Spatio-Temporal Modeling of Zika and Dengue Infections within Colombia
Abstract
1. Introduction
2. Materials and Methods
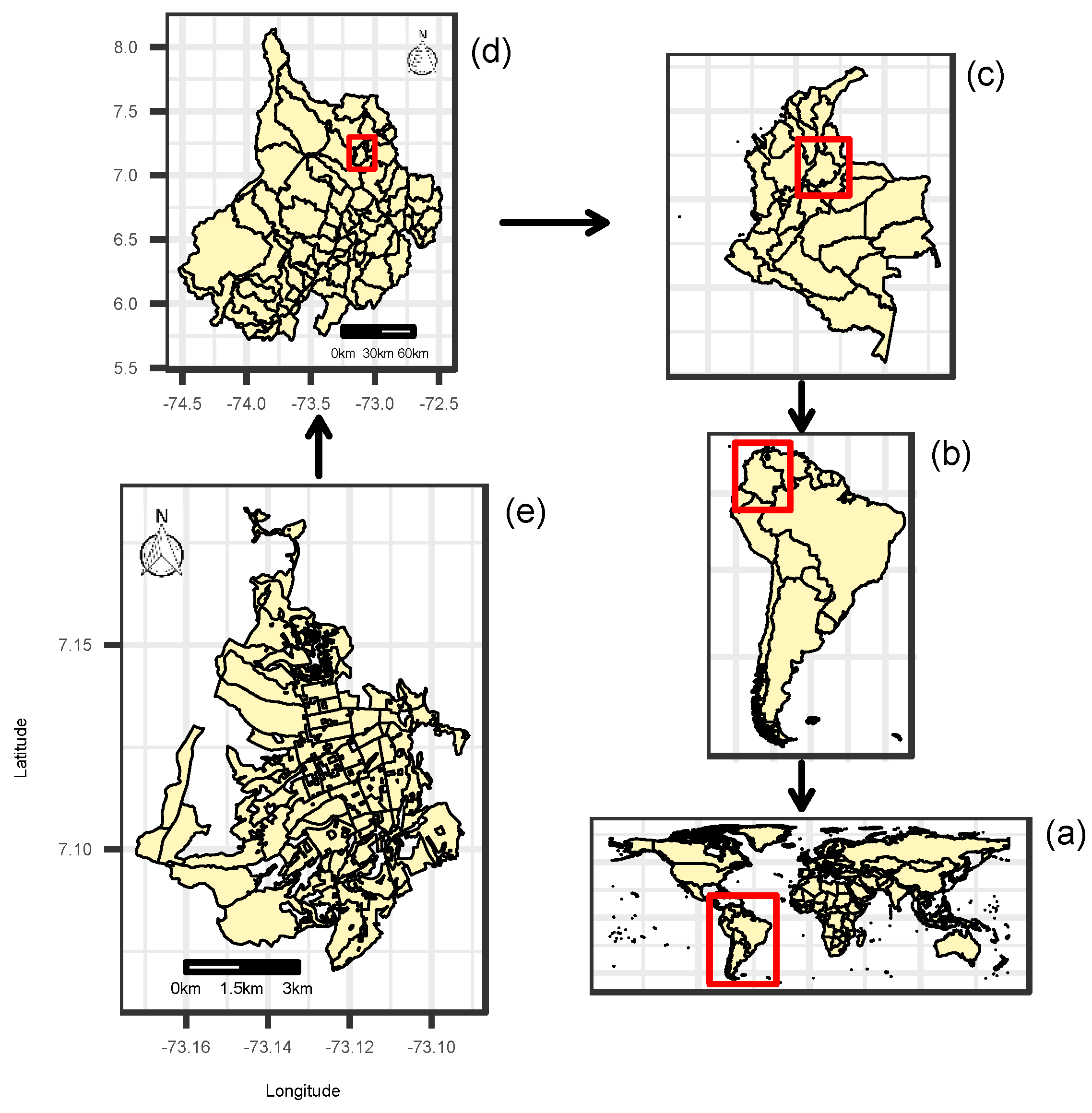
2.1. Zika and Dengue Data in Santander and Bucaramanga, Colombia
2.2. Expected Values for ZVD and Dengue
2.3. Spatio-Temporal Relative Risk Models
2.4. Inference
3. Results
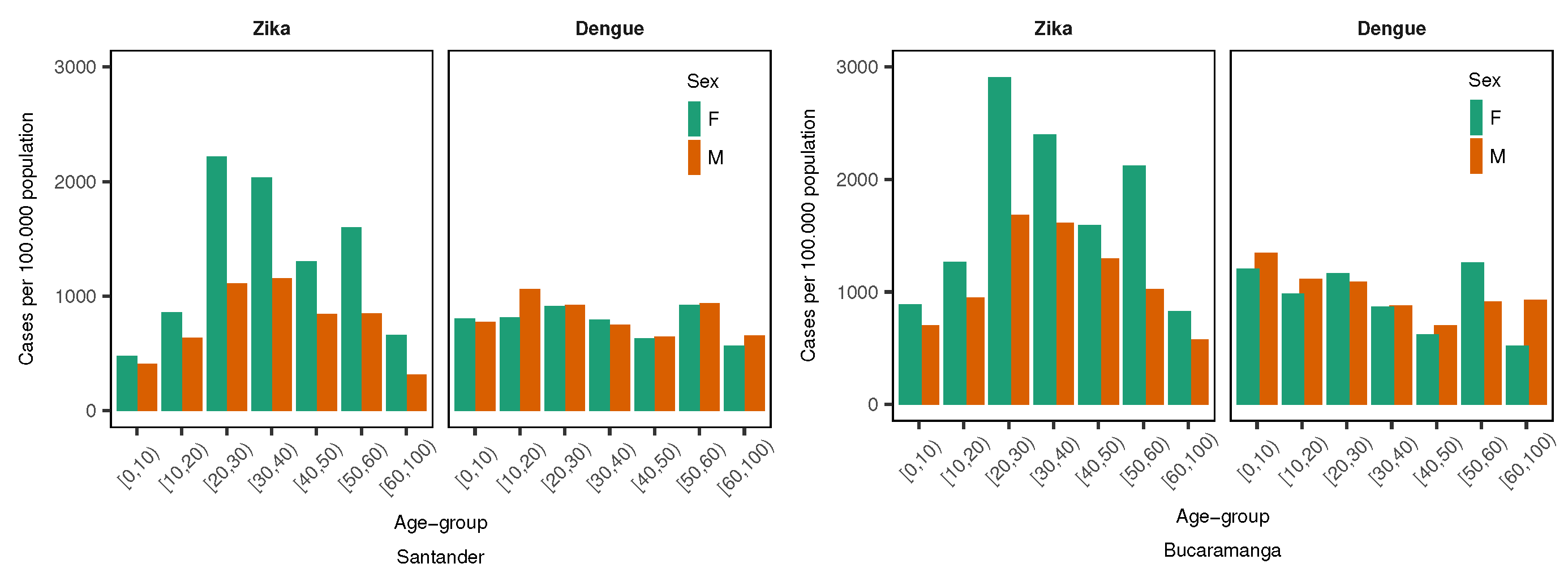
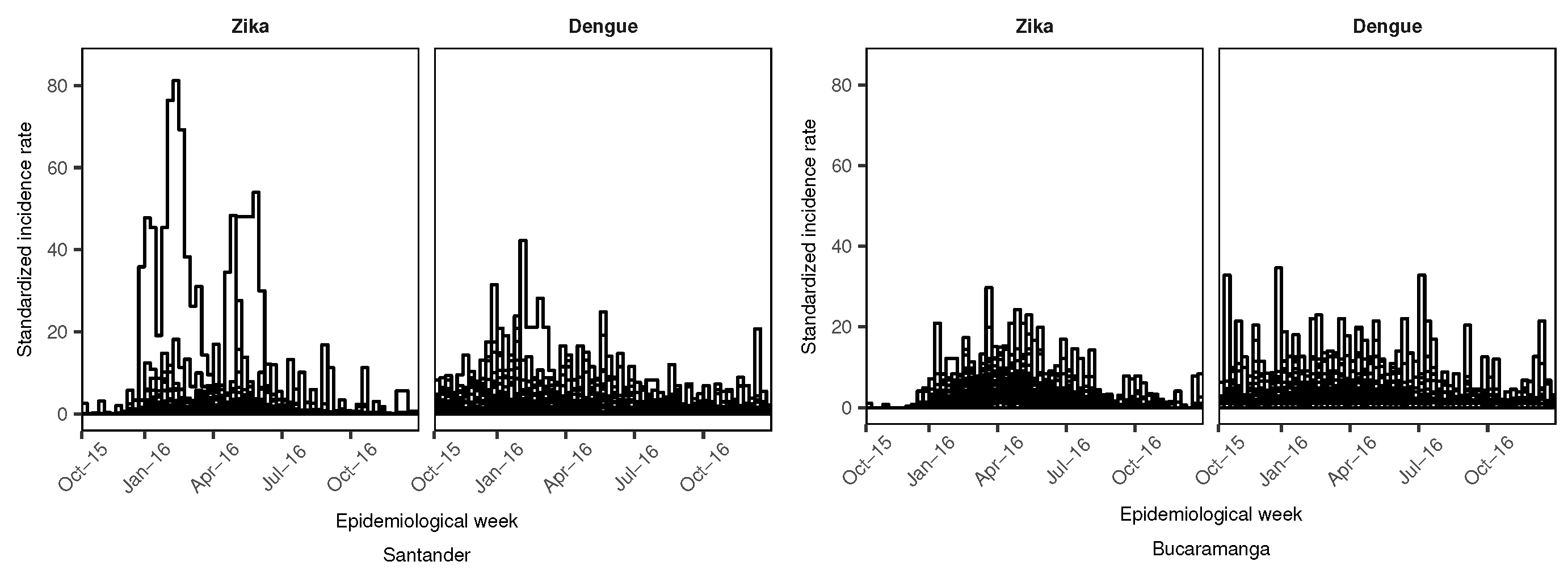
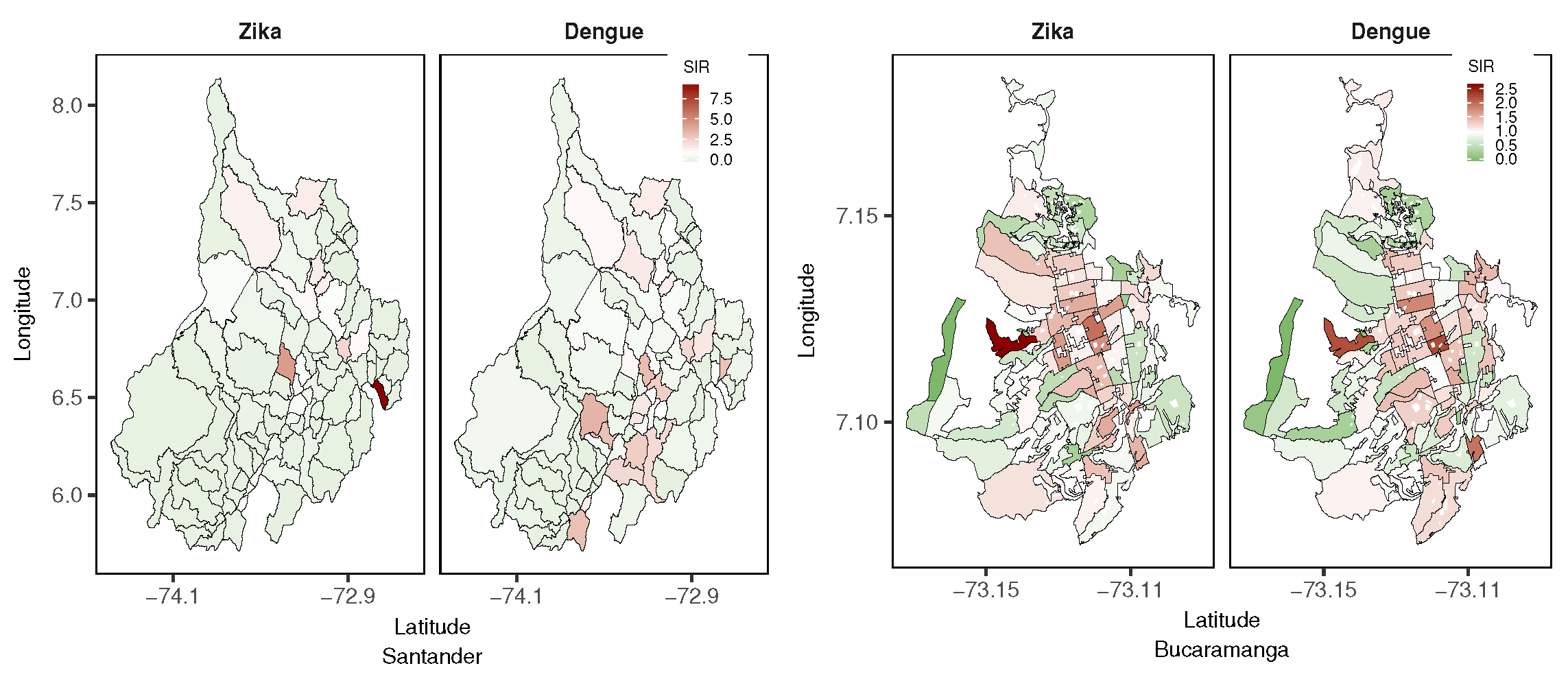
3.1. Exploratory Data Analysis
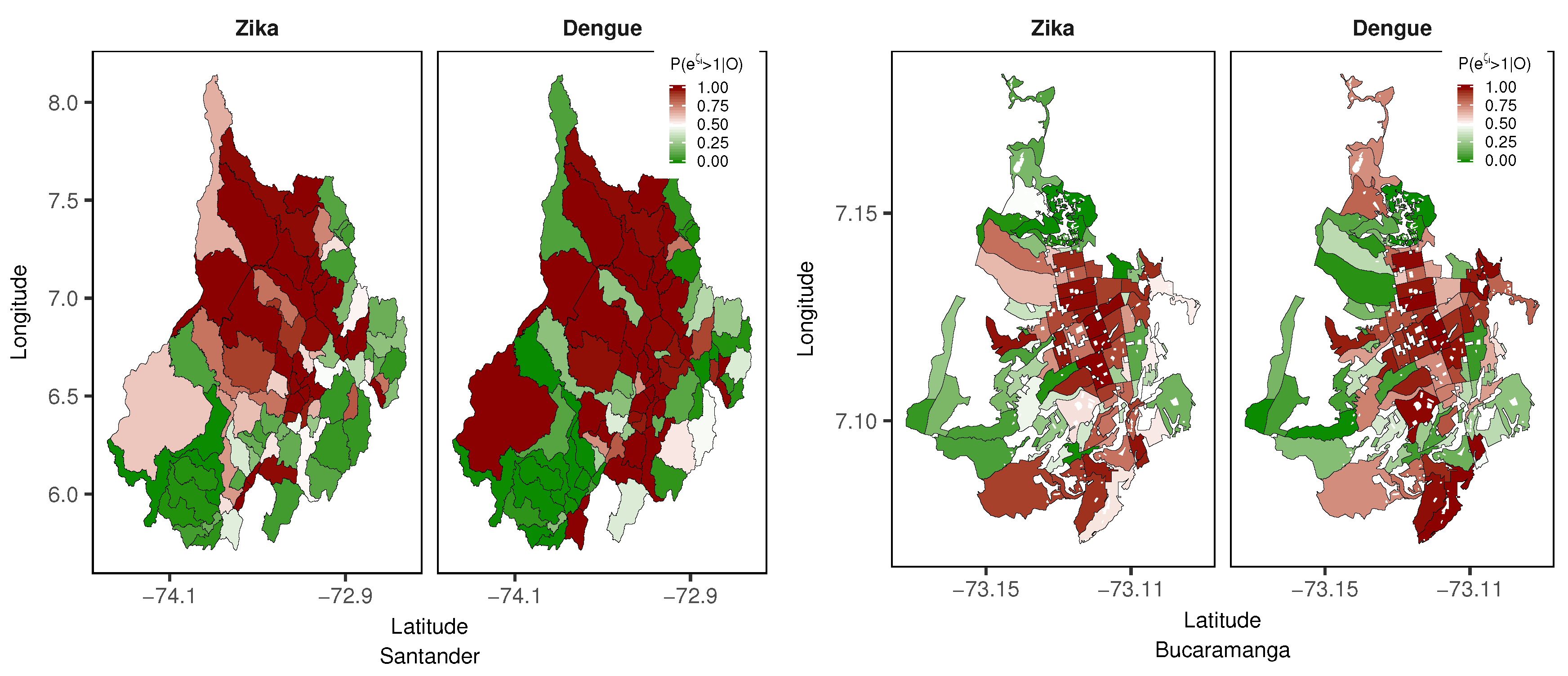
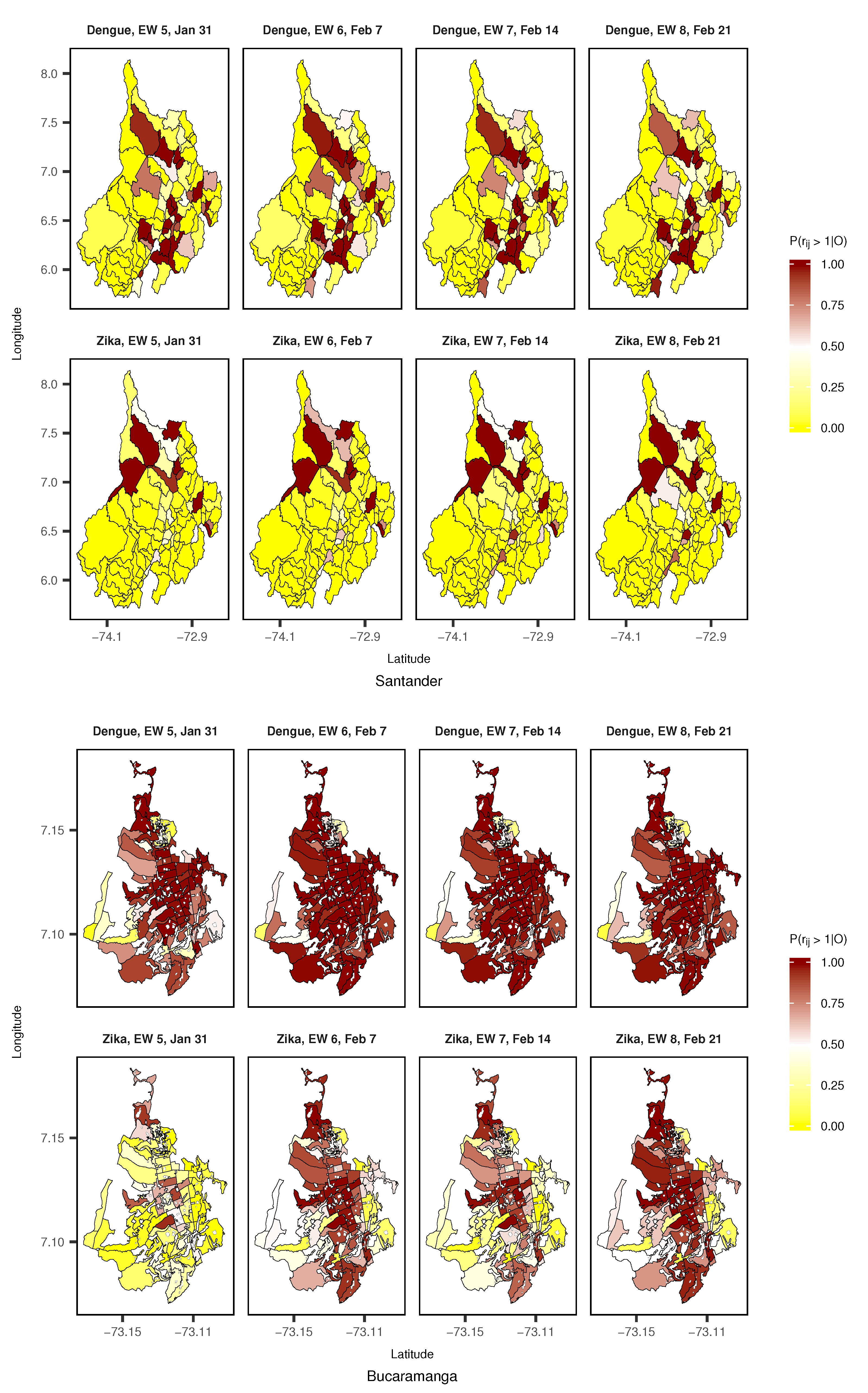
3.2. Model Findings
4. Discussion
5. Conclusions
Author Contributions
Funding
Conflicts of Interest
Abbreviations
| CI | Credible Intervals |
| CAR | Conditional Autorregressive |
| DANE | Departamento Nacional de Estadística |
| EW | Epidemiological Week |
| INLA | Integrated Nested Laplace Approximation |
| IR | Incidence Rate |
| LEB | Local Empirical Bayes |
| LS | Logarithmic Score |
| RW1 | Random Walk 1 |
| RW2 | Random Walk 2 |
| SD | Standard Deviation |
| SIR | Standardized Incidence Ratio |
| SIVIGILA | Sistema de Vigilancia en Salud Pública (Public Health Surveillance System) |
| TSIR | Time-dependent Susceptible-Infectious-Recovered |
| WAIC | Watanabe-Akaike Information Criterion |
| ZVD | Zika Virus Disease |
References
- Villar, L.A.; Rojas, D.P.; Besada-Lombana, S.; Sarti, E. Epidemiological Trends of Dengue Disease in Colombia (2000–2011): A Systematic Review. PLoS. Negl. Trop. Dis. 2015, 9, 1–16. [Google Scholar] [CrossRef] [PubMed]
- Plourde, A.R.; Bloch, E.M. A Literature Review of Zika Virus. Emerg. Infect. Dis. 2016, 22, 1185–1192. [Google Scholar] [CrossRef] [PubMed]
- Pan American Health Organization/World Health Organization. Zika Suspected and Confirmed Cases Reported by Countries and Territories in the Americas Cumulative Cases, 2015–2017; PAHO/WHO: Washington, DC, USA, 2017. [Google Scholar]
- National Health Institute. Weekly Epidemiologic Bulletin: Epidemiological Week Number 52 of 2016, 25 December–31 December; National Health Institute, Direction of Surveillance and Risk Analysis in Public Health: Bogotá, Colombia, 2016. (In Spanish)
- National Health Institute. Event Report: Dengue, 2016; National Health Institute, Direction of Surveillance and Risk Analysis in Public Health: Bogotá, Colombia, 2016. (In Spanish)
- Pacheco, O.; Beltrán, M.; Nelson, C.A.; Diana, V.M.S.; Natalia, T.M.D.; Farr, S.L.; Padilla, A.V.; Tong, V.T.; Esther, M.P.H.; Cuevas, M.S.; et al. Zika Virus Disease in Colombia—Preliminary Report. N. Engl. J. Med. 2016. [Google Scholar] [CrossRef] [PubMed]
- Rojas, D.P.; Dean, N.E.; Yang, Y.; Kenah, E.; Quintero, J.; Tomasi, S.; Ramirez, E.L.; Kelly, Y.; Castro, C.; Carrasquilla, G.; et al. The epidemiology and transmissibility of Zika virus in Girardot and San Andres island, Colombia, September 2015 to January 2016. Euro Surveill. 2016, 21, 30283. [Google Scholar] [CrossRef] [PubMed]
- Tolosa, N.; Tinker, S.C.; Pacheco, O.; Valencia, D.; Salas-Botero, D.; Tong, V.T.; Mercado, M.; Gilboaet, S.M. Zika Virus Disease in Children in Colombia, August 2015 to May 2016. Paediatr. Perinat. Epidemiol. 2017, 31, 537–545. [Google Scholar] [CrossRef] [PubMed]
- Rodriguez-Morales, A.J.; Patiño-Cadavid, L.J.; Lozada-Riasco, C.O.; Villamil-Gómez, W.E. Mapping Zika in municipalities of one coastal department of Colombia (Sucre) using geographic information systems during the 2015–2016 outbreak: Implications for public health and travel advice. Int. J. Infect. Dis. 2016, 48, 70–72. [Google Scholar] [CrossRef] [PubMed]
- Rodriguez-Morales, A.J.; Galindo-Marquez, M.L.; García-Loaiza, C.J. Mapping Zika virus infection using geographical information systems in Tolima, Colombia, 2015–2016. F1000Research 2016, 5, 568. [Google Scholar] [CrossRef] [PubMed]
- Rodriguez-Morales, A.J.; García-Loaiza, C.J.; Galindo-Marquez, M.L.; Sabogal-Roman, J.A.; Marin-Loaiza, S.; Lozada-Riascos, C.O.; Díaz-Quijano, F.A. Zika infection GIS-based mapping suggest high transmission activity in the border area of La Guajira, Colombia, a northeastern coast Caribbean department, 2015–2016: Implications for public health, migration and travel. Travel Med. Infect. Dis. 2016, 14, 286–288. [Google Scholar] [CrossRef] [PubMed]
- Rodriguez-Morales, A.J.; Haque, U.; Ball, J.D.; García-Loaiza, C.J.; Galindo-Marquez, M.L.; Sabogal-Romanm, J.A.; Marin-Loaiza, S.; Ayala, A.F.; Lozada-Riascos, C.O.; Diaz-Quijano, F.A.; et al. Spatial distribution of Zika virus infection in Northeastern Colombia. Infez. Med. 2017, 3, 241–246. [Google Scholar] [CrossRef]
- Rodriguez-Morales, A.J.; Ruiz, P.; Tabares, J.; Ossa, C.A.; Yepes-Echeverry, M.C.; Ramirez-Jaramillo, V.; Galindo-Marquez, M.L.; García-Loaiza, C.J.; Sabogal-Roman, J.A.; Parra-Valencia, E.; et al. Mapping the ecoepidemiology of Zika virus infection in urban and rural areas of Pereira, Risaralda, Colombia, 2015–2016: Implications for public health and travel medicine. Travel Med. Infect. Dis. 2017, 18, 57–66. [Google Scholar] [CrossRef] [PubMed]
- Towers, S.; Brauer, F.; Castillo-Chavez, C.; Falconar, A.K.I.; Mubayi, A.; Romero-Vivas, C.M.E. Estimate of the reproduction number of the 2015 Zika virus outbreak in Barranquilla, Colombia, and estimation of the relative role of sexual transmission. Epidemics 2016, 17, 50–55. [Google Scholar] [CrossRef] [PubMed]
- Ospina, J.; Hincapie-Palacio, D.; Ochoa, J.; Molina, A.; Rua, G.; Pajaro, D.; Arrubla, M.; Almanza, R.; Paredes, M.; Mubayi, A. Stratifying the potential local transmission of Zika in municipalities of Antioquia, Colombia. Trop. Med. Int. Health 2017, 22, 1249–1265. [Google Scholar] [CrossRef] [PubMed]
- Sebrango-Rodríguez, C.R.; Martínez-Bello, D.A.; Sánchez-Valdés, L.; Thilakarathne, P.J.; Del Fava, E.; Vand, S.P.; López-Quílez, A.; Shkedy, Z. Parameter Estimation and Real-Time Predictions of a Single Zika Outbreak Using Model Averaging. Epidemiol. Infect. 2017, 145, 2313–2323. [Google Scholar] [CrossRef] [PubMed]
- Lee, D. A comparison of conditional autoregressive models used in Bayesian disease mapping. Spat. Spatio Tempor. Epidemiol. 2011, 2, 79–89. [Google Scholar] [CrossRef] [PubMed]
- Louis, V.R.; Phalkey, R.; Horstick, O.; Ratanawong, P.; Wilder-Smith, A.; Tozan, Y.; Dambach, P. Modeling tools for dengue risk mapping—A systematic review. Int. J. Health Geogr. 2014, 13, 50. [Google Scholar] [CrossRef] [PubMed]
- Lowe, R.; Bailey, T.C.; Stephenson, D.B.; Graham, R.J.; Coelho, C.A.S.; S Carvalho, M.; Barcellos, C. Spatio-temporal modelling of climate-sensitive disease risk: Towards an early warning system for dengue in Brazil. Comput. Geosci. 2011, 37, 371–381. [Google Scholar] [CrossRef]
- Lowe, R.; Bailey, T.; Stephenson, D.; Jupp, T.; Graham, R.; Barcellos, C.; Carvalho, M. The development of an early warning system for climate-sensitive disease risk with a focus on dengue epidemics in Southeast Brazil. Stat. Med. 2013, 32, 864–883. [Google Scholar] [CrossRef] [PubMed]
- Lowe, R.; Barcellos, C.; Coelho, C.; Bailey, T.; Coelho, G.; Graham, R.; Jupp, T.; Massa-Ramalho, W.; Stephenson, D.; Rodó, X. Dengue outlook for the World Cup in Brazil: an early warning model framework driven by real-time seasonal climate forecasts. Lancet Infect. Dis. 2014, 14, 619–626. [Google Scholar] [CrossRef]
- Lowe, R.; Cazelles, B.; Paul, R.; Rodó, X. Quantifying the added value of climate information in a spatio-temporal dengue model. Stoch. Environ. Res. Risk Assess. 2016, 30, 2067–2078. [Google Scholar] [CrossRef]
- Restrepo, A.C.; Baker, P.; Clements, A.C.A. National spatial and temporal patterns of notified dengue cases, Colombia 2007–2010. Trop. Med. Int. Health 2014, 19, 863–871. [Google Scholar] [CrossRef] [PubMed]
- Arboleda, S.; Jaramillo, N.; Peterson, A.T. Mapping Environmental Dimensions of Dengue Fever Transmission Risk in the Aburrá Valley, Colombia. Int. J. Environ. Res. Public Health 2009, 6, 3040–3055. [Google Scholar] [CrossRef] [PubMed]
- Martínez-Bello, D.A.; López-Quílez, A.; Torres-Prieto, A. Bayesian dynamic modeling of time series of dengue disease case counts. PLoS. Negl. Trop. Dis. 2017, 11, e0005696. [Google Scholar] [CrossRef] [PubMed]
- Martínez-Bello, D.A.; López-Quílez, A.; Torres Prieto, A. Relative risk estimation of dengue disease at small spatial scale. Int. J. Health Geogr. 2017, 16, 31. [Google Scholar] [CrossRef] [PubMed]
- Martínez-Bello, D.; López-Quílez, A.; Torres Prieto, A. Spatiotemporal modeling of relative risk of dengue disease in Colombia. Stoch. Environ. Res. Risk Assess. 2018, 32, 1587–1601. [Google Scholar] [CrossRef]
- Stewart-Ibarra, A.; Muñoz, Á.; Ryan, S.; Ayala, E.; Borbor-Cordova, M.; Finkelstein, J.; Mejía, R.; Ordoñez, T.; Recalde-Coronel, G.; Rivero, K. Spatiotemporal clustering climate periodicity and social-ecological risk factors for dengue during an outbreak in Machala, Ecuador, in 2010. Infect. Dis. 2014, 14, 610. [Google Scholar] [CrossRef] [PubMed]
- Lippi, C.A.; Stewart-Ibarra, A.M.; Muñoz, Á.G.; Borbor-Cordova, M.J.; Mejía, R.; Rivero, K.; Castillo, K.; Cárdenas, W.B.; Ryan, S.J. The Social and Spatial Ecology of Dengue Presence and Burden during an Outbreak in Guayaquil, Ecuador, 2012. Int. J. Environ. Res. Public Health 2018, 15, 827. [Google Scholar] [CrossRef] [PubMed]
- Wijayanti, S.P.M.; Porphyre, T.; Chase-Topping, M.; Rainey, S.M.; McFarlane, M.; Schnettler, E.; Biek, R.; Kohl, A. The Importance of Socio-Economic Versus Environmental Risk Factors for Reported Dengue Cases in Java, Indonesia. PLoS. Negl. Trop. Dis. 2016, 10, 1–15. [Google Scholar] [CrossRef] [PubMed]
- Rue, H.; Martino, S.; Chopin, N. Approximate Bayesian inference for latent Gaussian models by using integrated nested Laplace approximations. J. R. Stat. Soc. Ser. B 2009, 71, 319–392. [Google Scholar] [CrossRef]
- Knorr-Held, L. Bayesian modelling of inseparable space-time variation in disease risk. Stat. Med. 2000, 19, 2555–2567. [Google Scholar] [CrossRef]
- Abd Naeeim, N.S.; Rahman, N.A. Estimating relative risk for dengue disease in Peninsular Malaysia using INLA. Malays. J. Fund. Appl. Sci. 2017, 13, 721–727. [Google Scholar] [CrossRef]
- National Health Institute of Colombia. Methodology of the Routinary Surveillance Statistical Operation; Health Ministry of Colombia, National Health Institute: Bogotá, Colombia, 2018. (In Spanish)
- National Administrative Department of Statistics (DANE). Urban Sector Level Layer, Department of Santander; National Administrative Department of Statistics (DANE): Bogotá, Colombia, 2005. (In Spanish)
- National Administrative Department of Statistics (DANE). Census 2005; National Administrative Department of Statistics (DANE): Bogotá, Colombia, 2005. (In Spanish)
- Banerjee, S.; Carlin, B.; Gelfand, A. Hierarchical Modeling and Analyisis for Spatial Data; Chapman & Hall/CRC: Boca Raton, FL, USA, 2015; p. 529. [Google Scholar]
- Leroux, B.G.; Lei, X.; Breslow, N. Estimation of disease rates in small areas: A new mixed model for spatial dependence. In Statistical Models in Epidemiology, the Environment and Clinical Trials; Halloran, M., Berry, D., Eds.; Springer: New York, NY, USA, 1999; pp. 179–191. [Google Scholar]
- Ugarte, M.D.; Adin, A.; Goicoa, T.; Militino, A.F. On fitting spatio-temporal disease mapping models using approximate Bayesian inference. Stat. Methods Med. Res. 2014, 23, 507–530. [Google Scholar] [CrossRef] [PubMed]
- Ugarte, M.; Adin, A.; Goicoa, T. Two-level spatially structured models in spatio-temporal disease mapping. Stat. Methods Med. Res. 2016, 25, 1080–1100. [Google Scholar] [CrossRef] [PubMed]
- R Core Team. R: A Language and Environment for Statistical Computing; R Foundation for Statistical Computing: Vienna, Austria, 2018. [Google Scholar]
- Goicoa, T.; Adin, A.; Ugarte, M.D.; Hodges, J.S. In spatio-temporal disease mapping models, identifiability constraints affect PQL and INLA results. Stoch. Environ. Res. Risk Assess. 2018, 32, 749–770. [Google Scholar] [CrossRef]
- Watanabe, S. Asymptotic equivalence of bayes cross validation and widely applicable information criterion in singular learning theory. J. Mach. Learn. Res. 2010, 11, 3571–3594. [Google Scholar]
- Gneiting, T.; Raftery, A.E. Strictly proper scoring rules, prediction, and estimation. J. Am. Stat. Assoc. 2007, 102, 359–378. [Google Scholar] [CrossRef]
- Krystosik, A.R.; Curtis, A.; Buritica, P.; Ajayakumar, J.; Squires, R.; Dávalos, D.; Pacheco, R.; Bhatta, M.P.; James, M.A. Community context and sub-neighborhood scale detail to explain dengue, chikungunya and Zika patterns in Cali, Colombia. PLoS ONE 2017, 12, e0181208. [Google Scholar] [CrossRef] [PubMed]
- Chien, L.-C.; Lin, R.-T.; Liao, Y.; Francisco, S.S.; Pérez, A. Surveillance on the endemic of Zika virus infection by meteorological factors in Colombia: A population-based spatial and temporal study. BMC Infect. Dis. 2018, 18, 180. [Google Scholar]
- Stewart-Ibarra, A.M.; Hargrave, A.; Diaz, A.; Kenneson, A.; Madden, D.; Romero, M.M.; Molina, J.P.; Macias, S.D. Psychological Distress and Zika, Dengue and Chikungunya Symptoms Following the 2016 Earthquake in Bahía de Caráquez, Ecuador. Int. J. Environ. Res. Public Health 2017, 14, 1516. [Google Scholar] [CrossRef] [PubMed]
- Riou, J.; Chiara, P.; Boelle, P.Y. A comparative analysis of Chikungunya and Zika transmission. Epidemics 2017, 19, 43–52. [Google Scholar] [CrossRef] [PubMed]
- Perkins, T.A.; Metcalf, C.J.E.; Grenfell, B.T.; Tatem, A.J. Estimating drivers of autochthonous transmission of Chikungunya virus in its invasion of the Americas. PLoS Curr. 2015, 7. [Google Scholar] [CrossRef] [PubMed]
- Aguiar, B.S.; Lorenz, C.; Virginio, F.; Suesdek, L.; Chiaravalloti-Neto, F. Potential risks of Zika and chikungunya outbreaks in Brazil: A modeling study. Int. J. Infect. Dis. 2018, 70, 20–29. [Google Scholar] [CrossRef] [PubMed]
- Lowe, R.; Barcellos, C.; Brasil, P.; Cruz, O.G.; Honório, N.A.; Kuper, H.; Carvalho, M.S. The Zika Virus Epidemic in Brazil: From Discovery to Future Implications. Int. J. Environ. Res. Public Health 2018, 15, 96. [Google Scholar] [CrossRef] [PubMed]
- Saiz, J.-C.; Martín-Acebes, M.A.; Bueno-Marí, R.; Salomón, O.D.; Villamil-Jiménez, L.C.; Heukelbach, J.; Alencar, C.H.; Armstrong, P.K.; Ortiga-Carvalho, T.M.; Mendez-Otero, R.; et al. Zika Virus: What Have We Learnt Since the Start of the Recent Epidemic? Front. Microbiol. 2017, 8, 1554. [Google Scholar] [CrossRef] [PubMed]
- Sallam, M.F.; Fizer, C.; Pilant, A.N.; Whung, P.-Y. Systematic Review: Land Cover, Meteorological, and Socioeconomic Determinants of Aedes Mosquito Habitat for Risk Mapping. Int. J. Environ. Res. Public Health 2017, 14, 1230. [Google Scholar] [CrossRef] [PubMed]
- Romero-Vega, L.; Pacheco, O.; de la Hoz-Restrepo, F.; Díaz-Quijano, F.A. Evaluation of dengue fever reports during an epidemic, Colombia. Rev. Sáude Públ. 2014, 48, 899–905. [Google Scholar] [CrossRef] [PubMed]
- National Health Institute of Colombia. Subregister of Zika in Girardot, Cundinamarca, 2015–2016. Inf. Quinc. Epidemiol. Nac. 2016, 21, 501–522. (In Spanish) [Google Scholar]


| Zika | Dengue | |||||||
|---|---|---|---|---|---|---|---|---|
| Deviance | p | WAIC | LS | Deviance | p | WAIC | LS | |
| Department of Santander | ||||||||
| No interaction | 6290.6 | 115.7 | 6592.6 | 3307.4 | 8308.4 | 112.7 | 8490.5 | 4236.5 |
| Type I | 4222.8 | 630.5 | 4855.0 | 4570.9 | 7278.4 | 623.9 | 7934.2 | 4156.7 |
| Type II | 4166.2 | 410.4 | 4562.9 | 2362.7 | 6979.7 | 435.3 | 7413.6 | 3738.7 |
| Type III | 4247.6 | 589.1 | 4856.3 | 4147.4 | 7314.4 | 589.0 | 7968.7 | 4143.6 |
| Type IV | 4206.4 | 382.1 | 4593.7 | 2437.6 | 7044.8 | 408.1 | 7470.9 | 3764.0 |
| City of Bucaramanga | ||||||||
| No interaction | 7852.1 | 105.0 | 7970.1 | 3985.3 | 7938.5 | 93.9 | 8042.5 | 4021.4 |
| Type I | 7659.3 | 275.0 | 7949.3 | 3980.8 | 7680.3 | 318.2 | 8018.5 | 4014.6 |
| Type II | 7537.5 | 263.7 | 7808.2 | 3907.3 | 7841.2 | 165.6 | 8024.2 | 4012.8 |
| Type III | 7653.2 | 247.7 | 7913.6 | 3961.5 | 7865.6 | 159.9 | 8040.7 | 4021.2 |
| Type IV | 7576.6 | 218.7 | 7804.1 | 3904.1 | 7839.7 | 155.8 | 8010.4 | 4005.7 |
| Zika | Dengue | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Mean | SD | 2.5% | 50% | 97.5% | Mean | SD | 2.5% | 50% | 97.5% | |
| Department of Santander | ||||||||||
| 0.61 | 0.17 | 0.26 | 0.63 | 0.90 | 0.50 | 0.18 | 0.17 | 0.50 | 0.84 | |
| 2.36 | 0.33 | 1.80 | 2.34 | 3.05 | 2.04 | 0.32 | 1.49 | 2.02 | 2.73 | |
| 0.32 | 0.04 | 0.24 | 0.31 | 0.41 | 0.11 | 0.02 | 0.08 | 0.11 | 0.16 | |
| 0.06 | 0.04 | 0.01 | 0.05 | 0.16 | 0.04 | 0.02 | 0.01 | 0.04 | 0.09 | |
| 0.36 | 0.02 | 0.31 | 0.36 | 0.40 | 0.23 | 0.01 | 0.20 | 0.23 | 0.25 | |
| City of Bucaramanga | ||||||||||
| 0.55 | 0.20 | 0.16 | 0.55 | 0.89 | 0.49 | 0.19 | 0.15 | 0.49 | 0.84 | |
| 0.48 | 0.07 | 0.36 | 0.48 | 0.64 | 0.52 | 0.08 | 0.39 | 0.51 | 0.68 | |
| 0.42 | 0.06 | 0.33 | 0.42 | 0.54 | 0.19 | 0.04 | 0.13 | 0.18 | 0.27 | |
| 0.07 | 0.06 | 0.01 | 0.06 | 0.25 | 0.07 | 0.04 | 0.02 | 0.07 | 0.16 | |
| 0.17 | 0.02 | 0.14 | 0.17 | 0.21 | 0.10 | 0.02 | 0.07 | 0.10 | 0.14 | |
© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Martínez-Bello, D.A.; López-Quílez, A.; Torres Prieto, A. Spatio-Temporal Modeling of Zika and Dengue Infections within Colombia. Int. J. Environ. Res. Public Health 2018, 15, 1376. https://doi.org/10.3390/ijerph15071376
Martínez-Bello DA, López-Quílez A, Torres Prieto A. Spatio-Temporal Modeling of Zika and Dengue Infections within Colombia. International Journal of Environmental Research and Public Health. 2018; 15(7):1376. https://doi.org/10.3390/ijerph15071376
Chicago/Turabian StyleMartínez-Bello, Daniel Adyro, Antonio López-Quílez, and Alexander Torres Prieto. 2018. "Spatio-Temporal Modeling of Zika and Dengue Infections within Colombia" International Journal of Environmental Research and Public Health 15, no. 7: 1376. https://doi.org/10.3390/ijerph15071376
APA StyleMartínez-Bello, D. A., López-Quílez, A., & Torres Prieto, A. (2018). Spatio-Temporal Modeling of Zika and Dengue Infections within Colombia. International Journal of Environmental Research and Public Health, 15(7), 1376. https://doi.org/10.3390/ijerph15071376






