceló-Soler, A.; Andrés-Rodríguez, L.; Peñarrubia-María, M.T.; Tuccillo, R.; Borraz-Estruch, G.; García-Campayo, J.; Feliu-Soler, A.; Luciano, J.V. Description and Narrative Review of Well-Established and Promising Psychological Treatments for Fibromyalgia. Mindfulness Compassion 2017, 2, 112–129. [Google Scholar] [CrossRef]
- Williams, A.C.d.C.; Fisher, E.; Hearn, L.; Eccleston, C. Psychological Therapies for the Management of Chronic Pain (Excluding Headache) in Adults. Cochrane Database Syst. Rev. 2020, 2020, CD007407. [Google Scholar] [CrossRef]
- Jahoda, A.; Stenfert Kroese, B.; Pert, C.; Jahoda, A.; Stenfert Kroese, B.; Pert, C. Mindfulness and Third Wave Therapies. In Cognitive Behaviour Therapy for People with Intellectual Disabilities; Palgrave Macmillan: London, UK, 2017; pp. 181–212. [Google Scholar]
- Kashdan, T.B.; Rottenberg, J. Psychological Flexibility as a Fundamental Aspect of Health. Clin. Psychol. Rev. 2010, 30, 865–878. [Google Scholar] [CrossRef]
- Kabat-Zinn Full Catastrophe Living, Revised Edition: How to Cope with Stress, Pain and Illness Using Mindfulness Meditation (Google EBook); Penguin Random House: New York, NY, USA, 2013; ISBN 140551700X.
- Segal, Z.V.; Williams, J.M.; Teasdale, J.D. Mindfulness-Based Cognitive Therapy for Depression: A New Approach to Preventing Relapse; Guilford Press: New York, NY, USA, 2002. [Google Scholar]
- Hayes, S.C.; Strosahl, K.D.; Wilson, K.G. Acceptance and Commitment Therapy: The Process and Practice of Mindful Change; Guilford Press: New York, NY, USA, 2011; ISBN 1609189620. [Google Scholar]
- Karayannis, N.V.; Sturgeon, J.A.; Kemani, M.K.; Mackey, S.C.; Greco, C.M.; Wicksell, R.K.; McCracken, L.M. Pain Acceptance and Psychological Inflexibility Predict Pain Interference Outcomes for Persons with Chronic Pain Receiving Pain Psychology. Scand. J. Pain 2023. [Google Scholar] [CrossRef]
- Martinez-Calderon, J.; Flores-Cortes, M.; Morales-Asencio, J.M.; Luque-Suarez, A. Pain-Related Fear, Pain Intensity and Function in Individuals With Chronic Musculoskeletal Pain: A Systematic Review and Meta-Analysis. J. Pain 2019, 20, 1394–1415. [Google Scholar] [CrossRef]
- Maurel, S.; Sáez-Francàs, N.; Calvo, N.; Alegre-Martín, J.; Castro-Marrero, J. Identifying Mindfulness and Acceptance as Mediators between Negative Affect, Functional Disability and Emotional Distress in Patients with Fibromyalgia. Clin. Exp. Rheumatol. 2022, 40, 1102–1111. [Google Scholar] [CrossRef]
- Soundararajan, K.; Prem, V.; Kishen, T.J. The Effectiveness of Mindfulness-Based Stress Reduction Intervention on Physical Function in Individuals with Chronic Low Back Pain: Systematic Review and Meta-Analysis of Randomized Controlled Trials. Complement. Ther. Clin. Pract. 2022, 49, 101623. [Google Scholar] [CrossRef]
- Lin, T.-H.; Tam, K.-W.; Yang, Y.-L.; Liou, T.-H.; Hsu, T.-H.; Rau, C.-L. Meditation-Based Therapy for Chronic Low Back Pain Management: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Pain Med. 2022, 23, 1800–1811. [Google Scholar] [CrossRef]
- Trindade, I.A.; Guiomar, R.; Carvalho, S.A.; Duarte, J.; Lapa, T.; Menezes, P.; Nogueira, M.R.; Patrão, B.; Pinto-Gouveia, J.; Castilho, P. Efficacy of Online-Based Acceptance and Commitment Therapy for Chronic Pain: A Systematic Review and Meta-Analysis. J. Pain 2021, 22, 1328–1342. [Google Scholar] [CrossRef]
- Sturgeon, J.A. Psychological Therapies for the Management of Chronic Pain. Psychol. Res. Behav. Manag. 2014, 7, 115–124. [Google Scholar] [CrossRef]
- Perez-Aranda, A.; Feliu-Soler, A.; Montero-Marin, J.; Garcia-Campayo, J.; Andres-Rodriguez, L.; Borras, X.; Rozadilla-Sacanell, A.; Penarrubia-Maria, M.T.; Angarita-Osorio, N.; McCracken, L.M.; et al. A Randomized Controlled Efficacy Trial of Mindfulness-Based Stress Reduction Compared with an Active Control Group and Usual Care for Fibromyalgia: The EUDAIMON Study. Pain 2019, 160, 2508–2523. [Google Scholar] [CrossRef]
- Veehof, M.M.; Trompetter, H.R.; Bohlmeijer, E.T.; Schreurs, K.M.G. Acceptance- and Mindfulness-Based Interventions for the Treatment of Chronic Pain: A Meta-Analytic Review. Cogn. Behav. Ther. 2016, 45, 5–31. [Google Scholar] [CrossRef]
- Parsons, C.E.; Crane, C.; Parsons, L.J.; Fjorback, L.O.; Kuyken, W. Home Practice in Mindfulness-Based Cognitive Therapy and Mindfulness-Based Stress Reduction: A Systematic Review and Meta-Analysis of Participants’ Mindfulness Practice and Its Association with Outcomes. Behav. Res. Ther. 2017, 95, 29–41. [Google Scholar] [CrossRef]
- Lloyd, A.; White, R.; Eames, C.; Crane, R. The Utility of Home-Practice in Mindfulness-Based Group Interventions: A Systematic Review. Mindfulness 2018, 9, 673–692. [Google Scholar] [CrossRef]
- Henriksson, C.M.; Liedberg, G.M.; Gerdle, B. Women with Fibromyalgia: Work and Rehabilitation. Disabil. Rehabil. 2005, 27, 685–694. [Google Scholar] [CrossRef]
- Feliu-Soler, A.; Pérez-Aranda, A.; Andrés-Rodríguez, L.; Butjosa, A.; Díaz, N.S.; Trujols, J.; Núñez, C.; Stephan-Otto, C.; Rozadilla-Sacanell, A.; Serrano-Blanco, A.; et al. Digging into the Construct of Fibrofog: Psychometric Properties of the Spanish Version of the Multidimensional Inventory of Subjective Cognitive Impairment in Patients with Fibromyalgia. J. Appl. Biobehav. Res. 2018, 23, e12134. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 Statement: An Updated Guideline for Reporting Systematic Reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Methley, A.M.; Campbell, S.; Chew-Graham, C.; McNally, R.; Cheraghi-Sohi, S. PICO, PICOS and SPIDER: A Comparison Study of Specificity and Sensitivity in Three Search Tools for Qualitative Systematic Reviews. BMC Health Serv. Res. 2014, 14, 579. [Google Scholar] [CrossRef]
- Zanca, J.M.; Gilchrist, C.; Ortiz, C.E.; Dyson-Hudson, T.A. Pilot Clinical Trial of a Clinical Meditation and Imagery Intervention for Chronic Pain after Spinal Cord Injury. J. Spinal Cord Med. 2022, 45, 339–353. [Google Scholar] [CrossRef]
- Mittal, T.K.; Evans, E.; Pottle, A.; Lambropoulos, C.; Morris, C.; Surawy, C.; Chuter, A.; Cox, F.; de Silva, R.; Mason, M.; et al. Mindfulness-Based Intervention in Patients with Persistent Pain in Chest (MIPIC) of Non-Cardiac Cause: A Feasibility Randomised Control Study. Open Heart 2022, 9, e001970. [Google Scholar] [CrossRef]
- Gardiner, P.; D’Amico, S.; Luo, M.; Haas, N. An Innovative Electronic Health Toolkit (Our Whole Lives for Chronic Pain) to Reduce Chronic Pain in Patients with Health Disparities: Open Clinical Trial. JMIR mHealth uHealth 2020, 8, e14768. [Google Scholar] [CrossRef]
- Cebolla, A.; Navarrete, J.; Gonzalez-Moret, R.; Cortes, X.; Soria, J.M.; Banos, R.M.; Lison, J.F. Effectiveness of a Blended Internet-Based Mindfulness Intervention in Inflammatory Bowel Disease Patients: A Mixed-Methods Non-Randomized Controlled Trial. Mindfulness 2021, 12, 2767–2780. [Google Scholar] [CrossRef]
- Trompetter, H.R.; Bohlmeijer, E.T.; Veehof, M.M.; Schreurs, K.M.G. Internet-Based Guided Self-Help Intervention for Chronic Pain Based on Acceptance and Commitment Therapy: A Randomized Controlled Trial. J. Behav. Med. 2014, 38, 66–80. [Google Scholar] [CrossRef]
- Wong, S.Y.; Chan, F.W.; Wong, R.L.; Chu, M.C.; Kitty Lam, Y.Y.; Mercer, S.W.; Ma, S.H. Comparing the Effectiveness of Mindfulness-Based Stress Reduction and Multidisciplinary Intervention Programs for Chronic Pain: A Randomized Comparative Trial. Clin. J. Pain 2011, 27, 724–734. [Google Scholar] [CrossRef]
- Zernicke, K.A.; Campbell, T.S.; Blustein, P.K.; Fung, T.S.; Johnson, J.A.; Bacon, S.L.; Carlson, L.E. Mindfulness-Based Stress Reduction for the Treatment of Irritable Bowel Syndrome Symptoms: A Randomized Wait-List Controlled Trial. Int. J. Behav. Med. 2012, 20, 385–396. [Google Scholar] [CrossRef]
- Zgierska, A.E.; Burzinski, C.A.; Cox, J.; Kloke, J.; Singles, J.; Mirgain, S.; Stegner, A.; Cook, D.B.; Bačkonja, M. Mindfulness Meditation-Based Intervention Is Feasible, Acceptable, and Safe for Chronic Low Back Pain Requiring Long-Term Daily Opioid Therapy. J. Altern. Complement. Med. 2016, 22, 610–620. [Google Scholar] [CrossRef]
- Carson, J.W.; Carson, K.M.; Jones, K.D.; Bennett, R.M.; Wright, C.L.; Mist, S.D. A Pilot Randomized Controlled Trial of the Yoga of Awareness Program in the Management of Fibromyalgia. Pain 2010, 151, 530–539. [Google Scholar] [CrossRef]
- Morone, N.E.; Greco, C.M.; Weiner, D.K. Mindfulness Meditation for the Treatment of Chronic Low Back Pain in Older Adults: A Randomized Controlled Pilot Study. Pain 2008, 134, 310–319. [Google Scholar] [CrossRef]
- Rosenzweig, S.; Greeson, J.M.; Reibel, D.K.; Green, J.S.; Jasser, S.A.; Beasley, D. Mindfulness-Based Stress Reduction for Chronic Pain Conditions: Variation in Treatment Outcomes and Role of Home Meditation Practice. J. Psychosom. Res. 2010, 68, 29–36. [Google Scholar] [CrossRef]
- Garland, E.L.; Thomas, E.; Howard, M.O. Mindfulness-Oriented Recovery Enhancement Ameliorates the Impact of Pain on Self-Reported Psychological and Physical Function Among Opioid-Using Chronic Pain Patients. J. Pain Symptom Manag. 2014, 48, 1091–1099. [Google Scholar] [CrossRef] [PubMed]
- Rae, L.; Dougherty, P.; Evertz, N. Yoga vs Stretching in Veterans With Chronic Lower Back Pain and the Role of Mindfulness: A Pilot Randomized Controlled Trial. J. Chiropr. Med. 2020, 19, 101–110. [Google Scholar] [CrossRef] [PubMed]
- Van Gordon, W.; Shonin, E.; Dunn, T.J.; Garcia-Campayo, J.; Griffiths, M.D. Meditation Awareness Training for the Treatment of Fibromyalgia Syndrome: A Randomized Controlled Trial. Br. J. Health Psychol. 2017, 22, 186–206. [Google Scholar] [CrossRef]
- Donnino, M.W.; Thompson, G.S.; Mehta, S.; Paschali, M.; Howard, P.; Antonsen, S.B.; Balaji, L.; Bertisch, S.M.; Edwards, R.; Ngo, L.H.; et al. Psychophysiologic Symptom Relief Therapy for Chronic Back Pain: A Pilot Randomized Controlled Trial. Pain Rep. 2021, 6, e959. [Google Scholar] [CrossRef]
- Cooperman, N.A.; Hanley, A.W.; Kline, A.; Garland, E.L. A Pilot Randomized Clinical Trial of Mindfulness-Oriented Recovery Enhancement as an Adjunct to Methadone Treatment for People with Opioid Use Disorder and Chronic Pain: Impact on Illicit Drug Use, Health, and Well-Being. J. Subst. Abus. Treat. 2021, 127, 108468. [Google Scholar] [CrossRef]
- Greenberg, J.; Lin, A.; Zale, E.L.; Kulich, R.J.; James, P.; Millstein, R.A.; Shapiro, H.; Schatman, M.E.; Edwards, R.R.; Vranceanu, A.M. Development And Early Feasibility Testing Of A Mind-Body Physical Activity Program For Patients With Heterogeneous Chronic Pain; The GetActive Study. J. Pain Res. 2019, 12, 3279–3297. [Google Scholar] [CrossRef]
- Johannsen, M.; O’Connor, M.; O’Toole, M.S.; Jensen, A.B.; Zachariae, R. Mindfulness-Based Cognitive Therapy and Persistent Pain in Women Treated for Primary Breast Cancer. Clin. J. Pain 2018, 34, 59–67. [Google Scholar] [CrossRef]
- Day, M.A.; Halpin, J.; Thorn, B.E. An Empirical Examination of the Role of Common Factors of Therapy during a Mindfulness-Based Cognitive Therapy Intervention for Headache Pain. Clin. J. Pain 2016, 32, 420–427. [Google Scholar] [CrossRef]
- Zgierska, A.E.; Burzinski, C.A.; Cox, J.; Kloke, J.; Stegner, A.; Cook, D.B.; Singles, J.; Mirgain, S.; Coe, C.L.; Backonja, M. Mindfulness Meditation and Cognitive Behavioral Therapy Intervention Reduces Pain Severity and Sensitivity in Opioid-Treated Chronic Low Back Pain: Pilot Findings from a Randomized Controlled Trial. Pain Med. 2016, 17, 1865–1881. [Google Scholar] [CrossRef]
- Chadi, N.; Weisbaum, E.; Malboeuf-Hurtubise, C.; Kohut, S.A.; Viner, C.; Kaufman, M.; Locke, J.; Vo, D.X. Can the Mindful Awareness and Resilience Skills for Adolescents (MARS-A) Program Be Provided Online? Voices from the Youth. Children 2018, 5, 115. [Google Scholar] [CrossRef]
- Day, M.A.; Ward, L.C.; Thorn, B.E.; Burns, J.; Ehde, D.M.; Barnier, A.J.; Mattingley, J.B.; Jensen, M.P. Mechanisms of Mindfulness Meditation, Cognitive Therapy, and Mindfulness-Based Cognitive Therapy for Chronic Low Back Pain. Clin. J. Pain 2020, 36, 740–749. [Google Scholar] [CrossRef]
- Seng, E.K.; Singer, A.B.; Metts, C.; Grinberg, A.S.; Patel, Z.S.; Marzouk, M.; Rosenberg, L.; Day, M.; Minen, M.T.; Lipton, R.B.; et al. Does Mindfulness-Based Cognitive Therapy for Migraine Reduce Migraine-Related Disability in People with Episodic and Chronic Migraine? A Phase 2b Pilot Randomized Clinical Trial. Headache 2019, 59, 1448–1467. [Google Scholar] [CrossRef]
- Chadi, N.; McMahon, A.; Vadnais, M.; Malboeuf-Hurtubise, C.; Djemli, A.; Dobkin, P.L.; Lacroix, J.; Luu, T.M.; Haley, N. Mindfulness-Based Intervention for Female Adolescents with Chronic Pain: A Pilot Randomized Trial. J. Can. Acad. Child Adolesc. Psychiatry 2016, 25, 159–168. [Google Scholar]
- Day, M.; Thorn, B.E.; Ward, L.C.; Rubin, N.; Hickman, S.D.; Scogin, F.; Kilgo, G.R. Mindfulness-Based Cognitive Therapy for the Treatment of Headache Pain: A Pilot Study. Clin. J. Pain 2014, 30, 152–161. [Google Scholar] [CrossRef]
- Hesse, T.; Holmes, L.G.; Kennedy-Overfelt, V.; Kerr, L.M.; Giles, L.L. Mindfulness-Based Intervention for Adolescents with Recurrent Headaches: A Pilot Feasibility Study. Evid.-Based Complement. Altern. Med. 2015, 2015, 508958. [Google Scholar] [CrossRef]
- Howarth, A.; Riaz, M.; Perkins-Porras, L.; Smith, J.G.; Subramaniam, J.; Copland, C.; Hurley, M.; Beith, I.; Ussher, M. Pilot Randomised Controlled Trial of a Brief Mindfulness-Based Intervention for Those with Persistent Pain. J. Behav. Med. 2019, 42, 999–1014. [Google Scholar] [CrossRef]
- Pradhan, E.K.; Baumgarten, M.; Langenberg, P.; Handwerger, B.; Gilpin, A.K.; Magyari, T.; Hochberg, M.C.; Berman, B.M. Effect of Mindfulness-Based Stress Reduction in Rheumatoid Arthritis Patients. Arthritis Rheum. 2007, 57, 1134–1142. [Google Scholar] [CrossRef]
- Ali, A.; Weiss, T.R.; Dutton, A.; McKee, D.; Jones, K.D.; Kashikar-Zuck, S.; Silverman, W.K.; Shapiro, E.D. Mindfulness-Based Stress Reduction for Adolescents with Functional Somatic Syndromes: A Pilot Cohort Study. J. Pediatr. 2017, 183, 184–190. [Google Scholar] [CrossRef]
- Hearn, J.H.; Finlay, K.A. Internet-Delivered Mindfulness for People with Depression and Chronic Pain Following Spinal Cord Injury: A Randomized, Controlled Feasibility Trial. Spinal Cord 2018, 56, 750–761. [Google Scholar] [CrossRef]
- Lin, J.; Chadi, N.; Shrier, L. Mindfulness-Based Interventions for Adolescent Health. Curr. Opin. Pediatr. 2019, 31, 469–475. [Google Scholar] [CrossRef]
- Abujaradeh, H.; Safadi, R.; Sereika, S.M.; Kahle, C.T.; Cohen, S.M. Mindfulness-Based Interventions Among Adolescents With Chronic Diseases in Clinical Settings: A Systematic Review. J. Pediatr. Health Care 2018, 32, 455–472. [Google Scholar] [CrossRef] [PubMed]
- Delgado-Suárez, I.; López-del-Hoyo, Y.; García-Campayo, J.; Pérez-Aranda, A.; Modrego-Alarcón, M.; Beltrán-Ruiz, M.; Gascón, S.; Montero-Marín, J. Testing the Efficacy of ‘Unlearning’, a Mindfulness and Compassion-Based Programme for Cultivating Nonviolence in Teenagers: A Randomised Controlled Trial. Front. Psychol. 2021, 12, 717736. [Google Scholar] [CrossRef] [PubMed]
- Dunning, D.; Tudor, K.; Radley, L.; Dalrymple, N.; Funk, J.; Vainre, M.; Ford, T.; Montero-Marin, J.; Kuyken, W.; Dalgleish, T. Do Mindfulness-Based Programmes Improve the Cognitive Skills, Behaviour and Mental Health of Children and Adolescents? An Updated Meta-Analysis of Randomised Controlled Trials. Evid. Based Ment. Health 2022, 25, 135–142. [Google Scholar] [CrossRef] [PubMed]
- Santos, A.; Crespo, I.; Pérez-Aranda, A.; Beltrán-Ruiz, M.; Puebla-Guedea, M.; García-Campayo, J. Attachment-Based Compassion Therapy for Reducing Anxiety and Depression in Fibromyalgia. Int. J. Environ. Res. Public Health 2022, 19, 8152. [Google Scholar] [CrossRef]
- Lam, S.U.; Riordan, K.M.; Simonsson, O.; Davidson, R.J.; Goldberg, S.B. Who Sticks with Meditation? Rates and Predictors of Persistence in a Population-Based Sample in the USA. Mindfulness 2023, 14, 66–78. [Google Scholar] [CrossRef]
- Hunt, C.A.; Hoffman, M.A.; Mohr, J.J.; Williams, A.-L. Assessing Perceived Barriers to Meditation: The Determinants of Meditation Practice Inventory-Revised (DMPI-R). Mindfulness 2020, 11, 1139–1149. [Google Scholar] [CrossRef]
- Williams, A.-L.; Dixon, J.; McCorkle, R.; Van Ness, P.H. Determinants of Meditation Practice Inventory: Development, Content Validation, and Initial Psychometric Testing. Altern. Ther. Health Med. 2011, 17, 16–23. [Google Scholar]
- Eysenbach, G. What Is E-Health? J. Med. Internet Res. 2001, 3, E20. [Google Scholar] [CrossRef]
- Liu, C.; Zhu, Q.; Holroyd, K.A.; Seng, E.K. Status and Trends of Mobile-Health Applications for IOS Devices: A Developer’s Perspective. J. Syst. Softw. 2011, 84, 2022–2033. [Google Scholar] [CrossRef]
- MacPherson, M.; Bakker, A.M.; Anderson, K.; Holtzman, S. Do Pain Management Apps Use Evidence-Based Psychological Components? A Systematic Review of App Content and Quality. Can. J. Pain 2022, 6, 33–44. [Google Scholar] [CrossRef]
- Lippke, S.; Gao, L.; Keller, F.M.; Becker, P.; Dahmen, A. Adherence With Online Therapy vs Face-to-Face Therapy and With Online Therapy vs Care as Usual: Secondary Analysis of Two Randomized Controlled Trials. J. Med. Internet Res. 2021, 23, e31274. [Google Scholar] [CrossRef] [PubMed]
- Baumeister, H.; Reichler, L.; Munzinger, M.; Lin, J. The Impact of Guidance on Internet-Based Mental Health Interventions—A Systematic Review. Internet Interv. 2014, 1, 205–215. [Google Scholar] [CrossRef]
- Erbe, D.; Eichert, H.C.; Riper, H.; Ebert, D.D. Blending Face-to-Face and Internet-Based Interventions for the Treatment of Mental Disorders in Adults: Systematic Review. J. Med. Internet Res. 2017, 19, e306. [Google Scholar] [CrossRef]
- Kakoschke, N.; Hassed, C.; Chambers, R.; Lee, K. The Importance of Formal versus Informal Mindfulness Practice for Enhancing Psychological Wellbeing and Study Engagement in a Medical Student Cohort with a 5-Week Mindfulness-Based Lifestyle Program. PLoS ONE 2021, 16, e0258999. [Google Scholar] [CrossRef]
- Morgan, L.P.K.; Graham, J.R.; Hayes-Skelton, S.A.; Orsillo, S.M.; Roemer, L. Relationships between Amount of Post-Intervention Mindfulness Practice and Follow-up Outcome Variables in an Acceptance-Based Behavior Therapy for Generalized Anxiety Disorder: The Importance of Informal Practice. J. Context. Behav. Sci. 2014, 3, 173–178. [Google Scholar] [CrossRef] [PubMed]
- Hilton, L.; Hempel, S.; Ewing, B.A.; Apaydin, E.; Xenakis, L.; Newberry, S.; Colaiaco, B.; Maher, A.R.; Shanman, R.M.; Sorbero, M.E.; et al. Mindfulness Meditation for Chronic Pain: Systematic Review and Meta-Analysis. Ann. Behav. Med. 2017, 51, 199–213. [Google Scholar] [CrossRef]
- Slattery, B.W.; Haugh, S.; O’Connor, L.; Francis, K.; Dwyer, C.P.; O’Higgins, S.; Egan, J.; McGuire, B.E. An Evaluation of the Effectiveness of the Modalities Used to Deliver Electronic Health Interventions for Chronic Pain: Systematic Review with Network Meta-Analysis. J. Med. Internet Res. 2019, 21, e11086. [Google Scholar] [CrossRef]
- Naranjo-Hernández, D.; Reina-Tosina, J.; Roa, L.M. Sensor Technologies to Manage the Physiological Traits of Chronic Pain: A Review. Sensors 2020, 20, 365. [Google Scholar] [CrossRef]
- Masheder, J.; Fjorback, L.; Parsons, C.E. “i Am Getting Something out of This, so i Am Going to Stick with It”: Supporting Participants’ Home Practice in Mindfulness-Based Programmes. BMC Psychol. 2020, 8, 91. [Google Scholar] [CrossRef]
- Campbell, M.; McKenzie, J.E.; Sowden, A.; Katikireddi, S.V.; Brennan, S.E.; Ellis, S.; Hartmann-Boyce, J.; Ryan, R.; Shepperd, S.; Thomas, J.; et al. Synthesis without meta-analysis (SWiM) in systematic reviews: Reporting guideline. BMJ 2020, 368, l6890. [Google Scholar] [CrossRef]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2023 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).