Abstract
Delirium is highly prevalent and leads to several bad outcomes for older long-term care (LTC) residents. For a more successful translation of delirium knowledge, Clinical Practice Guidelines (CPGs) tailored to LTC should be developed and applied based on the understanding of the barriers to implementation. This study was conducted to develop a CPG for delirium in LTC and to determine the barriers perceived by healthcare professionals related to the implementation of the CPG. We followed a structured, evidence- and theory-based procedure during the development process. After a systematic search, quality appraisal, and selection for eligible up-to-date CPGs for delirium, the recommendations applicable to the LTC were drafted, evaluated, and confirmed by an external group of experts. To evaluate the barriers to guideline uptake from the users’ perspectives, semi-structured interviews were conducted which resulted in four major themes: (1) a lack of resources, (2) a tendency to follow mindlines rather than guidelines, (3) passive attitudes, and (4) misunderstanding delirium care in LTC. To minimize adverse prognoses through prompt delirium care, the implementation of a CPG with an approach that comprehensively considers various barriers at the system, practice, healthcare professional, and patients/family levels is necessary.
1. Introduction
Delirium is a neuropsychiatric syndrome that manifests sudden change and fluctuation of attention, consciousness, and cognitive function [1]. It is known that older adults are particularly vulnerable to delirium due to being more likely to present representative risk factors of delirium such as older age, dementia, and reduced mobility [2]. In long-term care (LTC), where the older adult population is dominant, the prevalence of delirium reaches up to 70% and is even higher, up to 89%, in older adults with dementia [3,4]. Notably, delirium in this population is considered a medical emergency due to its negative prognosis caused by the failure to detect it early [5,6].
Delirium is often overlooked in various clinical settings, particularly in older adults [3]. There are several reasons why delirium screenings frequently fail in this population: the difficulty of differential diagnosis from delirium superimposed on dementia (DSD) or depression [7,8], the higher prevalence of persistent delirium and subsyndromal delirium (SSD) [9,10], and hypoactive delirium characterized by quiet and subtle symptoms [11]. In addition, healthcare professionals’ lack of delirium knowledge has been a major cause of underdiagnosis [12].
In LTC, unlike hospitals, the presence of an actual physician is limited, compelling all healthcare professionals who are at the bedside to play the central role in delirium management [13]. Additionally, in LTC, most residents are older adults who tend to stay for a relatively long time under the major purpose of conservative rather than active treatment, allowing them to be cared for from more long-term perspectives. These distinct contexts of LTC in many countries, as well as in Korea, make it difficult to directly apply existing Clinical Practice Guidelines (CPGs) for delirium. Furthermore, based on these features, the specific barriers related to the implementation of the CPG in this setting should be identified for more effective uptake of the CPG [14].
For a more successful translation of delirium knowledge, CPGs tailored to LTC should be applied based on the understanding of the barriers to implementation of CPGs [14]. Thus far, several delirium CPGs have been developed. However, to the best of our knowledge, there is no available CPG for delirium in LTC.
Thus, the aims of this study were set as following: (1) to develop and implement evidence-based CPGs for delirium specific to LTC and (2) to determine the barriers perceived by healthcare professionals related to the implementation of the CPGs. In this study, key questions for the development and appraisal of CPGs for delirium were written in the form of PICO (P: patient, I: intervention, C: comparison, O: outcome). “Patient” was set as older adults who are not limited to a specific treatment environment or specific patient group, “intervention” as a strategy for delirium management that includes three sub-domains: prevention, early detection, and intervention, “comparator” as conventional routine treatment, and “outcome” as usefulness and effectiveness. The key PICO questions are as follows.
- (1)
- What strategy is recommended for preventing delirium in older adults (concerning high-risk group management)?
- (2)
- What strategy is recommended for early detection of delirium in older adults?
- (3)
- What strategy is recommended for the intervention of delirium in older adults?
2. Materials and Methods
2.1. Development of the CPG
This study carried out an overall process based on the detailed steps of CAN-IMPLEMENT, which was developed by the Canadian Guideline Adaptation Study Group, using the Ottawa Model for Research Utilization (OMRU) and the Knowledge to Action (KTA) frameworks [14,15].
2.1.1. Search and Screen
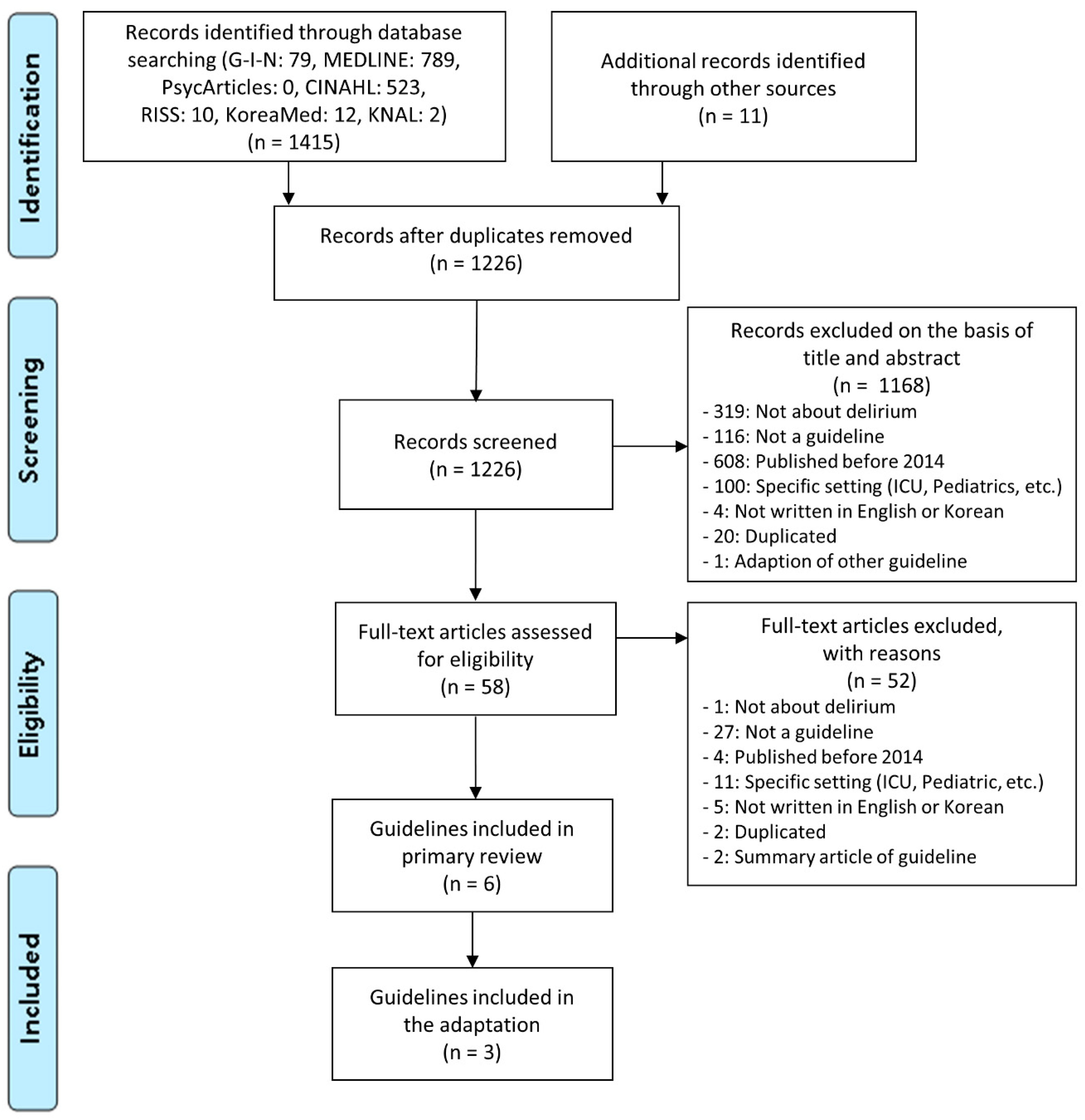
For discovering relevant CPGs, this study conducted a systematic search for CPGs with high-level evidence. The CAN-IMPLEMENT recommends using CPG search databases, country-specific databases, and the websites of guideline development organizations to collect evidence-based CPGs. Therefore, we utilized various CPG sources, including the websites of the Guidelines International Network (G-I-N), New Zealand Guideline Group (NZGG), National Institute for Health and Care Excellence (NICE), Scottish Intercollegiate Guidelines Network (SIGN), and Canadian Medical Association, as well as general databases including MEDLINE, CINAHL, PsycArticles, and Korean databases. Search terms related to “guideline” and “delirium” were used, but terms related to target patients (older adults), setting (LTC), or outcomes were not used, in order to obtain highly sensitive results. For a more extensive data search, the reference list of related studies and a Google search were also used. The CPGs were searched for and screened by two authors independently (E.J. and J.P.). The process was conducted in March 2019, and it was confirmed that there were no newly added CPGs in a repeat search following the same process in March 2020.
The selection criteria for CPGs were: (1) developed within the last five years and (2) published in English or Korean. The exclusion criteria were: (1) developed by an individual, (2) specific target setting other than LTC, such as an intensive care unit or emergency department, (3) specific target population other than older adults, (4) not an original CPG, and (5) quality assessment results of less than 50% for the Appraisal of Guidelines for Research and Evaluation II (AGREE II) [16].
2.1.2. Quality Assessment and Selection
In this step, to evaluate the quality of the CPGs, we used AGREE II, which is an evaluation tool for CPGs. AGREE II was developed with the aim of standardizing CPGs with different quality levels and measuring methodological rigor and transparency [16]. This tool consists of 23 items in six areas: scope and purpose, stakeholder involvement, rigor of development, clarity of presentation, applicability, and editorial independence. The CPGs were assessed and selected by two authors (E.J. and J.P.) independently.
2.1.3. Draft, Revise and Endorse Recommendations
For drafting recommendations, the core information of the selected CPGs was extracted using a predetermined Excel form (Table S1). In this study, recommendations were adapted based on the three PICO questions that were set in advance, and the level of evidence for each recommendation was extracted [17]. Through comparison of the detailed recommendations of each selected CPGs, only those mentioned in two or more CPGs were selected and then constructed according to the PICO questions.
For revision and confirmation of the draft, an external review was conducted by a group consisting of four experts (two professors qualified in geriatric care, a manager of LTC, and an experienced healthcare professional working in LTC for more than 10 years). For the overall evaluation of the drafted CPG, we used the questionnaire for assessments of CPGs [18], which consists of four domains: (1) guideline quality (need for a guideline on delirium, clearness of drafted CPG), (2) applicability (agreement, suitability for older LTC residents, predicted benefits and harms, acceptability of presented options, the possibility to be supported by most colleagues, expected effects), (3) acceptability (rigidity to apply, need for reorganization of services, technical concerns, economic aspects), and (4) comparative value (effectiveness, better use of resources). Additionally, each recommendation of the draft was evaluated in three domains: degree of agreement, applicability, and clinical importance, and an item was selected as significant when more than 80% agreement on it was reached.
2.2. Post-Interviews
To identify the barriers to implementation perceived by healthcare professionals, we conducted semi-structured interviews after the four-week implementation of the developed CPG in two LTC settings in South Korea. The developed CPG has been implemented by all staff including managers, nurses, social workers, physical therapists, and health assistants since May 2019. The healthcare professionals with more than three years of clinical experience, who agreed to be interviewed, were invited to participate. They were asked questions about the barriers or difficulties perceived during the implementation of the CPG. All interviews were audio-recorded and transcribed. For thematic analysis, the following six phases were applied: (1) familiarizing yourself with your data, (2) generating initial codes, (3) searching for themes, (4) reviewing themes, (5) defining and naming themes, and (6) producing the report [19].
2.3. Ethical Considerations
This study was carried out as part of the project “Development and Effectiveness of Delirium Education Program for LTC Healthcare Providers” and approved by the Ethical Committee at the university the authors belong to (KUIRB-2019-0038-01).
3. Results
3.1. Development of the CPG
3.1.1. Search and Screen
Figure 1 provides a detailed search and selection flow.
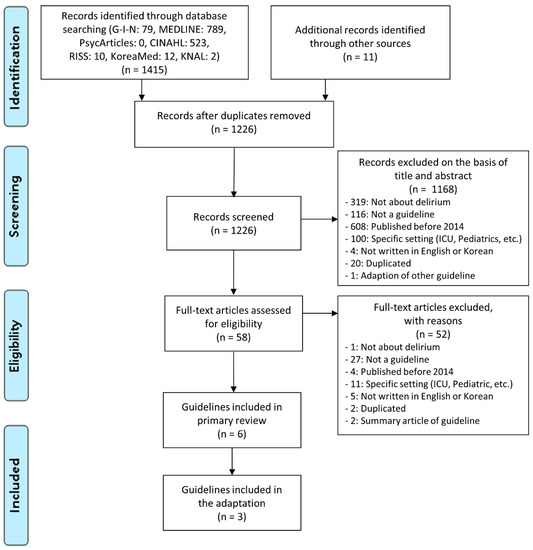
Figure 1.
Flow chart of the search for eligible CPGs. CPG, Clinical practice guideline; G-I-N, Guidelines International Network; KNAL, Korean National Assembly Library.
3.1.2. Quality Assessment and Selection
From the six CPGs included in the primary review, three that were evaluated at above 50% in quality assessment using AGREE II were included in the final review [17,20,21]. The characteristics of the included CPGs are presented in Table 1.

Table 1.
Characteristics of the included CPGs.
3.1.3. Draft, Revise, and Endorse Recommendations
Out of a total of 68 recommendations (Registered Nurses’ Association of Ontario (RNAO) = 16, NICE = 27, and SIGN = 25), after the exclusion of inapplicable ones (e.g., not possible to perform in LTC) and the integration of duplicated ones, 17 were finally selected as recommendations applicable to the clinical environment of LTC.
As a result of an external review by the expert panel, minor modifications, such as a change in wording or expressions for readability, were made. The recommendations with scores of 80% in three domains (degree of agreement, applicability, and clinical importance) were included in the final CPG. Overall evaluation using the questionnaire for assessments of CPGs also reached 80%. The final CPGs are presented in Table 2.

Table 2.
Recommendations of the developed guidelines.
3.2. Post Interviews
Ten healthcare professionals participated. They were all women, consisting of two managers, five registered nurses, three health assistants, with an average of 15.1 ± 10.7 years of clinical experience (range: 6 to 37). Face-to-face interviews, averaging 29 min in length (range: 12 to 61), were conducted between June to August 2019. A thematic analysis revealed four major themes (Table 3).

Table 3.
The perceived barriers to implementation of CPG for delirium by healthcare professionals.
4. Discussion
This study was conducted to develop a CPG for delirium in Korean LTC settings and to determine the barriers to its actual implementation. Although many CPGs for delirium have been developed globally, it is difficult to apply them directly to LTC because of different conditions, context, patient populations, and barriers related to implementation [22]. This study provided the latest evidence-based resources regarding delirium care for older LTC residents and also identified the possible barriers to consider for more effective implementation of CPG for delirium.
4.1. Recommendations of the CPG
4.1.1. Domain 1. Prevention through the Management of Risk Factors
For delirium prevention in LTC, the screening of delirium risk factors for all older adults at admission and whenever there is a change in their condition is essential (Recommendation 1) [17,20]. Since advanced age (>65 years) is a leading delirium risk factor, all older LTC residents should be considered high risk [20]. Furthermore, it should be taken into account that this population is also likely to have additional representative predisposing factors of delirium, such as multiple comorbidities, polypharmacy, and underlying cognitive impairment (Recommendation 1) [17,20].
Consequently, in LTC, all older residents should be routinely provided tailored strategies for delirium prevention via the continuous implementation of a package of multiple non-pharmacological approaches based on each individual’s risk factors, undertaken through the collaboration of a multi-disciplinary team (Recommendation 2) [17,20,21]. In addition, pharmacological risk reduction should also be applied (Recommendation 3). Notably, a systematic review of randomized controlled trials reported that a pharmacist-led medication review for LTC residents had a significant impact on decreasing delirium incidence [23]. Nevertheless, since pharmacists in this setting are in reality very limited in number, a detailed protocol for medical reviews by healthcare providers, such as nurses, who are on the front line of delirium care in this setting, should be further developed and disseminated.
4.1.2. Domain 2. Early Detection
For early detection, which is the most important factor in delirium care, it is essential to use a valid tool for screening delirium at least once a day (Recommendation 4) [17,20]. In particular, if there is an acute change or fluctuating course of cognitive functions, attention, or alertness, it should be detected using a screening tool immediately (Recommendation 4) [17,20,21]. It should also be noted that, in LTC where an older adult population is dominant, the differentiation of delirium from dementia and depression is particularly important (Recommendation 6) [17,20]. Additionally, healthcare providers should pay special attention to hypoactive delirium, which is more prevalent in this population (Recommendation 5) [20]. If delirium is suspected, it should be diagnosed by a qualified healthcare professional in a referred hospital or by attending physicians (a psychiatrist or a neurologist) who visit regularly (Recommendation 7) [17,20,21]. After delirium is diagnosed, it should be documented in the patient’s medical record and the patient and family notified. Their opinions should be respected concerning a preference for conservative rather than active management (Recommendation 8) [17,20,21].
4.1.3. Domain 3. Intervention
Healthcare providers should be aware that in most cases delirium has multiple causes and that they should systematically identify the underlying causes (Recommendation 9) [17,20,21]. When delirium is suspected or diagnosed, non-pharmacological treatment should be first implemented through multidisciplinary cooperation (Recommendation 11). The evidence of pharmacological intervention for delirium has not yet been clarified, but in the following situations—1. application of non-pharmacological intervention of delirium was ineffective, 2. the patient is distressed, or 3. there is a possibility of harming others or self)—medications for relieving delirium symptoms can be considered (Recommendation 13) [20]. Additionally, analgesics should be actively recommended for effective pain management since pain is one of the leading causes of delirium (Recommendation 14) [17].
In older adults who have not recovered after the intervention, there may be an existing cognitive impairment that may or may not have been discovered; hence, additional cognitive and physical function evaluations should be conducted (Recommendation 16) [17,20,21]. Throughout the process of delirium care, referring the patient to hospitals for appropriate follow-up by qualified healthcare professionals should be considered, if possible (Recommendation 17) [17,20,21].
Although specific recommendations about SSD, persistent delirium, and DSD were limited in the included CPGs due to a lack of evidence, healthcare providers in LTC should consider those conditions when delirium is not relieved or lasts a relatively long time [24]. Usually, the onset and course of most delirium episodes are acute and short-term, ranging from hours to days. However, the prevalence of persistent delirium that lasts several weeks to months is significantly higher in older adults [25] and even higher when including SSD, which is a partial delirium that does not fully meet the diagnostic criteria [9]. Especially in the older adults with dementia population, persistent delirium or SSD is more prevalent and has a worse prognosis [26,27]. As such, further study is necessary to create evidence-based recommendations on prevalent forms of delirium for older LTC residents, such as DSD or SSD.
In conclusion, it would be an effective strategy to apply the most important and basic recommendations (Recommendation 2, 4, 11) as a central framework for delirium management and implement the remaining recommendations together. First, preferentially, a valid tool for delirium screening should be successfully embedded in clinical practice. Among the widely used, validated, and easy-to-use (required time <5 min) tools for delirium detection, such as the 4 ‘A’ test (4AT) or Nursing delirium screening scale [28,29], an appropriate tool should be selected. Notably, the 4AT could be the first option, since SIGN recommends the tool be considered for use in community or other settings [21]. Second, an individualized care plan for delirium prevention and treatment should be developed and implemented at admission and continuously updated on a regular basis (e.g., weekly) by specific strategies suitable to each LTC context.
4.2. Barriers to Implementation of CPG
There have been some studies on barriers for delirium care conducted in the intensive care unit or palliative care [30,31], but studies in LTC settings are lacking. In this study, at the system level, a lack of resources and opportunities for delirium education was identified as a barrier to the implementation of CPG, which is in line with previous studies [30,31]. The healthcare professionals, in this study, needed delirium education and delirium screening tools applicable to LTC. Considering the limited presence of doctors who can immediately diagnosis and manage delirium in this setting, support strategies, such as the provision of more practical and detailed delirium education, and valid and simple tools for delirium detection, should be provided in the system level.
At the practice level, we identified the tendency of healthcare providers in LTC to rely on their own knowledge rather than the evidence-based guidelines as a barrier to guideline uptake. They chose to follow their own mindline rather than to follow the latest evidence-based guidelines. They regarded themselves as already familiar enough with all residents, having had no specific delirium concerns for many years. The problem revealed in this study was that managers of LTC settings, as well as other practitioners, also agreed to follow this tacit knowledge. A previous study also reported on nonreceptive organizational culture to evidence-based practice in LTC [32]. Despite the clear evidence of the benefits to LTC residents of evidence-based CPGs, their adoption in practice in LTC has remained slow and sporadic [33]. The LTC staffs, including especially the managers and administrators, need to understand why delirium practice should be improved, how the evidence-based CPG will improve practice, and what differences will be made in residents through the implementation of the CPG.
At the healthcare professionals level, the practitioners’ limited knowledge or experiences and passive attitude regarding delirium were identified as barriers to guideline uptake. Limited delirium knowledge can lead to lower confidence and passive attitudes regarding delirium care [34]. The interviewed healthcare professionals stated that there have been few delirium cases observed for many years, yet it should be noted that the reason why they observed few delirium cases might be their lack of delirium detection skills. In fact, a systematic review reported the prevalence of delirium in LTC is much lower in retrospective studies (1.75–2.3%) than overall (up to 70%) due to the possibility of many missed delirium cases by practitioners [3]. Delirium education for LTC practitioners, therefore, should be accompanied by specific strategies or tests to detect the main features of delirium that are likely to be mistaken as underlying cognitive disorders, such as how to detect inattention, altered alertness, or disorganized thinking.
At the patients/families’ level, their misunderstanding that delirium care is always an aggressive treatment was identified as a possible barrier to implementation of the CPG. Since delirium education for patients/families is recommended (Recommendation 12) [17,20], they should be informed that the main purpose of delirium care is to reduce the unfavorable prognoses of patients, such as sores, falls, and cognitive decline, and that it is essential in terms of securing the comfort and relief of suffering [5,6,35]. For improving the patients/families’ understanding, real cases of patients with experience of delirium could be helpful [17,35]. Further, educational materials should be separately developed for the residents and families based on the current best evidence of the developed CPG while reflecting their understandability and need for delirium care in LTC.
4.3. Limitations
There are some limitations in this study. First, since we only included CPGs published in English or Korean, there could be missing CPGs. Second, in this study, convenience sampling was used for the experts. However, all experts were qualified professors or healthcare professionals in the field with over 10 years of experience who could be expected to successfully evaluate the clinical applicability and feasibility of the developed CPG. Finally, the interviews for identifying barriers to implementation of the CPG were conducted in two LTC settings and all participants were female, so it might not cover all potential barriers and not be transferable to other LTC settings or LTC in other regions.
5. Conclusions
Based on the CPG developed in this study, delirium care for older LTC residents in Korea is expected to be improved. Moreover, the developed CPG could also be applied in LTC of other countries with similar contexts, patient populations, and staffing structures to Korea, with minor modifications and specific implementation strategies suitable to the local settings. The developed CPG consists of evidence-based and up-to-date recommendations that reflect the context and resources of general LTC settings. For optimal delirium management in LTC, it is also necessary to implement and continuously update the CPG based on the iterative evaluation of the barriers to implementation by involving users.
Supplementary Materials
The following are available online at https://www.mdpi.com/1660-4601/17/21/8255/s1: Table S1: Predetermined Excel Form for Data Extraction.
Author Contributions
Conceptualization, E.J. and S.O.C.; methodology, E.J., J.P. and S.O.C.; validation, E.J., J.P. and S.O.C.; formal analysis, E.J., J.P. and S.O.C.; investigation, E.J., J.P. and S.O.C.; resources, S.O.C.; data curation, E.J., J.P. and S.O.C.; writing—original draft preparation, E.J.; writing—review and editing, J.P. and S.O.C.; visualization, J.P.; supervision, S.O.C.; project administration, E.J. and S.O.C.; funding acquisition, S.O.C. All authors have read and agreed to the published version of the manuscript.
Funding
This research was supported by a National Research Foundation of Korea (NRF) grant funded by the Korean government (Ministry of Education, Science and Technology) (NRF-2017R1A2B4007896 and NRF-2019R1A2C1086122).
Acknowledgments
We thank the expert panel for their support of this study.
Conflicts of Interest
The authors declare no conflict of interest.
References
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; American Psychiatric Association: Arlington, VA, USA, 2013. [Google Scholar]
- Forsberg, M.M. Delirium update for postacute care and long-term care settings: A narrative review. J. Am. Osteopath. Assoc. 2017, 117, 32–38. [Google Scholar] [CrossRef] [PubMed]
- De Lange, E.; Verhaak, P.F.; van der Meer, K. Prevalence, presentation and prognosis of delirium in older people in the population, at home and in long term care: A review. Int. J. Geriatr. Psychiatry 2013, 28, 127–134. [Google Scholar] [CrossRef]
- Morichi, V.; Fedecostante, M.; Morandi, A.; Di Santo, S.G.; Mazzone, A.; Mossello, E.; Bo, M.; Bianchetti, A.; Rozzini, R.; Zanetti, E.; et al. A point prevalence study of delirium in italian nursing homes. Dement. Geriatr. Cogn. Disord. 2018, 46, 27–41. [Google Scholar] [CrossRef] [PubMed]
- Moon, K.J.; Park, H. Outcomes of patients with delirium in long-term care facilities: A prospective cohort study. J. Gerontol. Nurs. 2018, 44, 41–50. [Google Scholar] [CrossRef] [PubMed]
- Reynish, E.L.; Hapca, S.M.; De Souza, N.; Cvoro, V.; Donnan, P.T.; Guthrie, B. Epidemiology and outcomes of people with dementia, delirium, and unspecified cognitive impairment in the general hospital: Prospective cohort study of 10,014 admissions. BMC Med. 2017, 15, 140. [Google Scholar] [CrossRef] [PubMed]
- Brooke, J. Differentiation of delirium, dementia and delirium superimposed on dementia in the older person. Br. J. Nurs. 2018, 27, 363–367. [Google Scholar] [CrossRef] [PubMed]
- Marchington, K.L.; Carrier, L.; Lawlor, P.G. Delirium masquerading as depression. Palliat. Support. Care 2012, 10, 59–62. [Google Scholar] [CrossRef]
- Cole, M.G.; Bailey, R.; Bonnycastle, M.; McCusker, J.; Fung, S.; Ciampi, A.; Belzile, E. Frequency of full, partial and no recovery from subsyndromal deliriumin older hospital inpatients. Int. J. Geriatr. Psychiatry 2016, 31, 544–550. [Google Scholar] [CrossRef]
- Parrish, E. Delirium superimposed on dementia: Challenges and opportunities. Nurs. Clin. N. Am. 2019, 54, 541–550. [Google Scholar] [CrossRef]
- Khurana, V.; Gambhir, I.S.; Kishore, D. Evaluation of delirium in elderly: A hospital-based study. Geriatr. Gerontol. Int. 2011, 11, 467–473. [Google Scholar] [CrossRef]
- Baker, N.D.; Taggart, H.M.; Nivens, A.; Tillman, P. Delirium: Why are nurses confused? Medsurg Nurs. 2015, 24, 15–22. [Google Scholar] [PubMed]
- Lima, J.C.; Intrator, O.; Wetle, T. Physicians in nursing homes: Effectiveness of physician accountability and communication. J. Am. Med. Dir. Assoc. 2015, 16, 755–761. [Google Scholar] [CrossRef][Green Version]
- Graham, I.D.; Logan, J. Innovations in knowledge transfer and continuity of care. Can. J. Nurs. Res. 2004, 36, 89–103. [Google Scholar]
- Graham, I.D.; Logan, J.; Harrison, M.B.; Straus, S.E.; Tetroe, J.; Caswell, W.; Robinson, N. Lost in knowledge translation: Time for a map? J. Contin. Educ. Health Prof. 2006, 26, 13–24. [Google Scholar] [CrossRef]
- Brouwers, M.C.; Kho, M.E.; Browman, G.P.; Burgers, J.S.; Cluzeau, F.; Feder, G.; Fervers, B.; Graham, I.D.; Grimshaw, J.; Hanna, S.E. Agree ii: Advancing guideline development, reporting and evaluation in health care. CMAJ 2010, 182, E839–E842. [Google Scholar] [CrossRef]
- Registered Nurses’ Association of Ontario. Delirium, Dementia, and Depression in Older Adults: Assessment and Care; Registered Nurses’ Association of Ontario: Toronto, ON, USA, 2016. [Google Scholar]
- Brouwers, M.C.; Graham, I.D.; Hanna, S.E.; Cameron, D.A.; Browman, G.P. Clinicians’ assessments of practice guidelines in oncology: The capgo survey. Int. J. Technol. Assess. Health Care 2004, 20, 421–426. [Google Scholar] [CrossRef]
- Nowell, L.S.; Norris, J.M.; White, D.E.; Moules, N.J. Thematic analysis: Striving to meet the trustworthiness criteria. Int. J. Qual. Methods 2017, 16. [Google Scholar] [CrossRef]
- National Institute for Health and Care Excellence. 2018 Surveillance of Delirium: Prevention, Diagnosis and Management (Nice Guideline cg103). Available online: https://www.nice.org.uk/guidance/cg103/resources/2018-surveillance-of-delirium-prevention-diagnosis-and-management-nice-guideline-cg103-pdf-8546233843141 (accessed on 21 September 2020).
- Scottish Intercollegiate Guidelines Network (SIGN). Risk Reduction and Management of Delirium (sign 157): A National Clinical Guideline; Scottish Intercollegiate Guidelines Network: Edinburgh, UK, 2019. [Google Scholar]
- Wang, Z.; Norris, S.L.; Bero, L. The advantages and limitations of guideline adaptation frameworks. Implement. Sci. 2018, 13, 72. [Google Scholar] [CrossRef] [PubMed]
- Clegg, A.; Siddiqi, N.; Heaven, A.; Young, J.; Holt, R. Interventions for preventing delirium in older people in institutional long-term care. Cochrane Database Syst. Rev. 2014. [Google Scholar] [CrossRef]
- Kolanowski, A. Delirium in people living with dementia: A call for global solutions. Aging Ment. Health 2018, 22, 444–446. [Google Scholar] [CrossRef] [PubMed]
- Cole, M.G.; Ciampi, A.; Belzile, E.; Zhong, L. Persistent delirium in older hospital patients: A systematic review of frequency and prognosis. Age Ageing 2009, 38, 19–26. [Google Scholar] [CrossRef]
- Cole, M.G.; McCusker, J.; Voyer, P.; Monette, J.; Champoux, N.; Ciampi, A.; Belzile, E.; Vu, M. Core symptoms not meeting criteria for delirium are associated with cognitive and functional impairment and mood and behavior problems in older long-term care residents. Int. Psychogeriatr. 2014, 26, 1181–1189. [Google Scholar] [CrossRef]
- Kiely, D.K.; Marcantonio, E.R.; Inouye, S.K.; Shaffer, M.L.; Bergmann, M.A.; Yang, F.M.; Fearing, M.A.; Jones, R.N. Persistent delirium predicts greater mortality. J. Am. Geriatr. Soc. 2009, 57, 55–61. [Google Scholar] [CrossRef]
- Jeong, E.; Park, J.; Lee, J. Diagnostic test accuracy of the Nursing Delirium Screening Scale: A systematic review and meta-analysis. J. Adv. Nurs 2020, 76, 2510–2521. [Google Scholar] [CrossRef]
- Jeong, E.; Park, J.; Lee, J. Diagnostic Test Accuracy of the 4AT for Delirium Detection: A Systematic Review and Meta-Analysis. Int. J. Environ. Res. Pubblic Health 2020, 17, 7515. [Google Scholar] [CrossRef]
- Hosie, A.; Lobb, E.; Agar, M.; Davidson, P.M.; Phillips, J. Identifying the barriers and enablers to palliative care nurses’ recognition and assessment of delirium symptoms: A qualitative study. J. Pain Symptom Manag. 2014, 48, 815–830. [Google Scholar] [CrossRef]
- Rowley-Conwy, G. Barriers to delirium assessment in the intensive care unit: A literature review. Intensive Crit. Care Nurs. 2018, 44, 99–104. [Google Scholar] [CrossRef]
- Brazil, K.; Royle, J.A.; Montemuro, M.; Blythe, J.; Church, A. Moving to evidence-based practice in long-term care: The role of a best practise resource centre in two long-term care settings. J. Gerontol. Nurs. 2004, 30, 14–19. [Google Scholar] [CrossRef]
- Specht, J.K. Evidence based practice in long term care settings. J. Korean Acad. Nurs. 2013, 43, 145–153. [Google Scholar] [CrossRef]
- Jeong, E.; Chang, S.O. Exploring nurses’ recognition of delirium in the elderly by using Q-methodology. Jpn. J. Nurs. Sci. 2018, 15, 298–308. [Google Scholar] [CrossRef]
- Pollard, C.; Fitzgerald, M.; Ford, K. Delirium: The lived experience of older people who are delirious post-orthopaedic surgery. Int. J. Ment. Health Nurs. 2015, 24, 213–221. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).