Abstract
Background: There is increasing evidence that healthcare workers (HCWs) experience significant psychological distress during an epidemic or pandemic. Considering the increase in emerging infectious diseases and the ongoing COVID-19 pandemic, it is timely to review and synthesize the available evidence on the psychological impact of disease outbreaks on HCWs. Thus, we conducted a systematic review to examine the impact of epidemics and pandemics on the mental health of HCWs. Method: PubMed, PsycInfo, and PsycArticles databases were systematically searched from inception to June-end 2020 for studies reporting the impact of a pandemic/epidemic on the mental health of HCWs. Results: Seventy-six studies were included in this review. Of these, 34 (45%) focused on SARS, 28 (37%) on COVID-19, seven (9%) on MERS, four (5%) on Ebola, two (3%) on H1N1, and one (1%) on H7N9. Most studies were cross-sectional (93%) and were conducted in a hospital setting (95%). Common mental health symptoms identified by this review were acute stress disorder, depression, anxiety, insomnia, burnout, and post-traumatic stress disorder. The associated risk factors were working in high-risk environments (frontline), being female, being a nurse, lack of adequate personal protective equipment, longer shifts, lack of knowledge of the virus, inadequate training, less years of experience in healthcare, lack of social support, and a history of quarantine. Conclusion: HCWs working in the frontline during epidemics and pandemics experience a wide range of mental health symptoms. It is imperative that adequate psychological support be provided to HCWs during and after these extraordinary distressful events.
1. Introduction
The frequency of disease outbreaks has increased over the past century due to population growth, the increased interconnectedness of the world, microbial adaptation and change, economic development, changes in land use, and climate change [1]. Emerging infectious diseases that have caused epidemics over the past two decades include the severe acute respiratory syndrome (SARS) in 2003, Influenza A virus subtype H1N1 in 2009, Middle East respiratory syndrome coronavirus (MERS-COV) in 2012, Ebola Virus Disease (EVD) in 2014, the influenza A virus subtype H7N9, and the severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) in December 2019, which has resulted in the coronavirus disease 2019 (COVID-19) pandemic [2].
Disease outbreaks cause an unexpected increase in morbidity and mortality, which in turn cause an increased demand on healthcare facilities [3]. The rapid increase in patient populations drastically reduces the healthcare worker (HCW) to patient ratio thus increasing workload. HCWs suffer from both physical and mental fatigue because their working hours are increased and they may be asked to work more night shifts; thus, they do not have enough time to sleep, rest, and recuperate. As they work in the frontline, diagnosing, managing, and caring for sick patients, they experience a variety of mental health symptoms which may also persist after the epidemic has ended [4].
The massive influx of patients overwhelms the capacity of healthcare systems, giving rise to ethical dilemmas around the distribution of essential healthcare and medical supplies. HCWs constantly have to make “life or death” decisions, such as which patients to admit or not admit into intensive care and when to withdraw life support [5]. Due to the increased numbers of people dying, HCWs repeatedly break bad news, sometimes in ways they are not used to, including over the phone, thus making breaking bad news more distressing [6]. The news of continuously rising numbers of confirmed cases and deaths is emotionally overwhelming.
The shortage in supplies of personal protective equipment (PPE) may increase the risk and fear of contagion [7]. During this time, HCWs continuously live with anxiety and fear of contracting the disease more so when a colleague becomes infected or dies [8]. They fear transmitting the infection to their families as well as experiencing stigma and discrimination from their communities due to transmission fears. This type of stigmatization may even escalate to harassment, being denied access to public transport, physical violence, and eviction from their homes by landlords [9]. Social ostracization aggravates the occupational stress that HCWs are already facing as they battle the disease outbreak [10].
Overall, these negative psychological factors do not only affect the HCWs themselves, but also reduce their effectiveness in fighting epidemics, therefore indirectly affecting the whole population at large. This systematic review aims to synthesize the available evidence on the impact of epidemics and pandemics on the mental health of HCWs which will guide and inform best practice policies for psychological supports and mental health interventions for HCWs. Even though similar systematic reviews have been conducted recently [11,12,13,14,15,16], these were either specific to a single pandemic [11] (i.e., SARS) or Covid-19 [13,14,15,16], or with a small number of studies [12,13,16], and included only one study from low- and middle-income countries [12].
2. Materials and Methods
This systematic review followed the Preferred Reporting Items for Systematic Reviews and Meta-Analysis Protocols guidelines (PRISMA) [17]. However, the review is descriptive in nature, and the data extracted from the selected studies were summarized but not statistically combined owing to methodological heterogeneity. The study protocol was pre-registered with the National Institute for Health Research international prospective register of scientific reviews (PROSPERO, CRD42020186331) [18].
2.1. Data Sources and Search Strategy
A comprehensive systematic search of the most common databases—PubMed, PsycInfo, and PsycArticles, was conducted from inception to June-end 2020. Furthermore, the reference list of the retrieved articles and systematic reviews of similar topics were also examined to verify whether any potential studies had been left out. The author (O.C.C.) conducted the initial literature search. The full search strategy is available in Appendix A. Combinations of the following terms were used for the search:
Category 1: Population (healthcare professional, healthcare workers, physician, doctor, nurse)
Category 2: Exposure (epidemic, pandemic, SARS, MERS, Ebola, H1N1, H7N9, COVID 19). The terms epidemic and pandemic were defined according to the World Health Organization definitions. “An epidemic is the occurrence in a community or region of cases of an illness, specific health-related behavior, or other health-related events clearly in excess of normal expectancy” [19]. “A pandemic is the worldwide spread of a new disease” [20].
Category 3: Outcomes (mental health, mental disorder, psychological, depression, anxiety, stress, burden, insomnia, sleep disturbance, burnout, fear, stigma, discrimination).
Search results citations were downloaded to Endnote reference management software version X9 and duplicates were removed. The author (O.C.C.) performed the initial screening of titles and abstracts for relevance.
2.2. Eligibility Criteria
The following criteria were applied for papers to be included in the review:
- Studies reporting the impact of a pandemic/epidemic on mental health outcomes of health care workers.
- Cross-sectional, case–control, and cohort studies. Intervention studies were considered for inclusion only when they had sufficient details about the baseline mental health outcomes.
- Studies were selected if data was from an original study
- Studies had to be published in a peer reviewed journal.
- Only English language studies were included.
- No restrictions were placed on the publication date.
- There was no limit on the geographical location of studies.
Preprints, study protocols, and conference abstracts/proceedings were excluded.
2.3. Data Extraction and Quality Appraisal
The author (O.C.C.) checked the relevant studies for eligibility and extracted data from the eligible studies onto a standard Microsoft Excel data extraction form. A second reviewer (A.S.) independently verified the eligibility of the included studies. Any discrepancies were resolved by discussion. Full text articles for eligible studies were obtained. The data extraction form included the author(s) of the study, the publication year, country of study, details about study participants, study settings, study design, outcome measures used, and main findings. Furthermore, information necessary for evaluating study quality was also extracted from the eligible studies. Studies were assessed for methodological quality using the Joanna Briggs Institute (JBI) critical appraisal tools for cross sectional [21] and cohort studies [22].
2.4. Data Analysis and Synthesis
The authors analyzed and synthesized the results using a narrative text approach to summarize and explain the study findings focusing on prevalence of mental health outcomes, and the associated risk and protective factors.
3. Results
3.1. Study Selection Process
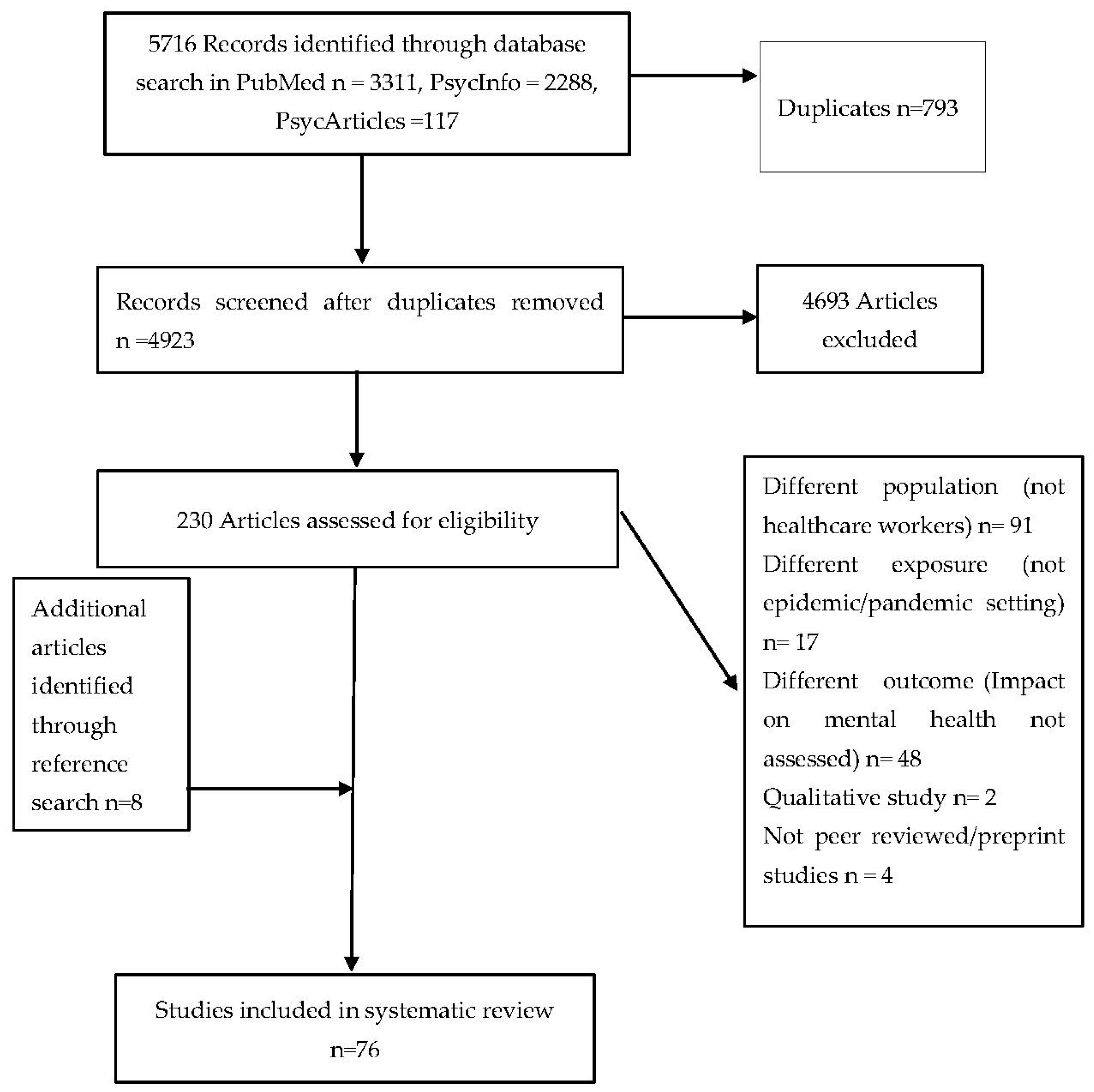
The three database searches yielded 5716 articles. After removal of 793 duplicates, the titles and abstracts of 4923 articles were screened. Two-hundred-and-thirty potential studies were identified, and the full texts were checked for eligibility. Sixty-eight articles met the inclusion criteria and eight more were identified through searching references of selected papers totaling 76 final studies. Details are provided in the PRISMA flowchart (Figure 1).
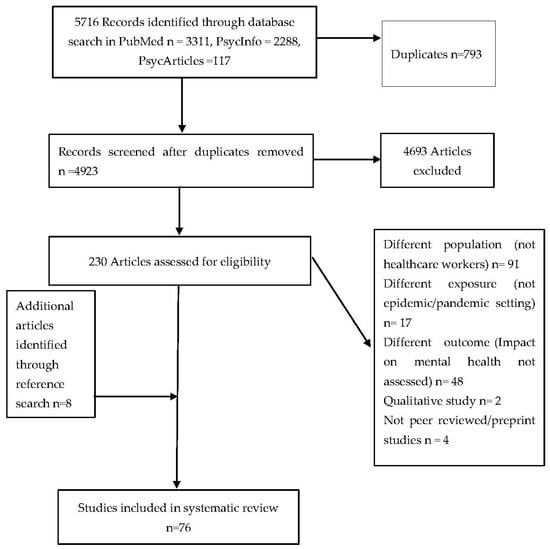
Figure 1.
PRISMA flow diagram of studies selected for inclusion in systematic review.
3.2. Characteristics of Selected Studies
The characteristics of the selected studies are shown in Table 1 and Table 2. Overall, seventy-six papers met the inclusion criteria. Of these, 34 (44%) focused on SARS, 28 (37%) on COVID-19, seven (9%) on MERS, four (5%) on Ebola, 2 (3%) on H1N1, and one (1%) on H7N9. The studies were conducted in different countries: 26 (34%) China; nine (12%) Taiwan; seven (9%) Canada; eight (11%) Hong Kong; seven (9%) Singapore; four (5%) Saudi Arabia; four (5%) Korea; one (1%) each from Germany, Greece, Iran, Italy, Japan, Liberia, Sierra Leonne, Nigeria, Turkey, and USA; and one was conducted in two countries Singapore and India. Most studies were conducted in a hospital setting 71 (95%), three in a general practice setting, and one at a rehabilitation center. Sixty studies (80%) included more than one type of HCW, 12 had only nurses, and three had only doctors/physicians. A higher proportion of studies 71 (93%) studies were cross-sectional and only 5 (7%) were cohort studies.

Table 1.
A summary of the cross-sectional studies included in this review.

Table 2.
A summary of the cohort studies included in this review.
3.3. Quality Appraisal
A more detailed assessment is available in Table 3 and Table 4. All eligible studies were included in the review, regardless of their quality assessment results. Of the 71 cross-sectional studies, 42 papers (59%) were of very good quality, five papers (7%) were of good quality, 15 papers (21%) were of average quality, and nine papers (13%) were of poor quality. Of the five cohort studies, one paper was of very good quality, two papers were of good quality, one paper had average quality, and one was of poor quality.

Table 3.
Critical appraisal of cross-sectional studies.

Table 4.
Critical appraisal of cohort studies.
3.4. Commonly Used Mental Health Instruments in This Analysis
The Impact of Events Scale (IES) and the Perceived Stress Scale (PSS) were the most common instruments used to measure stress. The Generalized Anxiety Disorder (GAD) and the Zung Self-Rating Anxiety Scale (SAS) were frequently used instruments to measure anxiety. Commonly used instruments to measure depression were the Patient Health Questionnaire (PHQ) and the Zung Self-Rating Depression Scale. Insomnia was often measured using the Insomnia Severity Index (ISI) and the Pittsburgh Sleep Quality Index (PSQI). Most studies which measured burnout used the Maslach’s Burnout Inventory.
3.5. Mental Health Findings
3.5.1. Stress
Stress was the most commonly measured mental health symptom. Any one of acute stress, distress, or post-traumatic stress symptoms was examined in forty-two studies [4,24,25,26,29,30,35,38,40,44,45,49,52,53,54,56,57,58,60,62,63,64,73,74,75,76,78,80,81,82,83,84,86,87,89,90,91,92,95,96,97]. The prevalence of stress varied, and it ranged from 5% to 80%. Ten studies identified that nurses experienced more distress compared to doctors [30,38,54,63,64,80,81,82,87,91]. HCWs providing direct care to confirmed cases of SARS and COVID 19 were more likely to be distressed compared to those who did not provide direct care [30,45,53,58,63,76,78,91,92]. Moving from a low risk ward to work in a high risk ward [75], more working time per week [35], frequent changes in infection control measures and protocols [79], seeing a colleague getting sick, being intubated or dying increased stress [57] while those who received adequate social support were least likely to have PTSD [90]. Having been in quarantine during the outbreak was associated with high levels of PTSD [4,62,83]. Availability of adequate PPE significantly reduced stress [38,49,90].
3.5.2. Anxiety and Fear
Anxiety and fear symptoms were examined in 29 studies [23,25,26,27,28,29,30,32,33,34,35,36,37,40,41,42,44,45,46,48,50,51,59,64,68,88,93,96,97]. The prevalence of anxiety varied and ranged from 7% to 78% across all virus exposures. Nine studies found that HCWs who had contact with confirmed cases had more anxiety compared to HCWs who had had no contact with confirmed cases [27,30,33,34,37,44,88,97]. A common cause of anxiety was worrying about transmitting infection to family members [41,51,88]. Nurses had higher anxiety scores compared to doctors [27,30,35,37,38,50,88]. Female healthcare workers were more likely to have anxiety compared to males [26,27,30,45,46,48,56,88]. Three studies from China compared anxiety levels of HCWs in Wuhan to those of HCWs in the outreach or other regions and found that HCWs in Wuhan, which was the epicenter of COVID-19 at that time, had significantly higher anxiety compared to HCWs in other regions of China [26,30,33]. Similar results were found in Canada were HCWs in Toronto who had more contact with SARS patients had higher levels of burnout and distress compared to HCWs in Hamilton where they had fewer confirmed cases [73]. Fear and anxiety were significantly increased when a colleague became infected or died. Anxiety and fear of infection were inversely related to availability of hospital resources, HCWs’ resilience and support from family and friends [26,28]. The increase in working hours during a disease outbreak was directly related to anxiety levels [27,35]. Lack of knowledge of the virus was also associated with an increase in anxiety [59].
3.5.3. Depression
Symptoms of depression were examined in 25 studies [23,25,26,28,29,30,32,34,36,37,38,40,42,44,45,46,48,49,50,59,62,67,71,96,97]. The prevalence of depression ranged from 8.9% and 74.2%. Five studies showed that depression was higher in females compared to males [30,45,46,49,50]. The frontline medical staff working in the respiratory, emergency, ICU, and infectious disease departments were twice more likely to suffer from depression than the non-clinical staff [30,34,44]. Nurses working in SARS units were more depressed than nurses in non-SARS units [97]. The HCWs in Wuhan, which was the epicenter of the COVID-19 pandemic, had higher levels of depression compared to HCWs outside Hubei province [26,30]. Increased working hours were associated with elevated depression and hopelessness [27,35]. Having a past exposure to traumatic events or pre-existing psychiatric disorder before the epidemic was associated with high levels of depressive symptoms [62,95]. Those HCWs with a marital status of being single were more likely than married HCWs to have high levels of depressive symptoms [46,62]. A history of being quarantined was associated with higher levels of depression [62]. Support from family and friends [26,28,34], psychological preparedness, altruistic acceptance, and perceived efficacy of dealing with the pandemic was associated with lower levels of depression [46,62].
3.5.4. Insomnia and Sleep Quality
Insomnia and sleep quality was assessed in 11 studies [23,29,30,36,37,38,42,44,48,71,97]. All 11 studies reported substantial sleep problems, ranging from 26% to 45%. Insomnia was independently associated with depression and anxiety [23,42]. In three studies, insomnia symptoms were higher in frontline HCWs compared to second line workers [30,36,37,42]. Nurses reported more sleep problems compared to other HCWs [30,37,38], and nurses working in SARS units were more likely to have insomnia compared to nurses working in non-SARS units [97]. HCWs in Wuhan reported more insomnia symptoms compared to healthcare workers in other areas out of Hubei province [30].
3.5.5. Burnout (Emotional Exhaustion)
Burnout (emotional exhaustion) was assessed in eight studies, and they all confirmed high levels of burnout in HCWs [28,43,58,70,72,73,88,96]. HCWs who worked in the frontline or had contact with confirmed cases were more likely to be emotionally exhausted compared to HCWs who were not in the frontline and who had no direct contact with confirmed cases [70,72,73,88], while one study reported different results in that front-line HCWs had lower levels of burnout compared to other HCWs. The possible explanation given by the researchers for this unexpected trend was front-line HCWs had received timely and accurate information hence they had a higher sense of control of their situation [43]. Two studies showed that HCWs who had spent more time in quarantine had higher levels of burnout [70]. Lower levels of organizational support, job stress and poor hospital resources, were directly related to emotional exhaustion [58,70,72]. Burnout was negatively correlated to self-efficacy, resilience and family support [28]. High anxiety scores predicted high levels of burnout [88].
3.5.6. Stigma
Five studies examined stigma and in all studies, HCWs had been stigmatized either by their family or by the community or both [52,76,78,83,92]. The prevalence of stigma in HCWs ranged from 20% to 49%. HCWs who were working in direct contact with confirmed cases and those who had been quarantined experienced higher levels of stigma [76,92]. One study which compared psychological morbidity of stigma between general practitioners and Chinese traditional practitioners found that general practitioners had more exposure to SARS patients and suffered more stigma than the Chinese traditional practitioners [92]
4. Discussion
This review showed that epidemics and pandemics have a negative impact on the psychological wellbeing of HCWs by the wide range of mental health symptoms, in particular stress, depression, anxiety, insomnia, fear, stigma, and emotional exhaustion.
This review identified common factors that increased the risk of mental health symptoms. Frontline HCWs working in high risk environments where they had direct contact with suspected and confirmed cases of SARS and COVID 19 reported more psychological symptoms compared to non-frontline HCWs working in low risk environments [30,31,34,36,37,43,44,45,48,53,58,63,65,66,69,73,75,76,85,91,92,96]. Working in direct contact with infectious patients was associated with higher levels of symptoms of anxiety, stress, insomnia, and depression due to the increased fear of contracting infection, greater concern of infecting family members, stigmatization, and isolation [34,54,72,88]. This might explain why nurses were found to be more stressed, anxious, depressed, and had poorer sleep quality compared to doctors. Most studies explained this to be due to the higher workload that nurses have and the more time they spend in direct contact with patients whilst nursing them [27,30,37,38,41,50,54,63,72,76,80,81,82,87,88,91]. HCWs in the epicenter of a pandemic experienced more psychological distress compared to HCWs in other regions due to the higher exposure to infectious patients [26,30,33,73]. Another occupational risk factor identified was the extent of healthcare experience that a HCW had. HCWs with less work experience were more likely to be stressed compared to HCWs with more years of work experience. Less experienced HCWs have less knowledge, skills, and are less able to self-regulate, thus they get stressed more easily compared to more experienced HCWs who have more knowledge and skills, and are thus more able to adapt [53,54,96].
Inadequate hospital equipment and the limited supply of personal protective equipment (PPE) were also associated with higher levels of psychological symptoms [23,34,38,58]. Being of female gender was also identified as a risk factor [27,29,30,38,39,45,48,49,50,54,56,62,81,85,91]. A history of exposure to other traumatic events before an t outbreak increased the risk of re-occurrence of a psychiatric disorder [62,95]. Having a high perceived risk of infection and low self-efficacy were also identified as risk factors associated with mental health symptoms [49,56,62,74,87]. HCWs who were unconfident about beating the outbreak [49,56,62,74,87] were more depressed and had a poor mental state compared to HCWs who were more confident and resilient [28,77]. Lack of knowledge of the virus and lack of outbreak management training was associated with low perceived self-efficacy. Constantly changing infection control measures and documentation processes also reduced self-efficacy and caused an increase in stress levels [45]. Having been quarantined was identified as a risk factor of depressive and post-traumatic stress symptoms. This was attributed to the increased fear of dying from the disease. Quarantining was associated with increased levels of fear and stress in HCWs due to the emotional isolation and loneliness experienced during quarantine [39,62,65,67,70,77,83].
Despite the limited number of cohort studies compared to cross sectional studies, the cohort studies conducted during the SARS epidemic confirmed the persistence of mental health symptoms up to a year after the pandemic has ended.
4.1. Protective Factors
Protective factors identified in this systematic review include adequate information, clear guidelines, training and organizational support [24,43,70,71,72,78,79,95], altruistic acceptance of risk, [62,65], availability of specialized equipment for treating patients, adequate personal protective equipment [49,57,74,78,90], having more years of healthcare experience [95], adequate time off work [68], and support from family and friends [71,90].
4.2. Strengths and Limitations of This Review
The strengths of this review are, first, that it identified a large number of studies conducted during and after the epidemics and pandemics that have occurred in the past twenty years, including the current COVID-19 pandemic. Second, results are generalizable as the included studies were from Asia, Europe, Africa, Middle East, and America. Third, most papers included in this review used standardized and previously validated instruments for measuring mental health symptoms. However, a potential limitation is that we only included published articles and excluded gray literature, which might have caused some publication bias. Another limitation is that there were only five cohort studies, 94% of the studies included were cross-sectional which implies that no causal inferences can be drawn. Furthermore, meta-analyses were not undertaken because of the methodological heterogeneity of the studies.
4.3. Recommendations for Future Research and Mental Health Practice
It is important to conduct more cohort studies to obtain a detailed picture of mental health symptoms at the different points of a disease outbreak, and to understand the long-term mental health impact of a pandemic or epidemic among HCWs.
The possible role of occupation and exposure on mental health needs to be examined further in future studies. While many studies have reported higher levels of mental health problems among female HCWs, it is still unclear whether gender is a sole influencing factor, or if gender is being confounded by other factors. For instance, most of the female HCWs were nurses, and nurses experience higher mental health problems due to their increased exposure and nature of work. Besides, previous studies have shown that nurses and doctors working in the emergency department and intensive care units are at a higher risk of burnout, depression, and job stress compared to their colleagues working in other hospital departments [98,99,100]. Therefore, future studies need to rule out these aspects, while determining the effects of a pandemic or epidemic on mental health.
Increasing age, and prior chronic medical conditions make a person more susceptible to the effects of a pandemic. Therefore, in future studies, it is important to address the association between these factors and mental health outcome.
Many studies used online platforms for data collection, and this method is known to increase the risk of sampling and response bias [101]. However, we consider this method as appropriate for the current studies as face-to-face data collection was not possible due to social distancing guidelines.
As this review identified many protective factors including adequate information about the pandemic, clear guidelines and training, social support, availability of specialized equipment for treating patients, adequate personal protective equipment, adequate time off work, may be provided to the HCWs for reducing adverse mental health outcome.
5. Conclusions
This systematic review provides a comprehensive narrative synthesis of the underlying negative impacts of epidemics and pandemics on the mental health of HCWs which include acute stress, post-traumatic stress disorders, severe depression, anxiety, burnout, insomnia, and stigmatization. It is apparent from this review that the current healthcare systems and many governments across the globe need to prioritize mobilizing resources to provide sufficient and necessary psychological support to HCWs during and after epidemics and pandemics.
Author Contributions
Conceptualization, O.C.C., A.S., Z.K. and E.A. Database search, O.C.C. Screening abstracts for relevance, O.C.C. Checked the relevant studies for eligibility and extracted data from the eligible studies onto a standard Microsoft Excel data extraction form, O.C.C. Independently verified the eligibility of the included studies, A.S. Discrepancies were resolved by discussion, O.C.C., A.S. and Z.K. Critical Appraisal of studies O.C.C., A.S. Data analysis and synthesis O.C.C. Writing—original draft preparation, O.C.C.; writing—review and editing, O.C.C., A.S., Z.K. and E.A.; Visualization, O.C.C., A.S., Z.K. and E.A.; Supervision, A.S., Z.K. and E.A. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
The data presented in this study are available at (online version link).
Conflicts of Interest
The authors declare no conflict of interest.
Appendix A. Search Strategy
The search was performed from May 2020 to end-June 2020. An English language limit was applied. No restrictions were placed on the publication date and location of study. The search terms were grouped into three categories:
Category 1: Population (“healthcare professional”, “healthcare workers”, physician, doctor, nurse)
Category 2: Exposure (epidemic, pandemic)
Category 3: Outcomes (“mental health”, “mental disorder”, psychological, depression, anxiety, stress, burden, insomnia, “sleep disturbance”, burnout, fear, stigma, discrimination).
Mesh terms and synonyms of the keywords were identified and used in the search.

Table A1.
PubMed Search.
Table A1.
PubMed Search.
| Search | Query | Items Found |
|---|---|---|
| #1 | (“health personnel” OR “ healthcare provider*” OR “healthcare worker*” OR “healthcare personnel” OR “ healthcare professional*” OR “healthcare staff” OR doctor OR physician OR “physician assistant*” OR nurse OR “healthcare assistant*” OR “allied health*” OR clinician OR “hospital worker*” OR “hospital staff” OR “hospital employee*”) | 1,923,975 |
| #2 | (epidemic* OR pandemic* OR SARS OR “severe acute respiratory syndrome” OR coronavirus OR MERS OR “middle east respiratory syndrome” OR MERS-CoV OR Ebola OR EVD OR H1N1 OR “influenza type A virus” OR H7N9 OR covid-19 OR 2019-nCoV OR SARS-COV-2 OR “2019 novel coronavirus”) | 220,091 |
| #3 | mental* OR psychiatric* OR psychological* OR resilience OR depression OR emotio* OR anxiety* OR nervous* OR stress* OR PTSD OR “post-traumatic stress disorder” OR insomnia OR “sleep disorder” OR DIMS OR “ disorder of initiating and maintaining sleep” OR burnout OR exhaustion OR fear OR panic OR stigma* OR discrimination OR “mental health” | 3,376,683 |
| #4 | #1 AND #2 AND #3 | 3311 |

Table A2.
PsycArticles Search.
Table A2.
PsycArticles Search.
| Search | Query | Items Found |
|---|---|---|
| #1 | (“health personnel” OR “ healthcare provider*” OR “healthcare worker*” OR “healthcare personnel” OR “ healthcare professional*” OR “healthcare staff” OR doctor OR physician OR “physician assistant*” OR nurse OR “healthcare assistant*” OR “allied health*” OR clinician OR “hospital worker*” OR “hospital staff” OR “hospital employee*”) | 17,759 |
| #2 | (epidemic* OR pandemic* OR SARS OR “severe acute respiratory syndrome” OR coronavirus OR MERS OR “middle east respiratory syndrome” OR MERS-CoV OR Ebola OR EVD OR H1N1 OR “influenza type A virus” OR H7N9 OR covid-19 OR 2019-nCoV OR SARS-COV-2 OR “2019 novel coronavirus”) | 932 |
| #3 | mental* OR psychiatric* OR psychological* OR resilience OR depression OR emotio* OR anxiety* OR nervous* OR stress* OR PTSD OR “post-traumatic stress disorder” OR insomnia OR “sleep disorder” OR DIMS OR “ disorder of initiating and maintaining sleep” OR burnout OR exhaustion OR fear OR panic OR stigma* OR discrimination OR “mental health” | 158,189 |
| #4 | #1 AND #2 AND #3 | 117 |

Table A3.
PsycInfo Search.
Table A3.
PsycInfo Search.
| #1 | (“health personnel” OR “ healthcare provider*” OR “healthcare worker*” OR “healthcare personnel” OR “ healthcare professional*” OR “healthcare staff” OR doctor OR physician OR “physician assistant*” OR nurse OR “healthcare assistant*” OR “allied health*” OR clinician OR “hospital worker*” OR “hospital staff” OR “hospital employee*”) | 344,711 |
| #2 | epidemic* OR pandemic* OR SARS OR “severe acute respiratory syndrome” OR coronavirus OR MERS OR “middle east respiratory syndrome” OR MERS-CoV OR Ebola OR EVD OR H1N1 OR “influenza type A virus” OR H7N9 OR covid-19 OR 2019-nCoV OR SARS-COV-2 OR “2019 novel coronavirus” | 41,531 |
| #3 | mental* OR psychiatric* OR psychological* OR resilience OR depression OR emotio* OR anxiety* OR nervous* OR stress* OR PTSD OR “post-traumatic stress disorder” OR insomnia OR “sleep disorder” OR DIMS OR “ disorder of initiating and maintaining sleep” OR burnout OR exhaustion OR fear OR panic OR stigma* OR discrimination OR “mental health” | 2,335,979 |
| #4 | #1 AND #2 AND #3 | 2288 |
Appendix B. Abbreviations in Table of Results
AIS Athens Insomnia Scale, BAI Beck Anxiety Inventory, BDI-II Beck Depression Inventory II, BHS Beck Hopelessness Scale, CAPS Clinician-Administered PTSD Scale, CES-D Centre for Epidemiologic Studies Depression Scale, CHQ Chinese health Questionnaire, CHQ-12 Chinese Health Questionnaire-12, COPE Coping Orientation to Problems Experienced, DASS-21 Depression, Anxiety and Stress Scale-21, DRS-15 Dispositional Resilience Scale-15, DTS-C Davidson Trauma Scale-Chinese version, ECR-R Experiences in Close Relationships-Revised, EPQ Eysenck Personality Questionnaire, FS-HPs Fear Scale for Healthcare Professionals, GAD-7 Generalized Anxiety Disorder-7, GHQ-28 General health Questionnaire -28, HAM-A Hamilton Anxiety Score, HAMD Hamilton Depression Scale, HADS Hospital Anxiety and Depression Scale, IES-R Impact Events Scale Revised, ISI -7 Insomnia severity index-7, K-10 Kessler Psychological Distress Scale-10, K-6 Kessler Psychological Distress Scale-6, MBI Maslach Burnout Inventory, MOS SF-36 Medical Outcome Study Short-Form 36 Survey, NHSDA National Household Survey on Drug Abuse, NRS Numeric Rating Scale, OLBI Oldenburg Burnout Inventory, OSSS Oslo Social Support Scale, PCL-C PTSD Checklist-Civilian Version, PC-PTSD Primary Care PTSD screen, PHQ-12 Patient Health Questionnaire-12, PHQ-9 Patient Health Questionnaire-9, PSDI Positive Symptom Distress Index, PSQI Pittsburgh Sleep Quality Index, PSS Perceived Stress Scale, PSS-10 perceived stress scale-10, SARS NSQ SARS Nurses’ Survey Questionnaire, SAS Self-Rating Anxiety Scale, SCID Structured Clinical Interview for DSM-IV, SCL-90 The 90-item symptom checklist, SCSQ Simplified coping style questionnaire, SDS Self-Rating Depression Scale, SES Self-Efficacy Scale, SF-12 Short Form Health Survey-12, SF-36 Short Form Health Survey-36, SFS SARS Fear Scale, SRSR SARS-Related Stress Reactions questionnaire, SSI Suicidal and self-harm ideation, SOS Stress Overload Scale, SPOS Survey of Perceived Organizational Support, SRQ-20 WHO Self-Reporting Questionnaire, STAI The State-Trait Anxiety Inventory, STAXI State-Trait Anger Expression Inventory, TCSQ Trait Coping Style Questionnaire, VAS Visual Analogue Scale, WCQ Ways of Coping Questionnaire, HCW Health Care Worker, HR High Risk, LR Low Risk SL Sierra Leonne, FMW Frontline Medical Workers, GP General Practitioner, TCM Traditional Chinese medicine, SARS Severe Acute Respiratory Syndrome, MERS-CoV Middle East Respiratory Syndrome Coronavirus, COVID Coronavirus Disease A/H1N1 Influenza A Subtype H1N1, EBV Ebolavirus Disease, HCA Healthcare Assistant, FL Frontline, UW Usual wards, PPE Personal protective equipment, PTSD Post-Traumatic Stress Disorder.
References
- Sim, F.; McKee, M.; Sim, F. Issues in Public Health; McGraw-Hill Education: Maidenhead, UK, 2011; ISBN 978-0-335-24422-5. [Google Scholar]
- WHO. Disease Outbreaks. Available online: http://www.who.int/emergencies/diseases/en/ (accessed on 13 July 2020).
- Levin, P.J.; Gebbie, E.N.; Qureshi, K. Can the health-care system meet the challenge of pandemic flu? Planning, ethical, and workforce considerations. Public Health Rep. 2007, 122, 573–578. [Google Scholar] [CrossRef]
- Lee, S.M.; Kang, W.S.; Cho, A.R.; Kim, T.; Park, J.K. Psychological impact of the 2015 MERS outbreak on hospital workers and quarantined hemodialysis patients. Compr. Psychiatry 2018, 87, 123–127. [Google Scholar] [CrossRef]
- Robert, R.; Kentish-Barnes, N.; Boyer, A.; Laurent, A.; Azoulay, E.; Reignier, J. Ethical dilemmas due to the Covid-19 pandemic. Ann. Intensive Care 2020, 10, 84. [Google Scholar] [CrossRef] [PubMed]
- Rimmer, A. How can I break bad news remotely? BMJ 2020, 369. [Google Scholar] [CrossRef]
- Shortage of Personal Protective Equipment Endangering Health Workers Worldwide. Available online: https://www.who.int/news-room/detail/03-03-2020-shortage-of-personal-protective-equipment-endangering-health-workers-worldwide (accessed on 14 July 2020).
- HSE Library. Bereavement Supports for Frontline Healthcare Staff Following the Death of a Colleague Due to COVID-19? Available online: https://hselibrary.ie/bereavement-supports-for-frontline-healthcare-staff-following-the-death-of-a-colleague-due-to-covid-19/ (accessed on 14 July 2020).
- Bagcchi, S. Stigma during the COVID-19 Pandemic. Lancet Infect. Dis. 2020, 20, 782. [Google Scholar] [CrossRef]
- Ellis-Petersen, H.; Azizur Rahman, S. Indian doctors being evicted from homes over coronavirus fears. The Guardian, 30 March 2020. [Google Scholar]
- Brooks, S.K.; Dunn, R.; Amlôt, R.; Rubin, G.J.; Greenberg, N. A systematic, thematic review of social and occupational factors associated with psychological outcomes in healthcare employees during an infectious disease outbreak. J. Occup. Environ. Med. 2018, 60, 248–257. [Google Scholar] [CrossRef] [Green Version]
- Kisely, S.; Warren, N.; McMahon, L.; Dalais, C.; Henry, I.; Siskind, D. Occurrence, prevention, and management of the psychological effects of emerging virus outbreaks on healthcare workers: Rapid review and meta-analysis. BMJ 2020, 369. [Google Scholar] [CrossRef]
- Vizheh, M.; Qorbani, M.; Arzaghi, S.M.; Muhidin, S.; Javanmard, Z.; Esmaeili, M. The mental health of healthcare workers in the COVID-19 pandemic: A systematic review. J. Diabetes Metab. Disord. 2020, 1–12. [Google Scholar] [CrossRef]
- Muller, A.E.; Hafstad, E.V.; Himmels, J.P.W.; Smedslund, G.; Flottorp, S.; Stensland, S.Ø.; Stroobants, S.; Van de Velde, S.; Vist, G.E. The mental health impact of the Covid-19 pandemic on healthcare workers, and interventions to help them: A rapid systematic review. Psychiatry Res. 2020, 293, 113441. [Google Scholar] [CrossRef]
- Allan, S.M.; Bealey, R.; Birch, J.; Cushing, T.; Parke, S.; Sergi, G.; Bloomfield, M.; Meiser-Stedman, R. The prevalence of common and stress-related mental health disorders in healthcare workers based in pandemic-affected hospitals: A rapid systematic review and meta-analysis. Eur. J. Psychotraumatol. 2020, 11. [Google Scholar] [CrossRef]
- Sanghera, J.; Pattani, N.; Hashmi, Y.; Varley, K.F.; Cheruvu, M.S.; Bradley, A.; Burke, J.R. The impact of SARS-CoV-2 on the mental health of healthcare workers in a hospital setting—A systematic review. J. Occup. Health 2020, 62. [Google Scholar] [CrossRef]
- Shamseer, L.; Moher, D.; Clarke, M.; Ghersi, D.; Liberati, A.; Petticrew, M.; Shekelle, P.; Stewart, L.A. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: Elaboration and explanation. BMJ 2015, 349. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- The Impact of Epidemics and Pandemics on the Mental Health of Healthcare Workers: A Systematic Review and Narrative Synthesis. Available online: https://www.crd.york.ac.uk/prospero/display_record.php?RecordID=186331 (accessed on 16 August 2020).
- WHO. Definitions: Emergencies. Available online: https://www.who.int/hac/about/definitions/en/ (accessed on 14 September 2020).
- WHO. What Is a Pandemic? Available online: http://www.who.int/csr/disease/swineflu/frequently_asked_questions/pandemic/en/ (accessed on 14 September 2020).
- Martin, J. Critical Appraisal Checklist for Analytical Cross Sectional Studies; Joanna Briggs Institute: Brisbane, Australia, 2017; Volume 7, Available online: https://jbi.global/sites/default/files/2019-05/JBI_Critical_Appraisal-Checklist_for_Analytical_Cross_Sectional_Studies2017_0.pdf (accessed on 16 August 2020).
- Martin, J. Critical Appraisal Checklist for Cohort Studies; Joanna Briggs Institute: Brisbane, Australia, 2017; Volume 7, Available online: https://jbi.global/sites/default/files/2019-05/JBI_Critical_Appraisal-Checklist_for_Cohort_Studies2017_0.pdf (accessed on 16 August 2020).
- Amerio, A.; Bianchi, D.; Santi, F.; Costantini, L.; Odone, A.; Signorelli, C.; Costanza, A.; Serafini, G.; Amore, M.; Aguglia, A. Covid-19 pandemic impact on mental health: A web-based cross-sectional survey on a sample of Italian general practitioners. Acta Bio. Med. Atenei. Parm. 2020, 91, 83–88. [Google Scholar] [CrossRef]
- Cai, H.; Tu, B.; Ma, J.; Chen, L.; Fu, L.; Jiang, Y.; Zhuang, Q. Psychological impact and coping strategies of frontline medical staff in hunan between January and March 2020 during the outbreak of coronavirus disease 2019 (COVID-19) in Hubei, China. Med. Sci. Monit. 2020, 26, e924171-1–e924171-16. [Google Scholar] [CrossRef] [Green Version]
- Chew, N.W.S.; Lee, G.K.H.; Tan, B.Y.Q.; Jing, M.; Goh, Y.; Ngiam, N.J.H.; Yeo, L.L.L.; Ahmad, A.; Ahmed Khan, F.; Napolean Shanmugam, G.; et al. A Multinational, multicentre study on the psychological outcomes and associated physical symptoms amongst healthcare workers during COVID-19 outbreak. Brain Behav. Immun. 2020, 88, 559–565. [Google Scholar] [CrossRef]
- Du, J.; Dong, L.; Wang, T.; Yuan, C.; Fu, R.; Zhang, L.; Liu, B.; Zhang, M.; Yin, Y.; Qin, J.; et al. Psychological symptoms among frontline healthcare workers during COVID-19 outbreak in Wuhan. Gen. Hosp. Psychiatry 2020. [Google Scholar] [CrossRef]
- Hacimusalar, Y.; Kahve, A.C.; Yasar, A.B.; Aydin, M.S. Anxiety and hopelessness levels in COVID-19 pandemic: A comparative study of healthcare professionals and other community sample in Turkey. J. Psychiatr. Res. 2020, 129, 181–188. [Google Scholar] [CrossRef] [PubMed]
- Hu, D.; Kong, Y.; Li, W.; Han, Q.; Zhang, X.; Zhu, L.X.; Wan, S.W.; Liu, Z.; Shen, Q.; Yang, J.; et al. Frontline nurses’ burnout, anxiety, depression, and fear statuses and their associated factors during the COVID-19 outbreak in Wuhan, China: A large-scale cross-sectional study. EClinical Med. 2020, 24, 100424. [Google Scholar] [CrossRef] [PubMed]
- Kang, L.; Ma, S.; Chen, M.; Yang, J.; Wang, Y.; Li, R.; Yao, L.; Bai, H.; Cai, Z.; Xiang Yang, B.; et al. Impact on mental health and perceptions of psychological care among medical and nursing staff in Wuhan during the 2019 novel coronavirus disease outbreak: A cross-sectional study. Brain Behav. Immun. 2020, 87, 11–17. [Google Scholar] [CrossRef] [PubMed]
- Lai, J.; Ma, S.; Wang, Y.; Cai, Z.; Hu, J.; Wei, N.; Wu, J.; Du, H.; Chen, T.; Li, R.; et al. Factors associated with mental health outcomes among health care workers exposed to coronavirus disease 2019. JAMA Netw. Open 2020, 3, e203976. [Google Scholar] [CrossRef] [PubMed]
- Li, Z.; Ge, J.; Yang, M.; Feng, J.; Qiao, M.; Jiang, R.; Bi, J.; Zhan, G.; Xu, X.; Wang, L.; et al. Vicarious traumatization in the general public, members, and non-members of medical teams aiding in COVID-19 control. Brain Behav. Immun. 2020, 88, 916–919. [Google Scholar] [CrossRef] [PubMed]
- Liang, Y.; Chen, M.; Zheng, X.; Liu, J. Screening for Chinese medical staff mental health by SDS and SAS during the outbreak of COVID-19. J. Psychosom. Res. 2020, 133, 110102. [Google Scholar] [CrossRef] [PubMed]
- Liu, C.-Y.; Yang, Y.; Zhang, X.-M.; Xu, X.; Dou, Q.-L.; Zhang, W.-W.; Cheng, A.S.K. The prevalence and influencing factors in anxiety in medical workers fighting COVID-19 in China: A cross-sectional survey. Epidemiol. Infect. 2020, 148, e98. [Google Scholar] [CrossRef] [PubMed]
- Lu, W.; Wang, H.; Lin, Y.; Li, L. Psychological status of medical workforce during the COVID-19 pandemic: A cross-sectional study. Psychiatry Res. 2020, 288, 112936. [Google Scholar] [CrossRef]
- Mo, Y.; Deng, L.; Zhang, L.; Lang, Q.; Liao, C.; Wang, N.; Qin, M.; Huang, H. Work stress among Chinese Nurses to support wuhan in fighting against COVID-19 epidemic. J. Nurs. Manag. 2020, 28, 1002–1009. [Google Scholar] [CrossRef] [Green Version]
- Qi, J.; Xu, J.; Li, B.-Z.; Huang, J.-S.; Yang, Y.; Zhang, Z.-T.; Yao, D.-A.; Liu, Q.-H.; Jia, M.; Gong, D.-K.; et al. The Evaluation of sleep disturbances for Chinese frontline medical workers under the outbreak of COVID-19. Sleep Med. 2020, 72, 1–4. [Google Scholar] [CrossRef]
- Que, J.; Shi, L.; Deng, J.; Liu, J.; Zhang, L.; Wu, S.; Gong, Y.; Huang, W.; Yuan, K.; Yan, W.; et al. Psychological impact of the COVID-19 pandemic on healthcare workers: A cross-sectional study in China. Gen. Psychiatr 2020, 33. [Google Scholar] [CrossRef] [PubMed]
- Shechter, A.; Diaz, F.; Moise, N.; Anstey, D.E.; Ye, S.; Agarwal, S.; Birk, J.L.; Brodie, D.; Cannone, D.E.; Chang, B.; et al. Psychological distress, coping behaviors, and preferences for support among New York healthcare workers during the COVID-19 pandemic. Gen. Hosp. Psychiatry 2020, 66, 1–8. [Google Scholar] [CrossRef]
- Sun, D.; Yang, D.; Li, Y.; Zhou, J.; Wang, W.; Wang, Q.; Lin, N.; Cao, A.; Wang, H.; Zhang, Q. Psychological impact of 2019 novel coronavirus (2019-NCoV) outbreak in health workers in China. Epidemiol. Infect. 2020, 148, e96. [Google Scholar] [CrossRef] [PubMed]
- Tan, B.Y.Q.; Chew, N.W.S.; Lee, G.K.H.; Jing, M.; Goh, Y.; Yeo, L.L.L.; Zhang, K.; Chin, H.-K.; Ahmad, A.; Khan, F.A.; et al. Psychological impact of the COVID-19 pandemic on health care workers in Singapore. Ann. Intern. Med. 2020. [Google Scholar] [CrossRef] [Green Version]
- Temsah, M.-H.; Al-Sohime, F.; Alamro, N.; Al-Eyadhy, A.; Al-Hasan, K.; Jamal, A.; Al-Maglouth, I.; Aljamaan, F.; Al Amri, M.; Barry, M.; et al. The psychological impact of COVID-19 pandemic on health care workers in a MERS-CoV endemic country. J. Infect. Public Health 2020, 13, 877–882. [Google Scholar] [CrossRef] [PubMed]
- Wang, S.; Xie, L.; Xu, Y.; Yu, S.; Yao, B.; Xiang, D. Sleep disturbances among medical workers during the outbreak of COVID-2019. Occup. Med. 2020, 70, 364–369. [Google Scholar] [CrossRef] [PubMed]
- Wu, Y.; Wang, J.; Luo, C.; Hu, S.; Lin, X.; Anderson, A.E.; Bruera, E.; Yang, X.; Wei, S.; Qian, Y. A Comparison of burnout frequency among oncology physicians and nurses working on the frontline and usual wards during the COVID-19 epidemic in Wuhan, China. J. Pain Symptom Manag. 2020, 60, e60–e65. [Google Scholar] [CrossRef]
- Wu, K.; Wei, X. Analysis of psychological and sleep status and exercise rehabilitation of front-line clinical staff in the fight against COVID-19 in China. Med. Sci. Monit. Basic Res. 2020, 26, e924085. [Google Scholar] [CrossRef] [PubMed]
- Xiao, X.; Zhu, X.; Fu, S.; Hu, Y.; Li, X.; Xiao, J. Psychological impact of healthcare workers in China during COVID-19 pneumonia epidemic: A multi-center cross-sectional survey investigation. J. Affect. Disord. 2020, 274, 405–410. [Google Scholar] [CrossRef] [PubMed]
- Xiaoming, X.; Ming, A.; Su, H.; Wo, W.; Jianmei, C.; Qi, Z.; Hua, H.; Xuemei, L.; Lixia, W.; Jun, C.; et al. The psychological status of 8817 hospital workers during COVID-19 epidemic: A cross-sectional study in Chongqing. J. Affect. Disord. 2020, 276, 555–561. [Google Scholar] [CrossRef]
- Xing, J.; Sun, N.; Xu, J.; Geng, S.; Li, Y. Study of the mental health status of medical personnel dealing with new coronavirus pneumonia. PLoS ONE 2020, 15. [Google Scholar] [CrossRef] [PubMed]
- Zhang, C.; Yang, L.; Liu, S.; Ma, S.; Wang, Y.; Cai, Z.; Du, H.; Li, R.; Kang, L.; Su, M.; et al. Survey of insomnia and related social psychological factors among medical staff involved in the 2019 novel coronavirus disease outbreak. Front. Psychiatry 2020, 11. [Google Scholar] [CrossRef]
- Zhang, S.X.; Liu, J.; Afshar Jahanshahi, A.; Nawaser, K.; Yousefi, A.; Li, J.; Sun, S. At the height of the storm: Healthcare staff’s health conditions and job satisfaction and their associated predictors during the epidemic peak of COVID-19. Brain Behav. Immun. 2020, 87, 144–146. [Google Scholar] [CrossRef]
- Zhu, J.; Sun, L.; Zhang, L.; Wang, H.; Fan, A.; Yang, B.; Li, W.; Xiao, S. Prevalence and influencing factors of anxiety and depression symptoms in the first-line medical staff fighting against COVID-19 in Gansu. Front. Psychiatry 2020, 11. [Google Scholar] [CrossRef] [PubMed]
- Alsubaie, S.; Temsah, M.H.; Al-Eyadhy, A.A.; Gossady, I.; Hasan, G.M.; Al-rabiaah, A.; Jamal, A.A.; Alhaboob, A.A.; Alsohime, F.; Somily, A.M. Middle East respiratory syndrome coronavirus epidemic impact on healthcare workers’ risk perceptions, work and personal lives. J. Infect. Dev. Ctries. 2019, 13, 920–926. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Park, J.-S.; Lee, E.-H.; Park, N.-R.; Choi, Y.H. Mental health of nurses working at a government-designated hospital during a MERS-CoV outbreak: A cross-sectional study. Arch. Psychiatr. Nurs. 2018, 32, 2–6. [Google Scholar] [CrossRef] [Green Version]
- Oh, N.; Hong, N.; Ryu, D.H.; Bae, S.G.; Kam, S.; Kim, K.-Y. Exploring nursing intention, stress, and professionalism in response to infectious disease emergencies: The experience of local public hospital nurses during the 2015 MERS outbreak in South Korea. Asian Nurs Res. 2017, 11, 230–236. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tang, L.; Pan, L.; Yuan, L.; Zha, L. Prevalence and related factors of post-traumatic stress disorder among medical staff members exposed to H7N9 patients. Int. J. Nurs. Sci. 2017, 4, 63–67. [Google Scholar] [CrossRef]
- Ji, D.; Ji, Y.-J.; Duan, X.-Z.; Li, W.-G.; Sun, Z.-Q.; Song, X.-A.; Meng, Y.-H.; Tang, H.-M.; Chu, F.; Niu, X.-X.; et al. Prevalence of psychological symptoms among ebola survivors and healthcare workers during the 2014-2015 ebola outbreak in Sierra Leone: A cross-sectional study. Oncotarget 2017, 8, 12784–12791. [Google Scholar] [CrossRef] [Green Version]
- Bukhari, E.E.; Temsah, M.H.; Aleyadhy, A.A.; Alrabiaa, A.A.; Alhboob, A.A.; Jamal, A.A.; Binsaeed, A.A. Middle east respiratory syndrome coronavirus (MERS-CoV) outbreak perceptions of risk and stress evaluation in nurses. J. Infect. Dev. Ctries 2016, 10, 845–850. [Google Scholar] [CrossRef] [Green Version]
- Khalid, I.; Khalid, T.J.; Qabajah, M.R.; Barnard, A.G.; Qushmaq, I.A. Healthcare workers emotions, perceived stressors and coping strategies during a MERS-CoV outbreak. Clin. Med. Res. 2016, 14, 7–14. [Google Scholar] [CrossRef] [Green Version]
- Kim, J.S.; Choi, J.S. Factors influencing emergency nurses’ burnout during an outbreak of Middle East respiratory syndrome coronavirus in Korea. Asian Nurs Res. 2016, 10, 295–299. [Google Scholar] [CrossRef] [Green Version]
- Lehmann, M.; Bruenahl, C.A.; Addo, M.M.; Becker, S.; Schmiedel, S.; Lohse, A.W.; Schramm, C.; Löwe, B. Acute ebola virus disease patient treatment and health-related quality of life in health care professionals: A controlled study. J. Psychosom. Res. 2016, 83, 69–74. [Google Scholar] [CrossRef]
- Li, L.; Wan, C.; Ding, R.; Liu, Y.; Chen, J.; Wu, Z.; Liang, C.; He, Z.; Li, C. Mental distress among liberian medical staff working at the China ebola treatment unit: A cross sectional study. Health Qual. Life Outcomes 2015, 13, 156. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Mohammed, A.; Sheikh, T.L.; Gidado, S.; Poggensee, G.; Nguku, P.; Olayinka, A.; Ohuabunwo, C.; Waziri, N.; Shuaib, F.; Adeyemi, J.; et al. An evaluation of psychological distress and social support of survivors and contacts of Ebola virus disease infection and their relatives in Lagos, Nigeria: A cross sectional study—2014. BMC Public Health 2015, 15. [Google Scholar] [CrossRef] [Green Version]
- Liu, X.; Kakade, M.; Fuller, C.J.; Fan, B.; Fang, Y.; Kong, J.; Guan, Z.; Wu, P. Depression after exposure to stressful events: Lessons learned from the severe acute respiratory syndrome epidemic. Compr. Psychiatry 2012, 53, 15–23. [Google Scholar] [CrossRef]
- Matsuishi, K.; Kawazoe, A.; Imai, H.; Ito, A.; Mouri, K.; Kitamura, N.; Miyake, K.; Mino, K.; Isobe, M.; Takamiya, S.; et al. Psychological impact of the pandemic (H1N1) 2009 on general hospital workers in Kobe. Psychiatry Clin. Neurosci. 2012, 66, 353–360. [Google Scholar] [CrossRef]
- Goulia, P.; Mantas, C.; Dimitroula, D.; Mantis, D.; Hyphantis, T. General hospital staff worries, perceived sufficiency of information and associated psychological distress during the A/H1N1 influenza pandemic. BMC Infect. Dis 2010, 10. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wu, P.; Fang, Y.; Guan, Z.; Fan, B.; Kong, J.; Yao, Z.; Liu, X.; Fuller, C.J.; Susser, E.; Lu, J.; et al. The psychological impact of the SARS epidemic on hospital employees in China: Exposure, risk perception, and altruistic acceptance of risk. Can. J. Psychiatry 2009, 54, 302–311. [Google Scholar] [CrossRef] [PubMed]
- Styra, R.; Hawryluck, L.; Robinson, S.; Kasapinovic, S.; Fones, C.; Gold, W.L. Impact on health care workers employed in high-risk areas during the Toronto SARS outbreak. J. Psychosom. Res. 2008, 64, 177–183. [Google Scholar] [CrossRef] [PubMed]
- Wu, P.; Liu, X.; Fang, Y.; Fan, B.; Fuller, C.J.; Guan, Z.; Yao, Z.; Kong, J.; Lu, J.; Litvak, I.J. Alcohol abuse/dependence symptoms among hospital employees exposed to a SARS outbreak. Alcohol. Alcohol. 2008, 43, 706–712. [Google Scholar] [CrossRef]
- Chen, N.-H.; Wang, P.-C.; Hsieh, M.-J.; Huang, C.-C.; Kao, K.-C.; Chen, Y.-H.; Tsai, Y.-H. Impact of severe acute respiratory syndrome care on the general health status of healthcare workers in Taiwan. Infect. Control. Hosp. Epidemiol. 2007, 28, 75–79. [Google Scholar] [CrossRef]
- Lin, C.; Peng, Y.; Wu, Y.; Chang, J.; Chan, C.; Yang, D. The psychological effect of severe acute respiratory syndrome on emergency department staff. Emerg. Med. J. 2007, 24, 12–17. [Google Scholar] [CrossRef]
- Marjanovic, Z.; Greenglass, E.R.; Coffey, S. The relevance of psychosocial variables and working conditions in predicting nurses’ coping strategies during the SARS crisis: An online questionnaire survey. Int. J. Nurs. Stud. 2007, 44, 991–998. [Google Scholar] [CrossRef]
- Chen, R.; Chou, K.-R.; Huang, Y.-J.; Wang, T.-S.; Liu, S.-Y.; Ho, L.-Y. Effects of a SARS prevention programme in Taiwan on nursing staff’s anxiety, depression and sleep quality: A longitudinal survey. Int. J. Nurs. Stud. 2006, 43, 215–225. [Google Scholar] [CrossRef]
- Fiksenbaum, L.; Marjanovic, Z.; Greenglass, E.R.; Coffey, S. Emotional exhaustion and state anger in nurses who worked during the SARS outbreak: The role of perceived threat and organizational support. Can. J. Community Ment. Health 2006, 25, 89–103. [Google Scholar] [CrossRef]
- Maunder, R.G.; Lancee, W.J.; Balderson, K.E.; Bennett, J.P.; Borgundvaag, B.; Evans, S.; Fernandes, C.M.B.; Goldbloom, D.S.; Gupta, M.; Hunter, J.J.; et al. Long-term psychological and occupational effects of providing hospital healthcare during SARS outbreak. Emerg. Infect. Dis 2006, 12, 1924–1932. [Google Scholar] [CrossRef]
- Chan, S.S.C.; Leung, G.M.; Tiwari, A.F.Y.; Salili, F.; Leung, S.S.K.; Wong, D.C.N.; Wong, A.S.F.; Lai, A.S.F.; Lam, T.H.; Chan, S.S.C.; et al. The Impact of Work-Related Risk on Nurses during the SARS Outbreak in Hong Kong. Fam. Community Health 2005, 28, 274–287. [Google Scholar] [CrossRef] [PubMed]
- Chen, C.-S.; Wu, H.-Y.; Yang, P.; Yen, C.-F. Psychological distress of nurses in Taiwan who worked during the outbreak of SARS. Psychiatr. Serv. 2005, 56, 76–79. [Google Scholar] [CrossRef]
- Grace, S.L.; Hershenfield, K.; Robertson, E.; Stewart, D.E. The occupational and psychosocial impact of SARS on academic physicians in three affected hospitals. Psychosomatics 2005, 46, 385–391. [Google Scholar] [CrossRef] [PubMed]
- Ho, S.M.Y.; Kwong-Lo, R.S.Y.; Mak, C.W.Y.; Wong, J.S. Fear of severe acute respiratory syndrome (SARS) among health care workers. J. Consult. Clin. Psychol 2005, 73, 344–349. [Google Scholar] [CrossRef]
- Koh, D.; Lim, M.K.; Chia, S.E.; Ko, S.M.; Qian, F.; Ng, V.; Tan, B.H.; Wong, K.S.; Chew, W.M.; Tang, H.K.; et al. Risk perception and impact of severe acute respiratory syndrome (SARS) on work and personal lives of healthcare workers in Singapore: What can we learn? Med. Care 2005, 43, 676–682. [Google Scholar] [CrossRef]
- Lee, S.-H.; Juang, Y.-Y.; Su, Y.-J.; Lee, H.-L.; Lin, Y.-H.; Chao, C.-C. Facing SARS: Psychological impacts on SARS team nurses and psychiatric services in a Taiwan general hospital. Gen. Hosp. Psychiatry 2005, 27, 352–358. [Google Scholar] [CrossRef]
- Phua, D.H.; Tang, H.K.; Tham, K.Y. Coping responses of emergency physicians and nurses to the 2003 severe acute respiratory syndrome outbreak. Acad. Emerg. Med. 2005, 12, 322–328. [Google Scholar] [CrossRef]
- Tham, K.; Tan, Y.; Loh, O.; Tan, W.; Ong, M.; Tang, H. Psychological morbidity among emergency department doctors and nurses after the SARS outbreak. Hong Kong J. Emerg. Med. 2005, 12, 215–223. [Google Scholar] [CrossRef]
- Wong, T.W.; Yau, J.K.Y.; Chan, C.L.W.; Kwong, R.S.Y.; Ho, S.M.Y.; Lau, C.C.; Lau, F.L.; Lit, C.H. The psychological impact of severe acute respiratory syndrome outbreak on healthcare workers in emergency departments and how they cope. Eur. J. Emerg. Med. 2005, 12, 13–18. [Google Scholar] [CrossRef] [PubMed]
- Bai, Y.; Lin, C.-C.; Lin, C.-Y.; Chen, J.-Y.; Chue, C.-M.; Chou, P. Survey of stress reactions among health care workers involved with the SARS outbreak. Psychiatr. Serv. 2004, 55, 1055–1057. [Google Scholar] [CrossRef]
- Chan, A.O.M.; Huak, C.Y. Psychological impact of the 2003 severe acute respiratory syndrome outbreak on health care workers in a medium size regional general hospital in Singapore. Occup Med. 2004, 54, 190–196. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chong, M.-Y.; Wang, W.-C.; Hsieh, W.-C.; Lee, C.-Y.; Chiu, N.-M.; Yeh, W.-C.; Huang, O.-L.; Wen, J.-K.; Chen, C.-L. psychological impact of severe acute respiratory syndrome on health workers in a tertiary hospital. Br. J. Psychiatry 2004, 185, 127–133. [Google Scholar] [CrossRef] [Green Version]
- Chua, S.E.; Cheung, V.; Cheung, C.; McAlonan, G.M.; Wong, J.W.S.; Cheung, E.P.T.; Chan, M.T.Y.; Wong, M.M.C.; Tang, S.W.; Choy, K.M.; et al. Psychological effects of the SARS outbreak in Hong Kong on high-risk health care workers. Can. J. Psychiatry 2004, 49, 391–393. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Nickell, L.A.; Crighton, E.J.; Tracy, C.S.; Al-Enazy, H.; Bolaji, Y.; Hanjrah, S.; Hussain, A.; Makhlouf, S.; Upshur, R.E.G. Psychosocial effects of SARS on hospital staff: Survey of a large tertiary care institution. CMAJ 2004, 170, 793–798. [Google Scholar] [CrossRef] [Green Version]
- Poon, E.; Liu, K.; Cheong, D.; Lee, C.; Yam, L.; Tang, W. Impact of severe acute respiratory syndrome on anxiety levels of frontline health care workers. Hong Kong Med. J. 2004, 10, 325–330. [Google Scholar]
- Sim, K.; Chong, P.N.; Chan, Y.H.; Soon, W.S.W. Severe acute respiratory syndrome-related psychiatric and posttraumatic morbidities and coping responses in medical staff within a primary health care setting in Singapore. J. Clin. Psychiatry 2004, 65, 1120–1127. [Google Scholar] [CrossRef]
- Sin, S.S.; Huak, C.Y. Psychological impact of the SARS outbreak on a Singaporean rehabilitation department including commentary by Leong, I., Thompson DR. Int. J. Ther. Rehabil. 2004, 11, 417–424. [Google Scholar] [CrossRef]
- Tam, C.W.C.; Pang, E.P.F.; Lam, L.C.W.; Chiu, H.F.K. Severe acute respiratory syndrome (SARS) in Hong Kong in 2003: Stress and psychological impact among frontline healthcare workers. Psychol. Med. 2004, 34, 1197–1204. [Google Scholar] [CrossRef]
- Verma, S.; Mythily, S.; Chan, Y.H.; Deslypere, J.P.; Teo, E.K.; Chong, S.A. Post-SARS psychological morbidity and stigma among general practitioners and traditional Chinese medicine practitioners in Singapore. Ann. Acad. Med. Singap. 2004, 33, 743–748. [Google Scholar]
- Wong, W.C.W.; Lee, A.; Tsang, K.K.; Wong, S.Y.S. How did general practitioners protect themselves, their family, and staff during the SARS epidemic in Hong Kong? J. Epidemiol. Community Health 2004, 58, 180–185. [Google Scholar] [CrossRef] [Green Version]
- Lung, F.-W.; Lu, Y.-C.; Chang, Y.-Y.; Shu, B.-C. Mental symptoms in different health professionals during the SARS attack: A follow-up study. Psychiatr. Q. 2009, 80, 107–116. [Google Scholar] [CrossRef]
- Lancee, W.J.; Maunder, R.G.; Goldbloom, D.S. Prevalence of psychiatric disorders among Toronto hospital workers one to two years after the SARS outbreak. Psychiatr. Serv. 2008, 59, 91–95. [Google Scholar] [CrossRef]
- McAlonan, G.M.; Lee, A.M.; Cheung, V.; Cheung, C.; Tsang, K.W.T.; Sham, P.C.; Chua, S.E.; Wong, J.G.W.S. Immediate and sustained psychological impact of an emerging infectious disease outbreak on health care workers. Can. J. Psychiatry 2007, 52, 241–247. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Su, T.-P.; Lien, T.-C.; Yang, C.-Y.; Su, Y.L.; Wang, J.-H.; Tsai, S.-L.; Yin, J.-C. Prevalence of psychiatric morbidity and psychological adaptation of the nurses in a structured SARS caring unit during outbreak: A prospective and periodic assessment study in Taiwan. J. Psychiatr. Res. 2007, 41, 119–130. [Google Scholar] [CrossRef]
- Bardhan, R.; Heaton, K.; Davis, M.; Chen, P.; Dickinson, D.A.; Lungu, C.T. A Cross sectional study evaluating psychosocial job stress and health risk in emergency department nurses. Int. J. Environ. Res. Public Health 2019, 16, 3243. [Google Scholar] [CrossRef] [Green Version]
- Sok, S.; Sim, H.; Han, B.; Park, S.J. Burnout and related factors of nurses caring for DNR patients in intensive care units, South Korea. Int. J. Environ. Res. Public Health 2020, 17, 8899. [Google Scholar] [CrossRef] [PubMed]
- González-Cabrera, J.M.; Fernández-Prada, M.; Iribar, C.; Molina-Ruano, R.; Salinero-Bachiller, M.; Peinado, J.M. Acute stress and anxiety in medical residents on the emergency department duty. Int. J. Environ. Res. Public Health 2018, 15, 506. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wright, K.B. Researching internet-based populations: Advantages and disadvantages of online survey research, online questionnaire authoring software packages, and web survey services. J. Comput. Mediat. Commun. 2005, 10. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).