Abstract
Multiple long-term conditions (MLTCs) are influenced in extent and nature by social determinants of health. Few studies have explored associations between household tenure and different definitions of MLTCs. This study aimed to examine associations between household tenure and MLTCs amongst working-age adults (16 to 64 years old, inclusive). This cross-sectional study used the 2019–2020 wave of an innovative dataset that links administrative data across health and local government for residents of a deprived borough in East London. Three definitions of MLTCs were operationalised based on a list of 38 conditions. Multilevel logistic regression models were built for each outcome and adjusted for a range of health and sociodemographic factors. Compared to working-age owner-occupiers, odds of basic MLTCs were 36% higher for social housing tenants and 19% lower for private renters (OR 1.36; 95% CI 1.30–1.42; p < 0.001 and OR 0.81, 95% CI 0.77–0.84, p < 0.001, respectively). Results were consistent across different definitions of MLTCs, although associations were stronger for social housing tenants with physical-mental MLTCs. This study finds strong evidence that household tenure is associated with MLTCs, emphasising the importance of understanding household-level determinants of health. Resources to prevent and tackle MLTCs among working-age adults could be differentially targeted by tenure type.
1. Introduction
The co-occurrence of multiple long-term conditions (MLTCs) within a single individual is a major public health challenge both globally and in the UK. The nature and extent of MLTCs is influenced by social determinants of health (SDoH) []. The role of individual- and area-level social determinants has been widely reported—prevalence and incidence of MLTCs are greater with increasing age, for women, for ethnic minorities, and those living with greater socioeconomic deprivation [,,,,,]. Yet recent evidence suggests that household-level SDoH (such as household tenure) are often overlooked as determinants of MLTCs despite comparatively large effect sizes for household compared to area-level SDoH []. In their landmark report, the Academy of Medical Sciences (AMS) concluded that most evidence focuses on “population or individual-level” determinants and that “it will be valuable to consider whether factors that operate at the household-level can also influence MLTCs” []. In addition, exploring these relationships amongst working-age adults has received little attention [,,]. This is despite recent evidence that suggests the median age of onset of MLTCs decreased from 56 years in 2004 to 46 years in 2019 [].
Household tenure—whether someone privately rents their home, rents from social housing, or owner-occupies—is widely considered a SDoH []. In recent years, homeownership in England has increased amongst older adults and decreased in mid-life, with the private rental market increasingly housing working-age adults []. First introduced in 1980, the UK Government’s Right to Buy policy and its future iterations enabled some more wealthier social housing tenants to legally buy their properties at a discount, resulting in tenure types more segregated by economic status and social class []. Different tenure types are thought to influence health through differences in exposure to various household- and area-level stressors, such as household overcrowding and access to green space [,,]. However, studies examining associations between household tenure and MLTCs report mixed results, have not explored associations in the English context and have not examined interactions between tenure and other household-level sociodemographic circumstances []. This is important as evidence suggests that context-specific factors such as degree of homeownership, and supply and conditions of rented housing may profoundly influence the meaning associated with residing in different tenures across geographies and over time [,,,].
Using an innovative dataset linking data from local government, health and social care, this study aimed to examine and quantify associations between household tenure and MLTCs amongst working-age adults residing in a deprived borough of East London.
2. Materials and Methods
2.1. Study Design, Data Source and Participants
This cross-sectional study uses the Care City Cohort, which links administrative health and social data across local government services, health providers, and health commissioners for residents of Barking and Dagenham (LBBD) []. Data are linked at both individual and household levels. LBBD is a deprived, outer borough of East London, with approximately 211,988 residents and a younger and more ethnically diverse population compared to the rest of England []. See Appendix A for an overview of the dataset and data linkage steps. This manuscript was prepared following the RECORD checklist [].
This study used a cross-section of the primary care and local government data taken on 1st April 2019. Individuals were included if they were of working age (between 16 and 64 years old, inclusive) [], identified as residents of the borough by Mayhew and Harper’s Residents’ Matrix [], and were not living in a residential home.
2.2. Outcome Measures: MLTCs
MLTCs status was determined based on the presence or absence of 38 long-term conditions recorded in a participant’s primary care record. Flags of these conditions were derived using publicly available code lists [].
This study operationalised three definitions of MLTCs in consultation with patients and clinicians:
- Basic MLTCs, the co-occurrence of two or more long-term conditions within a single individual;
- Physical-mental MLTCs, the co-occurrence of two or more long-term conditions within a single individual, one of which must be depression or anxiety and one of which must be a physical condition;
- Complex MLTCs, the co-occurrence of three or more long-term conditions affecting three or more different bodily systems within a single individual [].
The third definition was operationalised as conditions originating from different bodily systems are thought to be harder to treat due to different origins and/or treatment plans [,]. See Table A2 for the 38 conditions, how these conditions were grouped by bodily system and their distribution across the study cohort. Binary variables were created to indicate the presence or absence of each MLTCs outcome for each participant.
2.3. Main Exposure: Household Tenure
Individuals were defined as “owner-occupiers” if living in an owner-occupied household (outright or with a mortgage), “private renters” if living in a privately rented property, or “social housing tenants” if living in a socially rented household (from local government or a housing association). A fourth “unknown” category was created to account for missing data. Data on tenure were extracted from the council’s housing data systems.
2.4. Covariates
Data on age and sex were extracted from primary care records. Eight categories were created to code individuals’ ages in years (<16, 16–29, 30–44, 45–54, 55–64, 65–74, 75–84, and 85+). Sex was coded as male or female. Data on ethnicity were extracted from council records and coded into five categories: “White”, “Black”, “Asian”, “Other” and “Unknown”. Data on BMI and smoking status were extracted from primary care records. BMI was coded into five categories defined by the NHS as follows: underweight (below 18.5), healthy (between 18.5 and 24.9), overweight (between 25 and 29.9), obese (between 30 and 39.9) and morbidly obese (over 40), with a sixth “unknown” category to account for missing data. Smoking status data were coded into four categories: non-smoker, smoker, ex-smoker, or “unknown”.
Data on household welfare benefits, occupancy and household type were extracted from council housing records. Households receiving welfare benefits to support rental payments (‘housing benefit’) were classified by whether eligibility was based on receipt of other welfare benefits and, if so, the type: Employment Support and Allowance (ESA), Pension Credit, Income Support or Job Seeker’s Allowance (JSA). Two further categories reflecting households solely in receipt of housing benefit or in receipt of no benefits were created. Occupancy data were recorded into four categories to reflect 1–2, 3–5, 6–10 and 11 or more people within a household. Data on household type captured households as six types: adults with children, adults with no children, single adult with children, single adult, older adults with no children, and three generations.
To provide a marker of overall deprivation in each participants’ residential area relative to other areas in the borough, borough-specific Index of Multiple Deprivation (IMD) quintiles were calculated for each small geographical area (Lower Super Output Area; LSOA) using 2019 IMD scores []. Each LSOA comprised a maximum of 3000 residents and 1200 households [].
2.5. Main Data Analysis
Multilevel logistic regression modelling was used to explore associations between household tenure and MLTCs prevalence amongst working-age residents with complete data (see Table 1 and Figure A1). To assess the relative impact of adjusting for individual compared to household-level covariates on the association between tenure and MLTCs prevalence, we built three distinct models for each outcome. First, an unadjusted model with no covariates included. Second, a model adjusted for individual-level sociodemographic characteristics available in the dataset and found to be associated with both MLTCs prevalence and household tenure in previous literature [,,,]. These covariates were age, sex, ethnicity, BMI and smoking. The third and final model for each outcome additionally adjusted for household benefits receipt, occupancy and type to control for potential household-level factors correlated with both household tenure and MLTCs (see covariates above). We chose to adjust for household benefits receipt as it was the best proxy measure available in the dataset for other important covariates such as employment. We chose to adjust for household occupancy and type as a previous systematic review examining household- and area-level social determinants of MLTCs found these factors were associated with MLTCs prevalence in some contexts []. Model fit was assessed using Akaike’s Information Criteria (AIC). We considered multilevel models to account for the potential clustering of individuals within geographical areas, as individuals are likely to be more similar in terms of individual, household- and area-level factors if residing in the same areas than if residing in different areas. All models included random effects at the Lower Layer Output Area (LSOA) level to account for clustering within areas. Models were estimated using the lme4 package in R, using restricted maximum likelihood []. The 95% confidence intervals were calculated using the Wald test [].

Table 1.
Characteristics of study participants (N = 132,296).
2.6. Subgroup and Sensitivity Analyses
Three interaction terms were separately added to the final model for each outcome to evaluate potential interactions between household tenure and other household factors. We assessed interactions with receipt of benefits, household occupancy and type (see covariates above) as these are most likely to modify the association between housing tenure and MLTCs, and they also act at the household-level. Any differences in these household-level characteristics by tenure type can be found in Table A3.
3. Results
3.1. Participant Characteristics
Of the 232,671 participants whose primary care and local government records were successfully linked, 132,296 participants were eligible for inclusion in this study. A total of 78,379 records (33.7%) were excluded as individuals were not of working age, 21,847 records (9.39%) were excluded due to unconfirmed resident status and 95 were excluded due to living in a residential home (0.04%) (see Figure A1).
The 132,296 study participants resided in 59,535 households and 110 LSOAs. Table 1 gives an overview of the study participants. A total of 86,770 participants (65.6%) were between the ages of 16 and 44 years old and 68,004 (51.4%) were female. A total of 69,611 (52.6%) were of White ethnicity and 68,631 (51.8%) were overweight, obese or morbidly obese. A total of 54,324 participants (41.1%) were owner-occupiers, 39,885 (30.1%) were private renters and 35,776 (27.0%) were social housing tenants. Crude prevalence of basic, physical-mental, and complex MLTCs was 17.9% (23,683/132,296), 4.7% (6269/132,296) and 6.0% (7931/132,296), respectively.
The number of participants with missing data on tenure, ethnicity, BMI, and smoking status were 2311 (1.75%), 514 (0.39%), 25,415 (19.2%) and 13,054 (9.87%), respectively. A total of 102,430 participants had complete data across all variables and were included in analyses (see Figure A1).
3.2. Household Tenure and MLTCs
After adjusting for individual-level characteristics (age, sex, ethnicity, BMI, and smoking), social housing tenants were more likely to have basic MLTCs (OR 1.90; 95% CI 1.83–1.98), physical-mental MLTCs (OR 2.60, 95% CI 2.43–2.79,) and complex MLTCs (OR 2.23, 95% CI 2.10–2.37) when compared to owner-occupiers (Table 2). For private renters, there was no evidence of a difference in the odds of basic MLTCs compared to owner-occupiers (p = 0.630). Conversely, private renters were more likely to have physical-mental and complex MLTCs when compared to owner-occupiers (physical-mental MLTCs: OR 1.29, 95% CI 1.19–1.40; complex MLTCs: OR 1.16, 95% CI 1.08–1.25).

Table 2.
Estimated odds ratios of multiple long-term conditions (MLTCs) with household tenure for working-age adult residents with complete data (N = 102,430).
After additional adjustment for household-level characteristics (benefits receipt, occupancy, and household type), social housing tenants were still more likely to have MLTCs compared to owner-occupiers, but associations were weaker for all three definitions of MLTCs (basic MLTCs: OR 1.36, 1.30–1.42; physical-mental MLTCs: OR 1.46, 95% CI 1.35–1.58; complex MLTCs: OR 1.34; 95% CI 1.25–1.44). On the other hand, private renters were less likely to have basic MLTCs (OR 0.81, 95% CI 0.77–0.84), physical-mental MLTCs (OR 0.85, 95% CI 0.78–0.93) and complex MLTCs (OR 0.81, 95% CI 0.74–0.87) (Table 2). IMD quintiles were not included in final models for the three MLTCs outcomes as adding these resulted in poorer model fit.
3.3. Subgroup Analyses
Our subgroup analyses suggest subgroup effects according to household benefits receipt, occupancy and household type (see Table A4, Table A5 and Table A6). The odds of MLTCs for private renters (compared to owner-occupiers) were considerably stronger for households in receipt of benefits compared to those not receiving benefits. For example, odds of basic MLTCs were 76% greater for privately rented households where someone was in receipt of ESA compared to households not receiving ESA (OR 1.76, 95% CI 1.35–2.29). There was no evidence of an interaction between living in social housing and household benefits receipt (see Table A4). The odds of MLTCs for both social housing tenants and private renters (compared to owner-occupiers) were higher for single-adult households compared to households with adults and children. For example, the odds of basic MLTCs for social housing tenants compared to owner-occupiers were 31% greater for single-adult households (OR 1.31, 95% CI 1.15–1.50). Evidence for subgroup effects for other household types were weaker, with most interactions not statistically significant (see Table A6).
4. Discussion
4.1. Summary of Study Findings
Risk of MLTCs amongst working-age residents of a deprived East London borough was greater for social housing tenants and lower for privately renters, when compared to owner-occupiers. These associations remained significant after adjusting for a range of individual- and household-level characteristics and were consistent across different definitions of MLTCs. Other household-level variables—household benefits receipt, occupancy, and type—were important modifying factors, with associations between tenure and MLTCs greater for individuals in single-adult households and households in receipt of certain benefits.
4.2. Comparisons with Existing Literature
Our prevalence estimates are in keeping with previous estimates for this age group [,,,]. Prevalence of MLTCs was greater with increasing age and for females, consistent with previous literature [,]. However, prevalence was lower for ethnic minority compared with White participants, which contradicts many studies and may be an age-related effect [,,]. In this study, participants lived in a deprived borough in East London where older and younger individuals tend to be White and ethnic minorities, respectively.
We found that social housing tenants exhibited greater risk of MLTCs compared to owner-occupiers, aligning with findings from Northern Ireland yet contradicting those from a Hong Kong-based study [,]. This supports the idea that associations between household-level SDoH and MLTCs may be context specific, influenced by housing policy, supply and conditions of social housing, stigma and other household circumstances such as benefits receipt (see Table A3) []. In the UK specifically, social housing tenants may be exposed to various “hard” (material) and “soft” (psychological) factors that interact to cause or exacerbate MLTCs []. Evidence suggests social housing tenants in the UK have higher levels of C-reactive protein, a biomarker of inflammation associated with various long-term conditions [,]. In addition, social housing tenants have less control over the condition of their property and their built environment, and are less able to leave their property, whilst owner-occupying affords ontological security—the sense of security and control afforded when owning your home [,]. On top of this, the UK Housing Act (1998) requires social housing to be allocated based on certain criteria, one of which is ill health. As such, MLTCs may be a qualifying characteristic for eligibility for social housing, which may explain our estimated associations.
The lower risk of MLTCs found for private renters compared to owner-occupiers contradicts previous research from the US and Northern Ireland [,]. Our analyses adjusted for variables not adjusted for in these studies—household benefits receipt, occupancy, and household type. Our findings suggest these were important explanatory factors for the association between tenure and MLTCs, but they did not explain all of the additional risk experienced by social housing tenants, nor the decreased risk for private renters. In the UK, the private rental market is expanding considerably, and private renters are an increasingly heterogenous group in terms of their demographic, social and economic circumstances []. As such, more longitudinal, causal analyses are needed to unpick the complex relationships between different tenure types and MLTCs, taking into account the influence of other household characteristics.
We found that the association between tenure and MLTCs was greater for individuals in single-adult households and households with one or two occupants when compared to higher numbers of occupants. However, previous research examining associations between living alone and MLTC prevalence presents mixed results []. In our context, a deprived borough of East London, single-adult households may have less social support and be more financially uncertain than households with multiple occupants, increasing their vulnerability to any adverse effects imposed by their tenure []. We also found that the association between tenure and MLTCs was greater for individuals in households where someone was in receipt of certain benefits. Only one previous study has explored subgroup effects in the relationship between tenure and MLTCs and they similarly found that household financial burden mediated this relationship, albeit with a small effect []. Our findings support this work, and, again, suggest further research should capture data on, and account for, other household-level characteristics when examining relationships between tenure and MLTCs.
Differences in the risk of MLTCs with tenure type were not explained by commonly used area-level deprivation measures as most areas in our study are amongst the most deprived nationally []. These findings further demonstrate the importance of capturing data on, and understanding, household-level SDoH as this information could support service planning when area-level deprivation measures are unable to capture enough variation to model socioeconomic inequalities in MLTCs. In addition, our findings were consistent across different definitions of MLTCs, illustrating the importance of household tenure as a risk factor for MLTCs.
4.3. Strengths and Limitations
This is the first study to explore associations between household tenure and MLTCs in England. Our findings add to the current literature, and our analyses would not have been possible without the innovative linkage of primary care and local government data. We operationalised three definitions of MLTCs that captured different types of MLTCs with different degrees of complexity. We used publicly available code lists to determine the presence of each condition.
Our study was conducted in one deprived borough in East London and, whilst our findings could be generalisable to other urban areas, they may not hold in contexts that are less deprived, more rural and have different tenure profiles [,]. We restricted our analyses to complete cases, which assumes that any differences between individuals with missing and complete data are explained by differences in observed individual and household characteristics included in the regression models. We recognise that there may be other variables associated with the missing data that we have not adjusted for. However, this is unlikely to have significantly changed the results due to the limited role that BMI and smoking status have in the association between tenure and MLTCs prevalence []. We did not account for disease severity or symptom burden on the patient, or other dimensions of MLTCs such as frailty. We may have misclassified households where owner-occupiers privately rented rooms, which may have biased estimates towards the null if private renters who co-resided with their owner-occupying landlords differed systematically in their health compared to private renters who did not. In addition, our measure of household benefits receipt did not capture eligibility for benefits, and we could not adjust for other important factors such as education. The cross-sectional study design did not allow us to explore temporal relationships between tenure and MLTCs. We adjusted for household benefits receipt, occupancy, and household type as potential confounders, but also demonstrated important subgroup effects according to some of these characteristics. It is possible these variables may modify the relationship between tenure and MLTCs. More longitudinal analyses are needed to determine how these factors interact over time to impact MLTCs.
4.4. Implications for Practice and Policy
Most interventions for MLTCs focus on retired, older adults, yet our findings indicate that working-age adults are an important population to consider when aiming to address MLTCs. There is currently a gap in models of care or interventions aimed at working-age adults, for whom there may be greater opportunity for prevention of MLTCs through addressing SDoH than amongst older adults []. Initiatives that target preventative resources at working-age adults with MLTCs who live in social housing could slow the progression of MLTCs and improve health outcomes, ultimately saving future costs [].
5. Conclusions
This study finds strong evidence that risk of MLTCs amongst working-age residents of a deprived East London borough was greater for social housing tenants and lower for privately renters when compared to owner-occupiers. Associations were consistent across different definitions of MLTCs, which emphasises the importance of understanding and addressing household-level determinants of health. Our findings suggest that resources to prevent and tackle MLTCs could be differentially targeted by tenure type and that working-age adults are an important population to consider in preventative strategies. Further research should employ longitudinal research methods to assess temporal relationships between household social determinants and MLTCs.
Author Contributions
Conceptualisation, E.I., M.G., S.H., H.I.M., D.O. and J.S.; data curation, E.I.; formal analysis, E.I.; funding acquisition, J.S.; investigation, E.I.; methodology, E.I., M.G., H.I.M. and D.O.; project administration, E.I.; software, E.I.; supervision, M.G., S.H., H.I.M., D.O. and J.S.; writing—original draft, E.I.; writing—review and editing, E.I., M.G., S.H., H.I.M., D.O. and J.S. All authors have read and agreed to the published version of the manuscript.
Funding
This study is independent research funded by the National Institute for Health Research School for Public Health Research (Grant Reference Number PD-SPH -2015-10025) and the National Institute for Health Research Applied Research Collaboration (ARC) North Thames. The views expressed in this publication are those of the authors and not necessarily those of the National Institute for Health Research or the Department of Health and Social Care. The APC was funded by the National Institute for Health Research School for Public Health Research. DO is also supported by the National Institute for Health Research (NIHR) Biomedical Research Centre (BRC) at University College London Hospitals (UCLH).
Institutional Review Board Statement
This study was conducted in accordance with the Declaration of Helsinki. The study protocol was approved on 13th March 2020 by Care City’s formal process for data access (no project identification code provided).
Informed Consent Statement
Patient consent was waived as this work uses data provided by patients and collected by the NHS as part of their care and support. Only anonymised data were released.
Data Availability Statement
Restrictions apply to the availability of these data. Data were obtained from Care City and no applicable data are available without their permission. The study protocol is available on request.
Acknowledgments
The authors would like to thank Jenny Shand, Simon Lam and Phil Canham for their support with data access and their help with understanding the origins of the data. We would also like to thank Melvyn Jones, the Care City Community Board and the NIHR ARC North Thames Research Advisory Panel for their advice and expertise when developing our definitions of multiple long-term conditions.
Conflicts of Interest
The authors declare conflict of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, or in the decision to publish the results.
Appendix A. Overview of the Care City Cohort and Data Linkage Steps
In 2017, the leaders of Barking and Dagenham Council, North East London NHS Foundation Trust (NELFT) and Barking and Dagenham, Havering and Redbridge Clinical Commissioning Group (BHR CCG), and their Caldicott guardians (a senior person within each organisation who is responsible for protecting the confidentiality of people’s health and care information and making sure it is used properly), signed data sharing agreements to create a dataset that linked administrative data for the population of Barking and Dagenham (B&D) between 1st April 2011 and 31st March 2017. Since its creation, the dataset has been updated on an annual basis. It is hosted in the Barking and Dagenham, Havering, and Redbridge NHS Accredited Data Safe Haven, with governance and oversight provided by the Barking and Dagenham, Havering, and Redbridge Information Governance Steering Committee.
The dataset was created as part a larger research programme of work []. It contains routinely collected administrative health and social data across local government services, health providers, and health commissioners. Data are linked at the individual and household levels using linkage keys (replacing NHS numbers and Unique Property Reference Numbers; UPRNs). The data are pseudonymised and include information on sociodemographic characteristics, health variables, household variables and data on health and social care service utilisation. Data on all sociodemographic and health variables for each cross-section are taken as a snapshot on 1st April 2019 to account for in-year changes in variables. The dataset is not currently publicly available but was made available to the wider research community in Autumn 2020.
More information on the dataset can be found here [] and here []. More information on the codes and algorithms used to classify variables as part of the creation of the Care City Cohort can be found at this reference [].
This study used data from the 2019/20 cross-section of the Care City Cohort. We requested access to pseudonymised sociodemographic and health variables extracted from primary care data, and resident data extracted from local government data. We did not have access to other data available within the Care City Cohort, such as data on health and care service utilisation.
Data were provided unlinked with linkage keys, i.e., with the identification codes generated to replace NHS numbers and UPRNs. We used these to link the data at the individual and household levels. First, we linked the individual- and household-level local government data on Household_ID (the household-level identification code created by Care City to replace UPRNs). Second, we linked the individual-level primary care data to the linked local government data on Patient_ID (the individual-level identification code created by Care City to replace NHS numbers). Third, we linked a fourth dataset provided by Care City that detailed care homes in Barking and Dagenham and their Household_IDs. We linked this to the cohort data on Household_ID. Finally, we linked a fifth dataset from ONS that contained area-level deprivation data from 2019. We linked this dataset to the data on LSOA code (a unique number identifying each small area/LSOA in England). All linkages were conducted in R software using the merge function from the R base package. Figure A1 illustrates the results of the linkages of the separate primary care and local government datasets. A total of 232,671 individuals were linked across primary care and local government datasets (84.0% of the original primary care records).
To assess whether there were any potential selection biases in the linkage results, we calculated standardised differences in key variables for matched and unmatched primary care records []. Standardised differences of 0.2, 0.5, and 0.8 indicate small, medium and large effect sizes, respectively []. We were not able to assess potential biases in social variables extracted from local government records (i.e., in the household tenure variable and other household variables) as, by definition, unmatched primary care records did not have corresponding local government data. However, the number of unmatched local government records was considerably low (N = 369). Table A1 presents the results of analyses conducted to assess potential biases in the linkage results for matched and unmatched primary care records. These results indicate that selection biases were not introduced in selected variables originating from primary care records as a result of the success of data linkages, which is in keeping with previous analyses of this data [].
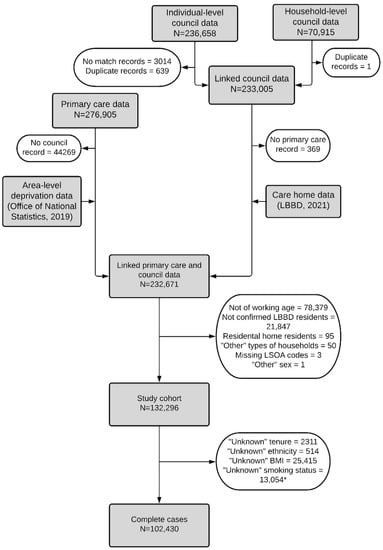
Figure A1.
Results of data linkages. * Number of participants with missing data on each variable sum to greater than 29,866 (132,296 minus 102,430) as some participants had missing data across more than one variable.

Table A1.
Results of analyses to assess potential biases in the linkage results for matched (N = 232,671) and unmatched (N = 44,269) primary care records.
Table A1.
Results of analyses to assess potential biases in the linkage results for matched (N = 232,671) and unmatched (N = 44,269) primary care records.
| Primary Care Matched Records N = 232,671 | Primary Care Unmatched Records N = 44,269 | Standardised Difference | |
|---|---|---|---|
| Age: N (%) | |||
| <16 | 57,402 (24.7) | 8877 (20.1) | 0.150 |
| 16–29 | 42,325 (18.2) | 8593 (19.4) | |
| 30–44 | 59,891 (25.7) | 11,942 (27.0) | |
| 45–54 | 30,738 (13.2) | 5679 (12.8) | |
| 55–64 | 21,338 (9.17) | 4101 (9.26) | |
| 65–74 | 11,602 (4.99) | 2461 (5.56) | |
| 75–84 | 6366 (2.74) | 1414 (3.19) | |
| 85+ | 3009 (1.29) | 1202 (2.72) | |
| Sex: N (%) | |||
| Female | 116,186 (49.9) | 21,787 (49.2) | 0.025 |
| Male | 116,484 (50.1) | 22,472 (50.8) | |
| Other/Missing | 1 (0.00) | 10 (0.00) | |
| Ethnicity *: N (%) | |||
| White | 76,524 (32.9) | 13,633 (31.4) | 0.128 |
| Black | 32,708 (14.1) | 5029 (11.4) | |
| Asian | 42,222 (18.1) | 9710 (21.9) | |
| Mixed | 6285 (2.70) | 1137 (2.57) | |
| Other | 4309 (1.85) | 831 (1.88) | |
| Unknown | 67,493 (29.0) | 13,629 (30.8) | |
| Basic MLTCs: N (%) | |||
| Present | 41,329 (17.8) | 7931 (17.9) | 0.004 |
| Absent | 191,342 (82.2) | 36,338 (82.1) | |
| Physical-mental MLTCs: N (%) | |||
| Present | 9077 (3.90) | 1542 (3.48) | 0.022 |
| Absent | 223,594 (96.1) | 42,727 (96.5) | |
| Complex MLTCs N (%): | |||
| Present | 17,721 (7.65) | 3562 (8.09) | 0.016 |
| Absent | 214,950 (92.4) | 40,707 (91.6) | |
| BMI categories: N (%) | |||
| Underweight | 11,645 (5.00) | 2115 (4.78) | 0.077 |
| Healthy weight | 48,101 (20.7) | 10,355 (23.4) | |
| Overweight | 49,180 (21.1) | 9493 (21.4) | |
| Obese | 37,566 (16.1) | 6612 (14.9) | |
| Morbidly obese | 6077 (2.61) | 934 (2.11) | |
| Unknown | 80,102 (34.4) | 14,760 (33.3) | |
| Smoking status: N (%) | |||
| Non-smoker | 107,326 (46.1) | 21,247 (48.0) | 0.043 |
| Ex-smoker | 24,385 (10.5) | 4620 (10.4) | |
| Smoker | 33,722 (14.5) | 6372 (14.4) | |
| Unknown | 67,238 (28.9) | 12,030 (27.2) |
MLTCs = multiple long-term conditions. * Variable taken from primary care records, unlike in the study analyses.

Table A2.
The 38 long-term conditions grouped by 10 bodily systems and their distribution across the study cohort (N = 132,296).
Table A2.
The 38 long-term conditions grouped by 10 bodily systems and their distribution across the study cohort (N = 132,296).
| Respiratory | N (%) |
| Asthma (currently treated) | 6551 (4.95) |
| Bronchiectasis | 143 (0.11) |
| Chronic obstructive pulmonary disorder | 1325 (1.00) |
| Sensory | |
| Blindness and low vision | 905 (0.68) |
| Chronic sinusitis | 1617 (1.22) |
| Hearing loss | 4726 (3.57) |
| Psoriasis or eczema | 812 (0.61) |
| Cardiovascular | |
| Atrial fibrillation | 451 (0.34) |
| Coronary heart disease | 1446 (1.09) |
| Heart failure | 302 (0.23) |
| Hypertension | 14,518 (11.0) |
| Peripheral vascular disease | 169 (0.13) |
| Endocrine | |
| Diabetes | 8728 (6.60) |
| Thyroid disorders | 4403 (3.33) |
| Cancer | |
| Cancer (in last 5 years) | 1157 (0.87) |
| Musculoskeletal | |
| Painful conditions | 7417 (5.61) |
| Rheumatoid arthritis (or other inflammatory polyarthropathies and systematic connective tissue disorders) | 2871 (2.17) |
| Mental health | |
| Alcohol problems | 1170 (0.88) |
| Anorexia and bulimia | 820 (0.62) |
| Anxiety (and other neurotic, stress-related and somatoform disorders) | 3935 (2.97) |
| Depression | 9055 (6.84) |
| Dementia | 58 (0.04) |
| Psychoactive substance misuse | 1451 (1.10) |
| Schizophrenia and bipolar | 8624 (6.52) |
| Neurological | |
| Epilepsy (currently treated) | 750 (0.57) |
| Learning disability | 905 (0.68) |
| Migraine | 331 (0.25) |
| Stroke and transient ischaemic attack | 844 (0.64) |
| Multiple sclerosis | 177 (0.13) |
| Parkinson’s disease | 54 (0.04) |
| Genitourinary | |
| Chronic kidney disease | 444 (0.34) |
| Prostate disorders | 666 (0.50) |
| Gastrointestinal | |
| Chronic liver disease and viral hepatitis | 1341 (1.01) |
| Constipation (treated) | 741 (0.56) |
| Diverticular disease of intestine | 893 (0.68) |
| Irritable bowel syndrome | 3914 (2.96) |
| Inflammatory bowel disease | 718 (0.54) |
| Peptic ulcer disease | 760 (0.57) |

Table A3.
Household benefits receipt, occupancy, and household type, by tenure for complete cases (N = 102,430).
Table A3.
Household benefits receipt, occupancy, and household type, by tenure for complete cases (N = 102,430).
| Owner-Occupied N = 43,444 | Social Housing N = 27,766 | Privately Rented N = 31,220 | |
|---|---|---|---|
| Household benefits receipt: N (%) | |||
| None | 41,670 (95.9) | 18,140 (65.3) | 21,337 (68.3) |
| ESA | 374 (0.86) | 2883 (10.4) | 1294 (4.14) |
| Pension | 405 (0.93) | 676 (2.43) | 419 (1.34) |
| Income Support | 135 (0.31) | 1143 (4.12) | 612 (1.96) |
| JSA | 32 (0.07) | 309 (1.11) | 134 (0.43) |
| Housing benefit only | 828 (1.91) | 4615 (16.6) | 7424 (23.8) |
| Household occupancy: N (%) | |||
| 1–2 | 9044 (20.8) | 8668 (31.2) | 6423 (20.6) |
| 3–5 | 26,458 (60.9) | 15,316 (55.2) | 16,978 (54.4) |
| 6–10 | 7531 (17.3) | 3668 (13.2) | 7153 (22.9) |
| 11+ | 411 (0.95) | 114 (0.41) | 666 (2.13) |
| Household type: N (%) | |||
| Adults with children | 17,749 (40.9) | 10,884 (39.2) | 17,313 (55.5) |
| Adults with no children | 15,888 (36.6) | 8917 (32.1) | 7164 (22.9) |
| Single adult with children | 1179 (2.71) | 2176 (7.84) | 2827 (9.06) |
| Single adult | 2948 (6.79) | 3593 (12.9) | 2380 (7.62) |
| Older cohabiting adults | 3615 (8.32) | 1602 (5.77) | 660 (2.11) |
| Three generations | 2065 (4.75) | 594 (2.14) | 876 (2.81) |
Note: the denominator for all variables is the number of individuals rather than households. +ESA = Employment Support and Allowance; JSA = Job Seeker’s Allowance.

Table A4.
Estimated odds ratios of basic, physical-mental, and complex MLTCs with household tenure when the final models tested for interactions between tenure and household benefits receipt for working-age adults residing in B&D in 2019/20 (N = 102,430).
Table A4.
Estimated odds ratios of basic, physical-mental, and complex MLTCs with household tenure when the final models tested for interactions between tenure and household benefits receipt for working-age adults residing in B&D in 2019/20 (N = 102,430).
| Independent Variables | Basic MLTCs | Physical-Mental MLTCs | Complex MLTCs | ||||
|---|---|---|---|---|---|---|---|
| OR (95% CI) | p Value | OR (95% CI) | p Value | OR (95% CI) | p Value | ||
| Tenure | OOC | - | - | - | - | - | - |
| Privately rented | 0.78 (0.74–0.82) | <0.001 | 0.77 (0.69–0.86) | <0.001 | 0.77 (0.70–0.84) | <0.001 | |
| Social housing | 1.38 (1.32–1.45) | <0.001 | 1.54 (1.41–1.68) | <0.001 | 1.34 (1.24–1.45) | <0.001 | |
| Household benefits receipt | No benefits | - | - | - | - | - | - |
| ESA | 4.21 (3.35–5.28) | <0.001 | 7.83 (6.04–10.1) | <0.001 | 6.85 (5.33–8.79) | <0.001 | |
| Pension credit | 1.52 (1.19–1.94) | <0.001 | 1.67 (1.08–2.57) | 0.021 | 1.62 (1.14–2.31) | 0.008 | |
| Income support | 2.78 (1.90–4.06) | <0.001 | 2.29 (1.24–4.25) | 0.008 | 2.39 (1.44–3.97) | <0.001 | |
| JSA | 0.96 (0.41–2.24) | 0.924 | 0.72 (0.10–5.39) | 0.752 | 1.60 (0.53–4.79) | 0.401 | |
| Housing benefit only | 1.92 (1.63–2.26) | <0.001 | 2.45 (1.89–3.17) | <0.001 | 1.92 (1.52–2.43) | <0.001 | |
| Tenure*Household benefitsreceipt | Privately rented*no benefits | - | - | - | - | - | - |
| Privately rented*ESA | 1.76 (1.35–2.29) | <0.001 | 1.42 (1.05–1.93) | 0.024 | 1.36 (1.01–1.83) | 0.043 | |
| Privately rented*pension credit | 1.40 (1.00–1.96) | 0.052 | 1.86 (1.05–3.31) | 0.034 | 1.57 (0.96–2.58) | 0.073 | |
| Privately rented*income support | 1.08 (0.71–1.66) | 0.711 | 1.47 (0.73–2.93) | 0.279 | 1.57 (0.87–2.84) | 0.137 | |
| Privately rented*JSA | 2.31 (0.90–5.90) | 0.080 | 1.97 (0.22–17.4) | 0.541 | 1.53 (0.44–5.36) | 0.509 | |
| Privately rented*housing benefit only | 0.92 (0.78–1.10) | 0.356 | 0.95 (0.71–1.28) | 0.752 | 1.03 (0.79–1.36) | 0.807 | |
| Tenure*Household benefits receipt (continued) | Social housing*no benefits | - | - | - | - | - | - |
| Social housing*ESA | 1.12 (0.88–1.43) | 0.359 | 0.74 (0.56–0.99) | 0.039 | 0.95 (0.72–1.25) | 0.708 | |
| Social housing*pension credit | 1.01 (0.75–1.36) | 0.956 | 0.93 (0.57–1.54) | 0.784 | 0.93 (0.60–1.42) | 0.724 | |
| Social housing*income support | 0.93 (0.62–1.39) | 0.714 | 1.14 (0.60–2.18) | 0.683 | 1.56 (0.91–2.68) | 0.106 | |
| Social housing*JSA | 1.59 (0.66–3.86) | 0.303 | 1.96 (0.25–15.1) | 0.519 | 1.08 (0.34–3.42) | 0.895 | |
| Social housing*housing benefit only | 0.96 (0.80–1.15) | 0.681 | 1.01 (0.76–1.33) | 0.966 | 1.21 (0.94–1.57) | 0.142 | |

Table A5.
Estimated odds ratios of basic, physical-mental, and complex MLTCs with household tenure when the final models tested for interactions between tenure and household occupancy for working-age adults residing in B&D in 2019/20 (N = 102,430).
Table A5.
Estimated odds ratios of basic, physical-mental, and complex MLTCs with household tenure when the final models tested for interactions between tenure and household occupancy for working-age adults residing in B&D in 2019/20 (N = 102,430).
| Independent Variables | Basic MLTCs | Physical-Mental MLTCs | Complex MLTCs | ||||
|---|---|---|---|---|---|---|---|
| OR (95% CI) | p Value | OR (95% CI) | p Value | OR (95% CI) | p Value | ||
| Tenure | OOC | - | - | - | - | - | - |
| Privately rented | 0.99 (0.91–1.08) | 0.800 | 1.04 (0.90–1.20) | 0.564 | 1.02 (0.89–1.16) | 0.782 | |
| Social housing | 1.54 (1.43–1.66) | <0.001 | 1.57 (1.40–1.77) | <0.001 | 1.61 (1.45–1.79) | <0.001 | |
| Occupancy categories | 1–2 occupants | - | - | - | - | - | - |
| 3–5 occupants | 1.03 (0.96–1.10) | 0.415 | 0.98 (0.87–1.11) | 0.781 | 1.04 (0.94–1.15) | 0.464 | |
| 6–10 occupants | 1.02 (0.93–1.13) | 0.611 | 0.82 (0.67–0.99) | 0.041 | 1.12 (0.96–1.31) | 0.141 | |
| 11+ occupants | 0.95 (0.70–1.28) | 0.727 | 0.68 (0.32–1.47) | 0.326 | 1.29 (0.80–2.08) | 0.291 | |
| Tenure*Occupancy | Privately rented*1–2 occupants | - | - | - | - | - | - |
| Privately rented*3–5 occupants | 0.77 (0.70–0.85) | <0.001 | 0.73 (0.61–0.87) | <0.001 | 0.74 (0.63–0.87) | <0.001 | |
| Privately rented*6–10 occupants | 0.73 (0.64–0.83) | <0.001 | 0.80 (0.62–1.03) | 0.089 | 0.66 (0.53–0.81) | <0.001 | |
| Privately rented*11+ occupants | 0.69 (0.46–1.03) | 0.072 | 0.88 (0.35–2.21) | 0.791 | 0.37 (0.18–0.75) | 0.006 | |
| Social housing*1–2 occupants | - | - | - | - | - | - | |
| Social housing*3–5 occupants | 0.84 (0.77–0.92) | <0.001 | 0.88 (0.77–1.02) | 0.093 | 0.78 (0.69–0.89) | <0.001 | |
| Social housing*6–10 occupants | 0.86 (0.75–0.97) | 0.019 | 0.97 (0.76–1.23) | 0.794 | 0.63 (0.51–0.78) | <0.001 | |
| Social housing*11+ occupants | 0.42 (0.22–0.78) | 0.007 | 0.86 (0.29–2.55) | 0.785 | 0.42 (0.17–1.04) | 0.060 | |

Table A6.
Estimated odds ratios of basic, physical-mental, and complex MLTCs with household tenure when the final models tested for interactions between tenure and household type for working-age adults residing in B&D in 2019/20 (N = 102,430).
Table A6.
Estimated odds ratios of basic, physical-mental, and complex MLTCs with household tenure when the final models tested for interactions between tenure and household type for working-age adults residing in B&D in 2019/20 (N = 102,430).
| Independent Variables | Basic MLTCs | Physical-Mental MLTCs | Complex MLTCs | ||||
|---|---|---|---|---|---|---|---|
| OR (95% CI) | p Value | OR (95% CI) | p Value | OR (95% CI) | p Value | ||
| Tenure | OOC | - | - | - | - | - | |
| Privately rented | 0.75 (0.70–0.81) | <0.001 | 0.81 (0.70–0.92) | <0.001 | 0.67 (0.59–0.75) | <0.001 | |
| Social housing | 1.40 (1.30–1.50) | <0.001 | 1.54 (1.35–1.75) | <0.001 | 1.22 (1.09–1.38) | <0.001 | |
| Household type | Adults with children | - | - | - | - | - | - |
| Adults with no children | 1.27 (1.19–1.35) | <0.001 | 1.28 (1.13–1.46) | <0.001 | 1.17 (1.05–1.30) | 0.003 | |
| Single adult with children | 0.92 (0.76–1.11) | 0.364 | 0.78 (0.53–1.17) | 0.233 | 0.72 (0.49–1.07) | 0.103 | |
| Single adult | 1.16 (1.04–1.30) | 0.009 | 1.46 (1.20–1.78) | <0.001 | 1.01 (0.85–1.21) | 0.892 | |
| Older cohabiting adults | 1.47 (1.34–1.62) | <0.001 | 1.35 (1.12–1.62) | 0.001 | 1.38 (1.19–1.60) | <0.001 | |
| Three generations | 1.06 (0.93–1.21) | 0.405 | 1.08 (0.81–1.43) | 0.592 | 1.14 (0.91–1.42) | 0.259 | |
| Tenure*Household type | Privately rented*adults with children | - | - | - | - | - | - |
| Privately rented*adults with no children | 1.09 (0.98–1.20) | 0.105 | 1.03 (0.85–1.24) | 0.788 | 1.25 (1.06–1.48) | 0.009 | |
| Privately rented*single adult with children | 1.17 (0.93–1.46) | 0.179 | 1.29 (0.82–2.04) | 0.267 | 1.18 (0.74–1.88) | 0.480 | |
| Tenure*Household type (continued) | Privately rented*single adult | 1.57 (1.34–1.82) | <0.001 | 1.39 (1.08–1.79) | 0.011 | 1.85 (1.46–2.35) | <0.001 |
| Privately rented*older cohabiting adults | 1.24 (1.00–1.53) | 0.052 | 1.37 (0.97–1.95) | 0.076 | 1.72 (1.28–2.32) | <0.001 | |
| Privately rented*three generations | 0.96 (0.75–1.23) | 0.774 | 0.91 (0.56–1.49) | 0.720 | 1.15 (0.77–1.72) | 0.494 | |
| Social housing*adults with children | - | - | - | - | - | - | |
| Social housing*adults with no children | 0.90 (0.82–0.99) | 0.029 | 0.88 (0.74–1.04) | 0.132 | 1.11 (0.96–1.28) | 0.170 | |
| Social housing*single adult with children | 1.22 (0.98–1.52) | 0.079 | 1.38 (0.90–2.14) | 0.142 | 1.49 (0.97–2.30) | 0.070 | |
| Social housing*single adult | 1.31 (1.15–1.50) | <0.001 | 1.07 (0.86–1.33) | 0.557 | 1.48 (1.21–1.81) | <0.001 | |
| Social housing*older cohabiting adults | 0.76 (0.65–0.89) | <.001 | 0.88 (0.68–1.13) | 0.315 | 0.87 (0.69–1.10) | 0.244 | |
| Social housing*three generations | 0.91 (0.70–1.17) | 0.451 | 0.79 (0.49–1.23) | 0.318 | 0.93 (0.61–1.41) | 0.728 | |
References
- The Academy of Medical Sciences. Multimorbidity: A Priority for Global Health Research; Academy of Medical Sciences: London, UK, 2018; pp. 1–127. [Google Scholar]
- Marengoni, A.; Angleman, S.; Melis, R.; Mangialasche, F.; Karp, A.; Garmen, A.; Meinow, B.; Fratiglioni, L. Aging with multimorbidity: A systematic review of the literature. Ageing Res. Rev. 2011, 10, 430–439. [Google Scholar] [CrossRef]
- Violán, C.; Foguet-Boreu, Q.; Flores-Mateo, G.; Salisbury, C.; Blom, J.; Freitag, M.; Glynn, L.; Muth, C.; Valderas, J.M. Prevalence, determinants and patterns of multimorbidity in primary care: A systematic review of observational studies. PLoS ONE 2014, 9, e102149. [Google Scholar] [CrossRef] [PubMed]
- Salisbury, C.; Johnson, L.; Purdy, S.; Valderas, J.M.; Montgomery, A. Epidemiology and impact of multimorbidity in primary care: A retrospective cohort study. Br. J. Gen. Pract. 2011, 61, 12–21. [Google Scholar] [CrossRef] [PubMed]
- Khanolkar, A.R.; Chaturvedi, N.; Kuan, V.; Davis, D.; Hughes, A.; Richards, M.; Bann, D.; Patalay, P. Socioeconomic inequalities in prevalence and development of multimorbidity across adulthood: A longitudinal analysis of the MRC 1946 National Survey of Health and Development in the UK. PLoS Med. 2021, 18, e1003775. [Google Scholar] [CrossRef]
- Barnett, K.; Mercer, S.W.; Norbury, M.; Watt, G.; Wyke, S.; Guthrie, B. Epidemiology of multimorbidity and implications for health care, research, and medical education: A cross-sectional study. Lancet 2012, 380, 37–43. [Google Scholar] [CrossRef] [Green Version]
- Ingram, E.; Ledden, S.; Beardon, S.; Gomes, M.; Hogarth, S.; McDonald, H.; Osborn, D.P.; Sheringham, J. Household and area-level social determinants of multimorbidity: A systematic review. J. Epidemiol. Community Health 2021, 75, 232–241. [Google Scholar] [CrossRef] [PubMed]
- Head, A.; Fleming, K.; Kypridemos, C.; Pearson-Stuttard, J.; O’Flaherty, M. Multimorbidity: The case for prevention. J. Epidemiol. Community Health 2021, 75, 242–244. [Google Scholar] [CrossRef]
- Head, A.; Fleming, K.; Kypridemos, C.; Schofield, P.; Pearson-Stuttard, J.; O’Flaherty, M. I Inequalities in incident and prevalent multimorbidity in England, 2004–2019: A population-based, descriptive study. Lancet Healthy Longev. 2021, 2, e489–e497. [Google Scholar] [CrossRef]
- Solar, O.; Irwin, A. A Conceptual Framework for Action on the Social Determinants of Health; WHO Document Production Services: Geneva, Switzerland, 2010. [Google Scholar] [CrossRef]
- Office for National Statistics. Living longer: Changes in Housing Tenure Over Time 2020. Available online: https://www.ons.gov.uk/releases/livinglongerchangesinhousingtenureovertime (accessed on 27 October 2021).
- Office for National Statistics. English Housing Survey 2019 to 2020: Headline Report 2020. Available online: https://www.gov.uk/government/statistics/english-housing-survey-2019-to-2020-headline-report (accessed on 27 October 2021).
- Ellaway, A.; Macintyre, S. Does housing tenure predict health in the UK because it exposes people to different levels of housing related hazards in the home or its surroundings? Health Place 1998, 4, 141–150. [Google Scholar] [CrossRef]
- Shaw, M. Housing and public health. Annu. Rev. Public Health 2004, 25, 397–418. [Google Scholar] [CrossRef] [Green Version]
- Macintyre, S.; Ellaway, A.; Hiscock, R.; Kearns, A.; Der, G.; McKay, L. What features of the home and the area might help to explain observed relationships between housing tenure and health? Evidence from the west of Scotland. Health Place 2003, 9, 207–218. [Google Scholar] [CrossRef]
- Reeves, A.; Clair, A.; McKee, M.; Stuckler, D. Reductions in the United Kingdom’s Government Housing Benefit and Symptoms of Depression in Low-Income Households. Am. J. Epidemiol. 2016, 184, 421–429. [Google Scholar] [CrossRef] [Green Version]
- Clair, A.; Hughes, A. Housing and health: New evidence using biomarker data. J. Epidemiol. Community Health 2019, 73, 256–262. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Shand, J. Towards Integrated Care: Using Linked Data to Explore Health and Social Care Utilisation for Adult Residents of Barking and Dagenham in 2016/17. Ph.D. Thesis, University College London (UCL), London, UK, 2020. [Google Scholar]
- London Borough of Barking and Dagenham. Joint Strategic Needs Assessment. 2018. Available online: https://www.lbbd.gov.uk/joint-strategic-needs-assessment-jsna (accessed on 7 November 2019).
- Benchimol, E.I.; Smeeth, L.; Guttmann, A.; Harron, K.; Moher, D.; Petersen, I.; Sørensen, H.T.; von Elm, E.; Langan, S.M.; RECORD Working Committee. The REporting of studies Conducted using Observational Routinely-collected health Data (RECORD) Statement. PLoS Med. 2015, 12, e1001885. [Google Scholar] [CrossRef] [PubMed]
- Office for National Statistics. Working Age Population. 2020. Available online: https://www.ethnicity-facts-figures.service.gov.uk/uk-population-by-ethnicity/demographics/working-age-population/latest (accessed on 21 March 2022).
- Harper, G.; Mayhew, L. Using Administrative Data to Count an Local Applications. Appl. Spat. Anal. Policy 2012, 5, 97–122. [Google Scholar] [CrossRef] [Green Version]
- Cambridge C@. Codes Lists Version 1.1—October 2018—Primary Care Unit. 2018. Available online: https://www.phpc.cam.ac.uk/pcu/cprd_cam/codelists/v11/ (accessed on 6 November 2019).
- Harrison, C.; Britt, H.; Miller, G.; Henderson, J. Examining different measures of multimorbidity, using a large prospective cross-sectional study in Australian general practice. BMJ Open 2014, 4, e004694. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Office for National Statistics. National Statistics—English Indices of Deprivation 2019. 2019. Available online: https://www.gov.uk/government/statistics/english-indices-of-deprivation-2019 (accessed on 13 September 2021).
- Office for National Statistics. Census Geography. 2011. Available online: https://www.ons.gov.uk/methodology/geography/ukgeographies/censusgeography (accessed on 13 September 2021).
- Bobo, W.V.; Yawn, B.P.; St. Sauver, J.L.; Grossardt, B.R.; Boyd, C.M.; Rocca, W.A. Prevalence of Combined Somatic and Mental Health Multimorbidity: Patterns by Age, Sex, and Race/Ethnicity. J. Gerontol. A Biol. Sci. Med. Sci. 2016, 71, 1483–1491. [Google Scholar] [CrossRef] [Green Version]
- Office for National Statistics. Home Ownership—Ethnicity Facts and Figures. 2020. Available online: https://www.ethnicity-facts-figures.service.gov.uk/housing/owning-and-renting/home-ownership/latest (accessed on 20 September 2021).
- Katikireddi, S.V.; Skivington, K.; Leyland, A.H.; Hunt, K.; Mercer, S.W. The contribution of risk factors to socioeconomic inequalities in multimorbidity across the lifecourse: A longitudinal analysis of the Twenty-07 cohort. BMC Med. 2017, 15, 152. [Google Scholar] [CrossRef]
- Bates, D.; Mächler, M.; Bolker, B.; Walker, S. Fitting linear mixed-effects models using lme4. J. Stat. Softw. 2015, 67, 48. [Google Scholar] [CrossRef]
- Doerken, S.; Avalos, M.; Lagarde, E.; Schumacher, M. Penalized logistic regression with low prevalence exposures beyond high dimensional settings. PLoS ONE 2019, 14, e0217057. [Google Scholar] [CrossRef] [Green Version]
- Johnson-Lawrence, V.; Zajacova, A.; Sneed, R. Education, race/ethnicity, and multimorbidity among adults aged 30–64 in the National Health Interview Survey. SSM—Popul. Health 2017, 3, 366–372. [Google Scholar] [CrossRef] [PubMed]
- Taylor, A.W.; Price, K.; Gill, T.K.; Adams, R.; Pilkington, R.; Carrangis, N.; Shi, Z.; Wilson, D. Multimorbidity: Not just an older person’s issue. Results from an Australian biomedical study. Soc. Psychiatry Psychiatr. Epidemiol. 2011, 46, 351. [Google Scholar] [CrossRef] [Green Version]
- Chung, R.Y.; Mercer, S.; Lai, F.T.T.; Yip, B.H.K.; Wong, M.C.S.; Wong, S.Y.S. Socioeconomic determinants of multimorbidity: A population-based household survey of Hong Kong Chinese. PLoS ONE 2015, 10, e0140040. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Ferry, F.R.; Rosato, M.G.; Curran, E.J.; O’Reilly, D.; Leavey, G. Multimorbidity among persons aged 25–64 years: A population-based study of social determinants and all-cause mortality. J. Public Health 2020, 44, e59–e67. [Google Scholar] [CrossRef] [PubMed]
- Ansar, W.; Ghosh, S. C-reactive protein and the biology of disease. Immunol. Res. 2013, 56, 131–142. [Google Scholar] [CrossRef] [PubMed]
- Hiscock, R.; Kearns, A.; MacIntyre, S.; Ellaway, A. Ontological security and psycho-social benefits from the home: Qualitative evidence on issues of tenure. Hous. Theory Soc. 2001, 18, 50–66. [Google Scholar] [CrossRef]
- Scanlon, K.; Kochan, B. Towards a Sustainable Private Rented Sector. The Lessons from Other Countries. 2011. Available online: http://eprints.lse.ac.uk/56070/1/Towards_a_sustainable_private_rented_sector.pdf (accessed on 29 June 2021).
- Palmer, G. “Single Person Households” Issues That JRF Should Be Thinking about. Joseph Rowntree Found. 2006. Available online: https://www.jrf.org.uk (accessed on 22 December 2021).
- Zaccai, J.H. How to assess epidemiological studies. Postgrad. Med. J. 2004, 80, 140–147. [Google Scholar] [CrossRef]
- Pigott, T.D. A Review of Methods for Missing Data. Educ. Res. Eval. 2001, 7, 353–383. [Google Scholar] [CrossRef] [Green Version]
- Care City Cohort 2019. Available online: https://www.carecity.london/component/content/article/95-what-we-do/216-care-city-cohort (accessed on 7 February 2022).
- Shand, J.; Morris, S.; Gomes, M. Understanding health and care expenditure by setting—Who matters to whom? J. Health Serv. Res. Policy 2020, 26, 77–84. [Google Scholar] [CrossRef]
- Harron, K.L.; Doidge, J.; Knight, H.E.; Gilbert, R.; Goldstein, H.; Cromwell, D.A.; Van Der Meulen, J.H. A guide to evaluating linkage quality for the analysis of linked data. Int. J. Epidemiol. 2017, 46, 1699–1710. [Google Scholar] [CrossRef] [PubMed] [Green Version]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).