Abstract
(1) Background: Despite the verified relationship between relatives’ characteristics and individual suicidal ideation, few studies have discussed the role of family members and lineal consanguinity independently according to whether they live together with the individuals or not. (2) Methods: The data in this study were collected in November 2019 and identified rural adults over 18 years old in Shandong as the survey objects, with a total of 879 valid cases included in this survey. Logistic regression analysis was employed to examine the risk factors affecting adults’ suicidal ideation and differentiate the effects of a family member and lineal consanguinity’s physical and mental health. Relatives’ physical and mental health were estimated by three aspects: whether they were suffering from chronic diseases, mental illness, or alcoholism. (3) Results: The study showed that a family member’s physical (OR = 2.303, p < 0.01) and mental health (OR = 5.877, p < 0.05) was related to suicidal ideation, but the association between lineal consanguinities’ physical and mental health and suicidal ideation were not supported. People over 40 years old (OR = 6.528, p < 0.05), from only-child families (OR = 4.335, p < 0.01), with household indebtedness (OR = 2.992, p < 0.001), or difficulty falling asleep (OR = 3.165, p < 0.001) had risk factors of suicidal ideation. (4) Conclusions: The physical and mental health of individuals’ family members are related to their suicidal ideation, and their lineal consanguinities’ physical and mental health are not related to suicidal ideation. These findings imply the different associations between family environment, genetic factors, and suicidal ideation. Family members’ health should be considered as a factor to prevent and control suicidal behaviors, including suicidal ideation.
1. Introduction
According to the World Health Organization (WHO)’s estimation, more than 700,000 people die by suicide each year, which means that approximately one person dies by suicide every 40 s in the world [1]. The latest report revealed that the age-standardized suicide rate was 6.7 per 100,000 people in 2019 globally [2]. Suicide not only brings a mental blow to the family but also causes a certain burden of disease and a negative impact on society [3,4,5]. In rural areas, the suicide rate was found to be higher than in urban neighborhoods in many countries around the world [6,7,8]. In China, although the recent suicide rate showed a downward trend [9], suicide is still one of the main causes of death for Chinese rural residents [10]. A study showed that rural areas, where employment and education opportunities were relatively few, accounted for 79 percent of suicides in China [11]. Suicidal ideation (SI), as one kind of suicidal behavior, is the first step of suicidal behavior and a strong predictor of subsequent suicidal behaviors [12,13]. A previous study reported that approximately 13.2% of people who experienced suicidal ideation in the past year attempted suicide [14]. In conclusion, suicidal ideation should be paid close attention to prevent suicide in rural residents.
Many studies have been conducted in recent decades to explore the factors associated with suicidal ideation among different populations [15,16,17,18] as well as the effects of environmental factors on suicide, such as the community and family environment [19,20,21,22,23]. Regarding environmental factors, relatives are closely connected to people’s lives, and their behaviors, experiences, and emotions could affect individuals’ mental health, which had been confirmed in previous studies [24,25,26,27]. While investigating the family consequences of suicide, studies have shown that relatives are affected by suicide and survivors may develop PTSD symptoms and worse mental health [28,29]. In addition to psychological trauma, those survivors also experienced difficulties in social interactions [30]. It was then necessary to provide support from their community, peers, family, and healthcare providers at this time so that they could return to normal life as soon as possible [31,32,33].
In addition, many studies further explored the role of relatives’ characteristics on suicidal ideation. For example, family conflicts, parenting styles, and separated parents were shown to be elements that result in unhealthy emotions and even suicidal behaviors [34,35,36,37]. However, family belongingness and a high educational level of relatives were found to be protective factors against suicidal ideation in different population groups [38,39]. Additionally, support from family was negatively related to suicidal ideation, which is attributed to reducing negative emotions [40,41]. In exploring the influence of relatives, several studies of twins committing suicide and familial cluster suicides confirmed the role of shared environment, showing that among relatives with the same heritability, the more environments they shared and the greater possibility of mutual influence, the higher the risk of suicide [42,43]. Therefore, when considering the effects of relatives on one’s suicidal ideation, the differences among these relatives should be considered. With the shared environment factor confirmed to be associated with suicidal behavior, the associations between living together and suicidal behavior can be assumed. In other words, the connection with suicidal ideation is different between a family member (FM) who lives with the individual and a lineal consanguinity (LC) who does not live with the individual but shares a blood relationship.
Regarding FMs, various studies have found that family characteristics are associated with individuals’ suicidal ideation. Previous studies proved that poor family functioning, family problems, and violence by family members could increase the incidence of suicidal ideation [44,45,46,47]. In addition to these behaviors, several studies indicate that a FM’s health is related to individual suicidal ideation. Concerning physical health, previous literature revealed that severe illness or death of fathers and spouses’ cancer were associated with their FM’s mental status [48]. In China, a study revealed that kids with diagnosed cancer would cause psychological injury to parents, such as desperation and suicidal ideation [49]. In addition to the influence of physical illness, family members suffering from mental illness, such as spouses, parents, and others, may affect the mental status and suicidal ideation of adults [50,51,52]. Alcohol use disorders, as one of the most common mental disorders, result in spousal depression and even suicidal ideation [53]. In addition, another investigation exploring the reasons behind suicidal ideation concluded that relatives’ sickness caused family instability and negative experiences, which could influence different personal life stages and eventually lead to the incidence of negative emotions [4,54,55]. Therefore, the health of FMs has been identified as an influencing factor in suicidal ideation. From another point of view, healthy family members may reduce the probability of suicidal ideation; for example, a suicide management guideline mentioned that the involvement of family members is a protective factor against suicide [56].
For LCs, however, little research has been committed to exploring their effects on suicidal ideation. Only in studies of suicide was the influence of LC’s behavior noticed. For example, a slew of studies showed that suicidal behavior had a tendency for family aggregation [57,58], which means that an attempted or completed suicide in the father’s generation may affect the offspring. In family genetic studies of suicidal behavior, the finding was that impulsive aggregation of a LC may contribute to the familial transmission of suicide [59]. Additionally, another study predicted that the activities or behavior of relatives, such as illegal drug use and aggressive behavior, resulted in a higher risk of suicidal individuals [60]. Hence, the role of LCs in the prevention of suicide has been verified, and it is necessary to further explore its effect on suicidal ideation.
Although the effect of the behavior of a LC on suicide has been identified, few studies have aimed to find the association between a LC’s health and an individual’s suicidal ideation. Furthermore, most studies aimed to observe the influence of relatives’ characteristics on an underage group, rather than adults, but this study focused on the adult population and tried to seek out a new way to prevent adult suicide. In the end, there were few studies examining the differences in the effect of FMs and LCs on suicidal ideation from the perspective of environmental impact. Therefore, the aim of the present study was to investigate the risk factors of suicidal ideation and distinguish the influences of FM’s health and LC’s health with the hope of providing evidence for suicide prevention among rural adults.
2. Materials and Methods
2.1. Participants and Survey Procedure
The data in this study were collected in November 2019. Respondents of this survey are adults over 18 years of age from the Shandong rural areas in China. Data was collected from Taierzhuang of Shandong province. Shandong, a major province of economy and agriculture, is located in eastern China. Seventeen cities are included in Shandong, and Taierzhuang District, seated in the south of Shandong province, belongs to Zaozhuang City. According to data from the seventh census in China, the resident population of the whole Taierzhuang District is 305,102, and inhabitants residing in rural regions account for 53.72% of the whole population [61]. Five towns in Taierzhuang District were all included in this investigation and a village was randomly chosen from each town. All residents over 18 years old in the village participated in this survey as long as they signed the informed consent. In total, 879 residents were included in this study, and the response rate was 94.9% (879/926).
A face-to-face interview was applied in process of collecting data. Interviewers were postgraduate students who had received professional training and were required to understand the whole research. Before the investigation, respondents and their families agreed to provide relevant information and signed a written informed consent form. As for collecting data, interviewers filled in questionnaires following the answers from the respondents. After the investigation, more than two students inspected the contents and modified the wrong or missing items.
2.2. Measures
2.2.1. Suicidal Ideation
The dependent variable of this survey is suicidal ideation. It is evaluated by the question “Have you ever seriously thought over committing suicide?” There existed two answers to this question, “yes” or “no”. Respondents were required to answer this question honestly based on if this thought had ever occurred in their whole life. This question had been used to evaluate suicidal ideation in many previous studies, such as in the exploration of suicidal ideation in college students and adults [20,35].
2.2.2. FM’s and LC’s Health
According to Chinese traditional habits, a FM refers to relatives living together with individuals currently, and a LC includes relatives who do not live together as adults but have blood relationships, such as uncles, brothers, and sisters. Investigators were asked to explain the differences between two types of relatives in the process of inquiring since the difference between living together and being related needed to be focused on and differentiated.
The health condition of relatives was estimated separately in this study. For FMs, the answer to the question “If your FM suffer from severe chronic diseases?” was used to represent physical health. As for mental health, alcohol use disorders were considered as one mental disorder based on a report from WHO [62]. Therefore, mental health was estimated by two questions. The first question was “If your FM suffer from severe mental illness?” and the other one was “If your FM indulge in excessive drinking?”. There were two answers to all questions, “yes” or “no”. For LCs, the inquiries were similar to the questions for FMs. Regarding physical health, this study used the question “If your LC suffer from severe chronic diseases?” for estimation. Mental health was addressed using the two questions, “If your LC suffer from severe mental illness?” and “If your LC indulge in excessive drinking?”.
2.2.3. Socio-Demographic Characteristics
The questionnaire also involved basic socio-demographic information, such as gender, age, occupation, marriage status, education level, and family composition. Gender was divided into two categories: male and female. Age was obtained by subtracting the year of birth from the current year and classified as 18–40 and >40 years old. Occupation types included farmers, students, personnel of public institutions, businessmen, and so on, but the occupation was reclassified into two categories, “freelancer” and “others”, for the convenience of data analysis. Marriage status was represented by married and other conditions “unmarried, divorced and widowed”. Considering the low educational level in rural areas, junior high school education was selected as the dividing line, and results were classified into primary school education and below and junior high school education level and above. The familial composition was evaluated by one question “Were you an only child?”
2.2.4. Household Indebtedness and Difficulty Falling Asleep
In addition to the above variables, household indebtedness and sleeping difficulty were also risk factors. The household indebtedness condition was estimated by the question “Was your family in debt?”, with two choices of answers, “yes” or “no”. Cannot fall asleep within 30 min was defined as difficulty falling asleep according to the PSQI, and there were four levels of the answer, “not”, “once a week”, “twice a week”, and “three times a week and above”. Similarly, we grouped the answers into two categories “yes” or “no” in the analysis of data.
2.3. Data Management and Analysis
IBM SPSS Statistics 26.0 was the main software for analyzing data. The Chi-square test was used to describe social-demographic characteristics and discover the single risk factors of suicidal ideation. Logistic regression analysis, differing from single-factor analysis, was applied to examine the effects of multiple independent variables on suicidal ideation. We coded all answers as “1” and “0” and considered the results to be statistically significant when the p-value was less than 0.05.
3. Results
3.1. Demographic Characteristics and Suicidal Ideation of the Sample
Table 1 presents the demographic characteristics of the sample, and a single-factor analysis for suicidal ideation was included in this table. A total of 879 sample cases were conducted in this study, of which, 322 were males and 557 were females. Results showed that 60 (6.83%) cases of rural residents had experienced suicidal ideation.

Table 1.
Characteristics and univariate analysis of suicidal ideation among the samples.
In Figure 1, for all the relatives, the results of the single-factor analysis indicated that there existed no significant differences in the incidence of suicidal ideation in relatives whether with mental illness and with alcoholism or not. According to the results, relatives with chronic disease (4.87% vs. 10.92%, p < 0.001) were associated with suicidal ideation. After classification, however, only having a FM with a chronic disease (5.16% vs. 11.82%, p < 0.001), mental illness (6.46% vs. 17.86%, p < 0.05), or alcoholism (6.39% vs. 14.00%, p < 0.05) were considered as risk factors.
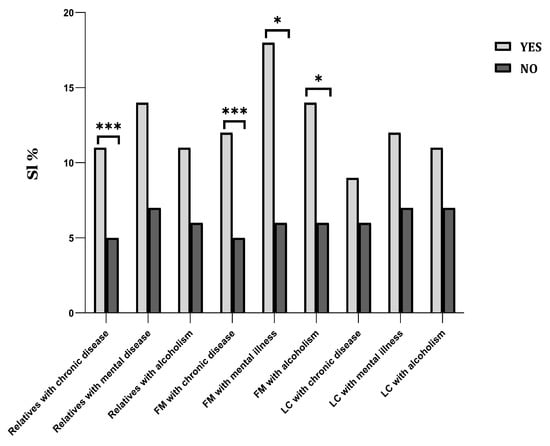
Figure 1.
Visual comparisons for suicidal ideation under different relatives’ characteristics. Note: FM = Family member, LC = lineal consanguinity, and SI = suicidal ideation; * p < 0.05, *** p < 0.001.
Regarding other factors in Table 1, the results of the single-factor analysis indicated that there existed no significant differences between different sexes, occupations, and marital statuses. The population over 40 years old, compared to the 18–40 population (8.17% vs. 1.18%, p < 0.001), had a higher prevalence of suicidal ideation. While comparing people with a junior high school degree and above (8.66% vs. 3.51%, p < 0.01), those with fewer years of education had a higher prevalence of suicidal ideation. Comparisons were also conducted between only-child families and multiple-child families; the result showed that people from only-child families (6.38% vs. 18.18%, p < 0.01) had a higher incidence of suicidal ideation. Regarding other conditions, risk factors included household indebtedness (4.66% vs. 12.06%, p < 0.001) and falling asleep with difficulty (3.37% vs. 12.17%, p < 0.001).
3.2. Logistic Regression Analysis of Suicidal Ideation
For further analysis of factors related to suicidal ideation in rural residents, suicidal ideation as the dependent variable, and demographic characteristics, sleep status, and relatives’ health as the independent variables, were included in Model 1 of the logistic regression analysis. All of the results are shown in Table 2. Results showed that an age > 40 (OR = 5.525, p = 0.026), from an only-child family (OR = 4.511, p = 0.004), household indebtedness (OR = 2.899, p < 0.001), difficulty falling asleep (OR = 3.057, p < 0.001), and relatives with chronic disease (OR = 2.051, p = 0.012) were associated with suicidal ideation. In Model 2, we classified the relatives further and included the variables on FM’s health and LC’s health. The results showed that an age >40 (OR = 6.528, p = 0.018), from an only child family (OR = 4.335, p = 0.006), household indebtedness (OR = 2.992, p < 0.001), difficulty falling asleep (OR = 3.165, p < 0.001), and a FM with chronic illness (OR = 2.303, p = 0.008) or mental illness (OR = 5.877, p = 0.028) were risk factors of suicidal ideation.

Table 2.
Logistic regression analysis of risk factors associated with suicidal ideation among rural adults {OR (95%CI)}.
4. Discussion
In this study, the main objective was to identify the influencing factors of suicidal ideation and differentiate the effect of FMs’ and LCs’ health on suicidal ideation among rural adults. Results showed that the prevalence of suicidal ideation in rural residents was 6.83% in this survey, which was close to the estimation of other studies, such as research in rural areas of Shandong Province and Zhejiang Province [63,64,65]. The relevant risk factors resulting in suicidal ideation included an age >40, an only child family, household indebtedness, and difficulty falling asleep. Concerning the effect of relatives’ health, the association between relatives with chronic disease and suicidal ideation was confirmed. The influences of relatives were then discussed from two aspects: FMs’ health and LCs’ health. To be specific, FMs’ health was more related to suicidal ideation compared to LCs’ health, and adults whose FMs had a chronic disease or mental illness were at a higher risk for suicidal ideation. For rural residents, family characteristics could affect one’s mental status [66,67]; the role of a FM’s health on suicidal ideation was proved in a study in rural Haiti, which was consistent with this result [68]. This could be because rural residents live in distant areas that lack transportation and sufficient income [69], and a FM’s illness may lead to increased pressure on individuals on account of less social service available.
Collectively, this study observed that relatives with chronic disease were associated with individuals’ suicidal ideation firstly, which was consistent with results concluded by previous research. Regarding this, relatives’ physical health was determined to be a risk factor affecting suicidal ideation in past studies [48,49]. The reasons for this relevance cause concern and explorations were presented in numerous studies. For example, a previous survey explained that a person developed fear or anxiety about losing a loved one after a relative was diagnosed with a pathogenic chronic disease [70]. Another study suggested that negative emotions from diagnosed relatives would cause an individual passive psychological experience [71]. Further analysis explaining this reason indicated that these passive psychological experiences were predictors of suicidal ideation, such as depression, anxiety, and hopelessness, in past findings [72,73,74]. Hence, the effect of the physical health of relatives on suicidal ideation was well established, and further exploration of relatives’ health needs to be carried out on this basis.
In the comparison of FMs and LCs, we found that FMs who suffer from chronic disease and mental illness had a strong connection with suicidal ideation, but a LC’s health was not associated with it. The greatest distinction between FMs and LCs lay in whether they live with the individual, that is, FMs share the living environment and LCs do not. Further exploration demonstrated that a safe family, public, and hospital environment were necessary for the prevention of suicide in adults. Relatedly, the environment was found to be a factor associated with the suicide rate of the elderly [75,76]. Studies found that adults would feel anxious and stressed while living together with diseased relatives [77], and even hopelessness or anxiety could be produced in the process of care and treatment [78]. Meanwhile, a previous result also showed that a FM’s chronic disease had a great connection with the negative emotions of adults, and unfavorable economic situations increased opportunities for one’s emotional distress [79]. Therefore, a FM’s chronic disease and mental illness could lead to suicidal ideation by means of the environment and negative emotions. However, there was no significant association between suicidal ideation and relatives with alcoholism in this study, whether in FMs or LCs. Previous studies supported that parental alcoholism had no direct impact on students’ suicidal ideation [80,81]. However, other hypotheses verified that spousal alcohol abuse may result in women’s suicidal behaviors [82,83]. As a result, further investigation into the effect of a FM’s or LC’s alcoholism needs to be launched and discussed.
Regarding other factors, the present study also found that there was a greater possibility of suicidal ideation in people over 40 years old. Previous studies also indicated that the prevalence of suicidal ideation in the middle-aged and elderly group was associated with loneliness, household financial problems, and poor perceived health [84,85]. This study also revealed that the prevalence of suicidal ideation was higher in people from only-child families, which was consistent with a previous result [86]. Experts explained that elderly people from rural areas, with a lack of pension provision and children, generally had a sense of responsibility to their parents, which resulted in an increase in the stress of life as an only child [87]. Therefore, more care should be given to rural adults for preventing suicide. This finding also demonstrated that household indebtedness was a risk factor influencing adults’ suicidal ideation. Similarly, a previous study mentioned that people with increased economic pressure caused by over-indebtedness were in danger of mental health problems, and the connection between the two varied depending on the debt amount and debt sources [88,89]. Difficulty falling asleep was identified as significant in this study of factors affecting suicidal ideation, which is consistent with the conclusions from previous studies [90,91]. A study of Australian adults showed that difficulty falling asleep, as one specific aspect of sleep disorder, strongly influenced the prevalence of suicidal ideation and played an independent role [92].
Collectively, a FM’s physical and mental health status, as one kind of factor of the living environment, could affect an individual’s mood and behaviors. Specific reasons may be the stress as a caregiver and negative emotions caused by the disease while living together. Furthermore, people over 40 years old, people from only-child families, people with household indebtedness, and people with difficulty falling asleep were considered to be in high-risk groups who were more likely to have suicidal ideation.
In this study, certain limitations should be considered. Firstly, the study only opened an investigation and collected data from rural areas of Taierzhuang District, and we should be cautious when interpreting the findings into other populations and regions. Secondly, the data of this study came from the self-reporting of respondents, which may have recall bias. Next, although on a large scale, differences between the effect of FMs and LCs on suicidal ideation were explored, but exact reasons for these differences were not evidenced in this study. Finally, the present study did not discover the effects of FMs’ and LCs’ alcoholism on suicidal ideation in adults, so further validation is required in future studies.
5. Conclusions
In conclusion, the prevalence of suicidal ideation in Shandong rural adults was 6.83%. Before categorization, only relatives with chronic disease were a risk factor for suicidal ideation. Comparing the influences of relatives’ health, results indicated that FMs who suffered from chronic disease and mental illness made an impact on suicidal ideation, and an evident correlation was not found in LCs. This difference reminded us that the psychological condition of adults with a FM suffering from health disorders should be monitored closely. In addition to studying the impact of relatives’ health on suicidal ideation, there needs to be more attention paid to people over 40 years old, people from only-child families, people with household indebtedness, and people with difficulty initiating sleep.
Focusing on adults with a FM suffering from physical and mental illness and publicizing the influence of the living environment on suicidal ideation are crucial. Hence, more measures need to be taken for reducing suicidal ideation by the melioration of FMs’ physical and mental health. More action needs to be taken in the community after identifying the impact of family members’ health on an individual’s suicidal ideation. The government should encourage the community to pay more attention to the mental health of a patient’s family members for the purpose of suicide prevention. Further, doctors need to focus on the role of relatives in the treatment of suicide, in order to reduce the suicide rate of rural residents, make suicide prevention and intervention plans based on the home environment, provide more social and psychological services, and improve family happiness for rural adults.
Author Contributions
Writing and data analysis, C.L.; Data collection, Z.W. and Y.W.; Guidance and supervision, L.S. All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by the National Natural Science Foundation of China [grant number 71974114].
Institutional Review Board Statement
The study was conducted in accordance with the Declaration of Helsinki, and approved by the Institutional Review Board (or Ethics Committee) of the School of Public Health, Shandong University (protocol code 20190802 and date of approval 9 August 2019).
Informed Consent Statement
Informed consent was obtained from all subjects involved in the study. Written informed consent has been obtained from the patient(s) to publish this paper.
Data Availability Statement
The data presented in this study are available on request from the corresponding author. The data are not publicly available due to the privacy of survey respondents.
Acknowledgments
We express gratitude to the subjects for their participation and cooperation. Furthermore, we also thank all interviewers for their efforts and help in this investigation.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Chadha, S.; Kamenov, K.; Cieza, A. The world report on hearing, 2021. Bull. World Health Organ. 2021, 99, 242. [Google Scholar] [CrossRef] [PubMed]
- WHO. Suicide Worldwide in 2019: Global Health Estimates; WHO: Geneva, Swtizerland, 2021.
- Anders, M. Suicide a serious health and social problem with the possibility of prevention. Cas. Lek. Cesk. 2017, 156, 58–67. [Google Scholar] [PubMed]
- McLaughlin, C.; McGowan, I.; O’Neill, S.; Kernohan, G. The burden of living with and caring for a suicidal family member. J. Ment. Health 2014, 23, 236–240. [Google Scholar] [CrossRef] [PubMed]
- McPhillips, R.; Nafees, S.; Elahi, A.; Batool, S.; Krishna, M.; Krayer, A.; Huxley, P.; Chaudhry, N.; Robinson, C. Knowledge, attitudes and experiences of self-harm and suicide in low-income and middle-income countries: Protocol for a systematic review. BMJ Open 2021, 11, e041645. [Google Scholar] [CrossRef]
- Liu, X.K.; Li, Q.F.; Han, D.C.; Cheng, W.; Song, N.; Hu, M.; Xiao, S.Y. The association between sleep and suicidality in the presence and absence of depressive symptoms: A cross-sectional study in rural China. Medicine 2022, 101, e29725. [Google Scholar] [CrossRef]
- Mohatt, N.V.; Kreisel, C.J.; Hoffberg, A.S.; Beehler, S.J. A Systematic Review of Factors Impacting Suicide Risk Among Rural Adults in the United States. J. Rural Health 2021, 37, 565–575. [Google Scholar] [CrossRef]
- Park, B.C.; Lester, D. Rural and urban suicide in South Korea. Psychol. Rep. 2012, 111, 495–497. [Google Scholar] [CrossRef]
- Yu, H.; Nie, C.; Zhou, Y.; Wang, X.; Wang, H.; Shi, X. Suicides in China from 2008–2017: A longitudinal epidemological study. Int. J. Crit. Illn. Inj. Sci. 2020, 10, 88–91. [Google Scholar]
- Li, M.; Katikireddi, S.V. Urban-rural inequalities in suicide among elderly people in China: A systematic review and meta-analysis. Int. J. Equity Health 2019, 18, 2. [Google Scholar] [CrossRef]
- Wang, C.W.; Chan, C.L.; Yip, P.S. Suicide rates in China from 2002 to 2011: An update. Soc. Psychiatry Psychiatr. Epidemiol. 2014, 49, 929–941. [Google Scholar] [CrossRef]
- Wolford-Clevenger, C.; Stuart, G.L.; Elledge, L.C.; McNulty, J.K.; Spirito, A. Proximal Correlates of Suicidal Ideation and Behaviors: A Test of the Interpersonal-Psychological Theory of Suicide. Suicide Life Threat. Behav. 2020, 50, 249–262. [Google Scholar] [CrossRef] [PubMed]
- Farooq, S.; Tunmore, J.; Ali, M.W.; Ayub, M. Suicide, self-harm and suicidal ideation during COVID-19: A systematic review. Psychiatry Res. 2021, 306, 114228. [Google Scholar] [CrossRef] [PubMed]
- Han, B.; Compton, W.M.; Gfroerer, J.; McKeon, R. Prevalence and correlates of past 12-month suicide attempt among adults with past-year suicidal ideation in the United States. J. Clin. Psychiatry 2015, 76, 295–302. [Google Scholar] [CrossRef] [PubMed]
- Yang, X.; Tian, K.; Wang, D.; Liu, G.; Liu, X.; Harrison, P. State Anhedonia and Suicidal Ideation in Adolescents. Crisis 2021, 42, 247–254. [Google Scholar] [CrossRef] [PubMed]
- Waters, A.F.; Peltier, M.R.; Roys, M.R.; Stewart, S.A.; Copeland, A.L. Smoking and suicidal ideation among college students: Smoking expectancies as potential moderators. J. Am. Coll. Health 2021, 69, 951–958. [Google Scholar] [CrossRef]
- Hwang, I.C.; Ahn, H.Y. Association between handgrip strength and suicidal ideation in Korean adults. J. Affect. Disord. 2021, 278, 477–480. [Google Scholar] [CrossRef]
- Sim, H.S.; Lee, S.G.; Kim, T.H. Physical Functioning, Depressive Symptoms, and Suicidal Ideation among Older Korean Adults. Int. J. Environ. Res. Public Health 2021, 18, 8781. [Google Scholar] [CrossRef]
- Zhang, J.; Sun, L. Suicide ideation and acceptability among females aged 15 to 34 years in rural China. J. Nerv. Ment. Dis. 2014, 202, 161–166. [Google Scholar] [CrossRef]
- Hwang, I.C.; Ahn, H.Y. Association between neighborhood environments and suicidal ideation among Korean adults. J. Affect. Disord. 2021, 295, 488–491. [Google Scholar] [CrossRef]
- Zhou, R.; Zhang, J. Effects of community stress and problems on residents’ psychopathology. Psychiatry Res. 2014, 215, 394–400. [Google Scholar] [CrossRef][Green Version]
- Lin, F.G.; Lin, J.D.; Hsieh, Y.H.; Chang, C.Y. Quarrelsome family environment as an enhanced factor on child suicidal ideation. Res. Dev. Disabil. 2014, 35, 3245–3253. [Google Scholar] [CrossRef] [PubMed]
- Shin, S.H.; Ko, S.J.; Yang, Y.J.; Oh, H.S.; Jang, M.Y.; Choi, J.M. Comparison of boys’ and girls’ families for actor and partner effect of stress, depression and parent-adolescent communication on middle school students’ suicidal ideation: Triadic data analysis. J. Korean Acad. Nurs. 2014, 44, 317–327. [Google Scholar] [CrossRef] [PubMed]
- Doi, S.; Fujiwara, T.; Isumi, A. Association between maternal adverse childhood experiences and mental health problems in offspring: An intergenerational study. Dev. Psychopathol. 2021, 33, 1041–1058. [Google Scholar] [CrossRef] [PubMed]
- Thapa, D.K.; Visentin, D.; Kornhaber, R.; Cleary, M. Migration of adult children and mental health of older parents ‘left behind’: An integrative review. PLoS ONE 2018, 13, e0205665. [Google Scholar] [CrossRef] [PubMed]
- Rafiq, M.; Sadiq, R. Caregiver Stress, Perceived Stigma and Mental Health in Female Family Members of Drug Addicts: Correlational Study. J. Pak Med. Assoc. 2019, 69, 1300–1303. [Google Scholar]
- Cobham, V.E.; McDermott, B.; Haslam, D.; Sanders, M.R. The Role of Parents, Parenting and the Family Environment in Children’s Post-Disaster Mental Health. Curr. Psychiatry Rep. 2016, 18, 53. [Google Scholar] [CrossRef]
- Erlangsen, A.; Fleischer, E.; Gunnell, D.; Nordentoft, M. Characteristics of Survivors of Suicide Seeking Counseling From an NGO in Denmark: Analyses of a National Database. Arch. Suicide Res. 2022, 26, 1362–1377. [Google Scholar] [CrossRef]
- Mitchell, A.M.; Terhorst, L. PTSD Symptoms in Survivors Bereaved by the Suicide of a Significant Other. J. Am. Psychiatr. Nurses Assoc. 2017, 23, 61–65. [Google Scholar] [CrossRef]
- McMenamy, J.M.; Jordan, J.R.; Mitchell, A.M. What do suicide survivors tell us they need? Results of a pilot study. Suicide Life Threat. Behav. 2008, 38, 375–389. [Google Scholar] [CrossRef]
- Barlow, C.A.; Waegemakers Schiff, J.; Chugh, U.; Rawlinson, D.; Hides, E.; Leith, J. An evaluation of a suicide bereavement peer support program. Death Stud. 2010, 34, 915–930. [Google Scholar] [CrossRef]
- Castelli Dransart, D.A. Reclaiming and Reshaping Life: Patterns of Reconstruction After the Suicide of a Loved One. Qual. Health Res. 2017, 27, 994–1005. [Google Scholar] [CrossRef] [PubMed]
- Dyregrov, K.; Dyregrov, A.; Nordanger, D. Support to relatives after suicide. Tidsskr. Nor. Laegeforening Tidsskr. Prakt. Med. Raekke 1999, 119, 4010–4015. [Google Scholar]
- Chae, W.; Park, E.C.; Jang, S.I. Suicidal ideation from parents to their children: An association between parent’s suicidal ideation and their children’s suicidal ideation in South Korea. Compr. Psychiatry 2020, 101, 152181. [Google Scholar] [CrossRef]
- Sun, L.; Zhou, C.; Xu, L.; Li, S.; Kong, F.; Chu, J. Suicidal ideation, plans and attempts among medical college students in china: The effect of their parental characteristics. Psychiatry Res. 2017, 247, 139–143. [Google Scholar] [CrossRef] [PubMed]
- Chahine, M.; Salameh, P.; Haddad, C.; Sacre, H.; Soufia, M.; Akel, M.; Obeid, S.; Hallit, R.; Hallit, S. Suicidal ideation among Lebanese adolescents: Scale validation, prevalence and correlates. BMC Psychiatry 2020, 20, 304. [Google Scholar] [CrossRef]
- da Silva, R.M.; do Nascimento Mangas, R.M.; Figueiredo, A.E.B.; de Souza Vieira, J.E.; de Sousa, G.S.; de Souza Cavalcanti, A.M.T.; de Souza Apolinário, A.V. The influence of family problems and conflicts on suicidal ideation and suicide attempts in elderly people. Cien. Saude. Colet. 2015, 20, 1703–1710. [Google Scholar]
- Chen, Y.; Zhu, L.J.; Fang, Z.M.; Wu, N.; Du, M.X.; Jiang, M.M.; Wang, J.; Yao, Y.S.; Zhou, C.C. The Association of Suicidal Ideation With Family Characteristics and Social Support of the First Batch of Students Returning to a College During the COVID-19 Epidemic Period: A Cross Sectional Study in China. Front. Psychiatry 2021, 12, 653245. [Google Scholar] [CrossRef]
- Parra, L.A.; van Bergen, D.D.; Dumon, E.; Kretschmer, T.; La Roi, C.; Portzky, G.; Frost, D.M. Family Belongingness Attenuates Entrapment and Buffers Its Association with Suicidal Ideation in a Sample of Dutch Sexual Minority Emerging Adults. Arch. Sex Behav. 2021, 50, 983–1001. [Google Scholar] [CrossRef]
- Kerr, D.C.; Preuss, L.J.; King, C.A. Suicidal adolescents’ social support from family and peers: Gender-specific associations with psychopathology. J. Abnorm. Child Psychol. 2006, 34, 103–114. [Google Scholar] [CrossRef]
- Boyd, D.T.; Quinn, C.R.; Jones, K.V.; Beer, O.W. Suicidal ideations and Attempts Within the Family Context: The Role of Parent Support, Bonding, and Peer Experiences with Suicidal Behaviors. J. Racial Ethn. Health Disparities 2022, 9, 1740–1749. [Google Scholar] [CrossRef]
- Linker, J.; Gillespie, N.A.; Maes, H.; Eaves, L.; Silberg, J.L. Suicidal ideation, depression, and conduct disorder in a sample of adolescent and young adult twins. Suicide Life Threat. Behav. 2012, 42, 426–436. [Google Scholar] [CrossRef] [PubMed]
- Tidemalm, D.; Runeson, B.; Waern, M.; Frisell, T.; Carlström, E.; Lichtenstein, P.; Långström, N. Familial clustering of suicide risk: A total population study of 11.4 million individuals. Psychol. Med. 2011, 41, 2527–2534. [Google Scholar] [CrossRef] [PubMed]
- Cong, C.W.; Ling, W.S.; Fitriana, M. Family functioning, coping strategy, and suicidal ideation among adolescents. J. Child Adolesc. Ment. Health 2020, 32, 131–140. [Google Scholar] [CrossRef] [PubMed]
- Ohtaki, Y.; Doki, S.; Kaneko, H.; Hirai, Y.; Oi, Y.; Sasahara, S.; Matsuzaki, I. Relationship between suicidal ideation and family problems among young callers to the Japanese crisis hotline. PLoS ONE 2019, 14, e0220493. [Google Scholar] [CrossRef] [PubMed]
- Carpena, M.X.; Costa, F.D.S.; Martins-Silva, T.; Xavier, M.O.; de Mola, C.L. Why Brazilian women suffer more from depression and suicidal ideation: A mediation analysis of the role of violence. Braz. J. Psychiatry 2020, 42, 469–474. [Google Scholar] [CrossRef]
- Guo, Y.; Ji, Y.; Huang, Y.; Jin, M.; Lin, Y.; Chen, Y.; Zhang, L.; Zhu, C.; Yu, F.; Wang, K. The Relationship Between Suicidal Ideation and Parental Attachment Among Adolescents: The Mediator of Anhedonia and Peer Attachment. Front. Psychol. 2021, 12, 727088. [Google Scholar] [CrossRef]
- Legleye, S.; Beck, F.; Peretti-Watel, P.; Chau, N.; Firdion, J. Suicidal ideation among young French adults: Association with occupation, family, sexual activity, personal background and drug use. J. Affect. Disord. 2010, 123, 108–115. [Google Scholar] [CrossRef]
- Chen, H.; He, Q.; Zeng, Y.; Wang, L.; Yu, H.; Yin, W.; Jiang, Y.; Liu, L. Feeling like the sky is falling down: Experiences of parents of adolescents diagnosed with cancer in one-child families in China—A qualitative study. J. Clin. Nurs. 2022, 31, 733–743. [Google Scholar] [CrossRef]
- Baek, J.; Youm, Y.; Kim, H.C. Gender differences in the longitudinal association between husbands’ and wives’ depressive symptoms among Korean older adults: The moderating effects of the spousal relationship. Qual. Life Res. 2021, 30, 3535–3546. [Google Scholar] [CrossRef]
- Atwoli, L.; Nock, M.K.; Williams, D.R.; Stein, D.J. Association between parental psychopathology and suicidal behavior among adult offspring: Results from the cross-sectional South African Stress and Health survey. BMC Psychiatry 2014, 14, 65. [Google Scholar] [CrossRef]
- Dos Santos Treichel, C.A.; da Rosa Jardim, V.M.; Kantorski, L.P.; Lima, M.G. Prevalence and factors associated with suicidal ideation among family caregivers of people with mental disorders. J. Clin. Nurs. 2019, 28, 3470–3477. [Google Scholar] [CrossRef] [PubMed]
- Min, J.; Yorgason, J.B.; Fast, J.; Chudyk, A. The Impact of Spouse’s Illness on Depressive Symptoms: The Roles of Spousal Caregiving and Marital Satisfaction. J. Gerontol. B Psychol. Sci. Soc. Sci. 2020, 75, 1548–1557. [Google Scholar] [CrossRef]
- Oladeji, B.D.; Gureje, O. Parental mental disorders and suicidal behavior in the Nigerian survey of mental health and well-being. Arch. Suicide Res. 2011, 15, 372–383. [Google Scholar] [CrossRef] [PubMed]
- Fukunishi, I.; Hosokawa, K. A study of psychological aspects of families living together with senile dementia. Jpn. J. Psychiatry Neurol. 1990, 44, 19–24. [Google Scholar] [CrossRef] [PubMed]
- Panesar, B.; Soni, D.; Khan, M.I.; Bdair, F.; Holek, M.; Tahir, T.; Woo, J.; Khumalo, N.; Thabane, L.; Samaan, Z. National suicide management guidelines with family as an interv’ention and suicide mortality rates: A systematic review protocol. BMJ Open 2020, 10, e034694. [Google Scholar] [CrossRef]
- World Health Organization. Preventing Suicide: A Global Imperative; World Health Organization: Geneva, Swtizerland, 2014.
- Qin, P.; Agerbo, E.; Mortensen, P.B. Suicide risk in relation to family history of completed suicide and psychiatric disorders: A nested case-control study based on longitudinal registers. Lancet 2002, 360, 1126–1130. [Google Scholar] [CrossRef] [PubMed]
- Brent, D.A.; Mann, J.J. Family genetic studies, suicide, and suicidal behavior. Am. J. Med. Genet. C Semin. Med. Genet. 2005, 133, 13–24. [Google Scholar] [CrossRef]
- Kim, C.D.; Séguin, M.; Therrien, N.; Riopel, G.; Chawky, N.; Lesage, A.D.; Turecki, G. Familial aggregation of suicidal behavior: A family study of male suicide completers from the general population. Am. J. Psychiatry 2005, 162, 1017–1019. [Google Scholar] [CrossRef]
- Taierzhuang District Bureau of Statistics. Bulletin of the Seventh National Census of Taierzhuang District; Seventh Census Commission Beijing: Beijing, China, 2021. [Google Scholar]
- WHO. WHO Simplifies Treatment of Mental and Neurological Disorders. 2010 [cited 2010 12-10]. Available online: https://www.who.int/news/item/10-12-2010-who-simplifies-treatment-of-mental-and-neurological-disorders (accessed on 26 March 2022).
- Jing, Z.; Li, J.; Fu, P.P.; Wang, Y.; Yuan, Y.; Zhao, D.; Hao, W.; Yu, C.; Zhou, C. Physical multimorbidity and lifetime suicidal ideation and plans among rural older adults: The mediating role of psychological distress. BMC Psychiatry 2021, 21, 78. [Google Scholar] [CrossRef]
- Zhang, J.; Stewart, R.; Phillips, M.; Shi, Q.; Prince, M. Pesticide exposure and suicidal ideation in rural communities in Zhejiang province, China. Bull. World Health Organ. 2009, 87, 745–753. [Google Scholar]
- Lu, L.; Xu, L.; Luan, X.; Sun, L.; Li, J.; Qin, W.; Zhang, J.; Jing, X.; Wang, Y.; Xia, Y.; et al. Gender difference in suicidal ideation and related factors among rural elderly: A cross-sectional study in Shandong, China. Ann. Gen. Psychiatry 2020, 19, 2. [Google Scholar] [CrossRef] [PubMed]
- Chen, X.; Su, J.; Jia, C.; Ma, Z.; Wang, G.; Zhou, L. The impact of suicidal death of rural older people to their relatives: Results from a national psychological autopsy study in China. J. Affect. Disord. 2019, 257, 307–313. [Google Scholar] [CrossRef] [PubMed]
- Lee, H. Personal and interpersonal factors related to suicidal ideation among rural vietnamese adolescents. Southeast Asian J. Trop. Med. Public Health 2016, 47, 1366–1378. [Google Scholar] [PubMed]
- Wagenaar, B.H.; Hagaman, A.K.; Kaiser, B.N.; McLean, K.E.; Kohrt, B.A. Depression, suicidal ideation, and associated factors: A cross-sectional study in rural Haiti. BMC Psychiatry 2012, 12, 149. [Google Scholar] [CrossRef]
- Chiu, H.F.K.; Dai, J.; Xiang, Y.T.; Chan, S.S.M.; Leung, T.; Yu, X.; Hou, Z.J.; Ungvari, G.S.; Caine, E.D. Suicidal thoughts and behaviors in older adults in rural China: A preliminary study. Int. J. Geriatr. Psychiatry 2012, 27, 1124–1130. [Google Scholar] [CrossRef]
- Inhestern, L.; Haller, A.-C.; Wlodarczyk, O.; Bergelt, C. Psychosocial Interventions for Families with Parental Cancer and Barriers and Facilitators to Implementation and Use—A Systematic Review. PLoS ONE 2016, 11, e0156967. [Google Scholar] [CrossRef]
- Hesamzadeh, A.; Dalvandi, A.; Maddah, S.B.; Khoshknab, M.F.; Ahmadi, F. Family Adaptation to Stroke: A Metasynthesis of Qualitative Research based on Double ABCX Model. Asian Nurs. Res. (Korean Soc. Nurs. Sci.) 2015, 9, 177–184. [Google Scholar] [CrossRef]
- Ribeiro, J.D.; Huang, X.; Fox, K.R.; Franklin, J.C. Depression and hopelessness as risk factors for suicide ideation, attempts and death: Meta-analysis of longitudinal studies. Br. J. Psychiatry 2018, 212, 279–286. [Google Scholar] [CrossRef]
- Pramukti, I.; Strong, C.; Sitthimongkol, Y.; Setiawan, A.; Pandin, M.G.R.; Yen, C.-F.; Lin, C.-Y.; Griffiths, M.D.; Ko, N.-Y. Anxiety and Suicidal Thoughts During the COVID-19 Pandemic: Cross-Country Comparative Study Among Indonesian, Taiwanese, and Thai University Students. J. Med. Internet. Res. 2020, 22, e24487. [Google Scholar] [CrossRef]
- Núñez, D.; Monjes, P.; Campos, S.; Wigman, J.T.W. Evidence for Specific Associations Between Depressive Symptoms, Psychotic Experiences, and Suicidal Ideation in Chilean Adolescents From the General Population. Front. Psychiatry 2020, 11, 552343. [Google Scholar] [CrossRef]
- Rihmer, Z.; Németh, A.; Kurimay, T.; Perczel-Forintos, D.; Purebl, G.; Döme, P. Recognition, care and prevention of suicidal behaviour in adults. Psychiatr. Hung. 2017, 32, 4–40. [Google Scholar] [PubMed]
- Jang, H.; Lee, W.; Kim, Y.-O.; Kim, H. Suicide rate and social environment characteristics in South Korea: The roles of socioeconomic, demographic, urbanicity, general health behaviors, and other environmental factors on suicide rate. BMC Public Health 2022, 22, 410. [Google Scholar] [CrossRef] [PubMed]
- Landefeld, C.S.; Winker, M.A.; Chernof, B. Clinical care in the aging century--announcing “Care of the aging patient: From evidence to action”. JAMA 2009, 302, 2703–2704. [Google Scholar] [CrossRef] [PubMed]
- Ma, S.-W.; Lai, S.; Yang, Y.-Y.; Zhou, Z.; Yang, B.-T.; Zheng, G.-Z.; Gao, J.; Lu, L. Relationships Between Anxiety Symptoms, Hopelessness and Suicidal Ideation Among Parental Caregivers of Mandarin-Speaking Children With Speech Impairment: The Mediating Effect of Depressive Symptoms. Front. Psychiatry 2021, 12, 648885. [Google Scholar] [CrossRef] [PubMed]
- Holmes, A.M.; Deb, P. The effect of chronic illness on the psychological health of family members. J. Ment. Health Policy Econ. 2003, 6, 13–22. [Google Scholar]
- Lee, E.S.; Bong, E.J. Impact of Parents’ Problem Drinking on Suicidal Ideation of Their University Student Children: The Multiple Mediating Effects of Childhood Trauma, Experiential Avoidance and Depression. J. Korean Acad. Nurs. 2018, 48, 565–577. [Google Scholar] [CrossRef]
- Wong, M.M.; Brower, K.J.; Zucker, R.A. Sleep problems, suicidal ideation, and self-harm behaviors in adolescence. J. Psychiatr. Res. 2011, 45, 505–511. [Google Scholar] [CrossRef]
- Pillay, A.L.; van der Veen, M.B.; Wassenaar, D.R. Non-fatal suicidal behaviour in women--the role of spousal substance abuse and marital violence. S. Afr. Med. J. 2001, 91, 429–432. [Google Scholar]
- Patkar, P.; Walia, T.S.; Singh, I.; Chaudhury, S.; Saldanha, D.; Diwan, C. Quality of life and suicidal ideation in wives of men with alcohol dependence: A hospital-based study. Ind. Psychiatry J. 2021, 30 (Suppl. S1), S184–S188. [Google Scholar]
- Miret, M.; Caballero, F.F.; Huerta-Ramírez, R.; Moneta, M.V.; Olaya, B.; Chatterji, S.; Haro, J.M.; Ayuso-Mateos, J.L. Factors associated with suicidal ideation and attempts in Spain for different age groups. Prevalence before and after the onset of the economic crisis. J. Affect. Disord. 2014, 163, 1–9. [Google Scholar] [CrossRef]
- Jo, A.; Jeon, M.; Oh, H. Age-differentiated Risk Factors of Suicidal Ideation among Young and Middle-aged Korean Adults. Osong Public Health Res. Perspect 2017, 8, 201–210. [Google Scholar] [CrossRef] [PubMed]
- Lew, B.; Kõlves, K.; Osman, A.; Abu Talib, M.; Ibrahim, N.; Siau, C.S.; Chan, C.M.H. Suicidality among Chinese college students: A cross-sectional study across seven provinces. PLoS ONE 2020, 15, e0237329. [Google Scholar] [CrossRef] [PubMed]
- Barrows, S.P. China’s One-Child Policy. JAMA 2016, 315, 2349–2350. [Google Scholar] [CrossRef]
- Rüger, H.; Löffler, I.; Ochsmann, E.; Alsmann, C.; Letzel, S.; Münster, E. Mental illness and over-indebtedness. Mental illness, social networks and financial strain in over-indebted persons. Psychother. Psychosom. Med. Psychol. 2010, 60, 250–254. [Google Scholar] [CrossRef] [PubMed]
- Meltzer, H.; Bebbington, P.; Brugha, T.; Jenkins, R.; McManus, S.; Dennis, M.S. Personal debt and suicidal ideation. Psychol. Med. 2011, 41, 771–778. [Google Scholar] [CrossRef]
- Dolsen, E.A.; Prather, A.A.; Lamers, F.; Penninx, B.W. Suicidal ideation and suicide attempts: Associations with sleep duration, insomnia, and inflammation. Psychol. Med. 2021, 51, 2094–2103. [Google Scholar] [CrossRef]
- Pigeon, W.R.; Pinquart, M.; Conner, K. Meta-analysis of sleep disturbance and suicidal thoughts and behaviors. J. Clin. Psychiatry 2012, 73, e1160–e1167. [Google Scholar] [CrossRef]
- Batterham, P.J.; Werner-Seidler, A.; Calear, A.L.; McCallum, S.; Gulliver, A. Specific aspects of sleep disturbance associated with suicidal thoughts and attempts. J. Affect. Disord. 2021, 282, 574–579. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).