Active School-Based Interventions to Interrupt Prolonged Sitting Improve Daily Physical Activity: A Systematic Review and Meta-Analysis
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design
2.2. Search Strategy
2.3. Criteria for Selection
2.4. Data Extraction
2.5. Risk of Bias and Methodological Quality of Clinical Trials
2.6. Data Synthesis and Analysis
3. Results
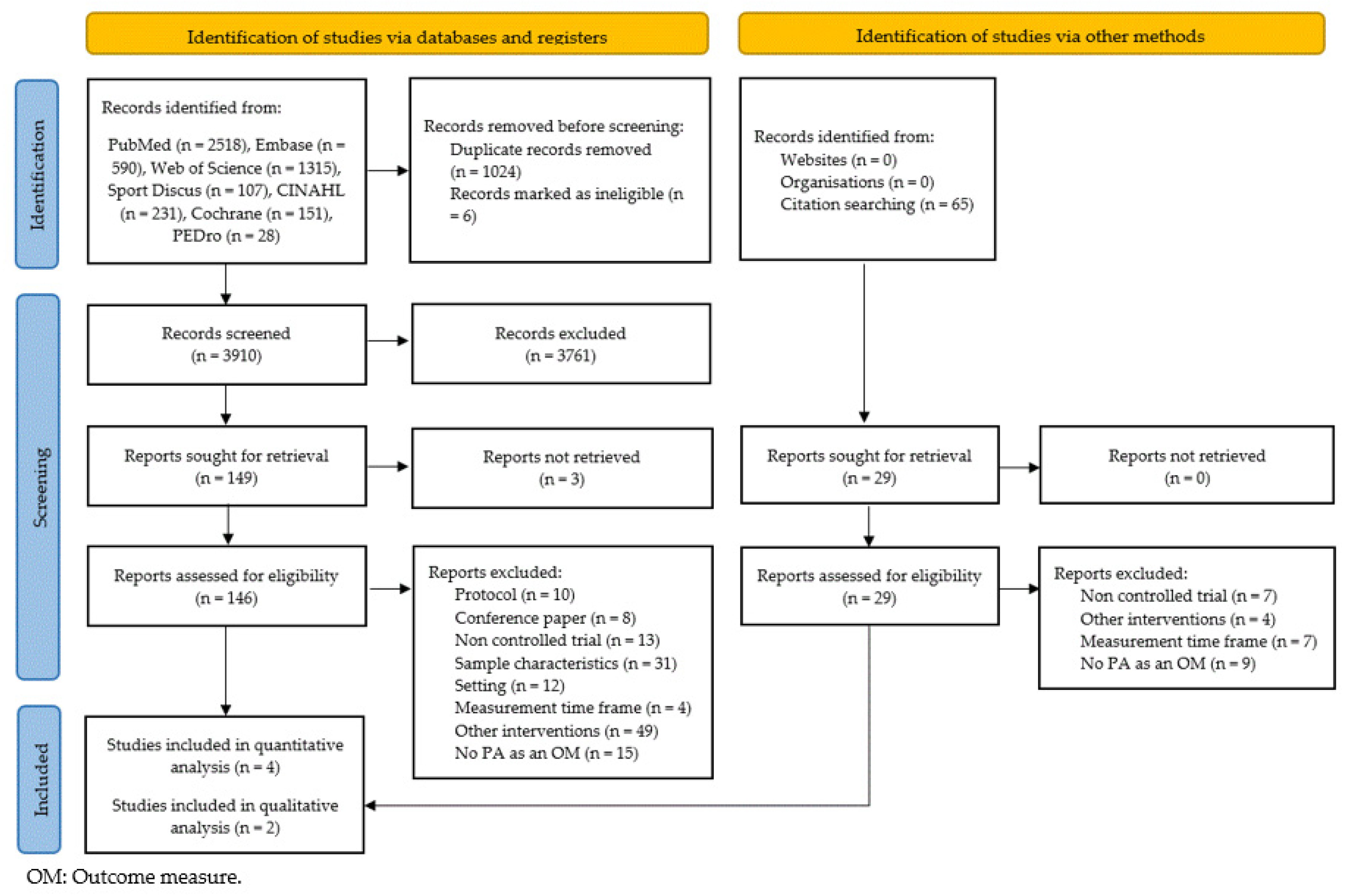
3.1. Literature Search and Screening
3.2. Characteristics of Eligible Studies
3.3. Risk of Bias and Methodological Quality of Clinical Trials
3.4. Synthesis of Results
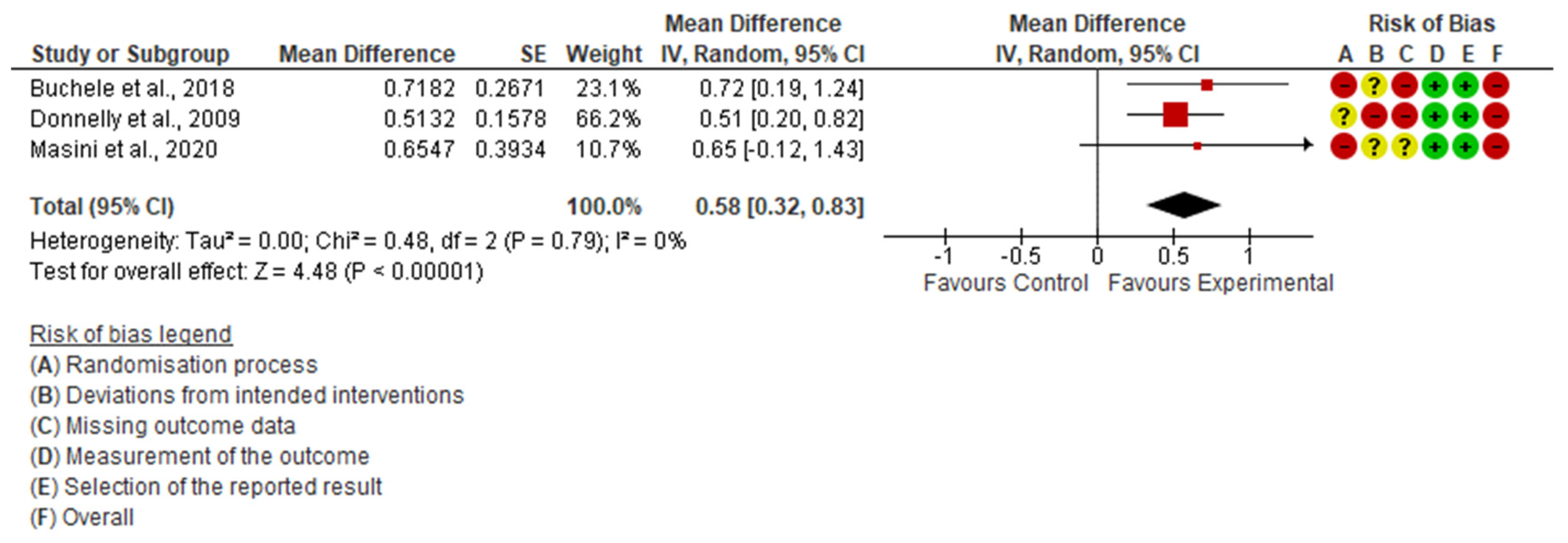
- Daily PA
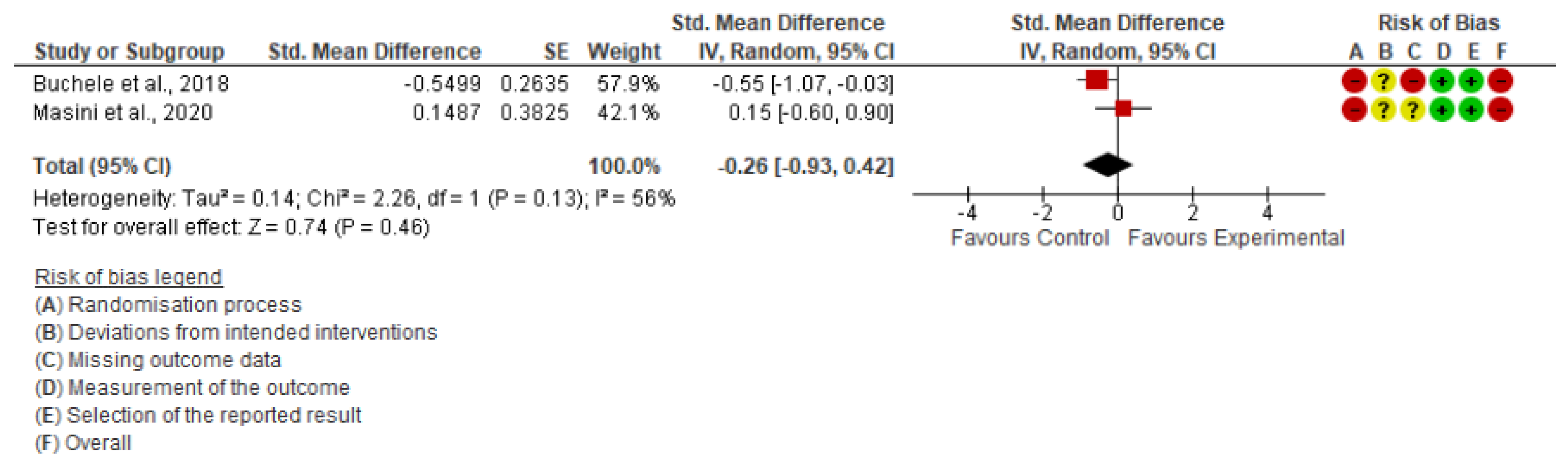
- Daily SB
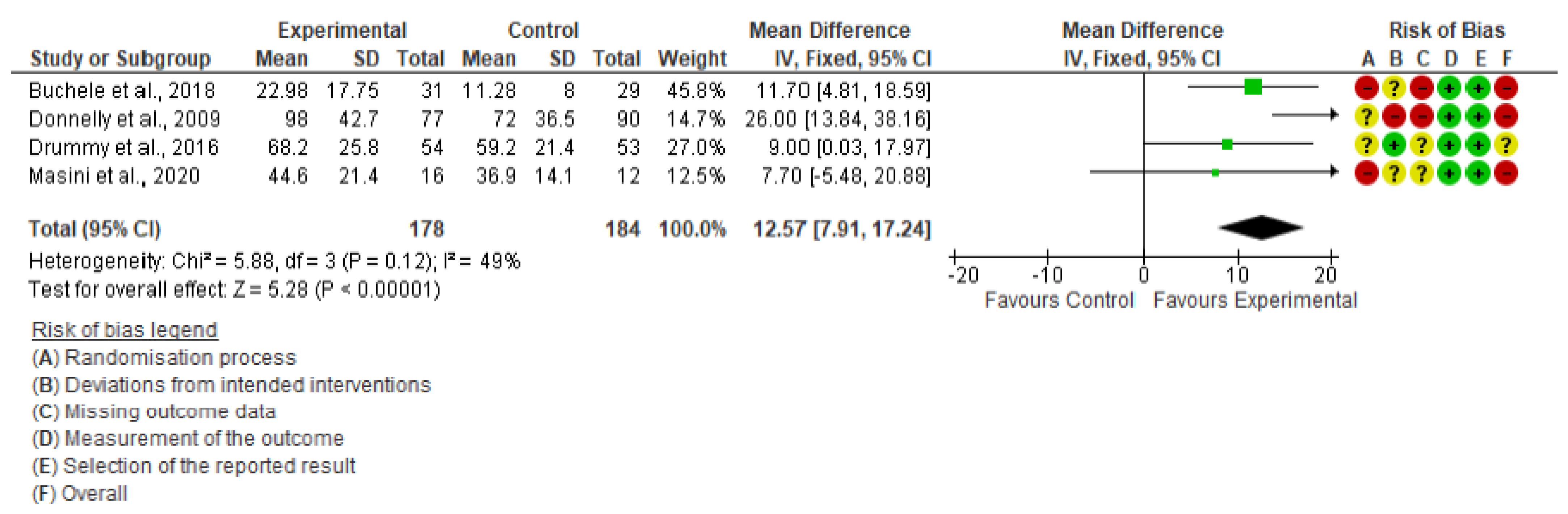
- Daily MVPA
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Tremblay, M.S.; Aubert, S.; Barnes, J.D.; Saunders, T.J.; Carson, V.; Latimer-Cheung, A.E.; Chastin, S.F.M.; Altenburg, T.M.; Chinapaw, M.J.M.; Aminian, S.; et al. Sedentary Behavior Research Network (SBRN)-Terminology Consensus Project process and outcome. Int. J. Behav. Nutr. Phys. Act. 2017, 14, 75. [Google Scholar] [CrossRef] [PubMed]
- Chaput, J.P.; Willumsen, J.; Bull, F.; Chou, R.; Ekelund, U.; Firth, J.; Jago, R.; Ortega, F.B.; Katzmarzyk, P.T. 2020 WHO guidelines on physical activity and sedentary behaviour for children and adolescents aged 5–17 years: Summary of the evidence. Int. J. Behav. Nutr. Phys. Act. 2020, 17, 141. [Google Scholar] [CrossRef] [PubMed]
- Auhuber, L.; Vogel, M.; Grafe, N.; Kiess, W.; Poulain, T. Leisure Activities of Healthy Children and Adolescents. Int. J. Environ. Res. Public Health 2019, 16, 2078. [Google Scholar] [CrossRef] [PubMed]
- Arundell, L.; Fletcher, E.; Salmon, J.; Veitch, J.; Hinkley, T. A systematic review of the prevalence of sedentary behavior during the after-school period among children aged 5–18 years. Int. J. Behav. Nutr. Phys. Act. 2016, 13, 93. [Google Scholar] [CrossRef] [PubMed]
- Tremblay, M.S.; Leblanc, A.G.; Carson, V.; Choquette, L.; Connor Gorber, S.; Dillman, C.; Duggan, M.; Gordon, M.J.; Hicks, A.; Janssen, I.; et al. Canadian Sedentary Behaviour Guidelines for the Early Years (aged 0–4 years). Metab Appl. Physiol. Nutr. Metab. 2012, 37, 370–391. [Google Scholar] [CrossRef] [PubMed]
- Tremblay, M.S.; Leblanc, A.G.; Janssen, I.; Kho, M.E.; Hicks, A.; Murumets, K.; Colley, R.C.; Duggan, M. Canadian sedentary behaviour guidelines for children and youth. Metab Appl. Physiol. Nutr. Metab. 2011, 36, 59–71. [Google Scholar] [CrossRef]
- dos Santos, G.; Guerra, P.H.; Milani, S.A.; Santos, A.B.D.; Cattuzzo, M.T.; Ré, A.H.N. Sedentary behavior and motor competence in children and adolescents: A review. Rev. Saude Publica 2021, 55, 1–14. [Google Scholar] [CrossRef]
- World Health Organization. Global Recommendations on Physical Activity for Health. Available online: https://news.ge/anakliis-porti-aris-qveynis-momava (accessed on 15 September 2022).
- Sampasa-Kanyinga, H.; Sampasa-Kanyinga, H.; Colman, I.; Colman, I.; Goldfield, G.S.; Goldfield, G.S.; Janssen, I.; Wang, J.; Wang, J.; Podinic, I.; et al. Combinations of physical activity, sedentary time, and sleep duration and their associations with depressive symptoms and other mental health problems in children and adolescents: A systematic review. Int. J. Behav. Nutr. Phys. Act. 2020, 17, 72. [Google Scholar] [CrossRef]
- Podnar, H.; Jurić, P.; Karuc, J.; Saez, M.; Barceló, M.A.; Radman, I.; Starc, G.; Jurak, G.; Đurić, S.; Potočnik, Ž.L.; et al. Comparative effectiveness of school-based interventions targeting physical activity, physical fitness or sedentary behaviour on obesity prevention in 6-to 12-year-old children: A systematic review and meta-analysis. Obes. Rev. 2021, 22, e13160. [Google Scholar] [CrossRef]
- Weaver, R.G.; Tassitano, R.M.; Tenório, M.C.M.; Brazendale, K.; Beets, M.W. Temporal Trends in Children’s School Day Moderate to Vigorous Physical Activity: A Systematic Review and Meta-Regression Analysis. J. Phys. Act. Health 2021, 18, 1446–1467. [Google Scholar] [CrossRef]
- World Health Organization. More Active People for a Healthier World; World Health Organization: Geneva, Switzerland, 2018. [Google Scholar]
- Hegarty, L.M.; Mair, J.L.; Kirby, K.; Murtagh, E.; Murphy, M.H. School-based Interventions to Reduce Sedentary Behaviour in Children: A Systematic Review. AIMS Public Health 2016, 3, 520–541. [Google Scholar] [CrossRef] [PubMed]
- Neil-Sztramko, S.E.; Caldwell, H.; Dobbins, M. School-based physical activity programs for promoting physical activity and fitness in children and adolescents aged 6 to 18. Cochrane Database Syst. Rev. 2021, 23, CD007651. [Google Scholar] [CrossRef]
- Page, M.J.; Moher, D.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. PRISMA 2020 explanation and elaboration: Updated guidance and exemplars for reporting systematic reviews. BMJ 2021, 372, n160. [Google Scholar] [CrossRef] [PubMed]
- University of Sydney PEDro. Physiotherapy Evidence Database. Available online: https://pedro.org.au/english/resources/pedro-scale (accessed on 15 September 2022).
- Higgins, J.P.; Thomas, J.; Chandler, J.; Cumpston, M.; Li, T.; Page, M.J.; Welch, V.A. Cochrane Handbook for Systematic Reviews of Interventions, 2nd ed.; John Wiley & Sons: Chichester, UK, 2019. [Google Scholar]
- De Morton, N.A. The PEDro scale is a valid measure of the methodological quality of clinical trials: A demographic study. Aust. J. Physiother. 2009, 55, 129–133. [Google Scholar] [CrossRef]
- Donnelly, J.E.; Greene, J.L.; Gibson, C.A.; Smith, B.K.; Washburn, R.A.; Sullivan, D.K.; DuBose, K.; Mayo, M.S.; Schmelzle, K.H.; Ryan, J.J.; et al. Physical Activity Across the Curriculum (PAAC): A randomized controlled trial to promote physical activity and diminish overweight and obesity in elementary school children. Prev. Med. 2009, 49, 336–341. [Google Scholar] [CrossRef] [PubMed]
- Drummy, C.; Murtagh, E.M.; McKee, D.P.; Breslin, G.; Davison, G.W.; Murphy, M.H. The effect of a classroom activity break on physical activity levels and adiposity in primary school children. J. Paediatr. Child Health 2016, 52, 745–749. [Google Scholar] [CrossRef] [PubMed]
- Buchele, H.; Chen, W. Technology-enhanced classroom activity breaks impacting children’s physical activity and fitness. J. Clin. Med. 2018, 7, 165. [Google Scholar] [CrossRef] [PubMed]
- Masini, A.; Marini, S.; Leoni, E.; Lorusso, G.; Toselli, S.; Tessari, A.; Ceciliani, A.; Dallolio, L. Active breaks: A pilot and feasibility study to evaluate the effectiveness of physical activity levels in a school based intervention in an Italian primary school. Int. J. Environ. Res. Public Health 2020, 17, 4351. [Google Scholar] [CrossRef] [PubMed]
- Pinto-Escalona, T.; Martínez-de-Quel, Ó. Diez minutos de actividad física interdisciplinaria mejoran el rendimiento académico. Apunts Educ. Fis. y Deportes 2019, 35, 82–94. [Google Scholar] [CrossRef]
- Reed, J.A.; Einstein, G.; Hahn, E.; Hooker, S.P.; Gross, V.P.; Kravitz, J. Examining the impact of integrating physical activity on fluid intelligence and academic performance in an elementary school setting: A preliminary investigation. J. Phys. Act. Health 2010, 7, 343–351. [Google Scholar] [CrossRef]
- Masini, A.; Marini, S.; Gori, D.; Leoni, E.; Rochira, A.; Dallolio, L. Evaluation of school-based interventions of active breaks in primary schools: A systematic review and meta-analysis. J. Sci. Med. Sport 2020, 23, 377–384. [Google Scholar] [CrossRef] [PubMed]
- Watson, A.; Timperio, A.; Brown, H.; Best, K.; Hesketh, K.D. Effect of classroom-based physical activity interventions on academic and physical activity outcomes: A systematic review and meta-analysis. Int. J. Behav. Nutr. Phys. Act. 2017, 14, 114. [Google Scholar] [CrossRef] [PubMed]
- Riley, N.; Lubans, D.R.; Holmes, K.; Morgan, P.J. Findings from the EASY Minds Cluster Randomized Controlled Trial: Evaluation of a Physical Activity Integration Program for Mathematics in Primary Schools. J. Phys. Act. Health 2016, 13, 198–206. [Google Scholar] [CrossRef] [PubMed]
- Ahamed, Y.; Macdonald, H.; Reed, K.; Naylor, P.-J.; Liu-Ambrose, T.; McKay, H. School-based physical activity does not compromise children’s academic performance. Med. Sci. Sports Exerc. 2007, 39, 371–376. [Google Scholar] [CrossRef]
- Carlson, J.A.; Engelberg, J.K.; Cain, K.L.; Conway, T.L.; Mignano, A.M.; Bonilla, E.A.; Geremia, C.; Sallis, J.F. Implementing classroom physical activity breaks: Associations with student physical activity and classroom behavior. Prev. Med. 2015, 81, 67–72. [Google Scholar] [CrossRef] [PubMed]
- Cain, K.L.; Sallis, J.F.; Conway, T.L.; Van Dyck, D.; Calhoon, L. Using accelerometers in youth physical activity studies: A review of methods. J. Phys. Act. Health 2013, 10, 437–450. [Google Scholar] [CrossRef]
- Chinapaw, M.J.M.; De Niet, M.; Verloigne, M.; De Bourdeaudhuij, I.; Brug, J.; Altenburg, T.M. From sedentary time to sedentary patterns: Accelerometer data reduction decisions in youth. PLoS ONE 2014, 9, e111205. [Google Scholar] [CrossRef]
- Borghese, M.M.; Borgundvaag, E.; McIsaac, M.A.; Janssen, I. Imputing accelerometer nonwear time in children influences estimates of sedentary time and its associations with cardiometabolic risk. Int. J. Behav. Nutr. Phys. Act. 2019, 16, 7. [Google Scholar] [CrossRef]
- Trost, S.G.; Loprinzi, P.D.; Moore, R.; Pfeiffer, K.A. Comparison of accelerometer cut points for predicting activity intensity in youth. Med. Sci. Sports Exerc. 2011, 43, 1360–1368. [Google Scholar] [CrossRef]
- Tassitano, R.M.; Weaver, R.G.; Tenório, M.C.M.; Brazendale, K.; Beets, M.W. Physical activity and sedentary time of youth in structured settings: A systematic review and meta-analysis. Int. J. Behav. Nutr. Phys. Act. 2020, 17, 160. [Google Scholar] [CrossRef]
- Wijndaele, K.; White, T.; Andersen, L.B.; Bugge, A.; Kolle, E.; Northstone, K.; Wedderkopp, N.; Ried-Larsen, M.; Kriemler, S.; Page, A.S.; et al. Substituting prolonged sedentary time and cardiovascular risk in children and youth: A meta-analysis within the International Children’s Accelerometry database (ICAD). Int. J. Behav. Nutr. Phys. Act. 2019, 16, 96. [Google Scholar] [CrossRef] [PubMed]
- Wu, X.Y.; Zhuang, L.H.; Li, W.; Guo, H.W.; Zhang, J.H.; Zhao, Y.K.; Hu, J.W.; Gao, Q.Q.; Luo, S.; Ohinmaa, A.; et al. The influence of diet quality and dietary behavior on health-related quality of life in the general population of children and adolescents: A systematic review and meta-analysis. Qual. Life Res. 2019, 28, 1989–2015. [Google Scholar] [CrossRef] [PubMed]
| Reference | Year | Country | Age | N | Sitting Time Interruption | Outcome Measures | |||||
|---|---|---|---|---|---|---|---|---|---|---|---|
| Age Range | Mean Age (SD) | PA | MVPA | SB | Tool | Other Outcome Measures | |||||
| Donelly, 2009 [19] | 2009 | USA | 6–9 | 2nd FEG 7.7 (0.3) 2nd FCG 7.8 (0.4) 2nd MEG 7.7 (0.4) 2nd MCG 7.8 (0.3) 3th FEG 8.7 (0.4) 3th FCG 8.7 (0.4) 3th MED 8.7 (0.3) 3th MCD 8.8 (0.4) | 454 | Weekly 90 min (10-min bout) for 3 years | x | x | Accelerometer (ActiGraph, 7163, Pensacola, FL) | BMI and academic achievement | |
| Drummy, 2016 [20] | 2016 | Ireland | 9–10 | 9.5 | 107 | 5 min 3 times/day for 12 weeks | x | Accelerometer (Actigraph GT1M, Actigraph LLC, Pensacole, FL, USA) | BMI and skinfold measurements | ||
| Buchele, 2018 [21] | 2018 | USA | 10–11 | x | 116 | Daily 6 min for 4 weeks (PAEB-C program) | x | x | x | Activity tracker (Fitbit Charger + Heart RateTM) | aerobic fitness |
| Masini, 2020 [22] | 2020 | Italy | 8–9 | 9.02 (0.11) | 28 | 10 min twice a day for 14 weeks | x | x | x | Accelerometer (ActiGraph wGT3X-BT, Actigraph LLC, Pensacole, FL, USA) | satisfaction |
| Pinto-Escalona, 2019 [23] | 2019 | Spain | 13–14 | 13.6 (0.7) | 116 | Daily 10 min for 5 days | x | Questionnaire for Assessing Physical Activity in Teenage Schoolchildren | academic achievement and attention | ||
| Reed, 2010 [24] | 2010 | USA | 8–9 | EG 9.42 CG 9.50 | 155 | 30 min 3 times/week for 4 months | x | Questionnaire Previous Day Physical Activity Recall (PDPAR) | fluid intelligence and academic achievement | ||
| 1. Eligibility Criteria Were Specified | 2. Random Allocation | 3. Concealed Allocation | 4. Groups Similar at Baseline | 5. Participants Blinding | 6. Teachers Blinding | 7. Outcome Assessors Blinding | 8. Less than 15% Dropouts | 9. Intention to Treat Analysis | 10. Between-Group Statistical Comparisons | 11. Point Measures and Variability Data | TOTAL | ||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| [19] | Donnelly, 2009 | 1 | 1 | 0 | 1 | 0 | 0 | 1 | 1 | 0 | 1 | 1 | 6 |
| [20] | Drummy, 2016 | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 1 | 1 | 5 |
| [21] | Buchele, 2018 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 0 | 1 | 1 | 3 |
| [22] | Masini, 2020 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 2 |
| [23] | Pinto-Escalona, 2019 | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 1 | 0 | 1 | 1 | 5 |
| [24] | Reed, 2010 | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 1 | 1 | 4 |
| TOTAL | 6 | 4 | 0 | 4 | 0 | 0 | 1 | 4 | 0 | 6 | 6 | 4.2 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Amor-Barbosa, M.; Ortega-Martínez, A.; Carrasco-Uribarren, A.; Bagur-Calafat, M.C. Active School-Based Interventions to Interrupt Prolonged Sitting Improve Daily Physical Activity: A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Public Health 2022, 19, 15409. https://doi.org/10.3390/ijerph192215409
Amor-Barbosa M, Ortega-Martínez A, Carrasco-Uribarren A, Bagur-Calafat MC. Active School-Based Interventions to Interrupt Prolonged Sitting Improve Daily Physical Activity: A Systematic Review and Meta-Analysis. International Journal of Environmental Research and Public Health. 2022; 19(22):15409. https://doi.org/10.3390/ijerph192215409
Chicago/Turabian StyleAmor-Barbosa, Marta, Anna Ortega-Martínez, Andoni Carrasco-Uribarren, and Maria Caridad Bagur-Calafat. 2022. "Active School-Based Interventions to Interrupt Prolonged Sitting Improve Daily Physical Activity: A Systematic Review and Meta-Analysis" International Journal of Environmental Research and Public Health 19, no. 22: 15409. https://doi.org/10.3390/ijerph192215409
APA StyleAmor-Barbosa, M., Ortega-Martínez, A., Carrasco-Uribarren, A., & Bagur-Calafat, M. C. (2022). Active School-Based Interventions to Interrupt Prolonged Sitting Improve Daily Physical Activity: A Systematic Review and Meta-Analysis. International Journal of Environmental Research and Public Health, 19(22), 15409. https://doi.org/10.3390/ijerph192215409