Abstract
Obesity, diabetes mellitus, and cardiovascular risk are real challenges in systemic lupus erythematosus (SLE) clinical practice and research. The evidence of the burden of these health problems in SLE patients is determined by the methods used to assess them. Therefore, the aim of this scoping review is to map current approaches in assessing obesity, diabetes mellitus, and cardiovascular risk burden in SLE patients and to identify existing knowledge gaps in this field. This rapid scoping review was conducted according to the Joanna Briggs Institute methodology and identified 274 articles, of which 73 were included. Most studies were conducted at European institutions and patients were recruited from specialist hospital clinics, the majority of whom were women. The burden of obesity and diabetes mellitus for SLE patients was assessed mainly in terms of prevalence, impact on disease activity, and cardiometabolic risk. The burden of cardiovascular risk was assessed using multiple approaches, mainly imaging and laboratory methods, and risk factor-based scores, although there is great heterogeneity and uncertainty between the methods used. This review highlights the importance of improving and standardizing the approach to obesity, diabetes, and cardiovascular risk in SLE patients through a holistic assessment that includes lifestyle, clinical, biological, and social aspects.
1. Introduction
Despite improvements in health outcomes in systemic lupus erythematosus (SLE) in recent years, these patients experience higher mortality than the general population [1]. One of the main causes of death in these patients is cardiovascular disease. The excess of cardiovascular disease in SLE patients is not fully explained by a higher prevalence of classical cardiovascular risk factors [2,3]. Numerous efforts have been made to understand the pathogenesis behind this phenomenon and to develop therapeutic strategies that allow adequate management of cardiovascular disease in this group [3,4]. However, at present, only the control of classic cardiovascular risk factors and disease activity with hydroxychloroquine and the lowest possible glucocorticoid dosage are the standard recommendations [5,6,7].
In this context, an adequate assessment of obesity, diabetes, and cardiovascular risk burden is particularly relevant for these patients and society. Systematic reviews have addressed this question by providing evidence of obesity and cardiovascular risk burden in SLE patients. The prevalence of obesity in SLE patients is very high, ranging from 28% to 50% depending on the measurement methods [8]. It appears that obesity is associated with more severe cognitive and renal involvement, alteration of the quality of life, and contributes to the enhanced cardiovascular risk in SLE patients [8]. Additionally, SLE patients exhibit a high cardiovascular risk, having up to 3 times more risk of developing cardiovascular disease than the general population [2,9,10,11]. Systematic reviews focused on the impact of diabetes mellitus in SLE patients were not found in scientific literature.
The evidence of the burden of these health problems in SLE patients is shaped by the methods used to assess them. In this regard, several approaches have emerged in recent years, ranging from molecular to imaging methods, including equations and indexes which do not always perform adequately or are useful in clinical practice [12,13,14]. The lack of consensus and the great heterogeneity in the way assessment methods are applied and interpreted has consolidated obesity, diabetes mellitus, and cardiovascular risk as a real challenge for SLE research and clinical practice [12,15].
Given these facts, it would be useful to know how current research is being conducted and what kind of evidence is available on this topic, as well as what are the gaps in current knowledge. To answer these questions, the best source is a scoping review that synthesizes and maps the evidence, while clarifying key concepts that can serve as a basis for future research development [16].
However, after searching MEDLINE, the Cochrane Database of Systematic Reviews, and JBI Evidence Synthesis, no current or ongoing scoping reviews on the topic were identified. Therefore, the aim of this scoping review is to map current approaches in assessing obesity, diabetes mellitus, and cardiovascular risk burden in SLE patients and to identify existing knowledge gaps in this field.
2. Materials and Methods
2.1. Protocol and Registration
To develop this rapid scoping review, the Joanna Briggs Institute (JBI)methodology [16] was followed and the Preferred Reporting Items for Systematic Reviews and Meta-Analysis extension for scoping reviews guidelines (PRISMA-ScR) were fulfilled [17]. A protocol was developed but not registered.
The following two research questions were posed: 1. What is known from the literature about current approaches to assess obesity, diabetes, and cardiovascular risk burden in SLE? and 2. What are the current knowledge gaps in this field?
2.2. Eligibility Criteria
Inclusion criteria were defined according to JBI recommendations for scoping reviews, based on “Population”, “Concept” and “Context”:
Population: Studies that include SLE human patients older than 18 years were considered for this review.
Concept: Studies that evaluate the obesity, diabetes mellitus, and cardiovascular risk burden were included. In the case of obesity and diabetes mellitus, only those studies that assessed at least one measure of burden other than the prevalence of obesity and/or diabetes in SLE patients were included. The burden was interpreted as the association of obesity and/or diabetes mellitus with SLE-specific and non-SLE-specific health outcomes. In the case of cardiovascular risk, we included those studies in which the authors stated the cardiovascular risk assessment method in SLE patients, regardless of the method used.
Context: For this review, studies were considered regardless of the country where they were conducted or the setting.
Types of studies: This review included peer-reviewed studies regardless of whether their design was quantitative, qualitative, or mixed, with the aim of capturing different approaches to disease burden assessment. Reviews, systematic reviews, conference abstracts, case reports, opinion articles, and gray literature were not considered.
2.3. Information Sources
Relevant papers were screened by searching the following bibliographic databases: MEDLINE and EMBASE. Since this was a rapid scoping review, it was not possible to extract relevant bibliography from the reference lists of the included articles.
2.4. Search Strategy
The search strategy was aimed at identifying original articles published between 2017 and April 2022. The search strategy was developed by an experienced librarian and refined through team discussion. The final search strategy for MEDLINE is available in Table 1, this strategy was adapted to EMBASE database.

Table 1.
Search strategy for MEDLINE (PubMed). The search was conducted on 3 May 2022.
To ensure an accurate evaluation of the literature and quality data extraction, only those studies published in the languages in which the authors are fluent (English and Spanish) were included.
2.5. Selection of Sources of Evidence
Once the search was completed, all identified citations were collated and loaded into EndNote 7.8/2016 (Clarivate Analytics, Philadelphia, PA, USA) and duplicates were removed. After a pilot test, titles and abstracts were examined by two independent reviewers to assess them against the review inclusion criteria. The full text of selected citations was evaluated in detail against the inclusion criteria by two independent reviewers. In cases where the full text was not available, the authors were contacted. Disagreements arising between reviewers at each stage of the selection process were resolved through discussion, or with a third reviewer. The results of the search and study inclusion process are reported in a flow chart of the PRISMA-ScR.
2.6. Data Charting Process
Data were extracted from the included articles by two independent reviewers using a data extraction tool developed by the authors. Extracted data included pertinent details about the participants, the concept, the context, the study methods, and the key findings relevant to the review question.
2.7. Synthesis of Results
The general characteristics of the included studies were synthesized using absolute frequencies and are presented in a table. The approaches used to assess the burden were analyzed independently in three groups: obesity, diabetes mellitus, and cardiovascular risk. The main methods identified were categorized and presented in a figure. The knowledge gaps found in the review were developed in narrative form in the text. Critical appraisal was not performed as it was not the objective of this research.
3. Results
3.1. Selection of Sources of Evidence
The search resulted in 274 references. After excluding duplicates and weighing titles, abstracts, and full text according to the inclusion criteria, we finally included 73 articles in this review. Figure 1 shows the screening process in a PRISMA flowchart.
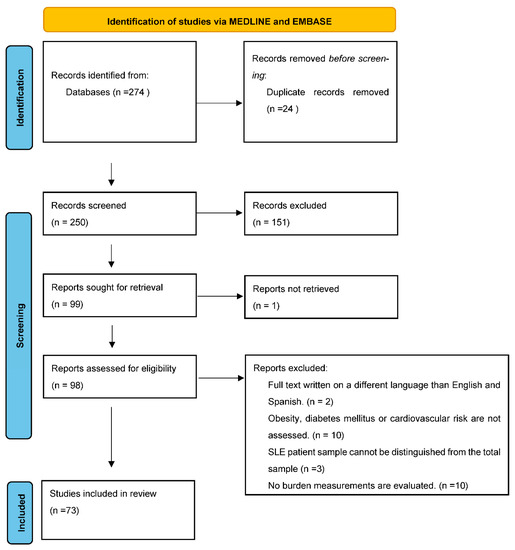
Figure 1.
PRISMA flow chart of the article selection process.
3.2. Characteristics of Sources of Evidence
The general characteristics of the included studies related to year of publication, geographic region, type of study reported by the authors, number of participants, percentage of women, and time frame are summarized in Table 2.

Table 2.
Study characteristics.
Most of the included studies were published in 2019 and represented SLE patients from Europe, although patients from 24 countries were included. The country that contributed to the most studies was Spain (n = 17), followed by the USA (n = 9).
Most of the studies were developed with samples of SLE patients recruited from specialized hospital clinics. More than half of the studies were able to recruit more than 100 patients with SLE. In 73% of the studies, the sample was composed of more than 90% of SLE female patients. In 50% of the studies, the authors reported a cross-sectional design and the time frame of the investigations in most cases was between 1 and 5 years.
3.3. Results of Individual Sources of Evidence
For each source of evidence included, the relevant results to the objective of this review are shown in the Supplementary Materials. All studies included in the obesity and diabetes mellitus group evaluated their prevalence (%) in SLE patients.
3.4. Synthesis of Results
The main methods identified to assess the burden of obesity, diabetes mellitus, and cardiovascular risk in SLE patients are categorized and presented in Figure 2.
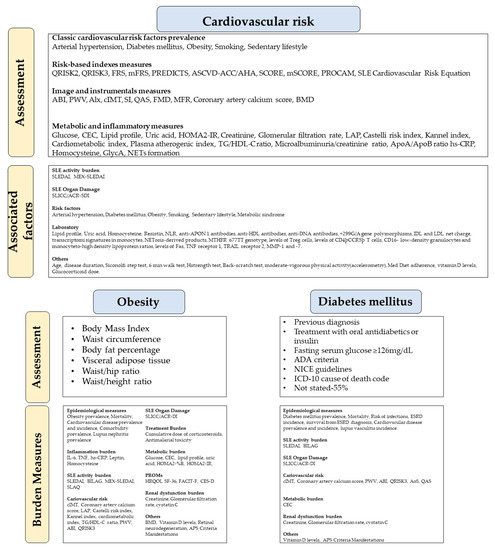
Figure 2.
Current approaches to assessing obesity, diabetes mellitus, and cardiovascular risk burden in SLE patients. (ABI: Ankle Brachial Index. ADA: American Diabetes Association. Alx: Augmentation index. AoS: Aortic stiffness. APS: Antiphospholipid syndrome. ASCVD-ACC/AHA: Pooled Cohort Risk Equations-American College of Cardiology/American Heart Association. BILAG: British Isles Lupus Assessment Group. BMD: Bone mineral density. CEC: Cholesterol Efflux Capacity. CES-D: Center for Epidemiological Studies-Depression. cIMT: Carotid intima-media thickness. CVD: Cardiovascular disease. ESRD: End-stage renal disease. FACIT-F: Functional Assessment of Chronic Illness Therapy—Fatigue. FMD: Flow-mediated dilation. FRS: Framingham Risk Score. GlycA: Glycoprotein acetylation. HOMA-IR: Homeostatic Model Assessment of Insulin Resistance. HRQOL-SF 36: Health-related quality of life -The Short Form-36 Health Survey. hs-CRP: High-sensitive C-reactive protein. ICD-10: International Classification of Diseases 10th Revision. IDL: Intermediate density lipoproteins. IL-6: Interleukin-6. LAP: Lipid accumulation product. LDL: low-density lipoprotein. Med Diet: Mediterranean diet. MEX-SLEDAI: Mexican Systemic Lupus Erythematosus Disease Activity Index. MFR: Myocardial flow reserve. mFRS: Modified Framingham Risk Score. MMP-1: Collagenase-1. MMP-7: Matrilysin. mSCORE: Modified Systematic Coronary Risk Evaluation. NETs: Neutrophil extracellular traps. NICE: National Institute for Health and Care Excellence. NLR: Neutrophil-to-lymphocyte ratio. PGA: Physician Global Assessment score. PON1: Serum paraoxonase and arylesterase 1. PREDICTS: Predictors of Risk for Elevated Flares, Damage Progression and Increased Cardiovascular Disease in Patients with SLE. PROCAM: Prospective Cardiovascular Münster Study risk calculator. PWV: Pulse wave velocity. QAS: quality arterial stiffness. QRISK3: QRESEARCH risk estimator, version 3. SCORE: Systematic Coronary Risk Evaluation. SLAQ: Systemic Lupus Activity Questionnaire. SLEDAI: Systemic Lupus Erythematosus Disease Activity Index. SLICC/ACR-DI: Systemic Lupus International Collaborating Clinics/American College of Rheumatology-Damage index. TG/HDL-C: Serum levels of triglyceride/high-density lipoprotein cholesterol ratio. TNF: tumor necrosis factor. TRAIL: TNF-related apoptosis-inducing ligand).
An important knowledge gap lies in the fact that it is not possible to ensure a causal relationship between the measures studied and the results, due to the methodological limitations of the study designs. Moreover, the influence of individual and contextual socioeconomic factors that may be shaping the impact of obesity, diabetes, and cardiovascular risk in SLE patients is largely unknown. Due to the marked predominance of female patients and the large number of European studies conducted, the burden of previously mentioned factors and the methods to assess them in male SLE patients as well as those living in other continents (South America, Africa, and Asia) has been poorly studied. On the other hand, the impact of obesity, diabetes mellitus, and cardiovascular risk on treatment outcomes, disability, health care utilization, and costs have been scarcely studied.
In summary, the magnitude and nature of the relationship between obesity, diabetes, and cardiovascular risk in SLE remain poorly understood. Although new methods have been developed and others refined, a specific strategy for cardiovascular risk stratification in these patients remains to be defined. Even if this milestone is achieved, the challenge remains to extrapolate the results to SLE patient populations that continue to be underrepresented in research in this area. Finally, there are few studies based on implementation science to evaluate these methods in daily clinical practice and to test the feasibility and effectiveness of different approaches.
4. Discussion
In this rapid exploratory review, we included 73 studies published between 2017 and April 2022 that evaluated the obesity, diabetes mellitus, and cardiovascular risk burden in patients with SLE.
Our results indicate that there is little recent evidence regarding the impact of diabetes mellitus on SLE patients. This could be influenced by the fact that many studies of cardiovascular risk exclude patients who already have diabetes mellitus. We also found multiple studies that evaluated the burden of obesity and cardiovascular risk in this group, although many studies evaluated both at the same time.
In the case of obesity, several methods were used to assess it, of which BMI was the most widespread and accessible. However, probably the measurement of body fat index by DXA is the most robust method that overcomes the limitations of BMI [19]. Despite this, there is little evidence comparing the performance of both methods in patients with SLE [20].
The greatest heterogeneity in the approaches used to evaluate the burden was found in the assessment of cardiovascular risk, where the authors used classical cardiovascular risk factors to modern imaging and molecular techniques, although many need validation in longitudinal studies [6,21,22,23,24,25]. We consider that this heterogeneity is due to the varied conditions in the different scenarios in which SLE clinical practice and research are developed. In the absence of a robust recommendation applicable to all patients, the assessment of individual cardiovascular risk relies on the judgment of physicians and their experience in the application of risk scores and laboratory and imaging methods [26].
The incorporation of SLE and the use of corticosteroids in risk scores seems to be a step in the right direction to establish a more accurate cardiovascular risk stratification tool for patients with SLE, although further optimization, standardization, and simplification are needed for use in daily practice [6,13,14,26,27].
In general, when evaluating the impact of the health problems studied in SLE patients, there was a lack of consideration and adjustment for socioeconomic factors [28]. Socioeconomic data are often easy to obtain, but researchers should be aware of their importance as they may modify the impact of obesity, diabetes mellitus, and cardiovascular risk in underserved SLE patient populations. An interesting alternative would be to develop a cardiovascular risk model for SLE patients that takes into account the increased risk associated with social deprivation, as does the QRISK scale.
Our results revealed that there are certain measures of burden that have been poorly evaluated in recent literature, such as the burden of treatment, disability, health care utilization, work participation, and, clearly, economic burden [13,28]. Most studies to date that have attempted to assess the impact of obesity and diabetes on the health outcomes of SLE patients have a cross-sectional design, so causality cannot be inferred [15,19,29,30,31]. This has determined that the role of obesity and diabetes in SLE remains poorly understood [19].
More than 50% of the included studies had a sample composed of more than 90% women. This finding was not surprising because of the differences in the prevalence of SLE according to sex. However, atherosclerosis affects men and women differently regarding incidence, prevalence, risk factors, pathogenesis, clinical manifestations, treatment, morbidity, and mortality. For optimal prevention and treatment of atherosclerosis, it is not self-evident that women and men show similar responses to risk factors or treatment; therefore, studies must present results according to sex. Whether the threat and risk factors of premature atherosclerosis in women with SLE are generalized to male patients is unknown [3,26,31].
In addition to the underrepresentation of male patients, the included studies had little ethnic diversity in their sample [3,13,32]. This fact, combined with only a minority of the studies being conducted in South America, Africa, and Asia, creates uncertainty about how obesity, diabetes mellitus, and cardiovascular risk are being assessed in these SLE patient populations and limits the extrapolation of results obtained from research conducted in other settings.
Considering the personalized care of patients, the potential impact of the clinical phenotype, cardiometabolic profile, and social context of each SLE patient on cardiovascular prognosis deserves further investigation [6].
Our rapid exploratory review has some limitations. We only performed a systematic search in two bibliographic databases, so we recognize that it is possible that studies of relevance to our research question may have been left out. Although the initial protocol included a search of the references of the selected articles in search of new studies that met our inclusion criteria, this process could not be carried out due to time constraints. An evidence quality appraisal was not performed as this was not in line with the objectives of this rapid exploratory review. However, to the best of our knowledge, this is the first scoping review that provides a panoramic and updated view on this topic and points out important gaps in knowledge in the area that serves as a basis for the development of future research.
5. Conclusions
Despite the evident interest of clinicians and researchers in obesity, diabetes mellitus, and cardiovascular risk in SLE, there is great heterogeneity and uncertainty in the methods used to assess their burden. Future research with robust methodological designs is needed to compare the different novel methods with those currently available in terms of their validity and usefulness in clinical practice.
Our rapid scoping review has captured the disparity in scientific production in this regard, where male SLE patients, as well as Asians, Africans, and South Americans are underrepresented. This fact limits the extrapolation of the existing scientific evidence to these groups and indicates lines of future research in this area.
Furthermore, our review highlights the importance of improving and standardizing the approach to obesity, diabetes, and cardiovascular risk in patients with SLE through a holistic assessment that includes lifestyle, clinical, biological, and social aspects. We believe that only in this way will we be able to understand, assess, and intervene in the complex mechanisms underlying the relationship between SLE, obesity, diabetes, and cardiovascular risk.
Supplementary Materials
The following supporting information can be downloaded at: https://www.mdpi.com/article/10.3390/ijerph192214768/s1, Table S1: Characteristics of individual evidence sources related to obesity. Table S2: Characteristics of individual evidence sources related to diabetes mellitus. Table S3: Characteristics of individual evidence sources related to cardiovascular risk. References [33,34,35,36,37,38,39,40,41,42,43,44,45,46,47,48,49,50,51,52,53,54,55,56,57,58,59,60,61,62,63,64,65,66,67,68,69,70,71,72,73,74,75,76,77,78,79,80,81,82,83,84,85] are cited in the Supplementary Materials.
Author Contributions
Conceptualization, H.H.-N., M.R.B.-L. and R.G.-H.; methodology, H.H.-N., M.R.B.-L., M.R. and J.J.M.-S.; software, M.R. and J.J.M.-S.; validation, L.C.-P., J.S.-C. and A.L.-S.; formal analysis, H.H.-N., M.R. and J.J.M.-S.; investigation, H.H.-N., M.R., J.J.M.-S., L.C.-P., J.S.-C. and A.L.-S.; data curation, L.C.-P., J.S.-C. and A.L.-S.; writing—original draft preparation, H.H.-N., M.R. and J.J.M.-S.; writing—review and editing, M.R.B.-L., C.R.-G., M.d.M.A.-G., I.P.d.P. and R.G.-H.; visualization, H.H.-N., M.R. and J.J.M.-S.; supervision, M.R.B.-L., C.R.-G., M.d.M.A.-G., I.P.d.P. and R.G.-H.; project administration, M.R.B.-L.; funding acquisition, M.R.B.-L. All authors have read and agreed to the published version of the manuscript.
Funding
This work was supported by grants from the Instituto de Salud Carlos III, co-funded by the Fondo Europeo de Desarrollo Regional-FEDER, grant PI18/00766 and “Centros de Investigación En Red” (CIBER, CB06/03/0018). Jaime Sanz Cánovas, Lidia Cobos Palacios, and Almudena López- Sampalo were supported by “Rio Hortega” program (CM20/00212, CM20/00125, and CM21/00110, respectively) and M Rosa Bernal-Lopez was supported by “Miguel Servet Type II” program (CPII/00014) from the ISCIII-Madrid (Spain), co-funded by the Fondo Europeo de Desarrollo Regional-FEDER. M Rosa Bernal Lopez (“Nicolas Monardes” program, C1-0005-2020) was supported by Consejeria de Salud, Junta de Andalucía, and Halbert Hernandez Negrin (PREDOC-00826) was supported by Consejería de Transformación Económica, Industria, Conocimiento y Universidades, Junta de Andalucía-Sevilla (Spain).
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
The data presented are available upon request from the corresponding author.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Lee, Y.H.; Choi, S.J.; Ji, J.D.; Song, G.G. Overall and cause-specific mortality in systemic lupus erythematosus: An updated meta-analysis. Lupus 2016, 25, 727–734. [Google Scholar] [CrossRef] [PubMed]
- Conrad, N.; Verbeke, G.; Molenberghs, G.; Goetschalckx, L.; Callender, T.; Cambridge, G.; Mason, J.C.; Rahimi, K.; McMurray, J.J.V.; Verbakel, J.Y. Autoimmune diseases and cardiovascular risk: A population-based study on 19 autoimmune diseases and 12 cardiovascular diseases in 22 million individuals in the UK. Lancet 2022, 400, 733–743. [Google Scholar] [CrossRef]
- Romero-Díaz, J.; Acosta-Hernández, R.I.; Criales-Vera, S.; Kimura-Hayama, E.; Domínguez-Quintana, M.; Morán-Contla, R.; Núñez-Alvarez, C.; Lara-Reyes, P.; Aguilar-Salinas, C.; Sánchez-Guerrero, J. Asymptomatic Coronary Artery Calcifications in Men with Systemic Lupus Erythematosus. J. Rheumatol. 2018, 45, 663–670. [Google Scholar] [CrossRef] [PubMed]
- Andrades, C.; Fuego, C.; Manrique-Arija, S.; Fernandez-Nebro, A. Management of cardiovascular risk in systemic lupus erythematosus: A systematic review. Lupus 2017, 26, 1407–1419. [Google Scholar] [CrossRef] [PubMed]
- Fanouriakis, A.; Kostopoulou, M.; Alunno, A.; Aringer, M.; Bajema, I.; Boletis, J.; Cervera, R.; Doria, A.; Gordon, C.; Govoni, M.; et al. 2019 update of the EULAR recommendations for the management of systemic lupus erythematosus. Ann. Rheum. Dis. 2019, 78, 736–745. [Google Scholar] [CrossRef] [PubMed]
- Drosos, G.C.; Vedder, D.; Houben, E.; Boekel, L.; Atzeni, F.; Badreh, S.; Boumpas, D.T.; Brodin, N.; Bruce, I.N.; González-Gay, M.; et al. EULAR recommendations for cardiovascular risk management in rheumatic and musculoskeletal diseases, including systemic lupus erythematosus and antiphospholipid syndrome. Ann. Rheum. Dis 2022, 81, 768–779. [Google Scholar] [CrossRef]
- Gwinnutt, J.M.; Wieczorek, M.; Balanescu, A.; Bischoff-Ferrari, H.A.; Boonen, A.; Cavalli, G.; de Souza, S.; de Thurah, A.; Dorner, T.E.; Moe, R.H.; et al. 2021 EULAR recommendations regarding lifestyle behaviours and work participation to prevent progression of rheumatic and musculoskeletal diseases. Ann. Rheum. Dis. 2022. [Google Scholar] [CrossRef]
- Versini, M.; Jeandel, P.Y.; Rosenthal, E.; Shoenfeld, Y. Obesity in autoimmune diseases: Not a passive bystander. Autoimmun. Rev. 2014, 13, 981–1000. [Google Scholar] [CrossRef]
- Henrot, P.; Foret, J.; Barnetche, T.; Lazaro, E.; Duffau, P.; Seneschal, J.; Schaeverbeke, T.; Truchetet, M.-E.; Richez, C. Assessment of subclinical atherosclerosis in systemic lupus erythematosus: A systematic review and meta-analysis. Jt. Bone Spine 2018, 85, 155–163. [Google Scholar] [CrossRef]
- Lu, X.; Wang, Y.; Zhang, J.; Pu, D.; Hu, N.; Luo, J.; An, Q.; He, L. Patients with systemic lupus erythematosus face a high risk of cardiovascular disease: A systematic review and Meta-analysis. Int. Immunopharmacol. 2021, 94, 107466. [Google Scholar] [CrossRef]
- Restivo, V.; Candiloro, S.; Daidone, M.; Norrito, R.; Cataldi, M.; Minutolo, G.; Caracci, F.; Fasano, S.; Ciccia, F.; Casuccio, A.; et al. Systematic review and meta-analysis of cardiovascular risk in rheumatological disease: Symptomatic and non-symptomatic events in rheumatoid arthritis and systemic lupus erythematosus. Autoimmun. Rev. 2022, 21, 102925. [Google Scholar] [CrossRef] [PubMed]
- Vazquez-Del Mercado, M.; Perez-Vazquez, F.J.; Gomez-Banuelos, E.; Chavarria-Avila, E.; Llamas-Garcia, A.; Arrona-Rios, K.I.; Diaz-Rubio, G.I.; Durán-Barragán, S.; Navarro-Hernández, R.E.; Jordán-Estrada, B.P.; et al. Subclinical parameters of arterial stiffness and arteriosclerosis correlate with QRISK3 in systemic lupus erythematosus. PLoS ONE 2018, 13, e0207520. [Google Scholar] [CrossRef] [PubMed]
- Drosos, G.C.; Konstantonis, G.; Sfikakis, P.P.; Tektonidou, M.G. Underperformance of clinical risk scores in identifying vascular ultrasound-based high cardiovascular risk in systemic lupus erythematosus. Eur. J. Prev. Cardiol. 2020, 28, 346–352. [Google Scholar] [CrossRef] [PubMed]
- Sivakumaran, J.; Harvey, P.; Omar, A.; Tayer-Shifman, O.; Urowitz, M.B.; Gladman, D.D.; Anderson, N.; Su, J.; Touma, Z. Assessment of cardiovascular risk tools as predictors of cardiovascular disease events in systemic lupus erythematosus. Lupus Sci. Med. 2021, 8, e000448. [Google Scholar] [CrossRef]
- Teh, P.; Zakhary, B.; Sandhu, V.K. The impact of obesity on SLE disease activity: Findings from the Southern California Lupus Registry (SCOLR). Clin. Rheumatol. 2019, 38, 597–600. [Google Scholar] [CrossRef] [PubMed]
- Peters, M.D.J.; Godfrey, C.; McInerney, P.; Munn, Z.; Tricco, A.C.; Khalil, H. Chapter 11: Scoping Reviews (2020 version). In JBI Manual for Evidence Synthesis; Aromataris, E., Munn, Z., Eds.; JJBI: Adelaide, Australia, 2020; Available online: https://synthesismanual.jbi.global (accessed on 20 January 2022).
- Tricco, A.C.; Lillie, E.; Zarin, W.; O’Brien, K.K.; Colquhoun, H.; Levac, D.; Moher, D.; Peters, M.D.J.; Horsley, T.; Weeks, L.; et al. PRISMA Extension for Scoping Reviews (PRISMA-ScR): Checklist and Explanation. Ann. Intern. Med. 2018, 169, 467–473. [Google Scholar] [CrossRef]
- Chew, C.; Reynolds, J.A.; Lertratanakul, A.; Wu, P.; Urowitz, M.; Gladman, D.D.; Fortin, P.R.; Bae, S.-C.; Gordon, C.; Clarke, A.E.; et al. Lower vitamin D is associated with metabolic syndrome and insulin resistance in systemic lupus: Data from an international inception cohort. Rheumatology 2021, 60, 4737–4747. [Google Scholar] [CrossRef]
- Patterson, S.L.; Schmajuk, G.; Jafri, K.; Yazdany, J.; Katz, P. Obesity is Independently Associated with Worse Patient-Reported Outcomes in Women with Systemic Lupus Erythematosus. Arthritis Care Res. 2019, 71, 126–133. [Google Scholar] [CrossRef]
- Li, Z.; Shang, J.; Zeng, S.; Wu, H.; Zhou, Y.; Xu, H. Altered body composition and increased visceral adipose tissue in premenopausal and late postmenopausal patients with SLE. Clin. Rheumatol. 2019, 38, 3117–3127. [Google Scholar] [CrossRef]
- Baragetti, A.; Ramirez, G.; Magnoni, M.; Garlaschelli, K.; Grigore, L.; Berteotti, M.; Scotti, I.; Bozzolo, E.; Berti, A.; Camici, P.; et al. Disease trends over time and CD4 + CCR5 + T-cells expansion predict carotid atherosclerosis development in patients with systemic lupus erythematosus. Nutr. Metab. Cardiovasc. Dis. 2018, 28, 53–63. [Google Scholar] [CrossRef]
- Wigren, M.; Svenungsson, E.; Mattisson, I.Y.; Gustafsson, J.T.; Gunnarsson, I.; Zickert, A.; Elvin, K.; Jensen-Urstad, K.; Bengtsson, A.; Gullstrand, B.; et al. Cardiovascular disease in systemic lupus erythematosus is associated with increased levels of biomarkers reflecting receptor-activated apoptosis. Atherosclerosis 2018, 270, 1–7. [Google Scholar] [CrossRef]
- López, P.; Rodríguez-Carrio, J.; Martínez-Zapico, A.; Pérez-Álvarez, Á.I.; Suárez-Díaz, S.; Mozo, L.; Benavente, L.; Caminal-Montero, L.; Suárez, A. Low-density granulocytes and monocytes as biomarkers of cardiovascular risk in systemic lupus erythematosus. Rheumatology 2020, 59, 1752–1764. [Google Scholar] [CrossRef] [PubMed]
- Casey, K.A.; Smith, M.A.; Sinibaldi, D.; Seto, N.L.; Playford, M.P.; Wang, X.; Carlucci, P.M.; Wang, L.; Illei, G.; Yu, B.; et al. Modulation of Cardiometabolic Disease Markers by Type I Interferon Inhibition in Systemic Lupus Erythematosus. Arthritis Rheumatol. 2021, 73, 459–471. [Google Scholar] [CrossRef] [PubMed]
- Bortoluzzi, A.; Chighizola, C.B.; Fredi, M.; Raschi, E.; Bodio, C.; Privitera, D.; Gonelli, A.; Silvagni, E.; Govoni, M.; Cavazzana, I.; et al. The IMMENSE Study: The Interplay between iMMune and ENdothelial Cells in Mediating Cardiovascular Risk in Systemic Lupus Erythematosus. Front. Immunol. 2020, 11, 572876. [Google Scholar] [CrossRef] [PubMed]
- Zhu, L.; Singh, M.; Lele, S.; Sahakian, L.; Grossman, J.; Hahn, B.; McMahon, M. Assessing the validity of QRISK3 in predicting cardiovascular events in systemic lupus erythematosus. Lupus Sci. Med. 2022, 9, e000564. [Google Scholar] [CrossRef] [PubMed]
- Jafri, K.; Ogdie, A.; Qasim, A.; Patterson, S.L.; Gianfrancesco, M.; Izadi, Z.; Katz, P.; Yazdany, J.; Schmajuk, G. Discordance of the Framingham cardiovascular risk score and the 2013 American College of Cardiology/American Heart Association risk score in systemic lupus erythematosus and rheumatoid arthritis. Clin. Rheumatol. 2018, 37, 467–474. [Google Scholar] [CrossRef]
- Borg, A.; Gomez, A.; Cederlund, A.; Cobar, F.; Qiu, V.; Lindblom, J.; Emamikia, S.; Enman, Y.; Pettersson, S.; Parodis, I. Contribution of abnormal BMI to adverse health-related quality of life outcomes after a 52-week therapy in patients with SLE. Rheumatology 2021, 60, 4205–4217. [Google Scholar] [CrossRef]
- Sola-Rodríguez, S.; Gavilán-Carrera, B.; Vargas-Hitos, J.A.; Sabio, J.M.; Morillas-De-Laguno, P.; Soriano-Maldonado, A. Physical Fitness and Body Composition in Women with Systemic Lupus Erythematosus. Medicina 2019, 55, 57. [Google Scholar] [CrossRef]
- Sola-Rodríguez, S.; Vargas-Hitos, J.A.; Gavilán-Carrera, B.; Rosales-Castillo, A.; Ríos-Fernández, R.; Sabio, J.M.; Soriano-Maldonado, A. Physical Fitness Attenuates the Impact of Higher Body Mass and Adiposity on Inflammation in Women with Systemic Lupus Erythematosus. Front. Immunol. 2021, 12, 729672. [Google Scholar] [CrossRef]
- Sola-Rodríguez, S.; Vargas-Hitos, J.; Gavilán-Carrera, B.; Rosales-Castillo, A.; Sabio, J.; Hernández-Martínez, A.; Martínez-Rosales, E.; Ortego-Centeno, N.; Soriano-Maldonado, A. Relative Handgrip Strength as Marker of Cardiometabolic Risk in Women with Systemic Lupus Erythematosus. Int. J. Environ. Res. Public Health 2021, 18, 4630. [Google Scholar] [CrossRef]
- Legge, A.; Blanchard, C.; Hanly, J.G. Physical activity, sedentary behaviour and their associations with cardiovascular risk in systemic lupus erythematosus. Rheumatology 2020, 59, 1128–1136. [Google Scholar] [CrossRef] [PubMed]
- Tziomalos, K.; Gkougkourelas, I.; Sarantopoulos, A.; Bekiari, E.; Makri, E.; Raptis, N.; Tselios, K.; Pantoura, M.; Hatzitolios, A.I.; Boura, P. Arterial stiffness and peripheral arterial disease in patients with systemic lupus erythematosus. Rheumatol. Int. 2017, 37, 293–298. [Google Scholar] [CrossRef] [PubMed]
- Di Battista, M.; Tani, C.; Elefante, E.; Chimera, D.; Carli, L.; Ferro, F.; Stagnaro, C.; Mosca, M. Framingham, ACC/AHA or QRISK3: Which is the best in systemic lupus erythematosus cardiovascular risk estimation? Clin. Exp. Rheumatol. 2020, 38, 602–608. [Google Scholar]
- Garcia-Garcia, P.; Castejon, R.; Tutor-Ureta, P.; Silvestre, R.A.; Mellor-Pita, S.; Jimenez-Ortiz, C.; Yebra-Bango, M. Serum cystatin C is associated with kidney function but not with cardiovascular risk factors or subclinical atherosclerosis in patients with Systemic Lupus Erythematosus. Clin. Rheumatol. 2017, 36, 2709–2717. [Google Scholar] [CrossRef] [PubMed]
- Ammar, W.; Taha, M.; Baligh, E.; Osama, D. Assessment of vascular stiffness using different modalities in patients with systemic lupus erythematosus: A case control study. Egypt. Heart J. 2020, 72, 24. [Google Scholar] [CrossRef]
- Shaaban, A.; Helmy, M.; Barakat, M.; Elneily, D.; Ahmed, O. Serum resistin, insulin resistance and carotid intima-media thickness as an indication of subclinical atherosclerosis in systemic lupus erythematosus patients. Egypt. Rheumatol. 2021, 43, 319–323. [Google Scholar] [CrossRef]
- Sánchez-Pérez, H.; Tejera-Segura, B.; De Vera-González, A.; Delgado, A.G.; Olmos, J.M.; Hernandez, J.L.; Corrales, A.; López-Mejías, R.; González-Gay, M.A.; Ferraz-Amaro, I. Insulin resistance in systemic lupus erythematosus patients: Contributing factors and relationship with subclinical atherosclerosis. Clin. Exp. Rheumatol. 2017, 35, 885–892. [Google Scholar]
- Pesqueda-Cendejas, K.; Parra-Rojas, I.; Mora-García, P.E.; Montoya-Buelna, M.; Ruiz-Ballesteros, A.I.; Meza-Meza, M.R.; Campos-López, B.; Rivera-Escoto, M.; Vizmanos-Lamotte, B.; Cerpa-Cruz, S.; et al. CRP Serum Levels Are Associated with High Cardiometabolic Risk and Clinical Disease Activity in Systemic Lupus Erythematosus Patients. J. Clin. Med. 2022, 11, 1849. [Google Scholar] [CrossRef]
- Čypienė, A.; Dadonienė, J.; Miltinienė, D.; Rinkūnienė, E.; Rugienė, R.; Stropuvienė, S.; Badarienė, J.; Laucevičius, A. The fact not to ignore: Mean blood pressure is the main predictor of increased arterial stiffness in patients with systemic rheumatic diseases. Adv. Med Sci. 2017, 62, 223–229. [Google Scholar] [CrossRef]
- López, P.; Rodríguez-Carrio, J.; Martínez-Zapico, A.; Pérez-Álvarez, Á.I.; López-Mejías, R.; Benavente, L.; Mozo, L.; Caminal-Montero, L.; González-Gay, M.A.; Suárez, A. Serum Levels of Anti-PON1 and Anti-HDL Antibodies as Potential Biomarkers of Premature Atherosclerosis in Systemic Lupus Erythematosus. Thromb. Haemost. 2017, 117, 2194–2206. [Google Scholar] [CrossRef]
- Rodríguez, M.; Guardiola, M.; Oliva, I.; Vallvé, J.C.; Ferré, R.; Masana, L.; Parra, S.; Ribalta, J.; Castro, A. Low-density lipoprotein net charge is a risk factor for atherosclerosis in lupus patients independent of lipid concentrations. Int. J. Rheum. Dis. 2019, 22, 480–487. [Google Scholar] [CrossRef] [PubMed]
- Yang, X.-F.; Ding, F.-M.; Ye, Y.-C.; Zhang, S.-Y. Relationship between Neutrophil-to-Lymphocyte Ratio and Pulse Wave Velocity in Young Patients with Systemic Lupus Erythematosus. Chin. Med. J. 2018, 131, 10–15. [Google Scholar] [CrossRef] [PubMed]
- Giannelou, M.; Nezos, A.; Fragkioudaki, S.; Kasara, D.; Maselou, K.; Drakoulis, N.; Ioakeimidis, D.; Moutsopoulos, H.M.; Mavragani, C.P. Contribution of MTHFR gene variants in lupus related subclinical atherosclerosis. Clin. Immunol. 2018, 193, 110–117. [Google Scholar] [CrossRef] [PubMed]
- García-Carrasco, M.; Soto-Santillán, P.; Mendoza-Pinto, C.; González-Ramírez, R.; López-Carmona, A.L.; Munguía-Realpozo, P.; Etchegaray-Morales, I.; Méndez-Martínez, S.; Gálvez-Romero, J.L.; López-Colombo, A.; et al. The Role of Circulating Regulatory T Cell Levels on Subclinical Atherosclerosis and Cardiovascular Risk Factors in Women with Systemic Lupus Erythematosus. Mediat. Inflamm. 2018, 2018, 3271572. [Google Scholar] [CrossRef] [PubMed]
- Mellor-Pita, S.; Tutor-Ureta, P.; Rosado, S.; Alkadi, K.; Granado, F.; Jimenez-Ortiz, C.; Castejon, R. Calcium and vitamin D supplement intake may increase arterial stiffness in systemic lupus erythematosus patients. Clin. Rheumatol. 2019, 38, 1177–1186. [Google Scholar] [CrossRef]
- Quevedo-Abeledo, J.C.; Rúa-Figueroa, Í.; Sánchez-Pérez, H.; Tejera-Segura, B.; de Vera-González, A.; González-Delgado, A.; Llorca, J.; González-Gay, M.; Ferraz-Amaro, I. Disease Damage Influences Cardiovascular Risk Reclassification Based on Carotid Ultrasound in Patients with Systemic Lupus Erythematosus. J. Rheumatol. 2019, 46, 483–491. [Google Scholar] [CrossRef]
- Petri, M.A.; Barr, E.; Magder, L.S. Development of a systemic lupus erythematosus cardiovascular risk equation. Lupus Sci. Med. 2019, 6, e000346. [Google Scholar] [CrossRef]
- Przywara-Chowaniec, B.; Blachut, D.; Harpula, J.; Beres, M.; Nowak, A.; Nowalany-Kozielska, E. Systemic Lupus Erythematosus, Its Impact on Selected Cardiovascular Risk Factors, and Correlation with Duration of Illness: A Pilot Study. Cardiol. Res. Pract. 2020, 2020, 7025329. [Google Scholar] [CrossRef]
- Fernandez-Garces, M.; Haro, G.; Mico, M.L. Predisposing factors to nonfatal cardiovascular events in women with systemic lupus erythematosus. An observational, cross-sectional, multicenter study in Spain from the risk/systemic lupus erythematosus thematic network. Medicine 2019, 98, e17489. [Google Scholar] [CrossRef]
- Masson, W.; Rossi, E.; Mora-Crespo, L.M.; Cornejo-Peña, G.; Pessio, C.; Gago, M.; Alvarado, R.N.; Scolnik, M. Cardiovascular risk stratification and appropriate use of statins in patients with systemic lupus erythematosus according to different strategies. Clin. Rheumatol. 2020, 39, 455–462. [Google Scholar] [CrossRef]
- Salvetti, M.; Paini, A.; Andreoli, L.; Stassaldi, D.; Aggiusti, C.; Bertacchini, F.; Rosei, C.A.; Piantoni, S.; Franceschini, F.; Tincani, A.; et al. Cardiovascular target organ damage in premenopausal systemic lupus erythematosus patients and in controls: Are there any differences? Eur. J. Intern. Med. 2020, 73, 76–82. [Google Scholar] [CrossRef] [PubMed]
- Patiño-Trives, A.M.; Pérez-Sánchez, C.; Pérez-Sánchez, L.; Luque-Tévar, M.; Ábalos-Aguilera, M.C.; Alcaide-Ruggiero, L.; Arias-de la Rosa, I.; Román-Rodríguez, C.; Seguí, P.; Espinosa, M.; et al. Anti-dsDNA Antibodies Increase the Cardiovascular Risk in Systemic Lupus Erythematosus Promoting a Distinctive Immune and Vascular Activation. Arterioscler. Thromb. Vasc. Biol. 2021, 41, 2417–2430. [Google Scholar] [CrossRef] [PubMed]
- Weber, B.N.; Stevens, E.; Barrett, L.; Bay, C.; Sinnette, C.; Brown, J.M.; Divakaran, S.; Bibbo, C.; Hainer, J.; Dorbala, S.; et al. Coronary Microvascular Dysfunction in Systemic Lupus Erythematosus. J. Am. Heart Assoc. 2021, 10, e018555. [Google Scholar] [CrossRef]
- Campos-López, B.; Meza-Meza, M.R.; Parra-Rojas, I.; Ruiz-Ballesteros, A.I.; Vizmanos-Lamotte, B.; Muñoz-Valle, J.F.; Montoya-Buelna, M.; Cerpa-Cruz, S.; Bernal-Hernández, L.E.; De la Cruz-Mosso, U. Association of cardiometabolic risk status with clinical activity and damage in systemic lupus erythematosus patients: A cross-sectional study. Clin. Immunol. 2021, 222, 108637. [Google Scholar] [CrossRef] [PubMed]
- Croca, S.C.; Griffin, M.; Farinha, F.; Isenberg, D.A.; Nicolaides, A.; Rahman, A. Total plaque area and plaque echogenicity are novel measures of subclinical atherosclerosis in patients with systemic lupus erythematosus. Rheumatology 2021, 60, 4185–4198. [Google Scholar] [CrossRef]
- Correa-Rodríguez, M.; Pocovi-Gerardino, G.; Callejas-Rubio, J.-L.; Ríos-Fernández, R.; Martín-Amada, M.; Cruz-Caparrós, M.-G.; DelOlmo-Romero, S.; Ortego-Centeno, N.; Rueda-Medina, B. Vitamin D Levels are Associated with Disease Activity and Damage Accrual in Systemic Lupus Erythematosus Patients. Biol. Res. Nurs. 2021, 23, 455–463. [Google Scholar] [CrossRef] [PubMed]
- Fox, H.; Jung, O.; Bartel, C.; Hauser, I.A.; Ehrlich, J.R. Profile of cardiovascular risk factors in patients with systemic Lupus erythematosus: The CArdiovascular Risk Assessment STudy in Lupus erythematosus (CASTLE SLE) study. J. Fur Kardiol. 2018, 25, 128–134. [Google Scholar]
- Chandrashekara, S.; Dhote, S.V.; Anupama, K.R. The Differential Influence of Immunological Process of Autoimmune Disease on Lipid Metabolism: A Study on RA and SLE. Indian J. Clin. Biochem. 2019, 34, 52–59. [Google Scholar] [CrossRef]
- Rashad, N.M.; Allam, R.M.; Said, D.; Ali, A.E.; Mohy, N.M.; Abomandour, H.G. Influence of +299G>A and +62GEfA resistin gene promoter variants on cardiovascular risk in Egyptian women with systemic lupus erythematosus. Egypt. Rheumatol. 2019, 41, 215–220. [Google Scholar] [CrossRef]
- Quevedo-Abeledo, J.C.; Sánchez-Pérez, H.; Tejera-Segura, B.; Armas-Rillo, L.; Armas-González, E.; Machado, J.D.; González-Gay, M.A.; Díaz-González, F.; Ferraz-Amaro, I. Differences in Capacity of High-Density Lipoprotein Cholesterol Efflux between Patients with Systemic Lupus Erythematosus and Rheumatoid Arthritis. Arthritis Care Res. 2021, 73, 1590–1596. [Google Scholar] [CrossRef]
- Pocovi-Gerardino, G.; Correa-Rodríguez, M.; Callejas-Rubio, J.-L.; Ríos-Fernández, R.; Martín-Amada, M.; Cruz-Caparros, M.-G.; Rueda-Medina, B.; Ortego-Centeno, N. Beneficial effect of Mediterranean diet on disease activity and cardiovascular risk in systemic lupus erythematosus patients: A cross-sectional study. Rheumatology 2021, 60, 160–169. [Google Scholar] [CrossRef] [PubMed]
- Pocovi-Gerardino, G.; Correa-Rodríguez, M.; Rubio, J.-L.C.; Fernández, R.R.; Amada, M.M.; Caparros, M.-G.C.; Rueda-Medina, B.; Ortego-Centeno, N. The Relationships of High-Sensitivity C-Reactive Protein and Homocysteine Levels with Disease Activity, Damage Accrual, and Cardiovascular Risk in Systemic Lupus Erythematosus. Biol. Res. Nurs. 2020, 22, 169–177. [Google Scholar] [CrossRef]
- Sánchez-Pérez, H.; Quevedo-Abeledo, J.C.; de Armas-Rillo, L.; Rua--Figueroa, Í.; Tejera-Segura, B.; Armas-González, E.; Machado, J.D.; García-Dopico, J.A.; Jimenez-Sosa, A.; Rodríguez--Lozano, C.; et al. Impaired HDL cholesterol efflux capacity in systemic lupus erythematosus patients is related to subclinical carotid atherosclerosis. Rheumatology 2020, 59, 2847–2856. [Google Scholar] [CrossRef] [PubMed]
- Ajeganova, S.; Gustafsson, T.; Lindberg, L.; Hafstrom, I.; Frostegard, J. Similar progression of carotid intima-media thickness in 7-year surveillance of patients with mild SLE and controls, but this progression is still promoted by dyslipidaemia, lower HDL levels, hypertension, history of lupus nephritis and a higher prednisolone usage in patients. Lupus Sci. Med. 2020, 7, e000362. [Google Scholar] [PubMed]
- Jordan-Gonzalez, P.; Shum, L.M.; Gonzalez-Sepulveda, L.; Vila, L.M. Clinical correlates and outcomes in a group of Puerto Ricans with systemic lupus erythematosus hospitalized due to severe infections. SAGE Open Med. 2018, 6, 2050312118778385. [Google Scholar] [CrossRef]
- Chanloung, W.; Kasitanon, N.; Wichainun, R.; Louthrenoo, W. Thrombotic risk assessment in patients with systemic lupus erythematosus: Validation of the adjusted-Global Antiphospholipid Syndrome Score (aGAPSS) in Thai patients. Int. J. Rheum. Dis. 2021, 24, 1510–1519. [Google Scholar] [CrossRef]
- Jiang, M.Y.; Hwang, J.C.; Feng, I.J. Impact of Diabetes Mellitus on the Risk of End-Stage Renal Disease in Patients with Systemic Lupus Erythematosus. Sci. Rep. 2018, 8, 6008. [Google Scholar] [CrossRef]
- Gergianaki, I.; Garantziotis, P.; Adamichou, C.; Saridakis, I.; Spyrou, G.; Sidiropoulos, P.; Bertsias, G. High Comorbidity Burden in Patients with SLE: Data from the Community-Based Lupus Registry of Crete. J. Clin. Med. 2021, 10, 998. [Google Scholar] [CrossRef]
- Falasinnu, T.; Chaichian, Y.; Simard, J.F. Impact of Sex on Systemic Lupus Erythematosus-Related Causes of Premature Mortality in the United States. J. Women’s Health 2017, 26, 1214–1221. [Google Scholar] [CrossRef]
- Gamal, S.M.; Mohamed, S.S.; Tantawy, M.; Siam, I.; Soliman, A.; Niazy, M.H. Lupus-related vasculitis in a cohort of systemic lupus erythematosus patients. Arch. Rheumatol. 2021, 36, 595–692. [Google Scholar] [CrossRef]
- Alian, S.; Khalil, S.; Zaghlol, R. Charlson Comorbidity Index in patients with systemic lupus erythematosus in Egypt and its relation with disease characteristics. Indian J. Rheumatol. 2019, 14, 277–282. [Google Scholar] [CrossRef]
- Behiry, M.E.; Salem, M.R.; Alnaggar, A.R. Assessment of nutritional status and disease activity level in Systemic Lupus Erythematosus patients at a tertiary care hospital. Rev. Colomb. De Reumatol. 2019, 26, 97–104. [Google Scholar]
- Dias-Santos, A.; Ferreira, J.T.; Pinheiro, S.; Cunha, J.P.; Alves, M.; Papoila, A.L.; Moraes-Fontes, M.F.; Proença, R. Neurodegeneration in systemic lupus erythematosus: Layer by layer retinal study using optical coherence tomography. Int. J. Retin. Vitr. 2020, 6, 15. [Google Scholar] [CrossRef] [PubMed]
- Seguro, L.P.C.; Paupitz, J.A.; Caparbo, V.F.; Bonfa, E.; Pereira, R.M.R. Increased visceral adipose tissue and altered adiposity distribution in premenopausal lupus patients: Correlation with cardiovascular risk factors. Lupus 2018, 27, 1001–1006. [Google Scholar] [CrossRef] [PubMed]
- Tsyhanyk, L.; Abrahamovych, U.; Abrahamovych, O.; Chemes, V.; Guta, S. Bone Mineral Density and the Prevalence of Its Disorders in Patients with Systemic Lupus Erythematosus and Syntropic Comorbid Lesions. Georgian Med. News 2021, 103–108. [Google Scholar]
- Pedrosa, T.D.N.; Kupa, L.D.V.K.; Pasoto, S.G.; Aikawa, N.E.; Duarte, N.; Borba, E.F.; Bonfá, E.; Silva, C.A.A. The influence of obesity on hydroxychloroquine blood levels in lupus nephritis patients. Lupus 2021, 30, 554–559. [Google Scholar] [CrossRef]
- Apostolopoulos, D.; Vincent, F.; Hoi, A.; Morand, E. Associations of metabolic syndrome in SLE. Lupus Sci. Med. 2020, 7, e000436. [Google Scholar] [CrossRef]
- Gomez, A.; Butrus, F.H.; Johansson, P.; Åkerström, E.; Soukka, S.; Emamikia, S.; Enman, Y.; Pettersson, S.; Parodis, I. Impact of overweight and obesity on patient-reported health-related quality of life in systemic lupus erythematosus. Rheumatology 2021, 60, 1260–1272. [Google Scholar] [CrossRef]
- Kang, J.-H.; Xu, H.; Choi, S.-E.; Park, D.-J.; Lee, J.-K.; Kwok, S.-K.; Kim, S.-K.; Choe, J.-Y.; Kim, H.-A.; Sung, Y.-K.; et al. Obesity increases the incidence of new-onset lupus nephritis and organ damage during follow-up in patients with systemic lupus erythematosus. Lupus 2020, 29, 578–586. [Google Scholar] [CrossRef]
- Meza-Meza, M.R.; Vizmanos-Lamotte, B.; Muñoz-Valle, J.F.; Parra-Rojas, I.; Garaulet, M.; Campos-López, B.; Montoya-Buelna, M.; Cerpa-Cruz, S.; Martínez-López, E.; Oregon-Romero, E.; et al. Relationship of Excess Weight with Clinical Activity and Dietary Intake Deficiencies in Systemic Lupus Erythematosus Patients. Nutrients 2019, 11, 2683. [Google Scholar] [CrossRef]
- Hammam, N.; Rashad, S.M.; Mohamed, A.A.A. Metabolic syndrome in systemic lupus erythematosus patients: Relationship to disease activity and neuropsychiatric lupus. Z. Rheumatol. 2018, 77, 938–945. [Google Scholar] [CrossRef] [PubMed]
- Mak, A.; Kow, N.Y.; Schwarz, H.; Gong, L.; Tay, S.H.; Ling, L.H. Endothelial dysfunction in systemic lupus erythematosus—A case-control study and an updated meta-analysis and meta-regression. Sci. Rep. 2017, 7, 7320. [Google Scholar] [CrossRef] [PubMed]
- Tektonidou, M.G.; Kravvariti, E.; Konstantonis, G.; Tentolouris, N.; Sfikakis, P.P.; Protogerou, A. Subclinical atherosclerosis in Systemic Lupus Erythematosus: Comparable risk with Diabetes Mellitus and Rheumatoid Arthritis. Autoimmun. Rev. 2017, 16, 308–312. [Google Scholar] [CrossRef] [PubMed]
- Tsang, A.S.M.W.; Bultink, I.E.; Heslinga, M.; Voskuyl, A.E. Both prolonged remission and Lupus Low Disease Activity State are associated with reduced damage accrual in systemic lupus erythematosus. Rheumatology 2017, 56, 121–128. [Google Scholar] [CrossRef] [PubMed]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).