Assessing Loneliness among Adults Receiving Outpatient Treatment with Medication for Opioid Use Disorder (MOUD)
Abstract
1. Introduction
Rurality, Loneliness, and SUD
2. Materials and Methods
Measures
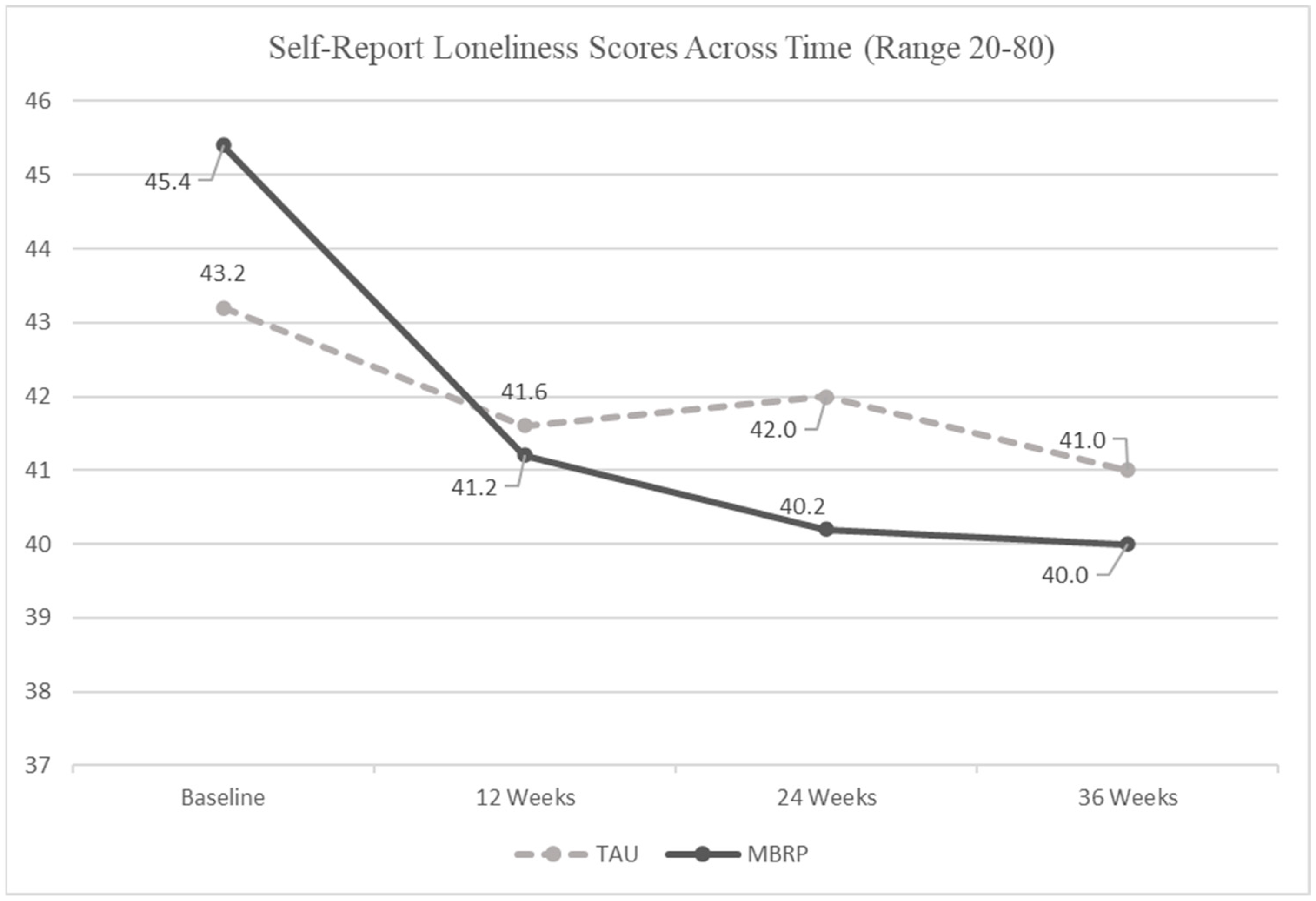
3. Results
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Grant, B.F.; Saha, T.D.; Ruan, W.J.; Goldstein, R.B.; Chou, S.P.; Jung, J.; Hasin, D.S. Epidemiology of DSM-5 drug use disorder: Results from the National Epidemiologic Survey on Alcohol and Related Conditions—III. JAMA Psychiatry 2016, 73, 39–47. [Google Scholar] [CrossRef] [PubMed]
- McCabe, S.E.; West, B.T.; Jutkiewicz, E.M.; Boyd, C.J. Multiple DSM-5 substance use disorders: A national study of US adults. Hum. Psychopharmacol. Clin. Experimental 2017, 32, e2625. [Google Scholar] [CrossRef] [PubMed]
- National Center for Drug Abuse Statistics. Drug Abuse Statistics. 2022. Available online: https://drugabusestatistics.org/ (accessed on 29 May 2022).
- National Center for Health Statistics. U.S. Overdose Deaths in 2021 Increased Half as Much as in 2020—But Are Still Up 15%. 2022. Available online: https://www.cdc.gov/nchs/pressroom/nchs_press_releases/2022/202205.htm (accessed on 29 May 2022).
- Jones, C.M.; McCance-Katz, E.F. Co-occurring substance use and mental disorders among adults with opioid use disorder. Drug Alcohol Depend. 2019, 197, 78–82. [Google Scholar] [CrossRef] [PubMed]
- Davis, M.A.; Lin, L.A.; Liu, H.; Sites, B.D. Prescription opioid use among adults with mental health disorders in the United States. J. Am. Board Fam. Med. 2017, 30, 407–417. [Google Scholar] [CrossRef]
- Kelly, T.M.; Daley, D.C. Integrated treatment of substance use and psychiatric disorders. Soc. Work Public Health 2013, 28, 388–406. [Google Scholar] [CrossRef] [PubMed]
- Ross, S.; Peselow, E. Co-Occurring Psychotic and Addictive Disorders. Clin. Neuropharmacol. 2012, 35, 235–243. [Google Scholar] [CrossRef]
- Kelly, D.; Steiner, A.; Mazzei, M.; Baker, R. Filling a void? The role of social enterprise in addressing social isolation and loneliness in rural communities. J. Rural. Stud. 2019, 70, 225–236. [Google Scholar] [CrossRef]
- Luo, Y.; Hawkley, L.C.; Waite, L.J.; Cacioppo, J.T. Loneliness, health, and mortality in old age: A national longitudinal study. Soc. Sci. Med. 2012, 74, 907–914. [Google Scholar] [CrossRef]
- Tremeau, F.; Antonius, D.; Malaspina, D.; Goff, D.C.; Javitt, D.C. Loneliness in schizophrenia and its possible correlates. An exploratory study. Psychiatry Res. 2016, 246, 211–217. [Google Scholar] [CrossRef]
- Horigian, V.E.; Schmidt, R.D.; Feaster, D.J. Loneliness, Mental Health, and Substance Use among US Young Adults during COVID-19. J. Psychoact. Drugs 2020, 53, 1–9. [Google Scholar] [CrossRef]
- Ingram, I.; Kelly, P.J.; Deane, F.P.; Baker, A.L.; Goh, M.C.W.; Raftery, D.K.; Dingle, G.A. Loneliness among people with substance use problems: A narrative systematic review. Drug Alcohol. Rev. 2020, 39, 447–483. [Google Scholar] [CrossRef]
- Stickley, A.; Koyanagi, A.; Koposov, R.; Schwab-Stone, M.; Ruchkin, V. Loneliness and health risk behaviours among Russian and U.S. adolescents: A cross-sectional study. BMC Public Health 2014, 14, 366. [Google Scholar] [CrossRef]
- Wootton, R.E.; Greenstone, H.S.R.; Abdellaoui, A.; Denys, D.; Verweij, K.J.H.; Munafò, M.R.; Treur, J.L. Bidirectional effects between loneliness, smoking and alcohol use: Evidence from a Mendelian randomization study. Addiction 2021, 116, 400–406. [Google Scholar] [CrossRef] [PubMed]
- Surkalim, D.L.; Luo, M.; Eres, R.; Gebel, K.; van Buskirk, J.; Bauman, A.; Ding, D. The prevalence of loneliness across 113 countries: Systematic review and meta-analysis. BMJ 2022, 376, e067068. [Google Scholar] [CrossRef]
- DiJulio, B.L.; Hamel, L.; Munana, C.; Brodie, M. Loneliness and Social Isolation in the United States, the United Kingdom, and Japan: An International Survey; Kaiser Family Foundation: San Francisco, CA, USA, 2018; Available online: https://files.kff.org/attachment/Report-Loneliness-and-Social-Isolation-in-the-United-States-the-United-Kingdom-and-Japan-An-International-Survey (accessed on 20 November 2019).
- Kaiser Family Foundation; The Economist. Survey on Loneliness and Social Isolation in the United States, the United Kingdom, and Japan. 2018. Available online: http://files.kff.org/attachment/Topline-Kaiser-Family-Foundation-The-Economist-Survey-on-Loneliness-and-Social-Isolation-in-the-United-States-the-United-Kingdom-and-Japan (accessed on 30 May 2022).
- National Academies of Sciences, Engineering, and Medicine. Social Isolation and Loneliness in Older Adults: Opportunities for the Health Care System; The National Academies Press: Washington, DC, USA, 2020. [Google Scholar] [CrossRef]
- Lee, E.E.; Depp, C.; Palmer, B.W.; Glorioso, D.; Daly, R.; Liu, J.; Jeste, D.V. High prevalence and adverse health effects of loneliness in community-dwelling adults across the lifespan: Role of wisdom as a protective factor. Int. Psychogeriatr. 2019, 31, 1447–1462. [Google Scholar] [CrossRef] [PubMed]
- NIH National Institutes on Aging. Loneliness and Social Isolation—Tips for Staying Connected. National Institutes of Health. 2021. Available online: https://www.nia.nih.gov/health/loneliness-and-social-isolation-tips-staying-connected#:~:text=Loneliness%20is%20the%20distressing%20feeling,while%20being%20with%20other%20people (accessed on 15 May 2021).
- Barg, F.K.; Huss-Ashmore, R.; Wittink, M.N.; Murray, G.F.; Bogner, H.R.; Gallo, J.J. A mixed methods approach to understanding loneliness and depression in older adults. J. Gerontol. Ser. B 2006, 61, S329–S339. [Google Scholar] [CrossRef] [PubMed]
- Theeke, L.A.; Mallow, J. Loneliness and quality of life in chronically ill rural older adults. Am. J. Nurs. 2013, 113, 28–37. [Google Scholar] [CrossRef] [PubMed]
- Petersen, J.; Kaye, J.; Jacobs, P.G.; Quinones, A.; Dodge, H.; Arnold, A.; Thielke, S. Longitudinal relationship between loneliness and social isolation in older adults: Results from the cardiovascular health study. J. Aging Health 2016, 28, 775–795. [Google Scholar] [CrossRef] [PubMed]
- Laudet, A.B.; Magura, S.; Vogel, H.S.; Knight, E.L. Perceived reasons for substance misuse among persons with a psychiatric disorder. Am. J. Orthopsychiatry 2004, 74, 365–375. [Google Scholar] [CrossRef]
- Polenick, C.A.; Cotton, B.P.; Bryson, W.C.; Birditt, K.S. Loneliness and Illicit Opioid Use Among Methadone Maintenance Treatment Patients. Subst. Use Misuse 2019, 54, 2089–2098. [Google Scholar] [CrossRef]
- Vyas, M.V.; Watt, J.A.; Yu, A.Y.; Straus, S.E.; Kapral, M.K. The association between loneliness and medication use in older adults. Age Ageing 2021, 50, 587–591. [Google Scholar] [CrossRef] [PubMed]
- Johnson, J.E.; Schonbrun, Y.C.; Nargiso, J.E.; Kuo, C.C.; Shefner, R.T.; Williams, C.A.; Zlotnick, C. “I know if I drink I won’t feel anything”: Substance use relapse among depressed women leaving prison. Int. J. Prison. Health 2013, 9, 169–186. [Google Scholar] [CrossRef] [PubMed]
- Newton, T.F.; De La Garza, R., 2nd; Kalechstein, A.D.; Tziortzis, D.; Jacobsen, C.A. Theories of addiction: Methamphetamine users’ explanations for continuing drug use and relapse. Am. J. Addict. 2009, 18, 294–300. [Google Scholar] [CrossRef] [PubMed]
- Hosseinbor, M.; Yassini Ardekani, S.M.; Bakhshani, S.; Bakhshani, S. Emotional and social loneliness in individuals with and without substance dependence disorder. Int. J. High Risk Behav. Addict. 2014, 3, e22688. [Google Scholar] [CrossRef]
- Theeke, L.A.; Mallow, J.A.; Moore, J.; McBurney, A.; Rellick, S.; VanGilder, R. Effectiveness of LISTEN on loneliness, neuroimmunological stress response, psychosocial functioning, quality of life, and physical health measures of chronic illness. Int. J. Nurs. Sci. 2016, 3, 242–251. [Google Scholar] [CrossRef]
- Veronese, N.; Galvano, D.; D’Antiga, F. Interventions for reducing loneliness: An umbrella review of intervention studies. Health Soc. Care Community 2021, 29, e89–e96. [Google Scholar] [CrossRef]
- Meit, M.; Heffernan, M.; Tanenbaum, E. Investigating the impact of the diseases of despair in Appalachia. J. Appalach. Health 2019, 1, 7–18. [Google Scholar] [CrossRef]
- Centers for Disease Control and Prevention (CDC). Drug Overdose Mortality by State. 2021. Available online: https://www.cdc.gov/nchs/pressroom/sosmap/drug_poisoning_mortality/drug_poisoning.htm (accessed on 17 September 2021).
- Department of Health and Human Resources (DHHR). West Virginia Experiences Increase in Overdose Deaths; Health Officials Emphasize Resources. 2020. Available online: https://dhhr.wv.gov/News/2021/Pages/West-Virginia-Experiences-Increase-in-Overdose-Deaths;-Health-Officials-Emphasize-Resources.aspx (accessed on 17 September 2021).
- Andrilla, C.H.A.; Moore, T.E.; Patterson, D.G.; Larson, E.H. Geographic distribution of providers with a DEA waiver to prescribe buprenorphine for the treatment of opioid use disorder: A 5-year update. J. Rural. Health 2019, 35, 108–112. [Google Scholar] [CrossRef]
- Henning-Smith, C.; Ecklund, A.; Lahr, M.; Evenson, A.; Moscovice, I.; Kozhimannil, K. Key Informant Perspectives on Rural Social Isolation and Loneliness. University of Minnesota Rural Health Research Center. 2018. Available online: http://rhrc.umn.edu/wp-content/uploads/2019/01/1539002382UMNpolicybriefKeyInformantPerspectivesonRuralSocialIsolationandLoneliness.pdf (accessed on 5 March 2021).
- Savikko, N.; Routasalo, P.; Tilvis, R.S.; Strandberg, T.E.; Pitkälä, K.H. Predictors and subjective causes of loneliness in an aged population. Arch. Gerontol. Geriatr. 2005, 41, 223–233. [Google Scholar] [CrossRef]
- Zullig, K.J.; Lander, L.R.; Tuscano, M.; Garland, M.; Hobbs, G.R.; Faulkenberry, L. Testing Mindfulness-Based Relapse Prevention with medications for opioid use disorder among adults in outpatient therapy: A quasi-experimental study. Mindfulness 2021, 12, 3036–3046. [Google Scholar] [CrossRef]
- Friedman, B.; Conwell, Y.; Delavan, R.L. Correlates of late-life major depression: A comparison of urban and rural primary care patients. Am. J. Geriatr. Psychiatry 2007, 15, 28–41. [Google Scholar] [CrossRef] [PubMed]
- Nkyi, A.K.; Ninnoni, J.P.K. Depression, Purpose in Life, Loneliness and Anxiety Among Patients with Substance Use Disorders in Ankaful Psychiatric Hospital in Ghana. J. Psychosoc. Rehabil. Ment. Health 2020, 7, 263–271. [Google Scholar] [CrossRef]
- Knapp, K.S.; Bunce, S.C.; Brick, T.R.; Deneke, E.; Cleveland, H.H. Daily associations among craving, affect, and social interactions in the lives of patients during residential opioid use disorder treatment. Psychol. Addict. Behav. 2020. Advance online publication. [Google Scholar] [CrossRef] [PubMed]
- Bowen, S.; Witkiewitz, K.; Dillworth, T.M.; Chawla, N.; Simpson, T.L.; Ostafin, B.; Larimer, M.E.; Blume, A.W.; Parks, G.A.; Marlatt, G.A. Mindfulness meditation and substance use in an incarcerated population. Psychol. Addict. Behav. 2006, 20, 343–347. [Google Scholar] [CrossRef] [PubMed]
- Bowen, S.; Witkiewitz, K.; Clifasefi, S.L.; Grow, G.; Chawla, N.; Hsu, S.H.; Carroll, H.A.; Harrop, E.; Collins, S.E.; Lustyk, M.K.; et al. Relative efficacy of mindfulness-based relapse prevention, standard relapse prevention, and treatment as usual for substance use disorders: A randomized clinical trial. JAMA Psychiatry 2014, 71, 547–556. [Google Scholar] [CrossRef]
- Creswell, J.D.; Irwin, M.R.; Burklund, L.J.; Lieberman, M.D.; Arevalo, J.M.; Ma, J.; Cole, S.W. Mindfulness-based stress reduction training reduces loneliness and pro-inflammatory gene expression in older adults: A small randomized controlled trial. Brain Behav. Immun. 2012, 26, 1095–1101. [Google Scholar] [CrossRef]
- Lindsay, E.K.; Young, S.; Brown, K.W.; Smyth, J.M.; Creswell, J.D. Mindfulness training reduces loneliness and increases social contact in a randomized controlled trial. Proc. Natl. Acad. Sci. USA 2019, 116, 3488–3493. [Google Scholar] [CrossRef]
- Teoh, S.L.; Letchumanan, V.; Lee, L.H. Can mindfulness help to alleviate loneliness? A systematic review and meta-analysis. Front. Psychol. 2021, 12, 402. [Google Scholar] [CrossRef]
- Zhang, N.; Fan, F.M.; Huang, S.Y.; Rodriguez, M.A. Mindfulness training for loneliness among Chinese college students: A pilot randomized controlled trial. Int. J. Psychol. 2018, 53, 373–378. [Google Scholar] [CrossRef]
- Hooker, S.A.; Lonergan-Cullum, M.; Levy, R.; Nissly, T.; Sherman, M.D. Longitudinal assessment of mental health and well-being in patients being treated with medications for opioid use disorder in primary care. Addict. Behav. Rep. 2021, 13, 100348. [Google Scholar] [CrossRef]
- Franken, I.H.A.; Hendriks, V.M.; van den Brink, W. Initial validation of two opiate craving questionnaires: The Obsessive Compulsive Drug Use Scale and the Desires for Drug Questionnaire. Addict. Behav. 2002, 27, 675–685. [Google Scholar] [CrossRef]
- Bentley, K.H.; Gallagher, M.W.; Carl, J.R.; Barlow, D.H. Development and validation of the Overall Depression Severity and Impairment Scale. Psychol. Assess. 2014, 26, 815–830. [Google Scholar] [CrossRef] [PubMed]
- Campbell-Sills, L.; Norman, S.B.; Craske, M.G.; Sullivan, G.; Lang, A.J.; Chavira, D.A.; Bystritsky, A.; Sherbourne, C.; Roy-Byrne, P.; Stein, M.B. Validation of a brief measure of anxiety-related severity and impairment: The Overall Anxiety Severity and Impairment Scale (OASIS). J. Affect. Disord. 2009, 112, 92–101. [Google Scholar] [CrossRef]
- Norman, S.B.; Hami Cissell, S.; Means-Christensen, A.J.; Stein, M.B. Development and validation of an overall anxiety severity and impairment scale (OASIS). Depress. Anxiety 2006, 23, 245–249. [Google Scholar] [CrossRef] [PubMed]
- Baer, R.A.; Smith, G.T.; Hopkins, J.; Krietemeyer, J.; Toney, L. Using self-report assessment methods to explore facets of mindfulness. Assessment 2006, 13, 27–45. [Google Scholar] [CrossRef] [PubMed]
- Russell, D. UCLA Loneliness Scale (Version 3): Reliability, validity, and factor structure. J. Personal. Assess. 1996, 66, 20–40. [Google Scholar] [CrossRef]
- Russell, D.W.; Peplau, L.A.; Cutrona, C.E. The revised UCLA Loneliness Scale: Concurrent and discriminant validity evidence. J. Personal. Soc. Psychol. 1980, 39, 472–480. [Google Scholar] [CrossRef]
- Groarke, J.M.; Berry, E.; Graham-Wisener, L.; McKenna-Plumley, P.E.; McGlinchey, E.; Armour, C. Loneliness in the UK during the COVID-19 pandemic: Cross-sectional results from the COVID-19 Psychological Wellbeing Study. PLoS ONE 2020, 15, e0239698. [Google Scholar] [CrossRef]
- Kuwert, P.; Knaevelsrud, C.; Pietrzak, R.H. Loneliness among older veterans in the United States: Results from the National Health and Resilience in Veterans Study. Am. J. Geriatr. Psychiatry 2014, 22, 564–569. [Google Scholar] [CrossRef]
- Wilson, C.; Moulton, B. Loneliness among Older Adults: A National Survey of Adults 45+. Knowledge Networks and Insight Policy Research; AARP: Washington, DC, USA, 2010; Available online: https://assets.aarp.org/rgcenter/general/loneliness_2010.pdf (accessed on 22 March 2022).
- McDonagh, J.; Williams, C.B.; Oldfield, B.J.; Cruz-Jose, D.; Olson, D.P. The Association of Loneliness and Non-prescribed Opioid Use in Patients With Opioid Use Disorder. J. Addict. Med. 2020, 14, 489–493. [Google Scholar] [CrossRef]
- Ingram, I.; Kelly, P.J.; Deane, F.P.; Baker, A.L.; Dingle, G.A. Perceptions of loneliness among people accessing treatment for substance use disorders. Drug Alcohol Rev. 2020, 39, 484–494. [Google Scholar] [CrossRef] [PubMed]
- Center for Substance Abuse Treatment (CSAT). Substance Abuse Treatment: Group Therapy; (Treatment Improvement Protocol (TIP) Series, No. 41) 1 Groups and Substance Abuse Treatment; Substance Abuse and Mental Health Services Administration: Rockville, MD, USA, 2005. Available online: https://www.ncbi.nlm.nih.gov/books/NBK64223/ (accessed on 26 November 2021).
- Dziedzic, B.; Sarwa, P.; Kobos, E.; Sienkiewicz, Z.; Idzik, A.; Wysokiński, M.; Fidecki, W. Loneliness and Depression among Polish High-School Students. Int. J. Environ. Res. Public Health 2021, 18, 1706. [Google Scholar] [CrossRef] [PubMed]
- Erzen, E.; Çikrikci, Ö. The effect of loneliness on depression: A meta-analysis. Int. J. Soc. Psychiatry 2018, 64, 427–435. [Google Scholar] [CrossRef] [PubMed]
- Chen, X.; Qiu, N.; Zhai, L.; Ren, G. Anxiety, Loneliness, Drug Craving, and Depression Among Substance Abusers in Sichuan Province, China. Front. Pharmacol. 2021, 12, 623360. [Google Scholar] [CrossRef]
- Volkow, N.D. Collision of the COVID-19 and addiction epidemics. Ann. Intern. Med. 2020, 173, 61–62. [Google Scholar] [CrossRef]

| Demographic | TAU (n = 45) | MBRP (n = 35) | Total | p-Value |
|---|---|---|---|---|
| Marital Status | 0.63 | |||
| Single | 28 (60.9%) | 18 (39.1%) | 46 | |
| Married | 8 (50.0%) | 8 (50.0%) | 16 | |
| Divorced or Separating | 9 (50.0%) | 9 (50.0%) | 18 | |
| Sex | 0.12 | |||
| Male | 24 (64.9%) | 13 (35.1%) | 37 | |
| Female | 21 (51.2%) | 20 (48.9%) | 41 | |
| Other | 0 (0.0%) | 2 (100.0%) | 2 | |
| Race | n/a | |||
| White | 45 (56.3%) | 35 (43.8%) | 80 | |
| Employment | 0.95 | |||
| Full Time | 18 (58.1%) | 13 (41.9%) | 31 | |
| Part Time | 8 (53.3%) | 7 (46.7%) | 15 | |
| Unemployed | 19 (55.9%) | 15 (44.1%) | 34 | |
| Education | 0.10 | |||
| Did Not Finish High School | 3 (37.5%) | 5 (62.5%) | 8 | |
| High School Graduate/GED | 30 (66.7%) | 15 (33/3%) | 45 | |
| Some College or Greater | 11 (40.1%) | 16 (59.3%) | 27 | |
| Insurance | 0.59 | |||
| Medicaid | 34 (52.3%) | 31 (47.8%) | 65 | |
| Medicare | 3 (0.6%) | 2 (0.4%) | 5 | |
| Private | 7 (70.0%) | 3 (30.0%) | 10 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Mills, R.; Zullig, K.J.; Theeke, L.A.; Lander, L.R.; Hobbs, G.R.; Herczyk, J.; Davis, S.M. Assessing Loneliness among Adults Receiving Outpatient Treatment with Medication for Opioid Use Disorder (MOUD). Int. J. Environ. Res. Public Health 2022, 19, 13481. https://doi.org/10.3390/ijerph192013481
Mills R, Zullig KJ, Theeke LA, Lander LR, Hobbs GR, Herczyk J, Davis SM. Assessing Loneliness among Adults Receiving Outpatient Treatment with Medication for Opioid Use Disorder (MOUD). International Journal of Environmental Research and Public Health. 2022; 19(20):13481. https://doi.org/10.3390/ijerph192013481
Chicago/Turabian StyleMills, Rosalina, Keith J. Zullig, Laurie A. Theeke, Laura R. Lander, Gerry R. Hobbs, Johnathan Herczyk, and Stephen M. Davis. 2022. "Assessing Loneliness among Adults Receiving Outpatient Treatment with Medication for Opioid Use Disorder (MOUD)" International Journal of Environmental Research and Public Health 19, no. 20: 13481. https://doi.org/10.3390/ijerph192013481
APA StyleMills, R., Zullig, K. J., Theeke, L. A., Lander, L. R., Hobbs, G. R., Herczyk, J., & Davis, S. M. (2022). Assessing Loneliness among Adults Receiving Outpatient Treatment with Medication for Opioid Use Disorder (MOUD). International Journal of Environmental Research and Public Health, 19(20), 13481. https://doi.org/10.3390/ijerph192013481







