Abstract
Background and Objectives: The present systematic review investigated the efficacy of lateral extra-articular tenodesis (LET) and anterolateral ligament (ALL) as lateral extra-articular procedures (LEAPs) for anterior cruciate ligament (ACL) reconstruction. ACL reconstruction using LEAP may reduce graft rupture and rotatory laxity and allow a quicker return to sports. The outcomes of interest were patient-reported outcome measures (PROMs), return to sport, laxity, failure rate, and safety profile. Materials and Methods: The present systematic review followed the 2020 PRISMA guidelines. In December 2024, PubMed, EMBASE, and Web of Science were accessed without constraints. All clinical investigations evaluating LEAP for ACL reconstruction were considered. Only studies that considered LET and ALL as LEAP were considered. Only studies using a hamstring tendon autograft associated with LET or ALL were considered. Results: Data from 27 clinical studies (3423 patients) were retrieved. The mean length of follow-up was 61.8 ± 39.5 months. ACL reconstruction using LEAP led to a statistically significant improvement in the Lysholm score (p < 0.01) and IKDC (p < 0.01). The mean joint laxity, as measured by the arthrometer, was 1.5 ± 1.8 mm. Finally, 72.3% (623 of 668) of patients returned to their pre-injury level of sport at a mean of 6.3 ± 4.4 months. At the last follow-up, the LET group showed greater IKDC (p = 0.04). On the other hand, there was a statistically significant greater rate of patients positive to the Lachman test (p < 0.01), return to sport (p < 0.01), and reoperation (p = 0.01). No significant differences were found in Lysholm scores (p = 0.6), Tegner scores (p = 0.2), arthrometer measurements (p = 0.2), Pivot shift test results (p = 0.1), time to return to sport (p = 0.3), and failure rates (p = 0.7). Conclusions: LEAP for ACL reconstructions seems to be effective and safe. Most patients returned to their pre-injury level of sport after a mean of 6 months. LET-based ACL reconstruction may be associated with greater clinical outcomes and a higher reoperation rate compared to ALL-based reconstruction.
1. Introduction
The prevalence of anterior cruciate ligament (ACL) injuries among young athletes has risen, with an annual increase of approximately 2.3% over the past two decades [1,2,3,4,5,6]. This trend is primarily attributed to the increasing involvement of youth in high-intensity competitive sports [7,8]. While traditional single-bundle ACL reconstruction has shown promise, concerns persist regarding residual rotational instability [9,10,11,12,13,14]. Previous studies have indicated that residual rotational instability persists in up to 25% of patients, often leading to suboptimal outcomes [15,16,17]. Researchers have explored various techniques to enhance stability, including anatomic and double-bundle reconstructions [18,19,20]. More recently, attention has shifted towards lateral extra-articular procedures (LEAP) for ACL reconstruction, specifically anterolateral ligament (ALL) reconstruction and lateral extra-articular tenodesis (LET) [21,22,23,24,25,26,27,28]. ACL reconstruction using LEAP may reduce graft rupture and rotatory laxity and allow a quicker return to sport [29,30]. The optimal surgical method is still debated, and previous investigations have mainly focused on PROMs, knee laxity, return to sport, and safety [31,32,33,34,35]. Initially introduced by Lemaire [36], LET has demonstrated improved anterolateral stability and clinical outcomes when combined with ACL reconstruction in several randomised controlled trials [25,29,33,37,38,39,40,41,42,43]. ALL has also emerged as an alternative for addressing rotational instability [2,24,40,44,45,46,47,48,49,50]. Given the advancements in understanding the anterolateral ligament complex, ALL offers a potentially more anatomically accurate reconstruction [47,51,52,53,54]. Despite these developments, evidence on clinical outcomes between LET and ALL in ACL reconstruction is still limited, and the optimal technique is still under debate. Previous biomechanical studies using cadaveric models have suggested superior properties for LET compared to ALL [55,56]. This systematic review aims to bridge this knowledge gap by evaluating the outcomes of LEAP and comparing outcomes of ALL and LET in ACL reconstruction regarding patient-reported outcome measures (PROMs), return to sport, joint laxity, and complication rate. The endpoint choice relates to their common use and recognised validity in clinical practice and research [57,58].
2. Methods
2.1. Eligibility Criteria
All clinical investigations evaluating LEAP for ACL reconstruction were considered. Only studies that considered LET and ALL as LEAP procedures were considered. Only studies using a hamstring tendon autograft associated with LET or ALL were considered. According to the authors’ capabilities, only articles published in the following languages were included: English, Italian, German, French, and Spanish. Eligible studies had to be published in peer-reviewed journals. Only studies with levels I to III of evidence, according to the Oxford Centre of Evidence-Based Medicine (OCEBM), [59] were included. Opinions, editorials, letters, and reviews were excluded, as were studies involving computational analyses, in vitro or animal experiments, biomechanical assessments, or cadaveric research. Studies focusing on allografts or synthetic grafts were also deemed ineligible. Finally, only studies with a minimum follow-up period of six months were considered, as this is the established cut-off for allowing sports resumption [60,61]. A shorter follow-up period could impair the assessment of the outcome [60,61].
2.2. Search Strategy
The present systematic review followed the guidelines defined in the 2020 Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) statement [62]. The following PICOT framework was established:
- P (Problem): ACL reconstruction;
- I (Intervention): LEAP;
- C (Comparison): LET vs. ALL;
- O (Outcomes): PROMs, complications, return to sport, laxity;
- T (Timing): minimum six months of follow-up.
2.3. Data Source
EMBASE, PubMed, and Web of Science were accessed in December 2024 without additional filters or temporal constraints. The Medical Subject Headings (MeSH) used in the database search were as follows: (“Anterior Cruciate Ligament”[Mesh] OR “Anterior Cruciate Ligament/physiopathology”[Mesh] OR “Anterior Cruciate Ligament Injuries”[Mesh] OR “Arthralgia/etiology”[Mesh] OR “Athletes”[Mesh] OR “Joint Instability/etiology”[Mesh] OR “Knee Joint”[Mesh] OR “Knee Joint / pathology”[Mesh] OR “Ligaments, Articular/injuries”[Mesh] OR anterior cruciate ligament OR Knee OR rotational instability OR Rotational laxity OR Knee injuries OR ACL OR anterior cruciate injuries OR ACL injuries) AND (“Anterior Cruciate Ligament/surgery”[Mesh] OR “Anterior Cruciate Ligament Injuries/surgery”[Mesh] OR “Anterior Cruciate Ligament Reconstruction”[Mesh] OR “Hamstring Tendons/surgery”[Mesh] OR “Hamstring Tendons/transplantation”[Mesh] OR “Joint Instability/surgery”[Mesh] OR “Knee Injuries/surgery”[Mesh] OR “Knee Joint/surgery”[Mesh] OR “Ligaments, Articular/surgery”[Mesh] OR “Tendon Transfer”[Mesh] OR “Tendons/transplantation”[Mesh] OR “Transplantation, Autologous”[Mesh] OR ACL reconstruction OR anterior cruciate ligament reconstruction OR Hamstring OR hamstring tendon graft OR reconstruction) AND (“Suture Techniques”[Mesh] OR “Tenodesis”[Mesh] OR “Tenodesis/methods”[Mesh] OR Anterolateral complex OR Anterolateral instability OR Anterolateral ligament OR Anterolateral ligament reconstruction OR Anterolateral reconstruction OR Combined with extraarticular tenodesis OR extra-articular reconstruction OR extra-capsular augmentation OR Lateral extra articular tenodesis OR Lateral tenodesis OR Lemaire procedure OR LET OR Modified Lemaire OR tenodesis OR ALL) AND (“Lysholm Knee Score”[Mesh] OR “Patient Reported Outcome Measures”[Mesh] OR “Postoperative Complications”[Mesh] OR “Quality of Life”[Mesh] OR “Range of Motion, Articular”[Mesh] OR “Recovery of Function”[Mesh] OR “Reoperation”[Mesh] OR “Return to Sport”[Mesh] OR “Treatment Outcome”[Mesh] OR graft failure OR graft rupture OR Pivot shift test OR Pivot-shift OR return to sport OR rotational stability OR PROMS OR Patient reported outcomes OR Lachman test).
2.4. Outcomes of Interest
Two authors (D.P. and T.B.) independently conducted data extraction. For each study, the following generalities were collected: author, year and journal of publication, study design, and length of the follow-up (months). The following data at baseline were retrieved: number of patients, number of women, mean age, and mean BMI. Data on the following PROMs at baseline and the last follow-up were retrieved: Lysholm score [58], International Knee Documentation Committee (IKDC) [63], and Tegner Activity Scale [58]. According to previously published reports, the minimally clinically important difference (MCID) is 13.8/100 for the IKDC, 9.9/100 for the Lysholm, and 0.5/10 for the Tegner Activity Scale [64,65,66,67]. Data on the KT-1000 and KT-2000 arthrometer [68], Pivot-shift, and Lachman tests were collected at the last follow-up to evaluate laxity. Data on the level of return and time to return to sport (months) were also collected. Data concerning failure (graft ruptures) and reoperation rates were extracted. Data extraction was performed using Microsoft Office Excel version 16.0 (Microsoft Corporation, Redmond, WA, USA).
2.5. Methodology Quality Assessment
Two authors (T.B. and D.P.) performed the methodological quality assessment. The revised Risk of Bias assessment tool (RoB2) [69,70], part of the Cochrane tool for assessing the Risk of Bias in randomised controlled trials (RoB) [71], was used. The following endpoints were considered: bias arising from the randomisation process, bias due to deviations from intended interventions, bias from missing outcome data, bias in the measurement of the outcome, and bias in the selection of reported results. Nonrandomised controlled trials (non-RCTs) were evaluated using the Risk of Bias in Nonrandomised Studies of Interventions (ROBINS-I) tool [72]. Seven domains of potential bias in non-RCTs were assessed. Two domains assess possible confounding factors and the nature of patient selection before the start of the comparative intervention. Bias in the classification of interventions is evaluated using another domain. The final four domains assess methodological quality after the intervention comparison has been implemented and relate to deviations from previously intended interventions, missing data, erroneous measurement of outcomes, and bias in the selection of reported outcomes. The figure of the ROBINS-I was elaborated using the Robvis Software (Risk-of-bias VISualization, Riskofbias.info, Bristol, UK) [73].
2.6. Statistical Analysis
The main author (F.M.) performed the statistical analyses following the recommendations of the Cochrane Handbook for Systematic Reviews of Interventions [74]. Descriptive statistics were calculated using IBM SPSS software, version 25 (International Business Machines Corporation, Armonk, NY, USA). Baseline comparability was assessed using the t-test, with p > 0.05 considered satisfactory. The arithmetic mean and standard deviation were used to report continuous data. The odd ratio (OR) was used as the effect measure for comparing dichotomous data. The unpaired t-test and the 2 test were performed for continuous and dichotomic data, respectively, with values of p < 0.05 considered statistically significant.
3. Results
3.1. Search Result
The systematic literature search resulted in the identification of 2023 articles. After removing duplicates, the abstracts of 1267 articles were screened for eligibility. A total of 1016 articles were excluded for the following reasons: mismatch with the predefined study design criteria (N = 384), full-text unavailability (N = 546), and language limitations (N = 86). Of the remaining 251 studies, another 224 were excluded after full-text evaluation. Consequently, a final selection of 27 studies was included in this systematic review. The literature search results are shown in Figure 1.
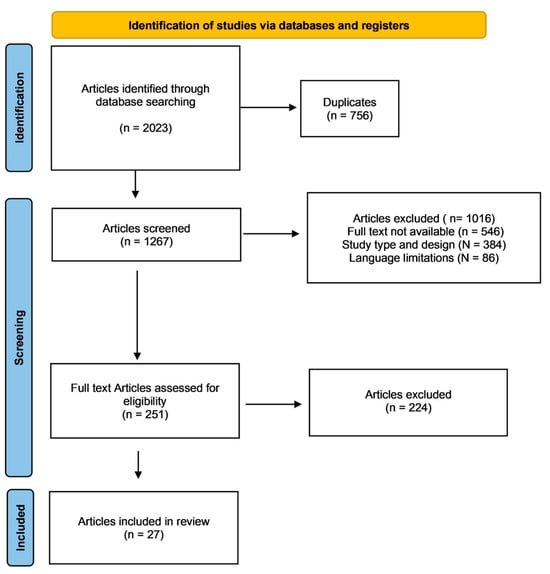
Figure 1.
Flowchart of the literature search.
3.2. Methodological Quality Assessment
The risk of bias in the 21 included non-RCTs was assessed using the ROBINS-I risk of bias. The risk of bias due to confounding was moderate in nearly three-fourths of the included non-RCTs. No bias was identified due to deviations from the intended intervention or the selection of reported results. Moreover, the risk of bias in all the other domains was judged to be low or moderate for nearly all studies. Only one article had significant issues in participant selection and was therefore classified as having a high risk of bias. Overall, 75% of the articles presented a low risk of bias, and the remaining non-RTS was found ut a moderate RoB, indicating an acceptable methodological quality (Figure 2).
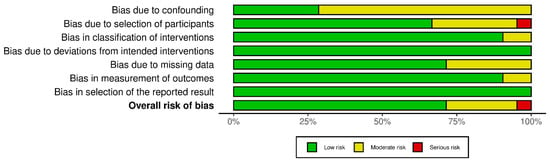
Figure 2.
ROBINS-I of the non-RCTs.
The Cochrane risk of bias assessment tool (ROB 2) was used to evaluate the six included RCTs. The analysis suggested a low risk of bias for half the articles in the first and third domains, while a moderate risk emerged in the remaining articles. Al other domains presented no concerns for any of the included RCTs. The overall RoB was estimated to be low for three articles and moderate for the others, suggesting acceptable methodological quality. Figure 3 shows the bias risk distribution across the included RCTs.
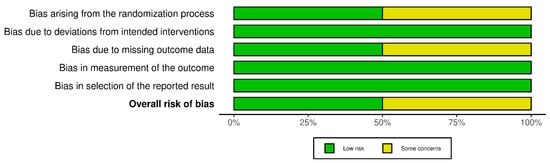
Figure 3.
ROB2 of the RCTs.
3.3. Patient Demographics
Data from 3423 patients were retrieved, 34.2% of whom (767 of 2245) were women. The mean length of follow-up was 61.8 ± 39.5 months. The mean age was 25.1 ± 4.3 years, and the mean BMI was 23.6 ± 1.6 kg/m2. Table 1 shows the generalities and demographics of the study.

Table 1.
Characteristics and patient baseline of the included studies.
3.4. Baseline Comparability
Between the groups, baseline comparability was evidenced in the mean length of follow-up, mean age, mean BMI, female/male ratio, Lysholm score, and IKDC score (Table 2).

Table 2.
Baseline comparability.
3.5. Efficacy of LEAP
ACL reconstruction using LEAP led to a statistically significant improvement in the Lysholm score (MD 31.4; p < 0.01) and IKDC (MD 29.1; p < 0.01) (Table 3). Good results were also found at the last follow-up in the Tegner score (6.8 ± 2.0); however, given the missing data at admission, its improvement was not analysed.

Table 3.
Results of PROMs (MD: mean difference; FU: follow-up; IKDC: International Knee Documentation Committee).
The Pivot shift and Lachman tests were positive in 15.8% (105 of 666) and 13.0% (87 of 668 patients), respectively. The mean joint laxity measured with the arthrometer was 1.5 ± 1.8 mm. Finally, 72.3% (623 of 668) of patients returned to the pre-injury level of sport at a mean of 6.3 ± 4.4 months. These data are shown in greater detail in Table 4.

Table 4.
Results of laxity tests, Tegner activity scale, and return to sport.
3.6. Comparison of ALL Versus LET
At the last follow-up, the IKDC scored greater in the LET group (MD 5.6; p = 0.04). No differences were found in the Lysholm (p = 0.6) and Tegner (p = 0.2) scores. No difference was found in laxity measured with the arthrometer (p = 0.2) and in the Pivot shift test (p = 0.1). On the other hand, the ALL group evidenced a statistically significantly greater rate of patients testing positive for the Lachman test (OR 3.1; p <0.01). No difference was found in the time to return to sport (p = 0.3), while a statistically significant higher rate of return to sport was found in the LET group (OR 0.5; p < 0.01). These results are shown in greater detail in Table 5 and Table 6.

Table 5.
Results of PROMs, laxity tests, and return to sport (IKDC: International Knee Documentation Committee; MD: mean difference; OR: odds ratio).

Table 6.
Percentage and time of return to sport for both procedures.
ALL demonstrated a lower reoperation rate (OR 0.7; p = 0.01). No difference was observed in the failure rate (p = 0.9). These results are shown in Table 7.

Table 7.
Results of the outcome: complications (OR: odds ratio).
4. Discussion
According to the main findings of the present systematic review, LEAP for ACL reconstruction seems to be effective and safe. ACL reconstruction using LEAP led to a statistically significant improvement in PROMs and stability, with the Lysholm and the IKDC scores increasing beyond their MCID [64,65,66]. Most patients returned to their pre-injury level of sport at a mean of 6 months. The LET subgroup was associated with greater outcomes than ALL; however, the value of the IKDC did not overcome its MCID, and therefore, its clinical relevance remains uncertain. Conversely, ACL reconstruction using LET is associated with a higher reoperation rate. On the other hand, no significant differences were found between the two groups in the Lysholm score (p = 0.6) and Tegner score (p = 0.2). These results may encourage ACL reconstruction using ALL (Table 8).

Table 8.
Advantages and disadvantages of LET and ALL.
Arthroscopic ACL reconstruction is the gold standard for restoring joint stability and function after an ACL tear [102,103]. LEAP has emerged as an additional procedure to enhance rotational stability following ACL reconstruction, improving general outcomes and lowering the risk of failure [104,105,106]. LET and ALL ACL reconstructions are examples of LEAP that improve rotational stability [29,31]. LET reinforces the lateral side of the knee and usually involves fixing a part of the ITB to the femur above the knee joint. In contrast, ALL consists of a more anatomical reconstruction of the anterolateral ligament with a free graft between the tibia and the femur [107,108]. LET and ALL ACL reconstructions vary mainly in surgical execution and anatomical targets [107,109,110,111]. There has yet to be a consensus on the ideal surgical procedure, and numerous studies have evaluated these techniques over the past years, focusing on PROMs, knee laxity, return to sport, and safety [31,32,33].
Previous studies evaluating LEAP for ACL reconstruction have shown controversial results. Coquard et al. [76], comparing 222 patients treated with traditional ACL reconstruction versus ALL ACL reconstruction, also reported no significant difference in the Tegner score. Bo-Ram et al. [33] conducted a meta-analysis including 20 studies involving 2376 patients comparing ACL in isolation versus ACL combined with LEAPs (LET or ALL). Despite some limitations related to the heterogeneity of the reported studies and the subjectivity in measurement, ACL reconstruction using LEAPs showed slight improvements in subjective scores [33]. LET and ALL reduced instability, but ALL performed slightly better, given its more anatomic approach [33]. ALL, in particular, significantly improves rotational stability and graft failure reduction when combined with ACL reconstruction [33]. Boksh et al. [112] recently conducted a systematic review evaluating ten comparative clinical studies (793 patients): 390 patients underwent isolated ACL reconstruction, and 403 received ACL reconstruction with augmentation (ALL or LET). Augmentation significantly improved IKDC scores compared to isolated ACL reconstruction and demonstrated better rotational stability [112]. The graft failure rate in this cohort was considerably lower, and few complications were reported [112]. Ho Jong Ra et al. [113] conducted a systematic review of 16 studies with 1442 patients, subdivided into 1048 receiving ACL reconstruction and ALL and 394 receiving ACL reconstruction using LET. Both techniques yield similar patient-reported functional outcomes, but ALL provides superior anterior knee stability compared to LET, with fewer complications [113]. While effective for rotational stability, LET has limitations due to overconstraint, non-anatomic graft orientation, and tension variability [113].
In the present study, joint laxity after LEAP was evaluated clinically using arthrometry, the Pivot Shift, and Lachman tests. A few patients still exhibited residual laxity, as assessed through the physical examination. Ibrahim et al. [83] found less anterior translation in the ALL group than in traditional reconstruction in 110 patients. Both procedures (ALL and LET) improve rotational stability [33]. ALL reconstruction may lead to better rotational stability, a lower risk of stiffness, and a lower rate of complications compared to LET [33]. Addressing rotational instability is crucial for decreasing secondary soft tissue damage risk [114]. LET seems to be associated with a higher risk of stiffness. A systematic review of 20 studies reported that knee stiffness was present in 10 studies (1284 patients), with a loss of full extension or flexion of >5° [33]. The variability in individuating instability and knee stiffness among different studies may be attributed to the varying definitions of stiffness and stability used by other authors [33]. In detail, a higher rate of patients in the ALL group was positive for the Lachman test, suggesting a higher residual anterior knee laxity compared to the LET group [33]. However, no differences were found between ALL and LET when tested with the KT-1000 arthrometer and the Pivot Shift test. A negative Lachman test has been described in most patients treated with LET [80]. On the other hand, LET combined with ACL reconstruction had significantly worse anterior knee stability than ALL in ACL reconstruction, with a higher proportion of knees graded as 2 or 3 on the Lachman test of 10.8% in the LET and 1.5% in the ALL [113]. The large difference in these findings across studies can be attributed to the low accuracy of the Lachman test [115].
In the present investigation, 72.3% of patients returned to sport within an average of 6.3 months after surgery. This finding emphasises the potential of LEAP ACL reconstruction in restoring knee function and enabling athletes to return to their previous competitive levels. A retrospective single-centre investigation comparing traditional versus ALL ACL reconstruction reported similar results in return to sport at the same level and return to competitive sport [75]. A greater rate of return to sport was seen in the LET group compared to the ALL group [75]. However, no significant differences were observed regarding the time to return to sport [75]. This finding regarding LET must be balanced with the associated higher reoperation rate observed in this cohort. The reason for reoperation is related to several complications [91]. LET can lead to overconstraint, particularly with techniques that involve rigid fixation or improper tensioning, which may cause limited knee motion and an increased risk of joint degeneration [116,117,118]. Furthermore, techniques using staples or other fixation devices have been associated with hardware irritation and subsequent hardware removal [81]. Some patients undergoing combined procedures required secondary meniscal procedures, such as meniscectomies or repairs, but these were not directly linked to LET [119]. Infections, hemarthrosis, cyclops lesions, and fibrous nodules are other causes of reoperation [120]. Marshall et al. [120] have reported that the most frequent complications associated with LET are graft failure, hematoma, infection, chronic pain, tunnel convergence, fixation device migration, muscular hernia, peroneal nerve palsy, and knee stiffness. The most frequent complications that do not influence the reoperation rate are anterior knee pain, symptomatic tibial tunnel cyst, dysesthesia, hemarthrosis, and growth disturbance [91]. While LET may provide higher early functional improvements, it is also associated with a higher risk of reoperation owing to the more invasive nature of the procedure. Indeed, LET usually requires extensive soft tissue dissection, potentially leading to complications such as stiffness, pain, or surgical site infections that may require reoperation [33,121,122].
According to the present systematic review, LET is associated with a slightly earlier functional recovery. Therefore, it may be suitable for specific cases needing a quick return to functional activities. Complications, including graft failure and reoperation, must be considered when deciding on the best surgical treatment [33]. The reoperation rate due to graft rupture is lower with LEAP than with isolated ACL reconstruction [75,104,123,124]. Pettinari et al. [104] conducted a retrospective, nonrandomised, matched-pair comparative analysis on 1102 patients over the age of 30. The LEAP group had a significantly lower graft failure rate—0.7% in the LEAP group versus 2.7% in the isolated ACL reconstruction group [104]. The authors also reported that patients aged 30-35 had a significantly higher risk of graft failure than those aged over 35 years old [104]. Furthermore, the LEAP group had a significantly lower rate of secondary meniscectomy, 2.2% versus 5.6%, compared to the isolated ACL reconstruction group [104]. Given its lower costs and comparable clinical outcomes, ACL reconstruction using LET is more cost-effective than ALL [125]. The lower incidence of graft failure in augmented ACL reconstruction can be explained by the shared spreading of load, which reduces micromovement of the graft in the tunnel, allowing a successful bone–tendon healing interface and a satisfactory return to sport [96,126,127]. In the present investigation, no differences were observed in failure rates between the LET and ALL groups. Both groups evidenced similar complication rates. This finding validates the overall safety profile of both procedures. Nevertheless, although not statistically significant, LET evidenced a greater rate of reoperations (9.6% versus 13.8%). Additional investigations are required to establish possible differences in the long term. Guzzini et al. [80], in a case series of 16 elite female football players treated with LET ACL reconstruction, reported no complications or re-ruptures, showing excellent outcomes in terms of stability, functional recovery, and return to sport. Similar results were found by Heard et al. [81], who reported that LET ACL reconstruction leads to a significantly lower graft rupture than traditional ACL reconstruction. Mechanisms behind the reported differences between LET and ALL are not fully understood. Some authors have conducted a biomechanical comparison of these techniques using cadaveric specimens, showing no data supporting the advantage of one over the other but indicating that both procedures led to optimal biomechanical results [128].
Several limitations are evident. The heterogeneity of the included studies in terms of follow-up length, variability in demographics, and differences in surgical techniques and rehabilitation protocols may reduce the validity of the present study’s results. Furthermore, this study mainly focused on clinical results and PROMs without evaluating any other diagnostic tests or imaging techniques, such as MRI, to assess the healing of the ligament. Only studies with a minimum follow-up of six months were considered. Arthroscopic management of ACL tears involves structural modifications to the knee joint, and the recovery process and the durability of outcomes often extend beyond the early postoperative period. Studies with a follow-up period shorter than 24 months may fail to capture late complications, secondary procedures, or the full extent of functional recovery, particularly in active populations like athletes. In addition, a minimum follow-up of 24 months is widely accepted in orthopaedic and sports medicine research as a standard for evaluating mid- to long-term outcomes. This timeframe ensures that the reported results reflect stable clinical and functional outcomes rather than transient or incomplete recoveries.
Most studies lacked a control group. Given the lack of quantitative data on the endpoints of interest, a meta-analysis was not possible. Given the lack of quantitative data and missing information, the time from injury to surgery was not analysed separately. Ferretti et al. [78] reported that the Tegner score improves significantly in LEAP ACL reconstruction in 100 patients, but a lower Tegner score is observed in patients with chronic tears. Another study [82] found no differences in knee stability, PROMs, complications, or failures in 130 acute versus chronic ALL ACL reconstructions, showing promising results regardless of the timing of surgery after injury. The lack of long-term data, particularly regarding graft longevity and long-term joint health, remains an essential gap in the literature [76]. While valuable, the reliance on PROMs and clinical tests may not fully capture the results of LEAP in facilitating return to sport, preventing new injuries, or mitigating degenerative changes. Furthermore, other vital tests reported in only a few studies that can give important information should be examined, including single-leg hop distance (SLHD), Limb Symmetry Index (LSI), and the Tampa Scale for Kinesiophobia (TSK). More studies are needed to compare these two procedures and explore their relative risks and advantages by establishing standardised criteria with defined outcomes. Future high-quality comparative studies with longer follow-up periods and RCTs are needed to validate the present results in a clinical setting.
5. Conclusions
LEAP for ACL reconstructions seems to be effective and safe. This procedure restores rotational stability, leading to good clinical results, optimal functional outcomes, and great patient satisfaction. Most patients returned to their pre-injury level of sport at a mean of 6 months. LET ACL reconstruction may be associated with greater clinical outcomes, but, on the other hand, it could be associated with a higher reoperation rate compared to ALL reconstruction.
Author Contributions
F.M.: conceptualization, formal analysis, project administration, writing—original draft prepara-tion, writing—review and editing; L.L.: writing—original draft preparation, writing—review and editing; Y.R.M.: writing—original draft preparation, writing—review and editing; T.B.: formal analysis, methodology; R.D.: writing—review and editing, supervision; A.D.C.: supervision, project administration; D.P.: formal analysis, methodology; N.M.: supervision, project administration, writing—review and editing. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Data are contained within this article.
Conflicts of Interest
The authors declare no conflicts of interest.
References
- Beck, N.A.; Lawrence, J.T.R.; Nordin, J.D.; DeFor, T.A.; Tompkins, M. ACL Tears in School-Aged Children and Adolescents Over 20 Years. Pediatrics 2017, 139, e20161877. [Google Scholar] [CrossRef]
- D’Ambrosi, R.; Meena, A.; Arora, E.S.; Attri, M.; Schafer, L.; Migliorini, F. Reconstruction of the anterior cruciate ligament: A historical view. Ann. Transl. Med. 2023, 11, 364. [Google Scholar] [CrossRef] [PubMed]
- Migliorini, F.; Eschweiler, J.; Mansy, Y.E.; Quack, V.; Tingart, M.; Driessen, A. Quadriceps tendon autograft for primary ACL reconstruction: A Bayesian network meta-analysis. Eur. J. Orthop. Surg. Traumatol. 2020, 30, 1129–1138. [Google Scholar] [CrossRef] [PubMed]
- Migliorini, F.; Cocconi, F.; Schafer, L.; Memminger, M.K.; Giorgino, R.; Maffulli, N. Anterior cruciate ligament reconstruction in skeletally immature patients is effective: A systematic review. Knee Surg. Sports Traumatol. Arthrosc. 2024, 32, 418–431. [Google Scholar] [CrossRef]
- Migliorini, F.; Cocconi, F.; Schafer, L.; Vaishya, R.; Kammer, D.; Maffulli, N. Bone-patellar tendon-bone, hamstring, and quadriceps tendon autografts for anterior cruciate ligament reconstruction in skeletally immature patients: A systematic review. Br. Med. Bull. 2024, 152, 16–27. [Google Scholar] [CrossRef] [PubMed]
- Zhang, X.F.; Liu, P.; Huang, J.W.; He, Y.H. Efficacy and safety of quadriceps tendon autograft versus bone-patellar tendon-bone and hamstring tendon autografts for anterior cruciate ligament reconstruction: A systematic review and meta-analysis. J. Orthop. Traumatol. 2024, 25, 65. [Google Scholar] [CrossRef]
- Dodwell, E.R.; Lamont, L.E.; Green, D.W.; Pan, T.J.; Marx, R.G.; Lyman, S. 20 years of pediatric anterior cruciate ligament reconstruction in New York State. Am. J. Sports Med. 2014, 42, 675–680. [Google Scholar] [CrossRef] [PubMed]
- Kakavas, G.; Malliaropoulos, N.; Blach, W.; Bikos, G.; Migliorini, F.; Maffulli, N. Ball heading and subclinical concussion in soccer as a risk factor for anterior cruciate ligament injury. J. Orthop. Surg. Res. 2021, 16, 566. [Google Scholar] [CrossRef]
- Jensen, H.A.; Nielsen, T.G.; Lind, M. Delaying anterior cruciate ligament reconstruction for more than 3 or 6 months results in lower risk of revision surgery. J. Orthop. Traumatol. 2024, 25, 19. [Google Scholar] [CrossRef] [PubMed]
- Migliorini, F.; Pilone, M.; Memminger, M.K.; Eschweiler, J.; Giorgino, R.; Maffulli, N. All-epiphyseal anterior cruciate ligament reconstruction yields superior sports performances than the trans-epiphyseal technique in skeletally immature patients: A systematic review. J. Orthop. Traumatol. 2024, 25, 7. [Google Scholar] [CrossRef]
- Migliorini, F.; Vecchio, G.; Eschweiler, J.; Schneider, S.M.; Hildebrand, F.; Maffulli, N. Reduced knee laxity and failure rate following anterior cruciate ligament reconstruction compared with repair for acute tears: A meta-analysis. J. Orthop. Traumatol. 2023, 24, 8. [Google Scholar] [CrossRef]
- Jebreen, M.; Maffulli, N.; Migliorini, F.; Arumugam, A. Known-group validity of passive knee joint position sense: A comparison between individuals with unilateral anterior cruciate ligament reconstruction and healthy controls. J. Orthop. Surg. Res. 2023, 18, 525. [Google Scholar] [CrossRef] [PubMed]
- Migliorini, F.; Oliva, F.; Eschweiler, J.; Torsiello, E.; Hildebrand, F.; Maffulli, N. Knee osteoarthritis, joint laxity and PROMs following conservative management versus surgical reconstruction for ACL rupture: A meta-analysis. Br. Med. Bull. 2023, 145, 72–87. [Google Scholar] [CrossRef]
- Zhang, L.; Li, C.; Zhang, J.; Zou, D.; Dimitriou, D.; Xing, X.; Tsai, T.Y.; Li, P. Significant race and gender differences in anterior cruciate ligament tibial footprint location: A 3D-based analysis. J. Orthop. Traumatol. 2023, 24, 33. [Google Scholar] [CrossRef]
- Chambat, P.; Guier, C.; Sonnery-Cottet, B.; Fayard, J.M.; Thaunat, M. The evolution of ACL reconstruction over the last fifty years. Int. Orthop. 2013, 37, 181–186. [Google Scholar] [CrossRef] [PubMed]
- Sood, M.; Kulshrestha, V.; Sachdeva, J.; Ghai, A.; Sud, A.; Singh, S. Poor Functional Outcome in Patients with Voluntary Knee Instability after Anterior Cruciate Ligament Reconstruction. Clin. Orthop. Surg. 2020, 12, 312–317. [Google Scholar] [CrossRef]
- Ristanis, S.; Stergiou, N.; Patras, K.; Vasiliadis, H.S.; Giakas, G.; Georgoulis, A.D. Excessive tibial rotation during high-demand activities is not restored by anterior cruciate ligament reconstruction. Arthroscopy 2005, 21, 1323–1329. [Google Scholar] [CrossRef] [PubMed]
- van Eck, C.F.; Lesniak, B.P.; Schreiber, V.M.; Fu, F.H. Anatomic single- and double-bundle anterior cruciate ligament reconstruction flowchart. Arthroscopy 2010, 26, 258–268. [Google Scholar] [CrossRef] [PubMed]
- Calvisi, V.; Lupparelli, S.; Rinonapoli, G.; Padua, R. Single-bundle versus double-bundle arthroscopic reconstruction of the anterior cruciate ligament: What does the available evidence suggest? J. Orthop. Traumatol. 2007, 8, 95–100. [Google Scholar] [CrossRef] [PubMed]
- Migliorini, F.; Torsiello, E.; Trivellas, A.; Eschweiler, J.; Hildebrand, F.; Maffulli, N. Bone-patellar tendon-bone versus two- and four-strand hamstring tendon autografts for ACL reconstruction in young adults: A Bayesian network meta-analysis. Sci. Rep. 2023, 13, 6883. [Google Scholar] [CrossRef]
- D’Ambrosi, R.; Migliorini, F.; Di Maria, F.; Anghilieri, F.M.; Di Feo, F.; Ursino, N.; Mangiavini, L.; Kambhampati, S.B.S. Italian research on anterior cruciate ligament: A bibliometric analysis. Eur. J. Orthop. Surg. Traumatol. 2024, 34, 2235–2243. [Google Scholar] [CrossRef]
- Delaloye, J.R.; Saithna, A. Editorial Commentary: Lateral Extra-articular Procedures Concomitant to Anterior Cruciate Ligament Reconstruction Must Balance Clinical Efficacy and the Risk of Kinematic Restraint. Arthroscopy 2022, 38, 3172–3174. [Google Scholar] [CrossRef]
- Foissey, C.; Thaunat, M.; Caron, E.; Haidar, I.; Vieira, T.D.; Gomes, L.; Freychet, B.; Sonnery-Cottet, B.; Fayard, J.M. Combining Anterior Cruciate Ligament Reconstruction With Lateral Extra-Articular Procedures in Skeletally Immature Patients Is Safe and Associated With a Low Failure Rate. Arthrosc. Sports Med. Rehabil. 2022, 4, e1941–e1951. [Google Scholar] [CrossRef]
- Geeslin, A.G.; Chahla, J.; LaPrade, R.F. Combined Anterior Cruciate Ligament and Lateral Extra-Articular Reconstruction. Arthroscopy 2022, 38, 2600–2601. [Google Scholar] [CrossRef]
- Guarino, A.; Farinelli, L.; Iacono, V.; Screpis, D.; Piovan, G.; Rizzo, M.; Mariconda, M.; Zorzi, C. Lateral extra-articular tenodesis and anterior cruciate ligament reconstruction in young patients: Clinical results and return to sport. Orthop. Rev. 2022, 14, 33696. [Google Scholar] [CrossRef] [PubMed]
- Lodhia, P.; Nazari, G.; Bryant, D.; Getgood, A.; McCormack, R.; Group, S.; Getgood, A.M.J.; Bryant, D.M.; Litchfield, R.; Willits, K.; et al. Performance of 5-Strand Hamstring Autograft Anterior Cruciate Ligament Reconstruction in the STABILITY Study: A Subgroup Analysis. Am. J. Sports Med. 2022, 50, 3502–3509. [Google Scholar] [CrossRef]
- Perelli, S.; Costa, G.G.; Terron, V.M.; Formagnana, M.; Bait, C.; Espregueira-Mendes, J.; Monllau, J.C. Combined Anterior Cruciate Ligament Reconstruction and Modified Lemaire Lateral Extra-articular Tenodesis Better Restores Knee Stability and Reduces Failure Rates Than Isolated Anterior Cruciate Ligament Reconstruction in Skeletally Immature Patients. Am. J. Sports Med. 2022, 50, 3778–3785. [Google Scholar] [CrossRef] [PubMed]
- Piedade, S.R.; Gorios, C.; Migliorini, F.; Maffulli, N. Combined anterior cruciate and lateral collateral ligaments reconstruction with ipsilateral hamstring autograft: Surgical technique. J. Orthop. Surg. Res. 2022, 17, 466. [Google Scholar] [CrossRef]
- Getgood, A.M.J.; Bryant, D.M.; Litchfield, R.; Heard, M.; McCormack, R.G.; Rezansoff, A.; Peterson, D.; Bardana, D.; MacDonald, P.B.; Verdonk, P.C.M.; et al. Lateral Extra-articular Tenodesis Reduces Failure of Hamstring Tendon Autograft Anterior Cruciate Ligament Reconstruction: 2-Year Outcomes From the STABILITY Study Randomized Clinical Trial. Am. J. Sports Med. 2020, 48, 285–297. [Google Scholar] [CrossRef] [PubMed]
- Rezansoff, A.; Firth, A.D.; Bryant, D.M.; Litchfield, R.; McCormack, R.G.; Heard, M.; MacDonald, P.B.; Spalding, T.; Verdonk, P.C.M.; Peterson, D.; et al. Anterior Cruciate Ligament Reconstruction Plus Lateral Extra-articular Tenodesis Has a Similar Return-to-Sport Rate to Anterior Cruciate Ligament Reconstruction Alone but a Lower Failure Rate. Arthroscopy 2024, 40, 384–396.e1. [Google Scholar] [CrossRef] [PubMed]
- Rhatomy, S.; Ariyanto, M.W.; Fiolin, J.; Dilogo, I.H. Comparison of clinical outcomes between isolated ACL reconstruction and combined ACL with anterolateral ligament reconstruction: A systematic review and meta-analysis. Eur. J. Orthop. Surg. Traumatol. 2023, 33, 685–694. [Google Scholar] [CrossRef] [PubMed]
- Grassi, A.; Zicaro, J.P.; Costa-Paz, M.; Samuelsson, K.; Wilson, A.; Zaffagnini, S.; Condello, V. Good mid-term outcomes and low rates of residual rotatory laxity, complications and failures after revision anterior cruciate ligament reconstruction (ACL) and lateral extra-articular tenodesis (LET). Knee Surg. Sports Traumatol. Arthrosc. 2020, 28, 418–431. [Google Scholar] [CrossRef]
- Na, B.R.; Kwak, W.K.; Seo, H.Y.; Seon, J.K. Clinical Outcomes of Anterolateral Ligament Reconstruction or Lateral Extra-articular Tenodesis Combined With Primary ACL Reconstruction: A Systematic Review With Meta-analysis. Orthop. J. Sports Med. 2021, 9, 23259671211023099. [Google Scholar] [CrossRef] [PubMed]
- Fang, Z.; Liu, W. Obesity-associated outcomes after ACL reconstruction: A propensity-score-matched analysis of the US Nationwide Inpatient Sample 2005-2018. J. Orthop. Traumatol. 2024, 25, 36. [Google Scholar] [CrossRef]
- Buhl, L.; Muller, S.; Nuesch, C.; Pagenstert, G.; Mundermann, A.; Egloff, C. Functional leg performance 2 years after ACL surgery: A comparison between InternalBrace-augmented repair versus reconstruction versus healthy controls. J. Orthop. Traumatol. 2023, 24, 52. [Google Scholar] [CrossRef]
- Ahn, J.H.; Patel, N.A.; Lin, C.C.; Lee, T.Q. The anterolateral ligament of the knee joint: A review of the anatomy, biomechanics, and anterolateral ligament surgery. Knee Surg. Relat. Res. 2019, 31, 12. [Google Scholar] [CrossRef]
- Anderson, A.F.; Snyder, R.B.; Lipscomb, A.B., Jr. Anterior cruciate ligament reconstruction. A prospective randomized study of three surgical methods. Am. J. Sports Med. 2001, 29, 272–279. [Google Scholar] [CrossRef] [PubMed]
- Porter, M.; Shadbolt, B. Modified Iliotibial Band Tenodesis Is Indicated to Correct Intraoperative Residual Pivot Shift After Anterior Cruciate Ligament Reconstruction Using an Autologous Hamstring Tendon Graft: A Prospective Randomized Controlled Trial. Am. J. Sports Med. 2020, 48, 1069–1077. [Google Scholar] [CrossRef] [PubMed]
- Castoldi, M.; Magnussen, R.A.; Gunst, S.; Batailler, C.; Neyret, P.; Lustig, S.; Servien, E. A Randomized Controlled Trial of Bone-Patellar Tendon-Bone Anterior Cruciate Ligament Reconstruction With and Without Lateral Extra-articular Tenodesis: 19-Year Clinical and Radiological Follow-up. Am. J. Sports Med. 2020, 48, 1665–1672. [Google Scholar] [CrossRef]
- Helito, C.P.; Sobrado, M.F.; Moreira da Silva, A.G.; Castro de Padua, V.B.; Guimaraes, T.M.; Bonadio, M.B.; Pecora, J.R.; Gobbi, R.G.; Camanho, G.L. The Addition of Either an Anterolateral Ligament Reconstruction or an Iliotibial Band Tenodesis Is Associated With a Lower Failure Rate After Revision Anterior Cruciate Ligament Reconstruction: A Retrospective Comparative Trial. Arthroscopy 2023, 39, 308–319. [Google Scholar] [CrossRef]
- Declercq, J.; Schuurmans, M.; Tack, L.; Verhelst, C.; Truijen, J. Combined lateral extra-articular tenodesis and anterior cruciate ligament reconstruction: Risk of osteoarthritis. Eur. J. Orthop. Surg. Traumatol. 2023, 33, 1075–1082. [Google Scholar] [CrossRef] [PubMed]
- Mahmoud, A.; Torbey, S.; Honeywill, C.; Myers, P. Lateral Extra-Articular Tenodesis Combined With Anterior Cruciate Ligament Reconstruction Is Effective in Knees With Additional Features of Lateral, Hyperextension, or Increased Rotational Laxity: A Matched Cohort Study. Arthroscopy 2022, 38, 119–124. [Google Scholar] [CrossRef] [PubMed]
- Mao, Y.; Zhang, K.; Li, J.; Fu, W. Supplementary Lateral Extra-articular Tenodesis for Residual Anterolateral Rotatory Instability in Patients Undergoing Single-Bundle Anterior Cruciate Ligament Reconstruction: A Meta-analysis of Randomized Controlled Trials. Orthop. J. Sports Med. 2021, 9, 23259671211002282. [Google Scholar] [CrossRef]
- Kunze, K.N.; Manzi, J.; Richardson, M.; White, A.E.; Coladonato, C.; DePhillipo, N.N.; LaPrade, R.F.; Chahla, J. Combined Anterolateral and Anterior Cruciate Ligament Reconstruction Improves Pivot Shift Compared With Isolated Anterior Cruciate Ligament Reconstruction: A Systematic Review and Meta-analysis of Randomized Controlled Trials. Arthroscopy 2021, 37, 2677–2703. [Google Scholar] [CrossRef]
- Sonnery-Cottet, B.; Haidar, I.; Rayes, J.; Fradin, T.; Ngbilo, C.; Vieira, T.D.; Freychet, B.; Ouanezar, H.; Saithna, A. Long-term Graft Rupture Rates After Combined ACL and Anterolateral Ligament Reconstruction Versus Isolated ACL Reconstruction: A Matched-Pair Analysis From the SANTI Study Group. Am. J. Sports Med. 2021, 49, 2889–2897. [Google Scholar] [CrossRef]
- Rosso, F.; Rossi, R.; Faletti, R.; Cantivalli, A.; Blonna, D.; Bonasia, D.E. Transepicondylar distance measured on MRI can predict the length of the graft required for different anterior cruciate ligament reconstruction (ACLR) techniques useful for revision surgery. J. Orthop. Traumatol. 2022, 23, 50. [Google Scholar] [CrossRef]
- Sonnery-Cottet, B.; Daggett, M.; Fayard, J.M.; Ferretti, A.; Helito, C.P.; Lind, M.; Monaco, E.; de Padua, V.B.C.; Thaunat, M.; Wilson, A.; et al. Anterolateral Ligament Expert Group consensus paper on the management of internal rotation and instability of the anterior cruciate ligament—Deficient knee. J. Orthop. Traumatol. 2017, 18, 91–106. [Google Scholar] [CrossRef] [PubMed]
- Agarwal, N.; Monketh, J.; Volpin, A. Clinical and mechanical outcomes in isolated anterior cruciate ligament reconstruction vs additional lateral extra-articular tenodesis or anterolateral ligament reconstruction. World J. Orthop. 2022, 13, 662–675. [Google Scholar] [CrossRef] [PubMed]
- Espejo-Reina, A.; Espejo-Reina, M.J.; Lombardo-Torre, M.; Sevillano-Perez, E.; Llanos-Rodriguez, A.; Espejo-Baena, A. Anterior Cruciate Ligament Revision Surgery Associated to Lateral Collateral and Anterolateral Ligaments Reconstruction With Single Achilles Tendon Allograft and Single Femoral Tunnel. Arthrosc. Tech. 2022, 11, e1769–e1777. [Google Scholar] [CrossRef]
- Mowbray, M.A.S.; Ireland, J. Personal and narrative review of the current management of the injured anterior cruciate ligament of the knee in the UK with reference to surgical treatment versus rehabilitation. BMJ Open Sport. Exerc. Med. 2022, 8, e001410. [Google Scholar] [CrossRef]
- Littlefield, C.P.; Belk, J.W.; Houck, D.A.; Kraeutler, M.J.; LaPrade, R.F.; Chahla, J.; McCarty, E.C. The Anterolateral Ligament of the Knee: An Updated Systematic Review of Anatomy, Biomechanics, and Clinical Outcomes. Arthroscopy 2021, 37, 1654–1666. [Google Scholar] [CrossRef] [PubMed]
- Xu, J.; Ye, Z.; Han, K.; Xu, C.; Zhao, J.; Dong, S. Anterolateral Structure Reconstructions With Different Tibial Attachment Sites Similarly Improve Tibiofemoral Kinematics and Result in Different Graft Force in Treating Knee Anterolateral Instability. Arthroscopy 2022, 38, 2684–2696. [Google Scholar] [CrossRef]
- Kelly, S.R.; Cutter, B.M.; Huish, E.G., Jr. Biomechanical Effects of Combined Anterior Cruciate Ligament Reconstruction and Anterolateral Ligament Reconstruction: A Systematic Review and Meta-analysis. Orthop. J. Sports Med. 2021, 9, 23259671211009879. [Google Scholar] [CrossRef] [PubMed]
- Kosy, J.D.; Soni, A.; Venkatesh, R.; Mandalia, V.I. The anterolateral ligament of the knee: Unwrapping the enigma. Anatomical study and comparison to previous reports. J. Orthop. Traumatol. 2016, 17, 303–308. [Google Scholar] [CrossRef]
- Spencer, L.; Burkhart, T.A.; Tran, M.N.; Rezansoff, A.J.; Deo, S.; Caterine, S.; Getgood, A.M. Biomechanical analysis of simulated clinical testing and reconstruction of the anterolateral ligament of the knee. Am. J. Sports Med. 2015, 43, 2189–2197. [Google Scholar] [CrossRef]
- Geeslin, A.G.; Chahla, J.; Moatshe, G.; Muckenhirn, K.J.; Kruckeberg, B.M.; Brady, A.W.; Coggins, A.; Dornan, G.J.; Getgood, A.M.; Godin, J.A.; et al. Anterolateral Knee Extra-articular Stabilizers: A Robotic Sectioning Study of the Anterolateral Ligament and Distal Iliotibial Band Kaplan Fibers. Am. J. Sports Med. 2018, 46, 1352–1361. [Google Scholar] [CrossRef] [PubMed]
- Al-Dadah, O.; Shepstone, L.; Donell, S.T. Clinical outcome measures in anterior cruciate ligament reconstruction: Clinician vs patient completed knee scores. Surgeon 2021, 19, e353–e360. [Google Scholar] [CrossRef]
- Briggs, K.K.; Lysholm, J.; Tegner, Y.; Rodkey, W.G.; Kocher, M.S.; Steadman, J.R. The reliability, validity, and responsiveness of the Lysholm score and Tegner activity scale for anterior cruciate ligament injuries of the knee: 25 years later. Am. J. Sports Med. 2009, 37, 890–897. [Google Scholar] [CrossRef] [PubMed]
- Howick, J.; Chalmers, I.; Glasziou, P.; Greenhalgh, T.; Heneghan, C.; Liberati, A.; Moschetti, I.; Phillips, B.; Thornton, H.; Goddard, O.; et al. The 2011 Oxford CEBM Levels of Evidence. Oxford Centre for Evidence-Based Medicine. 2011. Available online: https://www.cebm.net/index.aspx?o=5653 (accessed on 1 January 2025).
- Petersen, W.; Zantop, T. Return to play following ACL reconstruction: Survey among experienced arthroscopic surgeons (AGA instructors). Arch. Orthop. Trauma. Surg. 2013, 133, 969–977. [Google Scholar] [CrossRef]
- Zaffagnini, S.; Grassi, A.; Serra, M.; Marcacci, M. Return to sport after ACL reconstruction: How, when and why? A narrative review of current evidence. Joints 2015, 3, 25–30. [Google Scholar] [CrossRef]
- Page, M.J.; McKenzie, J.E.; Bossuyt, P.M.; Boutron, I.; Hoffmann, T.C.; Mulrow, C.D.; Shamseer, L.; Tetzlaff, J.M.; Akl, E.A.; Brennan, S.E.; et al. The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ 2021, 372, n71. [Google Scholar] [CrossRef]
- Grevnerts, H.T.; Terwee, C.B.; Kvist, J. The measurement properties of the IKDC-subjective knee form. Knee Surg. Sports Traumatol. Arthrosc. 2015, 23, 3698–3706. [Google Scholar] [CrossRef] [PubMed]
- Kunze, K.N.; Polce, E.M.; Ranawat, A.S.; Randsborg, P.H.; Williams, R.J., 3rd; Allen, A.A.; Nwachukwu, B.U.; Group, H.A.R.; Pearle, A.; Stein, B.S.; et al. Application of Machine Learning Algorithms to Predict Clinically Meaningful Improvement After Arthroscopic Anterior Cruciate Ligament Reconstruction. Orthop. J. Sports Med. 2021, 9, 23259671211046575. [Google Scholar] [CrossRef] [PubMed]
- Nwachukwu, B.U.; Chang, B.; Voleti, P.B.; Berkanish, P.; Cohn, M.R.; Altchek, D.W.; Allen, A.A.; Williams, R.J.R. Preoperative Short Form Health Survey Score Is Predictive of Return to Play and Minimal Clinically Important Difference at a Minimum 2-Year Follow-up After Anterior Cruciate Ligament Reconstruction. Am. J. Sports Med. 2017, 45, 2784–2790. [Google Scholar] [CrossRef] [PubMed]
- Ye, Z.; Zhang, T.; Wu, C.; Qiao, Y.; Su, W.; Chen, J.; Xie, G.; Dong, S.; Xu, J.; Zhao, J. Predicting the Objective and Subjective Clinical Outcomes of Anterior Cruciate Ligament Reconstruction: A Machine Learning Analysis of 432 Patients. Am. J. Sports Med. 2022, 50, 3786–3795. [Google Scholar] [CrossRef] [PubMed]
- Mostafaee, N.; Negahban, H.; Shaterzadeh Yazdi, M.J.; Goharpey, S.; Mehravar, M.; Pirayeh, N. Responsiveness of a Persian version of Knee Injury and Osteoarthritis Outcome Score and Tegner activity scale in athletes with anterior cruciate ligament reconstruction following physiotherapy treatment. Physiother. Theory Pract. 2020, 36, 1019–1026. [Google Scholar] [CrossRef] [PubMed]
- Arneja, S.; Leith, J. Review article: Validity of the KT-1000 knee ligament arthrometer. J. Orthop. Surg. 2009, 17, 77–79. [Google Scholar] [CrossRef]
- Sterne, J.A.C.; Savovic, J.; Page, M.J.; Elbers, R.G.; Blencowe, N.S.; Boutron, I.; Cates, C.J.; Cheng, H.Y.; Corbett, M.S.; Eldridge, S.M.; et al. RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ 2019, 366, l4898. [Google Scholar] [CrossRef]
- Higgins, J.P.T.; Savović, J.; Page, M.J.; Elbers, R.G.; Sterne, J.A.C. Chapter 8: Assessing risk of bias in a randomized trial. In Cochrane Handbook for Systematic Reviews of Interventions Version 6.3 (Updated February 2022); Higgins, J.P.T., Thomas, J., Chandler, J., Cumpston, M., Li, T., Page, M.J., Welch, V.A., Eds.; Cochrane: London, UK, 2022; Available online: https://training.cochrane.org/handbook/current/chapter-08 (accessed on 3 February 2025).
- Higgins, J.P.; Altman, D.G.; Gøtzsche, P.C.; Jüni, P.; Moher, D.; Oxman, A.D.; Savović, J.; Schulz, K.F.; Weeks, L.; Sterne, J.A. The Cochrane Collaboration’s tool for assessing risk of bias in randomised trials. BMJ 2011, 343, d5928. [Google Scholar] [CrossRef] [PubMed]
- Sterne, J.A.; Hernan, M.A.; Reeves, B.C.; Savovic, J.; Berkman, N.D.; Viswanathan, M.; Henry, D.; Altman, D.G.; Ansari, M.T.; Boutron, I.; et al. ROBINS-I: A tool for assessing risk of bias in non-randomised studies of interventions. BMJ 2016, 355, i4919. [Google Scholar] [CrossRef] [PubMed]
- McGuinness, L.A.; Higgins, J.P.T. Risk-of-bias VISualization (robvis): An R package and Shiny web app for visualizing risk-of-bias assessments. Res. Synth. Methods 2020, 12, 55–61. [Google Scholar] [CrossRef]
- Higgins, J.P.T.; Thomas, J.; Chandler, J.; Cumpston, M.; Li, T.; Page, M.J.; Welch, V.A. (Eds.) Cochrane Handbook for Systematic Reviews of Interventions Version 6.3 (Updated February 2022); Cochrane: London, UK, 2022; Available online: www.training.cochrane.org/handbook (accessed on 3 February 2025).
- Gonnachon, A.; Labattut, L.; Abdoul Carime, N.; Orta, C.; Baulot, E.; Martz, P. Does combined anterior cruciate ligament and anterolateral ligament reconstruction improve return to sport? Eur. J. Orthop. Surg. Traumatol. 2024, 34, 981–987. [Google Scholar] [CrossRef]
- Coquard, M.; Carrozzo, A.; Saithna, A.; Vigne, G.; Le Guen, M.; Fournier, Y.; Hager, J.P.; Vieira, T.D.; Sonnery-Cottet, B. Anterolateral Ligament Reconstruction Does Not Delay Functional Recovery, Rehabilitation, and Return to Sport After Anterior Cruciate Ligament Reconstruction: A Matched-Pair Analysis From the SANTI (Scientific ACL Network International) Study Group. Arthrosc. Sports Med. Rehabil. 2022, 4, e9–e16. [Google Scholar] [CrossRef] [PubMed]
- El-Azab, H.; Moursy, M.; Mohamed, M.A.; Elsayed, M. A comparison of the outcomes of anterior curciate ligament reconstruction with large-size graft versus reconstruction with average-size graft combined with extraarticular tenodesis. Injury 2023, 54, 976–982. [Google Scholar] [CrossRef] [PubMed]
- Ferretti, A.; Monaco, E.; Giannetti, S.; Caperna, L.; Luzon, D.; Conteduca, F. A medium to long-term follow-up of ACL reconstruction using double gracilis and semitendinosus grafts. Knee Surg. Sports Traumatol. Arthrosc. 2011, 19, 473–478. [Google Scholar] [CrossRef] [PubMed]
- Viglietta, E.; Ponzo, A.; Monaco, E.; Iorio, R.; Drogo, P.; Andreozzi, V.; Conteduca, F.; Ferretti, A. ACL Reconstruction Combined With the Arnold-Coker Modification of the MacIntosh Lateral Extra-articular Tenodesis: Long-term Clinical and Radiological Outcomes. Am. J. Sports Med. 2022, 50, 404–414. [Google Scholar] [CrossRef]
- Guzzini, M.; Mazza, D.; Fabbri, M.; Lanzetti, R.; Redler, A.; Iorio, C.; Monaco, E.; Ferretti, A. Extra-articular tenodesis combined with an anterior cruciate ligament reconstruction in acute anterior cruciate ligament tear in elite female football players. Int. Orthop. 2016, 40, 2091–2096. [Google Scholar] [CrossRef] [PubMed]
- Heard, M.; Marmura, H.; Bryant, D.; Litchfield, R.; McCormack, R.; MacDonald, P.; Spalding, T.; Verdonk, P.; Peterson, D.; Bardana, D.; et al. No increase in adverse events with lateral extra-articular tenodesis augmentation of anterior cruciate ligament reconstruction—Results from the stability randomized trial. J. Isakos 2023, 8, 246–254. [Google Scholar] [CrossRef] [PubMed]
- Helito, C.P.; Sobrado, M.F.; Giglio, P.N.; Bonadio, M.B.; Pécora, J.R.; Gobbi, R.G.; Camanho, G.L. Surgical Timing Does Not Interfere on Clinical Outcomes in Combined Reconstruction of the Anterior Cruciate Ligament and Anterolateral Ligament: A Comparative Study With Minimum 2-Year Follow-Up. Arthroscopy 2021, 37, 1909–1917. [Google Scholar] [CrossRef] [PubMed]
- Ibrahim, S.A.; Shohdy, E.M.; Marwan, Y.; Ramadan, S.A.; Almisfer, A.K.; Mohammad, M.W.; Abdulsattar, W.S.; Khirat, S. Anatomic Reconstruction of the Anterior Cruciate Ligament of the Knee With or Without Reconstruction of the Anterolateral Ligament: A Randomized Clinical Trial. Am. J. Sports Med. 2017, 45, 1558–1566. [Google Scholar] [CrossRef] [PubMed]
- Joseph, L.; Demey, G.; Chamu, T.; Schmidt, A.; Germain, A.; van Rooij, F.; Saffarini, M.; Dejour, D. Adding a modified Lemaire procedure to ACLR in knees with severe rotational knee instability does not compromise isokinetic muscle recovery at the time of return-to-play. J. Exp. Orthop. 2020, 7, 84. [Google Scholar] [CrossRef] [PubMed]
- Laboudie, P.; Douiri, A.; Bouguennec, N.; Biset, A.; Graveleau, N. Combined ACL and ALL reconstruction reduces the rate of reoperation for graft failure or secondary meniscal lesions in young athletes. Knee Surg. Sports Traumatol. Arthrosc. 2022, 30, 3488–3498. [Google Scholar] [CrossRef] [PubMed]
- Lee, D.W.; Lee, D.H.; Cho, S.I.; Yang, S.J.; Kim, W.J.; Lee, J.K.; Kim, J.G. Comparison of ACL and Anterolateral Ligament Reconstruction With Isolated ACL Reconstruction Using Hamstring Autograft: Outcomes in Young Female Patients With High-Grade Pivot Shift. Orthop. J. Sports Med. 2023, 11, 23259671231178048. [Google Scholar] [CrossRef]
- Lee, J.H.; Lee, G.B.; Chung, W.; Han, S.B.; Jang, K.M. Addition of anterolateral ligament reconstruction to primary anterior cruciate ligament reconstruction could benefit recovery of functional outcomes. Sci. Rep. 2024, 14, 11440. [Google Scholar] [CrossRef]
- Legnani, C.; Borgo, E.; Macchi, V.; Ventura, A. Restoring rotational stability following anterior cruciate ligament surgery: Single-bundle reconstruction combined with lateral extra-articular tenodesis versus double-bundle reconstruction. J. Comp. Eff. Res. 2022, 11, 729–736. [Google Scholar] [CrossRef] [PubMed]
- Marcacci, M.; Zaffagnini, S.; Giordano, G.; Iacono, F.; Presti, M.L. Anterior cruciate ligament reconstruction associated with extra-articular tenodesis: A prospective clinical and radiographic evaluation with 10- to 13-year follow-up. Am. J. Sports Med. 2009, 37, 707–714. [Google Scholar] [CrossRef]
- Meynard, P.; Pelet, H.; Angelliaume, A.; Legallois, Y.; Lavignac, P.; De Bartolo, R.; Fabre, T.; Costes, S. ACL reconstruction with lateral extra-articular tenodesis using a continuous graft: 10-year outcomes of 50 cases. Orthop. Traumatol. Surg. Res. 2020, 106, 929–935. [Google Scholar] [CrossRef]
- Monaco, E.; Carrozzo, A.; Saithna, A.; Conteduca, F.; Annibaldi, A.; Marzilli, F.; Minucci, M.; Sonnery-Cottet, B.; Ferretti, A. Isolated ACL Reconstruction Versus ACL Reconstruction Combined With Lateral Extra-articular Tenodesis: A Comparative Study of Clinical Outcomes in Adolescent Patients. Am. J. Sports Med. 2022, 50, 3244–3255. [Google Scholar] [CrossRef]
- Pioger, C.; Gousopoulos, L.; Hopper, G.P.; Vieira, T.D.; Campos, J.P.; El Helou, A.; Philippe, C.; Saithna, A.; Sonnery-Cottet, B. Clinical Outcomes After Combined ACL and Anterolateral Ligament Reconstruction Versus Isolated ACL Reconstruction With Bone-Patellar Tendon-Bone Grafts: A Matched-Pair Analysis of 2018 Patients From the SANTI Study Group. Am. J. Sports Med. 2022, 50, 3493–3501. [Google Scholar] [CrossRef] [PubMed]
- Porter, M.; Shadbolt, B. Modified iliotibial band tenodesis versus lateral extracapsular tenodesis, to augment anterior cruciate ligament reconstruction: A 2-year randomized controlled trial. ANZ J. Surg. 2022, 92, 2247–2253. [Google Scholar] [CrossRef]
- Saragaglia, D.; Pison, A.; Refaie, R. Lateral tenodesis combined with anterior cruciate ligament reconstruction using a unique semitendinosus and gracilis transplant. Int. Orthop. 2013, 37, 1575–1581. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Sonnery-Cottet, B.; Thaunat, M.; Freychet, B.; Pupim, B.H.; Murphy, C.G.; Claes, S. Outcome of a Combined Anterior Cruciate Ligament and Anterolateral Ligament Reconstruction Technique With a Minimum 2-Year Follow-up. Am. J. Sports Med. 2015, 43, 1598–1605. [Google Scholar] [CrossRef] [PubMed]
- Sonnery-Cottet, B.; Saithna, A.; Cavalier, M.; Kajetanek, C.; Temponi, E.F.; Daggett, M.; Helito, C.P.; Thaunat, M. Anterolateral Ligament Reconstruction Is Associated With Significantly Reduced ACL Graft Rupture Rates at a Minimum Follow-up of 2 Years: A Prospective Comparative Study of 502 Patients From the SANTI Study Group. Am. J. Sports Med. 2017, 45, 1547–1557. [Google Scholar] [CrossRef] [PubMed]
- Thaunat, M.; Clowez, G.; Saithna, A.; Cavalier, M.; Choudja, E.; Vieira, T.D.; Fayard, J.M.; Sonnery-Cottet, B. Reoperation Rates After Combined Anterior Cruciate Ligament and Anterolateral Ligament Reconstruction: A Series of 548 Patients From the SANTI Study Group With a Minimum Follow-up of 2 Years. Am. J. Sports Med. 2017, 45, 2569–2577. [Google Scholar] [CrossRef] [PubMed]
- Vadalà, A.P.; Iorio, R.; De Carli, A.; Bonifazi, A.; Iorio, C.; Gatti, A.; Rossi, C.; Ferretti, A. An extra-articular procedure improves the clinical outcome in anterior cruciate ligament reconstruction with hamstrings in female athletes. Int. Orthop. 2013, 37, 187–192. [Google Scholar] [CrossRef]
- Yang, H.Y.; Cheon, J.H.; Choi, J.H.; Song, E.K.; Seon, J.K. Combined Anterior Cruciate Ligament and Anterolateral Ligament Reconstruction Decreases Passive Anterior Tibial Subluxation Compared with Isolated Anterior Cruciate Ligament Reconstruction Despite Similar Rotational Stability and Clinical Outcomes. Arthroscopy 2023, 39, 2513–2524.e2. [Google Scholar] [CrossRef]
- Zaffagnini, S.; Marcacci, M.; Lo Presti, M.; Giordano, G.; Iacono, F.; Neri, M.P. Prospective and randomized evaluation of ACL reconstruction with three techniques: A clinical and radiographic evaluation at 5 years follow-up. Knee Surg. Sports Traumatol. Arthrosc. 2006, 14, 1060–1069. [Google Scholar] [CrossRef] [PubMed]
- Zaffagnini, S.; Bruni, D.; Russo, A.; Takazawa, Y.; Lo Presti, M.; Giordano, G.; Marcacci, M. ST/G ACL reconstruction: Double strand plus extra-articular sling vs double bundle, randomized study at 3-year follow-up. Scand. J. Med. Sci. Sports 2008, 18, 573–581. [Google Scholar] [CrossRef] [PubMed]
- Miller, M.; Feldman, M.D. Editorial Commentary: Anterior Cruciate Ligament Primary Repair Has Limited Indications and Outcomes Inferior to Anterior Cruciate Ligament Reconstruction. Arthroscopy, 2024; ahead of print. [Google Scholar] [CrossRef]
- Zhang, L.; Xu, J.; Luo, Y.; Guo, L.; Wang, S. Anatomic femoral tunnel and satisfactory clinical outcomes achieved with the modified transtibial technique in anterior cruciate ligament reconstruction: A systematic review and meta-analysis. Heliyon 2024, 10, e35824. [Google Scholar] [CrossRef] [PubMed]
- Pettinari, F.; Carrozzo, A.; Saithna, A.; Ali, A.A.; Alayane, A.; Barosso, M.; Vieira, T.D.; Sonnery-Cottet, B. Effect of Lateral Extra-Articular Procedures Combined With ACL Reconstruction on the Rate of Graft Rupture in Patients Aged Older Than 30 Years: A Matched-Pair Analysis of 1102 Patients From the SANTI Study Group. Am. J. Sports Med. 2024, 52, 1765–1772. [Google Scholar] [CrossRef]
- Moussa, M.K.; Lefèvre, N.; Valentin, E.; Coughlan, A.; Zgolli, A.; Gerometta, A.; Meyer, A.; Hardy, A. Impact of Lateral Extra-Articular Procedure Augmentation on Rerupture Risk and Tegner Activity Scale Outcomes in Adolescent Anterior Cruciate Ligament: A Matched Comparative Study With a Minimum 2-Year Follow-up. Am. J. Sports Med. 2024, 52, 892–901. [Google Scholar] [CrossRef]
- Saithna, A.; Daggett, M.; Helito, C.P.; Monaco, E.; Franck, F.; Vieira, T.D.; Pioger, C.; Kim, J.G.; Sonnery-Cottet, B. Clinical Results of Combined ACL and Anterolateral Ligament Reconstruction: A Narrative Review from the SANTI Study Group. J. Knee Surg. 2021, 34, 962–970. [Google Scholar] [CrossRef] [PubMed]
- Mathew, M.; Dhollander, A.; Getgood, A. Anterolateral Ligament Reconstruction or Extra-Articular Tenodesis: Why and When? Clin. Sports Med. 2018, 37, 75–86. [Google Scholar] [CrossRef]
- Gillet, B.; Blache, Y.; Rogowski, I.; Vigne, G.; Capel, O.; Sonnery-Cottet, B.; Fayard, J.M.; Thaunat, M. Isokinetic Strength After ACL Reconstruction: Influence of Concomitant Anterolateral Ligament Reconstruction. Sports Health 2022, 14, 176–182. [Google Scholar] [CrossRef] [PubMed]
- Getgood, A.; Brown, C.; Lording, T.; Amis, A.; Claes, S.; Geeslin, A.; Musahl, V. The anterolateral complex of the knee: Results from the International ALC Consensus Group Meeting. Knee Surg. Sports Traumatol. Arthrosc. 2019, 27, 166–176. [Google Scholar] [CrossRef] [PubMed]
- Firth, A.D.; Bryant, D.M.; Litchfield, R.; McCormack, R.G.; Heard, M.; MacDonald, P.B.; Spalding, T.; Verdonk, P.C.M.; Peterson, D.; Bardana, D.; et al. Predictors of Graft Failure in Young Active Patients Undergoing Hamstring Autograft Anterior Cruciate Ligament Reconstruction With or Without a Lateral Extra-articular Tenodesis: The Stability Experience. Am. J. Sports Med. 2022, 50, 384–395. [Google Scholar] [CrossRef] [PubMed]
- Kemler, B.; Coladonato, C.; Sonnier, J.H.; Campbell, M.P.; Darius, D.; Erickson, B.J.; Tjoumakaris, F.P.; Freedman, K.B. Evaluation of Failed ACL Reconstruction: An Updated Review. Open Access J. Sports Med. 2024, 15, 29–39. [Google Scholar] [CrossRef]
- Boksh, K.; Sheikh, N.; Chong, H.H.; Ghosh, A.; Aujla, R. The Role of Anterolateral Ligament Reconstruction or Lateral Extra-articular Tenodesis for Revision Anterior Cruciate Ligament Reconstruction: A Systematic Review and Meta-analysis of Comparative Clinical Studies. Am. J. Sports Med. 2024, 52, 269–285. [Google Scholar] [CrossRef]
- Ra, H.J.; Kim, J.H.; Lee, D.H. Comparative clinical outcomes of anterolateral ligament reconstruction versus lateral extra-articular tenodesis in combination with anterior cruciate ligament reconstruction: Systematic review and meta-analysis. Arch. Orthop. Trauma Surg. 2020, 140, 923–931. [Google Scholar] [CrossRef]
- Jonsson, H.; Riklund-Ahlstrom, K.; Lind, J. Positive pivot shift after ACL reconstruction predicts later osteoarthrosis: 63 patients followed 5-9 years after surgery. Acta Orthop. Scand. 2004, 75, 594–599. [Google Scholar] [CrossRef] [PubMed]
- Sokal, P.A.; Norris, R.; Maddox, T.W.; Oldershaw, R.A. The diagnostic accuracy of clinical tests for anterior cruciate ligament tears are comparable but the Lachman test has been previously overestimated: A systematic review and meta-analysis. Knee Surg. Sports Traumatol. Arthrosc. 2022, 30, 3287–3303. [Google Scholar] [CrossRef]
- Xu, J.; Qiao, Y.; Han, K.; Xu, C.; Dong, S.; Zhao, J. Modified Lemaire Lateral Extra-articular Tenodesis With the Iliotibial Band Strip Fixed on the Femoral Cortical Surface Reduces Laxity and Causes Less Overconstraint in the Anterolateral Lesioned Knee: A Biomechanical Study. Arthroscopy 2022, 38, 3162–3171. [Google Scholar] [CrossRef]
- Sigloch, M.; Coppola, C.; Hoermann, R.; Alt, P.; Schmoelz, W.; Mayr, R. Overconstraint Associated With a Modified Lemaire Lateral Extra-Articular Tenodesis Is Decreased by Using an Anterior Femoral Insertion Point in a Cadaveric Model. Arthroscopy, 2024; ahead of print. [Google Scholar] [CrossRef]
- Xu, J.; Han, K.; Lee, T.Q.; Xu, C.; Su, W.; Chen, J.; Yu, J.; Dong, S.; Zhao, J. Anterolateral Structure Reconstruction Similarly Improves the Stability and Causes Less Overconstraint in Anterior Cruciate Ligament-Reconstructed Knees Compared With Modified Lemaire Lateral Extra-articular Tenodesis: A Biomechanical Study. Arthroscopy 2022, 38, 911–924. [Google Scholar] [CrossRef]
- Jacquet, C.; Pioger, C.; Seil, R.; Khakha, R.; Parratte, S.; Steltzlen, C.; Argenson, J.N.; Pujol, N.; Ollivier, M. Incidence and Risk Factors for Residual High-Grade Pivot Shift After ACL Reconstruction With or Without a Lateral Extra-articular Tenodesis. Orthop. J. Sports Med. 2021, 9, 23259671211003590. [Google Scholar] [CrossRef] [PubMed]
- Marshall, D.C.; Silva, F.D.; Goldenberg, B.T.; Quintero, D.; Baraga, M.G.; Jose, J. Imaging Findings of Complications After Lateral Extra-Articular Tenodesis of the Knee: A Current Concepts Review. Orthop. J. Sports Med. 2022, 10, 23259671221114820. [Google Scholar] [CrossRef]
- Weber, A.E.; Zuke, W.; Mayer, E.N.; Forsythe, B.; Getgood, A.; Verma, N.N.; Bach, B.R.; Bedi, A.; Cole, B.J. Lateral Augmentation Procedures in Anterior Cruciate Ligament Reconstruction: Anatomic, Biomechanical, Imaging, and Clinical Evidence. Am. J. Sports Med. 2019, 47, 740–752. [Google Scholar] [CrossRef] [PubMed]
- Zhao, D.; Liang, G.H.; Pan, J.K.; Zeng, L.F.; Luo, M.H.; Huang, H.T.; Han, Y.H.; Lin, F.Z.; Xu, N.J.; Yang, W.Y.; et al. Risk factors for postoperative surgical site infections after anterior cruciate ligament reconstruction: A systematic review and meta-analysis. Br. J. Sports Med. 2023, 57, 118–128. [Google Scholar] [CrossRef] [PubMed]
- Duthon, V.B.; Magnussen, R.A.; Servien, E.; Neyret, P. ACL reconstruction and extra-articular tenodesis. Clin. Sports Med. 2013, 32, 141–153. [Google Scholar] [CrossRef]
- Lutz, C.; Casin, C.; Pioger, C.; Jacquot, X.; Jaeger, J.H.; Van Hille, W. Combined ACLR and lateral extra-articular tenodesis with a continuous iliotibial band autograft is a viable option in a population of athletes who participate in pivoting sports. Knee Surg. Sports Traumatol. Arthrosc. 2024, 33, 96–106. [Google Scholar] [CrossRef] [PubMed]
- Giusto, J.D.; Cohen, D.; Dadoo, S.; Grandberg, C.; Lott, A.; Hughes, J.D.; Ayeni, O.R.; Musahl, V. Lateral extra-articular tenodesis may be more cost-effective than independent anterolateral ligament reconstruction: A systematic review and economic analysis. J. ISAKOS 2024, 9, 689–698. [Google Scholar] [CrossRef] [PubMed]
- Sonnery-Cottet, B.; Lutz, C.; Daggett, M.; Dalmay, F.; Freychet, B.; Niglis, L.; Imbert, P. The Involvement of the Anterolateral Ligament in Rotational Control of the Knee. Am. J. Sports Med. 2016, 44, 1209–1214. [Google Scholar] [CrossRef]
- Wilson, T.C.; Kantaras, A.; Atay, A.; Johnson, D.L. Tunnel enlargement after anterior cruciate ligament surgery. Am. J. Sports Med. 2004, 32, 543–549. [Google Scholar] [CrossRef] [PubMed]
- Jette, C.; Gutierrez, D.; Sastre, S.; Llusa, M.; Combalia, A. Biomechanical comparison of anterolateral ligament anatomical reconstruction with a semi-anatomical lateral extra-articular tenodesis. A cadaveric study. Knee 2019, 26, 1003–1009. [Google Scholar] [CrossRef] [PubMed]
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Published by MDPI on behalf of the Lithuanian University of Health Sciences. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).