Abstract
The present study aimed to assess the changes in the prevalence and determinants of self-reported hypertension among older adults during the COVID-19 pandemic in Bangladesh. This repeated cross-sectional study was conducted on two successive occasions (October 2020 and September 2021), overlapping the first and second waves of the COVID-19 pandemic in Bangladesh. The survey was conducted through telephone interviews among Bangladeshi older adults aged 60 years and above. The prevalence of hypertension was measured by asking a question about whether a doctor or health professional told the participants that they have hypertension or high blood pressure and/or whether they are currently using medication to control it. We also collected information on the socio-economic characteristics of the participants, their cognitive ability, and their COVID-19-related attributes. A total of 2077 older adults with a mean age of 66.7 ± 6.4 years participated in the study. The samples were randomly selected on two successive occasions from a pre-established registry developed by the ARCED Foundation. Thus, the sample in the 2021-survey (round two; n = 1045) was not the same as that in the 2020-survey (round one; n = 1031) but both were drawn from the same population. The findings revealed that the prevalence of hypertension significantly increased across the two periods (43.7% versus 56.3%; p = 0.006). The odds of hypertension were 1.34 times more likely in round two than in the round one cohort (AOR 1.34, 95% CI 1.06–1.70). We also found that having formal schooling, poorer memory or concentration, and having had received COVID-19 information were all associated with an increased risk of hypertension in both rounds (p < 0.05). The findings of the present study suggest providing immediate support to ensure proper screening, control, and treatment of hypertension among older adults in Bangladesh.
1. Introduction
The world has been crippled by the pandemic outbreak caused by severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) since December 2019 [1]. As of 4 August 2022, COVID-19 has affected over 578 million people worldwide in at least 166 countries [2]. The number of deaths has already exceeded 6.4 million globally and is expected to increase further as the disease spreads rapidly [2]. Recent studies have shown that COVID-19 patients of older age and with a co-morbidity, such as cardiovascular disease, diabetes, hypertension, or chronic lung disease, are at a higher risk of infection with a higher mortality rate than the general population [3,4,5]. Hypertension was the most commonly reported co-morbidity in COVID-19 patients [6].
In recent years, hypertension, a non-communicable disease (NCD), has been recognised as the leading health issue as it affects 1.39 billion individuals worldwide [7], and the prevalence of hypertension increases with age (affecting approximately 70% of older adults) [8]. Evidence also suggests that the majority of the population with hypertension resides in low-income and middle-income countries (LMICs) [9]. Hypertension, responsible for 13% of global deaths, has become one of the most challenging concerns for world public health [10]. By 2025, hypertension-related deaths are anticipated to increase up to 30% worldwide and play a pivotal role in the rising global burden of disease and disability [11,12,13]. Experimental studies identified that SARS-CoV-2 infection could directly or indirectly trigger cardiovascular complications such as myocarditis, cardiomyopathy, and congestive heart failure [14,15]. Furthermore, there is evidence that ‘lockdown’, imposed due to COVID-19, may have exerted some negative consequences on health behaviours, such as increased smoking, poor diet, sedentary lifestyle, and increased alcohol use, resulting in an increased prevalence of chronic diseases including hypertension [16,17]. It is predicted that the COVID-19 pandemic will create another pandemic of NCDs, especially hypertension [18].
The COVID-19 pandemic has not ended yet in Bangladesh. The first wave of COVID-19 started in Bangladesh in early March 2020 and was harsh, and a second wave started at the end of March 2021 [19,20]. Despite government efforts, COVID-19 has reached all 64 administrative districts in Bangladesh, with more than 2 million confirmed cases and 29,298 deaths as of 4 August 2022 [2], with the highest death rate (45%) in the older population [21]. Notably, the aging population is also rapidly growing in Bangladesh; 13 million people are aged 60 years or above, which comprises 8% of the total population [22]. Pre-pandemic data suggests that the overall prevalence of hypertension was 31% in Bangladesh, and the prevalence was higher among the older population aged 60 years and above [23]. The uncertainties and mitigating measures related to the pandemic have changed peoples’ everyday lifestyles, and home confinement may increase the risk of hypertension Previous research also documented that aging is often associated with a lack of memory/cognitive abilities [24], which can be further aggravated during the COVID-19 pandemic [25]. The simultaneous presence of cognitive dysfunction and a high level of hypertension are reported among older adults [26,27]. Therefore, since the age of any individual is a risk factor for COVID-19 infection, cognition, and hypertension occurrence, the ongoing pandemic could significantly exacerbate the condition of hypertension among the older population in Bangladesh.
Pre-pandemic data suggests that the prevalence of hypertension was high among the older population in Bangladesh. According to the 2011 Bangladesh Demographic and Health Survey, the prevalence of hypertension was 35% and 40% among older adults aged 60–69 years and 70+ years, respectively [28]. A recent study, conducted immediately before the pandemic, documented that nearly half of the older adults were hypertensive [29]. Previous studies also identified several factors such as age, nutritional status, and sedentary lifestyles as well as pre-existing co-morbidities associated with hypertension among the adult population in Bangladesh [30,31,32]. However, no studies have documented the prevalence of hypertension in the older population and the changes in factors associated with hypertension over time during the COVID-19 pandemic in Bangladesh. To fill this important gap, we aimed to assess changes in the prevalence of self-reported hypertension in the older population in two timeframes during the COVID-19 pandemic in Bangladesh. We also explored the changes in factors associated with hypertension in the older population during the pandemic in Bangladesh. This research is particularly important from a policy perspective, as a scientific understanding of hypertension prevalence and its determinants is critical to appropriately identify the entry points for interventions to prevent and control hypertension among Bangladeshi older adults during the COVID-19 pandemic.
2. Materials and Methods
2.1. Study Design and Participants
This repeated cross-sectional study was conducted on two successive occasions, i.e., October 2020 and September 2021, overlapping with the first and second waves of the COVID-19 pandemic in Bangladesh. Data was collected from older Bangladeshi adults aged 60 years and above through telephone interviews. As we could not conduct the data collection face-to-face during the COVID-19 pandemic because of the restrictions in movements, we utilised a pre-established registry as a sampling frame that was developed by the ARCED Foundation. This registry was developed by merging the households’ contact information extracted from ten different community-based studies conducted by the ARCED Foundation to explore different social issues during 2016–2020, which included households from all eight administrative divisions of Bangladesh. This registry has also been used as a sampling frame in our previous studies [33,34]. Considering a 50% prevalence with a 5% margin of error, at the 95% confidence level, 90% power of the test, and a 95% response rate, a sample size of 1096 was calculated. However, during the 2020 survey, only 1032 of the approached eligible participants responded to the study, resulting in an overall response rate of approximately 94%. During the 2021 survey, 1045 of the approached eligible participants responded to the study, resulting in an overall response rate of approximately 95%. Based on the population distribution of older adults by geography in Bangladesh, we adopted a probability proportionate to size (of the eight divisions) approach to randomly select the desired number of older adults from each division [22]. Notably, the samples were selected randomly from the registry on two successive occasions (the 2020 survey and 2021 survey). Therefore, the sample was not identical on the two occasions, while the population remained the same. In fact, we ensured that the samples were not overlapped during the two rounds of survey and if there was any incidence of the same sample of the first round selected in the second round, it was replaced by another random selection. The detailed sampling strategy is presented in Figure 1.
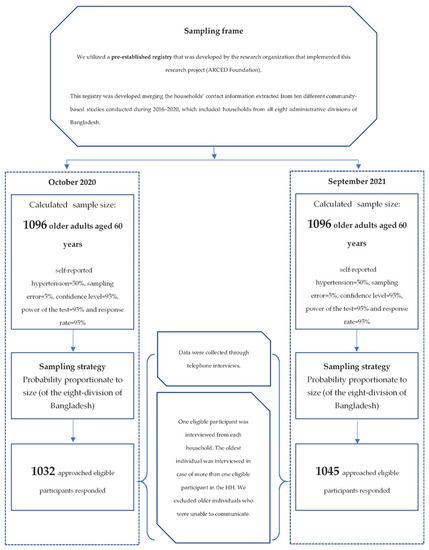
Figure 1.
Sampling strategy and participants selection.
2.2. Measures
2.2.1. Outcome Measure
The outcome of this study was self-reported hypertension. The participants were asked, “Have you told by a doctor or by a health professional that you have hypertension or high blood pressure?” The participants who answered ‘yes’ were also asked, “Are you currently taking any medicine for your hypertension?” [35]. Therefore, self-reported hypertension was defined as having been diagnosed with hypertension/high blood pressure and/or currently taking any medication for it.
2.2.2. Explanatory Variables
An extensive review of available studies guided the selection of explanatory variables [36,37,38,39,40,41]. Explanatory variables considered in this study were administrative division (Barishal, Chattogram, Dhaka, Mymensingh, Khulna, Rajshahi, Rangpur, and Sylhet), age (categorized as 60–69, and ≥70), sex (male/female), marital status (married/without partner), formal schooling (without formal schooling/with formal schooling), family size (≤4 or >4), family monthly income (BDT) (<5000, 5000–10,000, or >10,000), residence (urban/rural), current occupation (employed/unemployed or retired), living arrangement (living alone or with family), walking distance to the nearest health centre (<30 min/≥30 min), memory or concentration problems (no problem/low memory or concentration), and having received COVID-19-related information from health workers (yes/no).
To explore if the participants had any memory or concentration problem, we asked the participants: “Do you have any memory (remembering things properly) or concentration (could concentrate properly while doing any action) problem?” Meanwhile, participants were considered to have received COVID-19-related information from health workers if they mentioned that they received information about the risk factors and prevention of COVID-19.
2.3. Data Collection Tools and Techniques
A pre-tested semi-structured questionnaire was used to collect the information via a telephone interview. Data collection was accomplished electronically using the SurveyCTO mobile app (https://www.surveycto.com/, accessed on 1 May 2022) by trained research assistants, recruited based on previous experience of administering health surveys on the electronic platform. The research assistants were trained extensively before the data collection through Zoom meetings.
The English version of the questionnaire was first translated to the Bangla language and then back translated to English to ensure the content’s consistency. The questionnaire was then piloted among a small sample (n = 10) of older adults to refine the language in the final version. The tool used in the pilot study did not receive any corrections/suggestions from the participants about the contents developed in the Bengali language. We found the questionnaire was reliable with a good internal consistency (Cronbach’s α, 0.72)
2.4. Statistical Analysis
The distribution of the variables was assessed through descriptive analyses. Given our variables’ categorical nature, Chi-squared tests were performed to compare differences in the prevalence of hypertension by explanatory variables, with a 5% level of significance. We used a binary logistic regression model to determine the changes in the prevalence of hypertension after adjusting for all potential covariates in the pooled data. We also assessed the factors associated with hypertension in the first and second rounds of the survey. We executed two separate regression models (round one and round two), and the final models were selected based on the lowest AIC (Akaike information criterion) values. The variables with p < 0.25 in the unadjusted analysis were only included in the multiple regression model [42]. Crude odds ratio (cOR), adjusted odds ratio (aOR), and an associated 95% confidence interval (95% CI) are reported. All analyses were performed using the statistical software package Stata (Version 14.0).
2.5. Ethical Approval
This research was approved by the institutional review board of Institute of Health Economics, University of Dhaka, Bangladesh (Ref: IHE/2020/1037). We sought verbal informed consent from the participants before the survey and their participation was voluntary and without any compensation.
3. Results
3.1. Characteristics of the Participants
Table 1 shows the characteristics of the study participants by survey year. In terms of survey participant coverage, there was a significant difference across geographic areas; for example, the highest coverage was from the Dhaka division in the 2020 survey, while the highest coverage was from the Khulna division in the 2021 survey. In both surveys, most participants were 60–69 years old, male, married, without formal schooling, unemployed/retired, lived with family, and lived in rural areas (Table 1). However, participants’ characteristics (e.g., sex, marital status, education, and income) were significantly different across the survey years. Compared to the 2020 survey, a considerably lower proportion of participants in the 2021 survey was males (59% vs. 66%), married (77% vs. 81%), and without formal education (52% vs. 58%). The proportion of participants living with family, from rural areas, close to health facilities, and who had problems with memory and concentration increased significantly between the survey years. However, we found that fewer people received COVID-19-related information from health workers in the 2021 survey (Table 1).

Table 1.
Characteristics of the participants (n = 2077).
3.2. Changes in the Prevalence of Hypertension
Table 2 shows the changes in the prevalence of hypertension over time and their variation and association with participants’ characteristics. As seen in Table 2, the prevalence of hypertension was significantly increased between the two survey years among the participants (43.7% versus 56.3%; p = 0.006). Moreover, after adjusting for all potential covariates, compared to round one, the odds of hypertension were significantly higher in round two (AOR 1.34, 95% CI 1.06–1.70) (Table 3). The final regression model was adjusted for all the covariates presented in Table 1.

Table 2.
Change in hypertension prevalence over the time (n = 2077).

Table 3.
Odds of change in prevalence of hypertension over the time (n = 2077).
We can also see in Table 2, the prevalence of hypertension was significantly increased among the participants residing in divisions of Chattogram, Rangpur, and Sylhet (43.6% vs. 56.4%; 33.3% vs. 66.7%; and 36.4% vs. 63.6%, respectively), aged 60–69 years (44.8% vs. 55.2%), females (37.7% vs. 62.3%), without partners (35.4% vs. 64.6%), residents of rural areas (40.9% vs. 59.2%), and living with a family (42.4% vs. 57.7%). A significant increase in the prevalence of hypertension was also documented among those who received no formal schooling (35.4% vs. 64.6%), had a family income of 5000–10,000 BDT (32.0% vs. 68.0%) or >10,000 BDT (49.2% vs. 50.8%), were residing with a family with a size of no more than four members (35.8% vs. 64.2%), unemployed or retired (40.1% vs. 59.9%), living near a health facility (36.5% vs. 63.5%), had memory or concentration problems (32.9% vs. 67.1%), and did not receive COVID-19-related information from health workers (38.8% vs. 61.2%).
3.3. Changes in Factors Associated with Hypertension
Table 4 presents the factors associated with hypertension in the first and second survey rounds. In the adjusted analysis, we found that having formal schooling, low memory or concentration, and receiving COVID-19 information were significantly associated with an increased risk of hypertension (p < 0.05) in both rounds. In contrast, in round 1, only participants living alone had a higher risk of hypertension than those living with a family.

Table 4.
Changes in factors associated with hypertension among the participants.
4. Discussion
This study found that the hypertension prevalence in Bangladeshi older people increased significantly from 43.7% in 2020 to 56.3% in 2021. The prevalence of hypertension increased more among female participants than in their male counterparts. Having formal education, being unemployed or in retirement, having a low ability to concentrate, and interacting with health workers to get COVID-19-related information were also significantly associated with a higher prevalence of hypertension. To the best of our knowledge, these findings are novel in Bangladesh, meaning that no studies explored the changes in the prevalence of hypertension in older adults during the COVID-19 pandemic in Bangladesh. However, studies in other settings documented an increased prevalence of uncontrolled blood pressure among different population groups during the COVID-19 pandemic, compared to the pre-pandemic period [43,44,45,46]. For example, a longitudinal study conducted in the United States reported that the prevalence of hypertension increased significantly among female participants during the first year of the COVID-19 pandemic, from 38% in 2020 to 62% in 2021. The pandemic situation also severely affected healthcare professionals in low-income settings. A study conducted in India found that the COVID-19 pandemic significantly impacted the blood pressure of hospital staff, including doctors and nurses, with an alarming increase in risk to their health [47].
The COVID-19 pandemic forced many countries, including Bangladesh, to impose restrictions on the movement of citizens, including limiting social interactions, implementing lockdowns, and imposing strict quarantine protocols to prevent the spread of the virus [21,48]. These restrictions greatly impacted people’s lives and their psychosocial well-being. Frequent lockdowns and quarantines limited access to physical activity and regular exercise while increasing smoking and other unhealthy behaviours. Such harmful lifestyle choices directly affect uncontrolled blood pressure and increase the prevalence of hypertension at the population level [49]. The COVID-19 pandemic also affected access to regular health services for chronic disease management, particularly in developing countries where digitalised healthcare is not yet established. As a result, citizens could not access regular health check-ups and doctor consultations, and many healthcare facilities restricted entry or shut down due to the pandemic [50,51]. A recent study in Bangladesh also found that chronic disease management and routine health services for the older population were seriously hampered during the COVID-19 pandemic [51]. All of these factors might have contributed to an increase in the prevalence of hypertension during this pandemic.
This study identified educational status as an important predictor of hypertension. This is because educational status is associated with health literacy, which affects the capability of an individual to attain, process, and understand the health information and services necessary to make appropriate personal decisions [52]. Education can also lead to accurate health beliefs and decrease misconceptions, thus facilitating the making of informed lifestyle choices and promoting self-advocacy. A previous systematic review found that people with low educational status were twice as likely to be hypertensive (OR 2.02, 95% CI 1.55–2.63) compared to those with a higher educational status [53]. However, the results of our analysis contradicted this evidence, as we found that participants with formal education were more likely to have hypertension than those with no formal education. This may be because the people with formal education relied more on COVID-19 information that they collected from various sources, including the internet, which might have resulted in increased fear and anxiety. Evidence suggests that increased fear and anxiety are connected to high blood pressure [54,55]. A recent systematic review of 18 studies conducted in Southeast Asia reported mixed associations between education and chronic diseases related to multimorbidity [56]. Considering such fluctuating evidence, further studies are required to better understand the association between educational status and the prevalence of hypertension. Such studies could aid in the development of appropriate interventions to control hypertension in populations with low socio-economic status.
This study found that the unemployed or retired respondents who participated in round two of our survey study were 1.7 times more at risk of being hypertensive than the employed respondents. This may be because of the increased anxiety level among older people due to their lack of financial security caused by the pandemic. Previous studies in Bangladesh found that more than one-fourth of the participants were not receiving salaries due to the pandemic. Thus, they were more likely to suffer from anxiety and depressive symptoms [39,57]. Another important finding of our study was that participants with memory and concentration problems or low cognitive function were more likely to suffer from hypertension than those without these issues. Previous research also documented that hypertension is associated with cognitive impairment, such as loss of cognitive functions, memory, concentration, and language, which significantly decreases the quality of life with increasing age [58,59,60,61]. Previous research reported the simultaneous presence of increased hypertension and loss of cognitive abilities [26,27]. In particular, it is well established that hypertension can affect brain structure and function and it is most consistently linked to late-life cognitive decline and dementia [62]. However, whether cognitive decline increases the risk of hypertension is not well described in the literature [63].
Community health workers in Bangladesh have been well known for delivering health promotion activities including health education through a community-based approach [64]. Interacting with community healthcare workers may benefit patients’ health by facilitating the latter’s access to critical health information and providing psychosocial support [65]. However, this study found that participants who responded to both surveys and received COVID-19-related information from healthcare workers were more likely to suffer from hypertension than participants who did not receive COVID-19 information from healthcare workers. Although surprising, this finding provides critical information about the quality of health education-related services provided by healthcare workers during this time. Thus, healthcare workers may have lacked the COVID-19-related training needed to impart information to older people in Bangladesh. During the initial years of the COVID-19 pandemic, a vast amount of inappropriate or incorrect information was circulated across social media platforms, which may have negatively influenced healthcare workers’ knowledge. A recent WHO study found that the spread of COVID-19-related misinformation via social media and other digital platforms is a threat to global public health [66]. Therefore, it is critical to design and implement appropriate training for healthcare workers to provide correct COVID-19-related information to the older population of Bangladesh.
Strengths and Limitations of the Study
This study has several strengths. Firstly, this is the first study reporting the change in the prevalence of and factors associated with hypertension among the older population during the COVID-19 pandemic in Bangladesh. Second, this study represents one of the most unresearched population in Bangladesh during the COVID-19 pandemic.
Nevertheless, the study was subjected to several limitations as well. First, we could not develop a panel; instead, we followed a repeated cross-sectional design. Thus, the change suggests a trend observed in a population and does not indicate changes experienced at the individual level. Second, our study was limited to quantitative analysis and points to potential factors. A qualitative study may shed better light on the underlying reasons for the change. In addition, the hypertension was self-reported and was therefore subjected to reporting bias. Moreover, this study did not measure cognitive function with an appropriate clinically validated tool; thus, the findings must be interpreted cautiously.
5. Conclusions
The present study documented an increased prevalence of hypertension among the older population during the pandemic in Bangladesh. The study also highlighted those specific subgroups of the population, such as those having formal schooling, who had low memory or concentration, and who received COVID-19-related information, had a higher risk of increased prevalence of hypertension in both rounds. The findings are particularly crucial for policymakers and public health practitioners to emphasise the need to provide immediate support to ensure the prevention and early management of hypertension, specifically among the most vulnerable segment of the community during this pandemic. Adequate training and the involvement of community health workers could be of value in this regard. Specifically, they could undertake the tasks such as screening for hypertension and providing psychosocial supports during this emergency period.
Author Contributions
Conceptualisation, S.K.M.; methodology, S.K.M., A.M.A. and U.N.Y.; formal analysis, S.K.M.; writing—original draft preparation, S.K.M., A.M.A., U.N.Y., F.K., M.N.H., D.L. and A.A.C.; writing—review and editing, H.S. and D.L.; supervision, S.K.M. and A.M.A.; project administration, S.K.M., A.M.A. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
The study protocol was approved by the Institutional Review Board of the Institute of Health Economics, the University of Dhaka, Bangladesh (Ref: IHE/2020/1037).
Informed Consent Statement
Verbal informed consents were sought from the participants before administering the survey. Participation was voluntary, and participants did not receive any compensation.
Data Availability Statement
The data is available upon reasonable request from the corresponding author.
Acknowledgments
We acknowledge the role of Sadia Sumaia Chowdhury, Programme Manager, ARCED Foundation and Zahirul Islam, Project Associate, ARCED Foundation, for their support in data collection for the study.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Zhu, N.; Zhang, D.; Wang, W.; Li, X.; Yang, B.; Song, J.; Zhao, X.; Huang, B.; Shi, W.; Lu, R. A novel coronavirus from patients with pneumonia in China, 2019. N. Engl. J. Med. 2020, 382, 727–733. [Google Scholar] [CrossRef] [PubMed]
- WHO. WHO Coronavirus Disease (COVID-19) Dashboard. 2020. Available online: https://covid19.who.int/ (accessed on 1 May 2022).
- Singh, A.K.; Gupta, R.; Misra, A. Comorbidities in COVID-19: Outcomes in hypertensive cohort and controversies with renin angiotensin system blockers. Diabetes Metab. Syndr. Clin. Res. Rev. 2020, 14, 283–287. [Google Scholar] [CrossRef] [PubMed]
- Mancusi, C.; Grassi, G.; Borghi, C.; Ferri, C.; Muiesan, M.L.; Volpe, M.; Iaccarino, G.; SARS-RAS Investigator Group. Clinical Characteristics and Outcomes of Patients with COVID-19 Infection: The Results of the SARS-RAS Study of the Italian Society of Hypertension. High Blood Press. Cardiovasc. Prev. 2021, 28, 5–11. [Google Scholar] [CrossRef] [PubMed]
- Wu, Z.; McGoogan, J.M. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: Summary of a report of 72,314 cases from the Chinese Center for Disease Control and Prevention. JAMA 2020, 323, 1239–1242. [Google Scholar] [CrossRef] [PubMed]
- Mubarik, S.; Liu, X.; Eshak, E.S.; Liu, K.; Liu, Q.; Wang, F.; Shi, F.; Wen, H.; Bai, J.; Yu, C. The Association of Hypertension with the Severity of and Mortality from the COVID-19 in the Early Stage of the Epidemic in Wuhan, China: A Multicenter Retrospective Cohort Study. Front. Med. 2021, 8, 631. [Google Scholar] [CrossRef] [PubMed]
- Mills, K.T.; Stefanescu, A.; He, J. The global epidemiology of hypertension. Nat. Rev. Nephrol. 2020, 16, 223–237. [Google Scholar] [CrossRef]
- Mozaffarian, D.; Benjamin, E.J.; Go, A.S.; Arnett, D.K.; Blaha, M.J.; Cushman, M.; De Ferranti, S.; Després, J.-P.; Fullerton, H.J.; Howard, V.J. Heart disease and stroke statistics—2015 update: A report from the American Heart Association. Circulation 2015, 131, e29–e322. [Google Scholar] [CrossRef]
- Zhou, B.; Carrillo-Larco, R.M.; Danaei, G.; Riley, L.M.; Paciorek, C.J.; Stevens, G.A.; Gregg, E.W.; Bennett, J.E.; Solomon, B.; Singleton, R.K. Worldwide trends in hypertension prevalence and progress in treatment and control from 1990 to 2019: A pooled analysis of 1201 population-representative studies with 104 million participants. Lancet 2021, 398, 957–980. [Google Scholar] [CrossRef]
- Mendis, S.; Puska, P.; Norrving, B.; WHO. Global Atlas on Cardiovascular Disease Prevention and Control; World Health Organization: Geneva, Switzerland, 2011. [Google Scholar]
- Sarki, A.M.; Nduka, C.U.; Stranges, S.; Kandala, N.-B.; Uthman, O.A. Prevalence of hypertension in low-and middle-income countries: A systematic review and meta-analysis. Medicine 2015, 94, e1959. [Google Scholar] [CrossRef]
- Kearney, P.M.; Whelton, M.; Reynolds, K.; Muntner, P.; Whelton, P.K.; He, J. Global burden of hypertension: Analysis of worldwide data. Lancet 2005, 365, 217–223. [Google Scholar] [CrossRef]
- Mills, K.T.; Bundy, J.D.; Kelly, T.N.; Reed, J.E.; Kearney, P.M.; Reynolds, K.; Chen, J.; He, J. Global disparities of hypertension prevalence and control: A systematic analysis of population-based studies from 90 countries. Circulation 2016, 134, 441–450. [Google Scholar] [CrossRef] [PubMed]
- Edwards, S.; Small, J.D.; Geratz, J.D.; Alexander, L.K.; Baric, R.S. An experimental model for myocarditis and congestive heart failure after rabbit coronavirus infection. J. Infect. Dis. 1992, 165, 134–140. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Madjid, M.; Safavi-Naeini, P.; Solomon, S.D.; Vardeny, O. Potential effects of coronaviruses on the cardiovascular system: A review. JAMA Cardiol. 2020, 5, 831–840. [Google Scholar] [CrossRef] [PubMed]
- Central Statistics Office. Social Impact of COVID-19 Survey November 2020 Well-Being and Lifestyle under Level 5 Restrictions. 2020. Available online: https://www.cso.ie/en/releasesandpublications/ep/p-sic19wbl5/socialimpactofcovid-19surveynovember2020well-beingandlifestyleunderlevel5restrictions/ (accessed on 11 January 2022).
- I-PARC. Impact of COVID-19 Restrictions on Sport and Recreational Walking, Q1 2021. 2021. Available online: https://i-parc.ie/?p=2026 (accessed on 11 January 2022).
- Hall, G.; Laddu, D.R.; Phillips, S.A.; Lavie, C.J.; Arena, R. A tale of two pandemics: How will COVID-19 and global trends in physical inactivity and sedentary behavior affect one another? Prog. Cardiovasc. Dis. 2021, 64, 108. [Google Scholar] [CrossRef] [PubMed]
- Bari, R.; Sultana, F. Second Wave of COVID-19 in Bangladesh: An integrated and coordinated set of actions is crucial to tackle current upsurge of cases and deaths. Front. Public Health 2021, 9, 699918. [Google Scholar] [CrossRef] [PubMed]
- Daria, S.; Islam, M.R. The second wave of COVID-19 pandemic in Bangladesh: An urgent call to save lives. Asia Pac. J. Public Health 2021, 33, 665–666. [Google Scholar] [CrossRef] [PubMed]
- Huda, M.N.; Uddin, H.; Hasan, M.K.; Malo, J.S.; Duong, M.C.; Rahman, M.A. Examining Bangladesh’s responses to COVID-19 in light of Vietnam: Lessons learned. Glob. Biosecurity 2021, 3, 1–14. [Google Scholar]
- Bangladesh Bureau of Statistics. Elderly Population in Bangladesh: Current Features and Future Perspectives; Bangladesh Bureau of Statistics, Ministry of Bangladesh, Government of Bangladesh: Dhaka, Bangladesh, 2015.
- Chowdhury, M.Z.I.; Rahman, M.; Akter, T.; Akhter, T.; Ahmed, A.; Shovon, M.A.; Farhana, Z.; Chowdhury, N.; Turin, T.C. Hypertension prevalence and its trend in Bangladesh: Evidence from a systematic review and meta-analysis. Clin. Hypertens. 2020, 26, 10. [Google Scholar] [CrossRef]
- Murman, D.L. (Ed.) The Impact of Age on Cognition 2015; Thieme Medical Publishers: New York, NY, USA, 2015. [Google Scholar]
- Li, Y.; Godai, K.; Kido, M.; Komori, S.; Shima, R.; Kamide, K.; Kabayama, M. Cognitive decline and poor social relationship in older adults during COVID-19 pandemic: Can information and communications technology (ICT) use helps? BMC Geriatr. 2022, 22, 375. [Google Scholar] [CrossRef]
- Farron, M.R.; Kabeto, M.U.; Levine, D.A.; Wixom, C.R.; Langa, K.M. Blood pressure and cognitive function among older adults in India. J. Int. Med. Res. 2022, 50, 03000605211068720. [Google Scholar] [CrossRef]
- Lazo-Porras, M.; Ortiz-Soriano, V.; Moscoso-Porras, M.; Runzer-Colmenares, F.M.; Málaga, G.; Jaime Miranda, J. Cognitive impairment and hypertension in older adults living in extreme poverty: A cross-sectional study in Peru. BMC Geriatr. 2017, 17, 250. [Google Scholar] [CrossRef] [PubMed]
- Rahman, M.M.; Gilmour, S.; Akter, S.; Abe, S.K.; Saito, E.; Shibuya, K. Prevalence and control of hypertension in Bangladesh: A multilevel analysis of a nationwide population-based survey. J. Hypertens. 2015, 33, 465–472. [Google Scholar] [CrossRef] [PubMed]
- Hanif, A.A.M.; Shamim, A.A.; Hossain, M.M.; Hasan, M.; Khan, M.S.A.; Hossaine, M.; Ullah, M.A.; Sarker, S.K.; Rahman, S.M.M.; Mitra, D.K. Gender-specific prevalence and associated factors of hypertension among elderly Bangladeshi people: Findings from a nationally representative cross-sectional survey. BMJ Open 2021, 11, e038326. [Google Scholar] [CrossRef] [PubMed]
- Rahman, M.; Zaman, M.M.; Islam, J.Y.; Chowdhury, J.; Ahsan, H.A.M.N.; Rahman, R.; Hassan, M.; Hossain, Z.; Alam, B.; Yasmin, R. Prevalence, treatment patterns, and risk factors of hypertension and pre-hypertension among Bangladeshi adults. J. Hum. Hypertens. 2018, 32, 334–348. [Google Scholar] [CrossRef] [PubMed]
- Islam, J.Y.; Zaman, M.M.; Haq, S.A.; Ahmed, S.; Al-Quadir, Z. Epidemiology of hypertension among Bangladeshi adults using the 2017 ACC/AHA hypertension clinical practice guidelines and joint National Committee 7 guidelines. J. Hum. Hypertens. 2018, 32, 668–680. [Google Scholar] [CrossRef] [PubMed]
- Khanam, R.; Ahmed, S.; Rahman, S.; Al Kibria, G.M.; Syed, J.R.R.; Khan, A.M.; Moin, S.M.I.; Ram, M.; Gibson, D.G.; Pariyo, G. Prevalence and factors associated with hypertension among adults in rural Sylhet district of Bangladesh: A cross-sectional study. BMJ Open 2019, 9, e026722. [Google Scholar] [CrossRef]
- Mistry, S.K.; Harris, E.; Harris, M. Community health workers as healthcare navigators in primary care chronic disease management: A systematic review. J. Gen. Intern. Med. 2021, 36, 2755–2771. [Google Scholar] [CrossRef]
- Mistry, S.K.; Ali, A.R.M.; Hossain, M.; Yadav, U.N.; Ghimire, S.; Rahman, M.; Irfan, N.M.; Huque, R. Exploring depressive symptoms and its associates among Bangladeshi older adults amid COVID-19 pandemic: Findings from a cross-sectional study. Soc. Psychiatry Psychiatr. Epidemiol. 2021, 56, 1487–1497. [Google Scholar] [CrossRef]
- Du, M.; Yin, S.; Wang, P.; Wang, X.; Wu, J.; Xue, M.; Zheng, H.; Zhang, Y.; Liang, D.; Wang, R. Self-reported hypertension in Northern China: A cross-sectional study of a risk prediction model and age trends. BMC Health Serv. Res. 2018, 18, 475. [Google Scholar] [CrossRef]
- Abir, T.; Osuagwu, U.L.; Kalimullah, N.A.; Yazdani, D.M.N.-A.; Husain, T.; Basak, P.; Goson, P.C.; Mamun, A.A.; Permarupan, P.Y.; Milton, A.H. Psychological Impact of COVID-19 Pandemic in Bangladesh: Analysis of a Cross-Sectional Survey. Health Secur. 2021, 19, 468–478. [Google Scholar] [CrossRef]
- Mamun, M.A.; Sakib, N.; Gozal, D.; Bhuiyan, A.I.; Hossain, S.; Bodrud-Doza, M.; Al Mamun, F.; Hosen, I.; Safiq, M.B.; Abdullah, A.H. The COVID-19 pandemic and serious psychological consequences in Bangladesh: A population-based nationwide study. J. Affect. Disord. 2021, 279, 462–472. [Google Scholar] [CrossRef] [PubMed]
- Cheruvu, V.K.; Chiyaka, E.T. Prevalence of depressive symptoms among older adults who reported medical cost as a barrier to seeking health care: Findings from a nationally representative sample. BMC Geriatr. 2019, 19, 192. [Google Scholar] [CrossRef] [PubMed]
- Banna, M.H.A.; Sayeed, A.; Kundu, S.; Christopher, E.; Hasan, M.T.; Begum, M.R.; Kormoker, T.; Dola, S.T.I.; Hassan, M.M.; Chowdhury, S. The impact of the COVID-19 pandemic on the mental health of the adult population in Bangladesh: A nationwide cross-sectional study. Int. J. Environ. Health Res. 2020, 32, 850–861. [Google Scholar] [CrossRef] [PubMed]
- Mistry, S.K.; Ali, A.M.; Akther, F.; Yadav, U.N.; Harris, M.F. Exploring fear of COVID-19 and its correlates among older adults in Bangladesh. Glob. Health 2021, 17, 47. [Google Scholar] [CrossRef] [PubMed]
- Mistry, S.K.; Ali, A.M.; Irfan, N.M.; Yadav, U.N.; Siddique, R.F.; Peprah, P.; Reza, S.; Rahman, Z.; Casanelia, L.; O’Callaghan, C. Prevalence and correlates of depressive symptoms among Rohingya (forcibly displaced Myanmar nationals or FDMNs) older adults in Bangladesh amid the COVID-19 pandemic. Glob. Mental Health. Epidemiol. 2021, 8, e23. [Google Scholar] [CrossRef]
- Liang, K.Y.; Zeger, S.L. Longitudinal data analysis using generalized linear models. Biometrika 1986, 73, 13–22. [Google Scholar] [CrossRef]
- Wojciechowska, W.; Januszewicz, A.; Drożdż, T.; Rojek, M.; Bączalska, J.; Terlecki, M.; Kurasz, K.; Olszanecka, A.; Smólski, M.; Prejbisz, A. Blood Pressure and Arterial Stiffness in Association with Aircraft Noise Exposure: Long-Term Observation and Potential Effect of COVID-19 Lockdown. Hypertension 2021, 79, 325–334. [Google Scholar] [CrossRef]
- Feitosa, F.G.A.M.; Feitosa, A.D.M.; Paiva, A.M.G.; Mota-Gomes, M.A.; Barroso, W.S.; Miranda, R.D.; Barbosa, E.C.D.; Brandão, A.A.; Lima-Filho, J.L.; Sposito, A.C. Impact of the COVID-19 pandemic on blood pressure control: A nationwide home blood pressure monitoring study. Hypertens. Res. 2021, 45, 364–368. [Google Scholar] [CrossRef]
- Girerd, N.; Meune, C.; Duarte, K.; Vercamer, V.; Lopez-Sublet, M.; Mourad, J.-J. Evidence of a Blood Pressure Reduction during the COVID-19 Pandemic and Associated Lockdown Period: Insights from e-Health Data. Telemed. e-Health 2022, 28, 266–270. [Google Scholar] [CrossRef]
- Pengo, M.F.; Albini, F.; Guglielmi, G.; Mollica, C.; Soranna, D.; Zambra, G.; Zambon, A.; Bilo, G.; Parati, G. Home blood pressure during COVID-19-related lockdown in patients with hypertension. Eur. J. Prev. Cardiol. 2022, 25, e94–e96. [Google Scholar] [CrossRef]
- Gupta, A.; Maheshwari, A.; Verma, N.; Jagadeesha, A.; Dariya, S.S.; Sharma, A.; Saxena, D.; Srivastava, A.; Patni, B.; Das, D. Impact of COVID-19 pandemic on blood pressure of healthcare professionals during lockdown—An Indian Study. J. Hypertens. 2021, 39, e203. [Google Scholar] [CrossRef]
- Islam, M.T.; Talukder, A.K.; Siddiqui, M.N.; Islam, T. Tackling the COVID-19 pandemic: The Bangladesh perspective. J. Public Health Res. 2020, 9, 1794. [Google Scholar] [CrossRef] [PubMed]
- Hegde, S.M.; Solomon, S.D. Influence of physical activity on hypertension and cardiac structure and function. Curr. Hypertens. Rep. 2015, 17, 77. [Google Scholar] [CrossRef] [PubMed]
- Ghimire, R.; Adhikari, S. Effects of COVID-19 on non-communicable diseases and reproductive health services in a district hospital of Nepal. Arch. Pulmonol. Respir. Care 2020, 6, 065–067. [Google Scholar]
- Mistry, S.K.; Ali, A.R.M.M.; Yadav, U.N.; Ghimire, S.; Hossain, M.B.; Das Shuvo, S.; Saha, M.; Sarwar, S.; Nirob, M.M.H.; Sekaran, V.C. Older adults with non-communicable chronic conditions and their health care access amid COVID-19 pandemic in Bangladesh: Findings from a cross-sectional study. PLoS ONE 2021, 16, e0255534. [Google Scholar]
- Du, S.; Zhou, Y.; Fu, C.; Wang, Y.; Du, X.; Xie, R. Health literacy and health outcomes in hypertension: An integrative review. Int. J. Nurs. Sci. 2018, 5, 301–309. [Google Scholar] [CrossRef]
- Leng, B.; Jin, Y.; Li, G.; Chen, L.; Jin, N. Socioeconomic status and hypertension: A meta-analysis. J. Hypertens. 2015, 33, 221–229. [Google Scholar] [CrossRef]
- Pan, Y.; Cai, W.; Cheng, Q.; Dong, W.; An, T.; Yan, J. Association between anxiety and hypertension: A systematic review and meta-analysis of epidemiological studies. Neuropsychiatr. Dis. Treat. 2015, 11, 1121. [Google Scholar]
- Celik, M.; Yilmaz, Y.; Karagoz, A.; Kahyaoglu, M.; Cakmak, E.O.; Kup, A.; Celik, F.B.; Karaduman, A.; Kulahcioglu, S.; Izci, S. Anxiety disorder associated with the COVID-19 pandemic causes deterioration of blood pressure control in primary hypertensive patients. Medeni. Med. J. 2021, 36, 83. [Google Scholar]
- Feng, X.; Kelly, M.; Sarma, H. The association between educational level and multimorbidity among adults in Southeast Asia: A systematic review. PLoS ONE 2021, 16, e0261584. [Google Scholar] [CrossRef]
- Sultana, M.S.; Khan, A.H.; Hossain, S.; Islam, T.; Hasan, M.T.; Ahmed, H.U.; Khan, J.A.M. The association between financial hardship and mental health difficulties among adult wage earners during the COVID-19 pandemic in Bangladesh: Findings from a cross-sectional analysis. Front. Psychiatry 2021, 12, 635884. [Google Scholar] [CrossRef] [PubMed]
- Liu, L.; Hayden, K.M.; May, N.S.; Haring, B.; Liu, Z.; Henderson, V.W.; Chen, J.; Gracely, E.J.; Wassertheil-Smoller, S.; Rapp, S.R. Association between blood pressure levels and cognitive impairment in older women: A prospective analysis of the Women’s Health Initiative Memory Study. Lancet Healthy Longev. 2022, 3, E42–E53. [Google Scholar] [CrossRef]
- Petersen, R.C. Clinical practice. Mild cognitive impairment. N. Engl. J. Med. 2011, 364, 2227–2234. [Google Scholar] [CrossRef]
- Reitz, C.; Tang, M.-X.; Manly, J.; Mayeux, R.; Luchsinger, J.A. Hypertension and the risk of mild cognitive impairment. Arch. Neurol. 2007, 64, 1734–1740. [Google Scholar] [CrossRef] [PubMed]
- Yagi, S.; Akaike, M.; Aihara, K.-I.; Iwase, T.; Yoshida, S.; Sumitomo-Ueda, Y.; Ikeda, Y.; Ishikawa, K.; Matsumoto, T.; Sata, M. High plasma aldosterone concentration is a novel risk factor of cognitive impairment in patients with hypertension. Hypertens. Res. 2011, 34, 74–78. [Google Scholar] [CrossRef] [PubMed]
- Walker, K.A.; Power, M.C.; Gottesman, R.F. Defining the relationship between hypertension, cognitive decline, and dementia: A review. Curr. Hypertens. Rep. 2017, 19, 24. [Google Scholar] [PubMed]
- Wysocki, M.; Luo, X.; Schmeidler, J.; Dahlman, K.; Lesser, G.T.; Grossman, H.; Haroutunian, V.; Beeri, M.S. Hypertension is associated with cognitive decline in elderly people at high risk for dementia. Am. J. Geriatr. Psychiatry 2012, 20, 179–187. [Google Scholar] [CrossRef]
- Adams, A.M.; Vuckovic, M.; Graul, E.; Rashid, S.F.; Sarker, M. Supporting the role and enabling the potential of community health workers in Bangladesh’s rural maternal and newborn health programs: A qualitative study. J. Glob. Health Rep. 2020, 4, e2020029. [Google Scholar] [CrossRef]
- Mistry, S.K.; Harris-Roxas, B.; Yadav, U.N.; Shabnam, S.; Rawal, L.B.; Harris, M.F. Community health workers can provide psychosocial support to the people during COVID-19 and beyond in Low-and Middle-Income Countries. Front. Public Health 2021, 9, 666753. [Google Scholar] [CrossRef]
- Volkmer, I. Social Media and COVID-19: A Global Study of Digital Crisis Interaction among Gen Z and Millennials; WHO: Geneva, Switzerland, 2021. [Google Scholar]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).