Hybrid Surgery for Severe Mitral Valve Calcification: Limitations and Caveats for an Open Transcatheter Approach
Abstract
1. Introduction
2. Methods
2.1. Study Design
2.2. Search Strategy
2.3. Definition of Parameters
- Diagnosis of valvular lesions was made in accordance with the ESC guidelines [15].
- Adverse cerebrovascular events were defined as new-onset postoperative neurological symptoms, which were accompanied by a new computed tomography (CT) confirmed central nervous system (CNS) lesion [16].
- Preoperative risk assessment was performed by determining the European System for Cardiac Operative Risk Evaluation II (EuroSCORE II).
- Operative mortality was defined as in-hospital mortality and mortality within 30 days, regardless of cause.
2.4. Follow-Up
2.5. Statistical Analysis
3. Results
3.1. Patient and Imaging Characteristics
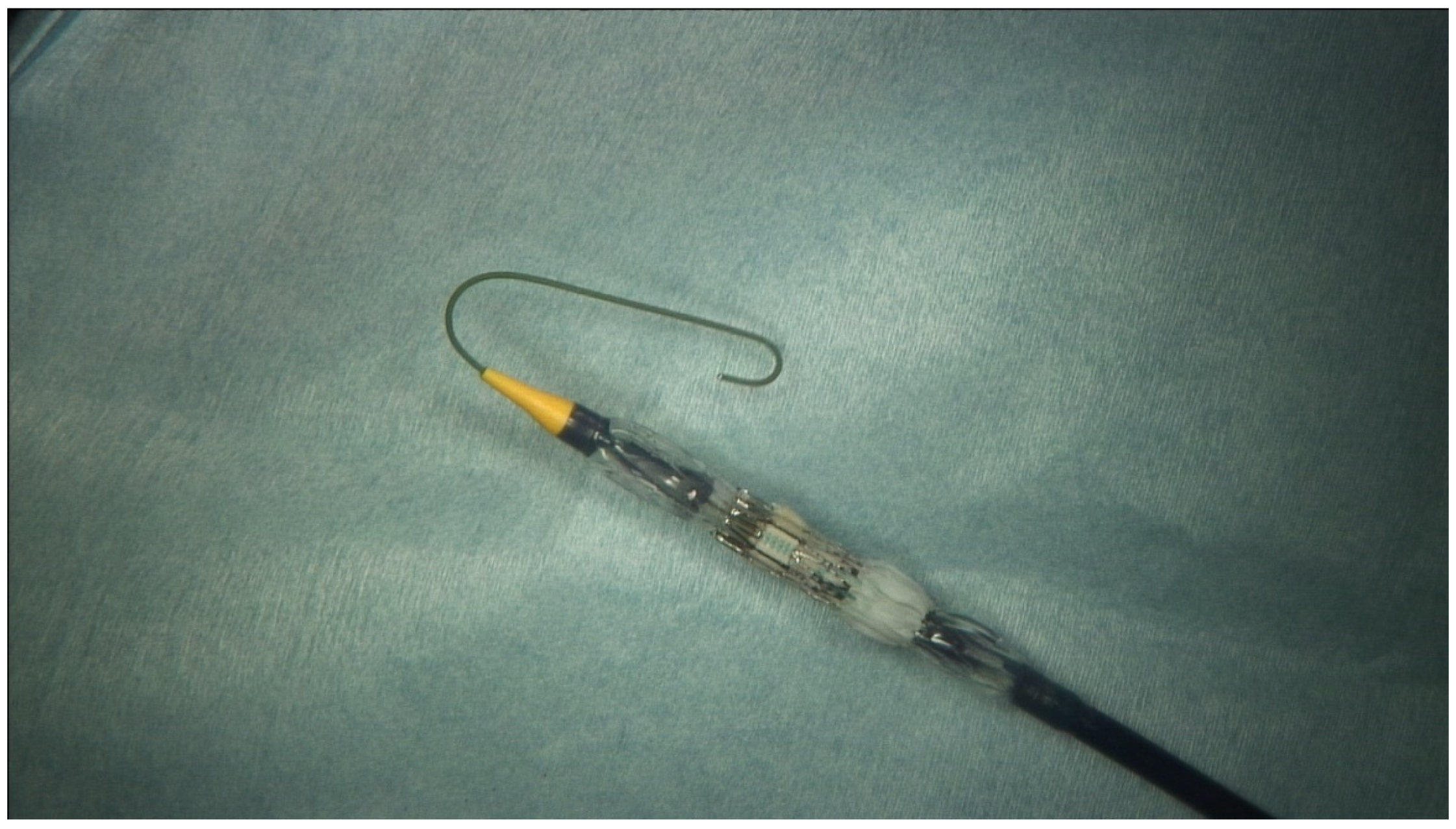
3.2. Operational Management
3.3. Concomitant Procedures
3.4. Postoperative Outcomes
3.5. Follow-Up
4. Discussion
4.1. Choice of Prosthesis
4.2. Operative Considerations
4.3. Limitations
5. Conclusions
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Conflicts of Interest
References
- Massera, D.; Trivieri, M.G.; Andrews, J.P.; Sartori, S.; Abgral, R.; Chapman, A.; Jenkins, W.S.; Vesey, A.T.; Doris, M.K.; Pawade, T.A.; et al. Disease Activity in Mitral Annular Calcification. Circ. Cardiovasc. Imaging 2019, 12, e008513. [Google Scholar] [CrossRef] [PubMed]
- Bedeir, K.; Kaneko, T.; Aranki, S. Current and evolving strategies in the management of severe mitral annular calcification. J. Thorac. Cardiovasc. Surg. 2018, 157, 555–566. [Google Scholar] [CrossRef]
- Feindel, C.M.; Tufail, Z.; David, T.E.; Ivanov, J.; Armstrong, S. Mitral valve surgery in patients with extensive calcification of the mitral annulus. J. Thorac. Cardiovasc. Surg. 2003, 126, 777–781. [Google Scholar] [CrossRef]
- Karlson, K.J.; Ashraf, M.M.; Berger, R.L. Rupture of Left Ventricle Following Mitral Valve Replacement. Ann. Thorac. Surg. 1988, 46, 590–597. [Google Scholar] [CrossRef]
- El Sabbagh, A.; Eleid, M.F.; Foley, T.A.; Al-Hijji, M.A.; Daly, R.C.; Rihal, C.S.; Said, S.M. Direct transatrial implantation of balloon-expandable valve for mitral stenosis with severe annular calcifications: Early experience and lessons learned†. Eur. J. Cardio-Thorac. Surg. 2017, 53, 162–169. [Google Scholar] [CrossRef]
- Praz, F.; Khalique, O.K.; Lee, R.; Veeragandham, R.; Russell, H.; Guerrero, M.; Islam, A.M.; Deaton, D.W.; Kaneko, T.; Kodali, S.K.; et al. Transatrial implantation of a transcatheter heart valve for severe mitral annular calcification. J. Thorac. Cardiovasc. Surg. 2018, 156, 132–142. [Google Scholar] [CrossRef]
- Guerrero, M.; Dvir, D.; Himbert, D.; Urena, M.; Eleid, M.; Wang, D.D.; Greenbaum, A.; Mahadevan, V.S.; Holzhey, D.; O’Hair, D.; et al. Transcatheter Mitral Valve Replacement in Native Mitral Valve Disease With Severe Mitral Annular Calcification: Results From the First Multicenter Global Registry. JACC Cardiovasc. Interv. 2016, 9, 1361–1371. [Google Scholar] [CrossRef] [PubMed]
- Murashita, T.; Suri, R.M.; Daly, R.C. Sapien XT Transcatheter Mitral Valve Replacement under Direct Vision in the Setting of Significant Mitral Annular Calcification. Ann. Thorac. Surg. 2016, 101, 1171–1174. [Google Scholar] [CrossRef]
- Dahle, G.; Rein, K.A.; Fiane, A.E. Edwards Sapien Xt in Native Stenotic Mitral Valve, Open Technique on Cardiopulmonary Bypass: An Option, but Safe? Innov. Technol. Tech. Cardiothorac. Vasc. Surg. 2016, 11, 288–290. [Google Scholar] [CrossRef] [PubMed]
- Yoon, S.-H.; Whisenant, B.K.; Bleiziffer, S.; Delgado, V.; Dhoble, A.; Schofer, N.; Eschenbach, L.; Bansal, E.; Murdoch, D.J.; Ancona, M.; et al. Outcomes of transcatheter mitral valve replacement for degenerated bioprostheses, failed annuloplasty rings, and mitral annular calcification. Eur. Heart J. 2018, 40, 441–451. [Google Scholar] [CrossRef]
- Urena, M.; Brochet, E.; LeComte, M.; Kerneis, C.; Carrasco, J.L.; Ghodbane, W.; Abtan, J.; Alkhoder, S.; Raffoul, R.; Iung, B.; et al. Clinical and haemodynamic outcomes of balloon-expandable transcatheter mitral valve implantation: A 7-year experience. Eur. Heart J. 2018, 39, 2679–2689. [Google Scholar] [CrossRef]
- Guerrero, M.; Urena, M.; Himbert, D.; Wang, D.D.; Eleid, M.; Kodali, S.; George, I.; Chakravarty, T.; Mathur, M.; Holzhey, D.; et al. 1-Year Outcomes of Transcatheter Mitral Valve Replacement in Patients With Severe Mitral Annular Calcification. J. Am. Coll. Cardiol. 2018, 71, 1841–1853. [Google Scholar] [CrossRef]
- Russell, H.M.; Guerrero, M.E.; Salinger, M.H.; Manzuk, M.A.; Pursnani, A.K.; Wang, D.; Nemeh, H.; Sakhuja, R.; Melnitchouk, S.; Pershad, A.; et al. Open Atrial Transcatheter Mitral Valve Replacement in Patients With Mitral Annular Calcification. J. Am. Coll. Cardiol. 2018, 72, 1437–1448. [Google Scholar] [CrossRef]
- Stewart, L.A.; Clarke, M.; Rovers, M.; Riley, R.D.; Simmonds, M.; Stewart, G.; Tierney, J.F. Preferred Reporting Items for a Systematic Review and Meta-analysis of Individual Participant Data: The PRISMA-IPD statement. JAMA 2015, 313, 1657–1665. [Google Scholar] [CrossRef] [PubMed]
- Vahanian, A.; Beyersdorf, F.; Praz, F.; Milojevic, M.; Baldus, S.; Bauersachs, J.; Capodanno, D.; Conradi, L.; De Bonis, M.; De Paulis, R.; et al. 2021 ESC/EACTS Guidelines for the management of valvular heart disease. Eur. Heart J. 2021, 60, 727–800. [Google Scholar] [CrossRef]
- Arrowsmith, J.E.; Grocott, H.P.; Reves, J.G.; Newman, M.F. Central nervous system complications of cardiac surgery. Br. J. Anaesth. 2000, 84, 378–393. [Google Scholar] [CrossRef]
- Price, J.; Glineur, D.; De Kerchove, L.; El Khoury, G. Mitral Valve Repair is Feasible Following Extensive Decalcification and Reconstruction of the Atrioventricular Groove. J. Heart Valve Dis. 2015, 24, 46–52. [Google Scholar] [PubMed]
- Papadopoulos, N.; Dietrich, M.; Christodoulou, T.; Moritz, A.; Doss, M. Midterm Survival after Decalcification of the Mitral Annulus. Ann. Thorac. Surg. 2009, 87, 1143–1147. [Google Scholar] [CrossRef]
- Asselbergs, F.W.; Mozaffarian, D.; Katz, R.; Kestenbaum, B.; Fried, L.F.; Gottdiener, J.S.; Shlipak, M.G.; Siscovick, D.S. Association of renal function with cardiac calcifications in older adults: The cardiovascular health study. Nephrol. Dial. Transplant. 2008, 24, 834–840. [Google Scholar] [CrossRef]
- Fox, C.S.; Vasan, R.S.; Parise, H.; Levy, D.; O’Donnell, C.J.; D’Agostino, R.B.; Benjamin, E.J. Mitral Annular Calcification Predicts Cardiovascular Morbidity and Mortality: The Framingham Heart Study. Circulation 2003, 107, 1492–1496. [Google Scholar] [CrossRef]
- Potpara, T.S.; Vasiljevic, Z.M.; Vujisic-Tesic, B.D.; Marinkovic, J.M.; Polovina, M.M.; Stepanovic, J.M.; Stankovic, G.R.; Ostojic, M.C.; Lip, G.Y.H. Mitral Annular Calcification Predicts Cardiovascular Morbidity and Mortality in Middle-aged Patients With Atrial Fibrillation: The Belgrade Atrial Fibrillation Study. Chest 2011, 140, 902–910. [Google Scholar] [CrossRef] [PubMed]
- Pressman, G.S.; Agarwal, A.; Braitman, L.E.; Muddassir, S.M. Mitral Annular Calcium Causing Mitral Stenosis. Am. J. Cardiol. 2010, 105, 389–391. [Google Scholar] [CrossRef] [PubMed]
- Kiefer, P.; Noack, T.; Seeburger, J.; Hoyer, A.; Linke, A.; Mangner, N.; Lehmkuhl, L.; Mohr, F.W.; Holzhey, D. Transapical Mitral Valve Implantation for Native Mitral Valve Stenosis Using a Balloon-Expandable Prosthesis. Ann. Thorac. Surg. 2017, 104, 2030–2036. [Google Scholar] [CrossRef][Green Version]
- Carrel, T.; Wenaweser, P.M.; Reineke, S.; Simon, R.; Eberle, B.; Windecker, S.; Huber, C. Worldwide first surgical implantation of a transcatheter valved stent in mitral position. Cardiovasc. Med. 2012, 15, 202–205. [Google Scholar] [CrossRef]
- Astarci, P.; Glineur, D.; De Kerchove, L.; El Khoury, G. Transcatheter valve used in a bailout technique during complicated open mitral valve surgery. Interact. Cardiovasc. Thorac. Surg. 2013, 17, 745–747. [Google Scholar] [CrossRef]
- Sinning, J.-M.; Mellert, F.; Schiller, W.; Welz, A.; Nickenig, G.; Hammerstingl, C. Transcatheter mitral valve replacement using a balloon-expandable prosthesis in a patient with calcified native mitral valve stenosis. Eur. Heart J. 2013, 34, 2609. [Google Scholar] [CrossRef]
- Ferrari, E.; Niclauss, L.; Locca, D.; Marcucci, C. On-pump fibrillating heart mitral valve replacement with the SAPIEN XT transcatheter heart valve. Eur. J. Cardio-Thorac. Surg. 2013, 45, 749–751. [Google Scholar] [CrossRef][Green Version]
- El-Eshmawi, A.; Love, B.; Bhatt, H.V.; Pawale, A.; Boateng, P.; Adams, D.H. Direct Access Implantation of a Melody Valve in Native Mitral Valve: A Hybrid Approach in the Presence of Extensive Mitral Annular Calcification. Ann. Thorac. Surg. 2015, 99, 1085. [Google Scholar] [CrossRef]
- Mellert, F.; Sinning, J.-M.; Werner, N.; Welz, A.; Grube, E.; Nickenig, G.; Hammerstingl, C. First-in-man transapical mitral valve replacement using the Direct Flow Medical® aortic valve prosthesis. Eur. Heart J. 2015, 36, 2119. [Google Scholar] [CrossRef]
- Lim, Z.Y.; Boix, R.; Prendergast, B.; Rajani, R.; Redwood, S.; Hancock, J.; Young, C.; Bapat, V. (First Reported Case of Transcatheter Mitral Valve Implantation in Mitral Annular Calcification with a Fully Repositionable and Self-Expanding Valve. Circ. Cardiovasc. Interv. 2015, 8, e003031. [Google Scholar] [CrossRef]
- Lee, R.; Fukuhara, S.; George, I.; Borger, M.A. Mitral valve replacement with a transcatheter valve in the setting of severe mitral annular calcification. J. Thorac. Cardiovasc. Surg. 2015, 151, e47–e49. [Google Scholar] [CrossRef]
- Langhammer, B.; Huber, C.; Windecker, S.; Carrel, T. Surgical antegrade transcatheter mitral valve implantation for symptomatic mitral valve disease and heavily calcified annulus. Eur. J. Cardio-Thorac. Surg. 2016, 51, 382–384. [Google Scholar] [CrossRef]
- Koeckert, M.S.; Loulmet, D.F.; Williams, M.R.; Neuburger, P.J.; Grossi, E.A. Robotic Transcatheter Mitral Valve Replacement Using the Sapien XT in the Setting of Severe Mitral Annular Calcification. J. Card. Surg. 2016, 31, 303–305. [Google Scholar] [CrossRef]
- Baumgarten, H.; Squiers, J.; Brinkman, W.T.; DiMaio, J.M.; Gopal, A.; Mack, M.J.; Smith, R.L. Implantation of Transcatheter Aortic Prosthesis in 3 Patients With Mitral Annular Calcification. Ann. Thorac. Surg. 2016, 102, e433–e435. [Google Scholar] [CrossRef]
- Ghosh-Dastidar, M.; Bapat, V. Transcatheter Valve Implantation in Mitral Annular Calcification During Open Surgery: Extended Collar Technique. Ann. Thorac. Surg. 2017, 104, e303–e305. [Google Scholar] [CrossRef] [PubMed][Green Version]
- Polomsky, M.; Koulogiannis, K.P.; Kipperman, R.M.; Cohen, B.M.; Magovern, C.J.; Slater, J.P.; Xydas, S.; Marcoff, L.; Brown, J.M. Mitral Valve Replacement With Sapien 3 Transcatheter Valve in Severe Mitral Annular Calcification. Ann. Thorac. Surg. 2017, 103, e57–e59. [Google Scholar] [CrossRef]
- Marcus, S.G.; Mahadevan, V.S.; Deuse, T. Hybrid Open Minimally Invasive Transcatheter Mitral Valve Replacement. Ann. Thorac. Surg. 2018, 106, e57–e59. [Google Scholar] [CrossRef]
- Lupon, E.; Lemaire, A.; Cron, C.; Marcheix, B. Surgical antegrade transcatheter valve implantation and heavily calcified heart. Asian Cardiovasc. Thorac. Ann. 2018, 26, 470–472. [Google Scholar] [CrossRef] [PubMed]
- Jeganathan, R.; Hamid, U.I.; Johnston, N.; Owens, C.; Spence, M.; Manoharan, G.; Nzewi, O. The role of surgical transcatheter valve implantation for the treatment of severe mitral annular calcification. J. Card. Surg. 2019, 34, 161–166. [Google Scholar] [CrossRef] [PubMed]
- Morita, S.; Takahashi, S.; Pernot, M.; Leroux, L.; Labrousse, L. Open-heart transseptal transcatheter mitral valve implantation with mitral annular calcification. J. Cardiol. Cases 2020, 22, 207–209. [Google Scholar] [CrossRef]
- Albacker, T.B.; Bakir, B.; Eldemerdash, A.; Elshaer, F.; Albacker, H.; Alawami, M.; Kashour, T. Surgical mitral valve replacement using direct implantation of Sapien 3 valve in a patients with severe mitral annular calcification without adjunctive techniques, a case report. J. Cardiothorac. Surg. 2020, 15, 42–45. [Google Scholar] [CrossRef] [PubMed]
- Tiwana, J.; Aldea, G.; Levin, D.B.; Johnson, K.; Don, C.W.; Dvir, D.; Mackensen, G.B.; Reisman, M.; McCabe, J.M. Contemporary Transcatheter Mitral Valve Replacement for Mitral Annular Calcification or Ring. JACC Cardiovasc. Interv. 2020, 13, 2388–2398. [Google Scholar] [CrossRef]
- Binder, R.K.; Rodés-Cabau, J.; Wood, D.A.; Mok, M.; Leipsic, J.; De Larochellière, R.; Toggweiler, S.; Dumont, E.; Freeman, M.; Willson, A.B.; et al. Transcatheter Aortic Valve Replacement with the SAPIEN 3: A new balloon-expandable transcatheter heart valve. JACC Cardiovasc. Interv. 2013, 6, 293–300. [Google Scholar] [CrossRef]
- Stone, G.W.; Adams, D.H.; Abraham, W.T.; Kappetein, A.P.; Généreux, P.; Vranckx, P.; Mehran, R.; Kuck, K.-H.; Leon, M.B.; Piazza, N.; et al. Clinical trial design principles and endpoint definitions for transcatheter mitral valve repair and replacement: Part 2: Endpoint definitions: A consensus document from the Mitral Valve Academic Research Consortium. Eur. Heart J. 2015, 36, 1878–1891. [Google Scholar] [CrossRef] [PubMed]
- Hu, J.; Chen, Y.; Cheng, S.; Zhang, S.; Wu, K.; Wang, W.; Zhou, Y. Transcatheter mitral valve implantation for degenerated mitral bioprostheses or failed surgical annuloplasty rings: A systematic review and meta-analysis. J. Card. Surg. 2018, 33, 508–519. [Google Scholar] [CrossRef]
- Magne, J.; Mathieu, P.; Dumesnil, J.G.; Tanne, D.; Dagenais, F.; Doyle, D.; Pibarot, P. Impact of Prosthesis-Patient Mismatch on Survival After Mitral Valve Replacement. Circulation 2007, 115, 1417–1425. [Google Scholar] [CrossRef] [PubMed]
- Oberweis, B.S.; Hamid, N.; Khalique, O.; George, I.; Nazif, T.; Vahl, T.; White, J.; Kodali, S.; Leon, M.; Hahn, R. Effective orifice area reference values with the different sizes of the sapien 3 balloon-expanding transcatheter aortic valve. J. Am. Coll. Cardiol. 2016, 67, 401. [Google Scholar] [CrossRef]
- Helmy, T.; Hui, D.S.; Smart, S.; Lim, M.J.; Lee, R. Balloon assisted translocation of the mitral anterior leaflet to prevent left ventricular outflow obstruction (BATMAN): A novel technique for patients undergoing transcatheter mitral valve replacement. Catheter. Cardiovasc. Interv. 2019, 95, 840–848. [Google Scholar] [CrossRef]
- Khan, J.M.; Lederman, R.J. BATMAN—Savior or vigilante? Catheter. Cardiovasc. Interv. 2020, 95, 849–850. [Google Scholar] [CrossRef]
- Saha, S.; Peterss, S.; Mueller, C.; Deseive, S.; Sadoni, S.; Hausleiter, J.; Massberg, S.; Hagl, C.; Joskowiak, D. Cardiac surgery following transcatheter aortic valve replacement. Eur. J. Cardio-Thorac. Surg. 2021, 60, 1149–1155. [Google Scholar] [CrossRef]
- De Palo, M.; Scicchitano, P.; Malvindi, P.G.; Paparella, D. Endocarditis in Patients with Aortic Valve Prosthesis: Comparison between Surgical and Transcatheter Prosthesis. Antibiotics 2021, 10, 50. [Google Scholar] [CrossRef] [PubMed]




| Demographic Data | (n = 6) |
|---|---|
| Age (years) | 76 ± 9 |
| Female (%) | 6 (100.0) |
| BMI (kg/m2) | 29 ± 4.5 |
| EuroSCORE II (%) | 5.7 ± 1.9 |
| NYHA III-IV (%) | 6 (100.0) |
| Chronic kidney disease (%) | 5 (83.3) |
| GFR (mL/min) | 55 ± 22 |
| Atrial fibrillation (%) | 4 (66.7) |
| COPD (%) | 3 (50.0) |
| FEV1 (l) | 1.6 ± 0.2 |
| Coronary artery disesase (%) | 2 (33.3) |
| Echocardiographic data | |
| LVEF (%) | 61.3 ± 11.6 |
| Impaired RV function (%) | 1 (16.7) |
| Severe aortic stenosis (%) | 2 (33.3) |
| Mild to moderate aortic regurgitation (%) | 1 (16.7) |
| Severe mitral regurgitation (%) | 3 (50.0) |
| Severe mitral stenosis (%) | 6 (100.0) |
| • MV dPmax (mmHg) | 26 ± 1.3 |
| • MV dPmean (mmHg) | 11.7 ± 3.4 |
| Moderate to severe Tricuspid regurgitation (%) | 1 (16.7) |
| Details of Surgery | (n = 6) |
|---|---|
| Duration of CPB (min) | 137 ± 60 |
| Cross-clamp time (min) | 95 ± 31 |
| Prosthesis size | |
| • 26 mm (%) | 1 (16.7) |
| • 29 mm (%) | 5 (83.3) |
| Concomitant procedures | |
| • Aortic valve replacement (%) | 2 (33.3) |
| • Morrow resection (%) | 1 (16.7) |
| • CABG (%) | 1 (16.7) |
| • LAAO (%) | 5 (83.3) |
| Intraoperative Echocardiographic data | |
| MV dP max (mmHg) | 11.5 ± 2.9 |
| MV dPmean (mmHg) | 5.2 ± 1.3 |
| LVOT dPmax (mmHg) | 25 ± 1.3 |
| LVOT dPmean (mmHg) | 12.5 ± 2.9 |
| None to trace paravalvular leakage | 6 (100.0) |
| Morbidities | |
| Re-explorative surgery (%) | 2 (33.3) |
| Surgical site infection (%) | 1 (16.7) |
| Renal replacement therapy (%) | 3 (50.0) |
| Nosocomial pneumonia (%) | 2 (33.3) |
| Outcomes | |
| Duration of mechanical ventilation (hours) | 76 ± 66 |
| ICU stay (days) | 9 ± 8 |
| Total hospital stay (days) | 26 ± 17 |
| Operative mortality (%) | 1 (16.7) |
| Author | Year | Valve Implanted | Nr. of Patients | Access | Adjunctive Procedures | PVL | Postoperative Mitral DPmean (mmHg) | Concomitant Procedures |
|---|---|---|---|---|---|---|---|---|
| Carrel et al. [24] (Switzerland) | 2012 | Sapien XT | 1 | Median sternotomy On pump Transatrial access | Valve fixed with sutures to the annulus | No | 2 | - |
| Astarci et al. [25] (Belgium) | 2013 | Sapien XT | 1 | Median sternotomy On pump Transatrial access | Bovine pericardium was used to seal a paravalvular leakage | No | 3 | SAVR and CABG |
| Sinning et al. [26] (Germany) | 2013 | Sapien XT | 1 | Transapical access | None | Mild | 3 | - |
| Ferrari et al. [27] (Switzerland) | 2013 | Sapien XT | 1 | Right Thoracotomy On pump Transatrial access | Sutures at commissures | No | - | - |
| El-Eshmawi et al. [28] (USA) | 2015 | Melody valve | 1 | Median sternotomy On pump Transatrial access | None | No | 3 | TVr, LAAE, Ablation |
| Mellert et al. [29] | 2015 | Direct flow medical | 1 | Transapical | None | Mild | 2 | - |
| Lim et al. [30] (United Kingdom) | 2015 | Lotus | 2 | Transapical | None | Mild | Case 1: 4 Case 2: 7 | - |
| Dahle et al. [9] (Norway) | 2015 | Sapien XT | 1 | Median sternotomy On pump Transatrial access | Anchoring sutures on the atrial wall | No | - | Modified Konno procedure with myectomy was performed later due to LVOT obstruction |
| Lee et al. [31] (USA) | 2016 | Sapien XT | 1 | Median sternotomy On pump Transatrial access | Anchoring sutures in the mitral annulus | Mild | 2 | SAVR |
| Langhammer et al. [32] (Switzerland) | 2016 | Sapien XT and Sapien 3 | 4 | Transatrial and transseptal | In two cases additional suture fixation and in two cases use of xeno-pericardial patch to reduce paravalvular leakage | Mild (1) | Case 1: 5 Case 2: 5 Case 3: 4 Case 4: 4 | Case 1: Maze procedure Case 3: CABG, septal myectomy |
| Koeckert et al. [33] (USA) | 2016 | Sapien XT | 1 | Robotic approach- On pump-Transatrial access | Placement of three periannular sutures | No | 3 | - |
| Baumgarten et al. [34] (USA) | 2016 | Sapien XT and Sapien 3 | 3 | lateral mini- thoracotomy-on pump-Transatrial access | None | Mild (1) | Case 1: 2 Case 2: normal Case 3: 4 | - |
| Murashita et al. [8] (USA) | 2016 | Sapien XT | 1 | Median sternotomy On pump Transatrial access | None | Trivial | 2 | - |
| Guerrero et al. [7] (Multicenter) | 2016 | Sapien XT, Sapien 3, Inovare | 64 | Direct open transatrial (9) Transapical (29) Transseptal (26) | mild or absent (95.1%), Severe (4.9%) | 5.8 ± 2.2 | TAVR (11) SAVR (6) | |
| El Sabbagh et al. [5] (USA) | 2017 | Sapien XT and Sapien 3 | 6 | Median sternotomy (3)/Right anterolateral thoracotomy (3)- On-pump- Transatrial (4)/Trans septal (2) | Anchoring stitches when necessary | Severe (3) Moderate (1) | 5 ± 1 | - |
| Ghosh-Dastidar et al. [35] (United Kingdom) | 2017 | Lotus | 1 | Initial transapical access followed by Median sternotomy- On pump- Transatrial access | Teflon collar and anchoring sutures | No | normal | - |
| Polomsky et al. [36] (USA) | 2017 | Sapien 3 | 2 | Median sternotomy- On pump- Transatrial access | Sutures at commissures | No | - | SAVR (2) |
| Praz et al. [6] (USA) | 2018 | Sapien XT and Sapien 3 | 26 | Median sternotomy (25)/Right thoracotomy (1)- On pump- Transatrial access | Felt strip and anchoring sutures | Mild (1) | 4 ± 2 | SAVR (11) |
| Sivan et al. [37] (USA) | 2018 | Sapien 3 | 1 | Right thoracotomy -On pump-Transatrial access | Pledgeted anchoring sutures | No | - | - |
| Lupon et al. [38] (France) | 2018 | Sapien 3 | 1 | Median sternotomy- On pump- Transatrial access | None | No | 4.5 | CABG |
| Russell et al. [13] (USA) | 2018 | Sapien 3 | 8 | Median sternotomy On pump Transatrial access | PTFE strip | Trace (6) Mild (1) | - | SAVR (1) TVr (2) |
| Jeganathan et al. [39] (United Kingdom) | 2019 | Sapien 3 | 2 | Median sternotomy On pump Transatrial access | Pledgeted anchoring sutures | No | Case 1: 2.7 Case 2: 7 | TVr (1) |
| Morita et al. [40] (Japan) | 2020 | Sapien 3 | 1 | Median sternotomy- On pump- Transseptal access | Use of felt strip and anchoring sutures | Mild | - | TVr |
| Albacker et al. [41] (Saudi Arabia) | 2020 | Sapien 3 | 1 | Median sternotomy On pump Transatrial access | None | No | 4 | - |
| Tiwana et al. [42] (USA) | 2020 | Sapien XT and Sapien 3 | 40 | Transapical (5) Transseptal (35) | None | 5.5 ± 2.1 | - |
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Bagaev, E.; Ali, A.; Saha, S.; Sadoni, S.; Orban, M.; Naebauer, M.; Mehilli, J.; Massberg, S.; Oberbach, A.; Hagl, C. Hybrid Surgery for Severe Mitral Valve Calcification: Limitations and Caveats for an Open Transcatheter Approach. Medicina 2022, 58, 93. https://doi.org/10.3390/medicina58010093
Bagaev E, Ali A, Saha S, Sadoni S, Orban M, Naebauer M, Mehilli J, Massberg S, Oberbach A, Hagl C. Hybrid Surgery for Severe Mitral Valve Calcification: Limitations and Caveats for an Open Transcatheter Approach. Medicina. 2022; 58(1):93. https://doi.org/10.3390/medicina58010093
Chicago/Turabian StyleBagaev, Erik, Ahmad Ali, Shekhar Saha, Sebastian Sadoni, Martin Orban, Michael Naebauer, Julinda Mehilli, Steffen Massberg, Andreas Oberbach, and Christian Hagl. 2022. "Hybrid Surgery for Severe Mitral Valve Calcification: Limitations and Caveats for an Open Transcatheter Approach" Medicina 58, no. 1: 93. https://doi.org/10.3390/medicina58010093
APA StyleBagaev, E., Ali, A., Saha, S., Sadoni, S., Orban, M., Naebauer, M., Mehilli, J., Massberg, S., Oberbach, A., & Hagl, C. (2022). Hybrid Surgery for Severe Mitral Valve Calcification: Limitations and Caveats for an Open Transcatheter Approach. Medicina, 58(1), 93. https://doi.org/10.3390/medicina58010093







