Abstract
Osteoporosis is a major public health problem affecting millions of people worldwide. Increasing knowledge, correcting health belief and promoting osteoprotective practices are effective measures for building and maintaining strong bone throughout ones’ life-span. This review aims to summarize the contemporary evidence on the knowledge, beliefs and practice of adolescents and young adults on bone health. We performed literature searches using the PubMed and Scopus databases to identify original studies from 2008 to May 2018 using the search terms “(knowledge OR beliefs OR attitude OR practice OR behaviours OR physical activity OR exercise OR diet OR nutrition) AND (young OR youth OR adolescents OR children OR young adults OR students OR teenager) AND (osteoporosis OR bone health)”. Of the 3206 articles found, 34 met the inclusion criteria. Studies showed that most adolescents and young adults had poor knowledge and expressed disinterest in osteoporosis. They believed that other diseases were more serious than osteoporosis, contributing to low perceived susceptibility and seriousness towards this disease. Popular media emerged as a platform to obtain information regarding osteoporosis. The lack of knowledge and misconceptions about osteoporosis led to poor osteoprotective practices. As a conclusion, the current evidence revealed a lack of awareness about osteoporosis among adolescents and young adults. Educational interventions may be useful to improve the awareness of osteoporosis among this population.
Keywords:
knowledge; beliefs; behaviours; diet; physical activity; adolescents; teenager; young adults; students; osteoporosis; bone health 1. Introduction
Osteoporosis is metabolic skeletal disease, in which the bone becomes porous, brittle, and more susceptible to fractures [1]. It is an increasingly important health problem as the elderly population expands rapidly worldwide [2]. An epidemiological study estimated that 9–38% women and 1–8% men >50 years from industrialized countries suffered from osteoporosis [3]. The skeletal system is in a state of constant regeneration, through the process of bone formation and resorption. Bone formation supersedes bone resorption during growth while the reverse occurs among the middle-aged and the elderly [4]. An imbalance in bone remodelling skewing towards resorption will lead to bone loss and eventually osteoporosis.
Osteoporosis is preventable by optimizing peak bone mass during skeletal growth, preserving bone mass during adulthood, and minimizing bone loss during old age [5]. The skeletal system undergoes rapid development between early childhood and late adolescence [6]. The greatest accrual of bone mineral density happens during adolescence, representing about 60% of the bone growth in a life time [6,7,8]. Up to 90 percent of peak bone mass is acquired by the age 18 in girls and 20 in boys, which makes youth the best time to invest in ones’ bone health [9]. Since the bone density decreases with age, acquisition of peak bone mass during the first three decades and the following retention of bone through middle-age are essential determinants for reducing the risk of osteoporosis [10].
Understanding the factors that encourage osteoporosis preventive behaviours is important for the prevention of this disease at the population level. The reasons for engaging in osteoporosis preventive behaviours are complex because they are influenced by personal and social factors [11]. A study showed that social capital indirectly affected calcium intake through social support, self-efficacy for calcium intake and self-efficacy for exercise. Self-efficacy directly affected calcium intake and exercise among young adults, while self-efficacy, social support and participation in sports teams were strongly associated with bone health in adolescent girls [12]. Besides, knowledge of osteoporosis was reported to influence calcium intake and exercise indirectly through self-efficacy among students [13]. Another study suggested that identifying the barriers to calcium supplement could be one of the strategies to increase their calcium intake and reduce osteoporosis risk [14]. The study found that the leading barrier for young adults to consume calcium supplements was the lack of knowledge about the importance of increasing calcium intake, the lack of motivation to start supplements, and the belief that their dietary calcium intake alone was sufficient.
It is important to understand the knowledge, belief and practice of adolescents and young adults towards osteoporosis so that strategies to optimize their peak bone mass can be devised [15]. In addition, with proper knowledge, they can also improve the bone health of their family as they are the caretakers of senior members in their family. The current review aimed to provide a contemporary view of the knowledge, belief and practice among younger populations regarding osteoporosis. Evidence from the latest decade was summarized to update the readers on the latest findings in this field.
2. Materials and Methods
A literature search was performed from 15 April 2018 to 15 May 2018 on the PubMed and Scopus databases using keywords “(knowledge OR beliefs OR attitude OR practice OR behaviours OR physical activity OR exercise OR diet OR nutrition) AND (young OR youth OR adolescents OR children OR young adults OR students OR teenager) AND (osteoporosis OR bone health)”. All original research articles published between 2008 and May 2018 were considered to provide an up-to-date view on knowledge, attitude and practice of youths regarding bone health/osteoporosis. In this review, the definition of adolescents and young adults of World Health Organization was adopted, whereby adolescents are any person between the age of 10 and 19 years, whereas young adults are any person between 20–36 years [16].
Our literature search identified 3206 articles (2273 from PubMed and 933 from Scopus). After removing duplicated articles (n = 128), each title and abstract for potential inclusion was screened. Studies involving participants aged ≥40 years and/or did not examine knowledge, attitude or practice regarding bone health/osteoporosis as the primary objective were excluded. Only original research articles written in English or Mandarin, with the main objective to study the knowledge, awareness, beliefs and practices among adolescents or young adults regarding bone health/osteoporosis, were included in this review. The full text of eligible articles was examined. Two reviewers decided articles to be included in the review. Any discrepancies between two reviewers were resolved by discussion. Data extraction on authors (year), subjects’ characteristics, study design, major findings were performed by the same authors. A total of 34 articles which met the criteria and provided sufficient information for data extraction and were included in this review (Figure 1).
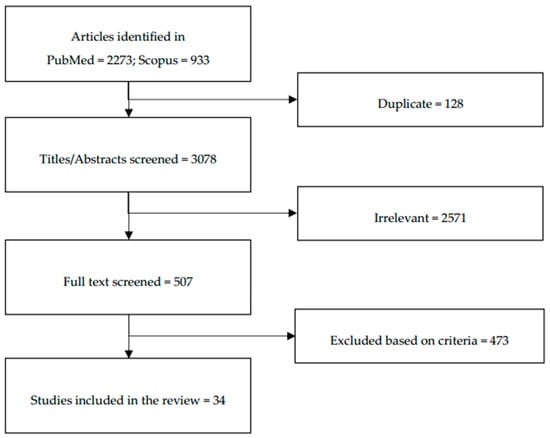
Figure 1.
Flow diagram of the stepwise selection of relevant studies.
3. Results
Thirty-four studies evaluating knowledge, attitude and practice regarding bone health/osteoporosis among adolescents and young adults were included in this review. The studies were performed in various countries and regions. The majority of the studies are from Saudi Arabia [15,17,18,19], Sri Lanka [20], Canada [21,22,23,24], Thailand [25,26] and South Korea [27,28,29,30], Jordan [31,32], Malaysia [33,34], China [35,36] and the rest are from United States [35], Nigeria [4], Taiwan [37], Syria [38], India [39], Poland [40], Denmark [41], U.K. [42], Iran [43], Pakistan [44], Columbia [45], the Basque region (Spain) [46], Japan [47] and Australia [48]. Most of the studies included in this review used either self-designed or validated questionnaire to assess the knowledge, attitude and practice among subjects regarding bone health/osteoporosis.
3.1. Knowledge Regarding Osteoporosis Among Adolescents and Young Adults
Out of the thirty-four studies, sixteen studies evaluated knowledge regarding osteoporosis. Only two studies [32,37] involved adolescents in their studies while others included young adult population. Background of the subjects varied among the studies; most of them were students from college [21,37], high school [32,37], polytechnic [4] or university [17,20,31,33,35,38,39,43,44,45]. The fields of study were medical and non-medical. Some of them were from the general population.
The knowledge level of the participants can be divided into good and poor. Four studies reported good knowledge levels among the younger generations regarding osteoporosis [31,33,37,39]. The studies recruited both male and female participants, consisting of university students [31,33,39] and a mixture of high school and college students [37]. Several factors contributed to the high level of osteoporosis knowledge among these studies. The subjects of the study of Amre et al. were nursing students. Integration of the preventive knowledge on osteoporosis into the learning and practice of the curriculum enhanced their understanding on this aspect of the disease. In comparison, they did not score well on the knowledge of pathophysiology because they did not apply this information [31]. Greater parental supervision on the bone health among Asian younger populations also contributed to a higher knowledge level on bone health [37]. Another multiracial study in Malaysia suggested that the ethnic group (Chinese) more susceptible to osteoporosis was more knowledgeable on the disease compared to the others (Malays and Indians) [33]. The students generally relied on teachers and textbooks to learn about osteoporosis [39]. These studies showed that the level of knowledge among younger generations depends on both formal education at school and parental supervision at home.
Six studies indicated that the adolescents or young adults had poor knowledge about osteoporosis [4,20,38,43,44]. From these studies, five studies [20,38,43,44] involved students from medical or health related disciplines and only one study was carried out among polytechnic students [4]. This is alarming because these students, who could be involved in the treatment and management of osteoporosis in the future, were not proficient on bone health. Gammage et al. recommended that these future health professionals should increase their knowledge on modifiable and non-modifiable risk factors of osteoporosis because most of the subjects failed to identify specific exercise related to bone health, genetic and medical conditions related to osteoporosis [21]. Part of this negligence also stemmed from the perception of the students that osteoporosis is a disease of the old age [4]. However, without adequate knowledge, the students, especially the females, would not be able to determine their own risk of developing the disease and change their health-related beliefs and behaviours [49].
Furthermore, some studies highlighted a difference in osteoporosis knowledge based on sex [17], study discipline [35] and country [45]. Alamri et al. demonstrated that female respondents were more knowledgeable compared to males, probably due to the belief that osteoporosis was a female disease [17]. A comparison study between US and Chinese university students showed that US students were more knowledgeable about osteoporosis. However, both groups were unable to identify the recommended daily calcium intake for adults [35]. Nguyen and Wang found that among health science programs, the level of education on osteoporosis differ significantly according to programs and levels of study of the students [45]. Thus, some students may not be equipped with sufficient knowledge to manage osteoporosis patients in the future.
The sources of bone health knowledge were discussed in some studies [15,25,32]. Three studies coherently indicated that the main source of knowledge regarding osteoporosis among teenagers was the television [15,25,32]. One study by Puttapitakpong et al. indicated that the internet was the second most popular source of information on bone health for teenagers [25]. This highlight the importance of media in educating adolescents and young adults about osteoporosis. The health care providers should also involve actively in osteoporosis awareness campaign through suitable channels.
A summary of the literature on the knowledge regarding osteoporosis among adolescents and young adults is listed in Table 1.

Table 1.
Knowledge regarding osteoporosis among adolescents and young adults.
3.2. Beliefs Regarding Osteoporosis among Adolescents and Young Adults
Beliefs regarding osteoporosis are also summarized in this review. The number of studies reporting high [17,21,22,35] and low [20,33,37,38,44] individual perceived susceptibility of suffering from osteoporosis was quite similar. Sex differences in beliefs regarding osteoporosis was also noted in some studies [17,21,22,35]. Three studies revealed that young women perceived higher susceptibility regarding osteoporosis than young men [21,22,35], and only one study found the inverse [17]. This could be because women are known to be more likely to develop osteoporosis [21]. Despite that, young women showed significant lower exercise efficacy as compared to men. The researchers predicted that this might be due to factors such as fewer previous experiences, less social support, and more injuries related to physical activity, especially during childhood and adolescence. A study by Shanti et al. revealed no significant differences in perceived seriousness and health motivation scores across age and gender groups [22].
Some studies reported low perceived susceptibility towards osteoporosis among adolescents or young adults [20,33,37,38,44]. Among the five studies, four involved students with medical or health related background [20,33,38,44], showing that perceived susceptibility to osteoporosis was unsatisfactory even among those with basic medical knowledge. Chen et al. suggested that age might play an important factor in the osteoporosis beliefs, especially among Asian adolescents who tend to stay with their family. They demonstrated that, in comparison with young adults, adolescents did not believe they would suffer from osteoporosis, probably due to their young age. In contrast, they obtained higher scores in seriousness and prevention of osteoporosis, probably because they lived with seniors with osteoporosis at home [37]. This was supported by another study showing that young females who had their mother with history of low trauma fracture were significantly more likely to perceive osteoporosis as a serious disease [38]. A study found that younger generations had lower perceived seriousness of osteoporosis compared to cancer and diabetes [33]. The researchers mentioned that this might be due to the misconceptions that osteoporosis is an inevitable part of ageing and it is not a lethal or serious disease [33]. Most people also considered other diseases, such as heart diseases, HIV and diabetes pose more serious health consequences than osteoporosis [33].
In some studies, despite the high perceived seriousness of osteoporosis, perceived barriers to osteoprotective behaviours remained high [23,35,38]. Among the barriers to meet the daily recommendation of calcium intake were high cost and inconvenience of milk products (packaging), as well as negative practices of dairy farmers (hormones were given to cows to encourage milk production) [23]. Cultural differences, as demonstrated between US and Chinese university students, also contributed to discrepancies between dietary and physical activity habits [35]. The typical Chinese diet consists of cereals and vegetables with a minimal intake of animal products, limiting calcium availability [50].
A summary of the literature on the beliefs regarding osteoporosis among adolescents and young adults is listed in Table 2.

Table 2.
Beliefs regarding osteoporosis among adolescents and young adults.
3.3. Practices Affecting Bone Health Among Adolescents and Young Adults
Attaining optimal peak bone mass through healthy diet and lifestyle is critical for osteoporosis prevention [51]. Among the studies, only one showed that subjects actively engaged in good dietary and lifestyle habits to maintain bone health [37]. Chen et al. showed that adolescent females had higher osteoprotective behaviour scores than young adult females in milk drinking, supplement taking and sun exposure [37]. Adolescent males scored higher in avoiding harmful behaviours such as smoking, alcohol, coffee, soft drinks consumption than young adult males [37]. This observation suggests that parental supervision may be effective in enforcing healthy behaviours among adolescents. However, the study identified patterns of behaviour rather than causes, so the predictive value of the variables could not be confirmed.
Seven other studies found that the subjects were not actively engaged in osteoprotective behaviours [15,18,20,30,32,40,44]. Only one study by Barzanji et al. recruited both sexes in their study and they indicated that females were less active physically and less exposed to the sun compared to males [15]. Hence, the investigators urged that there is a need to educate the youngsters about the importance of sunlight in maintaining optimal vitamin D level. It is also important to inform them about the most appropriate time of sun exposure during the day to protect the skin and have the benefit at the same time. Most studies indicated that adolescent females [18,32] or young adults [20,30,40,44] were not engaging in osteoprotective behaviours as evidenced by their dietary or lifestyle habits such as soft drink drinking [18], alcohol or coffee intake [30], lack of calcium intake [18,20,30,40,44] or physical activity [18,20,30,32,44] and less exposure to sun [30].
Besides calcium, vitamin D is another essential nutrient for the development and maintenance of bone. Two studies examined the effects of lifestyle on vitamin D status. Al-Daghri et al. demonstrated a widespread vitamin D deficiency in Saudi Arabian children and adults. They also noticed that frequency of fresh milk consumption was associated with vitamin D levels in the overall population and more specifically in children and female gender [19]. Tonneson et al. showed that the relative risk of vitamin D deficiency was significantly higher (p ≤ 0.001) for men (24.9%) compared with women (13.4%) from educational institutions in the Copenhagen area [41]. They also found that obese subjects; subjects who exercised 0–0.5 h a week; and subjects who consumed fast food once a week had higher risk to develop vitamin D deficiency. Smoking was also identified as a risk factor for vitamin D deficiency as chemicals from the cigarette might interfere with vitamin D metabolism [19].
A summary of the literature on the practices affecting bone health among adolescents and young adults is listed in Table 3.

Table 3.
Practices affecting bone health among adolescents and young adults.
3.4. Relationship between Knowledge, Lifestyle and Dietary Habits with Bone Health among Adolescents and Young Adults
Knowledge regarding osteoporosis was crucial in disease prevention. However, only one study reported a significant relationship between knowledge of osteoporosis with bone health indicated by QUS in young women [26]. This suggests more studies need to be done to validate the hypothesis that a higher knowledge level on osteoporosis could translate to better bone health in younger generations.
Physical activity is an important determinant of bone health among the youths [52]. The positive effects of physical activities on various aspects of bone health were illustrated in several studies [27,42]. Weight-bearing physical activity was found to increase both total hip and femoral neck bone mineral density, cortical and periosteal bone volumes in young men [42]. The larger cortical volumes might be contributed by a greater periosteal apposition among the subjects [42]. Bone-specific physical activity (BPAQ) scores was found to be positively correlated with BMD (total hip and femoral neck) of college women but not BMD at L2–L4 [28], suggesting a site-specific effect of those activities. Besides, past physical activity during adolescence was found to be as important as current physical activity for BMD in young adults [29].
Two studies indicated that avoidance of alcohol drinking and cigarette smoking were associated with better bone health [27,42]. In young men, cigarette smoking was associated with lower BMD and QUS indices, but not bone geometry [42]. Meanwhile, moderate alcohol consumption was associated with greater BMD in young men [42]. It is speculated that moderate alcohol intake stimulates the secretion of calcitonin [53] and/or the production of androstenedione by the adrenal which is converted to oestrone [54], thus explaining its bone protective effects. In contrast, Seo et al. found that the higher the alcohol use disorders identification test (AUDIT) scores, the lower the BMD of total femur and femoral neck among young women [27]. However, no significant difference in lumbar spine BMD by alcohol use was found in this study. These findings also supported the idea that the skeletal responsiveness to alcohol may differ by sites [55].
Ensuring sufficient calcium and vitamin D either from food or supplement may also help the younger generations to achieve better bone health [24,26,34,36,46,47,48]. Most studies identified a small but significant positive relationship between calcium intake and BMD or QUS indices [24,46,47,48]. One study found that subjects taking cheese regularly had a significantly higher BMD compared with non-takers [26], highlighting the importance of dairy product besides milk as a source of calcium to maintain bone health. Suriawati et al. showed that individuals with a higher intake of vitamin D alone or in combination with calcium resulted in significantly higher BMC quartiles [34]. A positive correlation between dietary vitamin D and BMD at L2–L4 had also been reported [28]. Some studies reported a negligible association between calcium and vitamin D intake and BMD or the prevalence of osteopenia [29]. This might be caused by under-reporting of the actual calcium and vitamin D intake.
Mu et al. observed a significant decreased risk of osteopenia/osteoporosis among those who practiced calcium food pattern and Chinese traditional pattern among university freshmen [36]. The results suggested that Chinese youths should adhere to a Chinese traditional dietary pattern and increase the intakes of calcium-rich food to maintain good bone health.
A summary of the literature on the relationship between knowledge of osteoporosis, lifestyle and dietary habits with bone health among adolescents and young adults is listed in Table 4.

Table 4.
Relationship between knowledge of osteoporosis, lifestyle and dietary habits with bone health among adolescents and young adults.
4. Perspectives
The present review showed that the knowledge of adolescents and young adults at school and university depends on formal education, but the general public might rely more on television and internet to learn about osteoporosis. A decrease reliance on health professionals for information on osteoporosis was also noted. Asian adolescents were also dependent on parental guidance to enforce their knowledge and osteoprotective behaviours. Hence, osteoporosis prevention should adopt a multidisciplinary approach to halt the progression of disease starting in youths. It would entail collaboration between medicine, formal education at school and informal education at home. Youths should be taught osteoprotective activities at school, and the parents should be responsible to supervise the osteoprotective habits at home. The switch of preferred health information source, from traditional and reliable sources like the health authority to the modern media calls for the involvement of the authority to engage with the youths via health promotion activities through interactive platform. It also entails health education to empower youths to differentiate between the reliable and unreliable sources of information. Although social media an option to obtain health related information, but there is a need to refer to school education program to get more accurate information.
Besides, most of the adolescents and young adults had low perceived susceptibility and seriousness of osteoporosis, leading to low practice of osteoprotective behaviours. Bone health is influenced by nutrition and lifestyle. Osteoporosis and the associated fractures are preventable by means of adequate nutrition and physical activity [56]. Lifestyle practices are formed early in life and may be carried into adulthood. There is an immediate need to increase osteoporosis awareness and subsequent beliefs, not only in elderly, but also in the younger generation. Awareness creation among the young generations is very important because, in addition to encouraging positive habits to prevent osteoporosis among them, they may also serve as agents to create awareness among their parents and the larger society [4].
Education programs can help in osteoporosis prevention. However, designing education programs for youths requires understanding on their information-seeking behaviours to ensure successful knowledge transfer [57]. One example is through the effective use of traditional and emerging social networks [57]. To address the lack of concern about future disease risk, the health promotion messages could interlace with their current interests in appearance and physical fitness. Successful health promotion should use positive wording to suggest small behavioural changes in diet and food choice that can be incorporated daily. Several education interventions have been implemented to increase the knowledge, beliefs and practices of adolescents or young adults regarding osteoporosis. These approaches include online pre-and post-intervention program [58], circuit training [59] and lecture combine with open discussion [60,61]. The outcome of the intervention was quite promising, however, to what extend that the youths will practice the osteoprotective practice might require further investigation. Besides, education programs regarding the importance of calcium and/or vitamin D have also been carried out [62,63,64]. These interventions utilize slide presentation and interactive group discussion [62], video presentation [63] or class-based nutrition intervention combining traditional lecture and interactive activities [64]. Intervention using slide presentation and interactive group discussion (8 weeks) was noticed to be less effective in changing the dietary calcium and vitamin D intake [62]. However, class-based nutrition intervention combining traditional lecture and interactive activities (15 weeks) successfully increased total milk consumption, specifically fat free milk, and encouraged the switch of milk choice favouring skim milk over low fat milk among students. A summary of the literature on education approaches carried out to improve knowledge, beliefs or practice of adolescents and young adults regarding osteoporosis were listed in Table 5.

Table 5.
Education approaches to improve knowledge, beliefs or practice of adolescents and young adults regarding osteoporosis.
There are several limitations regarding this review. Firstly, only two electronic databases were used for literature search, which might limit the number of studies found. Secondly, quality assessment of the studies included in this review is not conducted. In most studies, self-design questionnaires have been used. The reliability and validity of such questionnaires are questionable. The comparability of the studies would be enhanced if all the studies utilized a standard questionnaire for evaluating knowledge, beliefs or practice regarding osteoporosis. However, this was not possible as a myriad of questionnaires had been used. Besides, most of the studies summarized here were local data collected among certain college or university students, hence the results cannot be generalized for the whole nation. Although some of the study participants indicated that they engaged in osteoprotective behaviours, their dietary and supplement intake of nutrients important to bone, duration of physical activities was not explored further. Although some studies showed that participants had poor osteoporosis knowledge, health beliefs and practice on osteoporosis, it was not sure these factors translated to a poorer bone health. Thus, longitudinal studies are needed to examine changes in osteoprotective behaviours and their effects on bone health. A successful intervention program requires the cooperation of public with the researchers. Educational programs are important to deliver general and preventive knowledge of osteoporosis to the public. However, the public need to be motivated to change their diet or health habits to achieve a healthy lifestyle and prevent themselves from getting osteoporosis.
5. Conclusions
Adolescents and young adults have poor knowledge regarding osteoporosis. The lack of knowledge regarding osteoporosis leads to low perceived susceptibility and seriousness of osteoporosis. This is because the younger generations think that osteoporosis is a disease affecting only elderly. Perceptions of personal susceptibility and belief in the seriousness of a disease will influence behavioural change in disease prevention. Parental supervision is critical in assuring the practice of osteoprotective behaviours among the adolescents. Healthcare workers may play an important role in planning health education intervention strategies that are suitable for the younger generation to increase their awareness regarding osteoporosis.
Author Contributions
C.C.Y. performed the literature search and drafted the manuscript. N.M., S.I.-N. and K.-Y.C provided critical reviews of the manuscript. K.-Y.C. gave the final approval for the submission and publication of this manuscript.
Funding
We thank Universiti Kebangsaan Malaysia for supporting the study with grants GUP-2016–060 and AP-2017-009/1.
Conflicts of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
- Yamamoto, K. Definition and diagnostic criteria of osteoporosis in Japan. Clin. Calcium 2001, 11, 19–24. [Google Scholar] [PubMed]
- Svedbom, A.; Ivergård, M.; Hernlund, E.; Rizzoli, R.; Kanis, J.A. Epidemiology and economic burden of osteoporosis in Switzerland. Arch. Osteoporos. 2014, 9, 187. [Google Scholar] [CrossRef] [PubMed]
- Wade, S.W.; Strader, C.; Fitzpatrick, L.A.; Anthony, M.S.; O’Malley, C.D. Estimating prevalence of osteoporosis: Examples from industrialized countries. Arch. Osteoporos. 2014, 9, 182. [Google Scholar] [CrossRef] [PubMed]
- Njeze Ngozi, R.; Ikechukwu, O.; Miriam, A.; Olanike, A.-U.; Akpagbula Ulugo, D.; Njeze Nneze, C. Awareness of Osteoporosis in a Polytechnic in Enugu, South East Nigeria. Arch. Osteoporos. 2017, 12, 51. [Google Scholar] [CrossRef] [PubMed]
- NIH Consensus Development Panel. Osteoporosis Prevention, Diagnosis, and Therapy. JAMA 2001, 285, 785–795. [Google Scholar] [CrossRef]
- Stagi, S.; Cavalli, L.; Iurato, C.; Seminara, S.; Brandi, M.L.; de Martino, M. Bone metabolism in children and adolescents: Main characteristics of the determinants of peak bone mass. Clin. Cases Miner. Bone Metab. 2013, 10, 172–179. [Google Scholar] [PubMed]
- O’Brien, M. Exercise and osteoporosis. Irish J. Med. Sci. 2001, 170, 58–62. [Google Scholar] [CrossRef] [PubMed]
- McKay, H.A.; Bailey, D.A.; Mirwald, R.L.; Davison, K.S.; Faulkner, R.A. Peak bone mineral accrual and age at menarche in adolescent girls: A 6-year longitudinal study. J. Pediatr. 1998, 133, 682–687. [Google Scholar] [CrossRef]
- Wahba, S.A.; El-shaheed, A.A.; Tawheed, M.S.; Mekkawy, A.A. Osteoporosis knowledge, beliefs, and behaviours among Egyption female students. JASMR 2010, 5, 173–180. [Google Scholar]
- Bollenbacher, V.A. Effects of an Osteoporosis Educational Intervention: Knowledge and Self-Efficacy of Prevention in Young Adult Collegiate Females. Valpo Scholar. 2014. Available online: https://scholar.valpo.edu/cgi/viewcontent.cgi?article=1056&context=ebpr (accessed on 26 February 2018).
- Hsieh, C.H.; Wang, C.Y.; McCubbin, M.; Zhang, S.; Inouye, J. Factors influencing osteoporosis preventive behaviours: Testing a path model. J. Adv. Nurs. 2008, 62, 336–345. [Google Scholar] [CrossRef] [PubMed]
- Sharma, S.V.; Hoelscher, D.M.; Kelder, S.H.; Diamond, P.; Day, R.S. Hergenroeder, a psychosocial factors influencing calcium intake and bone quality in middle school girls. J. Am. Diet. Assoc. 2010, 110, 932–936. [Google Scholar] [CrossRef] [PubMed]
- Piaseu, N.; Schepp, K.; Belza, B. Causal analysis of exercise and calcium intake behaviours for osteoporosis prevention among young women in Thailand. Health Care Women Int. 2002, 23, 364–376. [Google Scholar] [CrossRef] [PubMed]
- Tyler, C.V.; Werner, J.J.; Panaite, V.; Snyder, S.M.; Ford, D.B.; Conway, J.L.; Young, C.W.; Powell, B.L.; Smolak, M.J.; Zyzanski, S.J. Barriers to supplemental calcium use among women in suburban family practice: A report from the cleveland clinic ambulatory research network (CleAR-eN). JABFM 2008, 21, 293–299. [Google Scholar] [CrossRef] [PubMed]
- Barzanji, A.T.; Alamri, F.A.; Mohamed, A.G. Osteoporosis: A study of knowledge, attitude and practice among adults in Riyadh, Saudi Arabia. J. Community Health 2013, 38, 1098–1105. [Google Scholar] [CrossRef] [PubMed]
- WHO. Health Topics: Adolescent Health. Available online: http://www.who.int/topics/adolescent_health/en/ (accessed on 1 May 2018).
- Alamri, F.A.; Saeedi, M.Y.; Mohamed, A.; Barzanii, A.; Aldayel, M.; Ibrahim, A.K. Knowledge, attitude, and practice of osteoporosis among Saudis. J. Egypt. Publ. Health Assoc. 2015, 90, 171–177. [Google Scholar] [CrossRef] [PubMed]
- Al-Raddadi, R.; Bahijri, S.; Borai, A.; AlRaddadi, Z. Prevalence of lifestyle practices that might affect bone health in relation to vitamin D status among female Saudi adolescents. Nutrition 2018, 45, 108–113. [Google Scholar] [CrossRef] [PubMed]
- Al-daghri, N.M.; Aljohani, N.; Al-attas, O.S.; Krishnaswamy, S.; Alfawaz, H. Dairy products consumption and serum 25-hydroxyvitamin D level in Saudi children and adults. Int. J. Clin. Exp. Pathol. 2015, 8, 8480–8486. [Google Scholar] [PubMed]
- Ediriweera de Silva, R.E.; Haniffa, M.R.; Gunathillaka, K.D.K.; Atukorala, I.; Fernando, E.D.; Perera, W.L. A descriptive study of knowledge, beliefs and practices regarding osteoporosis among female medical school entrants in Sri Lanka. Asia Pac. Fam. Med. 2014, 13, 15. [Google Scholar] [CrossRef] [PubMed]
- Gammage, K.L.; Gasparotto, J.; Mack, D.E.; Klentrou, P. Gender differences in osteoporosis health beliefs and knowledge and their relation to vigorous physical activity in university students. J. Am. Coll. Health 2011, 60, 58–64. [Google Scholar] [CrossRef] [PubMed]
- Shanthi Johnson, C.; McLeod, W.; Kennedy, L.; McLeod, K. Osteoporosis health beliefs among younger and older men and women. Health Educ. Behav. 2008, 35, 721–733. [Google Scholar] [CrossRef] [PubMed]
- Marcinow, M.L.; Randall Simpson, J.A.; Whiting, S.J.; Jung, M.E.; Buchholz, A.C. Young adults’ perceptions of calcium intake and health: A qualitative study. Health Educ. Behav. 2017, 44, 898–906. [Google Scholar] [CrossRef] [PubMed]
- Chouinard, L.E.; Simpson, J.R.; Buchholz, A.C. Predictors of bone mineral density in a convenience sample of young Caucasian adults living in Southern Ontario. Appl. Physiol. Nutr. Metab. 2012, 714, 706–714. [Google Scholar] [CrossRef] [PubMed]
- Puttapitakpong, P.; Chaikittisilpa, S.; Panyakhamlerd, K.; Nimnuan, C.; Jaisamrarn, U.; Taechakraichana, N. Inter-correlation of knowledge, attitude, and osteoporosis preventive behaviours in women around the age of peak bone mass. BMC Women Health 2014, 14, 35. [Google Scholar] [CrossRef] [PubMed]
- Iwasaki, E.; Morakote, N.; Chaovistsaree, S.; Matsuo, H. Bone mineral density and bone turnover among young women in Chiang Mai, Thailand. Kobe J. Med. Sci. 2014, 59, E149–E156. [Google Scholar] [PubMed]
- Seo, S.; Chun, S.; Newell, M.A.; Yun, M. Association between alcohol consumption and Korean young women’s bone health: A cross sectional study from the 2008 to 2011 Korea national health and nutrition examination survey. BMJ Open 2015, 5. [Google Scholar] [CrossRef] [PubMed]
- Kim, S.; So, W.; Kim, J.; Sung, D.J. Relationship between bone-specific physical activity scores and measures for body composition and bone mineral density in healthy young college women. PLoS ONE 2016, 11, e0162127. [Google Scholar] [CrossRef] [PubMed]
- Kim, J.; Jung, M.; Hong, Y.; Park, J.; Choi, B. Physical activity in adolescence has a positive effect on bone mineral density in young men. J. Prev. Med. Publ. Health 2013, 46, 89–95. [Google Scholar] [CrossRef] [PubMed]
- Park, D.-I.; Choi-Kwon, S.; Han, K. Health behaviours of Korean female nursing students in relation to obesity and osteoporosis. Nurs. Outlook 2015, 63, 504–511. [Google Scholar] [CrossRef] [PubMed]
- Amre, H.; Safadi, R.; Jarrah, S.; Al-Amer, R.; Froelicher, E. Jordanian nursing students’ knowledge of osteoporosis. Int. J. Nurs. Pract. 2008, 14, 228–236. [Google Scholar] [CrossRef] [PubMed]
- Al-Zu’bi, A.; Almuhtaseb, N.; Amayreh, I. Osteoporosis awareness in a sample of teenage girls in Jordan. Jordan Med. J. 2010, 44, 420–426. [Google Scholar]
- Khan, Y.H.; Sarriff, A.; Khan, A.H.; Mallhi, T.H. Knowledge, attitude and practice (KAP) survey of osteoporosis among students of a tertiary institution in Malaysia. J. Pharm. Res. 2014, 13, 155–162. [Google Scholar] [CrossRef]
- Suriawati, A.A.; Majid, H.A.; Al-Sadat, N.; Mohamed, M.N.A.; Jalaludin, M.Y. Vitamin D and calcium intakes, physical activity, and calcaneus bmc among school-going 13-year old Malaysian adolescents. Nutrients 2016, 8, 666. [Google Scholar] [CrossRef] [PubMed]
- Ford, M.A.; Bass, M.; Zhao, Y.; Bai, J.-B.; Zhao, Y. Osteoporosis knowledge, self-efficacy, and beliefs among college students in the USA and China. J. Osteoporos. 2011, 2011, 729219. [Google Scholar] [CrossRef] [PubMed]
- Mu, M.; Wang, S.; Sheng, J.; Zhao, Y.; Wang, G.; Liu, K.Y.; Hu, C.L.; Tao, F.B.; Wang, H.L. Dietary patterns are associated with body mass index and bone mineral density in Chinese freshmen. J. Am. Coll. Nutr. 2014, 33, 120–128. [Google Scholar] [CrossRef] [PubMed]
- Chen, S.-W.; Yang, S.-C.; Wang, R.-H.; Lin, M.L. Osteoporosis prevention behaviours practiced among youth in Taichung City, Taiwan. Am. J. Health Behav. 2012, 36, 736–745. [Google Scholar] [CrossRef] [PubMed]
- Sayed-Hassan, R.; Bashour, H.; Koudsi, A. Osteoporosis knowledge and attitudes: A cross-sectional study among female nursing school students in Damascus. Arch. Osteoporos. 2013, 8, 149. [Google Scholar] [CrossRef] [PubMed]
- Uddin, R.; Huda, N.H.; Jhanker, Y.M.; Jesmeen, T.; Imam, M.Z.; Akter, S. Awareness regarding the Importance of Calcium and vitamin D among the undergraduate pharmacy students in Bangladesh. BMC Res. Notes 2013, 6, 134. [Google Scholar] [CrossRef] [PubMed]
- Sidor, P.; Głąbska, D.; Włodarek, D. Analysis of the dietary factors contributing to the future osteoporosis risk in young Polish women. Natl. Inst. Publ. Health 2016, 67, 279–285. [Google Scholar]
- Tonnesen, R.; Hovind, P.H.; Jensen, L.T.; Schwarz, P. Determinants of vitamin D status in young adults: Influence of lifestyle, sociodemographic and anthropometric factors. BMC Public Health 2016, 16, 385. [Google Scholar] [CrossRef] [PubMed]
- Eleftheriou, K.I.; Rawal, J.S.; James, L.E.; Payne, J.R.; Loosemore, M.; Pennell, D.J.; Drenos, F.; Haddad, F.S.; Humphries, S.E.; Sanders, J.; et al. Bone structure and geometry in young men: The influence of smoking, alcohol intake and physical activity. Bone 2013, 52, 17–26. [Google Scholar] [CrossRef] [PubMed]
- Ghaffari, M.; Nasirzadeh, M.; Rakhshanderou, S.M.H.B.; Harooni, J. Osteoporosis-related knowledge among students of a medical sciences university in Iran: Calcium intake and physical activity. J. Med. Life 2015, 8, 203–208. [Google Scholar] [PubMed]
- Bilal, M.; Haseeb, A.; Merchant, A.Z.; Rehman, A.; Arshad, M.H.; Malik, M.; Rehman, A.H.U.; Rani, P.; Farhan, E.; Rehman, T.S.; et al. Knowledge, beliefs and practices regarding osteoporosis among female medical school entrants in Pakistan. Asia Pac. Fam. Med. 2017, 16, 6. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, V.H.; Wang, Z. Osteoporosis knowledge of students in relevant healthcare academic programs. J. Osteoporos. 2012, 2–5. [Google Scholar] [CrossRef] [PubMed]
- Hervás, G.; Ruiz-Litago, F.; Irazusta, J.; Fernández-Atutxa, A.; Fraile-Bermúdez, A.B.; Zarrazquin, I. Physical activity, physical fitness, body composition, and nutrition are associated with bone status in university students. Nutrients 2018, 10, 61. [Google Scholar] [CrossRef] [PubMed]
- Ito, S.; Ishida, H.; Uenishi, K.; Murakami, K.; Sasaki, S. The relationship between habitual dietary phosphorus and calcium intake, and bone mineral density in young Japanese women: A cross-sectional study. Asia Pac. J. Clin. Nutr. 2011, 20, 411–417. [Google Scholar] [PubMed]
- Liberato, S.C.; Bressan, J.; Hills, A.P. The role of physical activity and diet on bone mineral indices in young men: A cross-sectional study. J. Int. Soc. Sports Nutr. 2013, 10, 1. [Google Scholar] [CrossRef] [PubMed]
- Chan, M.F.; Kwong, W.S.; Zang, Y.L.; Wan, P.Y. Evaluation of an osteoporosis prevention education programme for young adults. J. Adv. Nurs. 2007, 57, 270–285. [Google Scholar] [CrossRef] [PubMed]
- Du, S.; Mroz, T.A.; Zhai, F.; Popkin, B.M. Rapid income growth adversely affects diet quality in China—Particularly for the poor! Soc. Sci. Med. 2004, 59, 1505–1515. [Google Scholar] [CrossRef] [PubMed]
- Heaney, R.P.; Abrams, S.; Dawson-Hughes, B.; Looker, A.; Marcus, R.; Matkovic, V.; Weaver, C. Peak bone mass. Osteoporos. Int. 2000, 11, 985–986. [Google Scholar] [CrossRef] [PubMed]
- Hammad, L.F.; Benajiba, N. Lifestyle factors influencing bone health in young adult women in Saudi Arabia. Afr. Health Sci. 2017, 17, 524–531. [Google Scholar] [CrossRef] [PubMed]
- Fehily, A.M.; Coles, R.J.; Evans, W.D.; Elwood, P.C. Factors affecting bone density in young adults. Am. J. Clin. Nutr. 1992, 56, 579–586. [Google Scholar] [CrossRef] [PubMed]
- Laitinen, K.; Valimaki, M. Alcohol and bone. Calcif. Tissue Int. 1991, 49, S70–S73. [Google Scholar] [CrossRef] [PubMed]
- Maurel, D.B.; Boisseau, N.; Benhamou, C.L.; Jaffre, C. Alcohol and bone: Review of does effects and mechanisms. Osteoporos. Int. 2012, 23, 1–16. [Google Scholar] [CrossRef] [PubMed]
- Stránský, M.; Ryšavá, L. Nutrition as prevention and treatment of osteoporosis. Physiol. Res. 2009, 58, 7–11. [Google Scholar]
- Holland, A. Osteoporosis knowledge translation for young adults: New directions for prevention programs. Health Promot. Chronic Dis. Prev. Can. 2017, 37, 229–237. [Google Scholar] [CrossRef] [PubMed]
- Schoenfeld, R.E.; Ng, P.; Henderson, K.; Wu, S.-Y. Using the internet to educate adolescents about osteoporosis: Application of a tailored web-education system. Health Promot. Pract. 2010, 11, 104–111. [Google Scholar] [CrossRef] [PubMed]
- Takahata, Y. Usefulness of circuit training at home for improving bone mass and muscle mass while losing fat mass in undergraduate female students. Lipids Health Dis. 2018, 17, 104. [Google Scholar] [CrossRef] [PubMed]
- Sanaeinasab, H.; Tavakoli, R.; Karimizarchi, A.; Amini, Z.H.; Farokhian, A.; Najarkolaei, F.R. The effectiveness of education using the health belief model in preventing osteoporosis among female students. East. Mediterr. Health J. 2013, 19 (Suppl. 3), 38–44. [Google Scholar] [CrossRef]
- Zhang, Y.-P.; Li, X.-M.; Wang, D.-L.; Guo, X.-Y.; Guo, X. Evaluation of educational program on osteoporosis awareness and prevention among nurse students in China. Nurs. Health Sci. 2012, 14, 74–80. [Google Scholar] [CrossRef] [PubMed]
- Bohaty, K.; Rocole, H.; Wehling, K.; Waltman, N. Testing the effectiveness of an educational intervention to increase dietary intake of calcium and vitamin D in young adult women. J. Am. Acad. Nurse Pract. 2008, 20, 93–99. [Google Scholar] [CrossRef] [PubMed]
- Goodman, S.; Morrongiello, B.; Meckling, K. A randomized, controlled trial evaluating the efficacy of an online intervention targeting vitamin D intake, knowledge and status among young adults. Int. J. Behav. Nutr. Phys. Act. 2016, 13, 116. [Google Scholar] [CrossRef] [PubMed]
- Ha, E.; Caine-bish, N.; Holloman, C.; Lowry-gordon, K. Evaluation of effectiveness of class-based nutrition intervention on changes in soft drink and milk consumption among young adults. Nutr. J. 2009, 6, 4–9. [Google Scholar] [CrossRef] [PubMed]
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).