Abstract
COVID-19 represents a threat to public health and the mental health of the aged population. Prevalence and risk factors of depression and anxiety have been reported in previous reviews in other populations; however, a systematic review on the factors associated with depression and anxiety in older adults is not currently present in the literature. We searched PubMed, Embase, Scopus, ProQuest Psychology Database, Science Direct, Cochrane Library and SciELO databases (23 February 2021). The results were obtained by entering a combination of MeSH or Emtree terms with keywords related to COVID-19, elderly, depression and anxiety in the databases. A total of 11 studies were included in the systematic review. Female gender, loneliness, poor sleep quality and poor motor function were identified as factors associated with both depression and anxiety. Aspects related to having a stable and high monthly income represent protective factors for both depression and anxiety, and exercising was described as protective for depression. This study synthesised information and analysed the main factors associated with depression and anxiety in the older population during the COVID-19 pandemic. However, the cross-sectional design of most of the included studies does not allow a causal relationship between the factors analysed and depression or anxiety.
Keywords:
COVID-19; depression; anxiety; mental health; older adults; aged; associated factors; risk factors 1. Introduction
The beginning of the COVID-19 pandemic marked a radical change in people’s lives, becoming a real threat to public health worldwide.
Many of the preventive measures adopted in different countries had among their main priorities protecting older people due to the severity of the manifestation of the disease and the high morbidity and mortality rates in this population [,,]. This situation can be expressed in the mortality rate increase among the population over 60 years of age, which was described to be up to 5 times higher than in other age groups [].
Inevitably the pandemic and its containment measures had a relevant impact on the sociocultural, economic, and psychological spheres [,,,,]. The prevention and mitigation of the disease itself have been the main focus of attention. Despite this, the minimisation of the negative consequences of isolation at the psychosocial level has often been in the background. In many countries, the public health policies adopted different measures, such as home lockdowns and closures of social gathering places []. In older people, social isolation is especially relevant due to the possible decrease in different functional aspects of the person and an increase in the difficulty in carrying out daily activities []. The consequences on mental health have been widely studied by many authors, who have described how the context of COVID-19 can affect the geriatric population’s mental state with disorders such as depression, anxiety, stress or insomnia [,,,,,,]. According to previous research, the prevalence of depression in older adults showed a significant increase from 7.2% to 19.8% since the beginning of the pandemic [] and psychogeriatric admissions increased by more than 21% []. The factors associated with different psychological conditions during the pandemic were investigated in a meta-analysis by Wang et al. [], which focused predominantly on the general population and reported that female gender, being aged <35, lower socio-economic status, higher risk of COVID-19 infection and longer media exposure were associated with psychological distress. The risk and protective factors of depression in older adults were described in a recent systematic review, which more homogeneously identified impairment, sleep disorders and chronic diseases as main risk factors, and physical activity as a protective factor; however, this review was not focused on the period of the COVID-19 pandemic, as the included studies were published between January 2000 and March 2020 []. To the best of our knowledge, no systematic reviews have been published to analyse the factors associated with depression and anxiety in the aged population during COVID-19. The identification and understanding of these factors represent a relevant aspect of minimising the impact on the psychosocial sphere of the adverse effects that the preventive and containment measures adopted during the pandemic may produce.
Hence, this study aimed to conduct a systematic review to explore the possible factors associated with depression and anxiety during the COVID-19 pandemic in a population older than 60 years.
We hypothesised that female gender, older age, poorer health conditions, loneliness, and a lower socio-economic status may be associated with depression and anxiety during the pandemic.
2. Materials and Methods
The presented systematic review was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses []. It was registered in the database for PROSPERO systematic reviews with the number CRD42021267998.
2.1. Search Strategy
The bibliographic search process was carried out in February 2021 in the following databases: PubMed, Embase, Scopus, ProQuest Psychology Database, Science Direct, Cochrane Library and SciELO. The results were obtained by entering a combination of MeSH or Emtree terms with keywords related to COVID-19, older adults, depression and anxiety in the databases. The search terms were combined with the Boolean operators AND and OR. To optimise the results, adjustments were made in the search procedure depending on the database used. The employed search terms and the search strategy used for each database are specified in the Supplementary Materials.
2.2. Eligibility Criteria
This systematic review included studies that analysed factors associated with depression or anxiety during the period of the COVID-19 pandemic, indicating that the subjects were ≥60 years of age, with original data, studies with a longitudinal or cross-sectional design, published in English, providing access to the full text, and expressing the predictive value of the factors associated with depression and/or anxiety with Odds Ratios (ORs) and their respective 95% confidence interval (CI).
The articles excluded for this review were those that did not show data on factors associated with depression and/or anxiety during the period of the COVID-19 pandemic, those that did not show original data (reviews, meta-analysis, opinion articles, study protocols, etc.) and clinical cases or case series. Studies with analysis stratified by age were excluded if the age of the total sample was <60.
2.3. Study Selection
The sequence for selecting the studies was, first, a search by combining MeSH terms and keywords in the different databases. Subsequently, duplicate articles were eliminated, and once the title and abstract had been read, potentially relevant articles were identified. When reading the entire document, the inclusion and exclusion criteria proposed for this review were considered.
Two independent reviewers oversaw the search process, selecting articles, and data extraction (G.C. and S.C.-B.). A third investigator (A.C.-U.) resolved any doubts of or discrepancies between the two principal investigators during this process.
For each article in this review, the following data were extracted: author, year of publication, type of study, characteristics of the participants, number of subjects, outcome measures and results obtained (Table 1 and Table 2).

Table 1.
Studies included that analyse factors associated with depression.

Table 2.
Studies included that analyse factors associated with anxiety.
2.4. Evaluation of the Quality of the Studies
The quality assessment of the included articles was carried out independently by the researchers G.C. and S.C.-B., with the researcher A.C.-U. in charge of resolving any discrepancies. The assessment was performed with the Joanna Briggs Institute scales for non-randomised studies []. These tools were previously used to determine the quality of cross-sectional and cohort studies included in other systematic reviews on factors associated with psychological stress resulting from the coronavirus disease [] and other emerging viruses []. The domains of the tools focus on the characteristics of the study population, the comparability of the groups, the validity and reliability of the exposure or outcome measurement method. The scales for cross-sectional and cohort studies evaluate 8 and 11 items, respectively (Table 3 and Table 4).

Table 3.
Joanna Briggs Institute tool for cross-sectional studies.

Table 4.
Joanna Briggs Institute tool for cohort studies.
3. Results
3.1. Study Selection
Our search (February 2021) identified 3756 citations from six databases. After removing duplicates, 2689 studies remained. From the 2689 studies, 2415 papers were excluded after screening the title and abstract. After reading 274 full-text papers, 263 were eliminated for not meeting the inclusion criteria. Finally, 11 studies were included in the current systematic review (Figure 1). The methodological quality of the included studies is summarised in Table 3 and Table 4.
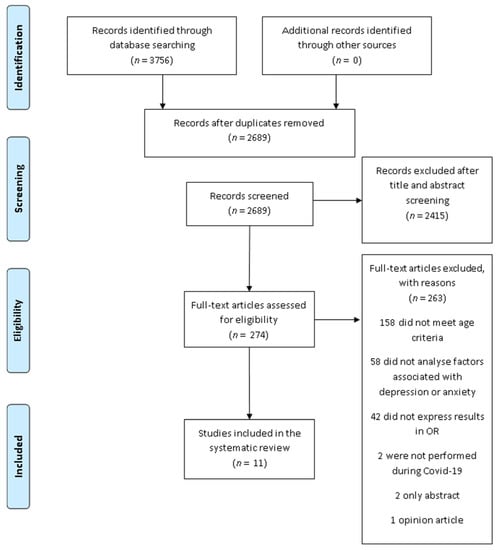
Figure 1.
PRISMA flow-chart of the study selection process.
3.2. Study Characteristics
Ten papers were cross-sectional studies [,,,,,,,,,], and one was a retrospective longitudinal study [].
Ten of the included studies investigated factors associated with depression [,,,,,,,,,], six with anxiety [,,,,,], and one unified both psychological outcomes in a single variable expressed as “depression or anxiety” []. Additionally, one of the studies analysed the associations with comorbid depression and anxiety [].
Among the included studies, five were from Europe [,,,,], four were from Asia [,,,], one was from North America [], and the last was from Latin America []. Specifically, the countries where the patients were recruited were: Italy [,], Spain [], United Kingdom [], France [], Japan [], Turkey [], Vietnam [], China [], Canada [] and various Spanish speaking countries of Latin America [].
The majority of studies were conducted among the general population [,,,,]. However, some of the papers included participants with specific characteristics: adults with mild cognitive impairment [,], psychiatric disorders [], Parkinson’s disease [], cardiometabolic disorders [] and COVID-19 [].
A variety of psychometric instruments were used to measure symptoms of anxiety and depression. The most often used tool was the Patient Health Questionnaire for depression (PHQ-9), used in four studies [,,,], followed by the Geriatric Depression Scale (GDS), used in two studies in the 5-item version [,] and one study in the 15-item version []. The following tools were used in the remainder of the studies: the Depression Rating Scale (DRS) [], the Depression items of the Hospital Anxiety and Depression Scale (HADS) [], the diagnostic criteria of the Diagnostic and Statistical Manual for Mental Disorders (DSM-5) [] and the Depression items of the Depression Anxiety Stress Scale (DASS) []. To assess anxiety, four studies used the Generalized Anxiety Disorder (GAD-7) [,,,], one the Geriatric Anxiety Inventory (GAI) [], one the anxiety items of the HADS [] and the last used the anxiety items of the DASS [].
3.3. Gender
Gender represents the socio-demographic factor most frequently associated with depression and anxiety. Its relationship with depression was analysed in seven studies [,,,,,,] and with anxiety in five studies [,,,,].
Five papers screened showed that the female gender is associated significantly with depression or anxiety, with Odds Ratio (OR) values ranging from 1.72 to 2.11 for depression [,,,] and from 1.98 to 3.32 for anxiety [,,].
Robb et al. [] investigated the association between female gender and changes in depression and anxiety symptoms; they found an association between female gender and worsening depression and anxiety since the pandemic.
Only one study included in this review described male gender as a significant risk factor for anxiety with OR: 17.12 (1.13–257.27) in Parkinson’s disease patients; in the same study, male gender was also reported as a risk factor for depression with OR: 5.66 (0.51–62.47). However, the association was not statistically significant in the last case [].
3.4. Age
A total of five publications analysed associations between age and depression or anxiety [,,,,]. Two studies reported a significant association between age and lower odds for anxiety or depression [,]. Specifically, Robb et al. [] found that with every five-year increase in age, there was a 19% (OR: 0.81 [0.77–0.85]) and 22% (OR: 0.78 [0.75–0.83]) lower risk of reporting feeling worse with regard to components of depression and anxiety, respectively; and Bobes-Bascarán et al. [] showed that younger age was a protective factor for anxiety (OR: 0.876 [0.800–0.960]). In addition, Kitani-Morii et al. [] reported that being aged between 70 and 79, in comparison to having an age of <70 years, represented a factor associated with depression in Parkinson’s disease patients (OR: 0.61 [0.05–0.08]). The remainder of the associations were not statistically significant.
3.5. Physical and Mental Conditions
Three studies analysed the association between different physical pathologies and depressive symptoms in older adults [,,]. Among these, only Carlos et al. [] found a statistically significant association between general health disorders and depression (OR: 2.45 [1.16–5.16]). Anxiety had a significant association with suffering flu symptoms [], having severe physical diseases [] and having COVID-19 symptoms for more than 14 days [] (OR: 4.01 [1.13–14.24]; 1.57 [1.05–2.35]; 7.584 [1.398–41.146], respectively).
Presenting past or current psychiatric disorders [] and a history of anxiety [] were predictive factors for depression. In contrast to these data, two studies included in this review suggest that having dementia [] or other psychiatric disorders [] may represent a protective factor for depression (OR: 0.69 [0.48–0.99]; 0.50 [0.35–0.71]).
Two studies reported a significant association between anxiety and these two factors: the presence of subjective cognitive decline [] and mental disorders [] (OR: 6.202 [3.005–12.799]; 4.39 [1.03–18.69], respectively).
One study reported that having schizophrenia and other psychiatric disorders may represent a protective factor for the combination of depression and anxiety (OR: 0.50 [0.26–0.97]; 0.53 [0.38–0.73]) [].
3.6. Sleep Quality
Different studies investigated the association of factors related to sleep quality with depression and anxiety. Carlos et al. [] reported that the presence of sleep disorders is significantly associated with depression (OR: 2.29 [1.06–4.93]). In line with these results, Li et al. [] showed that insomnia is associated with depression, anxiety and the combination of both of them (OR: 1.29 [1.24–1.34]; 1.15 [1.12–1.18]; 1.19 [1.16–1.23]). One study revealed that poor sleep quality has also been associated with worsening depressive symptoms and anxiety since the pandemic, with higher odds values for poorer sleep quality [].
3.7. Loneliness, Social Isolation and Personal Relationships
Several publications analysed the relationship between depression and anxiety with different factors within loneliness and social isolation.
Two studies reported that living alone may significantly predict depression and increase depressive symptoms [,]. In addition to living alone, Robb et al. [] analysed the feeling of loneliness, finding that feeling lonely more often has a strong association with experiencing a worsening of depressive symptoms (OR: 17.24 [13.20–22.50]) and anxiety (OR: 10.85 [8.39–14.03]).
The impact of personal relationships in older people was explored in different studies. Robb et al. [] suggest that being single, widowed or divorced represents a factor significantly associated with worsening depression after the beginning of the pandemic (OR: 1.37 [1.17–1.59]); by comparison, Bobes-Bascarán et al. [] report that never having been married represented a protective factor for depression (OR: 0.665 [0.456–0.970]). Bérard et al. [] show in their study that the worsening of the relationship with the partner from the beginning of the confinement is significantly associated with depression or anxiety (OR: 5.24 [2.11–13.0]).
Social media contact with family and friends is associated with improving and worsening anxiety symptoms []. Having friends or family with COVID-19 represents a factor significantly associated with depression (OR: 1.631 [1.247–2.132]) [].
3.8. Other Factors
Regarding socio-economic factors, a study carried out in Spain reports that being a civil servant and being retired represent protective factors for the presence of depression at the time of the pandemic (OR: 0.530 [0.293–0.957]; OR: 0.539 [0.311–0.934]) []; another study, in Turkey, assessed the amount of monthly income, and found that having a higher income was a significant protective factor for both depression and anxiety (OR: 0.13 [0.04–0.44]; OR: 0.07 [0.02–0.35]) [].
Several authors evaluated aspects of motor functions. In subjects with Parkinson’s disease, the second part of the MDS-UPDRS questionnaire shows a significant association with depression and anxiety (OR: 1.31 [1.04–1.66]; 1.36 [1.07–1.72]) []. Other authors reported that poorer functional mobility is associated with depression (OR: 1.86 [1.35–2.56]) [].
Physical activity is another variable that has been studied. Two studies found data in the same line. One author describes that less physical activity is associated with depression [], whereas another reports that exercising regularly may represent a protective factor (OR: 0.30 [0.12–0.72]) [].
Do et al. [] analysed the association between depression and health literacy in people with and without COVID-19, finding a significant association in patients with COVID-19 (OR: 0.91 [0.87–0.94]).
Two publications analysed nutritional factors: Piskorz et al. [] found significant associations of low consumption of fruit or vegetables and a reduced food intake with depression in patients with cardiometabolic disorders (OR: 1.46 [1.05–2.03]; 2.10 [1.68–2.62]); Bérard et al. [] reported that a pre-confinement Diet Quality Score > the median of the sample presented OR values of 0.51 (0.31–0.85) for depression or anxiety.
4. Discussion
The COVID-19 pandemic had a considerable impact on people’s lives, and especially on those of older adults. Mental health has been an issue of public concern, with disorders such as depression or anxiety among the most relevant conditions [,]. To the best of our knowledge, the present study is the first systematic review investigating the factors associated with depression and anxiety during the COVID-19 pandemic in people aged ≥60. The data from ten cross-sectional studies and one longitudinal study were analysed.
The factors reported were predominantly related to socio-demographic characteristics or physical and mental health aspects. Among the socio-demographic factors, the female gender is the most frequently associated with depression and anxiety [,,,,,,]. These findings are consistent with other reviews focused on the general population and healthcare workers during the pandemic [,] and more studies before COVID-19 [,,]. Previous research suggests that this gender disparity may be mediated by variables that concern work, economic, educational, neuro-hormonal, psychological and genetic aspects [,,,]. The economic crisis caused by the pandemic, combined with a baseline situation of social inequity, may be a trigger for an increased adverse psychological response. Gender inequity has been a cause of suffering for many women worldwide, leading to worse mental health outcomes in different contexts [,], including the SARS epidemic in 2003 [].
Regarding age, despite being the group of individuals most at risk of suffering from a severe form of the disease [,], and in contrast to our initial hypothesis, the results found in this review indicate that being older is a protective factor for depression or anxiety [,]. It is important to note that in our review, among the studies that analysed age as a predictor, three recruited their sample directly from older people [,,], one selected long-term care home residents with a mean age of 81.4 (±11.5) years [], and in one most of the participants were in the age range of 70–79 years (mean age 72.3 ± 10.9) []. Consequently, it must be considered that the comparisons between ages when calculating the OR were made within a relatively similar range. This may have led to obtaining less significant odds than comparing age groups with a greater difference. The results of a review carried out in the general population during the period of COVID-19 were in line with our data, and reported that younger ages presented a higher OR for both depression and anxiety [].
By comparison, pre-pandemic studies analysing the relationship between age and mental health outcomes associate the presence of depression and anxiety with the advance in age, with a prevalence among the older population ranging between 3% and 15% for anxiety and up to 42% for depression [,]. A possible explanation for this difference may be that, in the context of COVID-19, multiple control measures involved social restrictions and reduction of working activity in many areas. Younger people may have been more affected by such a radical lifestyle change. They may experience greater fear regarding their occupational and economic future than a population already retired or close to the retirement age and whose daily routine may have been affected in a minor way. Supporting this, one of the studies included in this review identified being retired and aspects related to having stable and high incomes as protective factors for depression [].
Physical and mental health have been previously associated with depression and anxiety [,,]. In our review, the results regarding the factors related to physical health show some variability depending on the outcome. Among the studies that investigated the relationship between several physical health variables and depression, two did not find statistically significant associations [,]; only one study reported that suffering health problems may represent a risk factor for depressive symptoms []. By comparison, in our study, different physical conditions presented a greater number of significant associations with anxiety, suggesting that flu symptoms [], severe physical illnesses [] and having more than 14 days with COVID-19 symptoms [] may represent possible risk factors. Mental health factors have several significant associations. However, whether these factors are associated with positive or negative outcomes may change according to the study: three studies identified the presence of current cognitive disorders as risk factors for depression and anxiety [,,], whereas two others reported that the presence of different psychiatric diagnoses represented protective factors for depression [,] and comorbid depression and anxiety []. It is interesting to note that the data collected in most of these studies was self-reported through surveys, although it was not clearly stated how the presence/absence of pathology was defined, and data was not collected via a clinical examination by a professional; these factors may lead to differences in the results. The factors in the health sphere that were more consistently associated with both depression and anxiety among the studies were those related to the presence of low quality of sleep [,,], and psychophysical comorbidity was among the most prevalent of the COVID-19 era [].
Several studies in this review explored many aspects of loneliness, social isolation and personal relationships. According to our findings, living or feeling alone are associated with both depression and anxiety [,]. In line with these data, several of the included authors found that being single, widowed, or divorced, or experiencing a worsening of relationships with their partner, is associated with worse psychological outcomes [,]. Another study showed that never having been married represented a protective factor for the presence of depressive symptoms []. Social isolation during the pandemic was described in a previous review as a risk factor in other populations []. Indeed, people’s social sphere has been one of the most affected by COVID-19 []. Containment measures, together with public health policies, resulted in a drastic reduction in social life, which could nearly be eradicated in the case of a home lockdown. It may be expected that in a context where a large degree of the development of social relationships occurs within the household, living alone, without a partner or with bad relationships with partners may predispose individuals to the development of depressive symptoms or anxiety. However, these considerations about social relationships may not extend to contacts via technology. One study included in our review shows that levels of social media contacts did not significantly alter the risk of reporting worsening depression and that their relationship with anxiety was unclear [].
Regarding the association between physical activity and depression, in our review, two studies consistently reported data associating a lower amount of physical activity with depression [], and that exercising may represent a protective factor against it []. The association of physical activity with depression has previously been investigated in the older population. Our results are consistent with a review conducted prior to the pandemic, which reported that having low physical activity levels may represent a risk factor for depressive symptoms []. Additionally, it should be considered that increased levels of physical activity may lead to better motor function, especially in an aged population.
Previous research associated depression with aspects related to a lower motor function, such as less grip strength [] or a slower gait speed []. The relationship of poorer function, disability and depression is often described as bidirectional, with the possibility that both factors influence each other []. In our study, the aspects of motor function that presented a significant association with depression were poorer functional mobility [] and poorer motor capacity in subjects with Parkinson’s disease [].
This review was subject to some limitations. First, only studies published in English were included. Considering the global nature of the COVID-19 pandemic, this may have led to the loss of information published in other languages. Including only peer-reviewed studies and not assessing the grey literature may have contributed to further loss of information. However, this criterion was chosen to establish a minimum quality standard for the publications to be included.
Furthermore, we must mention that our review only included studies in which the age of the total sample was ≥60 years, and excluded publications in which the sample was only presented in a stratified manner. This criterion was adopted considering that the population of interest was specified with terms related to older adults when conducting the bibliographic search. Moreover, it must be taken into account that the included studies were performed mostly within the first months since the beginning of the pandemic. Thus, considering the changes in public health policies and the evolution of the COVID-19 pandemic, the results of this systematic review can only be related to this period. Lastly, the design of the included studies must be considered. All the studies except one used a cross-sectional design, which does not allow information to be obtained to detect changes over time in the psychological state or estimate the real impact that the pandemic and its containment measures may have had on depression or anxiety. Similarly, it also limits the understanding of the causality between the factors and outcomes studied.
Our systematic review focused exclusively on describing the associated factors for depression and anxiety. However, the COVID-19 pandemic has led to multiple psychological conditions in the elderly population. Future studies may include other mental health outcomes, such as stress, insomnia or fear. Analysing the factors associated with a more significant number of disorders of the psychic sphere may positively impact the aspects that concern their prevention and treatment during the pandemic.
5. Conclusions
COVID-19 mainly affects older adults, as reflected in morbidity and mortality rates. Taking this into account, this review focused on the possible psychological aspect of the COVID-19 pandemic in this population by analysing the factors associated with depression and anxiety.
Female gender, loneliness, poor sleep quality and poor motor function were identified as factors associated with both depression and anxiety. Levels of physical activity or exercise were associated with depression, with lower levels of activity identified as risk factors and exercising regularly as a protective factor. Several physical health conditions may be associated with anxiety. Aspects related to having a stable and high monthly income represent protective factors for both depression and anxiety. A small number of studies suggested that being older may represent a protective factor for anxiety and depression; however, other studies did not find this association to be significant. Due to the lack of consistency between the studies analysed, the association between mental health status and depression or anxiety is unclear.
This study collected information and analysed the different factors associated with depression and anxiety in the aged population during the pandemic. However, the cross-sectional design of most of the included studies does not allow the formulation of a causal relationship between the factors analysed and depression or anxiety.
Supplementary Materials
The following are available online at https://www.mdpi.com/article/10.3390/ijerph182211859/s1.
Author Contributions
Conceptualization, G.C., Y.M.-R. and S.C.-B.; methodology, G.C., S.C.-B. and A.C.-U.; software, M.I.A.-C. and M.I.A.-E.; validation, Y.M.-R. and S.C.-B.; formal analysis, G.C., S.C.-B. and A.C.-U.; investigation, G.C. and Y.M.-R.; resources, G.C., A.C.-U. and Y.M.-R.; data curation, G.C., S.C.-B. and M.I.A.-C.; writing—original draft preparation, G.C., M.I.A.-C. and M.I.A.-E.; writing—review and editing, G.C., M.I.A.-C. and M.I.A.-E.; visualization, M.I.A.-C., S.C.-B. and M.I.A.-E.; supervision, Y.M.-R.; project administration, Y.M.-R. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare no conflict of interest.
References
- Wang, L.; He, W.; Yu, X.; Hu, D.; Bao, M.; Liu, H.; Zhou, J.; Jiang, H. Coronavirus disease 2019 in elderly patients: Characteristics and prognostic factors based on 4-week follow-up. J. Infect. 2020, 80, 639–645. [Google Scholar] [CrossRef]
- Verity, R.; Okell, L.C.; Dorigatti, I.; Winskill, P.; Whittaker, C.; Imai, N.; Cuomo-Dannenburg, G.; Thompson, H.; Walker, P.G.T.; Fu, H.; et al. Estimates of the severity of coronavirus disease 2019: A model-based analysis. Lancet Infect. Dis. 2020, 20, 669–677. [Google Scholar] [CrossRef]
- Chen, T.; Wu, D.; Chen, H.; Yan, W.; Yang, D.; Chen, G.; Ma, K.; Xu, D.; Yu, H.; Wang, H.; et al. Clinical characteristics of 113 deceased patients with coronavirus disease 2019: Retrospective study. BMJ 2020, 368, m1091. [Google Scholar] [CrossRef] [Green Version]
- Xiang, G.; Xie, L.; Chen, Z.; Hao, S.; Fu, C.; Wu, Q.; Liu, X.; Li, S. Clinical risk factors for mortality of hospitalized patients with COVID-19: Systematic review and meta-analysis. Ann. Palliat. Med. 2021, 10, 2723–2735. [Google Scholar] [CrossRef]
- Chu, I.Y.-H.; Alam, P.; Larson, H.J.; Lin, L. Social consequences of mass quarantine during epidemics: A systematic review with implications for the COVID-19 response. J. Travel Med. 2020, 27, taaa192. [Google Scholar] [CrossRef] [PubMed]
- Wang, Y.; Kala, M.P.; Jafar, T.H. Factors associated with psychological distress during the coronavirus disease 2019 (COVID-19) pandemic on the predominantly general population: A systematic review and meta-analysis. PLoS ONE 2020, 15, e0244630. [Google Scholar] [CrossRef]
- Luo, M.; Guo, L.; Yu, M.; Jiang, W.; Wang, H. The psychological and mental impact of coronavirus disease 2019 (COVID-19) on medical staff and general public—A systematic review and meta-analysis. Psychiatry Res. 2020, 291, 113190. [Google Scholar] [CrossRef]
- Marcén-Román, Y.; Gasch-Gallen, A.; de la Mota, I.V.M.; Calatayud, E.; Gómez-Soria, I.; Rodríguez-Roca, B. Stress Perceived by University Health Sciences Students, 1 Year after COVID-19 Pandemic. Int. J. Environ. Res. Public Health 2021, 18, 5233. [Google Scholar] [CrossRef] [PubMed]
- O’Sullivan, R.; Burns, A.; Leavey, G.; Leroi, I.; Burholt, V.; Lubben, J.; Holt-Lunstad, J.; Victor, C.; Lawlor, B.; Vilar-Compte, M.; et al. Impact of the COVID-19 Pandemic on Loneliness and Social Isolation: A Multi-Country Study. Int. J. Environ. Res. Public Health 2021, 18, 9982. [Google Scholar] [CrossRef] [PubMed]
- Lahiri, A.; Jha, S.S.; Bhattacharya, S.; Ray, S.; Chakraborty, A. Effectiveness of preventive measures against COVID-19: A systematic review of In Silico modeling studies in indian context. Indian J. Public Health 2020, 64, S156–S167. [Google Scholar] [CrossRef]
- Shankar, A.; McMunn, A.; Demakakos, P.; Hamer, M.; Steptoe, A. Social isolation and loneliness: Prospective associations with functional status in older adults. Health Psychol. 2017, 36, 179–187. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Grolli, R.E.; Mingoti, M.E.D.; Bertollo, A.G.; Luzardo, A.R.; Quevedo, J.; Réus, G.Z.; Ignácio, Z.M. Impact of COVID-19 in the Mental Health in Elderly: Psychological and Biological Updates. Mol. Neurobiol. 2021, 58, 1905–1916. [Google Scholar] [CrossRef]
- Maggi, G.; Baldassarre, I.; Barbaro, A.; Cavallo, N.D.; Cropano, M.; Nappo, R.; Santangelo, G. Mental health status of Italian elderly subjects during and after quarantine for the COVID-19 pandemic: A cross-sectional and longitudinal study. Psychogeriatrics 2021, 21, 540–551. [Google Scholar] [CrossRef] [PubMed]
- Levkovich, I.; Shinan-Altman, S.; Schvartz, N.E.; Alperin, M. Depression and Health-Related Quality of Life Among Elderly Patients during the COVID-19 Pandemic in Israel: A Cross-sectional Study. J. Prim. Care Community Health 2021, 12, 2150132721995448. [Google Scholar] [CrossRef]
- Gorrochategi, M.P.; Munitis, A.E.; Santamaria, M.D.; Etxebarria, N.O. Stress, Anxiety, and Depression in People Aged Over 60 in the COVID-19 Outbreak in a Sample Collected in Northern Spain. Am. J. Geriatr. Psychiatry 2020, 28, 993–998. [Google Scholar] [CrossRef]
- De Pue, S.; Gillebert, C.; Dierckx, E.; Vanderhasselt, M.-A.; De Raedt, R.; Bussche, E.V.D. The impact of the COVID-19 pandemic on wellbeing and cognitive functioning of older adults. Sci. Rep. 2021, 11, 1–11. [Google Scholar] [CrossRef]
- Briggs, R.; McDowell, C.P.; De Looze, C.; Kenny, R.A.; Ward, M. Depressive Symptoms Among Older Adults Pre– and Post–COVID-19 Pandemic. J. Am. Med. Dir. Assoc. 2021, 22, 2251–2257. [Google Scholar] [CrossRef]
- Lee, A.T.C.; Mo, F.Y.M.; Lam, L.C.W. Higher psychogeriatric admissions in COVID-19 than in severe acute respiratory syndrome. Int. J. Geriatr. Psychiatry 2020, 35, 1449–1457. [Google Scholar] [CrossRef]
- Maier, A.; Riedel-Heller, S.G.; Pabst, A.; Luppa, M. Risk factors and protective factors of depression in older people 65+. A systematic review. PLoS ONE 2021, 16, e0251326. [Google Scholar] [CrossRef] [PubMed]
- Liberati, A.; Altman, D.G.; Tetzlaff, J.; Mulrow, C.; Gøtzsche, P.C.; Ioannidis, J.P.A.; Clarke, M.; Devereaux, P.J.; Kleijnen, J.; Moher, D. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate healthcare interventions: Explanation and elaboration. BMJ 2009, 339, b2700. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bobes-Bascarán, T.; Sáiz, P.A.; Velasco, A.; Martínez-Cao, C.; Pedrosa, C.; Portilla, A.; de la Fuente-Tomas, L.; García-Alvarez, L.; García-Portilla, M.P.; Bobes, J. Early Psychological Correlates Associated With COVID-19 in A Spanish Older Adult Sample. Am. J. Geriatr. Psychiatry 2020, 28, 1287–1298. [Google Scholar] [CrossRef] [PubMed]
- Carlos, A.F.; Poloni, T.E.; Caridi, M.; Pozzolini, M.; Vaccaro, R.; Rolandi, E.; Cirrincione, A.; Pettinato, L.; Vitali, S.F.; Tronconi, L.; et al. Life during COVID-19 lockdown in Italy: The influence of cognitive state on psychosocial, behavioral and lifestyle profiles of older adults. Aging Ment. Health 2021, 1–10. [Google Scholar] [CrossRef]
- Robb, C.E.; De Jager, C.A.; Ahmadi-Abhari, S.; Giannakopoulou, P.; Udeh-Momoh, C.; McKeand, J.; Price, G.; Car, J.; Majeed, A.; Ward, H.; et al. Associations of Social Isolation with Anxiety and Depression During the Early COVID-19 Pandemic: A Survey of Older Adults in London, UK. Front. Psychiatry 2020, 11, 591120. [Google Scholar] [CrossRef] [PubMed]
- Di Santo, S.G.; Franchini, F.; Filiputti, B.; Martone, A.; Sannino, S. The Effects of COVID-19 and Quarantine Measures on the Lifestyles and Mental Health of People Over 60 at Increased Risk of Dementia. Front. Psychiatry 2020, 11, 578628. [Google Scholar] [CrossRef] [PubMed]
- Do, B.N.; Nguyen, P.-A.; Pham, K.M.; Nguyen, H.C.; Nguyen, M.H.; Tran, C.Q.; Nguyen, T.T.P.; Tran, T.V.; Pham, L.V.; Tran, K.V.; et al. Determinants of Health Literacy and Its Associations with Health-Related Behaviors, Depression Among the Older People With and Without Suspected COVID-19 Symptoms: A Multi-Institutional Study. Front. Public Health 2020, 8, 581746. [Google Scholar] [CrossRef]
- Li, W.; Zhao, N.; Yan, X.; Zou, S.; Wang, H.; Li, Y.; Xu, X.; Du, X.; Zhang, L.; Zhang, Q.; et al. The prevalence of depressive and anxiety symptoms and their associations with quality of life among clinically stable older patients with psychiatric disorders during the COVID-19 pandemic. Transl. Psychiatry 2021, 11, 1–8. [Google Scholar] [CrossRef] [PubMed]
- Kitani-Morii, F.; Kasai, T.; Horiguchi, G.; Teramukai, S.; Ohmichi, T.; Shinomoto, M.; Fujino, Y.; Mizuno, T. Risk factors for neuropsychiatric symptoms in patients with Parkinson’s disease during COVID-19 pandemic in Japan. PLoS ONE 2021, 16, e0245864. [Google Scholar] [CrossRef] [PubMed]
- McArthur, C.; Saari, M.; Heckman, G.A.; Wellens, N.; Weir, J.; Hebert, P.; Turcotte, L.; Jbilou, J.; Hirdes, J.P. Evaluating the Effect of COVID-19 Pandemic Lockdown on Long-Term Care Residents’ Mental Health: A Data-Driven Approach in New Brunswick. J. Am. Med. Dir. Assoc. 2021, 22, 187–192. [Google Scholar] [CrossRef] [PubMed]
- Piskorz, D.; Barragán, A.P.; Santi, R.L.; Vázquez, G.; Ortiz, G.S.; Zambrano, L.R.; Castillo, M.M.; Roa, C.; Baños, M.; Ramos, M.G.; et al. Psychological Impact of the Pandemic on Ambulatory Cardiometabolic Patients Without Evidence of SARS-CoV-2 Infection. The CorCOVID Latam Psy Study. Curr. Probl. Cardiol. 2021, 46, 100737. [Google Scholar] [CrossRef] [PubMed]
- Cigiloglu, A.; Ozturk, Z.A.; Efendioglu, E.M. How have older adults reacted to coronavirus disease 2019? Psychogeriatrics 2021, 21, 112–117. [Google Scholar] [CrossRef]
- Bérard, E.; Kai, S.H.Y.; Coley, N.; Bongard, V.; Ferrières, J. Lockdown-related factors associated with the worsening of cardiovascular risk and anxiety or depression during the COVID-19 pandemic. Prev. Med. Rep. 2021, 21, 101300. [Google Scholar] [CrossRef]
- Moola, S.; Munn, Z.; Sears, K.; Sfetcu, R.; Currie, M.; Lisy, K.; Tufanaru, C.; Qureshi, R.; Mattis, P.; & Mu, P. Conducting systematic reviews of association (etiology): The Joanna Briggs Institute’s approach. Int. J. Evid. 2015, 13, 163–169. [Google Scholar] [CrossRef] [PubMed]
- Kisely, S.; Warren, N.; McMahon, L.; Dalais, C.; Henry, I.; Siskind, D. Occurrence, prevention, and management of the psychological effects of emerging virus outbreaks on healthcare workers: Rapid review and meta-analysis. BMJ 2020, 369, m1642. [Google Scholar] [CrossRef] [PubMed]
- Swendeman, D.; Fehrenbacher, A.E.; Roy, S.; Das, R.; Ray, P.; Sumstine, S.; Ghose, T.; Jana, S. Gender disparities in depression severity and coping among people living with HIV/AIDS in Kolkata, India. PLoS ONE 2018, 13, e0207055. [Google Scholar] [CrossRef]
- Assariparambil, A.R.; Noronha, J.A.; Kamath, A.; Adhikari, P.; Nayak, B.S.; Shankar, R.; George, A. Depression among older adults: A systematic review of South Asian countries. Psychogeriatrics 2021, 21, 201–219. [Google Scholar] [CrossRef]
- Acciai, F.; Hardy, M. Depression in later life: A closer look at the gender gap. Soc. Sci. Res. 2017, 68, 163–175. [Google Scholar] [CrossRef] [PubMed]
- Qiu, Q.-W.; Qian, S.; Li, J.-Y.; Jia, R.-X.; Wang, Y.-Q.; Xu, Y. Risk factors for depressive symptoms among older Chinese adults: A meta-analysis. J. Affect. Disord. 2020, 277, 341–346. [Google Scholar] [CrossRef]
- Kuehner, C. Gender differences in unipolar depression: An update of epidemiological findings and possible explanations. Acta Psychiatr. Scand. 2003, 108, 163–174. [Google Scholar] [CrossRef]
- Lee, A.M.W.S.; Wong, J.G.; McAlonan, G.M.; Cheung, V.; Cheung, C.; Sham, P.C.; Chu, C.-M.; Wong, P.-C.; Tsang, K.W.; Chua, S.E. Stress and Psychological Distress among SARS Survivors 1 Year after the Outbreak. Can. J. Psychiatry 2007, 52, 233–240. [Google Scholar] [CrossRef] [Green Version]
- Bryant, C.; Jackson, H.; Ames, D. The prevalence of anxiety in older adults: Methodological issues and a review of the literature. J. Affect. Disord. 2008, 109, 233–250. [Google Scholar] [CrossRef]
- Zhao, Y.-J.; Jin, Y.; Rao, W.-W.; Li, W.; Zhao, N.; Cheung, T.; Ng, C.H.; Wang, Y.-Y.; Zhang, Q.-E.; Xiang, Y.-T. The prevalence of psychiatric comorbidities during the SARS and COVID-19 epidemics: A systematic review and meta-analysis of observa-tional studies. J. Affect. Disord. 2021, 287, 145–157. [Google Scholar] [CrossRef] [PubMed]
- Bishwajit, G.; O’Leary, D.P.; Ghosh, S.; Yaya, S.; Shangfeng, T.; Feng, Z. Physical inactivity and self-reported depression among middle- and older-aged population in South Asia: World health survey. BMC Geriatr. 2017, 17, 100. [Google Scholar] [CrossRef] [PubMed]
- Zasadzka, E.; Pieczyńska, A.; Trzmiel, T.; Kleka, P.; Pawlaczyk, M. Correlation between Handgrip Strength and Depression in Older Adults—A Systematic Review and a Meta-Analysis. Int. J. Environ. Res. Public Health 2021, 18, 4823. [Google Scholar] [CrossRef] [PubMed]
- Tsutsumimoto, K.; Doi, T.; Shimada, H.; Makizako, H.; Hotta, R.; Nakakubo, S.; Suzuki, T. Combined Effect of Slow Gait Speed and Depressive Symptoms on Incident Disability in Older Adults. J. Am. Med. Dir. Assoc. 2016, 17, 123–127. [Google Scholar] [CrossRef] [PubMed] [Green Version]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).