Abstract
This study aimed to determine the effect of a forest healing anti-aging program on psychological, physiological, and physical health in older people with mild cognitive impairment (MCI). Twenty-two older people with MCI living in the city participated in a forest healing anti-aging program. Psychological indicators included the mini-mental state examination (MMSE), Beck depression inventory (BDI), profile of mood states (POMS), World Health Organization Quality of Life instrument (WHOQOL), and the Pittsburgh sleep quality index (PSQI). Physiological indicators included vital signs, body composition, and blood analysis. Physical indicators included the senior fitness test (SFT), muscle strength, spatiotemporal parameter of gait, static balance, and dynamic balance. Psychological, physiological, and physical indicators were evaluated at first and second pre-measurement, post-measurement, and one-month follow-up. MMSE, BDI, POMS, WHOQOL, body composition, blood analysis, SFT, muscle strength, spatiotemporal parameter of gait, and dynamic balance were significantly different between pre- and post-measurement. Beck depression inventory, POMS, WHOQOL, PSQI, SFT, muscle strength (elbow flexor muscle, knee extensor muscle), spatiotemporal parameter of gait significantly improved continually until the one-month follow-up. In conclusion, the forest healing program had a positive effect on the psychological, physiological, and physical health of older people with MCI.
1. Introduction
Modern society is facing a population aging phase due to advances in medical technology and a low birth rate. According to the National Statistical Office of South Korea, the average life expectancy worldwide as of 2020 is 72.3 years, and by 2100, 80 years later, it is expected have increased by approximately 10 years to 81.7 years. In 2018, the proportion of the population aged 65 and over reached 14.3% in Korea, entering an aging society, which is expected to become a post-aged society by 2025 [1]. The aging phenomenon is not only occurring in Korea but also around the world, which means that the social economy of future societies will be very different from the present.
Dementia is one of the main causes of disability and dependence in older people around the world. Cognitive function of older people with dementia is significantly lower than that of normal older people of the same age, which negatively affects overall brain activities such as memory, thinking, understanding, learning, language judgment, and calculation. In 2015, the global socioeconomic cost of dementia was estimated to be $800 billion, equivalent to 1.1% of global gross domestic product (GDP) [2]. One way to mediate this rapid increase in the prevalence of dementia is to detect and cope with mild cognitive impairment (MCI) early. MCI refers to an intermediate stage between the decline in expected cognitive function due to normal aging and severe cognitive decline due to dementia [3]. The importance of treatment in older people with MCI is easily overlooked because their memory is slightly decreased, but their ability to perform daily activities is maintained. However, the conversion rate of dementia in people over 65 years of age who have MCI is approximately 15%, which is more than five times higher than that of older people without MCI. In Korea, the number of MCI patients reached 230,000 in 2018, an increase of approximately ten times compared to 2010, and the total cost of treatment reached 30.3 billion dollars in 2014. As the age of onset is also decreasing gradually, early detection and management of MCI, which is highly likely to progress to dementia, are necessary [4].
In an aging society, it is important not only to prolong life but also to lead a healthy life through well-being. However, in many countries, serious environmental pollution has occured due to rapid urbanization along with the aging population. This causes various psychological stresses or lowers the quality of life in older people [5]. Various intervention methods have been proposed worldwide to improve the physical and psychological health of older people, and among them, interventions through nature are emerging. Previous studies have reported that greater exposure to nature has a positive effect on human cognition and emotion [6], and physical activity in an environment such as a forest or grassland has a much more positive effect on mental health than indoor exercise [7,8]. In addition, it has been found that exercise that involves different landforms and altitudes, such as trekking, has positive effects on increasing the amount of physical activity [9]. In particular, in countries with abundant forest resources, forest healing is being proposed as a therapeutic intervention method for older people and various diseases.
Forest therapy is a natural therapy defined as activities that improve the health of the human body by utilizing various physical and environmental factors of nature. Its main purpose is to help maintain health and enhance immunity [10]. In Korea, 63.4% of the land is forest, and the Korea Forest Service is developing and distributing several forest healing programs using forest resources in response to the aging population and increase in chronic diseases. The Korea Forest Welfare Institute, an organization affiliated with the Korea Forest Service, operates forest healing programs at 15 forest welfare facilities, including the National Center for Forest Therapy, to provide optimal forest welfare services to the public [11].
To date, many positive effects of forest healing have been reported on the human body. People who have undergone forest therapy have decreased depression [12] and cortisol levels [13], and their mood states have improved [14]. It also reduces blood pressure [15] and activates parasympathetic nerves [16]. In a study that implemented a forest healing program for older people, it was reported that the cardio-ankle vascular index and forced expiratory volume were improved [17] and melatonin levels increased [18]. However, no studies have reported the effects of forest therapy on older people with MCI. Therefore, this study aimed to verify the effect of the forest healing anti-aging program on the psychological, physiological, and physical health of older people with MCI.
2. Materials and Methods
2.1. Participants
The participants of this study were recruited through poster advertisements at the Seoul Metropolitan Center for Dementia (37.47, 126.90) located in Geumcheon-gu, Seoul, from July to August 2020.
Among those wishing to participate, we recruited those who were 60 years or older, able to walk 10 m independently without a walking aid and had a score between 23 and 27 in the Korean version of the Mini-Mental State Examination (MMSE-K) [19]. The exclusion criteria were as follows: (1) persons who lack Korean skills and have limited communication, (2) persons with Parkinsonism or motor-impairing neurological disorders (e.g., stroke), (3) persons whose musculoskeletal disorders in the lower extremities (e.g., severe osteoarthritis or a history of knee/hip joint replacement surgery) could affect the performance of walking during a clinical examination, (4) persons who have taken neuroleptics or benzodiazepines and major depression drugs, (5) persons whose Beck depression index are 19 or more points, (6) persons who have visited the forest at least once a week, and (7) persons who perform moderate-intensity aerobic physical activities for more than 300 min per week.
To calculate the sample size, G*Power 3.1.9.7 was used, with an effect size of 0.25, a significance level of 0.05, and an α power of 0.8. Based on these values, with a 20% dropout rate, a total of 27 subjects were required. Therefore, 22 people participated in the experiment, and all participants completed the research participation agreement form before participating in the study. This study was approved by the Bioethics Review Committee of the Gachon University (1044396-202006-HR-111-02) and was registered with the Clinical Research Information Service (CRIS; KCT0005365).
2.2. Study Sites
This study was conducted at the National Center for Forest Therapy, located in Yecheon-gun (36.83, 128.47) and Yeongju-si (36.87, 128.49), Gyeongsangbuk-do, South Korea. The National Center for Forest Therapy consists of a central facility district of about 142 ha with buildings such as Forest of Healing, Barefoot Garden, and Forest Healing Camp Center. The forest path around the National Center for Forest Therapy is connected to Sobaeksan National Park, Myojeokbong, and Cheonbusan, which is approximately 50 km long and has a section with a deck road with an inclination of less than 8%, so that even older people can hike without difficulty.
The average temperature in September–October at the location was 21.43–11.60 degrees Celsius, and in fall, the five components (α-Pinene, β-Pinene, Camphene, Limonene, Camphor) with the highest concentration among the natural volatile organic compounds (NVOCs) were present at a rate of 77.91 pptv [20].
In this area, tree species, such as Pinus koraiensis Siebold and Zucc., Pinus densiflora Siebold and Zucc., and Quercus mongolica Fisch. ex Ledeb. form a mixed forest. In addition, various plant groups such as Larix kaempferi (Lamb.) Carrière, Lindera obtusiloba Blume, Koelreuteria paniculata Laxm., and Rhododendron mucronulatum Turcz. grow wild.
2.3. Procedure
The recruitment of participants for this study started in July and was completed in August 2020. The first pre-measurement started in mid-August 2020, and the intervention and evaluation were completed in November 2020. The flowchart in Figure 1 shows the research procedure that was used in this study.
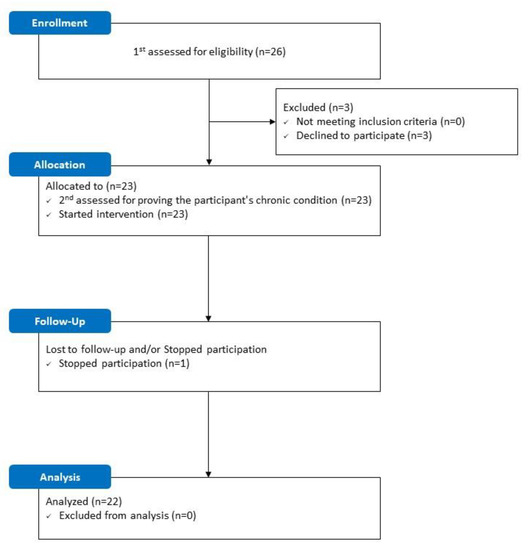
Figure 1.
Flowchart.
Before participating in the study, the participants were asked for their consent to use their personal information and were informed that all data would be encrypted and processed. Those who agreed to participate signed a consent form, and all research procedures were conducted in compliance with the Declaration of Helsinki of the World Medical Association.
Before the start of the forest healing anti-aging program, information on general characteristics and psychological, physiological, and physical indicators for 22 participants were evaluated using two pre-measurements. The participants performed two pre-measurements before participating in the program. To prove that a participant’s condition was chronic, the second pre-measurement was performed at an interval of at least one month after the first pre-measurement. On the day of the second pre-measurement, all participants underwent a forest healing anti-aging program for two days and one night over three weeks. After the schedule was completed, the measurement items that were performed during the two pre-measurements were evaluated in the same way to verify the effectiveness of the program. All evaluations were performed by one medical doctor, one nurse, and four physical therapists with more than three years of clinical experience.
2.4. Measurement
Except for blood analysis, all variables were evaluated at the first and second pre-measurement, post-measurement 4 h after the last intervention, and one-month follow-up-measurement. Blood collection and analysis were performed at the second pre-measurement and post-measurement.
2.4.1. Psychological Variables
The MMSE-K was used to screen the participants’ cognitive status and examine the changes in cognitive function. The MMSE-K has a total of 30 points, of which mild cognitive impairment falls between 23 and 27 points. This tool has high sensitivity and specificity and is widely used because of its excellent validity (0.93) [21].
The Korean version of the Beck depression inventory (K-BDI) was used for participant screening and depressive status. The K-BDI is a self-reporting tool designed to evaluate the presence and severity of depression. It consists of 21 items covering the cognitive, emotional, motivational, and physical domains of depression, and each item is scored on a scale of 0 to 3, for a total of 63 points. A score of 0–9 means no or minimal depression, a score of 10–18 means little or moderate depression, a score of 19–29 means moderate to severe depression, and a score of 30–63 means very severe depression. The overall reliability coefficient of the BDI is 0.882, and the test-retest reliability is 0.93, which is very high [22].
The Korean version of the profile of mood states (K-POMS) was used to examine the participants’ mood states. This tool evaluates an individual’s current feelings and attitudes using a five-point scale across 65 items. The mood state scale consists of six items: tension-anxiety (TA), depression-dejection (DD), anger-hostility (AH), fatigue-inertia (FI), confusion-bewilderment (CB), and vigor-activity (VA). After summing up the corresponding scores, the score of the VA item is excluded to calculate the total mood disturbance (TMD) score. Currently, the higher the total score in the remaining areas (except for the VA item), the more severe the mood disorder. The overall reliability coefficient of the K-POMS is 0.93 [23].
The Korean short version of the WHOQOL (K-WHOQOL-BREF) was used to measure the participants’ quality of life. This tool consists of 26 questions in five areas: overall quality of life and general health (OG), physical health (PH), psychological, social relationship (SR), and environmental health, and each question can be answered on a five-point Likert scale. The higher the score in each domain, the more positive the evaluation of the quality of life. The test-retest reliability of this scale is 0.841 and the overall reliability coefficient is 0.898 [24].
The Korean version of the Pittsburgh sleep quality index (K-PSQI) was used to evaluate the sleep quality of the participants. This tool is self-reported and consists of seven areas and 18 items. The details are as follows: (1) sleep quality, (2) sleep latency, (3) sleep duration, (4) habitual sleep efficiency, (5) sleep disturbance, (6) use of sleeping medication, and (7) daytime dysfunction. The sleep index can be calculated by adding up the scores of all seven items, out of a total of 21 points. The higher the score, the lower the quality of sleep. The overall reliability coefficient of this scale is 0.84 and the test-retest reliability is 0.65 [25].
2.4.2. Physiological Variables
Blood pressure and heart rate were measured using an automatic electronic sphygmomanometer (ACCUNIQ BP203, SELVAS Healthcare, Daejeon, Korea) to evaluate vascular risk factors, which are risk factors for dementia. The participants were placed on a curve with one arm relaxed and constant breathing.
A body composition analyzer (Inbody470, InBody Co., Seoul, Korea) was used to examine body composition changes in the participants. The tested variables were skeletal muscle mass, body fat mass, and total body water. The participants stood barefoot on the device and took correct measurement postures according to the evaluator’s instructions.
Approximately 5 mL of blood was collected by injection through a vein to examine biomarkers indicating the health status, stress, and emotional level of the participants. Blood was collected at 8 a.m. for the second pre-measurement and post-measurement by direct injection by medical personnel with more than 10 years of experience. The factors identified in the collected blood were as follows: cathepsin B, insulin-like growth factor 1 (IGF-1), cortisol, and C-reactive protein (CRP). Cathepsin B has been reported to be related to long-term memory [26] and IGF-1 has been reported to be related to the response time to stimuli [27]. Cortisol is a major factor related to stress [28], and it has been reported that CRP is related to chronic stress [29]. The collected blood was assigned a code for each participant so that personal information could not be identified. Blood analysis was performed by SCL Healthcare (Yongin-si, South Korea), an external analysis company. The reagents and analytical equipment used for each factor analysis are listed in Appendix A (Table A1).
2.4.3. Physical Variables
Functional fitness was assessed using the senior fitness test (SFT). The six components of the SFT are as follows: (1) arm curl, (2) chair stand, (3) 2-min step walk, (4) back scratch, (5) chair sit and reach, and (6) 8-ft up and go. This tool allows the evaluation of strength, endurance, flexibility, dynamic balance, and agility of the upper and lower extremities [30]. When the SFT was performed on older people with cognitive impairment, the test-retest reliability ranged from 0.93 to 0.98 [31].
The muscle strength of the elbow flexor (EF), knee extensor (KE), and ankle plantar flexor (APF) were measured using a digital hand-held dynamometer (microFET®, Hoggan Scientific, Salt Lake City, UT, USA), and a digital dynamometer (Jamar Plus, Sammons Preston, Bolingbrook, IL, USA; Jamar Pinch Gauge, Patterson Medical, Bolingbrook, IL, USA) was used to assess handgrip strength and finger pinch strength. The participant performed elbow flexion and knee extension according to the evaluator’s instructions in a sitting position in a chair and ankle plantar flexion in the supine position, while measuring the pushing force by placing the portable dynamometer in the opposite direction of the motion. The digital dynamometer evaluated hand and finger pinch strength using gripping tools in a sitting position on a chair. All tools used to measure muscle strength have a very high level of reliability, above 0.90 [32,33].
A GAITRite walkway (GAITRite®, CIR-systems Inc., Sparta, NJ, USA) with a size of 457.2 cm × 90.2 cm × 64 cm was used to analyze spatiotemporal changes in walking. To exclude accelerators and decelerators from the measurements, participants were instructed to start walking two meters in front of the mat’s start point and walk at a self-selected comfortable pace up to a marked line two meters behind the mat’s endpoint. Measurements were made twice, with a one-minute rest period between measurements. The sampling rate was set to 100 Hz, and data were collected and analyzed using GAITRite Platinum software (version 4.7.7), a dedicated software for GAITRite®. The measurements collected were as follows: velocity (cm/s), cadence (steps/min), step length (cm), stride length (cm), step time (s), swing time (s), stance time (s), and cycle time (s). The reliability of this tool is 0.92, which is very high, and the intra-rater correlation coefficient is 0.96 or more [34].
To evaluate static balance ability, an AMTI AccuSway (Advanced Mechanical Technology, Inc., Watertown, MA, USA) was used, and the participant’s sway velocity and sway area were analyzed in the standing position with eyes open and eyes closed. The reliability of this tool is 0.70–0.89 [35]. Dynamic balance ability was evaluated using the modified functional reach test by measuring the distance to reach forward, left, and right in a sitting position in a chair. The starting point was marked by raising the arm so that the participant’s trunk and upper arm formed a 90° angle in the direction to be measured. The intra-rater reliability of the measurement method is 0.96 or higher [36].
2.5. Intervention
Participants performed one session per week, two days per session, for a three-week forest healing program at the National Center for Forest Therapy. The forest healing program was based on the forest healing anti-aging program developed by the Korea Forest Service, which consists of detailed items that evenly cover the areas of the body, cognition, emotion, and nutrition (Table 1 and Table 2).

Table 1.
The forest healing anti-aging program schedule.

Table 2.
Composition of the forest healing anti-aging program.
During the intervention period of two days and one night, the participants stayed only at the facility within the National Center for Forest Therapy, and lodging and meals were also used within the facility. To move between programs, walking was used.
All interventions were conducted under the guidance of five forest healing instructors from the National Center for Forest Therapy who had extensive experience in guiding forest healing programs. The forest healing instructors who conducted the intervention had a bachelor’s degree or higher and had at least one year of experience in forest healing.
2.6. Statistics Analysis
All statistical analyses were performed using SPSS software version 25.0 (SPSS Inc., Chicago, IL, USA). Normality testing was performed using the Shapiro–Wilk test. A paired t-test was used for variables that satisfied normality to examine the difference between the first and second pre-measurements, and the Wilcoxon signed-rank test was used for variables that did not satisfy normality. A repeated measures analysis of variance (ANOVA) and paired t-test were used for variables satisfying normality to compare differences in measured values at each time point, and the Friedman test and the Wilcoxon signed-rank test were used for variables that did not satisfy normality. Post hoc analysis using the Wilcoxon signed-rank test was performed applying Bonferroni correction, and as a result, the significance level was set to p < 0.017. The statistical significance level was set at α = 0.05.
3. Results
3.1. General Characteristics of Participants
Twenty-six older city dwellers with MCI who met the inclusion criteria were recruited and participated in the first pre-measurement. Three participants later dropped out before the second pre-measurement due to personal circumstances, and additional participants dropped out after one intervention; thus, a total of 22 people finally participated in the study. The descriptive statistics of the participants’ general characteristics, such as age, sex, and body measurements, are shown in Table 3.

Table 3.
General Characteristics of Participants.
3.2. Baseline Background Characteristics
Among the variables measured at both time points, the difference between the first and second pre-measurements was not significant for all variables (p > 0.05) (Appendix A, Table A2). Since there was no significant difference between the first and second pre-measurements, the second pre-measurement values were set as the pre-measurement value (Pre) to investigate the effect of the forest healing anti-aging program. Blood analysis was only performed at the second pre-measurement.
3.2.1. Psychological Effects of the Forest Healing Anti-Aging Program
There was a significant difference in the MMSE scores (p < 0.05). There were significant differences between the pre- and post-measurements and between the post- and follow-up measurements (p < 0.017).
The BDI score was significantly different (p < 0.05). There were significant differences between the pre- and post-measurements and between the pre- and follow-up measurements (p < 0.05).
Among the POMS subcategories, there were significant differences in DD, AH, FI, and TMD (p < 0.05). DD, FI, and TMD had a significant difference between the pre- and post-measurements, and the items with a significant difference between pre- and follow-up measurements were DD, AH, FI, and TMD (DD, AH, TMD: p < 0.017; FI: p < 0.05).
Among the subcategories of the WHOQOL-BREF, there were significant differences in OG, PH, and SR (p < 0.05). The item with a significant difference between pre- and post-measurements was SR, and the items with significant differences between the pre- and follow-up measurements were OG and PH (OG, SR: p < 0.017; PH: < 0.05).
In the total PSQI score, there was a significant difference between the pre- and follow-up measurements (p < 0.05). There were no significant differences in the sub-items of the PSQI (p > 0.05) (Table 4).

Table 4.
Effect of psychological variables.
3.2.2. Physiological Effects of the Forest Healing Anti-Aging Program
There was no significant difference in all variables of vital signs (p > 0.05).
The body composition showed significant differences in the pre- and post-measurements and in the post- and follow-up measurements in all variables (p < 0.05).
Blood analysis revealed a significant difference in the cortisol levels (p < 0.05) (Table 5).

Table 5.
Effect of physiological variables.
3.2.3. Physical Effects of the Forest Healing Anti-Aging Program
Among the sub-items of SFT, there were significant differences between the pre- and post-measurements and between the pre- and follow-up measurements in AC, CS, 2SW, and 8UG (p < 0.05).
Among the dynamometer results, there were significant differences in EF, KE, and APF (p < 0.05). The items with significant differences between pre- and post-measurements were EF, KE, and APF, and the items with significant differences between pre- and follow-up measurements were EF and KE (EF, KE, APF: p < 0.05).
Significant differences were observed in all spatiotemporal gait variables (p < 0.05). The post hoc analysis showed a significant difference between the pre- and post- measurements in all variables, and the items with a significant difference between the pre- and follow-up measurements were swing time and stance time. The items that were present were step length and stride length (velocity, step length, stride length, swing time: p < 0.05; cadence, step time, stance time, cycle time: p < 0.017).
In the modified FRT, there was a significant difference between the pre- and post-measurements in the right and left directions (p < 0.05) (Table 6).

Table 6.
Effect of physical variables.
4. Discussion
This study was conducted to investigate the effects of the forest healing anti-aging program on the psychological, physiological, and physical health of older people with MCI, and the following results were obtained. First, the forest healing anti-aging program improved the psychological health of older people with MCI. Second, the forest healing anti-aging program improved the physiological health of older people with MCI. Third, the forest healing anti-aging program improved the physical health of older people with MCI.
4.1. Effects of Forest Healing Anti-Aging Program on Psychological Health
A study by Yu and Hsieh showed that the cognitive ability of participants who participated in a three-day forest healing workshop improved by 27.74% [37]. Similarly, the forest healing program improved scores in measures of cognitive ability of older people with mild cognitive impairment by 5.1%. Moreover, as the scores of BDI and DD of POMS decreased significantly, it was found that the forest healing anti-aging program was effective in improving depression in older people. Depression in older people tends to increase due to a decrease in physical health that occurs with increasing age, which may lead to a decrease in social relationships and QOL [38]. The participants experienced a new forest environment where they could experience various sensory stimuli (visual, auditory, and proprioceptive senses) outside the city where they normally live. In addition, to solve the task, group activities were performed through interactions with various people, and insufficient social relationships improved. Through these activities, participants were able to relieve negative emotions and obtain emotional stability, which was shown to improve the POMS and WHOQOL.
In the case of the PSQI, there was no significant difference in the sub-items but there was a significant change in the total score. Similarly, in a previous study, there was no significant change in PSQI when forest healing was performed over five nights and six days for cancer patients, but an increase in sleep time and sleep efficiency was found in the polysomnograph for evaluating sleep records [39]. In a previous study, the time spent in the forest per session was longer than that in our study; therefore, it was easy for the participants to adapt to the environment, and it seems that a positive effect was shown in the sleep record, which is a more objective indicator. In addition, among the participants in this study, those who were taking sleeping pills expressed that they experienced an increase in overall sleep quality, for example, they said that the drug dose decreased, or they stopped taking the drug after the forest healing intervention. Therefore, it is necessary to investigate the effect of the program on psychological health through adjustment for the intervention period and composition in a follow-up study.
4.2. Effect of Forest Healing Anti-Aging Program on Physiological Health
In terms of body composition, the skeletal muscle mass and total body water increased, and fat mass decreased. This seems to be because the amount of physical activity increased throughout the program. A decrease in physical activity in the older population decreases skeletal muscle mass and increases fat mass, thereby increasing the probability of sarcopenia and obesity [40]. A vicious cycle leading to physical deterioration can accelerate cognitive decline by lowering brain activity [41].
In factors related to muscle and stress in the blood, cortisol, a stress hormone, was significantly reduced, indicating that the forest healing program was effective in reducing the stress level of the participants. In previous studies, decreased cortisol levels were associated with greater exposure to forest environments, and older people experienced a decrease in cortisol levels after low-to-moderate exercise [42,43]. Although the participant’s baseline CRP level did not show a significant change due to the low value (1.07 mg/L) with a high standard deviation, CRP also showed a tendency to decrease. A positive effect of the anti-aging forest healing program can be expected through the tendency to decrease CRP, a plasma biomarker that is significantly related to chronic stress and cardiovascular disease. In the case of cathepsin B and IGF-1 related to cognitive function, there was no significant change, but there was a tendency to increase; therefore, a follow-up study is needed to investigate the effectiveness through the modification of the intervention period and intensity.
4.3. Effects of Forest Healing Anti-Aging Program on Physical Health
In this study, the forest healing anti-aging program significantly improved the functional fitness, muscle strength, gait function, and dynamic balance ability of the participants. Interestingly, to the best of our knowledge, no studies have investigated the effects of forest healing on physical health. This study is the first attempt to identify this, and there are limitations in comparing the effectiveness of this study with other studies.
The participants of this study were 60-year-olds who exercised for 300 min or less per week. The forest healing anti-aging program involved a physical activity-based task in the mountains for approximately 376 min for two days per session. Various inclinations and irregular surfaces, walking speeds, and physical activity with others would have improved the participants’ motor functions. In particular, the WHO recommends that moderate-intensity aerobic physical activity of 300 min or more per week has health benefits [44].
In this study, participants who experienced forest healing showed improvements in functional fitness by improving upper and lower extremity muscle strength, endurance, dynamic balance, and muscle strength of the elbow flexor, knee extensor, and ankle plantar flexor muscles. In addition, gait time, length, and velocity significantly improved, and dynamic balance in the sitting position increased. These results are presumed to induce improvement in various motor functions because the physical activity-based forest healing anti-aging program consists of various activities that require whole-body movement.
Kozakai et al. reported that an increase in leisure-time physical activity can improve muscle function in middle-aged and older populations [45]. Mountain hiking, which is a type of leisure, can have a great influence on proprioceptive sensory input because the slope, altitude, and ground conditions change every moment [46]. However, there was no significant improvement in some physical health factors (flexibility, grip strength, pinch grip strength, static balance, etc.). This is presumably because the program provided in this study consisted of movements that require gait and global muscle activity of the trunk and lower extremities rather than specific movements that require functional movements of the hands, flexibility, and static balance.
4.4. Sustainability of Forest Healing Program Effects
In psychological health, the follow-up effect was maintained in most variables, but in the MMSE, the effect was significantly reduced, and there was no difference from before the intervention (p > 0.017). In terms of physiological health, body composition, which showed a significant improvement in all variables immediately after the intervention, returned to the same level as that before the intervention (p > 0.017). Continuous activity is required to improve and maintain cognitive function and body composition in the older population with MCI. However, the improvement in most of the physical health indicators was found to remain effective after one month.
4.5. Significance and Limitations of This Study
Studies have demonstrated the psychological and physiological effects of forest healing applied to participants of various age groups, occupations, and diseases, but the identification of the physical effects has been insufficient. This study is valuable as it is the first study to simultaneously identify the psychological, physiological, and physical effects of applying a forest healing program to older people with MCI.
However, this study had several limitations. First, no control group could be compared with the forest healing program group in this study. As the intervention used in this study consists of an individual program that maximizes forest resources, it is difficult to apply the same intervention in an urban environment. Therefore, to explain the effect of this intervention, the setting of a control group for the same program, excluding only environmental factors, is required. Second, comparison with the urban forest environment was limited. This study was conducted in a facility designed to be suitable for the implementation of a forest healing program located in a high-altitude and forested environment, which would have provided the participants living in the city an opportunity to experience a completely new environment and activities. Therefore, it is necessary to verify whether this intervention has the same effect in an urban forest environment. Third, although 22 participants were targeted through sample size calculation, there is a limitation in generalizing the study results because of the small sample size. Fourth, blood analysis was performed only in the second pre-measurement and post-measurement. Therefore, it cannot be confirmed in this study whether the changes in blood analysis persist until one month later. Finally, this study did not clearly identify the effects of atmospheric, weather, and seasonal factors of forest healing on the psychological, physiological, and physical health of participants. In particular, the healthy effects of the different levels of biogenic volatile organic compounds (BVOCs) in the forest atmosphere were not investigated. As per previous studies, exposure to BVOCs was deemed to produce remarkable effects on human health [47]. Thus, these factors could be potential factors that can affect the effectiveness of forest healing, which we will elucidate in future studies.
5. Conclusions
The forest healing anti-aging program increased cognitive ability, decreased the degree of depression, and improved mood and sleep disturbances in older people with MCI. It also positively affected body composition and reduced stress hormones. Finally, the functional fitness and muscle strength, gait, and dynamic balance abilities of the participants improved.
Author Contributions
Conceptualization, H.-Y.C. and M.-G.L.; Methodology, J.-E.B., S.-C.H. and J.-H.J.; Supervision, S.-C.H., H.-Y.C., and M.-G.L.; Project administration, J.-E.B., J.-H.J., H.-J.S., and S.-Y.S.; Formal analysis, H.-J.S. and S.-H.K.; Investigation, S.-J.P. and M.-G.L.; Data curation, J.-H.J. and S.-H.K.; Writing—original draft preparation, J.-E.B., J.-H.J., and H.-Y.C.; Writing—review and editing, H.-Y.C. and M.-G.L. All authors have read and agreed to the published version of the manuscript.
Funding
This work was supported by the National Institute of Forest Science (task number: FM0400-2018-03-2020) and by the Gachon University research fund of 2020 (GCU-202002880001).
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the Bioethics Review Committee of the Gachon University (1044396-202006-HR-111-02, 14 August 2020). The study was registered with the Clinical Research Information Service No. KCT0005365.
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
Appendix A

Table A1.
Reagent information.
Table A1.
Reagent information.
| Variables | Reagent Name | Cat.no | Manufacturer | Country of Manufacture | Analysis Equipment |
|---|---|---|---|---|---|
| Cathepsin-B (pg/mL) | Human Cathepsin B | MBS175975 | Mybiosource | USA | spectramax190 |
| Cortisol (ug/dL) | Cortisol II | 7027150190 | Roche | Germany | cobas e801 |
| IGF-1 (ng/mL) | IGF | L2KIGF2 | Siemens | USA | Immulite xpi 2000 |
| CRP (mg/L) | CRPHS | 04628918190 | Roche | Germany | Cobas c502 |
IGF-1, insulin-like growth factor; CRP, C-reactive protein.

Table A2.
Differences between first and second pre-measurements.
Table A2.
Differences between first and second pre-measurements.
| Variables | Pre 1 | Pre 2 | p-Value |
|---|---|---|---|
| Psychological variables | |||
| MMSE (score) | 26.41 ± 0.67 | 26.64 ± 0.79 | 0.132 b |
| BDI (score) | 8.68 ± 5.69 | 8.36 ± 5.12 | 0.530 a |
| POMS (score) | |||
| Tension-Anxiety | 9.00 ± 5.44 | 8.73 ± 4.10 | 0.835 a |
| Depression-Dejection | 12.41 ± 9.42 | 12.27 ± 9.64 | 0.972 b |
| Anger-Hostility | 6.86 ± 6.74 | 7.00 ± 5.85 | 0.875 b |
| Fatigue-Inertia | 7.50 ± 5.20 | 7.36 ± 4.93 | 0.858 a |
| Confusion-Bewilderment | 8.41 ± 5.15 | 8.23 ± 4.02 | 0.838 a |
| Vigor-Activity | 18.64 ± 6.04 | 18.41 ± 6.08 | 0.789 a |
| Total mood disturbance | 25.55 ± 27.71 | 25.18 ± 24.86 | 0.715 b |
| WHOQOL-BREF (score) | |||
| Overall QOL and General health | 6.59 ± 1.22 | 6.45 ± 1.26 | 0.477 b |
| Physical health | 23.05 ± 3.37 | 23.18 ± 4.00 | 0.583 b |
| Psychological | 17.23 ± 3.16 | 18.23 ± 3.05 | 0.090 a |
| Social relationship | 9.68 ± 1.39 | 9.09 ± 1.15 | 0.097 b |
| Environmental | 24.91 ± 5.10 | 24.68 ± 4.70 | 0.795 a |
| Total | 81.45 ± 11.59 | 81.64 ± 12.45 | 0.916 a |
| PSQI (score) | |||
| Sleep quality | 1.23 ± 0.81 | 1.23 ± 0.61 | 1.000 b |
| Sleep latency | 1.45 ± 1.18 | 1.45 ± 0.80 | 1.000 b |
| Sleep duration | 0.45 ± 0.60 | 0.41 ± 0.67 | 0.564 b |
| Habitual sleep efficiency | 0.41 ± 0.91 | 0.36 ± 0.85 | 0.887 b |
| Sleep disturbance | 1.36 ± 0.49 | 1.32 ± 0.57 | 0.763 b |
| Use of sleeping medication | 0.32 ± 0.89 | 0.23 ± 0.69 | 0.317 b |
| Daytime dysfunction | 1.36 ± 1.00 | 1.45 ± 0.74 | 0.527 b |
| Total | 6.59 ± 3.63 | 6.45 ± 3.04 | 0.825 a |
| Physiological variables | |||
| Vital signs | |||
| Systolic pressure (mmHg) | 126.45 ± 15.05 | 128.55 ± 12.63 | 0.471 a |
| Diastolic pressure (mmHg) | 73.95 ± 9.06 | 74.59 ± 7.59 | 0.604 a |
| Pulse pressure (mmHg) | 52.50 ± 7.93 | 53.95 ± 8.39 | 0.550 a |
| Heart rate (bpm) | 75.09 ± 8.51 | 73.55 ± 11.71 | 0.478 a |
| Body compositions | |||
| Skeletal muscle mass (kg) | 22.90 ± 4.16 | 23.15 ± 4.03 | 0.082 b |
| Body fat mass (kg) | 19.31 ± 3.67 | 19.12 ± 3.61 | 0.110 a |
| Total body water (L) | 30.39 ± 5.32 | 30.55 ± 5.18 | 0.356 b |
| Blood compositions | |||
| Cathepsin-B (pg/mL) | - | 183497.71 ± 71436.06 | - |
| Cortisol (μg/dL) | - | 13.04 ± 3.31 | - |
| IGF-1 (ng/mL) | - | 121.40 ± 32.78 | - |
| CRP (mg/L) | - | 1.07 ± 0.87 | - |
| Physical variables | |||
| Senior Fitness Test | |||
| Arm curl (n) | 17.36 ± 3.67 | 17.68 ± 4.06 | 0.167 a |
| 30-sec chair stand (n) | 11.45 ± 3.60 | 11.73 ± 3.71 | 0.110 a |
| 2-min step walk (n) | 90.95 ± 13.44 | 92.50 ± 12.63 | 0.054 a |
| 8-ft up and go (sec) | 7.94 ± 1.38 | 7.71 ± 1.13 | 0.074 a |
| Back scratch (cm) | −8.84 ± 11.47 | −8.50 ± 10.81 | 0.955 b |
| Chair sit and reach (cm) | 12.25 ± 9.59 | 13.09 ± 6.41 | 0.945 b |
| Muscle strength | |||
| Elbow flexor (kg) | 12.50 ± 3.04 | 11.35 ± 3.61 | 0.051 a |
| Knee extensor (kg) | 13.30 ± 2.05 | 13.01 ± 1.85 | 0.118 a |
| Ankle plantar flexor (kg) | 13.42 ± 2.18 | 13.16 ± 2.08 | 0.087 a |
| Grip (kg) | 25.74 ± 7.40 | 25.52 ± 7.18 | 0.673 a |
| Pinch (kg) | 7.30 ± 1.48 | 7.12 ± 1.46 | 0.083 b |
| Spatiotemporal parameter of gait | |||
| Velocity (cm/s) | 117.91 ± 17.71 | 121.02 ± 16.19 | 0.083 a |
| Cadence (steps/min) | 117.92 ± 10.57 | 119.99 ± 10.08 | 0.059 a |
| Step length—Rt. (cm) | 60.07 ± 5.93 | 61.03 ± 5.14 | 0.180 a |
| Stride length—Rt. (cm) | 119.72 ± 11.25 | 121.06 ± 10.29 | 0.309 a |
| Step time—Rt. (sec) | 0.51 ± 0.05 | 0.50 ± 0.05 | 0.066 a |
| Swing time—Rt. (sec) | 0.39 ± 0.03 | 0.38 ± 0.03 | 0.155 a |
| Stance time—Rt. (sec) | 0.64 ± 0.07 | 0.62 ± 0.06 | 0.115 b |
| Cycle time—Rt. (sec) | 1.02 ± 0.10 | 1.01 ± 0.09 | 0.075 b |
| Static balance | |||
| EO-Sway area (mm2) | 1.52 ± 1.35 | 1.47 ± 0.87 | 0.835 b |
| EO-Sway velocity (mm/s) | 1.07 ± 0.30 | 1.11 ± 0.29 | 0.177 a |
| EC-Sway area (mm2) | 2.35 ± 2.40 | 3.13 ± 3.43 | 0.200 b |
| EC-Sway velocity (mm/s) | 1.54 ± 0.55 | 1.80 ± 0.78 | 0.057 b |
| Dynamic balance (cm) | |||
| Anterior | 49.87 ± 7.45 | 49.41 ± 12.18 | 0.861 a |
| Right | 30.66 ± 3.81 | 32.25 ± 3.07 | 0.073 a |
| Left | 28.50 ± 4.69 | 30.55 ± 5.46 | 0.058 a |
Data are expressed as mean ± SD; a, paired t-test; b, Wilcoxon signed-rank test; Pre 1, first pre-measurement; Pre 2, second pre-measurement; MMSE, mini-mental state examination; BDI, Beck depression inventory; POMS, profile of mood state; PSQI, Pittsburgh sleep quality index; Rt., right side; EO, eyes open; EC, eyes closed.
References
- Korean Statistical Information Service. Available online: https://kosis.kr/index/index.do (accessed on 10 January 2022).
- World Health Organization. Dementia. Available online: https://www.who.int/news-room/fact-sheets/detail/dementia (accessed on 10 January 2022).
- Kim, H.; Hong, J.P.; Kang, J.M.; Kim, W.; Maeng, S.; Cho, S.; Na, K.; Oh, S.H.; Park, J.W.; Cho, S.; et al. Cognitive Reserve and the Effects of Virtual Reality-based Cognitive Training on Elderly Individuals with Mild Cognitive Impairment and Normal Cognition. Psychogeriatrics 2021, 21, 552–559. [Google Scholar] [CrossRef] [PubMed]
- Ministry of Health and Welfare of South Korea. Mild Cognitive Impairment, A Stage before Dementia, Has Increased 4.3 Times in the Past 5 Years. Available online: https://www.korea.kr/news/pressReleaseView.do?newsId=156074845#sitemap-layer (accessed on 10 January 2022).
- Kabisch, N.; van den Bosch, M.; Lafortezza, R. The Health Benefits of Nature-Based Solutions to Urbanization Challenges for Children and the Elderly—A Systematic Review. Environ. Res. 2017, 159, 362–373. [Google Scholar] [CrossRef] [PubMed]
- White, M.P.; Alcock, I.; Grellier, J.; Wheeler, B.W.; Hartig, T.; Warber, S.L.; Bone, A.; Depledge, M.H.; Fleming, L.E. Spending at Least 120 Minutes a Week in Nature Is Associated with Good Health and Wellbeing. Sci. Rep. 2019, 9, 7730. [Google Scholar] [CrossRef] [PubMed]
- Barton, J.; Griffin, M.; Pretty, J. Exercise-, Nature- and Socially Interactive-Based Initiatives Improve Mood and Self-Esteem in the Clinical Population. Perspect. Public Health 2012, 132, 89–96. [Google Scholar] [CrossRef]
- Thompson Coon, J.; Boddy, K.; Stein, K.; Whear, R.; Barton, J.; Depledge, M.H. Does Participating in Physical Activity in Outdoor Natural Environments Have a Greater Effect on Physical and Mental Wellbeing than Physical Activity Indoors? A Systematic Review. Environ. Sci. Technol. 2011, 45, 1761–1772. [Google Scholar] [CrossRef]
- Choi, J.-H.; Shin, C.-S.; Yeoun, P.-S. Effects of Forest-Walking Exercise on Functional Fitness and Gait Pattern in the Elderly. J. Korean For. Soc. 2014, 103, 503–509. [Google Scholar] [CrossRef][Green Version]
- Korea Forest Service. Article 2, No. 4 of the Forest Culture and Recreation Act. Available online: https://www.law.go.kr/LSW/lsInfoP.do?lsId=010004#J2:0 (accessed on 10 January 2022).
- Korea Forest Welfare Institute. Forest Therapy. Available online: https://www.fowi.or.kr/user/contents/contentsView.do?cntntsId=39 (accessed on 10 January 2022).
- Hong, J.; Park, S.; Lee, J. Changes in Depression and Stress of the Middle-Aged and Older through Participation in a Forest Therapy Program for Dementia Prevention. J. People Plants Environ. 2019, 22, 699–709. [Google Scholar] [CrossRef]
- Kobayashi, H.; Song, C.; Ikei, H.; Park, B.-J.; Lee, J.; Kagawa, T.; Miyazaki, Y. Population-Based Study on the Effect of a Forest Environment on Salivary Cortisol Concentration. Int. J. Environ. Res. Public Health 2017, 14, 931. [Google Scholar] [CrossRef]
- Ochiai, H.; Ikei, H.; Song, C.; Kobayashi, M.; Miura, T.; Kagawa, T.; Li, Q.; Kumeda, S.; Imai, M.; Miyazaki, Y. Physiological and Psychological Effects of a Forest Therapy Program on Middle-Aged Females. Int. J. Environ. Res. Public Health 2015, 12, 15222–15232. [Google Scholar] [CrossRef]
- Ochiai, H.; Ikei, H.; Song, C.; Kobayashi, M.; Takamatsu, A.; Miura, T.; Kagawa, T.; Li, Q.; Kumeda, S.; Imai, M.; et al. Physiological and Psychological Effects of Forest Therapy on Middle-Aged Males with High-Normal Blood Pressure. Int. J. Environ. Res. Public Health 2015, 12, 2532–2542. [Google Scholar] [CrossRef]
- Song, C.; Ikei, H.; Kobayashi, M.; Miura, T.; Taue, M.; Kagawa, T.; Li, Q.; Kumeda, S.; Imai, M.; Miyazaki, Y. Effect of Forest Walking on Autonomic Nervous System Activity in Middle-Aged Hypertensive Individuals: A Pilot Study. Int. J. Environ. Res. Public Health 2015, 12, 2687–2699. [Google Scholar] [CrossRef] [PubMed]
- Lee, J.-Y.; Lee, D.-C. Cardiac and Pulmonary Benefits of Forest Walking versus City Walking in Elderly Women: A Randomised, Controlled, Open-Label Trial. Eur. J. Integr. Med. 2014, 6, 5–11. [Google Scholar] [CrossRef]
- Kim, J.Y.; Shin, C.S.; Lee, J.K. The Effects of Forest Healing Program on Mental Health and Melatonin of the Elderly in the Urban Forest. J. Korea Soc. Plants People Environ. 2017, 20, 95–106. [Google Scholar] [CrossRef]
- Zaudig, M. A New Systematic Method of Measurement and Diagnosis of “Mild Cognitive Impairment” and Dementia According to ICD-10 and DSM-III-R Criteria. Int. Psychogeriatr. 1992, 4, 203–219. [Google Scholar] [CrossRef] [PubMed]
- Park, J.H.; Park, S.H.; Lee, H.J.; Kang, J.W.; Lee, K.M.; Yeon, P.S. Study on NVOCs Concentration Characteristics by Season, Time and Climatic Factors: Focused on Pinus Densiflora Forest in National Center for Forest Therapy. J. People Plants Environ. 2018, 21, 403–409. [Google Scholar] [CrossRef]
- Kim, J.M.; Shin, I.S.; Yoon, J.S.; Lee, H.Y. Comparison of diagnostic validities between MMSE-K and K-MMSE for screening of dementia. J. Korean Neuropsychiatr. Assoc. 2003, 42, 124–130. [Google Scholar] [CrossRef]
- Song, Y.M.; Lee, H.K.; Kim, J.W.; Lee, K. Reliability and validity of the Korean Version of Beck Depression Inventory-II via the internet: Results from a university student sample. J. Korean Neuropsychiatr. Assoc. 2012, 51, 402–408. [Google Scholar] [CrossRef]
- Kim, E.J.; Lee, S.I.; Jeong, D.U.; Shin, M.S.; Yoon, I.Y. Standardization and reliability and validity of the Korean edition of Profile of Mood States (K-POMS). Sleep Med. Psychophysiol. 2003, 10, 39–51. [Google Scholar]
- Min, S.K.; Lee, C.I.; Kim, K.I.; Suh, S.Y.; Kim, D.K. Development of Korean version of WHO quality of life scale abbreviated version (WHOQOL-BREF). J. Korean Neuropsychiatr. Assoc. 2000, 39, 571–579. [Google Scholar]
- Sohn, S.I.; Kim, D.H.; Lee, M.Y.; Cho, Y.W. The Reliability and Validity of the Korean Version of the Pittsburgh Sleep Quality Index. Sleep Breath. 2012, 16, 803–812. [Google Scholar] [CrossRef]
- Kim, B.; Kang, S. Regular Leisure-Time Physical Activity Is Effective in Boosting Neurotrophic Factors and Alleviating Menopause Symptoms. Int. J. Environ. Res. Public Health 2020, 17, 8624. [Google Scholar] [CrossRef] [PubMed]
- Nobari, H.; Kargarfard, M.; Minasian, V.; Cholewa, J.M.; Pérez-Gómez, J. The Effects of 14-Week Betaine Supplementation on Endocrine Markers, Body Composition and Anthropometrics in Professional Youth Soccer Players: A Double Blind, Randomized, Placebo-Controlled Trial. J. Int. Soc. Sports Nutr. 2021, 18, 20. [Google Scholar] [CrossRef] [PubMed]
- Widmer, I.E.; Puder, J.J.; König, C.; Pargger, H.; Zerkowski, H.R.; Girard, J.; Müller, B. Cortisol Response in Relation to the Severity of Stress and Illness. J. Clin. Endocrinol. Metab. 2005, 90, 4579–4586. [Google Scholar] [CrossRef] [PubMed]
- Hapuarachchi, J.R.; Chalmers, A.H.; Winefield, A.H.; Blake-Mortimer, J.S. Changes in Clinically Relevant Metabolites with Psychological Stress Parameters. Behav. Med. 2003, 29, 52–59. [Google Scholar] [CrossRef] [PubMed]
- Jeon, S.; Kim, J. Effects of Augmented-Reality-Based Exercise on Muscle Parameters, Physical Performance, and Exercise Self-Efficacy for Older Adults. Int. J. Environ. Res. Public Health 2020, 17, 3260. [Google Scholar] [CrossRef]
- Hesseberg, K.; Bentzen, H.; Bergland, A. Reliability of the Senior Fitness Test in Community-Dwelling Older People with Cognitive Impairment. Physiother. Res. Int. 2015, 20, 37–44. [Google Scholar] [CrossRef]
- Bohannon, R.W. Test-Retest Reliability of Hand-Held Dynamometry during a Single Session of Strength Assessment. Phys. Ther. 1986, 66, 206–209. [Google Scholar] [CrossRef]
- Lindstrom-Hazel, D.; Kratt, A.; Bix, L. Interrater Reliability of Students Using Hand and Pinch Dynamometers. Am. J. Occup. Ther. 2009, 63, 193–197. [Google Scholar] [CrossRef]
- Van Uden, C.J.; Besser, M.P. Test-Retest Reliability of Temporal and Spatial Gait Characteristics Measured with an Instrumented Walkway System (GAITRite®). BMC Musculoskelet. Disord. 2004, 5, 13. [Google Scholar] [CrossRef]
- Swanenburg, J.; de Bruin, E.D.; Favero, K.; Uebelhart, D.; Mulder, T. The Reliability of Postural Balance Measures in Single and Dual Tasking in Elderly Fallers and Non-Fallers. BMC Musculoskelet. Disord. 2008, 9, 162. [Google Scholar] [CrossRef]
- Thompson, M.; Medley, A. Forward and Lateral Sitting Functional Reach in Younger, Middle-Aged, and Older Adults. J. Geriatr. Phys. Ther. 2007, 30, 43–48. [Google Scholar] [CrossRef] [PubMed]
- Yu, C.-P.; Hsieh, H. Beyond Restorative Benefits: Evaluating the Effect of Forest Therapy on Creativity. Urban For. Urban Green. 2020, 51, 126670. [Google Scholar] [CrossRef]
- Gurland, B. The Impact of Depression on Quality of Life of the Elderly. Clin. Geriatr. Med. 1992, 8, 377–386. [Google Scholar] [CrossRef]
- Kim, H.; Lee, Y.W.; Ju, H.J.; Jang, B.J.; Kim, Y.I. An Exploratory Study on the Effects of Forest Therapy on Sleep Quality in Patients with Gastrointestinal Tract Cancers. Int. J. Environ. Res. Public Health 2019, 16, 2449. [Google Scholar] [CrossRef]
- Tyrovolas, S.; Koyanagi, A.; Olaya, B.; Ayuso-Mateos, J.L.; Miret, M.; Chatterji, S.; Tobiasz-Adamczyk, B.; Koskinen, S.; Leonardi, M.; Haro, J.M. Factors Associated with Skeletal Muscle Mass, Sarcopenia, and Sarcopenic Obesity in Older Adults: A Multi-Continent Study. J. Cachexia Sarcopenia Muscle 2016, 7, 312–321. [Google Scholar] [CrossRef]
- Erickson, K.I.; Hillman, C.H.; Kramer, A.F. Physical Activity, Brain, and Cognition. Curr. Opin. Behav. Sci. 2015, 4, 27–32. [Google Scholar] [CrossRef]
- Kobayashi, H.; Song, C.; Ikei, H.; Park, B.-J.; Lee, J.; Kagawa, T.; Miyazaki, Y. Forest Walking Affects Autonomic Nervous Activity: A Population-Based Study. Front. Public Health 2018, 6, 278. [Google Scholar] [CrossRef]
- Taha, M.M.; Mounir, K.M. Acute Response of Serum Cortisol to Different Intensities of Resisted Exercise in the Elderly. Bull. Fac. Phys. Ther. 2019, 24, 20–25. [Google Scholar] [CrossRef]
- World Health Organization. Physical Activity. Available online: https://www.who.int/news-room/fact-sheets/detail/physical-activity (accessed on 10 January 2022).
- Kozakai, R.; Doyo, W.; Tsuzuku, S.; Yabe, K.; Miyamura, M.; Ikegami, Y.; Niino, N.; Ando, F.; Shimokata, H. Relationships of Muscle Strength and Power with Leisure-Time Physical Activity and Adolescent Exercise in Middle-Aged and Elderly Japanese Women. Geriatr. Gerontol. Int. 2005, 5, 182–188. [Google Scholar] [CrossRef]
- Prossegger, J.; Huber, D.; Grafetstätter, C.; Pichler, C.; Weisböck-Erdheim, R.; Iglseder, B.; Wewerka, G.; Hartl, A. Effects of Moderate Mountain Hiking and Balneotherapy on Community-Dwelling Older People: A Randomized Controlled Trial. Exp. Gerontol. 2019, 122, 74–84. [Google Scholar] [CrossRef]
- Antonelli, M.; Donelli, D.; Barbieri, G.; Valussi, M.; Maggini, V.; Firenzuoli, F. Forest Volatile Organic Compounds and Their Effects on Human Health: A State-of-the-Art Review. Int. J. Environ. Res. Public Health 2020, 17, 6506. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).