Effects of Parental Migration on Dental Caries of Six- to Eight-Year-Old Children Using Structural Equation Modeling
Abstract
1. Introduction
2. Materials and Methods
2.1. Study Design and Setting
2.2. Sampling Technique
2.3. Sample Sizes
2.4. Data Collection
2.5. Variables
2.6. Statistical Analysis
2.6.1. Data Management
2.6.2. Descriptive and Univariate Statistics
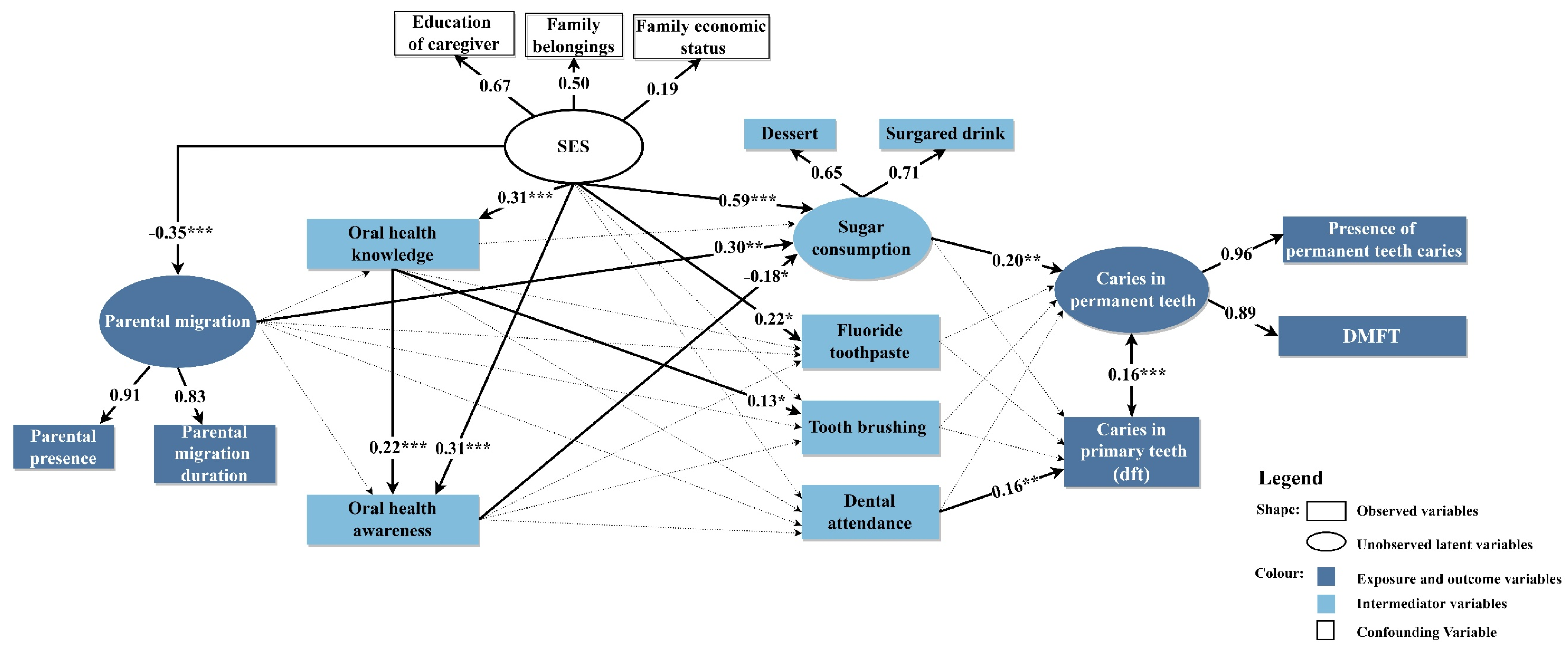
2.6.3. Structural Equation Modeling (SEM)
2.7. Ethics Statement
3. Results
4. Discussion
5. Conclusions
Supplementary Materials
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- National Bureau of Statistics of China (NBSC). Major Figures on 2020 Population Census of China; China Statistics Press: Beijing, China, 2020.
- United Nations Children’s Fund (UNICEF). Children “Left Behind”; United Nations Children’s Fund: New York, NY, USA, 2020. [Google Scholar]
- United Nations Children’s Fund (UNICEF); National Working Committee on Children and Women (NWCCW); National Bureau of Statistics of China (NBSC). Children in China: An Atlas of Social Indicators; United Nations Children’s Fund: Beijing, China, 2018.
- United Nations Educational Scientific and Cultural Organization (UNESCO) Bangkok. Policy Briefs on Internal Migration in Southeast Asia; United Nations Educational Scientific and Cultural Organization: Bangkok, Thailand, 2018. [Google Scholar]
- Fellmeth, G.; Rose-Clarke, K.; Zhao, C.; Busert, L.K.; Zheng, Y.; Massazza, A.; Sonmez, H.; Eder, B.; Blewitt, A.; Lertgrai, W.; et al. Health impacts of parental migration on left-behind children and adolescents: A systematic review and meta-analysis. Lancet 2018, 392, 2567–2582. [Google Scholar] [CrossRef]
- Shi, H.; Wang, Y.; Li, M.; Tan, C.; Zhao, C.; Huang, X.; Dou, Y.; Duan, X.; Du, Y.; Wu, T.; et al. Impact of parent-child separation on children’s social-emotional development: A cross-sectional study of left-behind children in poor rural areas of China. BMC Public Health 2021, 21, 823. [Google Scholar] [CrossRef] [PubMed]
- Wang, Q.; Liu, X. Peer victimization and nonsuicidal self-injury among Chinese left-behind children: The moderating roles of subjective socioeconomic status and social support. J. Interpers. Violence 2021, 36, 11165–11187. [Google Scholar] [CrossRef] [PubMed]
- Yang, Y.; Zheng, C.; Xie, M.; Yuan, S.; Zeng, Y.; Zhou, M.; Huang, S.; Zhu, Y.; Ye, X.; Zou, Z.; et al. Bullying victimization and life satisfaction among rural left-behind children in China: A cross-sectional study. Front. Pediatr. 2021, 9, 671543. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.; Yang, S.; Liao, Z.; Xu, L.; Li, C.; Zeng, H.; Song, J.; Zhang, L. Prevalence and care index of early childhood caries in mainland China: Evidence from epidemiological surveys during 1987-2013. Sci. Rep. 2016, 6, 18897. [Google Scholar] [CrossRef]
- Du, M.Q.; Li, Z.; Jiang, H.; Wang, X.; Feng, X.P.; Hu, Y.; Lin, H.C.; Wang, B.; Si, Y.; Wang, C.X.; et al. Dental caries status and its associated factors among 3- to 5-year-old children in China: A national survey. Chin. J. Dent. Res. Off. J. Sci. Sect. Chin. Stomatol. Assoc. 2018, 21, 167–179. [Google Scholar]
- Ji, Y.L.; Wang, Z.G.; Yang, B.S.; Sun, J.; He, J. Survey of oral health knowledge and habits of twelve years old left-behind children in Henan province countryside. Chin. J. Sch. Health 2015, 23, 1185–1187. [Google Scholar]
- Huang, Y.L.; Feng, X.; Zhang, W.L.; Han, W.Q.; Zhang, Y.H. Oral health knowledge and behavior of rural left-behind children in Henan province. Chin. Sch. Health 2011, 32, 77–78. [Google Scholar]
- Ji, Y.L.; Wang, Z.G.; Sun, J.; He, J. Oral health knowledge attitude and behavior among six-year-old left-behind rural children in Henan Province. Chin. J. Sch. Health 2015, 36, 844–846, 850. [Google Scholar]
- Ji, Y.L.; Wang, Z.G.; Yang, D.S.; Sun, J.; He, J. Analysis of the causes of permanent teeth and its influencing factors in 12-year-old children left behind in rural areas of Henan Province. Chin. Sch. Health 2015, 36, 1906–1908. [Google Scholar]
- Gan, M.F.; Gu, J.L.; Ye, C.; Tan, Z.B. Analysis on the status of caries among 12-year-old left-behind children and non-left-behind children in Guigang City, Guangxi. Guangxi Med. J. 2017, 39, 1750–1751. [Google Scholar]
- Qiu, R.; Li, Y.; Malla, M.; Yao, J.; Mo, D.; Dhakal, N.; Huang, H. Impact of parental migration on oral health outcomes of left-behind school-aged children in Luchuan, southern China. BMC Oral Health 2018, 18, 207. [Google Scholar] [CrossRef] [PubMed]
- FDI World Dental Federation. The challenge of oral disease—A call for global action. In The Oral Health Atlas, 2nd ed.; FDI World Dental Federation: Geneva, Switzerland, 2015. [Google Scholar]
- Qiu, R.M.; Lo, E.C.; Zhi, Q.H.; Zhou, Y.; Tao, Y.; Lin, H.C. Factors related to children’s caries: A structural equation modeling approach. BMC Public Health 2014, 14, 1071. [Google Scholar] [CrossRef] [PubMed]
- Qin, Y.; Zhang, R.; Yuan, B.; Xu, T.; Chen, H.; Yang, Y.; Hu, T. Structural equation modelling for associated factors with dental caries among 3-5-year-old children: A cross-sectional study. BMC Oral Health 2019, 19, 102. [Google Scholar] [CrossRef]
- Zhang, Y.; Li, K.Y.; Lo, E.C.M.; Wong, M.C.M. Structural equation model for parental influence on children’s oral health practice and status. BMC Oral Health 2020, 20, 56. [Google Scholar] [CrossRef]
- People’s Government of Qujing. Qujing Yearbook; Yunnan People’s Publishing House: Yunnan, China, 2018.
- Statistical Bureau of Zhanyi. Zhanyi Yearbook; Yunnan Publishing Group: Yunnan, China, 2021. [Google Scholar]
- Statistical Bureau of Huize. Huize Yearbook; Yunnan Publishing Group: Yunnan, China, 2021. [Google Scholar]
- Statistical Bureau of Xuanwei. Xuanwei Yearbook; Yunnan Publishing Group: Yunnan, China, 2021. [Google Scholar]
- Statistical Bureau of Yunnan Province. 2021 Yunnan Survey Yearbook, 1st ed.; Statistical Publishing House: Beijing, China, 2022. [Google Scholar]
- Cheng, M.L.; Xu, M.R.; Xie, Y.Y.; Gao, X.L.; Wu, H.J.; Wang, X.; Feng, X.P.; Tai, B.J.; Hu, Y.; Lin, H.C.; et al. Utilisation of oral health services and economic burden of oral diseases in China. Chin. J. Dent. Res. Off. J. Sci. Sect. Chin. Stomatol. Assoc. 2018, 21, 275–284. [Google Scholar]
- Zou, X.C.; Zhang, W.; Qian, Q.W.; Zhang, R.H.; Liu, J. Survey of dental service ability in Yunnan province. J. Kunming Med. Univ. 2016, 37, 35–40. [Google Scholar]
- Yuan, C.; Wang, X.Z.; Sun, X.Y.; Wang, X.; Feng, X.P.; Tai, B.J.; Hu, Y.; Lin, H.C.; Wang, B.; Si, Y.; et al. Oral Health Status of 12-year-olds from Regions with and without Coverage of the National Oral Health Comprehensive Intervention Program for Children in China. Chin. J. Dent. Res. Off. J. Sci. Sect. Chin. Stomatol. Assoc. 2018, 21, 299–306. [Google Scholar]
- People’s Government of Qujing. Qujing Yearbook; Yunnan People’s Publishing House: Yunnan, China, 2020.
- Kline, R.B. Principles and Practice of Structural Equation Modeling, 4th ed.; The Guilford Press: New York, NY, USA, 2015. [Google Scholar]
- World Health Organization (WHO). Oral Health Surveys: Basic Methods, 5th ed.; World Health Organization: Geneva, Switzerland, 2013.
- Quan, J.K.; Wang, X.Z.; Sun, X.Y.; Yuan, C.; Liu, X.N.; Wang, X.; Feng, X.P.; Tai, B.J.; Hu, Y.; Lin, H.C.; et al. Permanent teeth caries status of 12- to 15-year-olds in China: Findings from the 4th national oral health survey. Chin. J. Dent. Res. Off. J. Sci. Sect. Chin. Stomatol. Assoc. 2018, 21, 181–193. [Google Scholar]
- Huang, Y.K.; Chang, Y.C. Oral health: The first step to sustainable development goal 3. J. Formos. Med. Assoc. 2022, 121, 1348–1350. [Google Scholar] [CrossRef]
- Wen, P.Y.F.; Chen, M.X.; Zhong, Y.J.; Dong, Q.Q.; Wong, H.M. Global burden and inequality of dental caries, 1990 to 2019. J. Dent. Res. 2022, 101, 392–399. [Google Scholar] [CrossRef] [PubMed]
- Li, B.; Adab, P.; Cheng, K.K. The role of grandparents in childhood obesity in China—Evidence from a mixed methods study. Int. J. Behav. Nutr. Phys. Act. 2015, 12, 91. [Google Scholar] [CrossRef] [PubMed]
- Morita, A.; Matsuyama, Y.; Isumi, A.; Doi, S.; Ochi, M.; Fujiwara, T. Association between grandparent co-residence, socioeconomic status and dental caries among early school-aged children in Japan: A population-based prospective study. Sci. Rep. 2019, 9, 11345. [Google Scholar] [CrossRef] [PubMed]
- Farrow, C.V.; Haycraft, E.; Blissett, J.M. Teaching our children when to eat: How parental feeding practices inform the development of emotional eating-a longitudinal experimental design. Am. J. Clin. Nutr. 2015, 101, 908–913. [Google Scholar] [CrossRef]
- Braden, A.; Rhee, K.; Peterson, C.B.; Rydell, S.A.; Zucker, N.; Boutelle, K. Associations between child emotional eating and general parenting style, feeding practices, and parent psychopathology. Appetite 2014, 80, 35–40. [Google Scholar] [CrossRef] [PubMed]
- Uerlich, M.F.; Baker, S.R.; Day, P.F.; Brown, L.; Vettore, M.V. Common determinants of dental caries and obesity in children: A multi-ethnic nested birth cohort study in the United Kingdom. Int. J. Environ. Res. Public Health 2021, 18, 12561. [Google Scholar] [CrossRef]
- Marinho, V.C.; Higgins, J.P.; Sheiham, A.; Logan, S. Fluoride toothpastes for preventing dental caries in children and adolescents. Cochrane Database Syst. Rev. 2003, 2003, Cd002278. [Google Scholar] [CrossRef]
| Characteristic | LBC | NLBC | p | |
|---|---|---|---|---|
| Total | 259 (51.8) | 241 (48.2) | ||
| Parental migration durations | <0.001 | |||
| No | - | 191 (79.3) | ||
| <6 months | - | 50 (20.7) | ||
| 6–<12 months | 87 (33.6) | - | ||
| ≥12 months | 172 (66.4) | - | ||
| Parental presence | <0.001 | |||
| Both parents | 0 (0.0) | 191 (79.3) | ||
| Mother | 121 (46.7) | 32 (13.3) | ||
| Father | 18 (6.9) | 1 (0.4) | ||
| Grandparents | 97 (37.5) | 17 (7.1) | ||
| Others | 23 (8.9) | 0 (0.0) | ||
| Age of children | 0.40 | |||
| 6 | 91 (35.1) | 83 (34.4) | ||
| 7 | 132 (51.0) | 114 (47.3) | ||
| 8 | 36 (13.9) | 44 (18.3) | ||
| Sex of children | 0.19 | |||
| Female | 118 (45.6) | 124 (51.5) | ||
| Male | 141 (54.4) | 117 (48.5) | ||
| Age of caregivers | <0.001 | |||
| 11–29 | 31 (12.0) | 39 (16.2) | ||
| 30–49 | 118 (45.6) | 162 (67.2) | ||
| 50–85 | 84 (32.4) | 25 (10.4) | ||
| Sex of caregivers | 0.79 | |||
| Female | 194 (74.9) | 178 (73.9) | ||
| Male | 65 (25.1) | 63 (26.1) | ||
| Education level of caregivers | <0.001 | |||
| University | 2 (0.8) | 10 (4.1) | ||
| High school | 19 (7.3) | 40 (16.6) | ||
| Junior high school | 92 (35.5) | 85 (35.3) | ||
| Primary school | 95 (36.7) | 84 (34.9) | ||
| No formal schooling | 51 (19.7) | 22 (9.1) | ||
| Occupations of caregivers | 0.03 | |||
| Officials | 1 (0.4) | 8 (3.3) | ||
| Business owners | 37 (14.3) | 49 (20.3) | ||
| Farmers | 95 (36.7) | 81 (33.6) | ||
| Stay-at-home | 119 (45.9) | 99 (41.1) | ||
| Others | 7 (2.7) | 4 (1.7) | ||
| Variables | Parental Migration Durations (Months) | p | ||||
|---|---|---|---|---|---|---|
| No | <6 | 6–<12 | ≥12 | |||
| (n = 191) | (n = 50) | (n = 87) | (n = 172) | |||
| Frequency of sugar consumption in children | 0.44 | |||||
| Few/never | 83 (44.6) | 23 (46.0) | 34 (40.0) | 63 (36.8) | ||
| Once a day | 36 (19.4) | 7 (14.0) | 23 (27.1) | 42 (24.6) | ||
| Twice or more | 67 (36.0) | 20 (40.0) | 28 (32.9) | 66 (38.6) | ||
| Frequency of brushing in children | 0.02 | |||||
| Twice or more | 58 (31.4) | 19 (38.0) | 15 (17.2) | 59 (34.5) | ||
| Less than twice | 127 (68.6) | 31 (62.0) | 72 (82.8) | 112 (65.5) | ||
| Fluoride toothpaste used by children | 0.05 | |||||
| Yes | 88 (51.5) | 17 (38.6) | 29 (41.4) | 80 (54.4) | ||
| No * | 48 (28.1) | 11 (25.0) | 15 (21.4) | 37 (25.2) | ||
| Don’t know | 35 (20.5) | 16 (36.4) | 26 (37.1) | 30 (20.4) | ||
| Dental attendance of children in the past year | 0.27 | |||||
| Yes ** | 119 (62.3) | 25 (50.0) | 47 (54.0) | 94 (54.7) | ||
| No | 72 (37.7) | 25 (50.0) | 40 (46.0) | 78 (45.3) | ||
| Variables | Parental Migration Durations (Months) | p | ||||
|---|---|---|---|---|---|---|
| No | <6 | 6–<12 | ≥12 | |||
| (n = 191) | (n = 50) | (n = 87) | (n = 172) | |||
| Prevalence of caries, % * | ||||||
| Caries in permeant teeth | 30.89 | 20.00 | 28.74 | 19.77 | 0.03 | |
| Caries in primary teeth | 94.24 | 94.00 | 95.40 | 91.86 | 0.43 | |
| Total caries | 94.76 | 94.00 | 95.40 | 91.86 | 0.31 | |
| Number of caries, mean ** | ||||||
| Caries in permeant teeth (DMFT) | 0.68 | 0.38 | 0.55 | 0.39 | 0.39 | |
| Caries in primary teeth (dft) | 6.90 | 7.24 | 7.03 | 6.85 | 0.95 | |
| Total caries (DMFT + dft) | 7.58 | 7.62 | 7.59 | 7.24 | 0.88 | |
| Fit Index | Recommend Levels | This Model |
|---|---|---|
| χ2/df | <5.00 | 1.28 |
| RMSEA | <0.08 | 0.03 |
| SRMR | <0.08 | 0.04 |
| GFI | >0.90 | 0.99 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Liu, S.; Chongsuvivatwong, V.; Zhang, S.; Thearmontree, A. Effects of Parental Migration on Dental Caries of Six- to Eight-Year-Old Children Using Structural Equation Modeling. Int. J. Environ. Res. Public Health 2022, 19, 13470. https://doi.org/10.3390/ijerph192013470
Liu S, Chongsuvivatwong V, Zhang S, Thearmontree A. Effects of Parental Migration on Dental Caries of Six- to Eight-Year-Old Children Using Structural Equation Modeling. International Journal of Environmental Research and Public Health. 2022; 19(20):13470. https://doi.org/10.3390/ijerph192013470
Chicago/Turabian StyleLiu, Sichen, Virasakdi Chongsuvivatwong, Shinan Zhang, and Angkana Thearmontree. 2022. "Effects of Parental Migration on Dental Caries of Six- to Eight-Year-Old Children Using Structural Equation Modeling" International Journal of Environmental Research and Public Health 19, no. 20: 13470. https://doi.org/10.3390/ijerph192013470
APA StyleLiu, S., Chongsuvivatwong, V., Zhang, S., & Thearmontree, A. (2022). Effects of Parental Migration on Dental Caries of Six- to Eight-Year-Old Children Using Structural Equation Modeling. International Journal of Environmental Research and Public Health, 19(20), 13470. https://doi.org/10.3390/ijerph192013470







