Reduction of Multidrug-Resistant (MDR) Bacterial Infections during the COVID-19 Pandemic: A Retrospective Study
Abstract
1. Introduction
2. Methods
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Klevens, R.M.; Edwards, J.R.; Richards, C.L., Jr.; Horan, T.C.; Gaynes, R.P.; Pollock, D.A.; Cardo, D.M. Estimating health care-associated infections and deaths in U.S. hospitals, 2002. Public Health Rep. 2007, 122, 160–166. [Google Scholar] [CrossRef] [PubMed]
- Hospital-Acquired Infection (HAI) Diagnostics Market is Forecasted to Reach $4,386.6 Million by 2023, Growing at a CAGR of 7.6% During 2017–2023, P&S Intelligence. Available online: https://www.psmarketresearch.com/market-analysis/hospital-acquired-infection-diagnostics-market (accessed on 19 December 2020).
- Chan, M. Antimicrobial Resistance. Available online: https://www.who.int/news-room/fact-sheets/detail/antimicrobial-resistance (accessed on 19 December 2020).
- Pratt, R.J.; Pellowe, C.; Loveday, H.P.; Robinson, N.; Smith, G.W.; Barrett, S.; Davey, P.; Harper, P.; Loveday, C.; McDougall, C.; et al. Department of Health (England). The epic project: Developing national evidence-based guidelines for preventing healthcare associated infections. Phase I: Guidelines for preventing hospital-acquired infections. Department of Health (England). J. Hosp. Infect. 2001, 47, S3–S82. [Google Scholar] [CrossRef] [PubMed]
- Kwon, J.H.; Burnham, C.D.; Reske, K.A.; Liang, S.Y.; Hink, T.; Wallace, M.A.; Shupe, A.; Seiler, S.; Cass, C.; Fraser, V.J.; et al. Assessment of healthcare worker protocol deviations and self-contamination during personal protective equipment donning and doffing. Infect. Control. Hosp. Epidemiol. 2017, 38, 1077–1083. [Google Scholar] [CrossRef] [PubMed]
- Takagi, G.; Yagishita, K. Principles of disinfectant use and safety operation in medical facilities during coronavirus disease 2019 (COVID-19) outbreak. SN Compr. Clin. Med. 2020, 18, 1–4. [Google Scholar] [CrossRef] [PubMed] [PubMed Central]
- Zhu, N.; Zhang, D.; Wang, W.; Li, X.; Yang, B.; Song, J.; Zhao, X.; Huang, B.; Shi, W.; Lu, R.; et al. A novel Coronavirus from patients with Pneumonia in China, 2019. China novel Coronavirus investigating and research team. N. Engl. J. Med. 2020, 382, 727–733. [Google Scholar] [CrossRef] [PubMed]
- Available online: https://github.com/CSSEGISandData/COVID-19 (accessed on 19 December 2020).
- Martelletti, L.; Martelletti, P. Air pollution and the novel Covid-19 disease: A putative disease risk factor. SN Compr. Clin. Med. 2020, 1–5. [Google Scholar] [CrossRef] [PubMed]
- Wee, L.E.; Sim, X.Y.J.; Conceicao, E.P.; Aung, M.K.; Goh, J.Q.; Yeo, D.W.T.; Gan, W.H.; Chua, Y.Y.; Wijaya, L.; Tan, T.T.; et al. Containment of COVID-19 cases among healthcare workers: The role of surveillance, early detection, and outbreak management. Infect. Control. Hosp. Epidemiol. 2020, 41, 765–771. [Google Scholar] [CrossRef] [PubMed]
- Wee, L.E.; Hsieh, J.Y.C.; Phua, G.C.; Tan, Y.; Conceicao, E.P.; Wijaya, L.; Tan, T.T.; Tan, B.H. Respiratory surveillance wards as a strategy to reduce nosocomial transmission of COVID-19 through early detection: The experience of a tertiary-care hospital in Singapore. Infect. Control. Hosp. Epidemiol. 2020, 41, 820–825. [Google Scholar] [CrossRef] [PubMed]
- Magiorakos, A.P.; Srinivasan, A.; Carey, R.B.; Carmeli, Y.; Falagas, M.E.; Giske, C.G.; Harbarth, S.; Hindler, J.F.; Kahlmeter, G.; Olsson-Liljequist, B.; et al. Multidrug-resistant, extensively drug-resistant and pandrug-resistant bacteria: An international expert proposal for interim standard definitions for acquired resistance. Clin. Microbiol. Infect. 2012, 18, 268–281. [Google Scholar] [CrossRef] [PubMed]
- Yap, F.H.; Gomersall, C.D.; Fung, K.S.; Ho, P.L.; Ho, O.M.; Lam, P.K.; Lam, D.T.; Lyon, D.J.; Joynt, G.M. Increase in methicillin-resistant Staphylococcus aureus acquisition rate and change in pathogen pattern associated with an outbreak of severe acute respiratory syndrome. Clin. Infect. Dis. 2004, 39, 511–516. [Google Scholar] [CrossRef] [PubMed]
- Wee, L.E.I.; Conceicao, E.P.; Tan, J.Y.; Magesparan, K.D.; Amin, I.B.M.; Ismail, B.B.S.; Toh, H.X.; Jin, P.; Zhang, J.; Wee, E.G.L.; et al. Unintended consequences of infection prevention and control measures during COVID-19 pandemic. Am. J. Infect. Control 2020. [Google Scholar] [CrossRef] [PubMed]
- Bentivegna, E.; Alessio, G.; Spuntarelli, V.; Luciani, M.; Santino, I.; Simmaco, M.; Martelletti, P. Impact of COVID-19 prevention measures on risk of health care-associated Clostridium difficile infection. Am. J. Infect. Control 2020. [Google Scholar] [CrossRef] [PubMed]
- Ponce-Alonso, M.; Sáez de la Fuente, J.; Rincón-Carlavilla, A.; Moreno-Nunez, P.; Martínez-García, L.; Escudero-Sánchez, R.; Pintor, R.; García-Fernández, S.; Cobo, J. Impact of the coronavirus disease 2019 (COVID-19) pandemic on nosocomial Clostridioides difficile infection. Infect. Control Hosp. Epidemiol. 2020, 1–5. [Google Scholar] [CrossRef] [PubMed]
- Liew, Y.; Lee, W.H.L.; Tan, L.; Kwa, A.L.H.; Thien, S.Y.; Cherng, B.P.Z.; Chung, S.J. Antimicrobial stewardship programme: A vital resource for hospitals during the global outbreak of coronavirus disease 2019 (COVID-19). Int. J. Antimicrob. Agents 2020, 56, 106145. [Google Scholar] [CrossRef] [PubMed]
- Luciani, M.; Bentivegna, E.; Spuntarelli, V.; Amoriello Lamberti, P.; Guerritore, L.; Chiappino, D.; Nalli, G.; Proietta, M.; Del Porto, F.; Martelletti, P.; et al. Coinfection of tuberculosis pneumonia and COVID-19 in a patient vaccinated with Bacille Calmette-Guérin (BCG): Case report. SN Compr. Clin. Med. 2020, 1–4. [Google Scholar] [CrossRef] [PubMed]
- Bentivegna, E.; Luciani, M.; Spuntarelli, V.; Speranza, M.L.; Guerritore, L.; Sentimentale, A.; Martelletti, P. Extremely severe case of COVID-19 Pneumonia recovered despite bad prognostic indicators: A didactic report. SN Compr. Clin. Med. 2020, 1–4. [Google Scholar] [CrossRef] [PubMed]
- Bentivegna, E.; Sentimentale, A.; Luciani, M.; Speranza, M.L.; Guerritore, L.; Martelletti, P. New IgM seroconversion and positive RT-PCR test after exposure to the virus in recovered COVID-19 patient. J. Med. Virol. 2020. [Google Scholar] [CrossRef] [PubMed]
- Luciani, M.; Bentivegna, E.; Spuntarelli, V.; Lamberti, P.A.; Cacioli, G.; del Porto, F.; Sesti, G.; Martelletti, P.; de Biase, L. Recurrent COVID-19 pneumonia in the course of chemotherapy: Consequence of a weakened immune system? J. Med. Virol. 2020. [Google Scholar] [CrossRef] [PubMed]
- Louh, I.K.; Greendyke, W.G.; Hermann, E.A.; Davidson, K.W.; Falzon, L.; Vawdrey, D.K.; Ting, H.H. Clostridium difficile infection in acute care hospitals: Systematic review and best practices for prevention. Infect. Control Hosp. Epidemiol. 2017, 38, 476–482. [Google Scholar] [CrossRef] [PubMed]
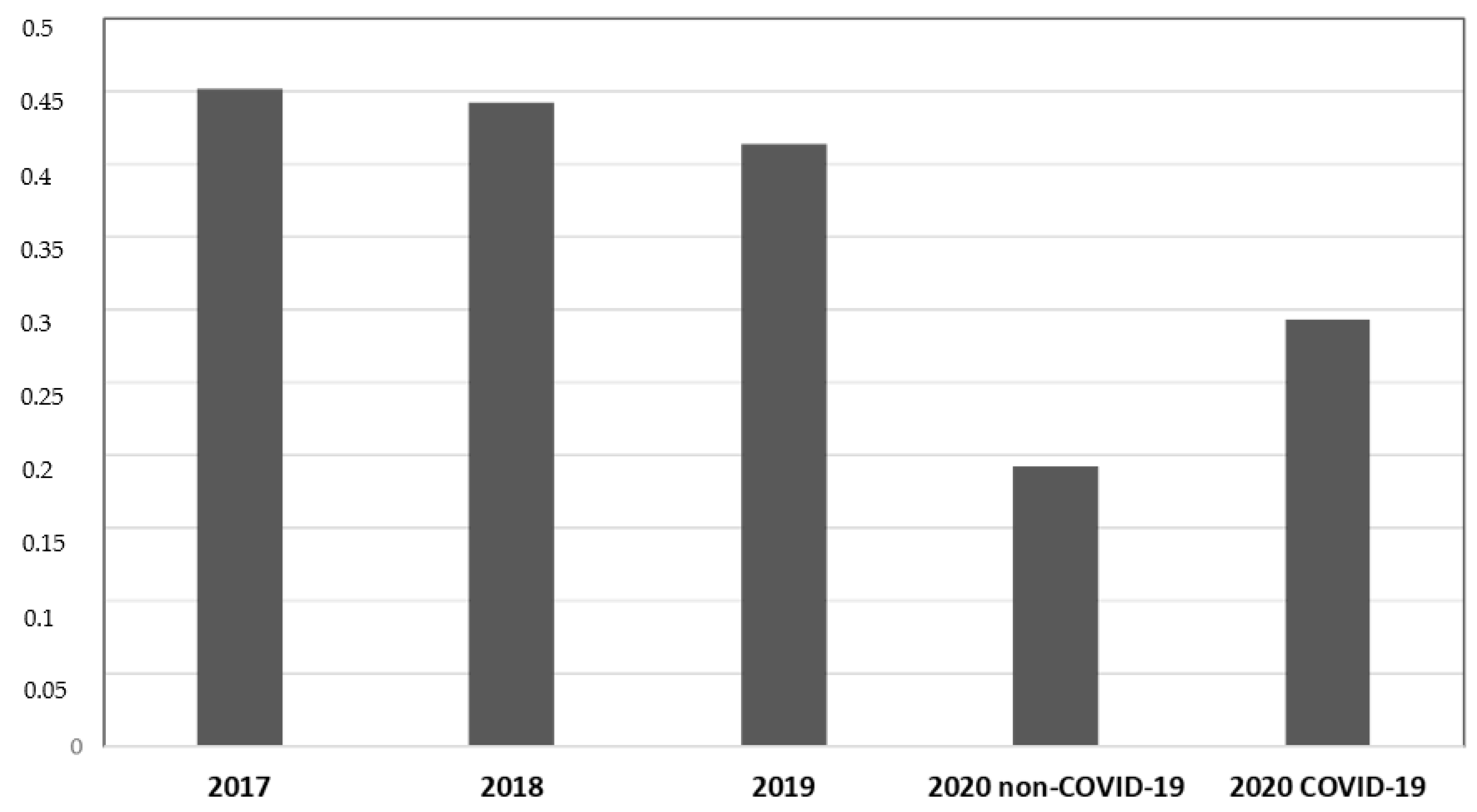

| Year | P # 2017 | P # 2018 | P # 2019 | P # 2020 Non-COVID-19 | P # 2020 COVID-19 |
|---|---|---|---|---|---|
| Discharges | 422 | 348 | 364 | 333 | 150 |
| Staphylococcus aureus | 7.7% | 13.8% | 15.4% | 4.2% * | 5.3% |
| Klebsiella pneumoniae | 12% | 6.6% | 9% | 4.8% * | 10.6% |
| Clostridium difficile | 9.2% | 7.2% | 6.6% | 3.3% * | 4.7% |
| Acinetobacter baumannii | 6.1% | 8% | 4.7% | 3% * | 5.3% |
| Escherichia coli | 0.4% | 0.6% | 0.3% | 0.3% | 0% |
| Enterococcus faecium | 2.4% | 2.6% | 2.7% | 2.7% | 2% |
| Pseudomonas aeruginosa | 1.2% | 3.4% | 2.2% | 0.6% | 1.3% |
| Enterococcus Faecalis | 0.7% | 1.4% | 0.3% | 0.3% | 0% |
| Stenotrophomonas maltophilia | 0% | 0.6% | 0% | 0% | 0% |
| Klebsiella variicola | 0% | 0% | 0.3% | 0% | 0% |
| Total | 45.2% | 44.2% | 41.4% | 19.2% * | 29.2% |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bentivegna, E.; Luciani, M.; Arcari, L.; Santino, I.; Simmaco, M.; Martelletti, P. Reduction of Multidrug-Resistant (MDR) Bacterial Infections during the COVID-19 Pandemic: A Retrospective Study. Int. J. Environ. Res. Public Health 2021, 18, 1003. https://doi.org/10.3390/ijerph18031003
Bentivegna E, Luciani M, Arcari L, Santino I, Simmaco M, Martelletti P. Reduction of Multidrug-Resistant (MDR) Bacterial Infections during the COVID-19 Pandemic: A Retrospective Study. International Journal of Environmental Research and Public Health. 2021; 18(3):1003. https://doi.org/10.3390/ijerph18031003
Chicago/Turabian StyleBentivegna, Enrico, Michelangelo Luciani, Luca Arcari, Iolanda Santino, Maurizio Simmaco, and Paolo Martelletti. 2021. "Reduction of Multidrug-Resistant (MDR) Bacterial Infections during the COVID-19 Pandemic: A Retrospective Study" International Journal of Environmental Research and Public Health 18, no. 3: 1003. https://doi.org/10.3390/ijerph18031003
APA StyleBentivegna, E., Luciani, M., Arcari, L., Santino, I., Simmaco, M., & Martelletti, P. (2021). Reduction of Multidrug-Resistant (MDR) Bacterial Infections during the COVID-19 Pandemic: A Retrospective Study. International Journal of Environmental Research and Public Health, 18(3), 1003. https://doi.org/10.3390/ijerph18031003







