The Influence of Maturity Status on Anthropometric Profile and Body Composition of Youth Goalkeepers
Abstract
1. Introduction
2. Materials and Methods
2.1. Participants
2.2. Anthropometry and Body Composition
2.3. Age and Maturity Status
2.4. Statistical Analysis
3. Results
3.1. Anthropometric Profile
3.2. Body Composition
3.3. Correlation between Years from Peak Height Velocity (YPHV) and Anthropometric Measures
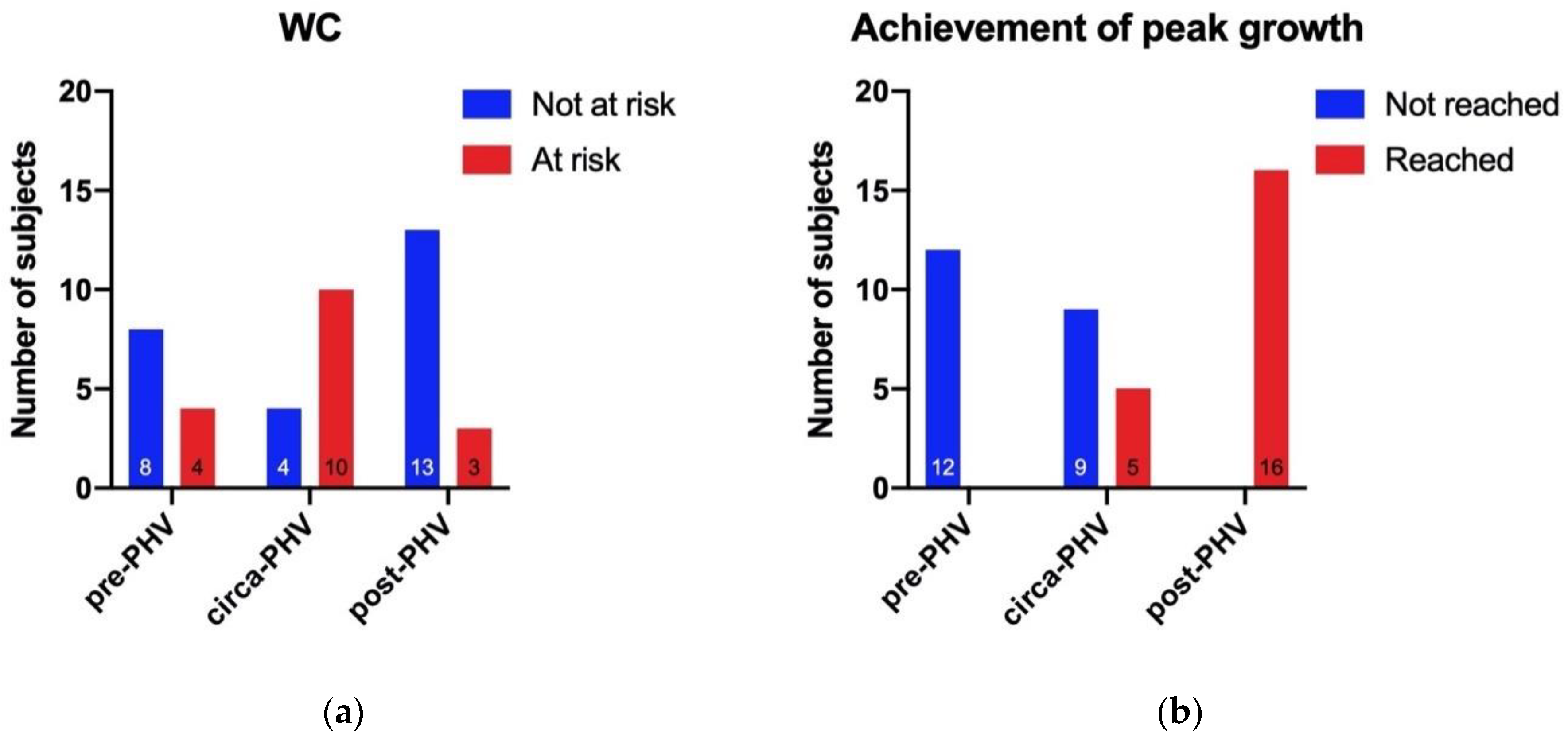
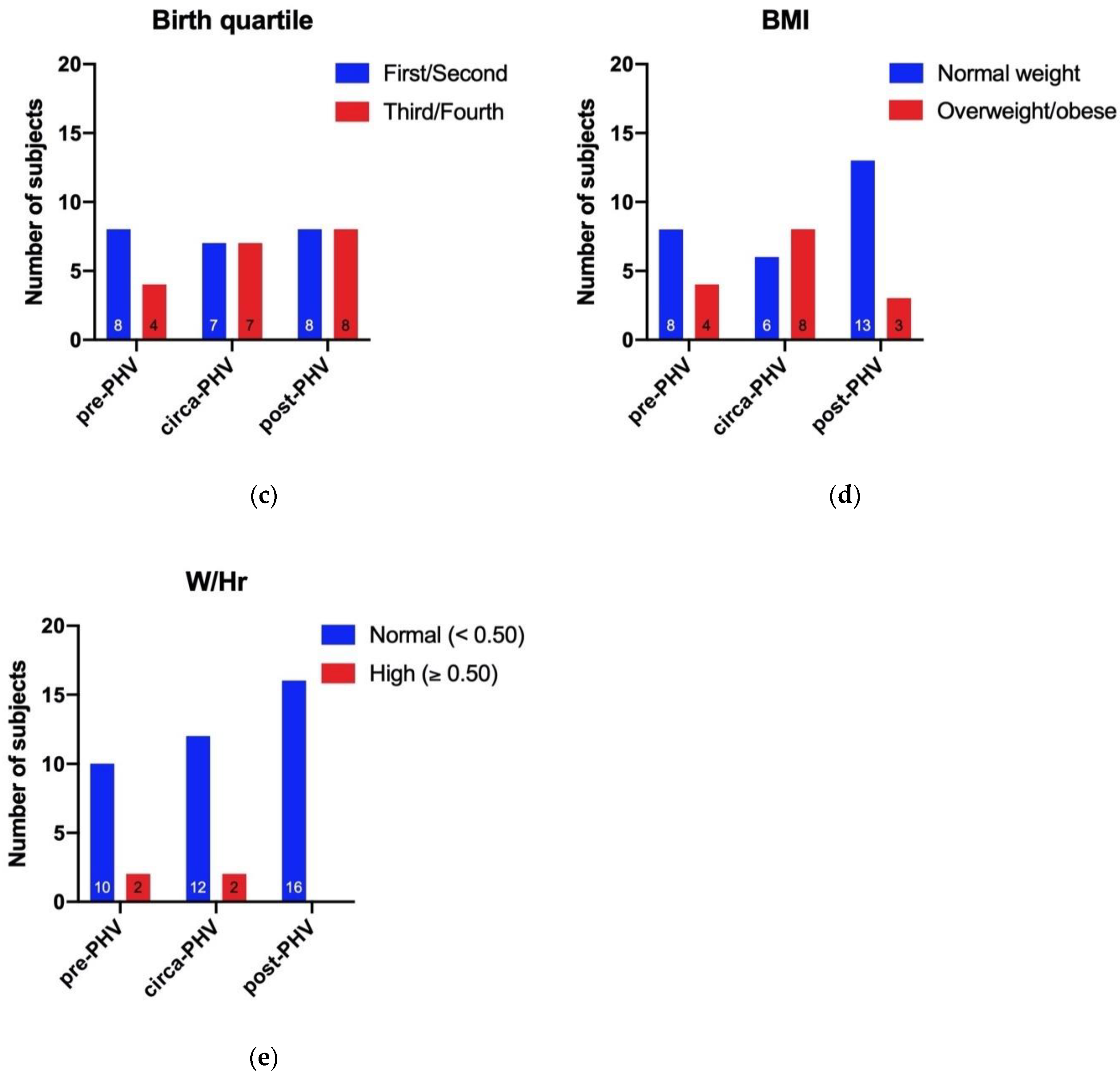
3.4. Categories for Body Mass Index (BMI), Waist Circumference (WC), Waist to Height Ratio (W/Hr), Birth Quartile, and Achievement of Peak Growth
4. Discussion
Limitations
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
References
- WHO. Physical Status: The Use and Interpretation of Anthropometry. Report of A WHO Expert Committee; World Health Organization: Geneva, Switzerland, 1995; ISBN 978-92-4-120854-3. [Google Scholar]
- Bhattacharya, A.; Pal, B.; Mukherjee, S.; Roy, S.K. Assessment of nutritional status using anthropometric variables by multivariate analysis. BMC Public Health 2019, 19. [Google Scholar] [CrossRef] [PubMed]
- Sherar, L.B.; Mirwald, R.L.; Baxter-Jones, A.D.G.; Thomis, M. Prediction of adult height using maturity-based cumulative height velocity curves. J. Pediatrics 2005, 147, 508–514. [Google Scholar] [CrossRef] [PubMed]
- Mirwald, R.L.; G. Baxter-Jones, A.D.; Bailey, D.A.; Beunen, G.P. An assessment of maturity from anthropometric measurements. Med. Sci. Sports Exerc. 2002, 34, 689–694. [Google Scholar] [CrossRef] [PubMed]
- Rinaldo, N.; Toselli, S.; Gualdi-Russo, E.; Zedda, N.; Zaccagni, L. Effects of Anthropometric Growth and Basketball Experience on Physical Performance in Pre-Adolescent Male Players. Int. J. Env. Res. Public Health 2020, 17, 2196. [Google Scholar] [CrossRef] [PubMed]
- Petri, C.; Campa, F.; Hugo Teixeira, V.; Izzicupo, P.; Galanti, G.; Pizzi, A.; Badicu, G.; Mascherini, G. Body Fat Assessment in International Elite Soccer Referees. J. Funct. Morphol. Kinesiol. 2020, 5, 38. [Google Scholar] [CrossRef]
- Högström, G.M.; Pietilä, T.; Nordström, P.; Nordström, A. Body Composition and Performance: Influence of Sport and Gender Among Adolescents. J. Strength Cond. Res. 2012, 26, 1799–1804. [Google Scholar] [CrossRef]
- Silva, A.M.; Fields, D.A.; Heymsfield, S.B.; Sardinha, L.B. Relationship Between Changes in Total-Body Water and Fluid Distribution With Maximal Forearm Strength in Elite Judo Athletes. J. Strength Cond. Res. 2011, 25, 2488–2495. [Google Scholar] [CrossRef]
- Collings, P.J.; Westgate, K.; Väistö, J.; Wijndaele, K.; Atkin, A.J.; Haapala, E.A.; Lintu, N.; Laitinen, T.; Ekelund, U.; Brage, S.; et al. Cross-Sectional Associations of Objectively-Measured Physical Activity and Sedentary Time with Body Composition and Cardiorespiratory Fitness in Mid-Childhood: The PANIC Study. Sports Med. 2017, 47, 769–780. [Google Scholar] [CrossRef]
- Lago-Peñas, C.; Casais, L.; Dellal, A.; Rey, E.; Domínguez, E. Anthropometric and Physiological Characteristics of Young Soccer Players According to Their Playing Positions: Relevance for Competition Success. J. Strength Cond. Res. 2011, 25, 3358–3367. [Google Scholar] [CrossRef]
- Figueiredo, A.J.; Gonçalves, C.E.; Coelho E Silva, M.J.; Malina, R.M. Youth soccer players, 11–14 years: Maturity, size, function, skill and goal orientation. Ann. Hum. Biol. 2009, 36, 60–73. [Google Scholar] [CrossRef] [PubMed]
- Malina, R.M.; Eisenmann, J.C.; Cumming, S.P.; Ribeiro, B.; Aroso, J. Maturity-associated variation in the growth and functional capacities of youth football (soccer) players 13–15 years. Eur. J. Appl. Physiol. 2004, 91, 555–562. [Google Scholar] [CrossRef]
- Gil, S.M.; Gil, J.; Ruiz, F.; Irazusta, A.; Irazusta, J. Physiological and Anthropometric Characteristics of Young Soccer Players According to Their Playing Position: Relevance for the Selection Process. J. Strength Cond. Res. 2007, 21, 438. [Google Scholar] [CrossRef]
- Gil, S.M.; Zabala-Lili, J.; Bidaurrazaga-Letona, I.; Aduna, B.; Lekue, J.A.; Santos-Concejero, J.; Granados, C. Talent identification and selection process of outfield players and goalkeepers in a professional soccer club. J. Sports Sci. 2014, 32, 1931–1939. [Google Scholar] [CrossRef]
- Carling, C.; Le Gall, F.; Reilly, T.; Williams, A.M. Do anthropometric and fitness characteristics vary according to birth date distribution in elite youth academy soccer players? Relative age effect in elite youth soccer. Scand. J. Med. Sci. Sports 2008, 19, 3–9. [Google Scholar] [CrossRef]
- Musch, J.; Grondin, S. Unequal Competition as an Impediment to Personal Development: A Review of the Relative Age Effect in Sport. Dev. Rev. 2001, 21, 147–167. [Google Scholar] [CrossRef]
- Helsen, W.F.; van Winckel, J.; Williams, A.M. The relative age effect in youth soccer across Europe. J. Sports Sci. 2005, 23, 629–636. [Google Scholar] [CrossRef]
- Cobley, S.; Baker, J.; Wattie, N.; McKenna, J. Annual Age-Grouping and Athlete Development: A Meta-Analytical Review of Relative Age Effects in Sport. Sports Med. 2009, 39, 235–256. [Google Scholar] [CrossRef]
- Singh, G.K.; Kogan, M.D.; Van Dyck, P.C.; Siahpush, M. Racial/Ethnic, Socioeconomic, and Behavioral Determinants of Childhood and Adolescent Obesity in the United States: Analyzing Independent and Joint Associations. Ann. Epidemiol. 2008, 18, 682–695. [Google Scholar] [CrossRef]
- Roberts, J.D.; Rodkey, L.; Ray, R.; Knight, B.; Saelens, B.E. Electronic media time and sedentary behaviors in children: Findings from the Built Environment and Active Play Study in the Washington DC area. Prev. Med. Rep. 2017, 6, 149–156. [Google Scholar] [CrossRef]
- Ala-Kitula, A.; Peltonen, J.; Finni, T.; Linnamo, V. Physical activity on days with and without soccer practice in 12–13 year-old boys. Sci. Med. Footb. 2019, 3, 245–250. [Google Scholar] [CrossRef]
- Izzicupo, P.; Di Blasio, A.; Di Credico, A.; Gaggi, G.; Vamvakis, A.; Napolitano, G.; Ricci, F.; Gallina, S.; Ghinassi, B.; Di Baldassarre, A. The Length and Number of Sedentary Bouts Predict Fibrinogen Levels in Postmenopausal Women. Int. J. Environ. Res. Public Health 2020, 17, 3051. [Google Scholar] [CrossRef] [PubMed]
- Kokkinos, P.; Sheriff, H.; Kheirbek, R. Physical Inactivity and Mortality Risk. Cardiol. Res. Pract. 2011, 2011, 1–10. [Google Scholar] [CrossRef]
- Ricci, F.; Izzicupo, P.; Moscucci, F.; Sciomer, S.; Maffei, S.; Di Baldassarre, A.; Mattioli, A.V.; Gallina, S. Recommendations for Physical Inactivity and Sedentary Behavior During the Coronavirus Disease (COVID-19) Pandemic. Front. Public Health 2020, 8. [Google Scholar] [CrossRef]
- Ceschia, A.; Giacomini, S.; Santarossa, S.; Rugo, M.; Salvadego, D.; Da Ponte, A.; Driussi, C.; Mihaleje, M.; Poser, S.; Lazzer, S. Deleterious effects of obesity on physical fitness in pre-pubertal children. Eur. J. Sport Sci. 2016, 16, 271–278. [Google Scholar] [CrossRef] [PubMed]
- Must, A.; Anderson, S.E. Body mass index in children and adolescents: Considerations for population-based applications. Int. J. Obes. 2006, 30, 590–594. [Google Scholar] [CrossRef]
- Nevill, A.M.; Stewart, A.D.; Olds, T.; Holder, R. Relationship between adiposity and body size reveals limitations of BMI. Am. J. Phys. Anthropol. 2006, 129, 151–156. [Google Scholar] [CrossRef]
- Maffeis, C.; Banzato, C.; Talamini, G. Waist-to-Height Ratio, a Useful Index to Identify High Metabolic Risk in Overweight Children. J. Pediatrics 2008, 152, 207–213.e2. [Google Scholar] [CrossRef]
- Wells, J.C.K. Measurement: A critique of the expression of paediatric body composition data. Arch. Dis. Child. 2001, 85, 67–72. [Google Scholar] [CrossRef]
- Shypailo, R.J.; Wong, W.W. Fat and fat-free mass index references in children and young adults: Assessments along racial and ethnic lines. Am. J. Clin. Nutr. 2020. [Google Scholar] [CrossRef]
- Addo, O.Y.; Himes, J.H. Reference curves for triceps and subscapular skinfold thicknesses in US children and adolescents. Am. J. Clin. Nutr. 2010, 91, 635–642. [Google Scholar] [CrossRef] [PubMed]
- de Arriba Muñoz, A.; Domínguez Cajal, M.; Rueda Caballero, C.; Labarta Aizpún, J.I.; Mayayo Dehesa, E.; Ferrández Longás, Á. Sitting height/standing height ratio in a Spanish population from birth to adulthood. Arch Argent Pediatr 2013, 111, 309–314. [Google Scholar] [CrossRef] [PubMed]
- Bedogni, G.; Iughetti, L.; Ferrari, M.; Malavolti, M.; Poli, M.; Bernasconi, S.; Battistini, N. Sensitivity and specificity of body mass index and skinfold thicknesses in detecting excess adiposity in children aged 8–12 years. Ann. Hum. Biol. 2003, 30, 132–139. [Google Scholar] [CrossRef]
- Savva, S.; Tornaritis, M.; Savva, M.; Kourides, Y.; Panagi, A.; Silikiotou, N.; Georgiou, C.; Kafatos, A. Waist circumference and waist-to-height ratio are better predictors of cardiovascular disease risk factors in children than body mass index. Int. J. Obes. 2000, 24, 1453–1458. [Google Scholar] [CrossRef]
- Ashwell, M.; Gibson, S. Waist-to-height ratio as an indicator of ‘early health risk’: Simpler and more predictive than using a ‘matrix’ based on BMI and waist circumference. BMJ Open 2016, 6, e010159. [Google Scholar] [CrossRef] [PubMed]
- Cacciari, E.; Milani, S.; Balsamo, A.; Spada, E.; Bona, G.; Cavallo, L.; Cerutti, F.; Gargantini, L.; Greggio, N.; Tonini, G.; et al. Italian cross-sectional growth charts for height, weight and BMI (2 to 20 yr). J. Endocrinol. Investig. 2006, 29, 581–593. [Google Scholar] [CrossRef]
- Opstoel, K.; Pion, J.; Elferink-Gemser, M.; Hartman, E.; Willemse, B.; Philippaerts, R.; Visscher, C.; Lenoir, M. Anthropometric Characteristics, Physical Fitness and Motor Coordination of 9 to 11 Year Old Children Participating in a Wide Range of Sports. PloS ONE 2015, 10, e0126282. [Google Scholar] [CrossRef]
- Slaughter, M.H.; Lohman, T.G.; Boileau, R.A.; Horswill, C.A.; Stillman, R.J.; Van Loan, M.D.; Bemben, D.A. Skinfold equations for estimation of body fatness in children and youth. Hum. Biol. 1988, 60, 709–723. [Google Scholar]
- McCarthy, H.; Jarrett, K.; Crawley, H. The development of waist circumference percentiles in British children aged 5.0–16.9 y. Eur. J. Clin. Nutr. 2001, 55, 902–907. [Google Scholar] [CrossRef]
- McCarthy, H.D.; Ashwell, M. A study of central fatness using waist-to-height ratios in UK children and adolescents over two decades supports the simple message—‘Keep your waist circumference to less than half your height’. Int. J. Obes. 2006, 30, 988–992. [Google Scholar] [CrossRef]
- Emmonds, S.; Morris, R.; Murray, E.; Robinson, C.; Turner, L.; Jones, B. The influence of age and maturity status on the maximum and explosive strength characteristics of elite youth female soccer players. Sci. Med. Footb. 2017, 1, 209–215. [Google Scholar] [CrossRef]
- Cohen, J. Statistical Power Analysis for the Behavioral Sciences, 2nd ed.; Routledge: New York, NY, USA, 2013; ISBN 978-0-203-77158-7. [Google Scholar]
- Schober, P.; Boer, C.; Schwarte, L.A. Correlation Coefficients: Appropriate Use and Interpretation. Anesth. Analg. 2018, 126, 1763–1768. [Google Scholar] [CrossRef]
- Loomba-Albrecht, L.A.; Styne, D.M. Effect of puberty on body composition. Curr. Opin. Endocrinol. Diabetes Obes. 2009, 16, 10–15. [Google Scholar] [CrossRef] [PubMed]
- Siervogel, R.M.; Demerath, E.W.; Schubert, C.; Remsberg, K.E.; Chumlea, W.C.; Sun, S.; Czerwinski, S.A.; Towne, B. Puberty and Body Composition. Horm. Res. Paediatr. 2003, 60, 36–45. [Google Scholar] [CrossRef]
- Xu, S.; Xue, Y. Pediatric obesity: Causes, symptoms, prevention and treatment. Exp. Ther. Med. 2016, 11, 15–20. [Google Scholar] [CrossRef]
- Kim, J.; Lim, H. Nutritional Management in Childhood Obesity. J. Obes. Metab. Syndr. 2019, 28, 225–235. [Google Scholar] [CrossRef]
- Scarafile, G. Childhood obesity in Italian primary schools: Eating habits, physical activity and perception of weight by parents. Rev. Health Care 2015, 6, 129–139. [Google Scholar] [CrossRef][Green Version]
- Robinson, T.N.; Banda, J.A.; Hale, L.; Lu, A.S.; Fleming-Milici, F.; Calvert, S.L.; Wartella, E. Screen Media Exposure and Obesity in Children and Adolescents. Pediatrics 2017, 140, S97–S101. [Google Scholar] [CrossRef]
- Huang, H.; Wan Mohamed Radzi, C.; Salarzadeh Jenatabadi, H. Family Environment and Childhood Obesity: A New Framework with Structural Equation Modeling. Int. J. Environ. Res. Public Health 2017, 14, 181. [Google Scholar] [CrossRef]
- Egan, B.; Zierath, J.R. Exercise Metabolism and the Molecular Regulation of Skeletal Muscle Adaptation. Cell Metab. 2013, 17, 162–184. [Google Scholar] [CrossRef]
- Di Credico, A.; Izzicupo, P.; Gaggi, G.; Di Baldassarre, A.; Ghinassi, B. Effect of Physical Exercise on the Release of Microparticles with Angiogenic Potential. Appl. Sci. 2020, 10, 4871. [Google Scholar] [CrossRef]
- Camera, D.M.; Smiles, W.J.; Hawley, J.A. Exercise-induced skeletal muscle signaling pathways and human athletic performance. Free Radic. Biol. Med. 2016, 98, 131–143. [Google Scholar] [CrossRef]
- Izzicupo, P.; Ghinassi, B.; D’Amico, M.A.; Di Blasio, A.; Gesi, M.; Napolitano, G.; Gallina, S.; Di Baldassarre, A. Effects of ACE I/D Polymorphism and Aerobic Training on the Immune–Endocrine Network and Cardiovascular Parameters of Postmenopausal Women. J. Clin. Endocrinol. Metab. 2013, 98, 4187–4194. [Google Scholar] [CrossRef]
- Izzicupo, P.; D’Amico, M.A.; Bascelli, A.; Di Fonso, A.; D’Angelo, E.; Di Blasio, A.; Bucci, I.; Napolitano, G.; Gallina, S.; Di Baldassarre, A. Walking training affects dehydroepiandrosterone sulfate and inflammation independent of changes in spontaneous physical activity. Menopause J. North Am. Menopause Soc. 2012, 1. [Google Scholar] [CrossRef] [PubMed]
- Gaggi, G.; Di Credico, A.; Izzicupo, P.; Antonucci, I.; Crescioli, C.; Di Giacomo, V.; Di Ruscio, A.; Amabile, G.; Alviano, F.; Di Baldassarre, A.; et al. Epigenetic Features of Human Perinatal Stem Cells Redefine Their Stemness Potential. Cells 2020, 9, 1304. [Google Scholar] [CrossRef] [PubMed]
- Falone, S.; Mirabilio, A.; Passerini, A.; Izzicupo, P.; Cacchio, M.; Gallina, S.; Baldassarre, A.D.; Amicarelli, F. Aerobic Performance and Antioxidant Protection in Runners. Int. J. Sports Med. 2009, 30, 782–788. [Google Scholar] [CrossRef] [PubMed]
- Izzicupo, P.; Di Valerio, V.; D’Amico, M.A.; Di Mauro, M.; Pennelli, A.; Falone, S.; Alberti, G.; Amicarelli, F.; Miscia, S.; Gallina, S.; et al. Nad(P)H Oxidase and Pro-Inflammatory Response during Maximal Exercise: Role of C242T Polymorphism of the P22PHOX Subunit. Int. J. Immunopathol. Pharmacol. 2010, 23, 203–211. [Google Scholar] [CrossRef]
- Filardi, T.; Ghinassi, B.; Di Baldassarre, A.; Tanzilli, G.; Morano, S.; Lenzi, A.; Basili, S.; Crescioli, C. Cardiomyopathy Associated with Diabetes: The Central Role of the Cardiomyocyte. Int. J. Mol. Sci. 2019, 20, 3299. [Google Scholar] [CrossRef]
- D’amico, M.A.; Ghinassi, B.; Izzicupo, P.; Di Ruscio, A.; Di Baldassarre, A. IL-6 Activates PI3K and PKCζ Signaling and Determines Cardiac Differentiation in Rat Embryonic H9c2 Cells: IL-6 and cardiac differentiation of H9C2 cells. J. Cell. Physiol. 2016, 231, 576–586. [Google Scholar] [CrossRef]
- Exel, J.; Mateus, N.; Travassos, B.; Gonçalves, B.; Gomes, I.; Leite, N.; Sampaio, J. Off-Training Levels of Physical Activity and Sedentary Behavior in Young Athletes: Preliminary Results during a Typical Week. Sports 2018, 6, 141. [Google Scholar] [CrossRef]
- Izzicupo, P.; Di Baldassarre, A.; Ghinassi, B.; Reichert, F.F.; Kokubun, E.; Nakamura, F.Y. Can Off-Training Physical Behaviors Influence Recovery in Athletes? A Scoping Review. Front. Physiol. 2019, 10. [Google Scholar] [CrossRef]
- Anderson, L.; Close, G.L.; Morgans, R.; Hambly, C.; Speakman, J.R.; Drust, B.; Morton, J.P. Assessment of Energy Expenditure of a Professional Goalkeeper From the English Premier League Using the Doubly Labeled Water Method. Int. J. Sports Physiol. Perform. 2019, 14, 681–684. [Google Scholar] [CrossRef]
| Pre-PHV (n = 12) | Circa-PHV (n = 14) | Post-PHV (n = 16) | ||||||
|---|---|---|---|---|---|---|---|---|
| M ±SD | Min–Max | M ±SD | Min–Max | M ±SD | Min–Max | p | η2p | |
| YPHV a,b,c | −2.02 ± 0.93 | −4.10–−1.1 | −0.26 ± 0.74 | −1.0–1.0 | 1.99 ± 0.71 | 1.10–3.60 | <0.001 | 0.822 |
| Age (years) a,b,c | 11.43 ± 1.37 | 8.80–13.04 | 12.86 ± 1.33 | 10.35–15.0 | 15.58 ± 0.62 | 14.30–16.70 | <0.001 † | - |
| Height (cm) a,b,c | 149.85 ± 7.64 | 133.30–157.70 | 166.43 ± 7.61 | 156.65–179.35 | 177.00 ± 5.22 | 171.30–189.30 | <0.001 | 0.737 |
| Weight (kg) a,b | 44.06 ± 7.88 | 25.90–54.70 | 62.66 ± 10.17 | 47.30–84.55 | 69.29 ± 10.51 | 57.80–99.00 | <0.001 | 0.551 |
| Sitting Height (cm) a,b,c | 77.23 ± 3.55 | 69.0–81.50 | 85.94 ± 4.29 | 82.0–94.0 | 92.69 ± 3.53 | 88.0–99.0 | <0.001 | 0.738 |
| Arm Span (cm) a,b,c | 152.13 ± 10.28 | 130.60–161.0 | 169.9 ± 9.11 | 159.0–185.05 | 180.13 ± 6.95 | 169.45–192.0 | <0.001 | 0.640 |
| AS/Hr | 1.02 ± 0.03 | 0.95–1.04 | 1.02 ± 0.02 | 0.99–1.05 | 1.01 ± 0.02 | 0.98–1.04 | 0.522 † | - |
| SH/Hr | 0.52 ± 0.01 | 0.50–0.54 | 0.52 ± 0.01 | 0.48–0.54 | 0.52 ± 0.01 | 0.50–0.54 | 0.330 † | - |
| Triceps Skinfold c | 13.77 ± 6.44 | 5.50–23.0 | 15.61 ± 5.91 | 5.50–25.0 | 9.97 ± 3.31 | 6.0–18.0 | 0.042 † | - |
| Subscapular Skinfold | 8.31 ± 4.88 | 3.50–20.75 | 10.36 ± 4.38 | 5.0–21.0 | 7.63 ± 1.99 | 5.0–12.75 | 0.143 † | - |
| MAC (cm) a,b | 23.68 ± 2.87 | 17.50–27.50 | 26.89 ± 4.31 | 15.90–33.90 | 28.30 ± 2.03 | 25.50–34.0 | 0.002 | 0.275 |
| MAMC (cm) a,b,c | 19.36 ± 1.59 | 15.62–22.12 | 21.99 ± 3.70 | 11.19–26.05 | 25.17 ± 1.57 | 22.63–28.35 | <0.001† | - |
| MAA (cm2) a,b | 45.26 ± 10.51 | 24.38–60.21 | 58.96 ± 17.20 | 20.13–91.50 | 64.07 ± 9.54 | 51.77–92.04 | 0.002 | 0.281 |
| MAMA (cm2) a,b,c | 30.02 ± 4.77 | 19.42–38.94 | 39.52 ± 11.17 | 9.97–54.03 | 50.63 ± 6.39 | 40.78–63.98 | <0.001 | 0.543 |
| MAFA (cm2) | 15.23 ± 7.99 | 4.97–27.47 | 19.44 ± 9.03 | 5.81–37.47 | 13.45 ± 5.13 | 7.37–28.06 | 0.168† | - |
| AFI b,c | 31.81 ± 11.26 | 15.08–45.63 | 32.79 ± 10.77 | 15.08–50.47 | 20.64 ± 5.46 | 13.00–30.94 | 0.005† | - |
| WC (cm) a,b | 66.59 ± 6.59 | 54.40–79.50 | 75.21 ± 6.96 | 62.0–87.40 | 74.09 ± 4.47 | 68.25–87.15 | 0.001 | 0.285 |
| W/Hr | 0.46 ± 0.05 | 0.39–0.55 | 0.45 ± 0.04 | 0.37–0.53 | 0.42 ± 0.02 | 0.38–0.48 | 0.029† | - |
| PAH (cm) | 180.98 ± 3.26 | 175.29–186.42 | 179.23 ± 7.88 | 166.90–190.61 | 182.16 ± 6.07 | 174.39–197.91 | 0.434 | 0.042 |
| %PAH a,b,c | 82.79 ± 3.76 | 75.28–86.62 | 92.89 ± 2.87 | 86.54–95.60 | 97.22 ± 2.97 | 87.74–99.86 | <0.001 † | - |
| BMI (kg/m2) a,b | 19.62 ± 3.38 | 13.60–26.00 | 22.57 ± 2.69 | 18.50–27.60 | 22.06 ± 2.64 | 18.90–30.0 | 0.031 | 0.163 |
| FM (kg) a,b | 8.11 ± 1.47 | 5.27–10.98 | 10.93 ± 2.22 | 7.30–14.99 | 10.33 ± 1.76 | 8.59–15.50 | 0.001 | 0.295 |
| %FM a,b,c | 18.47 ± 1.25 | 16.81–20.65 | 17.36 ± 1.27 | 15.02–19.47 | 14.87 ± 0.58 | 13.86–15.96 | <0.001† | - |
| FMI c | 3.63 ± 0.75 | 2.77–5.21 | 3.94 ± 0.68 | 2.77–5.37 | 3.29 ± 0.48 | 2.64–4.71 | 0.016† | - |
| FFMI a,b | 15.98 ± 2.69 | 10.85–20.77 | 18.61 ± 2.06 | 15.69–22.37 | 18.77 ± 2.19 | 16.06–25.33 | 0.005 | 0.235 |
| Selected Variables | Correlation with YPHV (Pearson’s r or Spearman’s Rho) | p | Lower 95% CI–Upper 95% CI |
|---|---|---|---|
| Weight | 0.767 | <0.001 | 0.604–0.869 |
| Height | 0.921 | <0.001 | 0.856–0.957 |
| Arm Span | 0.875 | <0.001 | 0.778–0.931 |
| AS/Hr | 0.138 † | 0.382 | 0.424–0.173 |
| Sitting Height | 0.941 | <0.001 | 0.892–0.968 |
| SH/Hr | 0.289 † | 0.064 | 0.017–0.545 |
| Triceps Skinfold | 0.284 † | 0.069 | 0.541–0.022 |
| Subscapular Skinfold | 0.034 † | 0.830 | 0.335–0.273 |
| MAC | 0.550 | <0.001 | 0.295–0.732 |
| MAMC | 0.809 † | <0.001 | 0.670–0.893 |
| MAA | 0.541 | <0.001 | 0.284–0.726 |
| MAMA | 0.763 | <0.001 | 0.598–0.866 |
| MAFA | 0.087 † | 0.584 | −0.381–0.223 |
| AFI | 0.437 † | 0.004 | 0.654–−0.153 |
| WC | 0.405 | 0.008 | 0.115–0.631 |
| W/Hr | 0.343 † | 0.026 | 0.586–−0.043 |
| PAH | 0.159 | 0.313 | 0.152–0.442 |
| %PAH | 0.941 † | <0.001 | 0.893–0.968 |
| BMI | 0.319 | 0.039 | 0.017–0.568 |
| FM | 0.404 | 0.008 | 0.114–0.631 |
| %FM | 0.878 † | <0.001 | 0.933–−0.783 |
| FMI | 0.260 † | 0.097 | 0.522–0.048 |
| FFMI | 0.457 | 0.002 | 0.178–0.668 |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2020 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Di Credico, A.; Gaggi, G.; Ghinassi, B.; Mascherini, G.; Petri, C.; Di Giminiani, R.; Di Baldassarre, A.; Izzicupo, P. The Influence of Maturity Status on Anthropometric Profile and Body Composition of Youth Goalkeepers. Int. J. Environ. Res. Public Health 2020, 17, 8247. https://doi.org/10.3390/ijerph17218247
Di Credico A, Gaggi G, Ghinassi B, Mascherini G, Petri C, Di Giminiani R, Di Baldassarre A, Izzicupo P. The Influence of Maturity Status on Anthropometric Profile and Body Composition of Youth Goalkeepers. International Journal of Environmental Research and Public Health. 2020; 17(21):8247. https://doi.org/10.3390/ijerph17218247
Chicago/Turabian StyleDi Credico, Andrea, Giulia Gaggi, Barbara Ghinassi, Gabriele Mascherini, Cristian Petri, Riccardo Di Giminiani, Angela Di Baldassarre, and Pascal Izzicupo. 2020. "The Influence of Maturity Status on Anthropometric Profile and Body Composition of Youth Goalkeepers" International Journal of Environmental Research and Public Health 17, no. 21: 8247. https://doi.org/10.3390/ijerph17218247
APA StyleDi Credico, A., Gaggi, G., Ghinassi, B., Mascherini, G., Petri, C., Di Giminiani, R., Di Baldassarre, A., & Izzicupo, P. (2020). The Influence of Maturity Status on Anthropometric Profile and Body Composition of Youth Goalkeepers. International Journal of Environmental Research and Public Health, 17(21), 8247. https://doi.org/10.3390/ijerph17218247









