Abstract
Background and Objectives: Tactile sensibility is an important characteristic for evaluating the masticatory efficiency in different occlusal situations. When a tooth is extracted, relevant proprioceptors from the periodontal ligament get lost; and after the rehabilitation of this abscess by means of oral prosthesis, this sensibility decreases influencing masticatory function. Osseoperception is a sensitive phenomenon associated with dental implants that allows an increased tactile sensibility to those wearing implant prostheses. The purpose of this study was to determine the difference in tactile sensibility values between implant prosthesis, complete dentures, and natural teeth through a review of the available literature. Materials and Methods. In order to dissect the information, 24 articles from 2004 to 2021 were analyzed from MEDLINE, PubMed Central, and Web of Science databases. These articles were directly related to measuring tactile sensibility in different situations and demonstrating the influence of osseoperception in an improved masticatory function. Results: Tactile sensibility in implant prosthesis is slightly reduced compared with natural dentition but presents improved values with regard to complete dentures. Conclusions: Implant prosthesis are more effective during masticatory function than complete dentures, as they present an increased tactile sensibility, very similar to that present in natural dentition. This enhanced sensibility in implants is due to the osseoperception phenomenon.
1. Introduction
Tactile sensibility associated with teeth has a great relevance for achieving the proper behavior of the masticatory system. The periodontium has lots of different kinds of mechanoreceptors that are able to detect a low gauge stimulus, such as a small amount of pressure or position modifications. This sensitive phenomenon avoids the execution of great occlusal forces that may damage teeth, allowing a correct oral function. After tooth extraction, the receptors inside the periodontal ligament disappear, as well as the important sensitive information so useful during chewing [1]. For centuries, a lot of different types of prostheses have been designed to replace missing teeth with better or worse results. Complete dentures might be unstable and damage soft tissues, giving the patient unsatisfactory results. Currently, after the emergence, normalization, and protocolization of osseointegrated implants and their rehabilitations, a great alternative to conventional prostheses has been achieved [2] since implant prostheses are related to the osseoperception phenomenon that enables an improvement in functional integration.
Osseoperception consists of the sensation arising from mechanical stimulation of an implant prosthesis transmitted by mechanoreceptors from the masticatory system, along with a modification in central neural processing. Nowadays, the behavior of this sensibility is not well understood, and more clinical studies about this subject are needed. However, it is believed that mechanoreceptors from adjacent tissues are involved, such as masticatory muscles, temporomandibular joint, or gums. It is even thought that residual periodontal mechanoreceptors that remain after dental extraction might be responsible for capturing and transmitting osseoperception [3]. As a result of this mechanical sensibility, a remodeling of the central nervous system occurs in order to adapt itself to a new sensitive and motor function since cortical brain areas that were in charge of taking in some kind of stimulus acquire another sensitive goal by integrating implant-supported prostheses [4].
Anterior studies about osseoperception are aimed at monitoring this mechanical sensibility to see its origin. Specifically, two kinds of investigations are carried out in order to measure the influence of osseoperception: psychophysical studies and neurophysiological studies. Prevailing are the psychophysical studies, as they are able to connect patients’ psychological response with receptors’ sensitive response [4,5].
The theoretical basis of these studies is the implant’s tactile sensibility, which allows, for instance, the achievement of an inhibitory muscle response against traumatic occlusal forces by detecting a really fine stimulus.
Tactile sensibility can also be divided into two types: active tactile sensibility and passive tactile sensibility. Active tactile sensibility gauges patients’ perception when detecting some strange element between teeth during masticatory function, and it is measured in micrometers. On the other hand, passive tactile sensibility consists of the lower force that can be detected when applied to an implant or a natural tooth and is measured in Newtons. Additionally, it is an independent parameter from the patient’s perception. The main difference between these kinds of sensibility is that the passive one only measures individual neuronal receptors that exist on peri-implant areas; while the active one evaluates the whole masticatory function, regarding both receptors near implants and those ones located in more distant areas, such as the temporomandibular joint or masticatory muscles [4].
In this context, the purpose of this study was to determine the differences in tactile sensibility values between conventional complete dentures, implant-supported prostheses, and natural dentition. Regarding implant-supported prostheses, the study analyzed the influence of osseoperception on increased tactile sensibility.
2. Materials and Methods
2.1. Study Design
A review of tactile sensibility linked to osseoperception phenomenon was carried out, including articles during the period comprising January 2004 to December 2021 covering only articles published in English.
We performed study selection according to the PRISMA (Preferred Reporting Items for Systematic Review and Meta-Analyses) guidelines for reporting systematic reviews. This revision has been registered in PROSPERO (registration code 301737).
The search strategy was conducted using the population, intervention, comparison, and outcome (PICO) framework based on the following question: “Do prostheses on implants have greater osseoperception than conventional prostheses?”
To answer this question, a sample population group of patients undergoing treatment with implant prostheses was selected
2.2. Inclusion Criteria
Both research and review articles were included. At first, we added review articles that explained in a clear way the osseoperception phenomenon and its relation between tactile sensibility. Second, we studied research articles consisting of psychophysical and neurophysiological investigations, such as the measurement of active and tactile sensibility in different prosthetic rehabilitations, using interocclusal foils or customized devices.
2.3. Exclusion Criteria
Studies concerning the links between osseoperception and implant integration or other parameters not related to tactile sensibility were not included, except for those concerning periodontal neurophysiology; nor did we include those articles in which the full text was unavailable. Finally, 107 articles were rejected from this investigation due to their lack of a relationship with the review objectives or for being duplicates, as shown in the flowchart (Figure 1).
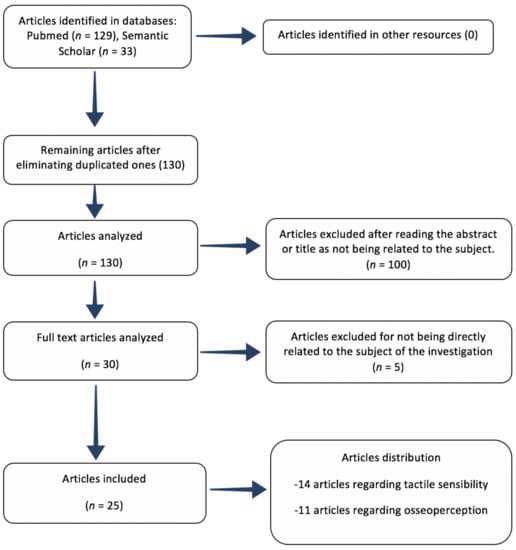
Figure 1.
PubMed flowchart summarizing the review process.
2.4. Variables
Among all studies reviewed, the relation between osseoperception and tactile sensibility in natural dentition and some kind of prosthetic rehabilitation was assessed.
2.5. Resources
Bibliographical Resources
The medical database PubMed–MEDLINE was consulted, as well as Semantic Scholar. Social media ResearchGate was used as a complement in order to obtain some full-text articles under consent from their authors.
Keywords used were “osseoperception”, “tactile sensibility”, “interocclusal perception”, “interocclusal thickness”, and “oral somatosensory function”. A cross-search was also performed using these terms: “osseoperception and tactile sensibility” and “osseoperception and interocclusal thickness”.
3. Results
Twenty-five articles were chosen among all the literature reviewed so as to analyze the influence of osseoperception on an improved tactile sensibility and its related values in every prosthetic rehabilitation or natural dentition.
Following, there is a flowchart summarizing article selection (Figure 1) as well as two tables; first one showing all review articles (Table 1) and second one showing all clinical investigations (Table 2). These tables also describe every author, year of publication, type of investigation, study objective, and results.

Table 1.
Review article results.

Table 2.
Clinical investigation results.
A first clinical study that demonstrated the presence of nervous fibers around implants in humans was conducted by Corpas et al. [16], showing that it was necessary to extract failed implants from patients’ bone and to analyze them by using a microscope. Research results showed the presence of mielinic and amielinic fibers in Haversian canals of bone tissues surrounding implant threads. In addition to this, there was a study that demonstrated the presence of changes in the cortical brain after rehabilitating dental abscesses with implants [20].
Analyzing tactile sensibility, there was a higher number of investigations of active tactile sensibility than passive tactile sensibility because active tactile sensibility is easier to measure mechanically and better reflects masticatory function clinically.
The main investigations of tactile sensibility thresholds in different prosthetic rehabilitations and natural teeth were those from Enkling [19,21,22,25], Shala [13], Reveredo [17], Kazemi [18], Grieznis [23], or Batista [24]. In conclusion, the thresholds in implant-supported prosthesis were lower than those in complete dentures and very similar to those present in natural dentition, and this fact allowed an increased sensibility in dental implants that facilitated the functional integration of these prostheses [7,8,11].
4. Discussion
Nowadays the behavior of osseoperception is not well known, as there are not many studies concerning this subject, especially studies related to active and passive tactile sensibility. Some studies are focused on the mechanisms of osseoperception in the cortical brain [20,28], and others describe how this phenomenon influences somatosensorial perception—for instance, the review from Haggard [29]. At first glance, the review articles are useful for understanding how osseoperception works and the way it is related to tactile sensibility.
Among all of the reviews selected referring to osseoperception, the studies of Mishra and Bhatnagar stood out. Mishra [2] concludes that osseoperception is the phenomenon that causes an improved functional integration of dental implants, which is represented by an increased tactile sensibility. Bhatnaghar’s review [1] also states that there is a clear improvement in function regarding implant-supported prosthesis thanks to osseoperception and tactile sensibility [30].
Other reviews such as those by Abarca, Van Steenberghe, Jacobs, and Kumar [3,4,11,31] are focused on the analysis of osseoperception and its relation to masticatory muscles and its neurophysiological implications. Studies show how an implant prosthesis presents a better physiological and functional integration than complete dentures and that its behavior is more natural, as well as the importance of a correct occlusion [32,33]. However, although their masticatory efficiency is correct, patients with an implant prosthesis suffer more muscle fatigue and lower biting force under extreme effort than those preserving natural dentition [34]. Second, in Feine’s investigation [35], it is explained how the evaluation of masticatory ability in prosthetic rehabilitation is a subjective parameter, suggesting that further studies must rely on patients’ opinions about comfort sensations while wearing a prosthesis rather than its stability.
Tanaka [14] also performed an investigation that concretely measured the influence of osseoperception in oral function by using immediate loading protocols and analyzing the adaptation results after rehabilitation. Results showed a gradual improvement in bite force, not including any improvement in masticatory efficiency or food roughness perception [36]. Regarding studies about tactile sensibility in natural teeth, it is important to analyze Trulsson’s review [9], which is focused on describing periodontal receptors and their relevant proprioceptive function for a proper functioning of a masticatory system that is affected after dental extractions [37,38,39].
Among active tactile sensibility investigations, Enkling’s research stands out [19], which intended to establish a comparison of perception between implants and natural teeth by using fine copper leaf gauges that patients were asked to notice during chewing. Results showed a really low sensibility threshold that was very close to natural dentition. In addition, he stated the great relevance of a correct occlusal setting, as some sensibility values are as low as micrometers in size, which suggests that tiny interferences in occlusion can be perceived by the patient in both implant prosthesis and natural teeth [40].
Another research study concerning active tactile sensibility was conducted by Shala [13], who studied sensibility associated with complete denture carriers. This investigation compared patients who had been wearing prostheses for several years with respect to new carriers, in order to measure the adaptation during the passage of the time. Regarding these results, after wearing a prosthesis for fifteen weeks, the sensibility suffered an improvement, although the sensibility threshold remained three times higher than natural dentition.
Kazemi [18] also investigated active tactile sensibility in implants with respect to natural teeth, concluding that sensibility in implants is slightly reduced compared with natural teeth. In Reveredo’s [17] research, the active tactile sensibility threshold was increased two times with respect to natural dentition.
One of the few available studies about passive tactile sensibility was that of Grieznis’ [23], which compared sensibility between implants and natural teeth. In passive studies, interocclusal leaf gauges are not needed for measuring perception, so direct stimulus was applied on the implants without any kind of patient participation. In this case, the threshold discrepancy was much higher than that regarding active studies, as the implant threshold was also higher. This was due to the lack of participation of remote receptors far away from peri-implant areas, which are not included in passive studies [41,42].
According to the bibliography reviewed, osseoperception is a phenomenon whose existence is proved, yet it is not well or accurately known how it works. In 2005, a consensus statement was published [12] involving several investigators dedicated to the study of osseoperception in which they regarded osseoperception as the mechanical sensibility related to dental implants. This statement suggested that the presence of mechanoreceptors located in muscle, articular, mucous, and periosteal tissues was responsible for this sensibility, along with a neurophysiological change in superior neural centers. Subsequently, there have been more articles studying this phenomenon and its repercussions in correct oral function [43,44].
After the Corpas [16] investigation, the presence of nervous fibers surrounding peri-implant tissues was clear, so that existence of osseoperception became more evident. To be able to make a more accurate statement, more studies about active and passive sensibility are needed, as currently they are very scarce.
There is a consensus about considering that both active and passive tactile sensibility are increased in patients who have been rehabilitated with implant prosthesis compared with those wearing complete dentures, and this is due to osseointegration. Otherwise, differences in sensibility values present large discrepancies between some studies, causing contradictory results in some cases. This happens fundamentally because of the lack of homogeneity in some parameters such as research groups, experimental methods, or statistical approach. For instance, Kazemi [18] describes the wide differences in active sensibility values while studying bibliographical references in which the rank varied from 10 to 100 μm. Generally, sensibility thresholds in implants are higher than those in natural dentition, although they are closer to them than those in complete dentures, as some investigators such as Enkling, Kazemi, or Reveredo assert [17,18,25].
It is interesting to note how a difference between thresholds increases in passive tactile sensibility studies, as in the Grieznis study [23]; this is due to the fact that during this kind of procedure there is an activation of peri-implant proprioceptors, while receptors from other areas such as masticatory muscles or the temporomandibular joint keep quiescent.
There is a general coincidence in every investigation about the subject, and it consists of the really low sensibility threshold in both natural dentition and implant prosthesis and the response to very fine stimuli, as the detection of tiny elements with a few micrometers of thickness becomes possible. If we extrapolate these results to daily clinical performance, it is easy to realize the effects of our rehabilitations in masticatory function. Small occlusal variations can be detected by the patients, and tiny interferences may cause important occlusal alterations. This fact reaffirms the relevance of a correct occlusal settling after performing any prosthetic rehabilitation [23].
5. Conclusions
Implant prostheses present an increased tactile sensibility compared with complete dentures, and their values are closer to those in natural dentition, as have been shown in neurophysiological and psychophysical studies. This improved sensibility entails a better masticatory function in patients rehabilitated with implant-supported prostheses. As a result, these rehabilitations are a great alternative to complete dentures when treating edentulism.
Osseoperception is the phenomenon responsible for this upgrade of sensory perception in these kind of rehabilitations, although its operation is not well known yet.
In order to understand osseoperception in detail and to evaluate more precisely the tactile sensibility of implant prostheses, more studies are needed, and these investigations must have outcome criteria that are more homogeneous.
Author Contributions
Conceptualization, D.G.-G. and J.L.-M.; methodology, J.F.-F.; software, I.D.-Z.; validation, J.L.-M. and J.F.-F.; formal analysis, J.F.-F.; investigation, I.D.-Z.; resources, D.G.-G.; data curation, D.G.-G.; writing—original draft preparation, D.G.-G.; writing—review and editing, J.F.-F.; visualization, I.D.-Z.; supervision, J.L.-M.; project administration, J.F.-F.; funding acquisition, D.G.-G. All authors have read and agreed to the published version of the manuscript.
Funding
This research received no external funding.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
Not applicable.
Conflicts of Interest
The authors declare they have no potential conflict of interest with respect to the research, authorship, and/or publication of this article.
References
- Bhatnagar, V.M.; Karani, J.T.; Khanna, A.; Badwaik, P.; Pai, A. Osseoperception: An Implant Mediated Sensory Motor Control—A Review. J. Clin. Diagn. Res. 2015, 9, 18–20. [Google Scholar] [CrossRef]
- Mishra, S.K.; Chowdhary, R.; Chrcanovic, B.R.; Brånemark, P.I. Osseoperception in Dental Implants: A Systematic Review. J. Prosthodont. 2016, 25, 185–195. [Google Scholar] [CrossRef]
- Johnsen, S.E.; Trulsson, M. Receptive field properties of human periodontal afferents responding to loading of premolar and molar teeth. J. Neurophysiol. 2003, 89, 1478–1487. [Google Scholar] [CrossRef]
- Jacobs, R.; Van Steenberghe, D. From osseoperception to implant-mediated sensory-motor interactions and related clinical implications. J. Oral Rehabil. 2006, 33, 282–292. [Google Scholar] [CrossRef]
- Tabot, G.A.; Kim, S.S.; Winberry, J.E.; Bensmaia, S.J. Restoring tactile and proprioceptive sensation through a brain interface. Neurobiol. Dis. 2015, 83, 191–198. [Google Scholar] [CrossRef]
- Flanagan, D. Bite force and dental implant treatment: A short review. Med. Devices 2017, 10, 141–148. [Google Scholar] [CrossRef] [PubMed]
- Higaki, N.; Goto, T.; Ishida, Y.; Watanabe, M.; Tomotake, Y.; Ichikawa, T. Do sensation differences exist between dental implants and natural teeth?: A meta-analysis. Clin. Oral. Impl. Res. 2014, 25, 1307–1310. [Google Scholar] [CrossRef] [PubMed]
- Kumar, L. Osseoperception in Implants Supported Prosthesis—A Review. Online J. Med. Med. Sci. Res. 2012, 1, 1–4. [Google Scholar]
- Trulsson, M. Sensory-motor function of human periodontal mechanoreceptors. J. Oral Rehab. 2006, 33, 262–273. [Google Scholar] [CrossRef] [PubMed]
- Abarca, M.; Van Steenberghe, D.; Malevez, C.; Jacobs, R. The neurophysiology of osseointegrated oral implants. A clinically underestimated aspect. J. Oral Rehab. 2006, 33, 161–169. [Google Scholar] [CrossRef]
- Van Steenberghe, D.; Jacobs, R. Jaw motor inputs originating from osseointegrated oral implants. J. Oral Rehab. 2006, 33, 274–281. [Google Scholar] [CrossRef] [PubMed]
- Klineberg, I.; Calford, M.B.; Dreher, B.; Henry, P.; Macefield, V.; Miles, T.; Trulsson, M. A consensus statement on osseoperception. Clin. Exp. Pharmacol. Physiol. 2005, 32, 145–146. [Google Scholar] [CrossRef] [PubMed]
- Shala, K.S.; Dula, L.J.; Pustina-Krasniqi, T.; Bicaj, T.; Ahmedi, E.F.; Lila-Krasniqi, Z.; Tmava-Dragusha, A. Evaluation of Sensibility Threshold for Interocclusal Thickness of Patients Wearing Complete Dentures. Int. J. Dent. 2017, 1, 1–5. [Google Scholar] [CrossRef]
- Tanaka, M.; Bruno, C.; Jacobs, R.; Torisu, T.; Murata, H. Short-term follow-up of masticatory adaptation after rehabilitation with an immedately loaded implant-supported prosthesis: A pilot assessment. Int. J. Implant. Dent. 2017, 3, 1–7. [Google Scholar] [CrossRef] [PubMed]
- Bakshi, P.V.; Thakur, S.; Kulkami, S. Perception by Osseointegrated Dental Implants Supporting a Fixed Prosthesis: A Prospective Study. Int. J. Oral Maxillofac. Implant. 2017, 32, 1346–1350. [Google Scholar] [CrossRef]
- dos Santos Corpas, L.; Lambrichts, I.; Quirynen, M.; Collaert, B.; Politis, C.; Vrielinck, L.; Jacobs, R. Peri-implant bone innervation: Histological findings in humans. Eur. J. Oral Implantol. 2014, 7, 283–292. [Google Scholar]
- Reveredo, A.M.; Shetty, S.; Babu, C.S.; Kumar, G.S.; Priya, K.S.; Pandurangappa, R.; Shetty, A. Evaluation of active tactile perception of single tooth implant prosthesis. Int. J. Oral Implantolol. Clin. Res. 2013, 4, 1–6. [Google Scholar]
- Kazemi, M.; Geramipanah, F.; Negahdari, R.; Rakhshan, V. Active tactile sensibility of single-tooth implants versus natural dentition: A split-mouth double-blind randomized clinical trial. Clin. Implant. Dent. Relat. Res. 2014, 16, 947–955. [Google Scholar] [CrossRef]
- Enkling, N.; Heussner, S.; Nicolay, C.; Bayer, S.; Mericske-Stern, R.; Utz, K.H. Tactile sensibility of single-tooth implants and natural teeth under local anesthesia of the natural antagonistic teeth. Clin. Implant. Dent. Relat. Res. 2012, 14, 273–280. [Google Scholar] [CrossRef]
- Habre-Hallage, P.; Dricot, L.; Jacobs, R.; van Steenberghe, D.; Reychler, H.; Grandin, C.B. Brain plasticity and cortical correlates of osseoperception revealed by punctate mehanical stimulation of osseointegrated oral implants during fMRI. Eur. J. Oral Implantolol. 2012, 5, 175–190. [Google Scholar]
- Enkling, N.; Utz, K.H.; Bayer, S.; Stern, R.M. Osseoperception: Active tactile sensibility of osseointegrated dental implants. Int. J. Oral Maxillofac. Implant. 2010, 25, 1159–1167. [Google Scholar]
- Enkling, N.; Nicolay, C.; Bayer, S.; Mericske-Stern, R.; Utz, K.-H. Investigating interocclusal perception in tactile teeth sensibility using symmetric and asymmetric analysis. Clin. Oral Investig. 2010, 14, 683–690. [Google Scholar] [CrossRef][Green Version]
- Grieznis, L.; Apse, P.; Blumfelds, L. Passive tactile sensibility of teeth and osseointegrated dental implants in the maxilla. Stomatologija 2010, 12, 80–86. [Google Scholar]
- Batista, M.; Bonachela, W.; Soares, J. Progressive recovery of osseoperception as a function of the cobination of implant-suported prostheses. Clin. Oral Impl. Res. 2008, 19, 565–569. [Google Scholar] [CrossRef]
- Enkling, N.; Nicolay, C.; Utz, K.H.; Jöhren, P.; Wahl, G.; Mericske-Stern, R. Tactile sensibility of single-tooth implants and natural teeth. Clin. Oral Impl. Res. 2007, 18, 231–233. [Google Scholar] [CrossRef]
- El Sheik, A.M. Passive tactile sensibility in edentulous subjects treated with dental implants: A pilot study. J. Prosthet. Dent. 2004, 91, 26–32. [Google Scholar] [CrossRef]
- Hoshino, K.; Miura, H.; Morikawa, O.; Kato, H.; Okada, D.; Shinki, T. Influence of occlusal height for an implant prosthesis on the periodontal tissues of the antagonist. J. Med. Dent. Sci. 2004, 51, 187–196. [Google Scholar]
- Teichert, M.; Bolz, J. How Senses Work Together: Cross-Modal Interactions between Primary Sensory Cortices. Neural Plast. 2018, 2018, 11. [Google Scholar] [CrossRef] [PubMed]
- Haggard, P.; de Boer, L. Oral Somatosensory awareness. Neurosci. Biobehav. Rev. 2014, 47, 469–484. [Google Scholar] [CrossRef]
- Fugazzotto, P.A. Success and failure rates of osseointegrated implants in function in regenerated bone for 72 to 133 months. Int. J. Oral Maxillofac. Implant. 2005, 20, 77–83. [Google Scholar]
- Kumar, A.; Castrillon, E.; Trulsson, M.; Svensson, K.G.; Svensson, P. Fine motor control of the jaw following alteration of orofacial afferent inputs. Clin. Oral Investig. 2017, 21, 613–626. [Google Scholar] [CrossRef]
- Gross, M.D. Occlusion in implant dentistry. A review of the literature of prosthetic determinants and current concepts. Aust. Dent. J. 2008, 53, S60–S68. [Google Scholar] [CrossRef]
- Kayumi, S.; Takayama, Y.; Yokoyama, A.; Ueda, N. Effect of bite force in occlusal adjustment of dental implants on the distribution of occlusal pressure: Comparison among three bite forces in occlusal adjustment. Int. J. Implant. Dent. 2015, 1, 14. [Google Scholar] [CrossRef]
- Ysander, M.; Brånemark, R.; Olmarker, K.; Myers, R.R. Intramedullary osseointegration: Development of a rodent model and study of histology and neuropeptide changes around titanium implants. J. Rehabil. Res. Dev. 2001, 38, 183–190. [Google Scholar] [PubMed]
- Feine, J.S.; Lund, J.P. Measuring chewing ability in randomized controlled trials with edentulous populations wearing implant prostheses. J. Oral Rehab. 2006, 33, 301–308. [Google Scholar] [CrossRef] [PubMed]
- Fernandes, C.P.; Glantz, P.O.; Svensson, S.A.; Bergmark, A. A novel sensor for bite force determinations. Dent. Mater. 2003, 19, 118–126. [Google Scholar] [CrossRef]
- Nagasawa, M.; Takano, R.; Maeda, T.; Uoshima, K. Observation of the bone surrounding an overloaded implant in a novel rat model. Int. J. Oral Maxillofac. Implant. 2013, 28, 109–116. [Google Scholar] [CrossRef]
- Ben-Gal, G.; Lipovetsky-Adler, M.; Haramaty, O.; Sharon, E.; Smidt, A. Existing concepts and a search for evidence: A review on implant occlusion. Compend. Contin. Educ. Dent. 2013, 34, 26–31. [Google Scholar] [PubMed]
- Miki, K.; Honma, S.; Ebara, S.; Kumamoto, K.; Murakami, S.; Wakisaka, S. Changes in the Distribution of Periodontal Nerve Fibers during Dentition Transition in the Cat. PLoS ONE 2015, 10, e0129826. [Google Scholar] [CrossRef]
- Nishiuraa, H.; Tabatab, T.; Watanabea, M. Response properties of slowly and rapidly adapting periodontal mechanosensitive neurones in the primary somatosensory cortex of the cat. Arch. Oral Biol. 2000, 45, 833–842. [Google Scholar] [CrossRef]
- Jacobs, R.; Brånemark, R.; Olmarker, K.; Rydevik, B.; Steenberghe, D.V.; Brånemark, P.I. Evaluation of the psychophysical detection threshold level for vibrotactile and pressure stimulation of prosthetic limbs using bone anchorage or soft tissue support. Prosthet. Orthot. Int. 2000, 24, 133–142. [Google Scholar] [CrossRef] [PubMed]
- Lambrichts, I.; Creemers, J.; van Steenberghe, D. Morphology of neural endings in the human periodontal ligament: An electron microscopic study. J. Periodontal. Res. 1992, 27, 191–196. [Google Scholar] [CrossRef] [PubMed]
- Ahn, D.; Doutova, E.; McNaughton, K.; Light, A.; Närhi, M.; Maixner, W. Functional properties of tooth pulp neurons responding to thermal stimulation. J. Dent. Res. 2012, 91, 401–406. [Google Scholar] [CrossRef] [PubMed]
- Bodegård, A.; Geyer, S.; Grefkes, C.; Zilles, K.; Roland, P.E. Hierarchicalprocessing of tactile shape in the human brain. Neuron 2001, 31, 317–328. [Google Scholar] [CrossRef]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).