Healthy Choices in Midlife Predict Survival to Age 85 in Women: The Tromsø Study 1979–2019
Abstract
:1. Introduction
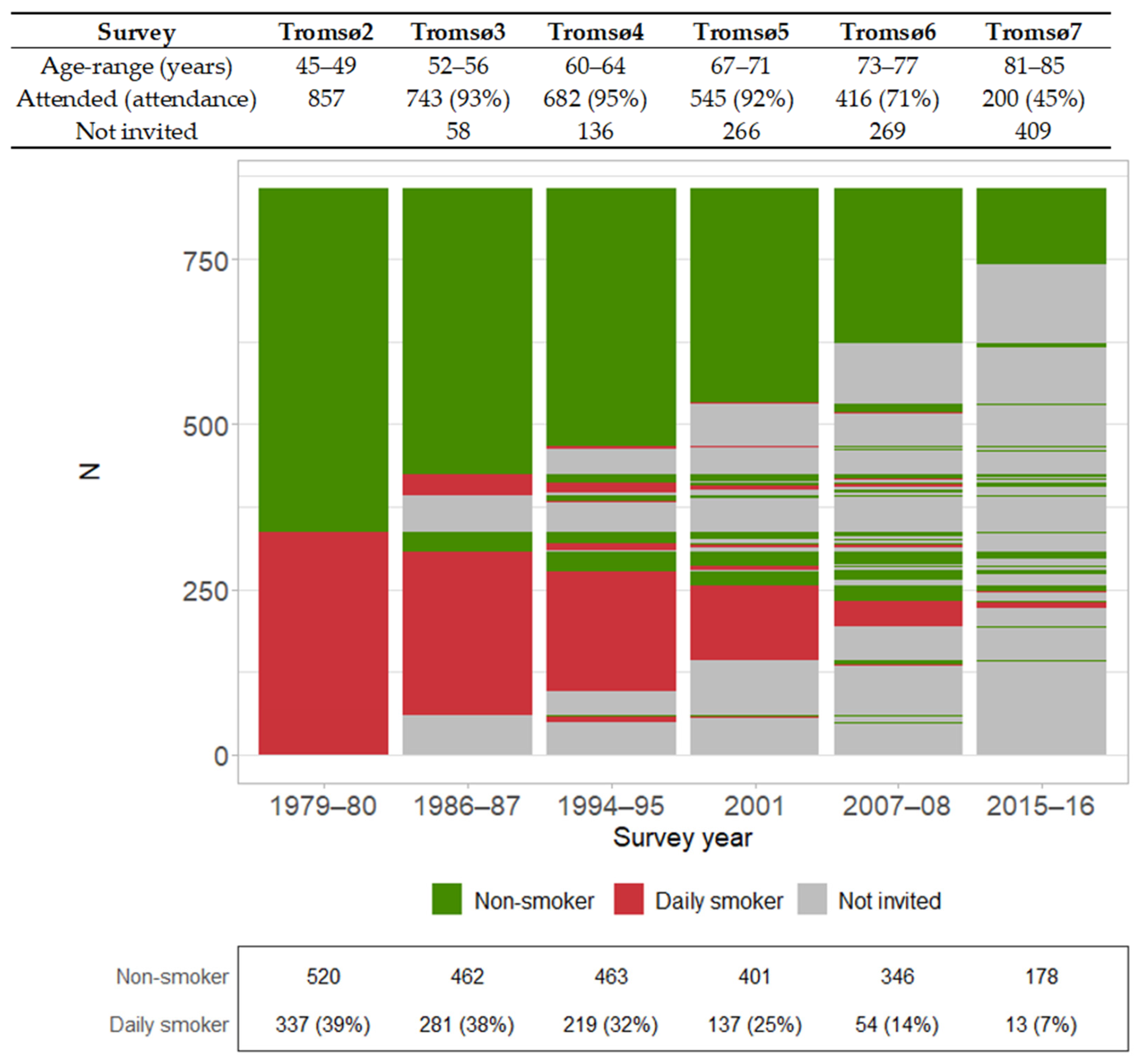
2. Materials and Methods
2.1. Study Population
2.2. Endpoint and Risk Factors
2.3. Statistical Analysis
2.4. Ethics
3. Results
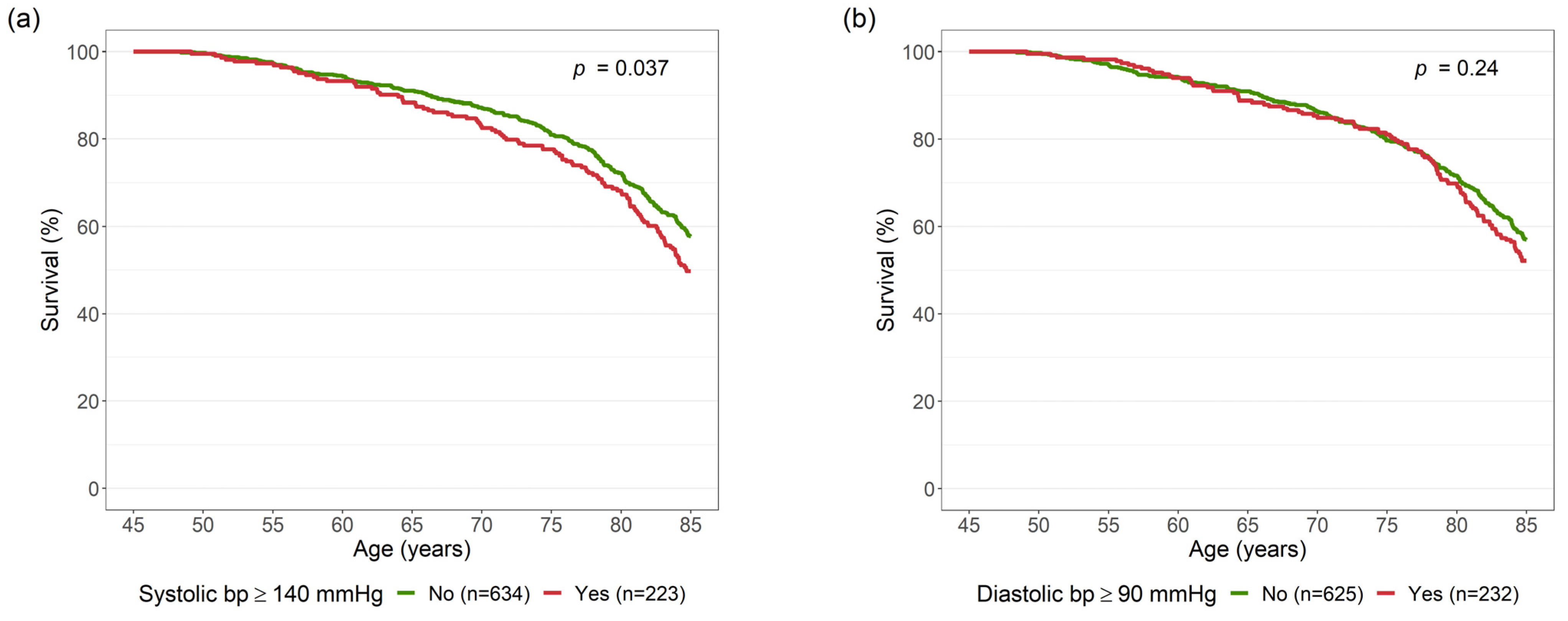
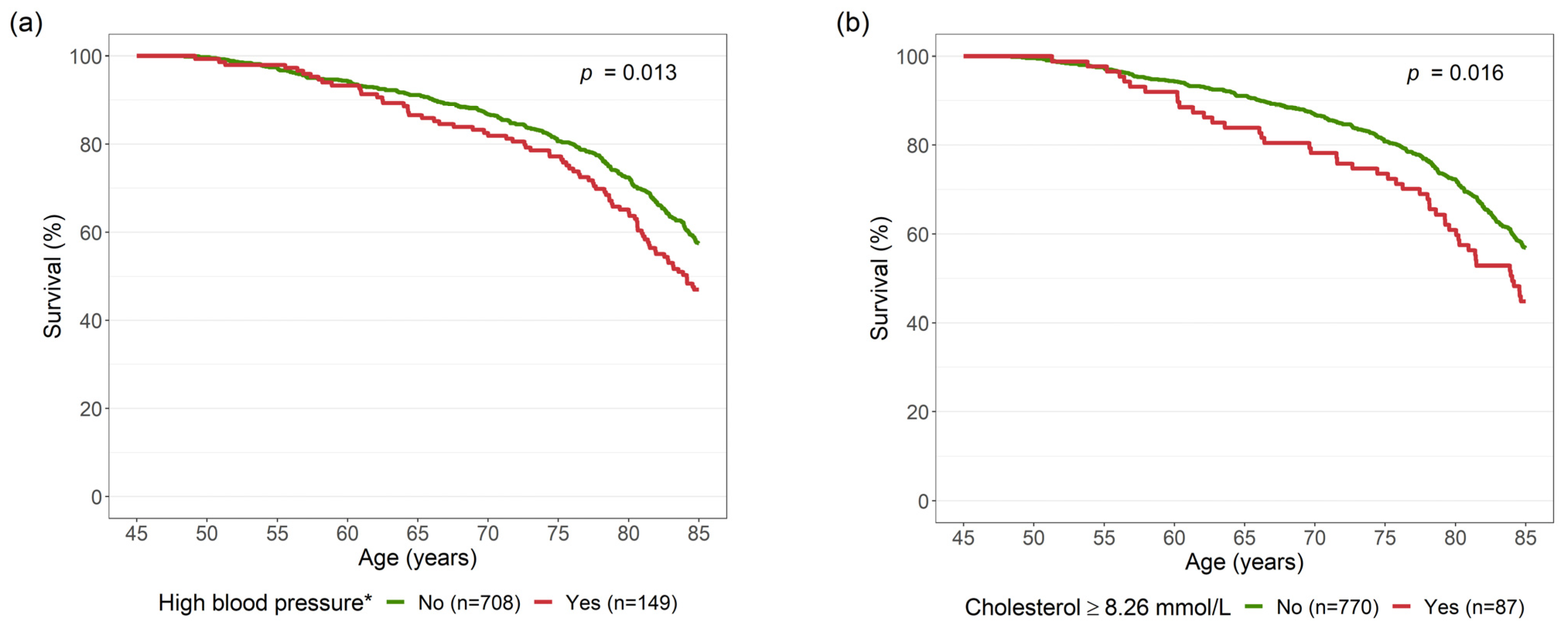
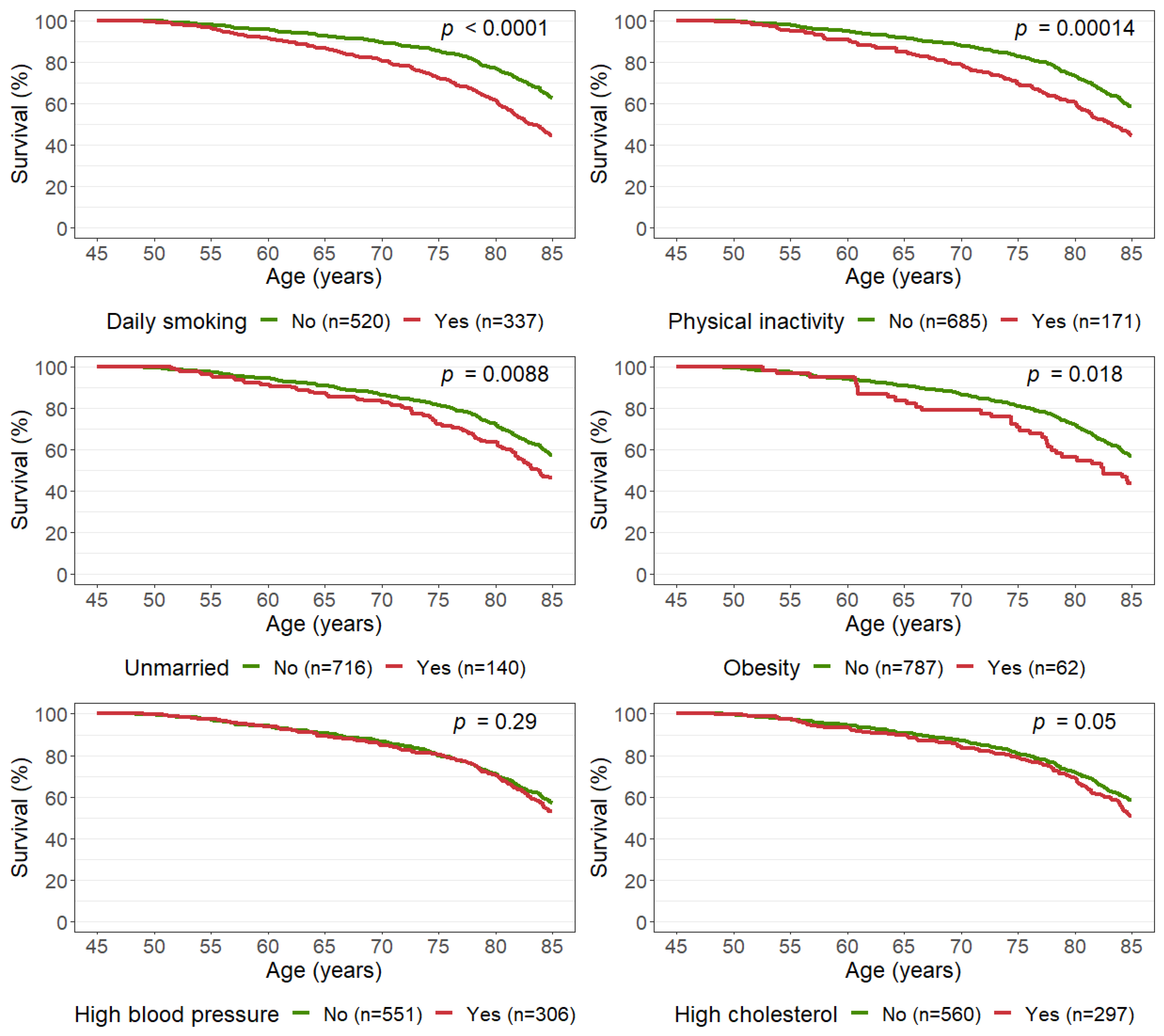
3.1. Single Risk Factors
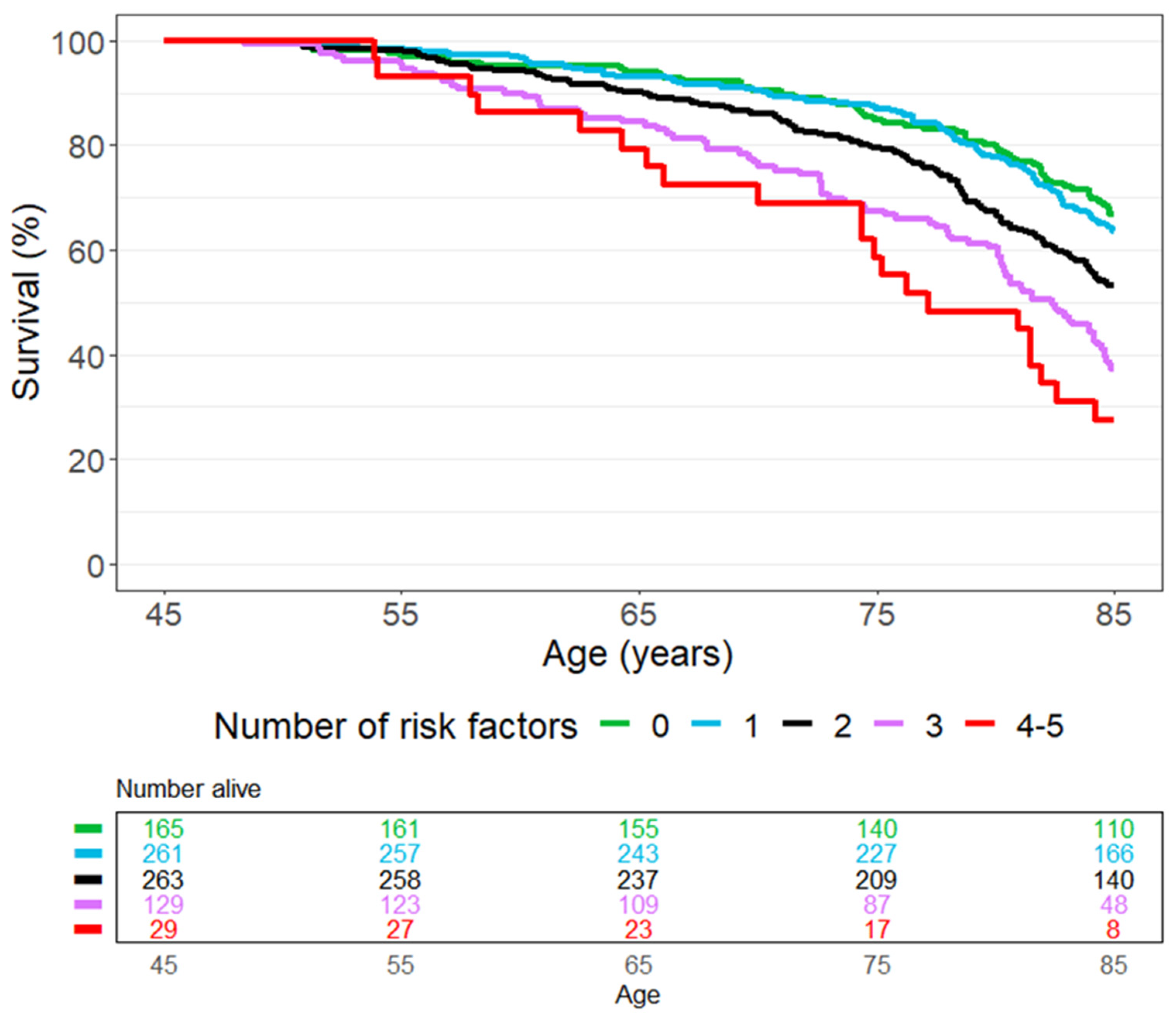
3.2. Number of Risk Factors
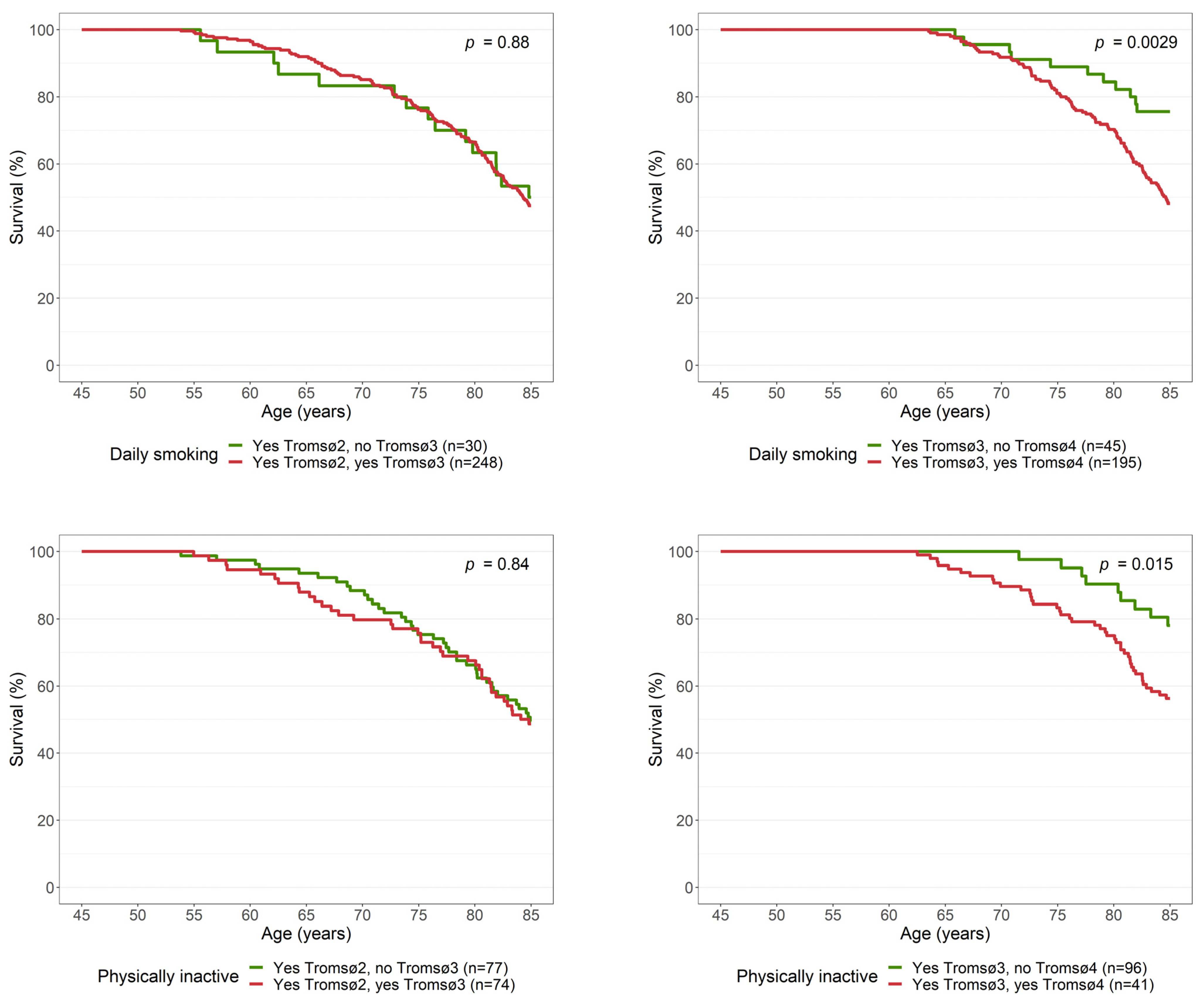
3.3. Changes in Daily Smoking and Physical Inactivity from Midlife to Older Age
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
Appendix A
High Blood Pressure and High Cholesterol
| Diastolic Blood Pressure ≥ 90 mmHg | |||
|---|---|---|---|
| Systolic Blood Pressure ≥ 140 mmHg | No | Yes | Total |
| No | 560 | 85 | 645 |
| Yes | 76 | 136 | 212 |
| Total | 636 | 221 | 857 |
| Risk Factor | Hazard Ratio | 95% Confidence Interval | p-Value |
|---|---|---|---|
| Daily smoking | 1.78 | 1.45, 2.19 | <0.001 |
| Physical inactivity | 1.41 | 1.11, 1.79 | 0.005 |
| Unmarried | 1.36 | 1.05, 1.76 | 0.018 |
| Obesity | 1.79 | 1.20, 2.69 | 0.004 |
| High blood pressure * | 1.36 | 1.06, 1.76 | 0.017 |
| High cholesterol ** | 1.30 | 0.96, 1.77 | 0.094 |
References
- Roser, M.; Ortiz-Ospina, E.; Ritchie, H. Life Expectancy. Our World in Data. 2013. Available online: https://ourworldindata.org/life-expectancy (accessed on 24 October 2021).
- WHO. Life Expectancy at Birth (Years). Available online: https://www.who.int/data/gho/data/indicators/indicator-details/GHO/life-expectancy-at-birth-(years) (accessed on 24 October 2021).
- Newman, A.B.; Murabito, J.M. The epidemiology of longevity and exceptional survival. Epidemiol. Rev. 2013, 35, 181–197. [Google Scholar] [CrossRef] [PubMed]
- Herskind, A.M.; McGue, M.; Holm, N.V.; Sorensen, T.I.; Harvald, B.; Vaupel, J.W. The heritability of human longevity: A population-based study of 2872 Danish twin pairs born 1870–1900. Hum. Genet. 1996, 97, 319–323. [Google Scholar] [CrossRef] [PubMed]
- Terry, D.F.; Pencina, M.J.; Vasan, R.S.; Murabito, J.M.; Wolf, P.A.; Hayes, M.K.; Levy, D.; D’Agostino, R.B.; Benjamin, E.J. Cardiovascular risk factors predictive for survival and morbidity-free survival in the oldest-old Framingham Heart Study participants. J. Am. Geriatr. Soc. 2005, 53, 1944–1950. [Google Scholar] [CrossRef] [PubMed]
- Brenn, T. Survival to Age 90 in Men: The Tromso Study 1974–2018. Int. J. Environ. Res. Public Health 2019, 16, 2028. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Urtamo, A.; Jyvakorpi, S.K.; Kautiainen, H.; Pitkala, K.H.; Strandberg, T.E. Major cardiovascular disease (CVD) risk factors in midlife and extreme longevity. Aging Clin. Exp. Res. 2020, 32, 299–304. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Yates, L.B.; Djousse, L.; Kurth, T.; Buring, J.E.; Gaziano, J.M. Exceptional longevity in men: Modifiable factors associated with survival and function to age 90 years. Arch. Intern. Med. 2008, 168, 284–290. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wilhelmsen, L.; Svardsudd, K.; Eriksson, H.; Rosengren, A.; Hansson, P.O.; Welin, C.; Oden, A.; Welin, L. Factors associated with reaching 90 years of age: A study of men born in 1913 in Gothenburg, Sweden. J. Intern. Med. 2011, 269, 441–451. [Google Scholar] [CrossRef] [PubMed]
- Jacobsen, B.K.; Eggen, A.E.; Mathiesen, E.B.; Wilsgaard, T.; Njolstad, I. Cohort profile: The Tromso Study. Int. J. Epidemiol. 2012, 41, 961–967. [Google Scholar] [CrossRef] [PubMed]
- Available online: www.tromsostudy.com (accessed on 12 January 2022).
- Morseth, B.; Hopstock, L.A. Time trends in physical activity in the Tromso study: An update. PLoS ONE 2020, 15, e0231581. [Google Scholar] [CrossRef] [PubMed]
- Brenn, T. The Tromso Heart-Study—Alcoholic Beverages and Coronary Risk-Factors. J. Epidemiol. Commun. Health 1986, 40, 249–256. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Jacobsen, B. Frequency of alcohol use and the level of education. J. Intern. Med. 1989, 225, 417–422. [Google Scholar] [CrossRef] [PubMed]
- Løvsletten, O.; Njølstad, I.; Wilsgaard, T.; Hopstock, L.A.; Jacobsen, B.K.; Bønaa, K.H.; Eggen, A.E.; Løchen, M.L. Is the ongoing obesity epidemic partly explained by concurrent decline in cigarette smoking? Insights from a longitudinal population study. The Tromsø Study 1994–2016. Prev. Med. 2021, 147, 106533. [Google Scholar] [CrossRef] [PubMed]
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2021. [Google Scholar]
- Wickham, H. ggplot2: Elegant Graphics for Data Analysis; Springer: New York, NY, USA, 2016. [Google Scholar]
- Jones, M.; Hockey, R.; Mishra, G.D.; Dobson, A. Visualising and modelling changes in categorical variables in longitudinal studies. BMC Med. Res. Methodol. 2014, 14, 32. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Stanaway, J.D.; Afshin, A.; Gakidou, E.; Lim, S.S.; Abate, D.; Abate, K.H.; Abbafati, C.; Abbasi, N.; Abbastabar, H.; Abd-Allah, F. Global, regional, and national comparative risk assessment of 84 behavioural, environmental and occupational, and metabolic risks or clusters of risks for 195 countries and territories, 1990–2017: A systematic analysis for the Global Burden of Disease Study 2017. Lancet 2018, 392, 1923–1994. [Google Scholar]
- Mok, A.; Khaw, K.T.; Luben, R.; Wareham, N.; Brage, S. Physical activity trajectories and mortality: Population based cohort study. BMJ 2019, 365, l2323. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Brandts, L.; van den Brandt, P.A. Sex-specific associations between smoking habits and reaching longevity: Netherlands Cohort Study. Geriatr. Gerontol. Int. 2018, 18, 1249–1258. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kravdal, O. Large and Growing Social Inequality in Mortality in Norway: The Combined Importance of Marital Status and Own and Spouse’s Education. Popul. Dev. Rev. 2017, 43, 645. [Google Scholar] [CrossRef] [Green Version]
- Lee, L.O.; James, P.; Zevon, E.S.; Kim, E.S.; Trudel-Fitzgerald, C.; Spiro, A.; Grodstein, F.; Kubzansky, L.D. Optimism is associated with exceptional longevity in 2 epidemiologic cohorts of men and women. Proc. Natl. Acad. Sci. USA 2019, 116, 18357–18362. [Google Scholar] [CrossRef] [PubMed] [Green Version]
| Characteristic | Overall N = 857 1 | Alive at Age 85 N = 477 1 | Died before Age 85 N = 380 1 |
|---|---|---|---|
| Daily smoking | 337 (39%) | 150 (31%) | 187 (49%) |
| Physical inactivity | 171 (20%) | 76 (16%) | 95 (25%) |
| Unmarried | 140 (16%) | 65 (14%) | 75 (20%) |
| Body mass index (kg/m2) | 23.6 (21.8, 26.0) | 23.5 (21.8, 25.8) | 23.7 (21.8, 26.4) |
| Obesity | 62 (7.3%) | 27 (5.7%) | 35 (9.3%) |
| High blood pressure | 306 (36%) | 162 (34%) | 144 (38%) |
| Blood pressure medication | 43 (5.0%) | 18 (3.8%) | 25 (6.6%) |
| Systolic blood pressure (mmHg) | 126 (118, 138) | 126 (116, 138) | 127 (118, 140) |
| Diastolic blood pressure (mmHg) | 82 (76, 90) | 82 (76, 88) | 84 (78, 90) |
| Total cholesterol (mmol/L) | 6.50 (5.75, 7.39) | 6.44 (5.71, 7.32) | 6.65 (5.79, 7.51) |
| High cholesterol | 297 (35%) | 151 (32%) | 146 (38%) |
| Risk Factors | Hazard Ratio | 95% Confidence Interval | p-Value |
|---|---|---|---|
| Daily smoking | 1.77 | 1.44, 2.19 | <0.001 |
| Physical inactivity | 1.43 | 1.12, 1.82 | 0.004 |
| Unmarried | 1.37 | 1.06, 1.78 | 0.015 |
| Obesity | 1.67 | 1.17, 2.38 | 0.005 |
| High blood pressure | 1.16 | 0.94, 1.44 | 0.2 |
| High cholesterol | 1.17 | 0.95, 1.44 | 0.2 |
| Characteristic | Hazard Ratio | 95% Confidence Interval | p-Value |
|---|---|---|---|
| Quitter 1 (Tromsø2 and Tromsø3) | 1.07 | 0.62, 1.83 | 0.8 |
| Quitter 1 (Tromsø3 and Tromsø4) | 0.41 | 0.22, 0.78 | 0.006 |
| Physically inactive → active 2 (Tromsø2 and Tromsø3) | 1.24 | 0.76, 2.05 | 0.4 |
| Physically inactive → active 2 (Tromsø3 and Tromsø4 3) | 0.44 | 0.21, 0.92 | 0.029 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Løvsletten, O.; Brenn, T. Healthy Choices in Midlife Predict Survival to Age 85 in Women: The Tromsø Study 1979–2019. Int. J. Environ. Res. Public Health 2022, 19, 5219. https://doi.org/10.3390/ijerph19095219
Løvsletten O, Brenn T. Healthy Choices in Midlife Predict Survival to Age 85 in Women: The Tromsø Study 1979–2019. International Journal of Environmental Research and Public Health. 2022; 19(9):5219. https://doi.org/10.3390/ijerph19095219
Chicago/Turabian StyleLøvsletten, Ola, and Tormod Brenn. 2022. "Healthy Choices in Midlife Predict Survival to Age 85 in Women: The Tromsø Study 1979–2019" International Journal of Environmental Research and Public Health 19, no. 9: 5219. https://doi.org/10.3390/ijerph19095219
APA StyleLøvsletten, O., & Brenn, T. (2022). Healthy Choices in Midlife Predict Survival to Age 85 in Women: The Tromsø Study 1979–2019. International Journal of Environmental Research and Public Health, 19(9), 5219. https://doi.org/10.3390/ijerph19095219






