Abstract
We aimed to evaluate the impacts of disability on the diagnosis, treatment, and prognosis of bile duct cancer (BDC) according to the severity and type of disability. Patients diagnosed with BDC were selected from an age- and sex-matched population (1:3 ratio) with or without disabilities from the National Disability Database, the Korean Central Cancer Registry, and the Korean National Health Insurance claims database. The cohort included 15,065 patients with BDC, with a significantly lower rate in those with severe disabilities than in people without or with mild disabilities (110.6 vs. 136.5 vs. 147.6 per 105 persons, respectively). People with severe disabilities were diagnosed with BDC at an earlier age but were less likely to undergo surgery (adjusted odds ratio (aOR) = 0.52, 95% confidence interval (CI): 0.45–0.61) or chemotherapy (aOR = 0.76, 95% CI: 0.61–0.95) compared to those without disabilities. This trend was more evident in patients with mental disabilities. The overall and cancer-specific mortality rates were higher in patients (especially women) with disabilities than in those without. There needs systemic approach to ensure equal access to quality cancer care for people with disabilities.
1. Introduction
Cancer diagnosis and treatment are determined by socio-economic factors as well as tumor biological factors [1,2]. Low-income people are often diagnosed with cancer at a later stage, are less likely to receive standard therapy, and have shorter survival times [2]. In South Korea, disability-related health disparities are reported in terms of health factors such as insufficient physical activity, being underweight or overweight [3], and lower participation in health screening programs [4]. People with disabilities are less likely to undergo staging work-up and intensive treatment for lung [5] and breast cancers [6]. They are also more likely to die prematurely because of cardiovascular disease or cancer [7]. However, disparities vary depending on the cancer, disability type, severity, and living area [5,6,8]. People with severe disabilities; communication, brain, or mental disabilities; or those living in rural areas have less access to cancer screening [9]. However, people with mild disabilities are more likely to use health services than those without disabilities [10]. To the best of our knowledge, there have been no studies on the effects of disabilities on the clinical characteristics, management, and prognosis of bile duct cancer (BDC).
BDC is more prevalent in Asian countries than in Western countries [11]. In South Korea, BDC was the ninth-most common cancer and sixth cause of cancer-related mortality in 2017 [12]. Most patients present with advanced disease and less than 30% are eligible for curative resection. The 5-year survival rate is less than 30% despite improvements in prognosis in recent years [12]. Therefore, early diagnosis and intensive treatment are necessary to improve the prognosis of BDC [13].
In South Korea, all people are covered by universal health insurance. The coinsurance for cancer work-up and treatment is only 5% of the total medical costs, with a maximum copay for low-income people of only approximately USD 1000 since 2016. In addition, Korea has a national disability registration system, which defines disability type and severity according to preset criteria and medical diagnosis. These are optimal conditions for examining disparities in BDC related to disabilities. Using the linked administrative database in Korea, we investigated the potential disparities in the diagnosis, treatment, and survival of patients diagnosed with BDC between people with and without disabilities.
2. Materials and Methods
2.1. Data Sources and Case Selection
This study obtained data from the Korean National Disability Registry (KNDR) [14], the Korean Central Cancer Registry (KCCR), and the Korean National Health Insurance (KNHI) claims database. The KNDR contains information about disability type and severity, and included 93.8% of the total population with disabilities in 2011. The KCCR, a nationwide government-sponsored cancer registry, includes information regarding age and date at diagnosis, cancer site, and Surveillance, Epidemiology, and End Results (SEER) summary stage, and included 97.2% of cancer cases in 2017 [12]. Among SEER staging categories (localized, regional, metastatic, and unknown), the unknown stage is assigned if the primary cancer site is unknown or sufficient evidence is not available to adequately assign a stage. The KNHI provides universal health insurance to all Koreans, and the database contains information regarding patient health insurance premium, residential area, comorbid diseases, diagnosis, imaging and laboratory results, treatment, and mortality. Information from the KNDR was merged with data from the KCCR and KNHI claims database for the period 2002–2015 using personal identification numbers.
We identified 2,776,450 persons with disabilities from 2009 to 2013 in an age- and sex-matched population (1:3 ratio) that also included 8,329,350 people without disabilities. Fifteen disability types listed in the KNDR were categorized as physical, communication, brain, mental, or affecting the major internal organs (Supplementary Table S1). Physical disability was the most common type (1,436,219 people, 51.7%), followed by communication disability (585,986 people, 21.1%), brain disability (307,026 people, 11.1%), mental disability (307,026, 11.1%), and major internal organ disability (139,499 people, 5.0%). Disability severity is graded from 1 (very severe) to 6 (very mild) based on functional losses and clinical impairment that are determined by a specialist. In this study, disability severity was also classified as severe (grades 1–3) or mild (grades 4–6), with 1,091,794 people (39.3%) in the severe group and 1,684,656 people (60.7%) in the mild group. Among the entire cohort, 67.4% were <65 years old and 32.6% were ≥65 years old; 58.5% were men and 41.5% were women. People with mental disabilities had the youngest median age (33.6 years). The KNHI premium was used to estimate household income because it is calculated based on income, property, and automobile taxes for each household; household income was categorized as: below the poverty line (lowest) and quartiles I, II, III, and IV (highest), as defined by the KNHI [2]. The proportion of people below the poverty line was 7.1% in the entire cohort, 16.9% in the disabled group, and 3.9% in the non-disabled group. Approximately half of the people with mental disabilities (45.8%) had incomes below the poverty line (Supplementary Table S2).
We subsequently identified 16,865 patients with diagnosed BDC (intrahepatic cholangiocarcinoma C22.1 and extrahepatic cholangiocarcinoma C24.0–24.9) and excluded patients who were <19 years old (n = 0), had no information regarding health insurance premiums (n = 201), or had a diagnosis of other non-thyroid cancer (n = 1599). Finally, 3693 patients with disabilities and 11,372 patients without disabilities at BDC diagnosis were enrolled in the study population (Figure 1). The study protocol was approved by the Institutional Review Board of Chungbuk National University (CBNU-201708-BM-501-01; Cheongju, South Korea).
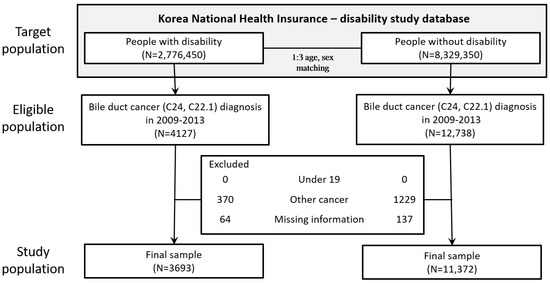
Figure 1.
CONSORT diagram.
For each patient, information was collected about sex, age, severity and type of disability, Charlson comorbidity index (CCI), and presence of comorbidities including hypertension (HTN), diabetes mellitus (DM), coronary heart disease (CHD), stroke, chronic obstructive pulmonary disease (COPD), and cholelithiasis. Information on socioeconomic factors such as income level and location of residence, including whether it was an endemic area for clonorchiasis, was collected. We also selected data regarding BDC such as date at diagnosis, SEER summary stage (local, regional, distant, and unknown), specific treatment (surgery, radiotherapy, and chemotherapy), and overall and cancer-specific mortality.
2.2. Outcomes and Statistical Analyses
Descriptive analyses were performed to determine the distributions of patients with and without disabilities according to age, sex, and income level in patients with BDC. The chi-square test was used to compare categorical variables. The relative probability of receiving surgery and chemotherapy were calculated using logistic regression analyses and adjusted for age, sex, CCI, income, location of residence, and cancer stage. All patients were followed until death or 31 December 2017. The survival outcomes and related risk factors were determined using the Kaplan–Meier method with the log-rank test and multivariate Cox proportional hazards regression analysis. To confirm the assumption of proportionality, we used the graphic method by plotting log hazard estimates against observation periods. Each covariate that was used for adjustment had a Schoenfeld residual indicating that the proportional-hazard assumption was fulfilled (p > 0.1 for all covariates). All statistical analyses were performed using SAS software (version 9.4; SAS Institute, Inc., Cary, NC, USA) and p ≤ 0.05 was considered to denote statistical significance.
3. Results
3.1. Diagnosis of BDC
The diagnostic rate of BDC was slightly lower in people with disabilities than in those without (133.0 vs. 136.5 per 105 people, respectively). In addition, the rates were significantly lower in people with severe disabilities compared to those with mild disabilities (110.6 vs. 147.6 per 105 people, respectively). Among disability types, patients with mental disabilities had the lowest diagnostic rate, followed by those with internal organ disabilities. The mean age at BDC diagnosis was younger in severely disabled people than in mildly or non-disabled people (68.9 vs. 69.8 vs. 70.3 years, respectively). People with mental or internal organ disabilities were diagnosed with BDC at an earlier age than were people with other types of disabilities. Severely disabled people with BDC had a higher CCI than mildly disabled or non-disabled people (2.3 vs. 1.9 vs. 1.4, respectively). Patients with brain or internal organ disabilities had a higher CCI and a higher prevalence of HTN, DM, CHD, stroke, and COPD compared to patients with other types of disabilities. The proportion of BDC patients among individuals with incomes below the poverty line was higher in the disabled group than in the non-disabled group, especially in those with severe disabilities and mental disabilities. The diagnostic rate of BDC was lowest in people with severe disabilities and incomes below the poverty line (71.3 per 105 people; Figure 2). More patients with BDC in the disabled group than in the non-disabled group lived in rural (p < 0.0001) and endemic areas for clonorchiasis (p = 0.035) (Table 1).
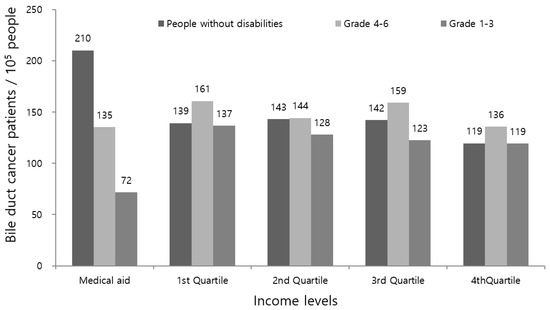
Figure 2.
Comparison of income level structure in patients with BDC between those with or without disabilities (household income level was categorized as: below the poverty line (medical aid, lowest income level) and quartiles I, II, III, and IV (highest); disability severity was also classified as severe (grades 1–3) or mild (grades 4–6)).

Table 1.
General characteristics of the patients with bile duct cancer (BDC).
3.2. Analysis of Treatment Behaviors
There were no differences in SEER stages in patients with or without disabilities. However, a higher proportion of localized or unknown stages was observed in the severely disabled group compared to the mildly disabled group for all types of disabilities. Patients with brain or mental disabilities had a higher unknown stage of BDC compared to patients with other types of disabilities (Table 2).

Table 2.
Disability characteristics in patients with localized, regional, and metastatic bile duct cancer.
Among the 15,065 patients with BDC, 5318 (35.3%) received surgery. The proportion of patients who received surgery was slightly lower in those with disabilities than in those without (32.7% vs. 36.2%; adjusted odds ratio (aOR) = 0.83, 95% confidence interval (CI): 0.76–0.91) after adjusting for age, sex, CCI, income, location of residence, and cancer stage. This disparity was more significant in the severe group (24.3% vs. 36.2%; aOR = 0.52, 95% CI: 0.45–0.61), with the surgery rate gradually increasing from grade 1 to grade 3. Among disability types, patients with severe grades of mental (aOR = 0.31, 95% CI: 0.17–0.57), brain (aOR = 0.34, 95% CI: 0.24–0.47), or internal organ (aOR = 0.38, 95% CI: 0.24–0.60) disabilities had the lowest rates of surgery. Among the 15,065 patients with BDC, 1,579 (10.5%) received chemotherapy. There were no differences in chemotherapy rates between patients with disabilities and those without (10.0% vs. 10.6%; aOR = 0.90, 95% CI: 0.79–1.03). However, patients with severe disabilities received less chemotherapy than did those without disabilities (9.2% vs. 10.6%; aOR = 0.75, 95% CI: 0.61–0.95). Among the various disability types, severe brain (aOR = 0.58, 95% CI: 0.37–0.90) were associated with lower rates of chemotherapy compared to other disability types (Table 3 and Table 4).

Table 3.
Treatment patterns according to the disability characteristics in patients with bile duct cancer.

Table 4.
Factors influencing level of surgery, chemotherapy or conservative management in patient with bile duct cancer.
3.3. Survival Analysis
The median BDC-specific survival time among all patients was 11.3 months; 10.4 and 11.5 months in patients with and without disabilities, respectively. After adjusting for age, sex, income, endemic area, CCI, and SEER stage, we observed poorer BDC-specific mortality in patients with disabilities than in those without (536.1 vs. 486.1 per 1000 persons; adjusted hazard ratio (aHR) = 1.05, 95% CI: 1.01–1.10) (Table 5, Figure 3, and Supplementary Figure S1). Among patients with disabilities, the aHR of overall and BDC-specific mortality increased in patients with severe disabilities from grade 3 to grade 1. Patients with mild disabilities (all types) had a mortality rate similar to that of patients without disabilities (Table 5 and Supplementary Table S3-1).

Table 5.
Cancer-specific mortality in patient with bile duct cancer.
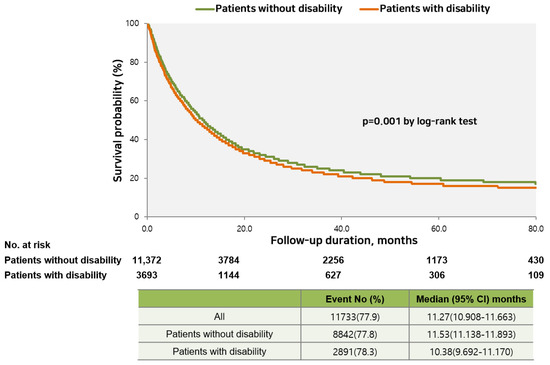
Figure 3.
Comparison of cancer-specific survival between patients with and without disabilities.
Among the various disability types, patients with severe brain (aHR = 1.65, 95% CI: 1.29–2.12) or mental disabilities (aHR = 1.65, 95% CI: 1.29–2.12) exhibited poorer BDC-specific mortality. When overall and BDC-specific mortality was analyzed separately in men and women, the overall hazard ratio was slightly higher in men than in women with disabilities (Table 6 and Table 7 and Supplementary Tables S3-2 and S3-3). However, mortality was higher in women with mental disabilities compared to their male counterparts.

Table 6.
Cancer-specific mortality in male patients diagnosed with bile duct cancer.

Table 7.
Cancer-specific mortality in female patients diagnosed with bile duct cancer.
4. Discussion
This study demonstrated that people with disabilities were less likely to be diagnosed, less likely to receive standard treatment, and had lower BDC survival rates compared to those without disabilities. Evident trends were found in patients with severe disabilities or in those with brain or mental disabilities. People with severe disabilities, mental disabilities, and lower incomes had a lower diagnosis rate of BDC in this study. South Korea operates a medical benefits system that provides almost free basic medical services to people at the lowest income level. Among people without disabilities, the diagnosis rates of BDC were higher in individuals with incomes below the poverty line than in the upper income groups. However, in people with severe disabilities, the lowest diagnosis rate was observed among individuals with incomes below the poverty line. These results demonstrate that the current economic support is not sufficient to overcome barriers to accessing medical services that are faced by low-income, severely disabled people [15]. More comprehensive support is needed in terms of managing physical mobility, provision of care, providing easy-to-read information, and improving the awareness regarding the health problems of disabled people.
The diagnosis rate of BDC also varied according to disability type, with the lowest diagnosis rate observed in people with mental (intellectual or psychological) disabilities. Consistent with a previous report [16], this study revealed that people with mental disabilities had a poorer economic status compared to those with other types of disabilities. Therefore, the poor economic status of patients with mental disabilities may also interfere with BDC diagnosis.
Unknown stages of BDC were more frequently reported for those with severe disabilities or brain or mental disorders. This diagnostic outcome was correlated with a less comprehensive evaluation of the tumor extent. These patients were at the lowest income level, had a higher CCI, or lived in rural areas, which interfered with the proper evaluation of BDC. A previous study in Korea reported that disabilities or comorbidities influence tumor stage at diagnosis [17].
The mean age of patients at BDC diagnosis was slightly younger in those with disabilities than in those without, and this trend was prominent in those with severe disabilities. People with disabilities have a higher CCI and were more likely to live in endemic areas for clonorchiasis, which may lead to the development of BDC at an earlier age. Among the various comorbidities, DM was a risk factor for BDC [18] and was more prevalent in disabled people. In addition, patients with mental disabilities were diagnosed at the youngest age, and had a relatively short average life span [19] that could preclude survival until BDC diagnosis.
The BDC treatment patterns also varied according to disability status. Disabled patients underwent less surgery and chemotherapy compared to those without disabilities. These trends were more prominent in patients with severe disabilities or with brain, mental, or internal organ disabilities. Intensive treatment such as surgical resection and adjuvant or palliative chemotherapy is necessary to achieve a good long-term prognosis in BDC [20]. These results were in line with the results of previous studies on different malignancies [5]. A less comprehensive evaluation of tumor extent and less intensive treatment were associated with a lower survival rate in BDC patients with disabilities than in those without disabilities.
Patients with mental disabilities may not correctly perceive or express their symptoms, which may also delay diagnosis and treatment. Thus, special efforts are needed to obtain accurate information from these patients and to appropriately communicate the treatment that they should receive. For example, experts recommend that interactions with individuals with intellectual disabilities involve plenty of time, simple words, patience, and repeated explanations [21].
In this study, women with severe mental disabilities had a worse prognosis than men despite better overall and cancer-specific mortality. Women usually encounter more disadvantages in life compared to men; thus, when women and men without disabilities are compared, the magnitude of the differences may be lower [16]. Women with disabilities may be more likely than their male counterparts to experience stress due to higher rates of poverty, social isolation, violence, and other forms of victimization as well as chronic health problems [22]. Our results showed that such adverse impacts were exacerbated in female BDC patients with mental disabilities.
In this study, we grouped the 15 types of disabilities (limb, visual, auditory, linguistic, brain, facial, kidney, heart, liver, respiratory system, ostomy, epilepsy, intellectual, autistic, and mental) into the following categories: physical (limb, facial, epilepsy), communication (visual, auditory, linguistic), brain, mental (intellectual, autistic, mental), and internal organ impairment (kidney, heart, liver, lung, intestine). We also classified severity levels into two groups: severe (grades 1–3) and mild (grades 4–6). In this study, disparities were more prominent in those with mental disorders, who were the most disadvantaged for every indicator.
To the best of our knowledge, this is the first study to comprehensively analyze potential disparities in the whole spectrum of BDC patients as they relate to disabilities, including the stage at diagnosis, treatment received, and overall and cancer-specific mortality. The strengths of the study included the large number of participants constituting a representative sample, the inclusion of a wide range of disability types, and accurate disability diagnoses.
However, this study had some limitations. First, the use of population-based registries precluded more detailed analyses regarding the other risk factors of BDC, such as primary sclerosing cholangitis, choledochal cysts, or an anomalous union of the pancreaticobiliary duct. However, these specific risk factors are too rare to be identified in many patients [23]. We evaluated the presence of gallstones and the endemic areas of clonorchiasis, because gallstones [24] and clonorchiasis [25] are major risk factors for BDC in Asian countries. Second, detailed information about treatments, such as surgical pathology or chemotherapy cycles, could not be obtained. Despite these limitations, this is the first study to examine the impacts of disability on the diagnosis and treatment of BDC.
5. Conclusions
In conclusion, this study revealed that Korean patients with disabilities face various barriers in terms of BDC diagnosis and receiving effective treatment. These barriers may prevent patients with disabilities from receiving an early diagnosis, staging work-up, and intensive treatment compared to people without disabilities. Therefore, we suggest that economic support must be combined with social support for people with disabilities, including improved awareness of their disabilities, better provision of general care, better communication strategies, and a more inclusive environment.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/ijerph192416625/s1, Figure S1: Comparison of cancer-specific survival by disability severity; Table S1: Disability categories; Table S2: Baseline characteristics of the target population; Table S3-1: Overall mortality in patients with bile duct cancer; Table S3-2: Overall mortality in men patients diagnosed with bile duct cancer; Table S3-3: Overall mortality in female patients diagnosed with bile duct cancer.
Author Contributions
Conceptualization, S.M.P., S.Y.K. and J.H.P. (Jong Hyock Park); methodology, D.W.S. and J.H.P. (Jong Hyock Park); software, K.E.Y. and J.H.P. (Jong Heon Park); validation, S.Y.K., K.E.Y. and J.H.P. (Jong Heon Park); formal analysis, K.E.Y. and J.H.P. (Jong Heon Park); investigation, S.M.P. and S.Y.K.; resources, S.Y.K. and J.H.P. (Jong Hyock Park); data curation, D.W.S. and J.H.P. (Jong Heon Park); writing—original draft preparation, S.M.P., S.Y.K.; writing—review and editing, J.-H.H. and J.H.P. (Jong Hyock Park); visualization, K.E.Y.; supervision, J.H.P. (Jong Hyock Park); project administration, J.H.P. (Jong Hyock Park); funding acquisition, S.Y.K. and J.H.P. All authors have read and agreed to the published version of the manuscript.
Funding
This work was supported by the R&D grant (No. 2016007) on rehabilitation by Korea National Rehabilitation Center Research Institute, Ministry of Health & Welfare, and the National Research Foundation of Korea (NRF) grant funded by the Ministry of Education (No. 2019R1D1A3A03103862, No. 2022R1I1A3070074) and by the Korea government (MSIT) (2019R1A2C1087507).
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Institutional Review Board of Chungbuk National University (CBNU-201708-BM-501-01; Cheongju, South Korea).
Informed Consent Statement
Patient consent was waived because we used the National Disability Database, the Korean Central Cancer Registry, and the Korean National Health Insurance claims database that are secondary data.
Data Availability Statement
Not applicable.
Acknowledgments
We thank the Korean Ministry of Health and Welfare for its administrative support to link the data, and the Korean National Health Insurance Services for their provision of cancer screening data.
Conflicts of Interest
The authors declare no conflict of interest. The funders had no role in the design of the study; in the collection, analyses, or interpretation of data; in the writing of the manuscript, or in the decision to publish the results.
References
- Antwi, S.O.; Mousa, O.Y.; Patel, T. Racial, ethnic, and age disparities in incidence and survival of intrahepatic cholangiocarcinoma in the United States 1995–2014. Ann. Hepatol. 2018, 17, 604–614. [Google Scholar] [CrossRef] [PubMed]
- Yoon, T.H.; Lee, S.Y.; Kim, C.W.; Kim, S.Y.; Jeong, B.G.; Park, H.K. Inequalities in medical care utilization by South Korean cancer patients according to income: A retrospective cohort study. Int. J. Health. Serv. 2011, 41, 51–66. [Google Scholar] [CrossRef] [PubMed]
- Ko, K.D.; Lee, K.Y.; Cho, B.; Park, M.S.; Son, K.Y.; Ha, J.H.; Park, S.M. Disparities in health-risk behaviors, preventive health care utilizations, and chronic health conditions for people with disabilities: The Korean national health and nutrition examination survey. Arch. Phys. Med. Rehabil. 2011, 92, 1230–1237. [Google Scholar] [CrossRef] [PubMed]
- Shin, D.W.; Lee, J.W.; Jung, J.H.; Han, K.; Kim, S.Y.; Choi, K.S.; Park, J.H.; Park, J.H. Disparities in cervical cancer screening among women with disabilities: A national database study in South Korea. J. Clin. Oncol. 2018, 36, 2778–2786. [Google Scholar] [CrossRef] [PubMed]
- Shin, D.W.; Cho, J.H.; Noh, J.M.; Han, H.; Han, K.; Park, S.H.; Kim, S.Y.; Park, J.H.; Park, J.H.; Kawachi, I. Disparities in the diagnosis and treatment of lung cancer among people with disabilities. J. Thorac. Oncol. 2019, 14, 163–175. [Google Scholar] [CrossRef] [PubMed]
- McCarthy, E.P.; Ngo, L.H.; Roetzheim, R.G.; Chirikos, T.N.; Li, D.; Drews, R.E.; Iezzoni, L.I. Disparities in breast cancer treatment and survival for women with disabilities Ann. Intern. Med. 2006, 145, 637–645. [Google Scholar]
- Kim, Y.E.; Lee, Y.R.; Yoon, S.J.; Kim, Y.A.; Oh, I.H. Years of life lost due to premature death in people with disabilities in Korea: The Korean national burden of disease study framework. J. Korean Med. Sci. 2019, 34, e22. [Google Scholar] [CrossRef] [PubMed]
- Iezzoni, L.I.; Ngo, L.H.; Li, D.; Roetzheim, R.G.; Drews, R.E.; McCarthy, E.P. Treatment disparities for disabled medicare beneficiaries with stage I non-small cell lung cancer. Arch. Phys. Med. Rehabil. 2008, 89, 595–601. [Google Scholar] [CrossRef]
- Horner-Johnson, W.; Dobbertin, K.; Iezzoni, L.I. Disparities in receipt of breast and cervical cancer screening for rural women age 18 to 64 with disabilities. Womens Health Issues 2015, 25, 246–253. [Google Scholar] [CrossRef]
- Park, J.H.; Lee, J.S.; Lee, J.Y.; Gwack, J.; Park, J.H.; Kim, Y.I.; Kim, Y. Disparities between persons with and without disabilities in their participation rates in mass screening. Eur. J. Public Health 2009, 19, 85–90. [Google Scholar] [CrossRef] [PubMed]
- Razumilava, N.; Gores, G.J. Cholangiocarcinoma. Lancet 2014, 383, 2168–2179. [Google Scholar] [CrossRef] [PubMed]
- Korea Central Cancer Registry. Annual Report of Cancer Statistics in Korea in 2017; Ministry of Health and Welfare: Sejong, Korea, 2019.
- Blechacz, B. Cholangiocarcinoma: Current Knowledge and New Developments. Gut Liver 2017, 11, 13–26. [Google Scholar] [CrossRef] [PubMed]
- Statistics Korea. Survey on Persons with Disabilities; Korea Institute for Health and Social Affair: Seoul, Korea, 2011.
- Lee, J.E.; Kim, H.R.; Shin, H.I. Accessibility of medical services for persons with disabilities: Comparison with the general population in Korea. Disabil. Rehabil. 2014, 36, 1728–1734. [Google Scholar] [CrossRef]
- Kavanagh, A.M.; Krnjacki, L.; Aitken, Z.; LaMontagne, A.D.; Beer, A.; Baker, E.; Bentley, R. Intersections between disability, type of impairment, gender and socio-economic disadvantage in a nationally representative sample of 33,101 working-aged Australians. Disabil. Health J. 2015, 8, 191–199. [Google Scholar] [CrossRef] [PubMed]
- Park, B.R.; Kim, S.Y.; Shin, D.W.; Yang, H.K.; Park, J.H. Influence of socioeconomic status, comorbidity, and disability on late-stage cancer diagnosis. Osong Public Health Res. Perspect. 2017, 8, 264–270. [Google Scholar] [CrossRef]
- Petrick, J.L.; Yang, B.; Altekruse, S.F.; Van Dyke, A.L.; Koshiol, J.; Graubard, B.I.; McGlynn, K.A. Risk factors for intrahepatic and extrahepatic cholangiocarcinoma in the United States: A population-based study in SEER-Medicare. PLoS ONE 2017, 12, e0186643. [Google Scholar] [CrossRef]
- Martínez-Leal, R.; Salvador-Carulla, L.; Linehan, C.; Walsh, P.; Weber, G.; Van Hove, G.; Määttä, T.; Azema, B.; Haveman, M.; Buono, S.; et al. The impact of living arrangements and deinstitutionalisation in the health status of persons with intellectual disability in Europe. J. Intellect. Disabil. Res. 2011, 55, 858–872. [Google Scholar] [CrossRef] [PubMed]
- Murakami, Y.; Uemura, K.; Sudo, T.; Hashimoto, Y.; Nakashima, A.; Kondo, N.; Sakabe, R.; Ohge, H.; Sueda, T. Prognostic factors after surgical resection for intrahepatic, hilar, and distal cholangiocarcinoma. Ann. Surg. Oncol. 2011, 18, 651–658. [Google Scholar] [CrossRef] [PubMed]
- Riddle, I.R.; Romelczyk, S.; Sparling, E. Effective Communication for Health Care Providers: A Guide to Caring for People with Disabilities; Center for Disabilities Studies, University of Delaware: Newark, DE, USA, 2011. [Google Scholar]
- Palombi, B. Women with disabilities: The cultural context of disability, feminism, able-bodied privilege, and microaggressions. In The Oxford Handbook of Feminist Multicultural Counseling Psychology; Oxford university press: Oxford, MS, USA, 2018. [Google Scholar]
- Chapman, R.W. Risk factors for biliary tract carcinogenesis. Ann. Oncol. 1999, 10 (Suppl. 4), 308–311. [Google Scholar] [CrossRef] [PubMed]
- Hsing, A.W.; Gao, Y.T.; Han, T.Q.; Rashid, A.; Sakoda, L.C.; Wang, B.S.; Shen, M.C.; Zhang, B.H.; Niwa, S.; Chen, J.; et al. Gallstones and the risk of biliary tract cancer: A population-based study in China. Br. J. Cancer 2007, 97, 1577–1582. [Google Scholar] [CrossRef]
- Shin, H.R.; Oh, J.K.; Lim, M.K.; Shin, A.; Kong, H.J.; Jung, K.W.; Won, Y.J.; Park, S.; Park, S.J.; Hong, S.T. Descriptive epidemiology of cholangiocarcinoma and clonorchiasis in Korea. J. Korean Med. Sci. 2010, 25, 1011–1016. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).