Abstract
Numerous harmful factors that affect the human body from birth to old age cause many disturbances, e.g., in the structure of the genome, inducing cell apoptosis and their degeneration, which leads to the development of many diseases, including cancer. Among the factors leading to pathological processes, microbes, viruses, gene dysregulation and immune system disorders have been described. The function of a protective agent may be played by lactoferrin as a “miracle molecule”, an endogenous protein with a number of favorable antimicrobial, antiviral, antioxidant, immunostimulatory and binding DNA properties. The purpose of this article is to present the broad spectrum of properties and the role that lactoferrin plays in protecting human cells at all stages of life.
1. Introduction
Throughout life, from birth to old age, the human body is exposed to a myriad of harmful factors such as toxins, environmental pollutants, pathogens and disease processes including cancer. One common phenomenon that occurs as a result of an imbalance between the production and accumulation of reactive oxygen species (ROS) in cells and tissues and the body’s antioxidant defense mechanisms is oxidative stress. Excessive production and accumulation of ROS is a common denominator of toxicity, being involved in the development and progression of over 100 diseases; therefore, much effort has been devoted to the discovery of effective drugs that prevent the damage induced by ROS [1,2]. These include direct antioxidants or weak oxidants, whose mechanism of action is to increase the activity of endogenous antioxidant mechanisms. Nonetheless, the use of such compounds ends with conflicting epidemiological results in subjects treated with synthetic antioxidants. It is also known that too strong an antioxidant response may not be beneficial [3] as in the case of high-dose vitamin E supplementation, increasing the risk of prostate cancer in healthy men or lung cancer and heart disease in smokers as a result of excessive β-carotene supplementation [4,5].
Therefore, the problem is to maintain a proper balance between ROS and therapeutics with antioxidant properties. Recently, much attention has been focused on lactoferrin (LF), a protein derived from milk, as a potent compound against oxidative stress damage.
Nevertheless, LF is a multifunctional protein that deserves to be called a “miracle molecule”, exhibiting a number of other beneficial properties such as anti-pathogenic, anti-cancer, anti-inflammatory, immunomodulatory and DNA-regulatory activities [6,7]. Recent reports indicate its therapeutic properties in the treatment of neurodegenerative diseases associated with aging, as well as stress-related emotional disorders [8,9].
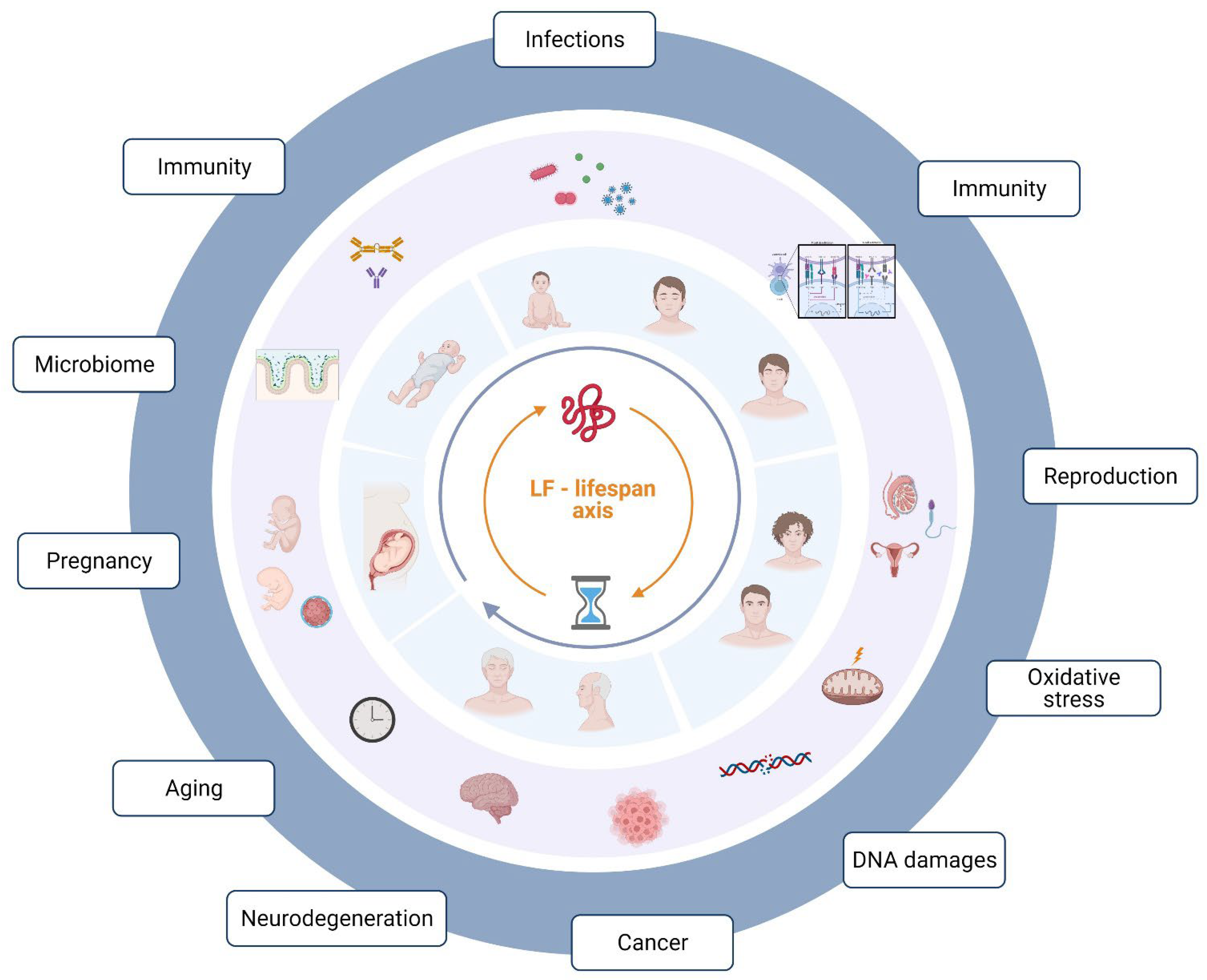
The purpose of this article was to summarize the wide range of properties of lactoferrin, a “wonder molecule” that plays an important role in health and pathology at all stages of life (Figure 1).
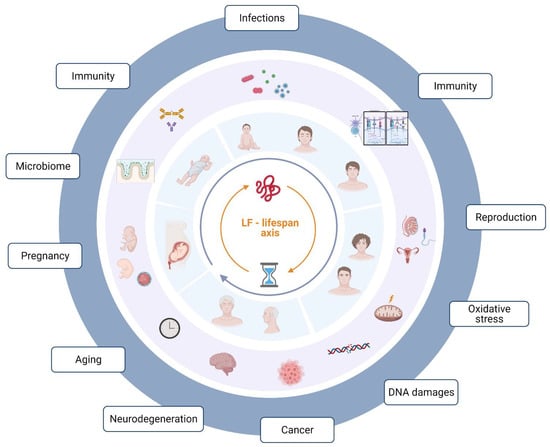
Figure 1.
Lactoferrin in human physiological states and pathology—lifespan correlation. Illustration was created in BioRender.com (accessed on 28 April 2022).
2. Lactoferrin—Characteristics and Properties
Lactoferrin (LF) is a component of the whey protein of milk of most mammals, probably with the exception of dogs and rats. The concentration of lactoferrin in milk depends on the phase of lactation. It has been proven that colostrum can contain up to seven times more LF than mature milk [10]. Human body cells can produce lactoferrin and it is also found in many organs and cells of the human body. Its presence has been confirmed in kidneys, lungs, gallbladder, pancreas, intestine, liver, prostate, saliva, tears, sperm, cerebrospinal fluid, urine, bronchial secretions, vaginal discharge, synovial fluid, umbilical cord blood, blood plasma, and cells of the immune system [10,11,12]. It is present wherever the body needs quick and effective protection against external threats.
LF consists of a simple polypeptide chain that consists of two globular lobes with a carboxyl (C) and an amino (N) end connected by an α helix. Each lobe is made of two domains known as C1, C2, N1 and N2, which form a β-sheet [13]. Because of genetic polymorphism and different post-transcriptional and post-translational processing, lactoferrin can occur in many variants [14]. The multifunctionality of LF is due to the fact that it belongs to the class of hybrid proteins, possessing both ordered domains and functionally important intrinsically disordered regions containing sites of various post-translational modifications, such as phosphorylation, acetylation, lipidation, ubiquitination or glycosylation among others, affecting its biological function [15]. An example of LF heterogeneity is the existence of several glycosylation isoforms. The number of N-linked glycosylation sites is species specific. For instance, three potential glycosylation sites have been found in human lactoferrin and five in bovine lactoferrin [13]. Glycosylation plays an important role in regulating LF stability and resistance to proteolysis by increasing the solubility of secreted proteins and increasing the binding of LF to certain cell types or specific receptors. However, it has little effect on properties of LF such as thermal stability or iron binding and release [15].
The major isoform is secreted lactoferrin, which consists of 689 amino acids and has a molecular weight of about 80 kDa. It is odorless and well soluble in water. It shows resistance to heating for several hours at 56 °C, while at temperatures above 80–90 °C it denatures.
LF is a protein with multifaceted effects on the body, not all mechanisms of which have been thoroughly investigated yet, which is why it is referred to as a multipotent protein [16]. Chemically, it is a glycoprotein that, due to its homology of sequence with serum transferrin, is classified as a member of the transferrin family, a protein that can bind to iron ions. Lactoferrin, as the name suggests (lacto + ferrin = milk + iron), is iron binding milk protein, which helps to balance iron levels in the body [11,12,17]. Excess iron can be toxic because it has the ability to donate electrons to oxygen, resulting in the formation of reactive oxygen species (ROS) such as superoxide anions and hydroxyl radicals. LF, thanks to the ability to strongly and reversibly bind iron ions, supports the body in maintaining the homeostasis of this important micronutrient. LF has a high affinity for iron, several hundred times greater than the affinity of transferrin [18], and each lobe of LF can bind to an iron ion [13]. There is a high probability that lactoferrin can also bind copper, zinc and manganese ions [10,19]. In addition, as a result of the chelation process, which reduces the iron overload caused by the accumulation of iron in many organs, leading to free radical generation and dysfunction, the availability of Fe to pathogens that need it for their growth is reduced [20]. Interestingly, LF is capable of reversibly chelating two Fe(III) ions per molecule with high affinity, as well as retaining iron up to pH values as low as 3.0, specific to infectious and inflammatory areas [21].
LF also has the ability to modulate lipid metabolism, which translates not only into better regulation of satiety mechanisms, but also helps fight the tendency to adipose tissue accumulation. The available studies also show a positive role of this protein in reducing fatty liver [22]. It supports the proper functioning of the intestines and increases the absorption of nutrients. Lactoferrin is not only a prebiotic that supports the growth of probiotic bacteria in the digestive system [23,24,25], but also potentiates the effects of some antibiotics (e.g., vancomycin) [26]. Following the antibiotic therapy, LF contributes to the restoration of the balance of the intestinal microbiota and protects against the multiplication of pathogens and the development of local and systemic inflammation [23,24,25].
LF is also known as a factor that promotes osteogenesis and bone health and inhibits the osteolytic process [27,28,29,30].
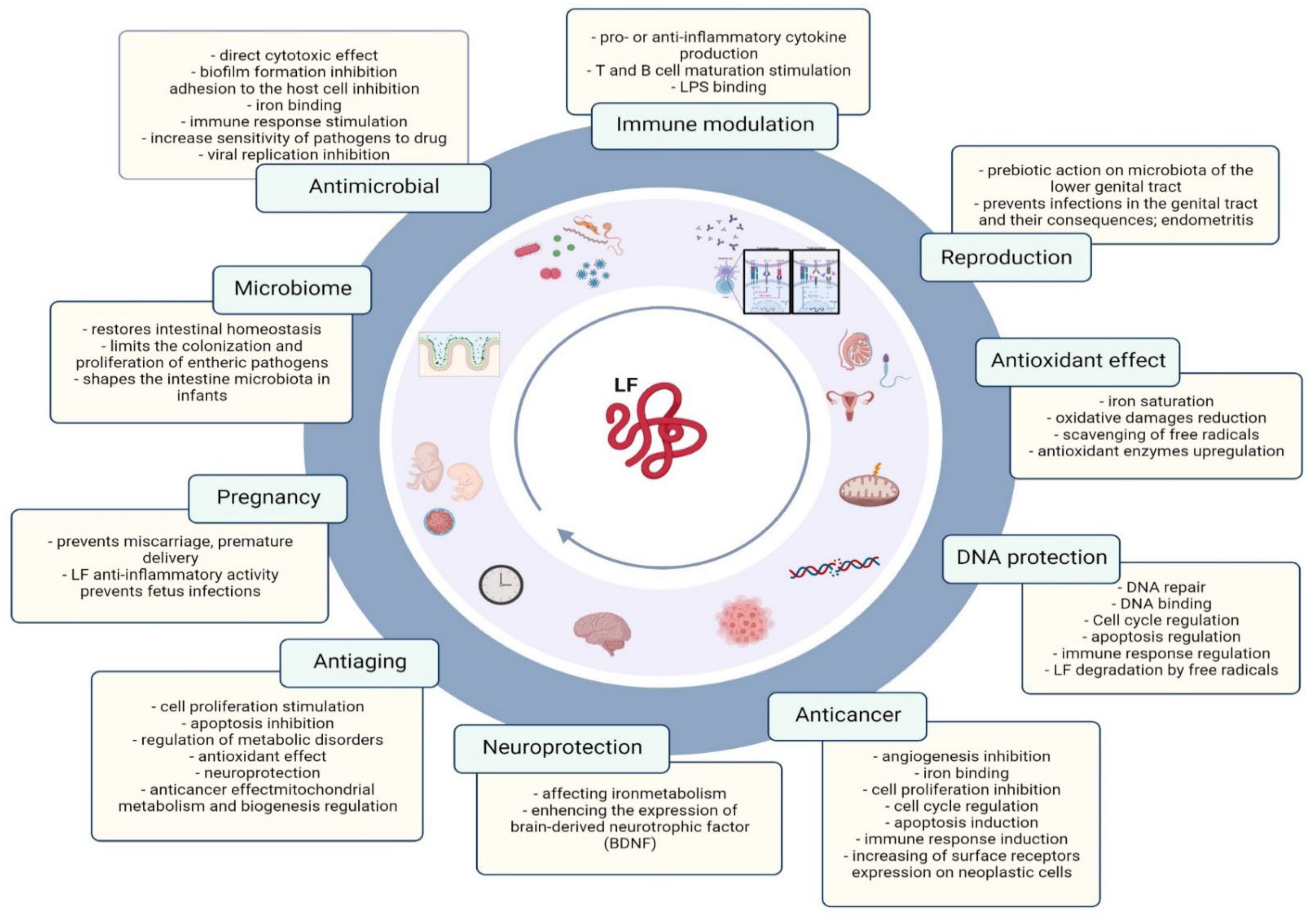
LF may protect against oxidative stress, which is related to its aforementioned ability to bind iron, which is known to have oxidative properties in large amounts [12,19,31]. The available studies indicate the high effectiveness of lactoferrin in reducing the level of cytotoxins H2O2 and increasing FRAP (ferric reducing antioxidant power) both in the intra- and extracellular space [32]. It has been shown that another antioxidant mechanism of lactoferrin is its ability to counteract the so-called oxygen explosion in neutrophils, which results in the production of large amounts of free radicals that damage cells [33]. Figure 2 summarizes the beneficial effects of lactoferrin during lifespan.
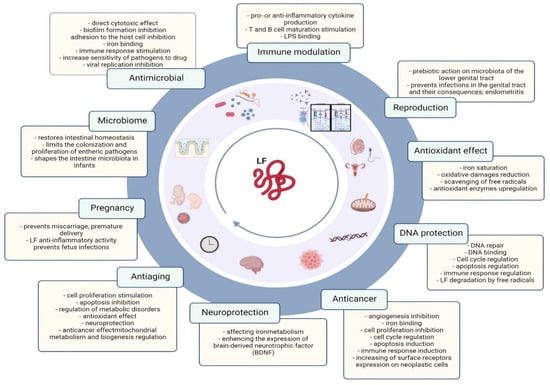
Figure 2.
Lactoferrin properties related to the human lifespan. Illustration was created in BioRender.com.
2.1. Immune System—Effects of Lactoferrin on Foetus, Infants and Reproduction
When discussing lactoferrin, it is often said that it is “unable” to affect the body due to digestion; however, scientific evidence suggests that it is hydrolyzed to stable, immunologically active peptides upon contact with the acidic environment of the gastric juice. Lactoferrin preparations are effective after oral administration, which has been confirmed in numerous studies, including clinical ones [32,34,35,36,37,38]. LF can reach the intestine, mainly in the form of peptide fragments, where they act locally on the microbiota and the immune system associated with the local mucosa, thereby enhancing the immunity of all mucous membranes in the body [11,39,40].
In children suffering from diarrhea, oral lactoferrin both alleviated the course and reduced the frequency [40,41]. Published studies using lactoferrin in children have positively evaluated its use for both gastrointestinal infections and sepsis in neonates, and lactoferrin supply in preterm infants is recommended to be introduced as soon as possible [42,43]. It is also very interesting that, in pregnant women, intravaginal lactoferrin is one of the preventive measures reducing the risk of premature delivery [10,41]. LF supports normal tissue development in the fetus, including normal ossification, adequate iron availability and absorption, protects against infection and inflammation, and benefits both mother and fetus [44]. LF acts as a probiotic, protecting the lower genital tract and preventing the consequences of inflammation both during pregnancy and before pregnancy, thus aiding fertility. Lactoferrin is present in the follicular fluid, but results of studies on its effect on oocyte maturation and quality are inconclusive [45,46]. The role of lactoferrin in male fertility is still under intense debate and research [47,48]. It can protect against infections of the male genital tract and regulate iron levels in sperm, thus influencing its quality. This appears to be a good potential marker of sperm quality [47]. This issue is the subject of ongoing clinical trials—ClinicalTrials.gov Identifier: NCT05171504.
There are indications that bovine lactoferrin has the same clinical effects in newborns and infants as human lactoferrin [38]. Fungal infections were also significantly less frequent in children receiving lactoferrin [49].
The two main lines of defense our body relies on when it comes into contact with an antigen are innate and acquired immunity [50]. The former is non-specific, depends on inherited genes and provides some protection from birth. Lactoferrin is an important component of innate immunity [51,52]. Acquired immunity is specific (i.e., dependent on recognized antigens), develops throughout life and allows for a precise response to emerging threats. It is known that the immune system of infants is immature; in contrast to innate immunity, acquired immunity of infants needs to be developed [53]. During the maturation of the immune system, children are supported by their mother’s antibodies. Already in the fetal period, the baby receives a set of IgG immunoglobulins from the mother, which it uses for immunological defense for the first months after birth. However, over time, this supply runs out and the infant’s body has to rely on its own developing immune system. Meanwhile, the baby receives IgA antibodies by consuming their mother’s milk (for this reason they are often referred to as secretory antibodies) [52,54]. As research shows, babies who are breastfed for the first six months are significantly healthier, thanks in part to other substances in breast milk that help support the immune system during this critical period [52,55]. The combination of these three elements; IgG antibodies obtained before birth and IgA contained in breast milk together with lactoferrin constitute a great part of the infant’s immunity in the first months of life [52]. In addition, LF may enhance the effect of antibodies. It has an immunomodulatory potential, both through the influence on the production of cytokines (mainly TNF-alpha, IL-6 and IL-10) and reactive oxygen species, as well as on the functions of lymphocytes and monocytes [56].
LF stimulates the action of receptors inter alia for vitamin D, which is very important for osteogenesis and immune response [57]. LF has a protective effect, supports the development of children, especially in the neonatal and infancy period, is a protective factor during gastrointestinal infections and necrotic enteritis in infants [34,38,54,58,59], and reduces the risk of sepsis in infants [35].
For years, clinical trials have been underway based on the use of lactoferrin in the treatment of children, and even extremely premature babies [34,35,36,37,38,49,58,59,60,61]. An important aspect is the lack of reported side effects, which makes lactoferrin a safe protein even for the youngest patients. Administration of bovine lactoferrin to children with low birth weight successfully protects them against sepsis and necrotic enteritis. The properties of lactoferrin make it not only an important factor regulating the work of our body, but also a potential therapeutic tool [38].
It seems necessary to re-emphasize that studies with the use of lactoferrin mainly include tissue models and animal models, as well as clinical trials involving newborns, infants and children. But we are still unsure of its potential for adults. The supplementation of that group of human population still needs further detailed studies.
2.2. Antitoxic and Antipathogenic Properties
Numerous studies have confirmed the beneficial effects of LF on the intestinal epithelium. This protein stimulates the growth, differentiation and secretory activity of epithelial cells, which optimizes the digestive processes and absorption of nutrients and protects against the action of pathogens and food allergens [61,62]. LF also protects the intestinal epithelium from the toxic effects of reactive oxygen species (ROS), bacterial toxins and xenobiotics such as nonsteroidal anti-inflammatory drugs (NSAIDs) [31,63,64,65]. Importantly, LF also protects against gastrointestinal tract infections, both viral and bacterial, fungal and protozoal [32,66]. Many tests have demonstrated the protective effect of LF in the states of endotoxemia, bacteremia, sepsis and necrotic enteritis in neonates [35,36,58,67,68,69], in inflammatory colitis [70,71] and after partial bowel resection [72]. LF has antibacterial properties in relation to Gram-negative and Gram-positive bacteria, thanks to which it is helpful for fighting pathogens, prevents the formation of biofilm by pathogenic bacteria, such as Staphylococcus aureus or blue oil rod (Pseudomonas aeruginosa) [66,73]. LF supports the treatment of gastric infection caused by Helicobacter pylori [74]. The mechanism of action of LF may, inter alia, include the direct inhibition or killing of microbial cells, activation/inhibition of the immune system, or enhancement of intestinal epithelial tightness by stimulating the production of tight junction proteins. In addition, the binding of iron by LF makes its absence associated with a concomitant halt in bacterial growth, which protects the body from infection. [20]. It also has an immunomodulating effect, stimulating the body to synthesize cytokines and chemokines as well as accelerating the maturation of cells of the immune system [17,50,51,75].
Human lactoferrin (abbreviated as hLF,) possesses 77% similarities with the bovine form (bLF) in the aspect of amino acid sequences, although bovine lactoferrin is usually studied, because it is easier to obtain. It has been estimated that in a glass of cow’s milk we will find about 25-75 mg of this protein. At the same time, it seems that bLF is not an ideal choice due to differences that may alter its antiviral and antimicrobial potential when used in human therapy, but some authors highlight its stronger antimicrobial activity [76].
LF also has antiviral properties and works synergistically with antiviral drugs such as acyclovir, ribavirin or zidovudine [77]. LF is able to bind to receptors, such as ACEII (Figure 1), used by SARS-CoV-2 as an anchor site in the cell membrane and thus inhibit the adsorption of the pathogen to the cell. In addition, LF is able to block the pathogen’s surface receptors and prevent it from binding to the target cell [78,79,80].
Its antifungal properties, including against dermatophytes and supporting the action of antimycotic drugs has been shown [49,81]. In addition it has an antiparasitic effect, e.g., against the motile parasite (Plasmodium vivax) that causes malaria and the protozoan Toxoplasma gondii causing toxoplasmosis [82].
For more detailed information on the LF activity against bacteria, viruses, fungi, and parasites, see the review by Gruden and Urlih [83].
2.3. Anticancer Activity
One of the many properties of LF is its anticancer activity. This may be related not only to preventing antioxidant stress and inflammation, which contribute to DNA damage and tumorigenesis, but also to preventing the development of, or inhibiting, cancer by stimulating the adaptive immune response [7]. This is the case for colorectal cancer, the epidemiology of which is mainly related to age and lifestyle factors [84] and in the case of childhood leukemia where long-term consumption of breast milk may prevent the risk of developing leukemia due to the immunoprotective properties of the LF present [85]. Furthermore, LF may directly inhibit proliferation, survival, migration, metastasis and accelerating cancer cell death [86,87].
It has been confirmed that, in the presence of LF, various cancer cells undergo remarkable damage such as cell cycle arrest, damage to the cytoskeleton and induction of apoptosis, as well as decreased cell migration [13,86]. The postulated property of LF by which it activates signaling pathways to generate deleterious effects on cancer cells may be interaction with proteoglycans, glycosaminoglycans, and sialic acid, high levels of which are presented by cancer cells. This may also explain the high cytotoxic selectivity of LF against cancer cells only [13,87,88]. Besides, the ability of LF to enter the cell nucleus is likely the primary mechanism by which it exerts its pleiotropic functions, including anticancer. Nuclear LF (called delta) acts as a transcription factor and causes activation of expression target genes such as Bax, SelH, DcpS, UBE2E1, Skp1 and GTF2F2 and shows the anticancer, anti-proliferating and pro-apoptotic activities [89,90,91,92]. This corresponds to decreased levels of LF and delta LF expression in tumor cells, which often correlates with greater tumor progression and poor prognosis [91,93,94].
LF also binds iron, which is heavily involved in the metabolic requirements of some cancer cells, and blocks angiogenesis, i.e., prevents the formation of new blood vessels, thereby inhibiting tumor growth and metastasis or directing the tumor toward apoptosis [21,95].
An interesting feature of LF that deserves attention, in addition to its proven safety and its low antigenicity and selectivity for cancer cells, which could be used in brain tumor therapy, is its passage through the blood–brain barrier [87].
2.4. Aging and Aging-Related Diseases
Aging can be defined as: “the progressive accumulation of changes with time associated with or responsible for the ever-increasing susceptibility to disease and death which accompanies advancing age”, and the factors that lead to aging: “the sum of the deleterious free radical reactions going on continuously throughout the cells and tissues constitutes the aging process or is a major contributor to it” [96] and “changes in molecular structure and, hence, function” [97]. In summary, aging is a complex natural phenomenon occurring as a consequence of the passage of time, environmental factors and genetics that increase susceptibility to developing systemic diseases, including metabolic disorders (diabetes mellitus), cardiovascular, neurodegenerative and respiratory diseases as well as rheumatoid arthritis, cancers or dementia [8,98,99,100].
The pleiotropic anti-aging effect of LF is related to its antioxidant, anti-inflammatory and anticancer effects, as well as the assurance of neuroprotection or the alleviation of mitochondrial dysfunction and systemic disorders [8].
LF antioxidant potential leads to cells’ and organs’ protection finally extending its lifespan [101]. In addition, due to regulation of numerous genes expression (inhibition of NF-κB, mTORC1 and caspase via the Erk and Akt pathways), LF regulates cell growth, proliferation, apoptosis and inflammation. It suppresses the senescence and apoptosis of mesenchymal stem cells (MSCs) [102,103], promotes both the formation of granulation tissue and re-epithelialization (proliferation and migration of fibroblasts and keratinocytes stimulation and enhancement of extracellular matrix components synthesis) [104,105]. Moreover, due to the induction of the targeted apoptosis of senescent cells or the disruption of the senescence-associated secretory phenotype (SASP), LF restores tissue homeostasis [99,100]. Interestingly, LF usefulness has been shown for treatment, diagnosis or monitoring age-related diseases [106,107,108,109,110,111,112,113,114,115,116,117,118,119,120]. For example, it may act as a neuroprotective agent in Alzheimer’s disease (AD) and Parkinson’s disease (PD) [111,115,116] leading to the improvement of cognitive function and attenuation of brain senescence [121]. The possible mechanism of LF action includes iron-binding dependent manner (upregulation of divalent metal transporter 1 (DMT1) and transferrin receptor (TFR) and downregulation ferroportin 1 (Fpn1)) [117,118] and/or iron-binding independent manner (regulation of the p-Akt/PTEN or the ERK-CREB pathway in HIF-1-dependent manner) [118,119,120]. Furthermore, LF preserves mitochondrial calcium homeostasis in degenerated dopaminergic neurons [122]. Moreover, LF regulates body fat metabolism limiting obesity (probable downregulation of adipogenic genes and upregulation of fatty acid synthase and acetyl CoA carboxylase in adipocytes) [123,124] and glucose metabolism in patients with type 2 diabetes mellitus via improvement of the insulin-signaling response in adipocytes (up-phosphorylation of Akt serine 473 and up-expression of glucose transport 4 and insulin receptor 1) [107,124,125,126]. In patients with cardiovascular diseases, bLF exerts proangiogenic effects and reduces blood pressure [127]. Interestingly, LF delays the process of senile osteoporosis due to its antioxidant effect and inhibition of osteoblast senescence related genes (IGF1 signaling pathway) [128,129]. LF function as a biomarker molecule is presented in Table 1.

Table 1.
Increased level of LF in the diagnosis and monitoring of aging-associated diseases.
2.5. Lactoferrin in the Human Diet and Therapy of Diseases
Lactoferrin is an important component in the human diet. Due to its high nutritional value, its antibacterial, antiviral, anti-cancer properties and regulation of the activity of the immune system [17], it has also been used in the pharmaceutical and food industries and in the production of feed additives. Currently, we can find it in products such as dietary supplements and infant formula. Lactoferrin obtained from cow’s milk is used, among others, in the production of infant formulas, foodstuffs for special medical purposes, milk, yoghurt drinks, ice cream and cookies, dietary supplements, and processed cereal products. It is also appreciated in the cosmetic (e.g., in cosmetics and toothpaste) and pharmaceutical industries [42,44,130,131].
It is a safe raw material, which is confirmed by the documents issued by the European Parliament (EP) [132], European Food Safety Authority (EFSA) [133] and the Food and Drug Administration (FDA) in the United States [134]. However, bovine LF, like any protein in cow’s milk, can cause an allergy, which is often called protein blemish. Therefore, the consumption of lactoferrin carries the risk of abnormal reactions in the body, and preparations containing this ingredient should not be taken in the case of suspected or diagnosed allergy to cow’s milk proteins. On the other hand, people who do not have allergies, but suffer from lactose intolerance, can choose preparations with LF, with a clearly defined lack of milk sugar in its composition [26,135,136,137,138].
It is also worth mentioning that LF, as a naturally occurring protein in saliva and produced by salivary glands in the oral cavity, has protective properties and is supposed to provide homeostasis in the oral cavity [17]. The ability to bind iron ions by LF provides antibacterial activity in the oral cavity. The use of products with LF further supplements it in the oral or nasal cavity, thus strengthening the first protective barrier against bacteria and viruses from the outside [60,139,140,141,142,143]. The effectiveness of LF has been established in numerous in vitro, animal, and human studies in which LF, used in oral and vaginal formulations, positively altered the ecosystem of the reproductive tract by eliminating pathogenic microorganisms and increasing Lactobacillus species, re-establishing the state of eubiosis and protecting from dangerous consequences of dysbiosis, such as premature labor or miscarriage [6,144].
So far, most of the data on the positive effects of LF in pathological conditions are mainly based on studies in animal models. To date, studies in animal models have shown a significant increase in survival in rodents when sepsis developed after injection of E. coli [145]. Subsequent work revealed the strong anti-inflammatory effect of LF in models with induced gastritis or enteritis. However, the most promising results come from experiments based on the administration of lactoferrin to subjects with immature digestive systems (possibly due to an underdeveloped intestinal microbiome). Calves and newborn rats were characterized by better absorption of nutrients and a significant increase in intestinal villi length and stimulation of the development of the immune system [40,142,146,147,148,149]. Lactoferrin was reported to protect against oxidative stress-induced mitochondrial dysfunction and DNA damage, thus modulating innate immune responsiveness which can further alter the production of immune regulatory mediators that are important for directing the development of adaptive immune function [12,19,31,39,75,150]. Such LF action was revealed both in cell culture and within an animal model of endotoxemia. In fact, mitochondria from lipopolysaccharide (LPS)-treated animals released significantly higher amounts of H2O2 than those isolated from LF-pre-treated plus LPS-challenged animals [150]. This mechanism is of fundamental protective importance at the beginning of an infection. After the infection phase, lactoferrin shows a strong immunotropic effect: it stimulates the cells of the immune system to mature rapidly and enhance the immune response.
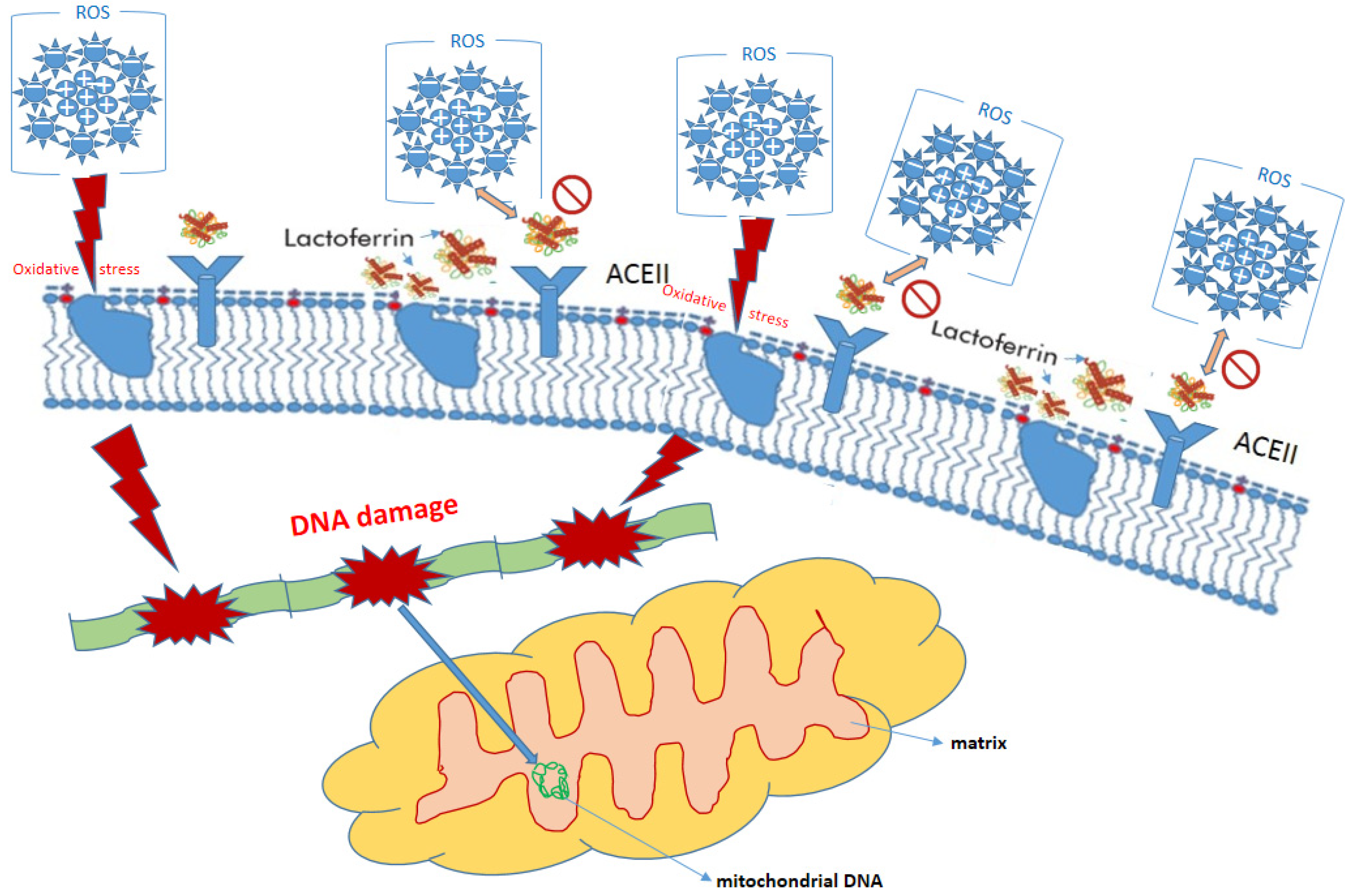
In order to not rely only on animal studies, it is worth recalling clinical trials. Among adults, it was possible to notice an improvement in the condition of people suffering from chronic H. pylori infection (the most common cause of peptic ulcer disease) in a form resistant to conventional treatment [151]. The results of studies involving patients suffering from various types of cancer are also promising, although preliminary. The anticancer effects of supplementation with LF in the gastrointestinal tract cancer and protection against colon cancer, stomach cancer, liver cancer and pancreatic cancer may be explained by the antioxidant properties of lactoferrin [12,152,153,154,155] (Figure 3).
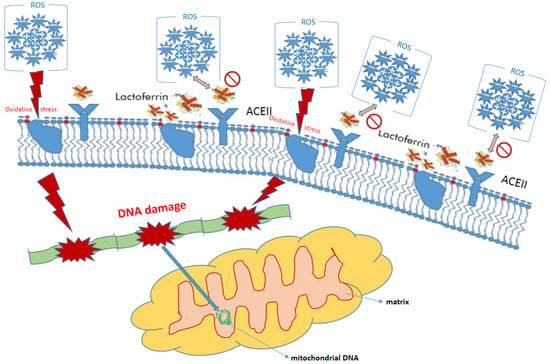
Figure 3.
Protective role of lactoferrin in eukaryotic cell.
Nevertheless, if we consider using LF in therapy, the form of its administration is very important. Lactoferrin is a hydrophilic substance, therefore in the non-liposomal version it has very limited absorption from the stomach [19]. In free form, it is decomposed there by hydrochloric acid and enzymes (proteases). Therefore, the bioavailability of the free form of lactoferrin may be limited. The use of small liposome vesicles may be beneficial in this case [156,157,158]. Nanoliposomes protect lactoferrin from destruction by digestive juices, allowing the intact protein to pass into the duodenum, from there into the general circulation, ensuring its high bioavailability [159] and impact on iron ions homeostasis, the skeletal system and, of course, the immune system.
LF administered in a phosphatidylcholine encapsulated form also has the potential to penetrate deep into the mucosa, and due to the small size of the nanoliposome (100 nm) compared to the virus size (150 nm), it is more competitive in reaching receptors on target cells where it settles in front of the virus [156,157]. It is important to note that the mucous membranes lining the oral or nasal cavities are very permeable, so this additional protection against viruses based on nanolactoferrin is very relevant.
3. Conclusions
Lactoferrin is a multifunctional protein derived from milk with high affinity for iron ions. It is known that iron is necessary for microorganisms to grow and reproduce, so the sequestration of iron significantly reduces their pathogenic potential. LF has numerous beneficial properties—antibacterial, antiviral, antifungal and antiparasitic, as well as immunomodulatory, anti-inflammatory and anticancer properties—that may play an important role in maintaining health from fetal life to old age. Currently, LF is an ingredient in many supplements and medicines, but a thorough understanding of the mechanisms of its beneficial effects requires further in-depth research.
Author Contributions
Conceptualization, resources, data curation writing—original draft preparation, writing—review and editing, visualization, supervision, project administration: P.K. (Paweł Kowalczyk), K.K. (Katarzyna Kaczyńska), P.K. (Patrycja Kleczkowska), I.B.-O., K.K. (Karol Kramkowski) and D.S.; funding acquisition, K.K. (Karol Kramkowski). All authors have read and agreed to the published version of the manuscript.
Funding
This research was funded by Medical University of Białystok, Poland. no.: SUB/2/DN/22/001/2201.
Institutional Review Board Statement
Not applicable.
Informed Consent Statement
Not applicable.
Data Availability Statement
On request of those interested.
Conflicts of Interest
The authors declare no conflict of interest.
Compliance with Ethical Standards
This article does not contain any studies with human participants performed by any of the authors.
References
- Poljsak, B.; Šuput, D.; Milisav, I. Achieving the Balance between ROS and Antioxidants: When to Use the Synthetic Antioxidants. Oxidative Med. Cell. Longev. 2013, 2013, 956792. [Google Scholar] [CrossRef] [PubMed]
- Kowalczyk, P.; Sulejczak, D.; Kleczkowska, P.; Bukowska-Ośko, I.; Kucia, M.; Popiel, M.; Wietrak, E.; Kramkowski, K.; Wrzosek, K.; Kaczyńska, K. Mitochondrial Oxidative Stress—A Causative Factor and Therapeutic Target in Many Diseases. Int. J. Mol. Sci. 2021, 22, 13384. [Google Scholar] [CrossRef] [PubMed]
- Parekattil, S.J.; Esteves, S.C.; Agarwal, A. Harmful Effects of Antioxidant Therapy. In Male Infertility; Springer: Berlin/Heidelberg, Germany, 2020. [Google Scholar]
- Klein, E.A.; Thompson, I.M.; Tangen, C.M.; Crowley, J.J.; Lucia, M.S.; Goodman, P.J.; Minasian, L.M.; Ford, L.G.; Parnes, H.L.; Gaziano, J.M.; et al. Vitamin E and the risk of prostate cancer: The Selenium and Vitamin E Cancer Prevention Trial (SELECT). JAMA 2011, 306, 1549–1556. [Google Scholar] [CrossRef] [PubMed]
- Alpha-Tocopherol Beta Carotene Cancer Prevention Study Group. The effect of vitamin E and beta carotene on the incidence of lung cancer and other cancers in male smokers. N. Engl. J. Med. 1994, 330, 1029–1035. [Google Scholar] [CrossRef]
- Artym, J.; Zimecki, M. Antimicrobial and Prebiotic Activity of Lactoferrin in the Female Reproductive Tract: A Comprehensive Review. Biomedicines 2021, 9, 1940. [Google Scholar] [CrossRef]
- Bielecka, M.; Cichosz, G.; Czeczot, H. Antioxidant, antimicrobial and anticarcinogenic activities of bovine milk proteins and their hydrolysates—A review. Int. Dairy J. 2021, 127, 105208. [Google Scholar] [CrossRef]
- Li, B.; Zhang, B.; Liu, X.; Zheng, Y.; Han, K.; Liu, H.; Wu, C.; Li, J.; Fan, S.; Peng, W.; et al. The effect of lactoferrin in aging: Role and potential. Food Funct. 2021, 13, 501–513. [Google Scholar] [CrossRef]
- Guzmán-Mejía, F.; Vega-Bautista, A.; Molotla-Torres, D.E.; Aguirre-Garrido, J.F.; Drago-Serrano, M.E. Bovine lactoferrin as a Modulator of Neuroendocrine Components of Stress. Curr. Mol. Pharmacol. 2021, 14, 1037–1045. [Google Scholar] [CrossRef]
- Bukowska-Osko, I.; Popiel, M.; Kowalczyk, P. The Immunological Role of the Placenta in SARS-CoV-2 Infection-Viral Transmission, Immune Regulation, and Lactoferrin Activity. Int. J. Mol. Sci. 2021, 22, 5799. [Google Scholar] [CrossRef]
- Baker, H.M.; Baker, E.N. A structural perspective on lactoferrin function. Biochem. Cell Biol. 2012, 90, 320–328. [Google Scholar] [CrossRef]
- Legrand, D.; Pierce, A.; Elass, E.; Carpentier, M.; Mariller, C.; Mazurier, J. Lactoferrin Structure and Functions. Bioact. Compon. Milk 2008, 606, 163–194. [Google Scholar] [CrossRef]
- Rascón-Cruz, Q.; Espinoza-Sánchez, E.A.; Siqueiros-Cendón, T.S.; Nakamura-Bencomo, S.I.; Arévalo-Gallegos, S.; Iglesias-Figueroa, B.F. Lactoferrin: A Glycoprotein Involved in Immunomodulation, Anticancer, and Antimicrobial Processes. Molecules 2021, 26, 205. [Google Scholar] [CrossRef] [PubMed]
- Mariller, C.; Hardivillé, S.; Hoedt, E.; Huvent, I.; Pina-Canseco, S.; Pierce, A. Delta-lactoferrin, an intracellular lactoferrin isoform that acts as a transcription factor. Biochem. Cell Biol. 2012, 90, 307–319. [Google Scholar] [CrossRef] [PubMed]
- Albar, A.; Almehdar, H.; Uversky, V.; Redwan, E. Structural Heterogeneity and Multifunctionality of Lactoferrin. Curr. Protein Pept. Sci. 2014, 15, 778–797. [Google Scholar] [CrossRef] [PubMed]
- Alexander, D.B.; Iigo, M.; Yamauchi, K.; Suzui, M.; Tsuda, H. Lactoferrin: An alternative view of its role in human biological fluids. Biochem. Cell Biol. 2012, 90, 279–306. [Google Scholar] [CrossRef] [PubMed]
- Siqueiros-Cendón, T.; Arévalo-Gallegos, S.; Iglesias-Figueroa, B.F.; García-Montoya, I.A.; Salazar-Martínez, J.; Rascón-Cruz, Q. Immunomodulatory effects of lactoferrin. Acta Pharmacol. Sin. 2014, 35, 557–566. [Google Scholar] [CrossRef] [PubMed]
- Mazurier, J.; Spik, G. Comparative study of the iron-binding properties of human transferrins: I. Complete and sequential iron saturation and desaturation of the lactotransferrin. Biochim. Biophys. Acta (BBA)-Gen. Subj. 1980, 629, 399–408. [Google Scholar] [CrossRef]
- Wang, B.; Timilsena, Y.P.; Blanch, E.; Adhikari, B. Lactoferrin: Structure, function, denaturation and digestion. Crit. Rev. Food Sci. Nutr. 2019, 59, 580–596. [Google Scholar] [CrossRef]
- Arnold, R.R.; Brewer, M.; Gauthier, J.J. Bactericidal activity of human lactoferrin: Sensitivity of a variety of microorganisms. Infect. Immun. 1980, 28, 893–898. [Google Scholar] [CrossRef]
- Rosa, L.; Cutone, A.; Lepanto, M.S.; Paesano, R.; Valenti, P. Lactoferrin: A Natural Glycoprotein Involved in Iron and Inflammatory Homeostasis. Int. J. Mol. Sci. 2017, 18, 1985. [Google Scholar] [CrossRef]
- Artym, J. A remedy against obesity? The role of lactoferrin in the metabolism of glucose and lipids. Postepy Hig. Med. Dosw. (Online) 2012, 66, 937–953. [Google Scholar] [CrossRef] [PubMed]
- Petschow, B.W.; Talbott, R.D.; Batema, R.P. Ability of lactoferrin to promote the growth of Bifidobacterium spp. in vitro is independent of receptor binding capacity and iron saturation level. J. Med. Microbiol. 1999, 48, 541–549. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chen, P.-W.; Ku, Y.-W.; Chu, F.-Y. Influence of bovine lactoferrin on the growth of selected probiotic bacteria under aerobic conditions. BioMetals 2014, 27, 905–914. [Google Scholar] [CrossRef] [PubMed]
- Kim, W.-S.; Ohashi, M.; Tanaka, T.; Kumura, H.; Kim, G.-Y.; Kwon, I.-K.; Goh, J.-S.; Shimazaki, K.-I. Growth-promoting effects of lactoferrin on L. acidophilus and Bifidobacterium spp. BioMetals 2004, 17, 279–283. [Google Scholar] [CrossRef] [PubMed]
- Bruni, N.; Capucchio, M.T.; Biasibetti, E.; Pessione, E.; Cirrincione, S.; Giraudo, L.; Corona, A.; Dosio, F. Antimicrobial Activity of Lactoferrin-Related Peptides and Applications in Human and Veterinary Medicine. Molecules 2016, 21, 752. [Google Scholar] [CrossRef]
- Cornish, J.; Callon, K.E.; Naot, D.; Palmano, K.P.; Banovic, T.; Bava, U.; Watson, M.; Lin, J.; Tong, P.C.; Chen, Q.; et al. Lactoferrin Is a Potent Regulator of Bone Cell Activity and Increases Bone Formation In Vivo. Endocrinology 2004, 145, 4366–4374. [Google Scholar] [CrossRef] [Green Version]
- Zhang, J.; Han, X.; Shan, Y.; Zhang, L.; Du, M.; Liu, M.; Yi, H.; Ma, Y. Effect of bovine lactoferrin and human lactoferrin on the proliferative activity of the osteoblast cell line MC3T3-E1 in vitro. J. Dairy Sci. 2018, 101, 1827–1833. [Google Scholar] [CrossRef] [Green Version]
- Lorget, F.; Clough, J.; Oliveira, M.; Daury, M.-C.; Sabokbar, A.; Offord, E. Lactoferrin reduces in vitro osteoclast differentiation and resorbing activity. Biochem. Biophys. Res. Commun. 2002, 296, 261–266. [Google Scholar] [CrossRef]
- Grey, A.; Zhu, Q.; Watson, M.; Callon, K.; Cornish, J. Lactoferrin potently inhibits osteoblast apoptosis, via an LRP1-independent pathway. Mol. Cell. Endocrinol. 2006, 251, 96–102. [Google Scholar] [CrossRef]
- Shoji, H.; Oguchi, S.; Shinohara, K.; Shimizu, T.; Yamashiro, Y. Effects of Iron-Unsaturated Human Lactoferrin on Hydrogen Peroxide-Induced Oxidative Damage in Intestinal Epithelial Cells. Pediatr. Res. 2007, 61, 89–92. [Google Scholar] [CrossRef] [Green Version]
- Artym, J.; Zimecki, M. Milk-derived proteins and peptides in clinical trials. Postepy Hig. Med. Dosw. 2013, 67, 800–816. [Google Scholar] [CrossRef] [PubMed]
- Mayadas, T.N.; Cullere, X.; Lowell, C.A. The Multifaceted Functions of Neutrophils. Annu. Rev. Pathol. Mech. Dis. 2014, 9, 181–218. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Chen, K.; Chai, L.; Li, H.; Zhang, Y.; Xie, H.-M.; Shang, J.; Tian, W.; Yang, P.; Jiang, A.C. Effect of bovine lactoferrin from iron-fortified formulas on diarrhea and respiratory tract infections of weaned infants in a randomized controlled trial. Nutrition 2016, 32, 222–227. [Google Scholar] [CrossRef] [PubMed]
- Manzoni, P.; Rinaldi, M.; Cattani, S.; Pugni, L.; Romeo, M.G.; Messner, H.; Stolfi, I.; Decembrino, L.; Laforgia, N.; Vagnarelli, F.; et al. Bovine Lactoferrin Supplementation for Prevention of Late-Onset Sepsis in Very Low-Birth-Weight Neonates: A Randomized Trial. JAMA 2009, 302, 1421–1428. [Google Scholar] [CrossRef]
- Sherman, M.P.; Sherman, J.; Arcinue, R.; Niklas, V. Randomized Control Trial of Human Recombinant Lactoferrin: A Substudy Reveals Effects on the Fecal Microbiome of Very Low Birth Weight Infants. J. Pediatr. 2016, 173, S37–S42. [Google Scholar] [CrossRef] [Green Version]
- Johnston, W.H.; Ashley, C.; Yeiser, M.; Harris, C.L.; Stolz, S.I.; Wampler, J.L.; Wittke, A.; Cooper, T.R. Growth and tolerance of formula with lactoferrin in infants through one year of age: Double-blind, randomized, controlled trial. BMC Pediatr. 2015, 15, 173. [Google Scholar] [CrossRef] [Green Version]
- Manzoni, P. Clinical Studies of Lactoferrin in Neonates and Infants: An Update. Breastfeed. Med. 2019, 14, S25–S27. [Google Scholar] [CrossRef] [Green Version]
- Debbabi, H.; Dubarry, M.; Rautureau, M.; Tomé, D. Bovine lactoferrin induces both mucosal and systemic immune response in mice. J. Dairy Res. 1998, 65, 283–293. [Google Scholar] [CrossRef]
- Baldi, A.; Ioannis, P.; Chiara, P.; Eleonora, F.; Roubini, C.; Vittorio, D. Biological effects of milk proteins and their peptides with emphasis on those related to the gastrointestinal ecosystem. J. Dairy Res. 2005, 72, 66–72. [Google Scholar] [CrossRef]
- Balmer, S.E.; Scott, P.H.; Wharton, B.A. Diet and faecal flora in the newborn: Lactoferrin. Arch. Dis. Child. 1989, 64, 1685–1690. [Google Scholar] [CrossRef] [Green Version]
- Cleminson, J.S.; Zalewski, S.P.; Embleton, N.D. Nutrition in the preterm infant: What’s new? Curr. Opin. Clin. Nutr. Metab. Care 2016, 19, 220–225. [Google Scholar] [PubMed]
- ELFIN Investigators Group. Enteral lactoferrin supplementation for very preterm infants: A randomised placebo-controlled trial. Lancet 2019, 393, 423–433. [Google Scholar] [CrossRef] [Green Version]
- Artym, J.; Zimecki, M.; Kruzel, M. Lactoferrin for Prevention and Treatment of Anemia and Inflammation in Pregnant Women: A Comprehensive Review. Biomedicines 2021, 9, 898. [Google Scholar] [CrossRef] [PubMed]
- Yanaihara, A.; Mitsukawa, K.; Iwasaki, S.; Otsuki, K.; Kawamura, T.; Okai, T. High concentrations of lactoferrin in the follicular fluid correlate with embryo quality during in vitro fertilization cycles. Fertil. Steril. 2007, 87, 279–282. [Google Scholar] [CrossRef]
- Mostafa, M.H.; Faisal, M.M.; Mohamed, N.R.; Idle, F.H. Effect of Follicular Fluid Lactoferrin Level on Oocytes Quality and Pregnancy Rate in Intracytoplasmic Sperm Injection Cycles. Open J. Obstet. Gynecol. 2019, 9, 745–754. [Google Scholar] [CrossRef] [Green Version]
- Omes, C.; De Amici, M.; Tomasoni, V.; Todaro, F.; Torre, C.; Nappi, R.E. Myeloperoxidase and lactoferrin expression in semen fluid: Novel markers of male infertility risk? Immunobiology 2020, 225, 151999. [Google Scholar] [CrossRef]
- Buckett, W.M.; Luckas, M.J.; Gazvani, M.; Aird, I.A.; Lewis-Jones, D.I. Seminal plasma lactoferrin concentrations in normal and abnormal semen samples. J. Androl. 1997, 18, 302–304. [Google Scholar] [CrossRef]
- Manzoni, P.; Stolfi, I.; Messner, H.; Cattani, S.; Laforgia, N.; Romeo, M.G.; Bollani, L.; Rinaldi, M.; Gallo, E.; Quercia, M.; et al. Bovine Lactoferrin Prevents Invasive Fungal Infections in Very Low Birth Weight Infants: A Randomized Controlled Trial. Pediatrics 2012, 129, 116–123. [Google Scholar] [CrossRef]
- Drago-Serrano, M.E.; Campos-Rodríguez, R.; Carrero, J.C.; De La Garza, M. Lactoferrin: Balancing Ups and Downs of Inflammation Due to Microbial Infections. Int. J. Mol. Sci. 2017, 18, 501. [Google Scholar] [CrossRef] [Green Version]
- Actor, J.K.; Hwang, S.-A.; Kruzel, M.L. Lactoferrin as a Natural Immune Modulator. Curr. Pharm. Des. 2009, 15, 1956–1973. [Google Scholar] [CrossRef] [Green Version]
- Cacho, N.T.; Lawrence, R.M. Innate Immunity and Breast Milk. Front. Immunol. 2017, 8, 584. [Google Scholar] [CrossRef] [Green Version]
- Zasada, M.; Kwinta, P.; Durlak, W.; Bik-Multanowski, M.; Madetko-Talowska, A.; Pietrzyk, J.J. Development and Maturation of the Immune System in Preterm Neonates: Results from a Whole Genome Expression Study. BioMed Res. Int. 2014, 2014, 498318. [Google Scholar] [CrossRef] [PubMed]
- Harbeson, D.; Ben-Othman, R.; Amenyogbe, N.; Kollmann, T. Outgrowing the Immaturity Myth: The Cost of Defending From Neonatal Infectious Disease. Front. Immunol. 2018, 9, 1077. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Vargas-Bello-Pérez, E.; Márquez-Hernández, R.I.; Hernández-Castellano, L.E. Bioactive peptides from milk: Animal determinants and their implications in human health. J. Dairy Res. 2019, 86, 136–144. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zimecki, M.; Spiegel, K.; Właszczyk, A.; Kübler, A.; Kruzel, M.L. Lactoferrin increases the output of neutrophil precursors and attenuates the spontaneous production of TNF-alpha and IL-6 by peripheral blood cells. Arch. Immunol. Ther. Exp. 1999, 47, 113–118. [Google Scholar]
- Li, Y.; Huang, J.; Wang, J.; Ma, M.; Lu, Y.; Wang, R.; Guo, H. Lactoferrin Is a Potential Activator of the Vitamin D Receptor in Its Regulation of Osteogenic Activities in C57BL/6J Mice and MC3T3-E1 Cells. J. Nutr. 2021, 151, 2105–2113. [Google Scholar] [CrossRef]
- Meyer, M.P.; Alexander, T. Reduction in necrotizing enterocolitis and improved outcomes in preterm infants following routine supplementation with Lactobacillus GG in combination with bovine lactoferrin. J. Neonatal Perinat. Med. 2017, 10, 249–255. [Google Scholar] [CrossRef]
- Chen, K.; Zhang, G.; Chen, H.; Cao, Y.; Dong, X.; Li, H.; Liu, C. Dose Effect of Bovine Lactoferrin Fortification on Iron Metabolism of Anemic Infants. J. Nutr. Sci. Vitaminol. 2020, 66, 24–31. [Google Scholar] [CrossRef] [Green Version]
- Weimer, K.E.D.; Roark, H.; Fisher, K.; Cotten, C.M.; Kaufman, D.A.; Bidegain, M.; Permar, S.R. Breast Milk and Saliva Lactoferrin Levels and Postnatal Cytomegalovirus Infection. Am. J. Perinatol. 2020, 38, 1070–1077. [Google Scholar] [CrossRef]
- Zhang, P.; Sawicki, V.; Lewis, A.; Hanson, L.; Nuijens, J.H.; Neville, M.C. Human Lactoferrin in the Milk of Transgenic Mice Increases Intestinal Growth in Ten-Day-Old Suckling Neonates. Adv. Exp. Med. Biol. 2001, 501, 107–113. [Google Scholar] [CrossRef]
- Buccigrossi, V.; De Marco, G.; Bruzzese, E.; Ombrato, L.; Bracale, I.; Polito, G.; Guarino, A. Lactoferrin Induces Concentration-Dependent Functional Modulation of Intestinal Proliferation and Differentiation. Pediatr. Res. 2007, 61, 410–414. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hirotani, Y.; Ikeda, K.; Kato, R.; Myotoku, M.; Umeda, T.; Ijiri, Y.; Tanaka, K. Protective Effects of Lactoferrin against Intestinal Mucosal Damage Induced by Lipopolysaccharide in Human Intestinal Caco-2 Cells. Yakugaku Zasshi 2008, 128, 1363–1368. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kruzel, M.L.; Harari, Y.; Chen, C.-Y.; Castro, G.A. Lactoferrin Protects Gut Mucosal Integrity During Endotoxemia Induced by Lipopolysaccharide in Mice. Inflammation 2000, 24, 33–44. [Google Scholar] [CrossRef] [PubMed]
- Troost, F.J.; Saris, W.H.M.; Brummer, R.-J.M. Recombinant human lactoferrin ingestion attenuates indomethacin-induced enteropathy in vivo in healthy volunteers. Eur. J. Clin. Nutr. 2003, 57, 1579–1585. [Google Scholar] [CrossRef] [PubMed]
- Jenssen, H.; Hancock, R.E.W. Antimicrobial properties of lactoferrin. Biochimie 2009, 91, 19–29. [Google Scholar] [CrossRef] [PubMed]
- Chissov, V.I.; Iakubovskaia, R.I.; Nemtsova, E.R.; Osipova, N.; Edeleva, N.V.; Utkin, M.M.; Zviagin, A.A. Antioxidants treatment of severe post-operative pyoinflammatory and septic complications. Khirurgiia 2008, 11, 14–19. [Google Scholar]
- Edde, L.; Hipolito, R.B.; Hwang, F.F.Y.; Headon, D.R.; Shalwitz, R.A.; Sherman, M.P. Lactoferrin protects neonatal rats from gut-related systemic infection. Am. J. Physiol. Liver Physiol. 2001, 281, G1140–G1150. [Google Scholar] [CrossRef] [PubMed]
- Kruzel, M.L.; Zimecki, M.; Actor, J.K. Lactoferrin in a Context of Inflammation-Induced Pathology. Front. Immunol. 2017, 8, 1438. [Google Scholar] [CrossRef] [PubMed]
- Alexander, D.B.; Iigo, M.; Abdelgied, M.; Ozeki, K.; Tanida, S.; Joh, T.; Takahashi, S.; Tsuda, H. Bovine lactoferrin and Crohn’s disease: A case study. Biochem. Cell Biol. 2017, 95, 133–141. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Li, L.; Ren, F.; Yun, Z.; An, Y.; Wang, C.; Yan, X. Determination of the effects of lactoferrin in a preclinical mouse model of experimental colitis. Mol. Med. Rep. 2013, 8, 1125–1129. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Wu, J.; Chen, J.; Wu, W.; Shi, J.; Zhong, Y.; van Tol, E.A.F.; Tang, Q.; Cai, W. Enteral supplementation of bovine lactoferrin improves gut barrier function in rats after massive bowel resection. Br. J. Nutr. 2014, 112, 486–492. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Lizzi, A.R.; Carnicelli, V.; Clarkson, M.M.; DI Giulio, A.; Oratore, A. Lactoferrin Derived Peptides: Mechanisms of Action and their Perspectives as Antimicrobial and Antitumoral Agents. Mini Rev. Med. Chem. 2009, 9, 687–695. [Google Scholar] [CrossRef] [PubMed]
- Tolone, S.; Pellino, V.; Vitaliti, G.; Lanzafame, A.; Tolone, C. Evaluation of Helicobacter Pylori eradication in pediatric patients by triple therapy plus lactoferrin and probiotics compared to triple therapy alone. Ital. J. Pediatr. 2012, 38, 63. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Artym, J.; Kocięba, M.; Zaczyńska, E.; Adamik, B.; Kübler, A.; Zimecki, M.; Kruzel, M. Immunomodulatory properties of human recombinant lactoferrin in mice: Implications for therapeutic use in humans. Adv. Clin. Exp. Med. 2018, 27, 391–399. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Tomita, M.; Wakabayashi, H.; Yamauchi, K.; Teraguchi, S.; Hayasawa, H. Bovine lactoferrin and lactoferricin derived from milk: Production and applications. Biochem. Cell Biol. 2002, 80, 109–112. [Google Scholar] [CrossRef] [PubMed]
- Berlutti, F.; Pantanella, F.; Natalizi, T.; Frioni, A.; Paesano, R.; Polimeni, A.; Valenti, P. Antiviral Properties of Lactoferrin—A Natural Immunity Molecule. Molecules 2011, 16, 6992–7018. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Miotto, M.; Di Rienzo, L.; Bò, L.; Boffi, A.; Ruocco, G.; Milanetti, E. Molecular Mechanisms Behind Anti SARS-CoV-2 Action of Lactoferrin. Front. Mol. Biosci. 2021, 8, 607443. [Google Scholar] [CrossRef]
- Salaris, C.; Scarpa, M.; Elli, M.; Bertolini, A.; Guglielmetti, S.; Pregliasco, F.; Blandizzi, C.; Brun, P.; Castagliuolo, I. Protective Effects of Lactoferrin against SARS-CoV-2 Infection In Vitro. Nutrients 2021, 13, 328. [Google Scholar] [CrossRef]
- Wang, Y.; Wang, P.; Wang, H.; Luo, Y.; Wan, L.; Jiang, M.; Chu, Y. Lactoferrin for the treatment of COVID-19 (Review). Exp. Ther. Med. 2020, 20, 272. [Google Scholar] [CrossRef]
- Wakabayashi, H.; Uchida, K.; Yamauchi, K.; Teraguchi, S.; Hayasawa, H.; Yamaguchi, H. Lactoferrin given in food facilitates dermatophytosis cure in guinea pig models. J. Antimicrob. Chemother. 2000, 46, 595–602. [Google Scholar] [CrossRef]
- León-Sicairos, N.; Ordaz-Pichardo, C.; Carrero, J.C.; de la Garza, M. Lactoferrin in the Battle against Intestinal Parasites: A Review. In Natural Remedies in the Fight Against Parasites; Intechopen: London, UK, 2017. [Google Scholar] [CrossRef] [Green Version]
- Gruden, Š.; Ulrih, N.P. Diverse Mechanisms of Antimicrobial Activities of Lactoferrins, Lactoferricins, and Other Lactoferrin-Derived Peptides. Int. J. Mol. Sci. 2021, 22, 11264. [Google Scholar] [CrossRef] [PubMed]
- Ramírez-Rico, G.; Drago-Serrano, M.E.; León-Sicairos, N.; de la Garza, M. Lactoferrin: A Nutraceutical with Activity against Colorectal Cancer. Front. Pharmacol. 2022, 13, 855852. [Google Scholar] [CrossRef] [PubMed]
- Amitay, E.L.; Keinan-Boker, L. Breastfeeding and Childhood Leukemia Incidence. JAMA Pediatrics 2015, 169, e151025. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Zhang, Y.; Lima, C.F.; Rodrigues, L.R. Anticancer effects of lactoferrin: Underlying mechanisms and future trends in cancer therapy. Nutr. Rev. 2014, 72, 763–773. [Google Scholar] [CrossRef] [Green Version]
- Cutone, A.; Rosa, L.; Ianiro, G.; Lepanto, M.S.; Bonaccorsi di Patti, M.C.; Valenti, P.; Musci, G. Lactoferrin’s Anti-Cancer Properties: Safety, Selectivity, and Wide Range of Action. Biomolecules 2020, 10, 456. [Google Scholar] [CrossRef] [Green Version]
- Iglesias-Figueroa, B.F.; Siqueiros-Cendón, T.S.; Gutierrez, D.A.; Aguilera, R.J.; Espinoza-Sánchez, E.A.; Arévalo-Gallegos, S.; Varela-Ramirez, A.; Rascón-Cruz, Q. Recombinant human lactoferrin induces apoptosis, disruption of F-actin structure and cell cycle arrest with selective cytotoxicity on human triple negative breast cancer cells. Apoptosis 2019, 24, 562–577. [Google Scholar] [CrossRef]
- Mariller, C.; Benaïssa, M.; Hardivillé, S.; Breton, M.; Pradelle, G.; Mazurier, J.; Pierce, A. Human delta-lactoferrin is a transcription factor that enhances Skp1 (S-phase kinase-associated protein) gene expression. FEBS J. 2007, 274, 2038–2053. [Google Scholar] [CrossRef]
- Hardivillé, S.; Escobar-Ramírez, A.; Pina-Canceco, S.; Elass, E.; Pierce, A. Delta-lactoferrin induces cell death via the mitochondrial death signaling pathway by upregulating bax expression. BioMetals 2014, 27, 875–889. [Google Scholar] [CrossRef]
- Mariller, C.; Hardivillé, S.; Hoedt, E.; Benaïssa, M.; Mazurier, J.; Pierce, A. Proteomic approach to the identification of novel delta-lactoferrin target genes: Characterization of DcpS, an mRNA scavenger decapping enzyme. Biochimie 2009, 91, 109–122. [Google Scholar] [CrossRef]
- Hoedt, E.; Chaoui, K.; Huvent, I.; Mariller, C.; Monsarrat, B.; Burlet-Schiltz, O.; Pierce, A. SILAC-Based Proteomic Profiling of the Human MDA-MB-231 Metastatic Breast Cancer Cell Line in Response to the Two Antitumoral Lactoferrin Isoforms: The Secreted Lactoferrin and the Intracellular Delta-Lactoferrin. PLoS ONE 2014, 9, e104563. [Google Scholar] [CrossRef] [Green Version]
- Siebert, P.D.; Huang, B.C.B. Identification of an alternative form of human lactoferrin mRNA that is expressed differentially in normal tissues and tumor-derived cell lines. Proc. Natl. Acad. Sci. USA 1997, 94, 2198–2203. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hoedt, E.; Hardivillé, S.; Mariller, C.; Elass, E.; Perraudin, J.-P.; Pierce, A. Discrimination and evaluation of lactoferrin and delta-lactoferrin gene expression levels in cancer cells and under inflammatory stimuli using TaqMan real-time PCR. BioMetals 2010, 23, 441–452. [Google Scholar] [CrossRef] [PubMed]
- Kazan, H.H.; Urfali-Mamatoglu, C.; Gunduz, U. Iron metabolism and drug resistance in cancer. BioMetals 2017, 30, 629–641. [Google Scholar] [CrossRef] [PubMed]
- Harman, D. The aging process. Proc. Natl. Acad. Sci. USA 1981, 78, 7124–7128. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Hayflick, L. Entropy Explains Aging, Genetic Determinism Explains Longevity, and Undefined Terminology Explains Misunderstanding Both. PLoS Genet. 2007, 3, e220. [Google Scholar] [CrossRef]
- Cardoso, A.L.; Fernandes, A.; Aguilar-Pimentel, J.A.; De Angelis, M.H.; Guedes, J.R.; Brito, M.A.; Ortolano, S.; Pani, G.; Athanasopoulou, S.; Gonos, E.S.; et al. Towards frailty biomarkers: Candidates from genes and pathways regulated in aging and age-related diseases. Ageing Res. Rev. 2018, 47, 214–277. [Google Scholar] [CrossRef]
- Birch, J.; Gil, J. Senescence and the SASP: Many therapeutic avenues. Genes Dev. 2020, 34, 1565–1576. [Google Scholar] [CrossRef]
- Childs, B.G.; Durik, M.; Baker, D.J.; Van Deursen, J.M. Cellular senescence in aging and age-related disease: From mechanisms to therapy. Nat. Med. 2015, 21, 1424–1435. [Google Scholar] [CrossRef] [Green Version]
- Martorell, P.; Llopis, S.; Gonzalez, N.; Ramón, D.; Serrano, G.; Torrens, A.; Serrano, J.M.; Navarro, M.; Genovés, S. A nutritional supplement containing lactoferrin stimulates the immune system, extends lifespan, and reduces amyloidβpeptide toxicity inCaenorhabditis elegans. Food Sci. Nutr. 2016, 5, 255–265. [Google Scholar] [CrossRef]
- Park, S.Y.; Jeong, A.-J.; Kim, G.-Y.; Jo, A.; Lee, J.E.; Leem, S.-H.; Yoon, J.-H.; Ye, S.K.; Chung, J.W. Lactoferrin Protects Human Mesenchymal Stem Cells from Oxidative Stress-Induced Senescence and Apoptosis. J. Microbiol. Biotechnol. 2017, 27, 1877–1884. [Google Scholar] [CrossRef] [Green Version]
- Raghavan, S.; Malayaperumal, S.; Mohan, V.; Balasubramanyam, M. A comparative study on the cellular stressors in mesenchymal stem cells (MSCs) and pancreatic β-cells under hyperglycemic milieu. Mol. Cell. Biochem. 2020, 476, 457–469. [Google Scholar] [CrossRef] [PubMed]
- Takayama, Y.; Aoki, R. Roles of lactoferrin on skin wound healing1This article is part of Special Issue entitled Lactoferrin and has undergone the Journal’s usual peer review process. Biochem. Cell Biol. 2012, 90, 497–503. [Google Scholar] [CrossRef] [PubMed]
- Tang, L.; Wu, J.; Ma, Q.; Cui, T.; Andreopoulos, F.; Gil, J.; Valdes, J.; Davis, S.; Li, J. Human lactoferrin stimulates skin keratinocyte function and wound re-epithelialization. Br. J. Dermatol. 2010, 163, 38–47. [Google Scholar] [CrossRef] [PubMed]
- Moreno-Navarrete, J.M.; Ortega, F.J.; Bassols, J.; Castro, A.; Ricart, W.; Fernández-Real, J.M. Association of Circulating Lactoferrin Concentration and 2 Nonsynonymous LTF Gene Polymorphisms with Dyslipidemia in Men Depends on Glucose-Tolerance Status. Clin. Chem. 2008, 54, 301–309. [Google Scholar] [CrossRef] [Green Version]
- Moreno-Navarrete, J.M.; Ortega, F.J.; Bassols, J.; Ricart, W.; Fernández-Real, J.M. Decreased Circulating Lactoferrin in Insulin Resistance and Altered Glucose Tolerance as a Possible Marker of Neutrophil Dysfunction in Type 2 Diabetes. J. Clin. Endocrinol. Metab. 2009, 94, 4036–4044. [Google Scholar] [CrossRef] [Green Version]
- Vengen, I.T.; Dale, A.C.; Wiseth, R.; Midthjell, K.; Videm, V. Lactoferrin is a novel predictor of fatal ischemic heart disease in diabetes mellitus type 2: Long-term follow-up of the HUNT 1 study. Atherosclerosis 2010, 212, 614–620. [Google Scholar] [CrossRef]
- Fernández-Real, J.M.; García-Fuentes, E.; Moreno-Navarrete, J.M.; Murri-Pierri, M.; Garrido-Sánchez, L.; Ricart, W.; Tinahones, F. Fat Overload Induces Changes in Circulating Lactoferrin That Are Associated With Postprandial Lipemia and Oxidative Stress in Severely Obese Subjects. Obesity 2010, 18, 482–488. [Google Scholar] [CrossRef]
- Santos-Silva, A.; Rebelo, I.; Castro, E.; Belo, L.; Catarino, C.; Monteiro, I.; Almeida, M.D.; Quintanilha, A. Erythrocyte damage and leukocyte activation in ischemic stroke. Clin. Chim. Acta 2002, 320, 29–35. [Google Scholar] [CrossRef]
- Carro, E.; Bartolome, F.; Bermejo-Pareja, F.; Villarejo-Galende, A.; Molina, J.A.; Ortiz, P.; Calero, M.; Rabano, A.; Cantero, J.L.; Orive, G. Early diagnosis of mild cognitive impairment and Alzheimer’s disease based on salivary lactoferrin. Alzheimer’s Dement. Diagn. Assess. Dis. Monit. 2017, 8, 131–138. [Google Scholar] [CrossRef]
- Yu, S.Y.; Sun, L.; Liu, Z.; Huang, X.Y.; Zuo, L.J.; Cao, C.J.; Zhang, W.; Wang, X.M. Sleep disorders in Parkinson’s disease: Clinical features, iron metabolism and related mechanism. PLoS ONE 2013, 8, e82924. [Google Scholar] [CrossRef] [Green Version]
- Langhorst, J.; Boone, J. Fecal lactoferrin as a noninvasive biomarker in inflammatory bowel diseases. Drugs Today 2012, 48, 149–161. [Google Scholar] [CrossRef] [PubMed]
- Stanczyk, J.; Kowalski, M.L.; Grzegorczyk, J.; Szkudlinska, B.; Jarzebska, M.; Marciniak, M.; Synder, M. RANTES and Chemotactic Activity in Synovial Fluids From Patients With Rheumatoid Arthritis and Osteoarthritis. Mediat. Inflamm. 2005, 2005, 343–348. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- González-Sánchez, M.; Bartolome, F.; Antequera, D.; Puertas-Martín, V.; González, P.; Gómez-Grande, A.; Llamas-Velasco, S.; Martín, A.H.-S.; Pérez-Martínez, D.; Villarejo-Galend, A.; et al. Decreased salivary lactoferrin levels are specific to Alzheimer’s disease. EBioMedicine 2020, 57, 102834. [Google Scholar] [CrossRef] [PubMed]
- Abdelhamid, M.; Jung, C.-G.; Zhou, C.; Abdullah, M.; Nakano, M.; Wakabayashi, H.; Abe, F.; Michikawa, M. Dietary Lactoferrin Supplementation Prevents Memory Impairment and Reduces Amyloid-β Generation in J20 Mice. J. Alzheimer’s Dis. 2020, 74, 245–259. [Google Scholar] [CrossRef] [PubMed]
- Liu, H.; Wu, H.; Zhu, N.; Xu, Z.; Wang, Y.; Qu, Y.; Wang, J. Lactoferrin protects against iron dysregulation, oxidative stress, and apoptosis in 1-methyl-4-phenyl-1,2,3,6-tetrahydropyridine (MPTP)-induced Parkinson’s disease in mice. J. Neurochem. 2019, 152, 397–415. [Google Scholar] [CrossRef]
- Xu, S.-F.; Zhang, Y.-H.; Wang, S.; Pang, Z.-Q.; Fan, Y.-G.; Li, J.-Y.; Wang, Z.-Y.; Guo, C. Lactoferrin ameliorates dopaminergic neurodegeneration and motor deficits in MPTP-treated mice. Redox Biol. 2018, 21, 101090. [Google Scholar] [CrossRef]
- Mohamed, W.A.; Salama, R.M.; Schaalan, M.F. A pilot study on the effect of lactoferrin on Alzheimer’s disease pathological sequelae: Impact of the p-Akt/PTEN pathway. Biomed. Pharmacother. 2019, 111, 714–723. [Google Scholar] [CrossRef]
- Li, Y.-Q.; Guo, C. A Review on Lactoferrin and Central Nervous System Diseases. Cells 2021, 10, 1810. [Google Scholar] [CrossRef]
- Zheng, J.; Xie, Y.; Li, F.; Zhou, Y.; Qi, L.; Liu, L.; Chen, Z. Lactoferrin improves cognitive function and attenuates brain senescence in aged mice. J. Funct. Foods 2019, 65, 103736. [Google Scholar] [CrossRef]
- Rousseau, E.; Michel, P.P.; Hirsch, E. The Iron-Binding Protein Lactoferrin Protects Vulnerable Dopamine Neurons from Degeneration by Preserving Mitochondrial Calcium Homeostasis. Mol. Pharmacol. 2013, 84, 888–898. [Google Scholar] [CrossRef] [Green Version]
- Moreno-Navarrete, J.M.; Ortega, F.J.; Sabater-Masdeu, M.; Ricart, W.; Fernández-Real, J.M. Proadipogenic effects of lactoferrin in human subcutaneous and visceral preadipocytes. J. Nutr. Biochem. 2011, 22, 1143–1149. [Google Scholar] [CrossRef] [PubMed]
- Moreno-Navarrete, J.M.; Ortega, F.J.; Ricart, W.; Fernández-Real, J.M. Lactoferrin increases 172ThrAMPK phosphorylation and insulin-induced p473SerAKT while impairing adipocyte differentiation. Int. J. Obes. 2009, 33, 991–1000. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Kaczmarek, N.; Jamka, M.; Walkowiak, J. An association of selected polymorphisms of the lactoferrin gene and genes for lactoferrin receptors in the prevalence of metabolic disorders in obese subjects. Pol. Merkur. Lekarski. 2020, 48, 120–123. [Google Scholar] [PubMed]
- Mayeur, S.; Spahis, S.; Pouliot, Y.; Levy, E. Lactoferrin, a Pleiotropic Protein in Health and Disease. Antioxid. Redox Signal. 2016, 24, 813–836. [Google Scholar] [CrossRef] [Green Version]
- Ikeda, Y.; Tajima, S.; Izawa-Ishizawa, Y.; Kihira, Y.; Ishizawa, K.; Yoshida, S.; Ken-ichi, A.; Koichiro, T.; Toshiaki, T. Bovine Milk–derived Lactoferrin Exerts Proangiogenic Effects in an Src-Akt-eNOS–dependent Manner in Response to Ischemia. J. Cardiovasc. Pharmacol. 2013, 61, 423–429. [Google Scholar] [CrossRef]
- Shi, P.; Fan, F.; Chen, H.; Xu, Z.; Cheng, S.; Lu, W.; Du, M. A bovine lactoferrin–derived peptide induced osteogenesis via regulation of osteoblast proliferation and differentiation. J. Dairy Sci. 2020, 103, 3950–3960. [Google Scholar] [CrossRef]
- Chen, X.-W.; Li, Y.-H.; Zhang, M.-J.; Chen, Z.; Ke, D.-S.; Xue, Y.; Hou, J.M. Lactoferrin ameliorates aging-suppressed osteogenesis via IGF1 signaling. J. Mol. Endocrinol. 2019, 63, 63–75. [Google Scholar] [CrossRef]
- Sadeghi, O.; Milajerdi, A.; Siadat, S.D.; Keshavarz, S.A.; Sima, A.R.; Vahedi, H.; Adibi, P.; Esmaillzadeh, A. Effects of soy milk consumption on gut microbiota, inflammatory markers, and disease severity in patients with ulcerative colitis: A study protocol for a randomized clinical trial. Trials 2020, 21, 565. [Google Scholar] [CrossRef]
- Yang, Z.; Jiang, R.; Chen, Q.; Wang, J.; Duan, Y.; Pang, X.; Jiang, S.; Bi, Y.; Zhang, H.; Lönnerdal, B.; et al. Concentration of Lactoferrin in Human Milk and Its Variation during Lactation in Different Chinese Populations. Nutrients 2018, 10, 1235. [Google Scholar] [CrossRef] [Green Version]
- Available online: https://foodsupplementseurope.org (accessed on 28 April 2022).
- EFSA Panel on Dietetic Products. Nutrition and Allergies: Scientific opinion on bovine lactoferrin. EFSA J. 2012, 10, 2701. [Google Scholar] [CrossRef] [Green Version]
- GRAS Notice (GRN), No. 669, Cow’s Milk-Derived Lactoferrin. Available online: https://www.fda.gov (accessed on 12 September 2021).
- Wakabayashi, H.; Yamauchi, K.; Abe, F. Quality control of commercial bovine lactoferrin. BioMetals 2018, 31, 313–319. [Google Scholar] [CrossRef] [PubMed]
- Goodman, R.E.; Taylor, S.L.; Yamamura, J.; Kobayashi, T.; Kawakami, H.; Kruger, C.L.; Thompson, G.P. Assessment of the potential allergenicity of a Milk Basic Protein fraction. Food Chem. Toxicol. 2007, 45, 1787–1794. [Google Scholar] [CrossRef] [PubMed]
- Kurittu, J.; Lönnberg, S.; Virta, M.; Karp, M. Qualitative Detection of Tetracycline Residues in Milk with a Luminescence-Based Microbial Method: The Effect of Milk Composition and Assay Performance in Relation to an Immunoassay and a Microbial Inhibition Assay. J. Food Prot. 2000, 63, 953–957. [Google Scholar] [CrossRef] [PubMed]
- Hogendorf, A.; Stańczyk-Przyłuska, A.; Sieniwicz-Luzeńczyk, K.; Wiszniewska, M.; Arendarczyk, J.; Banasik, M.; Fendler, W.; Kowalski, M.; Zeman, K. Is there any association between secretory IgA and lactoferrin concentration in mature human milk and food allergy in breastfed children. Med. Wieku Rozw. 2013, 17, 47–52. [Google Scholar]
- Gleerup, H.S.; Jensen, C.S.; Høgh, P.; Hasselbalch, S.G.; Simonsen, A.H. Lactoferrin in cerebrospinal fluid and saliva is not a diagnostic biomarker for Alzheimer’s disease in a mixed memory clinic population. EBioMedicine 2021, 67, 103361. [Google Scholar] [CrossRef]
- Zhang, Y.; Lu, C.; Zhang, J. Lactoferrin and Its Detection Methods: A Review. Nutrients 2021, 13, 2492. [Google Scholar] [CrossRef]
- Ramenzoni, L.L.; Hofer, D.; Solderer, A.; Wiedemeier, D.; Attin, T.; Schmidlin, P.R. Origin of MMP-8 and Lactoferrin levels from gingival crevicular fluid, salivary glands and whole saliva. BMC Oral Health 2021, 21, 385. [Google Scholar] [CrossRef]
- Rosa, L.; Lepanto, M.S.; Cutone, A.; Ianiro, G.; Pernarella, S.; Sangermano, R.; Musci, G.; Ottolenghi, L.; Valenti, P. Lactoferrin and oral pathologies: A therapeutic treatment. Biochem. Cell Biol. 2021, 99, 81–90. [Google Scholar] [CrossRef]
- Sangermano, R.; Pernarella, S.; Straker, M.; Lepanto, M.S.; Rosa, L.; Cutone, A.; Valenti, P.; Ottolenghi, L. The treatment of black stain associated with of iron metabolism disorders with lactoferrin: A litterature search and two case studies. Clin. Ter. 2019, 170, e373–e381. [Google Scholar]
- Superti, F.; De Seta, F. Warding Off Recurrent Yeast and Bacterial Vaginal Infections: Lactoferrin and Lactobacilli. Microorganisms 2020, 8, 130. [Google Scholar] [CrossRef] [Green Version]
- Moreau, M.C.; Duval-Iflah, Y.; Muller, M.C.; Raibaud, P.; Vial, M.; Gabilan, J.C.; Daniel, N. Effect of orally administered bovine lactoferrin and bovine IgG on the establishment of Escherichia coli in the digestive tract of gnotobiotic mice and human newborn infants. Ann. Microbiol. (Paris) 1983, 134B, 429–441. [Google Scholar] [PubMed]
- Hao, Y.; Wang, J.; Teng, D.; Wang, X.; Mao, R.; Yang, N.; Ma, X. A prospective on multiple biological activities of lactoferrin contributing to piglet welfare. Biochem. Cell Biol. 2021, 99, 66–72. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, D.N.; Jiang, P.-P.; Stensballe, A.; Bendixen, E.; Sangild, P.T.; Chatterton, D.E. Bovine lactoferrin regulates cell survival, apoptosis and inflammation in intestinal epithelial cells and preterm pig intestine. J. Proteom. 2016, 139, 95–102. [Google Scholar] [CrossRef] [PubMed]
- Nguyen, D.N.; Li, Y.; Sangild, P.T.; Bering, S.B.; Chatterton, D.E.W. Effects of bovine lactoferrin on the immature porcine intestine. Br. J. Nutr. 2013, 111, 321–331. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Garcia, C.; Duan, R.D.; Brévaut-Malaty, V.; Gire, C.; Millet, V.; Simeoni, U.; Bernard, M.; Armand, M. Bioactive compounds in human milk and intestinal health and maturity in preterm newborn: An overview. Cell. Mol. Biol. 2013, 59, 108–131. [Google Scholar]
- Kruzel, M.L.; Actor, J.K.; Radak, Z.; Bacsi, A.; Saavedra-Molina, A.; Boldogh, I. Lactoferrin decreases LPS-induced mitochondrial dysfunction in cultured cells and in animal endotoxemia model. Innate Immun. 2009, 16, 67–79. [Google Scholar] [CrossRef] [Green Version]
- Tursi, A.; Elisei, W.; Brandimarte, G.; Giorgetti, G.M.; Modeo, M.E.; Aiello, F. Effect of lactoferrin supplementation on the effectiveness and tolerability of a 7-day quadruple therapy after failure of a first attempt to cure Helicobacter pylori infection. Med. Sci. Monit. 2007, 13, CR187–CR190. [Google Scholar]
- Zhang, Z.; Lu, M.; Chen, C.; Tong, X.; Li, Y.; Yang, K.; Lv, H.; Xu, J.; Qin, L. Holo-lactoferrin: The link between ferroptosis and radiotherapy in triple-negative breast cancer. Theranostics 2021, 11, 3167–3182. [Google Scholar] [CrossRef]
- Yin, C.M.; Wong, J.H.; Xia, J.; Ng, T.B. Studies on anticancer activities of lactoferrin and lactoferricin. Curr. Protein Pept. Sci. 2013, 14, 492–503. [Google Scholar] [CrossRef]
- Arias, M.; Hilchie, A.L.; Haney, E.F.; Bolscher, J.G.M.; Hyndman, M.E.; Hancock, R.E.W.; Vogel, H.J. Anticancer activities of bovine and human lactoferricin-derived peptides. Biochem. Cell Biol. 2017, 95, 91–98. [Google Scholar] [CrossRef] [Green Version]
- Ma, J.; Guan, R.; Shen, H.; Lu, F.; Xiao, C.; Liu, M.; Kang, T. Comparison of anticancer activity between lactoferrin nanoliposome and lactoferrin in Caco-2 cells in vitro. Food Chem. Toxicol. 2013, 59, 72–77. [Google Scholar] [CrossRef] [PubMed]
- Abad, I.; Conesa, C.; Sánchez, L. Development of Encapsulation Strategies and Composite Edible Films to Maintain Lactoferrin Bioactivity: A Review. Materials 2021, 14, 7358. [Google Scholar] [CrossRef]
- Aguilar-Pérez, K.M.; Avilés-Castrillo, J.I.; Medina, D.I.; Parra-Saldivar, R.; Iqbal, H.M.N. Insight Into Nanoliposomes as Smart Nanocarriers for Greening the Twenty-First Century Biomedical Settings. Front. Bioeng. Biotechnol. 2020, 8, 579536. [Google Scholar] [CrossRef] [PubMed]
- Guan, R.; Ma, J.; Wu, Y.; Lu, F.; Xiao, C.; Jiang, H.; Kang, T. Development and characterization of lactoferrin nanoliposome: Cellular uptake and stability. Nanoscale Res. Lett. 2012, 7, 679. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Liu, W.; Ye, A.; Liu, W.; Liu, C.; Singh, H. Stability during in vitro digestion of lactoferrin-loaded liposomes prepared from milk fat globule membrane-derived phospholipids. J. Dairy Sci. 2013, 96, 2061–2070. [Google Scholar] [CrossRef] [PubMed] [Green Version]
Publisher’s Note: MDPI stays neutral with regard to jurisdictional claims in published maps and institutional affiliations. |
© 2022 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (https://creativecommons.org/licenses/by/4.0/).