Rapid Recurrence of Giant Multilocular Prostatic Cystadenoma after Laparoscopic Excision for Primary Case: A Case Report
Abstract
:1. Introduction
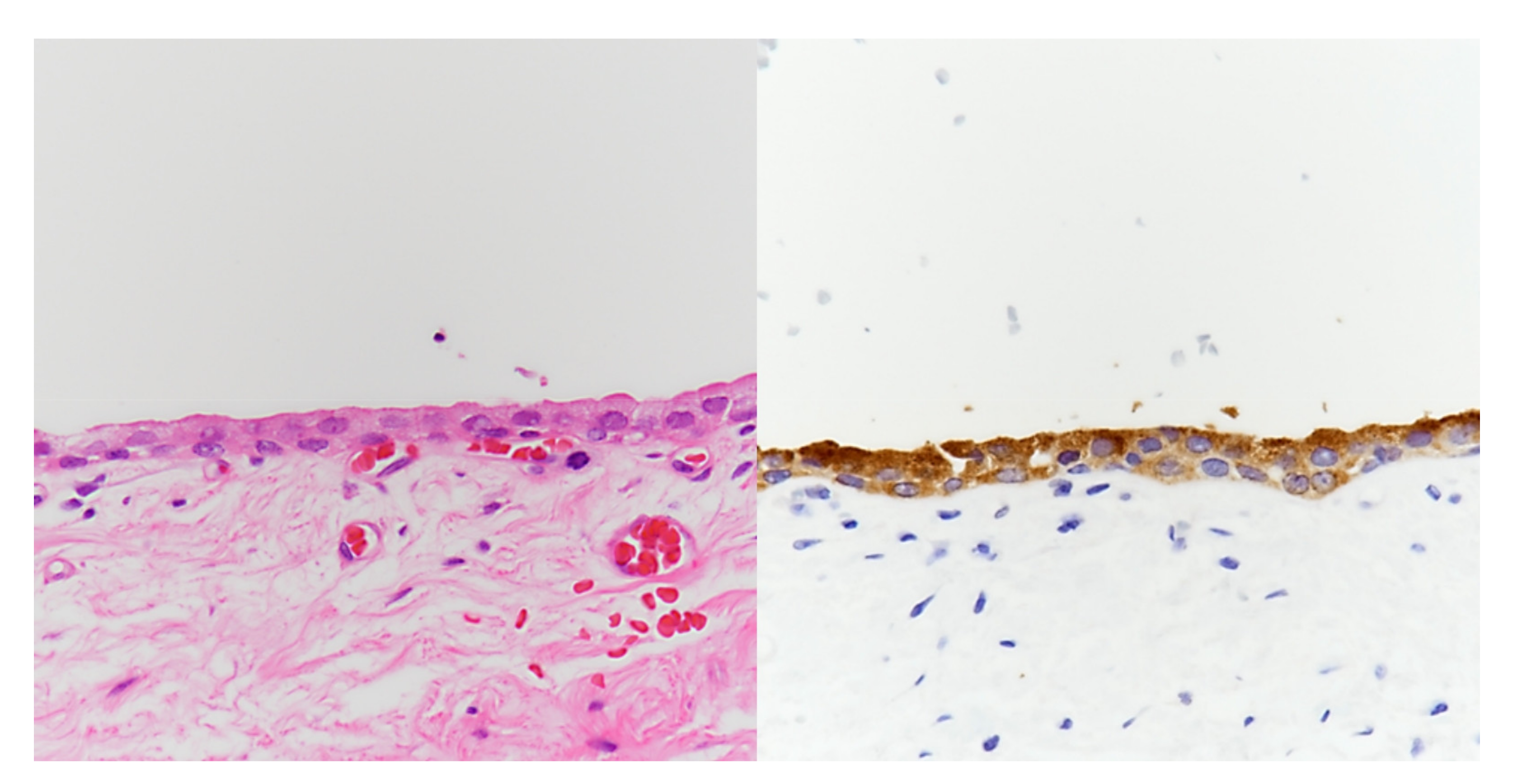
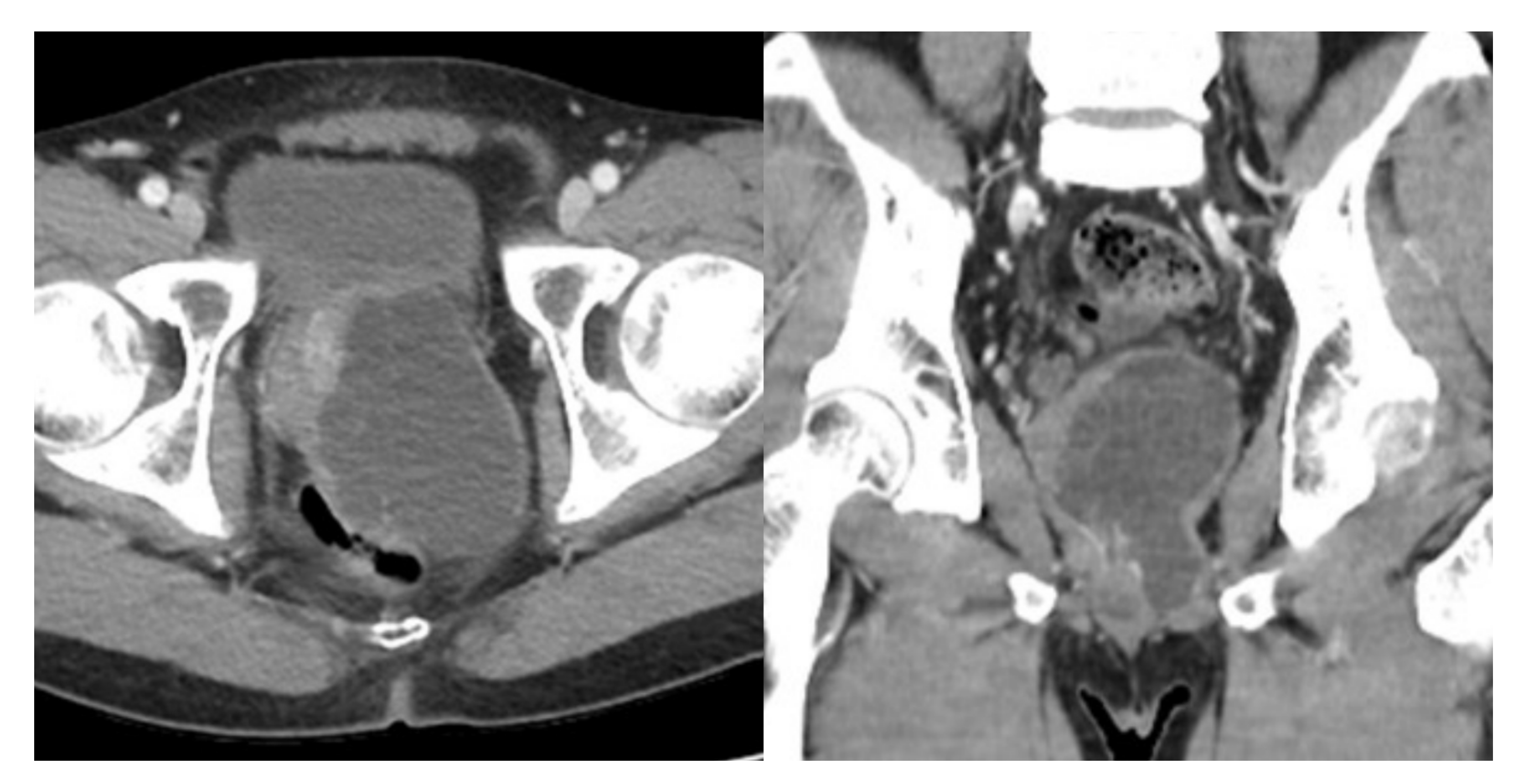
2. Case Report
3. Discussion
Author Contributions
Funding
Institutional Review Board Statement
Informed Consent Statement
Data Availability Statement
Acknowledgments
Conflicts of Interest
References
- Watanabe, J.; Konishi, T.; Takeuchi, H.; Tomoyoshi, T. A case of giant prostatic cystadenoma. Hinyokika Kiyo 1990, 36, 1077–1079. [Google Scholar] [PubMed]
- Maluf, H.M.; King, M.E.; DeLuca, F.R.; Navarro, J.; Talerman, A.; Young, R.H. Giant multilocular prostatic cystadenoma: A distinctive lesion of the retroperitoneum in men. A report of two cases. Am. J. Surg. Pathol. 1991, 15, 131–135. [Google Scholar] [CrossRef] [PubMed]
- Nakamura, Y.; Shida, D.; Shibayama, T.; Yoshida, A.; Matsui, Y.; Shinoda, Y.; Iwata, S.; Kanemitsu, Y. Giant multilocular prostatic cystadenoma. World J. Surg. Oncol. 2019, 17, 42. [Google Scholar] [CrossRef] [PubMed]
- Baad, M.; Ericson, K.; Yassan, L.; Oto, A.; Eggener, S.; Nottingham, C.U.; Richards, K.A.; Thomas, S. Giant Multilocular Cystadenoma of the Prostate. Radiographics 2015, 35, 1051–1055. [Google Scholar] [CrossRef] [PubMed]
- Levy, D.A.; Gogate, P.A.; Hampel, N. Giant multilocular prostatic cystadenoma: A rare clinical entity and review of the literature. J. Urol. 1993, 150, 1920–1922. [Google Scholar] [CrossRef]
- Lim, D.J.; Hayden, R.T.; Murad, T.; Nemcek, A.A., Jr.; Dalton, D.P. Multilocular prostatic cystadenoma presenting as a large complex pelvic cystic mass. J. Urol. 1993, 149, 856–859. [Google Scholar] [CrossRef]
- Kirsch, A.J.; Newhouse, J.; Hibshoosh, H.; O’Toole, K.; Ritter, J.; Benson, M.C. Giant multilocular cystadenoma of the prostate. Urology 1996, 48, 303–305. [Google Scholar] [CrossRef]
- Seong, B.M.; Cheon, J.; Lee, J.G.; Kim, J.J.; Chae, Y.S. A case of multilocular prostatic cystadenoma. J. Korean Med. Sci. 1998, 13, 554–558. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Matsumoto, K.; Egawa, S.; Iwabuchi, K.; Baba, S. Prostatic cystadenoma presenting as a large multilocular mass. Int. J. Urol. 2002, 9, 410–412. [Google Scholar] [CrossRef] [PubMed]
- Rusch, D.; Moinzadeh, A.; Hamawy, K.; Larsen, C. Giant multilocular cystadenoma of the prostate. AJR Am. J. Roentgenol. 2002, 179, 1477–1479. [Google Scholar] [CrossRef] [PubMed]
- Allen, E.A.; Brinker, D.A.; Coppola, D.; Diaz, J.I.; Epstein, J.I. Multilocular prostatic cystadenoma with high-grade prostatic intraepithelial neoplasia. Urology 2003, 61, 644. [Google Scholar] [CrossRef]
- Datta, M.W.; Hosenpud, J.; Osipov, V.; Young, R.H. Giant multilocular cystadenoma of the prostate responsive to GnRH antagonists. Urology 2003, 61, 225. [Google Scholar] [CrossRef]
- Olgun, D.C.; Onal, B.; Mihmanli, I.; Kantarci, F.; Durak, H.; Demir, H.; Cetinel, B. Giant multilocular cystadenoma of the prostate: A rare cause of huge cystic pelvic mass. Korean J. Urol. 2012, 53, 209–213. [Google Scholar] [CrossRef] [PubMed]
- Fan, L.W.; Chang, Y.H.; Shao, I.H.; Wu, K.F.; Pang, S.T. Robotic surgery in giant multilocular cystadenoma of the prostate: A rare case report. World J. Clin. Cases 2020, 8, 4215–4222. [Google Scholar] [CrossRef] [PubMed]
- Yang, W.B.; Zhang, X.W.; Yang, J.; Li, Q.; Xu, T.; Bai, W.J. Transurethral resection of prostate treatment for recurrence of a multilocular prostatic cystadenoma: A case report. J. Peking Univ. Health Sci. 2018, 50, 740–742. [Google Scholar]
- El Rahman, D.A.; Zago, T.; Verduci, G.; Baroni, G.; Berardinelli, M.L.; Pea, U.; Morandi, E.; Castoldi, M. Transperitoneal laparoscopic treatment for recurrence of a giant multilocular prostatic cystadenoma: A case report and review of the literature. Arch. Ital. Di Urol. Androl. 2016, 88, 66–67. [Google Scholar] [CrossRef] [PubMed]
- Seo, H.J.; Lee, N.R.; Son, S.K.; Kim, D.K.; Rha, K.H.; Lee, S.H. Comparison of Robot-Assisted Radical Prostatectomy and Open Radical Prostatectomy Outcomes: A Systematic Review and Meta-Analysis. Yonsei Med. J. 2016, 57, 1165–1177. [Google Scholar] [CrossRef] [PubMed] [Green Version]

Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2021 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).
Share and Cite
Choi, T.-S.; Lee, D.-G.; Yoo, K.-H.; Min, G.-E. Rapid Recurrence of Giant Multilocular Prostatic Cystadenoma after Laparoscopic Excision for Primary Case: A Case Report. Medicina 2021, 57, 870. https://doi.org/10.3390/medicina57090870
Choi T-S, Lee D-G, Yoo K-H, Min G-E. Rapid Recurrence of Giant Multilocular Prostatic Cystadenoma after Laparoscopic Excision for Primary Case: A Case Report. Medicina. 2021; 57(9):870. https://doi.org/10.3390/medicina57090870
Chicago/Turabian StyleChoi, Tae-Soo, Dong-Gi Lee, Koo-Han Yoo, and Gyeong-Eun Min. 2021. "Rapid Recurrence of Giant Multilocular Prostatic Cystadenoma after Laparoscopic Excision for Primary Case: A Case Report" Medicina 57, no. 9: 870. https://doi.org/10.3390/medicina57090870
APA StyleChoi, T.-S., Lee, D.-G., Yoo, K.-H., & Min, G.-E. (2021). Rapid Recurrence of Giant Multilocular Prostatic Cystadenoma after Laparoscopic Excision for Primary Case: A Case Report. Medicina, 57(9), 870. https://doi.org/10.3390/medicina57090870





