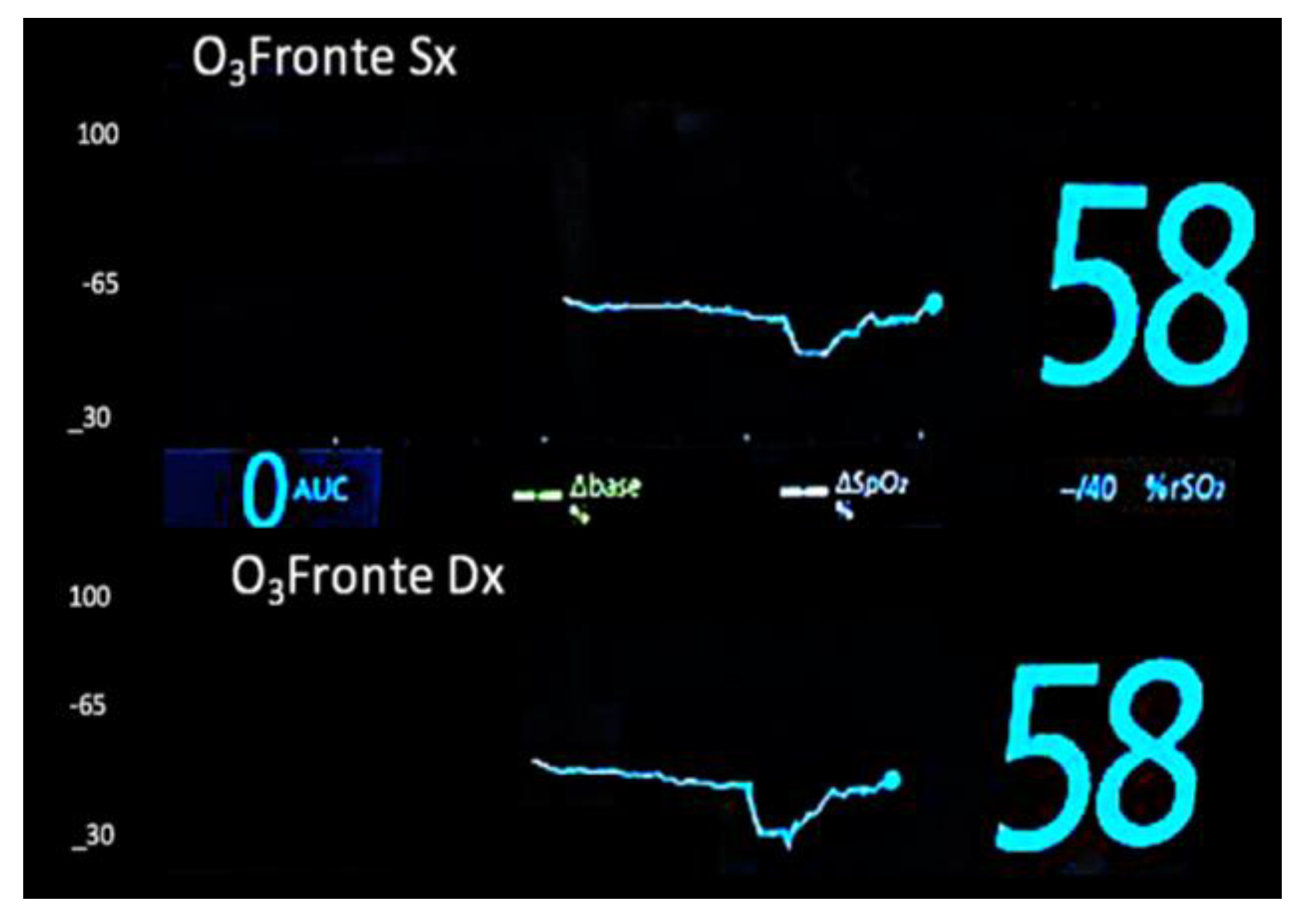
The Role of Continuous Monitoring of Venous Drainage Flow and Integrated Oxygen Extraction (ERiO2) via Bilateral Near-Infrared Spectroscopy in Cerebral Perfusion During Aortic Arch Surgery
Abstract
1. Introduction
2. Materials and Methods
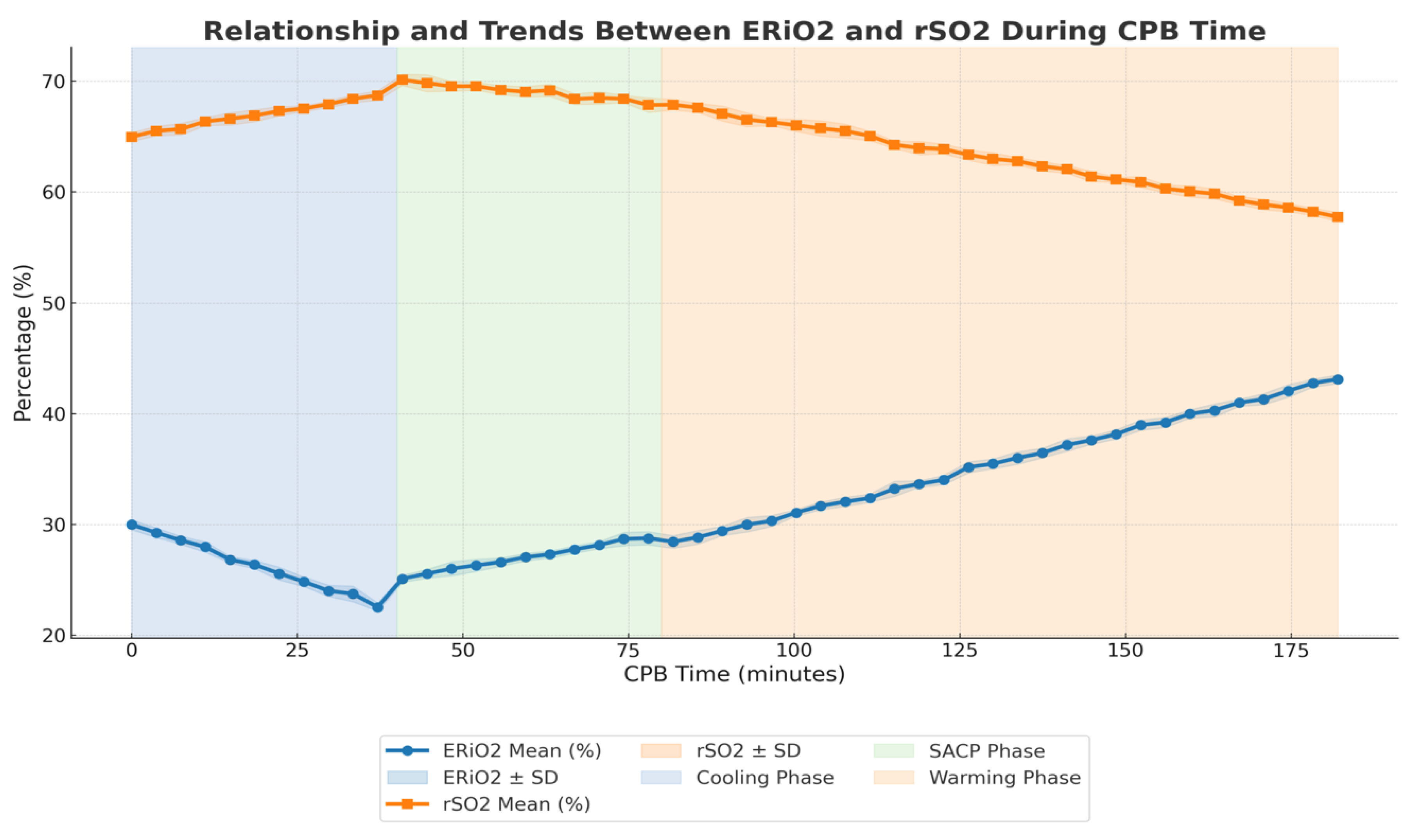
3. Results
4. Discussion
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Braverman, A.C. Acute aortic dissection: Clinician update. Circulation 2010, 122, 184–188. [Google Scholar] [CrossRef] [PubMed]
- Di Mauro, M.; Iacò, A.L.; Di Lorenzo, C.; Gagliardi, M.; Varone, E.; Al Amri, H.; Calafiore, A.M. Cold reperfusion before rewarming reduces neurological events after deep hypothermic circulatory arrest. Eur. J. Cardiothorac. Surg. 2013, 43, 168–173. [Google Scholar] [CrossRef] [PubMed]
- Yujian, Y.; Juan, L.; Peiyun, Z.; Yaoguang, F.; Khan, A.; Zhengwen, L. Application of Bilateral Cerebral Perfusion + Balloon Occlusion of Descending Aorta + Antegrade Perfusion of Lower Body in Debakey Type I Aortic Dissection. J. Coll. Physicians Surg. Pak. 2024, 34, 1484–1489. [Google Scholar] [CrossRef] [PubMed]
- Condello, I.; Montemurro, V.; De Rosis, M.G.; Nasso, G. Selective monitoring of superior and inferior vena cava drainage flows in bicaval cannulation: Potential clinical benefits of proximal junction placement on the CPB side. Perfusion 2024, 18, 2676591241295576. [Google Scholar] [CrossRef] [PubMed]
- Kazui, T. Total arch replacement with separated graft technique and selective antegrade cerebral perfusion. Ann. Cardiothorac. Surg. 2013, 2, 353–357. [Google Scholar] [CrossRef]
- Abdulwahab, H.A.M.; Kolashov, A.; Haneya, A.; Klump, H.; Moza, A.; Arab, M.F.; Shoaib, M.; Zayat, R.; Khattab, M.A. Temperature management in acute type A aortic dissection treatment: Deep vs. moderate hypothermic circulatory arrest. Is colder better? Front. Cardiovasc. Med. 2024, 11, 1447007. [Google Scholar] [CrossRef] [PubMed]
- Langenhorst, J.; Benkert, A.; Peterss, S.; Feuerecker, M.; Scheiermann, T.; Scheiermann, P.; Witte, M.; Benkert, A.; Bayer, A.; Prueckner, S.; et al. Agreement of in-ear temperature to core body temperature measures during invasive whole-body cooling for hypothermic circulatory arrest in aortic arch surgery. Sci. Rep. 2024, 14, 27607. [Google Scholar] [CrossRef]
- Peng, Q.; Cai, M.; Chen, X.; Lin, T.; Meng, W.; Guan, L.; Zhu, P.; Zheng, S.; Lu, J.; Zhou, P. Nadir oxygen delivery during cardiopulmonary bypass in acute type A aortic dissection repair. J. Thorac. Dis. 2023, 15, 4859–4868. [Google Scholar] [CrossRef]
- Luehr, M.; Bachet, J.; Mohr, F.W.; Etz, C.D. Modern temperature management in aortic arch surgery: The dilemma of moderate hypothermia. Eur. J. Cardiothorac. Surg. 2014, 45, 27–39. [Google Scholar] [CrossRef]
- Berger, T.; Rylski, B.; Czerny, M.; Kreibich, M. Selective antegrade cerebral perfusion: How to perfuse? Eur. J. Cardiothorac. Surg. 2023, 63, ezad139. [Google Scholar] [CrossRef] [PubMed]
- Friess, J.O.; Beeler, M.; Yildiz, M.; Guensch, D.P.; Levis, A.; Gerber, D.; Wollborn, J.; Jenni, H.; Huber, M.; Schönhoff, F.; et al. Determination of selective antegrade perfusion flow rate in aortic arch surgery to restore baseline cerebral near-infrared spectroscopy values: A single-centre observational study. Eur. J. Cardiothorac. Surg. 2023, 63, ezad047. [Google Scholar] [CrossRef] [PubMed]


| Variable | Value |
|---|---|
| Sample Size (n) | 10 |
| Mean Body Surface Area (BSA, m2) | 1.8 ± 0.1 |
| Mean BMI (kg/m2) | 26.5 ± 3.2 |
| Mean EuroSCORE | 7.8 ± 2.5 |
| Type A Dissections (urgent, n) | 4 |
| Aortic Arch Aneurysms (n) | 6 |
| Mean Age (years) | 64.3 ± 7.8 |
| Male (n, %) | 6, 60% |
| Hypertension (n, %) | 8, 80% |
| Diabetes (n, %) | 2, 20% |
| History of Smoking (n, %) | 5, 50% |
| Mean LVEF (%) | 55% ± 5% |
| Preoperative Neurological Deficits (n, %) | 0, None |
| Variable | Value |
|---|---|
| CPB Time (minutes) | 182 ± 15 |
| Cross-Clamp Time (minutes) | 98 ± 12 |
| Cooling Phase Duration (minutes) | 29 ± 3 |
| Reperfusion Phase Duration (minutes) | 10 ± 1.5 |
| Rewarming Phase Duration (minutes) | 40 ± 5 |
| Cerebral Perfusion Time (minutes) | 40 ± 6 |
| Circulatory Arrest Time (minutes) | 42 ± 7 |
| Target Core Temperature (°C) | 36.8 |
| SACP Flow Rate (mL/min) | 620 ± 30 |
| Venous Return Flow on SACP (mL/min) | 570 ± 25 |
| rSO2 SACP (%) | 65 ± 5% |
| ERiO2 SACP (%) | 28 ± 4% |
| Hemoglobin (Hb, g/dL) | 9.5 ± 1.0 |
| Flow During Cooling (L/min) | 4.00 ± 0.14 |
| Flow During Warming (L/min) | 5.00 ± 0.14 |
| DO2i During Cooling (mL/min/m2) | 320 ± 30 |
| DO2i During Warming (mL/min/m2) | 350 ± 35 |
| Mean Arterial Pressure (mmHg) | 65 ± 5 |
| Transfusion Rate (units/patient) | 1.2 ± 0.3 |
| Variable | Value |
|---|---|
| Neurological Deficits | None |
| Mechanical Ventilation Duration (hours) | 8.5 ± 2.3 |
| ICU Stay Duration (hours) | 48 ± 12 |
| Hospital Stay Duration (days) | 10 ± 3 |
| 30-day Mortality Rate (%) | 0% |
Disclaimer/Publisher’s Note: The statements, opinions and data contained in all publications are solely those of the individual author(s) and contributor(s) and not of MDPI and/or the editor(s). MDPI and/or the editor(s) disclaim responsibility for any injury to people or property resulting from any ideas, methods, instructions or products referred to in the content. |
© 2025 by the authors. Published by MDPI on behalf of the Lithuanian University of Health Sciences. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Condello, I.; Speziale, G.; Fiore, F.; Nasso, G. The Role of Continuous Monitoring of Venous Drainage Flow and Integrated Oxygen Extraction (ERiO2) via Bilateral Near-Infrared Spectroscopy in Cerebral Perfusion During Aortic Arch Surgery. Medicina 2025, 61, 226. https://doi.org/10.3390/medicina61020226
Condello I, Speziale G, Fiore F, Nasso G. The Role of Continuous Monitoring of Venous Drainage Flow and Integrated Oxygen Extraction (ERiO2) via Bilateral Near-Infrared Spectroscopy in Cerebral Perfusion During Aortic Arch Surgery. Medicina. 2025; 61(2):226. https://doi.org/10.3390/medicina61020226
Chicago/Turabian StyleCondello, Ignazio, Giuseppe Speziale, Flavio Fiore, and Giuseppe Nasso. 2025. "The Role of Continuous Monitoring of Venous Drainage Flow and Integrated Oxygen Extraction (ERiO2) via Bilateral Near-Infrared Spectroscopy in Cerebral Perfusion During Aortic Arch Surgery" Medicina 61, no. 2: 226. https://doi.org/10.3390/medicina61020226
APA StyleCondello, I., Speziale, G., Fiore, F., & Nasso, G. (2025). The Role of Continuous Monitoring of Venous Drainage Flow and Integrated Oxygen Extraction (ERiO2) via Bilateral Near-Infrared Spectroscopy in Cerebral Perfusion During Aortic Arch Surgery. Medicina, 61(2), 226. https://doi.org/10.3390/medicina61020226








